Dear Editor,
We report a case of a patient who suffers from hypersensitivity pneumonitis (HP) due to bird exposure, for whom the use of a FFP2 mask has proven to be an effective therapeutic measure.
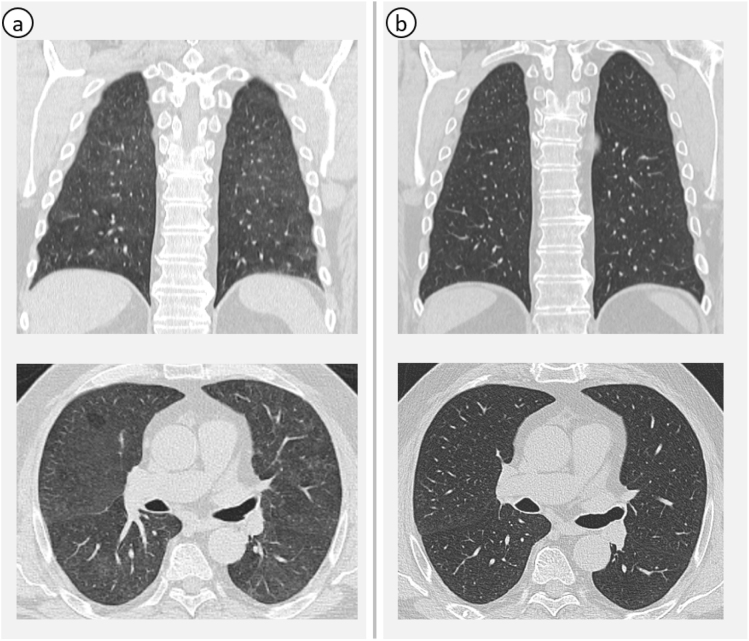
The patient is a 66-year-old male with absence of tobacco habit but who has been exposed to birds because he is a breeder and a bird shop owner. Due to suffering from dyspnea and nonproductive cough during the previous 3 weeks, the patient decided to go to Hospital. The pulmonary auscultation revealed bilateral crackles and complementary diagnostic exams were performed. The computed tomography (CT) of the thorax showed diffuse centrilobular nodules and air-trapping (Fig. 1a). Respiratory function tests (RFT) showed a decrease in both, forced vital capacity and carbon monoxide diffusion (FVC 72%, DLCO 51%). Serological tests were carried out and confirmed the presence of specific IgG antibodies against avian antigens. The patient, based on the latest classification of ATS/JRS/ALAT HP guidelines, was diagnosed with moderate confidence of HP, based on antigen exposure, clinical and radiologic features.1 This case was assessed by the ILD multidisciplinary committee, supporting the diagnosis of HP without conducting other diagnosis test, as bronchoalveolar lavage (BAL) or lung biopsy. The patient was skeptical that birds were causing his illness, therefore his exposure to birds did not cease. He received corticosteroids therapy (prednisone 40 mg initially, with progressive decrease) during 4 months with little response. When COVID-19 pandemic began, the patient started using FFP2 masks while working at the bird shop, with a significant improvement of symptoms. During the follow-up, a chest CT and RFT were carried out, showing a normal RFT (FVC 80%, DLCO 83%) and the disappearance of the centrilobular pattern and air-trapping (Fig. 1b).
Fig. 1.
Thorax CT (coronal and axial images). (a) Centrilobular nodules and air-trapping, suggesting non-fibrotic HP. (b) Disappearance of the radiological pattern of HP, after using FFP2 mask.
The principal aim of this report is to highlight the importance of removing the exposure to the inciting antigen, as it is the main responsible for the development of the HP, and also, for its maintenance.
HP is an interstitial lung disease (ILD) caused by exposure to an inhaled antigen in susceptible individuals, who develop an exaggerated immune response. In the latest guidelines, HP is divided into fibrotic and non-fibrotic forms. The radiological findings of non-fibrotic HP are small, ill-defined centrilobular nodules, air-trapping, and ground glass opacities with a patchy distribution (mosaic attenuation). Fibrotic HP may manifest as traction bronchiectasis, loss of volume or honeycombing. In some cases, it may be necessary to carry out additional tests such as BAL and lung biopsy. A BAL lymphocyte count >30% is associated with HP, but its absence does not exclude it.1, 2, 3 In our case, according to the recommendation of 2021 CHEST guidelines and the assessment of the ILD multidisciplinary committee of our center, BAL was unnecessary because of high pre-test probability of HP, which was based on the exposure history, the clinical onset and the radiological pattern.2 However, the ATS/JRS/ALAT HP guidelines always recommends performing the BAL.1
The most important treatment is the withdrawal of antigenic exposure.4 In our case, the patient refused to cease contact with birds. However, by using a FPP2 mask during working hours, he improved. The use of a respiratory protection mask has been identified for years as a measure to avoid exposition.5 In 1965, Reed et al. reported the case of a patient who continued handling his birds using a “protective mask”, without clinical worsening.6 We would like to emphasize the critical role of FFP2 mask in this patient, which may suggest an alternative to avoid the antigen for people who cannot cease direct exposure definitely.
In cases of non-fibrotic HP, patients with normal RFT or mild impairment, it is enough to remove the inciting antigen with a close follow-up. However, corticosteroids or immunosuppressive therapy (as azathioprine, mycophenolate mofetil or rituximab) should be considered in cases of severe lung function impairment or progressive disease. Once HP becomes fibrotic, antifibrotic therapy may be required.3
To conclude, with this report we highlight the importance of antigen avoidance in HP, to improve outcomes. The antigen exposure is a trigger of development and progression of HP, and the inability to remove it is considered as a risk factor for ILD progression and mortality. In case this is not possible, other tools, as FFP2 can be helpful and an effective therapeutic measure.
Informed consent
This consent has been obtained.
Funding
We declare that no funding was received for this article.
Authors’ contributions
All the authors mentioned in the manuscript have participated and supported the elaboration of the manuscript.
Conflicts of interest
None declared.
References
- 1.Raghu G., Remy-Jardin M., Ryerson C.J., Myers J.L., Kreuter M., Vasakova M., et al. Diagnosis of hypersensitivity pneumonitis in adults: an official ATS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2020;202:e36–e69. doi: 10.1164/rccm.202005-2032ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fernández Pérez E.R., Travis W.D., Lynch D.A., Brown K.K., Johannson K.A., Selman M., et al. Diagnosis and evaluation of hypersensitivity pneumonitis. Chest. 2021;160:e97–e156. doi: 10.1016/j.chest.2021.03.066. [DOI] [PubMed] [Google Scholar]
- 3.Hamblin M., Prosch H., Vašáková M. Diagnosis, course and management of hypersensitivity pneumonitis. Eur Respir Rev. 2022;31:210169. doi: 10.1183/16000617.0169-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nishida T., Kawate E., Ishiguro T., Kanauchi T., Shimizu Y., Takayanagi N. Antigen avoidance and outcome of nonfibrotic and fibrotic hypersensitivity pneumonitis. ERJ Open Res. 2022;8 doi: 10.1183/23120541.00474-2021. 00474-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hendrick D.J., Marshall R., Faux J.A., Krall J.M. Protective value of dust respirators in extrinsic allergic alveolitis: clinical assessment using inhalation provocation tests. Thorax. 1981;36:917–921. doi: 10.1136/thx.36.12.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reed C.E., Sosman A., Barbee R.A. Pigeon-breeders’ lung. A newly observed interstitial pulmonary disease. JAMA. 1965;193:261–265. doi: 10.1001/jama.1965.03090040005001. [DOI] [PubMed] [Google Scholar]