Abstract
Anterior shoulder dislocation (ASD) is the most common type of dislocation presented to the emergency department (ED) with severe pain and limitation of range of movement. Procedural sedation and analgesia are commonly used for ASD, but regional techniques are gaining popularity. Interscalene brachial plexus block is effective but has several limitations. Suprascapular nerve block (SSNB) has been explored for this indication. The SSNB is commonly performed using the posterior approach in a sitting position and can be technically difficult in dislocated patients. Recently, anterior subomohyoid approach performed in the lower neck has been described but has not yet been reported in the ED. We, hereby, report our experience of using low-volume ultrasound-guided anterior SSNB for procedural analgesia in 10 patients with ASD.
Keywords: Anterior shoulder dislocation, emergency department, pain, suprascapular nerve
Introduction
Acute anterior shoulder dislocation (ASD) is the most common type of dislocation presented to the emergency department (ED).[1] ASD is usually associated with severe pain and discomfort, and the delay in reduction may lead to a number of acute and chronic complications.[2] The reduction of ASD is mostly achieved under procedural analgesia (PA) and sedation which obtund the patient’s consciousness and can be detrimental in ED.[3] The regional analgesia (RA) techniques, including nerve blocks, are the safer alternatives and gaining increasing acceptance in ED settings for PA.[4] Interscalene brachial plexus block (ISBPB) is the standard RA technique used for ASD.[5,6] However, the ISBPB is invariably associated with phrenic nerve (PN) palsy and can be detrimental to patients with a limited respiratory reserve, thereby undesirable in ED settings.[4-6] The suprascapular nerve (SSN) is a terminal branch of the brachial plexus which provides a major sensory supply (up to 75%) to the shoulder joint.[7] A suprascapular nerve block (SSNB) can provide effective analgesia comparable to ISBPB without the risk of PN palsy.[7] Both anterior and posterior approaches can be undertaken for SSNB, few reports that exist on the use of SSNB in the ED have focused on the posterior approach.[7-9] The anterior technique, however, remains underutilized in ED settings for this indication, and there is a paucity of literature in this regard. We describe the use of the anterior subomohyoid approach of SSNB using a low volume of local anesthetic (LA) for PA for 10 patients presented to the ED with ASD.
Case Report
Ten patients presenting to our ED with an ASD were explained about potential analgesic modalities to reduce the dislocation. Patients with suspected neurological deficits and any preexisting respiratory diseases were excluded from SSNB. The patients were prepared for the block in the procedure room after applying standard monitors and keeping the resuscitation drugs and equipment ready. The SSNBs were performed under aseptic conditions with a high-frequency linear probe (5–13 Hz) which was placed transversely above the clavicle to visualize the supraclavicular brachial plexus and then traced toward the cricoid at the interscalene level to locate the cervical nerve roots C5, C6 (splitting into two), and C7 [Figure 1a]. The C5 nerve root is traced laterally to locate a branch beneath the inferior belly of the omohyoid [Figure 1b]. The LA 1% lignocaine was infiltrated around the nerve by inserting a nerve block needle inplane to the transducer probe from the lateral to the medial side. The baseline pain score and pain score 10 min after the block was recorded in the Numerical Rating Scale (NRS). The patients’ demographic variables and clinical profiles are depicted in Table 1. All the patients were monitored for 1 h after the block for any adverse effects. The mean age of the patients was 34.8 ± 11.69 years, and all were male patients. The mean duration of presentation to ED after dislocation was 4.0 ± 1.88 h. The mean baseline pain score in NRS was 9.3 ± 0.82. The mean pain score at 10 min postblock was 3.3 ± 0.67. The mean volume of lignocaine required for the nerve block was 4.2 ± 1.68 ml. Successful reduction was done in all the cases without any need for rescue analgesics. All patients were discharged on oral analgesics the same day, and the mean pain score at the time of discharge was 2.2 ± 0.91. None of the patients suffered any block-related complications or were readmitted for any complications. Written informed consent was obtained from all the patients included in this case series.
Figure 1.
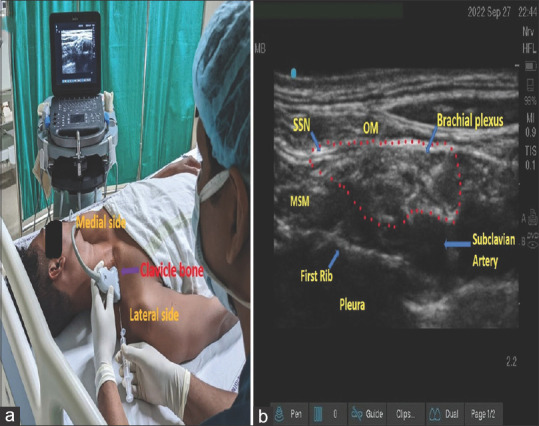
(a) Linear probe position in supraclavicular fossa; (b) Sonoanatomy showing SSN. SSN: Suprascapular nerve, OM: Omohyoid muscle, MSM: Middle scalene muscle
Table 1.
Demographic and clinical profile of patients presented with shoulder dislocation (n=10)
| Age (years)/sex | Type of ASD | Duration after dislocation (h) | Pain score in NRS (baseline) | Pain score in NRS after 10 min of block | The volume of LA drugs used (ml) | Pain score in NRS at discharge |
|---|---|---|---|---|---|---|
| 40/male | Right | 5 | 10 | 3 | 8 | 2 |
| 32/male | Right | 2 | 10 | 3 | 5 | 1 |
| 42/male | Left | 3 | 10 | 4 | 5 | 2 |
| 32/male | Left | 4 | 9 | 3 | 4 | 3 |
| 36/male | Right | 6 | 8 | 4 | 4 | 2 |
| 29/male | Right | 8 | 10 | 3 | 3 | 4 |
| 22/male | Right | 3 | 9 | 4 | 3 | 1 |
| 62/male | Right | 4 | 8 | 2 | 3 | 2 |
| 32/male | Right | 2 | 10 | 4 | 3 | 2 |
| 21/male | Left | 3 | 9 | 3 | 3 | 3 |
LA: Local anesthesia, NRS: Numerical Rating Scale, ASD: Anterior shoulder dislocation
Discussion
Shoulder joints can be dislocated anteriorly, posteriorly, and inferiorly, but ASD is the most common.[1] Various techniques for PA during the reduction of ASD have been reported in the literature.[2,3] Systemic analgesia can be provided by intravenous procedural sedation (midazolam, fentanyl, and remifentanil) and Entonox.[3] However, these techniques obtund the patient’s consciousness and protective airway reflexes and often delay the recovery.[3] RA has the edge over PA since it provides effective pain relief and is devoid of systemic side effects. The nerve block techniques for the reduction of ASD include ISBPB, supraclavicular brachial plexus block, intra-articular LA infiltration, and SSNB.[1] Although ISBPB is the most effective regional anesthesia technique, its use is under scrutiny in view of the high incidence of diaphragmatic palsy, possible neurological deficits, and other serious adverse effects.[3] Hemidiaphragmatic palsy can increase the length of stay and is undesirable for ED patients.[6,10] The major critical structures such as the spinal canal, pleura, and vertebral artery in the vicinity can be injured during ISBPB.[4,6]
The SSNB was first described in 1941 by Wertheim and Rovenstein to treat severe chronic shoulder pathology.[11] SSN arises from the upper trunk (C5 and C6) at the level of the inferior belly of the omohyoid and travels toward the superior border of the scapula.[12] Conventionally, the SSN was blocked by the posterior approach at the suprascapular notch.[7-9] Recently, the anterior subomohyoid approach has been described, where it is accessed proximally at the point, and where it branches off from the superior trunk just lateral to the supraclavicular brachial plexus below the inferior belly of the omohyoid muscle.[10] It has been suggested that the many articular branches of the SSN have already innervated the shoulder joint before it reaches the suprascapular notch.[10,12] Hence, the posterior approach may not be as effective as the anterior approach, although there is no head-to-head comparison. Considering the effective pain relief achieved in all 10 patients after the use of a low dose of LA in anterior SSNB, the approach can be a promising option for PA in these cases. Furthermore, since the block site at the subomohyoid level is far away from the PN and major vessels, the chances of PN block and local anesthesia systemic toxicity (LAST) are practically very low with a low-dose LA.[6,10,12,13] Thus, SSNB can be safer compared to proximal plexus blocks such as ISBPB in high-risk cases with pulmonary pathologies, multiple comorbidities, obesity, and increased age.[4,6]
SSNB is less commonly reported in the ED for shoulder procedures despite its favorable side effect profile.[7-9] Hassen et al. reported a reduction of ASD in a 66-year-old female under the SSNB.[7] Authors documented a shorter length of ED stay as compared to those receiving sedation.[7] Tezel et al. compared the SSNB to procedural sedation in a randomized trial enrolling 41 patients.[8] There was no difference in the success of reduction or patient satisfaction, but the stay in ED got significantly decreased.[8] In our series also, all the patients could be discharged on a day care basis within a few hours of admission and without any adverse effects. Kaya et al. conducted this block in a case with recurrent ASD, and pain in the visual analog scale decreased from 95 to 45.[14] In our series also, a reduction in the mean NRS from around 9.3–3.3 (i.e., six points) was noted. Herring et al. conducted the SSNB for adhesive capsulitis in ED and could successfully do shoulder manipulation procedure.[9] All these previous reports utilized the posterior approach to SSNB, whereas in our series, we have explored the anterior approach to SSNB.[7-9]
In traumatic ASD, there is a distortion of shoulder anatomy in addition to local tissue edema that complicates the posterior SSNB approach due to poor sonoanatomy and that makes the conditions difficult due to the deeper structures.[1,2] The anterior approach is superficial and technically easier. The LA volume typically used for the posterior approach is 10–15 ml.[8,9] In contrast, comparatively less volume of LA (mean 4.2 ml) can achieve the desired effect in the anterior approach as demonstrated in our report.[6] In our initial experiences, we used 8 ml of 1% lignocaine which was brought down to 3 ml under ultrasound guidance in our most recent blocks and resulted in effective analgesia. The low-dose LA can minimize the chances of the LAST.[10,13] Using lignocaine has an advantage rather than using a long-acting LA or a combination of both.[13] Furthermore, the anterior approach can be performed in a supine position, whereas the posterior approach requires a sitting position which may not be possible or uncomfortable for many trauma patients.
Conclusion
This case series highlights the role of anterior SSNB in providing effective PA for ASD reduction using low concentration and volume of LA under ultrasound guidance. The low-dose LA can minimize the chances of PN involvement and LAST. Considering the favorable risk-benefit profile of this technique, SSNB should be further explored in ED for this indication.
Conflicts of interest
Not declared.
Consent to participate
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Funding
None declared.
References
- 1.Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am. 2010;92:542–9. doi: 10.2106/JBJS.I.00450. [DOI] [PubMed] [Google Scholar]
- 2.Perron AD, Ingerski MS, Brady WJ, Erling BF, Ullman EA. Acute complications associated with shoulder dislocation at an academic Emergency Department. J Emerg Med. 2003;24:141–5. doi: 10.1016/s0736-4679(02)00717-5. [DOI] [PubMed] [Google Scholar]
- 3.Godwin SA, Burton JH, Gerardo CJ, Hatten BW, Mace SE, Silvers SM, et al. Clinical policy:procedural sedation and analgesia in the emergency department. Ann Emerg Med. 2014;63:247–58. doi: 10.1016/j.annemergmed.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 4.Mohanty CR, Varghese JJ, Panda R, Sahoo S, Mishra TS, Radhakrishnan RV, et al. Ultrasound-guided selective peripheral nerve block compared with the sub-dissociative dose of ketamine for analgesia in patients with extremity injuries. Am J Emerg Med. 2023;63:94–101. doi: 10.1016/j.ajem.2022.10.020. [DOI] [PubMed] [Google Scholar]
- 5.Ghodki PS, Singh ND. Incidence of hemidiaphragmatic paresis after peripheral nerve stimulator versus ultrasound guided interscalene brachial plexus block. J Anaesthesiol Clin Pharmacol. 2016;32:177–81. doi: 10.4103/0970-9185.168263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mohanty CR, Singh N, Das S, Radhakrishnan RV. Re: Ultrasound-guided interscalene block versus intravenous analgesia and sedation for reduction of first anterior shoulder dislocation. Am J Emerg Med. 2022;58:347–8. doi: 10.1016/j.ajem.2022.04.015. [DOI] [PubMed] [Google Scholar]
- 7.Hassen GW, Bergmann-Dumont D, Duvvi A, Sudol S, Choy D, Yeo T, et al. The use of a suprascapular nerve block to facilitate the reduction of an anterior shoulder dislocation: An alternative for elderly and patients with cardiopulmonary comorbidities? J Emerg Med. 2022;63:265–71. doi: 10.1016/j.jemermed.2022.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Tezel O, Kaldirim U, Bilgic S, Deniz S, Eyi YE, Ozyurek S, et al. Acomparison of suprascapular nerve block and procedural sedation analgesia in shoulder dislocation reduction. Am J Emerg Med. 2014;32:549–52. doi: 10.1016/j.ajem.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 9.Herring AA, Stone MB, Nagdev A. Ultrasound-guided suprascapular nerve block for shoulder reduction and adhesive capsulitis in the ED. Am J Emerg Med. 2011;29:3. doi: 10.1016/j.ajem.2010.08.024. e1-3. [DOI] [PubMed] [Google Scholar]
- 10.Abdallah FW, Wijeysundera DN, Laupacis A, Brull R, Mocon A, Hussain N, et al. Subomohyoid anterior suprascapular block versus interscalene block for arthroscopic shoulder surgery: A multicenter randomized trial. Anesthesiology. 2020;132:839–53. doi: 10.1097/ALN.0000000000003132. [DOI] [PubMed] [Google Scholar]
- 11.Milowsky J, Rovenstine EA. Suprascapular nerve block;evaluation in the therapy of shoulder pain. Anesthesiology. 1949;10:76–81. doi: 10.1097/00000542-194901000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Tran J, Peng PWH, Agur AMR. Anatomical study of the innervation of glenohumeral and acromioclavicular joint capsules:implications for image-guided intervention. Reg Anesth Pain Med. 2019:1–7. doi: 10.1136/rapm-2018-100152. [DOI] [PubMed] [Google Scholar]
- 13.Mohanty CR, Radhakrishnan RV, Singh N, Shaji IM. Re: Why ethyl chloride spray in arterial blood gas sampling? Am J Emerg Med. 2022;62:113–4. doi: 10.1016/j.ajem.2022.08.020. [DOI] [PubMed] [Google Scholar]
- 14.Kaya M, Eksert S, Akay S, Kantemir A, Keklikci K. Interscalene or suprascapular block in a patient with shoulder dislocation. Am J Emerg Med. 2017;35:195. doi: 10.1016/j.ajem.2016.06.103. e1-3. [DOI] [PubMed] [Google Scholar]


