Abstract
Introduction:
The scaphoid fracture is the most common type of carpal fracture, and disruption of the proximal row of carpal bones alters wrist mechanics altering the stabilization that permits the wrist to work efficiently. When the displacement is at least 2 mm, the majority of surgeons would preferentially operatively intervene in this fracture. Non-union of the fracture will occur when left untreated. The gold standard for treatment is open reduction and internal fixation using autologous bone graft. This case report is the first to describe the integration of the Hintermann™ Distractor, used as an integral part of the surgery in scaphoid waist fracture fixation to improve fracture stabilization, preparation, and compression.
Case Report:
A 20-year-old male presented with a volar flexed scaphoid non-union, 4 months after the initial injury. Open reduction internal fixation, with the use of the Hintermann™ Distractor, facilitated ease of reduction and placement of Russe graft.
Conclusion:
Scaphoid waist non-unions with volar angulation and an associated DISI deformity can lead to a significant decrease in function. This case study is the first to describe the use of a foot and ankle instrument to assist with fracture preparation and distraction to place a corticocancellous strut graft in the scaphoid fracture efficiently. This case study demonstrates the efficiency of the technique.
Keywords: Foot & Ankle, Hintermann, Integration
Learning Point of the Article:
Tools outside a surgeon‘s armamentarium may prove to be a very beneficial treatment for the patient.
Introduction
Scaphoid fractures and non-unions are the most common types of carpal fractures, and their annual incidence is approximately 4.3/10,000 people mainly occurring in young active males [1]. These types of fractures typically occur when falling on an outstretched hand with the wrist extended [2]. It is considered displaced when there is a gap of 1 mm within the fracture [3]. Disruption of the proximal row of carpal bones alters wrist mechanics altering the stabilization that permits the wrist to work efficiently [2]. Loss of radial stabilization leads to the resultant collapse of the carpus into an extension instability pattern, with the lunate tilted dorsally [4]. When the displacement is at least 2 mm or a volar flexed deformity, the majority of surgeons would preferentially operatively intervene to stabilize this fracture [2]. Acute treatment of fractures and non-unions is thought to accelerate the return to normal function, but it does expose the patient to surgical risks [2, 5, 6, 7]. Surgical treatment does avoid the stiffness associated with cast treatment and significantly reduces the incidence of non-union and malunion in the scaphoid bone [8, 9, 10, 11, 12].
One of the standard treatments for a volar flexed scaphoid waist fracture or a non-union is open reduction and internal fixation using an autologous bone graft [13, 14, 15, 16]. Restoration of scaphoid length and correction of the flexed deformity with the insertion of a bone graft wedge can restore carpal alignment and restore function [4]. There is no literature on the use of the foot and ankle instrument, the Hintermann™ Distractor, to treat scaphoid waist fractures. A clinical image depicting the instrument can be seen in Fig. 1. The only literature of reference where it is used outside of foot and ankle surgery is described in a distal radius osteotomy technique [17]. Hence, this case report is the first to describe the integration of the Hintermann™ Distractor, used as an integral part of the surgery in scaphoid waist fracture fixation to improve fracture preparation and distraction.
Figure 1.

Hintermann™ device.
The patient was informed that data concerning the case would be submitted for publication, and he provided consent.
Case Report
The patient is a 20-year-old, non-smoker, non-diabetic, active male with a body mass index of 24 who sustained a scaphoid fracture secondary to falling off his bike. This injury occurred in his non-dominant hand. The patient was initially treated conservatively and then referred by his primary care physician for a consult with the subspecialized hand orthopedic surgeon.
The patient sustained the injury approximately 4 months before the consultation. He went on to develop a symptomatic non-union of the scaphoid with carpal collapse. Initial consultation radiographs were obtained, demonstrated in Fig. 2. The standard scaphoid view of the wrist demonstrates a volar flexed fracture of the middle third of the scaphoid bone with displacement.
Figure 2.

Pre-operative scaphoid view of the left wrist.
The patient described the pain as 5 out of 10 for severity, and “sharp” in nature. He had point tenderness over the anatomic snuffbox. There was no surrounding erythema or ecchymosis of note. The working diagnosis was a closed left displaced non-union of the middle third of the scaphoid and carpal collapse of the left wrist. The tentative plan was to obtain a computed tomography (CT) of the left wrist to further evaluate and preoperatively plan.
Standard CT with 1 mm cuts was obtained, and different slices are demonstrated here in Fig. 3. The axial slice demonstrates the severity of the displacement. The results were thoroughly discussed with the patient, and the collective plan was determined to proceed with surgery.
Figure 3.
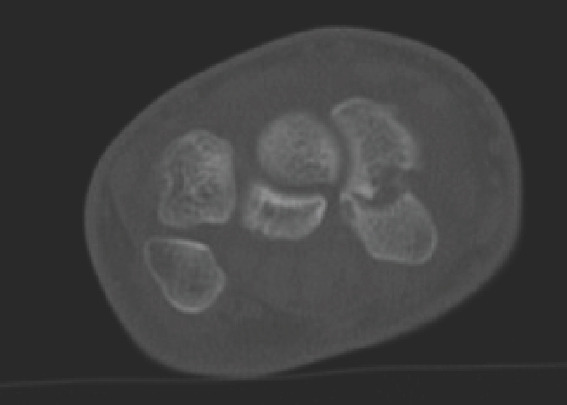
Axial CT view of the left wrist.
The patient was placed in the supine position, and the operative extremity was prepped and draped in an orthopedic sterile fashion. We proceeded with the standard volar approach to the scaphoid. The incision was centered over the flexor carpi radialis (FCR) tendon, beginning 4 cm proximal to the wrist crease. At the wrist crease, the incision was angled radially towards the scapho-trapezial joint. After sharp dissection was carried out and hemostasis was obtained, the tendon sheath of the FCR was sharply dissected and the tendon was retracted radially. The deep fascia of the sheath was then exposed, and sharp dissection was carried out to split the fibers. A bump was used to extend and ulnarly deviate the wrist to fully expose the scaphoid. The capsule was then sharply dissected obliquely in line longitudinally with the bone.
After the fracture was visualized, a 0.062 K-wire was placed perpendicularly to the long access of the scaphoid into the proximal and distal fragments of the scaphoid. The Hintermann™ Distractor was then utilized to distract the fracture site at this point. Curettage was then performed on both the proximal and distal aspects of the fracture to remove any fibrous tissue down to the bleeding subchondral bone. The autologous corticocancellous bone graft from the distal radius was then fashioned at the fracture site. The Hintermann™ Distractor was then utilized to compress the fracture after an adequate autologous bone graft was placed in the fracture site. This foot and ankle device very efficiently distracted, compressed, and maintained reduction for this unique fracture. Standard views were obtained using the intra-operative fluoroscopic machine. The lateral is depicted in Fig. 4, demonstrating near anatomic alignment.
Figure 4.

Intra-operative lateral fluoroscopic image using the device.
Then a 0.045 K-wire was placed longitudinally across the fracture site, drilled in standard fashion, and measured. The appropriately sized headless compression was placed across the fracture site. Multiple fluoroscopic views were obtained to confirm maintained reduction and no extrusion of hardware. The wound was irrigated and closed, and the patient was placed in a short thumb spica splint until follow-up.
The patient presented 7 days after surgery for the first post-operative visit. New radiographs were obtained to assess fixation as shown in Fig. 5. The scaphoid views demonstrate maintained reduction and no signs of hardware failure.
Figure 5.

Post-operative scaphoid view of the left wrist.
The patient now described the pain as 2 out of 10 for severity, with only mild irritation around suture sites. The patient was otherwise distally neurovascularly intact on an exam. The patient demonstrated disabilities of the arm, shoulder, and hand (QuickDASH) score of 35.25 on this visit. The patient was transitioned to a removable thumb spica brace, and a follow-up appointment was scheduled for 3 months later.
Discussion
The majority of hand surgeons have come to a consensus that volar flexed scaphoid fractures and non-unions should be operatively treated [14, 18, 19, 20]. The goal is to provide pain relief, improve hand and wrist function, and prevent osteoarthritis [21]. New literature is demonstrating that non-vascularized bone grafting material has comparable outcomes to vascularized bone graft [21], and recent meta-analysis demonstrates excellent union rates when scaphoid non-unions are treated operatively with bone grafting and rigid fixation [22]. Moreover, any tool that may provide a mechanical advantage to prepare the fracture, provide stabilization, and compress the fracture could prove to be very advantageous in the fixation of scaphoid fractures.
This patient presented months after his initial injury with increased pain and a significant decrease in the function of the wrist. The scaphoid bone plays a pivotal role in stability and function, so restoring its normal kinetics is crucial [23]. When preoperatively planning for the treatment of an acutely flexed deformity or non-union in a scaphoid waist fracture, the discussion is between open versus percutaneous fixation, dorsal versus volar approach, and non-vascularized versus vascularized bone graft options. Open reduction and internal fixation have been shown to significantly lower the incidence of non-unions in scaphoid fracture fixation [8]. The main advantage of the volar approach is better visualization for fracture fixation in waist-type morphologic fractures [23].
As with any anatomic fracture reduction, it is important to remove any fibrotic tissue to prepare the fracture site. The senior author recommended using the Hintermann™ Distractor to assist with fracture preparation. It allowed for control in multiple planes while gapping the fracture site for preparation in an efficient manner. It also assisted with controlled compression after the bone graft was placed in the fracture site to promote union. And finally, it stabilized the provisional fixation while a compression screw was placed. Overall, it efficiently facilitated a successful preparation and reduction of the scaphoid fracture.
This case study attempts to introduce a new technique for scaphoid fracture fixation, which is not yet performed in hospitals elsewhere. Current techniques, using K-wires, do not have the control that the Hintermann™ Distractor affords intraoperatively. The success with the integration of specific foot and ankle instruments into hand surgery, especially in scaphoid waist fractures, may prove to be alternatives to assist surgeons in fracture preparation and fixation.
The only limitation of this study is the lack of long-term outcomes and time-to-union results. However, this case report introduces novel technique pearls to assist in scaphoid waist fracture preparation and fixation to promote better outcomes.
Conclusion
Scaphoid waist non-unions with volar angulation and an associated DISI deformity can lead to a significant decrease in function. This case study is the first to describe the use of a foot and ankle instrument to assist with fracture preparation and distraction to place a corticocancellous strut graft in the scaphoid fracture efficiently. This case study demonstrates the efficiency of the technique.
Clinical Message.
Pre-operative planning with an open mind can lead to improved treatment options for the patient.
Biography

Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Elgayar L, Elmajee M, Aljawadi A, Abdelaal A, Khan S, Pillai A. A systematic review of mechanical stabilization by screw fixation without bone grafting in the management of stable scaphoid non-union. J Clin Orthop Trauma. 2021;17:112–7. doi: 10.1016/j.jcot.2021.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dias JJ, Brealey SD, Fairhurst C, Amirfeyz R, Bhowal B, Blewitt N, et al. Surgery versus cast immobilisation for adults with a bicortical fracture of the scaphoid waist (SWIFFT):A pragmatic, multicentre, open-label, randomised superiority trial. Lancet. 2020;396:390–401. doi: 10.1016/S0140-6736(20)30931-4. [DOI] [PubMed] [Google Scholar]
- 3.Dias JJ, Singh HP. Displaced fracture of the waist of the scaphoid. J Bone Joint Surg Br. 2011;93:1433–9. doi: 10.1302/0301-620X.93B11.26934. [DOI] [PubMed] [Google Scholar]
- 4.Bindra R, Bednar M, Light T. Volar wedge grafting for scaphoid nonunion with collapse. J Hand Surg Am. 2008;33:974–9. doi: 10.1016/j.jhsa.2008.04.024. [DOI] [PubMed] [Google Scholar]
- 5.Mack GR, Bosse MJ, Gelberman RH, Yu E. The natural history of scaphoid non-union. J Bone Joint Surg Am. 1984;66:504–9. [PubMed] [Google Scholar]
- 6.Grewal R, King GJ. An evidence-based approach to the management of acute scaphoid fractures. J Hand Surg Am. 2009;34:732–4. doi: 10.1016/j.jhsa.2008.12.027. [DOI] [PubMed] [Google Scholar]
- 7.Hegazy G, Alshal E, Abdelaal M, Abdelaziz M, Moawad M, Saqr YM, et al. Kirschner wire versus Herbert screw fixation for the treatment of unstable scaphoid waist fracture nonunion using corticocancellous iliac bone graft:Randomized clinical trial. Int Orthop. 2020;44:2385–93. doi: 10.1007/s00264-020-04730-7. [DOI] [PubMed] [Google Scholar]
- 8.Li H, Guo W, Guo S, Zhao S, Li R. Surgical versus nonsurgical treatment for scaphoid waist fracture with slight or no displacement:A meta-analysis and systematic review. Medicine (Baltimore) 2018;97:e13266. doi: 10.1097/MD.0000000000013266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gutow AP. Percutaneous fixation of scaphoid fractures. J Am Acad Orthop Surg. 2007;15:474–85. doi: 10.5435/00124635-200708000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Bedi A, Jebson PJ, Hayden RJ, Jacobson JA, Martus JE. Internal fixation of acute, nondisplaced scaphoid waist fractures via a limited dorsal approach:An assessment of radiographic and functional outcomes. J Hand Surg Am. 2007;32:326–33. doi: 10.1016/j.jhsa.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 11.Deghani M, Nekoei F, Fatahi F, Teimouri M. Comparative study of results and complications of three methods in treatment of scaphoid fractures. J Isfahan Med Sch. 2010;28:408–15. [Google Scholar]
- 12.Ring D, Jupiter JB, Herndon JH. Acute fractures of the scaphoid. J Am Acad Orthop Surg. 2000;8:225–31. doi: 10.5435/00124635-200007000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Polmear MM, Anderson AB, Lanier PJ, Orr JD, Nesti LJ, Dunn JC. Bone morphogenetic protein in scaphoid nonunion:A systematic review. J Wrist Surg. 2021;10:184–9. doi: 10.1055/s-0040-1722332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pinder RM, Brkljac M, Rix L, Muir L, Brewster M. Treatment of scaphoid nonunion:A systematic review of the existing evidence. J Hand Surg Am. 2013;38:872–7. doi: 10.1016/j.jhsa.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 15.Rancy SK, Swanstrom MM, DiCarlo EF, Sneag DB, Lee SK, Wolfe SW, et al. Success of scaphoid nonunion surgery is independent of proximal pole vascularity. J Hand Surg Eur Vol. 2018;43:32–40. doi: 10.1177/1753193417732003. [DOI] [PubMed] [Google Scholar]
- 16.Caporrino FA, Dos Santos JB, Penteado FT, de Moraes VY, Belloti JC, Faloppa F. Dorsal vascularized grafting for scaphoid nonunion:A comparison of two surgical techniques. J Orthop Trauma. 2014;28:e44–8. doi: 10.1097/BOT.0b013e3182a4a91a. [DOI] [PubMed] [Google Scholar]
- 17.Sarker SF, Walsh SP. The use of the Hintermann™Distractor in distal radius osteotomy. J Hand Surg Eur Vol. 2014;39:894–6. doi: 10.1177/1753193413478268. [DOI] [PubMed] [Google Scholar]
- 18.Elzinga K, Chung KC. Volar radius vascularized bone flaps for the treatment of scaphoid nonunion. Hand Clin. 2019;35:353–63. doi: 10.1016/j.hcl.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 19.Geissler WB, Adams JE, Bindra RR, Lanzinger WD, Slutsky DJ. Scaphoid fractures:What's hot, what's not. J Bone Joint Surg Am. 2012;94:169–81. doi: 10.2106/JBJS.942icl. [DOI] [PubMed] [Google Scholar]
- 20.Quadlbauer S, Pezzei C, Beer T, Jurkowitsch J, Keuchel T, Schlintner C, et al. Treatment of scaphoid waist nonunion by one, two headless compression screws or plate with or without additional extracorporeal shockwave therapy. Arch Orthop Trauma Surg. 2019;139:281–93. doi: 10.1007/s00402-018-3087-6. [DOI] [PubMed] [Google Scholar]
- 21.Zhang H, Gu J, Liu H, Yuan C. Pedicled vascularized versus non-vascularized bone grafts in the treatment of scaphoid non-union:A meta-analysis of comparative studies. ANZ J Surg. 2021;91:E682–9. doi: 10.1111/ans.16894. [DOI] [PubMed] [Google Scholar]
- 22.Jauregui JJ, Seger EW, Hesham K, Walker SE, Abraham R, Abzug JM. Operative management for pediatric and adolescent scaphoid nonunions:A meta-analysis. J Pediatr Orthop. 2019;39:e130–3. doi: 10.1097/BPO.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 23.Soufi M, See A, Hassan S. Scaphoid fractures and non-union:A review of current evidence. Orthop Trauma. 2021;35:198–207. [Google Scholar]


