Abstract
Background:
While there is an increasing interest in patient safety and in transforming safety culture in the perioperative environment, it is not clear what methods are being used to understand, assess, and influence safety culture and climate.
Objective:
This work seeks to uncover what instruments and measures are used to assess safety culture in the perioperative environment. The work investigates how these measures are applied in baseline assessments and in interventions in the perioperative environment to enhance/support safety culture.
Methods:
We conducted a scoping review of the English language peer-reviewed literature.
Results:
Only two of 15 studies included clinical outcomes. Three studies considered process and adherence measures and one on cognitive aids to support behavioral norms. Three studies addressed collecting baseline data with no interventions mentioned. The interventions in the rest included bundles, multi-component interventions, cognitive aids, and/or training.
Conclusion:
There is no consensus on what dependent measures to include in perioperative safety culture studies. Study investigators are encouraged to collect and analyze data about engaging in behaviors that prevent, respond to, or resolve safety issues, and related factors that support understanding their effects. They are encouraged to consider focusing on measures at the individual, team, and organizational level.
Keywords: Communication, patient safety, perioperative environment, safety culture, teamwork
Introduction
Improving the safety of patient care is a top priority in the perioperative environment in order to minimize preventable deaths, post-surgical complications, and preventable adverse events. 1 2 3 4 Improved protocols (e.g., checklists), practices (e.g., infection control), and artifacts (e.g., cognitive aids) can help 5, 6. For example the World Health Organization (WHO)’s Surgical Safety Checklist7 was developed to decrease errors and adverse events, and to improve surgeon, anesthesia provider and nurse teamwork and communication during surgery. The checklist aims to aid in adherence to protocol steps (such as confirming the patient’s name, procedure, and incision location) including anticipatory guidance (such as the key concerns for recovery and patient management) and anticipatory critical events (such as considering if there any patient-specific concerns).
However, in the complex perioperative environment, a broader perspective beyond implementing checklists to establish behavioral norms is needed to address safety culture. In addition to behavioral norms and artifacts, organizational safety culture is a composed of assumptions about the nature of the workplace and its components as well as values about safety measured through perceptions and attitudes (i.e., safety climate 8 9). Behavioral factors that prevent, respond to, or resolve safety issues not only help to improve safety outcomes but also to reinforce safety culture over time. Bisbey et al. 9 highlight the importance of such enacting behaviors including a fair work environment with the ability to report near misses and errors without punishment, teamwork and collaboration across services and organizational levels to address safety problems, and effective communication between individuals, teams, and management. Bisbey et al. 9 note that organizational, group or unit level, and individual enabling factors support workers to adopt the appropriate norms, values, and assumptions. Organizational level enabling factors include dimensions such as leader commitment and prioritization of safety as well as policies and resources for safety. At the group or unit level, factors such as cohesion and psychological safety influence safety culture. At the individual level, enabling factors including safety knowledge, employee sense of control, and individual commitment to safety impact safety culture are also important.
While there is an increasing interest in patient safety and in transforming culture in the perioperative environment, it is not clear what methods are being used to understand, assess, and influence safety culture and climate. Thus, this work seeks to uncover what instruments and measures are used to assess safety culture in the perioperative environment. It analyzes whether the measures support investigating enabling factors that create conditions conducive for safe behavioral norms, values, and assumptions and the enacting behaviors that support observing and learning from one’s own and others’ behaviors. The work investigates how these measures are applied in the baseline assessments and in interventions in the perioperative environment to enhance/support safety culture.
Methods
We conducted a scoping review of the English language peer-reviewed literature using Arksey and O’Malley’s10 methodological framework. A scoping review was an appropriate choice, given the interest in evidence regarding how the perioperative area measures safety culture.
We conducted a search from January 1, 2006 to December 1, 2022, in PubMed. See Table 1 for search terms and inclusion and exclusion criteria. In the United States, the Patient Safety and Quality Improvement Act of 2005 established a voluntary reporting system designed to enhance the data available to assess and resolve patient safety and health care quality issues11. The Act authorized the Agency for Healthcare Research and Quality (AHRQ) to list patient safety organizations and to create a network of patient safety databases. Thus, inclusion criteria included manuscripts published after 2005. Studies were limited to those conducted on health care systems in the United States, given the highly contextual nature of patient safety, implementation research, and translation for a similar standard of care. In addition, studies that included perioperative staff were considered.
Table 1.
Inclusion and exclusion criteria and search terms
| Inclusion criteria | Exclusion criteria |
|---|---|
| Published after 2005 | Protocol paper |
| Peer-reviewed | Literature review |
| Published in English | All patients are non-human |
| Setting in the United States | Topic not about perioperative safety culture |
| No analysis | |
| No perioperative staff included as participants in study |
Search terms: periop* AND “safety culture”
Information from retrieved publications were exported into Microsoft Excel®. Duplicates were removed. A two-stage review process was implemented to evaluate publication appropriateness for inclusion. First, the authors independently reviewed titles and abstracts against the inclusion criteria. Second, the authors independently evaluated and rated the full publication for inclusion. Differences over inclusion were resolved through discussion to reach consensus. See Figure 1 for a flow diagram (based on Page et al.12) of the article selection process.
Figure 1.
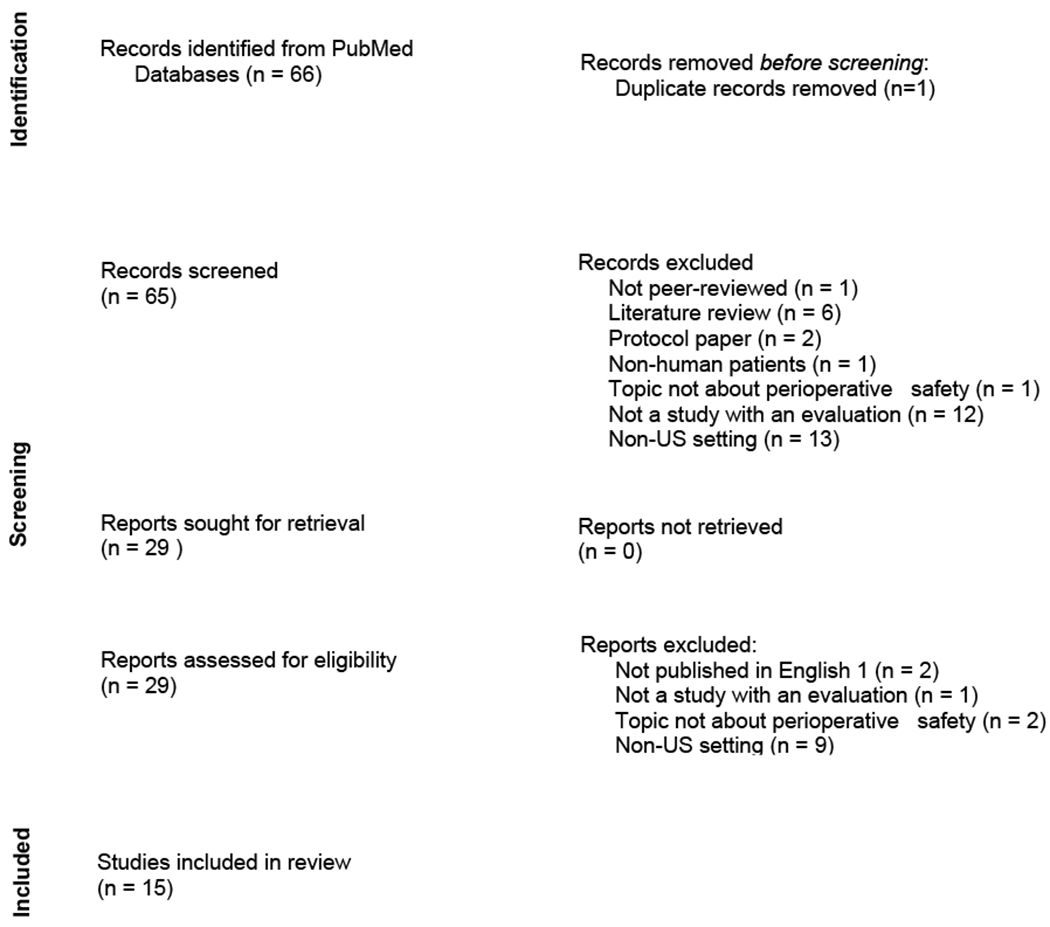
PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and registers only. (Adapted from Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71)
To address the research questions, a multi-step process was used. Both authors separately reviewed the methods and results sections of the selected manuscripts and summarized the measures collected. Second, in a Microsoft Excel® spreadsheet, one author (BH) extracted the questions in the survey instruments and any other measures collected in each study. Third, the authors used an inductive content analysis technique13 to develop categories for each question/measure. The authors independently developed categories. Differences over the categorization were resolved through discussion to reach consensus.
Results
Study settings
Table 2 summarizes the settings of the reviewed studies. Eleven of the 15 studies were conducted at one hospital or center. Three recruited from more than one hospital or center 14 15 16 while one recruited from a local professional society chapter17.
Table 2.
Manuscript purpose and select methods
| Manuscript | Purpose/ Intervention/Initiatives | Instruments/Measures | Setting | Participants |
|---|---|---|---|---|
| Barr et al. (2020) | Assess safety culture, ICU team collaboration, and work environment Determine whether organizational characteristics were associated with ICU Liberation (ABCDEF) Bundle implementation Determine level of agreement between physician and nurse leaders around ICU organizational characteristics and bundle implementation |
Survey domains with respondent, ICU, and hospital characteristics; organizational characteristics of work environment (collaboration, safety culture); and bundle implementation phases Safety Organizing Scale (SOS) |
43 of 72 acute care hospitals with adult ICUs in Michigan | 28 ICU physicians 45 ICU nurses |
| Carney et al. (2010) | After team training and implementation of the Surgical Safety checklist: Assess teamwork differences between perioper. nurses and surgeons Examine implications of differences for improving practice patterns in the OR |
Safety Attitudes Questionnaire | 34 Veterans Health Administration hospitals | 312 surgeons 378 perioper. nurses |
| Falcone et al. (2021) | Assess perioperative safety initiatives: Pulse surveys with feedback for safety concerns; Multidisciplinary safety training; Safety culture champion team; New safety processes with standard training; Missions and tenets; Intraoperative huddle process; Pathways for resolution of safety concerns; Time-out and prevention of retained foreign object process |
Two question custom survey: Climate of trust in work area Others responding with grace and gratitude Process adherence and engagement Training feedback |
Urban, >600 bed pediatric academic medical center | 230 survey respondents from “selected staff” |
| Goldhaber-Fiebert et al. (2016) | Assess perspectives on OR safety culture regarding emergency manual (cognitive aid) use before and after implementation Describe emergency manual use during critical events. |
Custom pre/post-implementation surveys | Dept. of Anesth., Perioper. and Pain Medicine at Stanford Univ. School of Medicine | Anesth. residents Pre: 34 Post:42 |
| Halvorson et al. (2016) | Assess design of an ideal transfer process for transfers from ICUs to acute care units and associated structured handoff tool (checklist) | Adherence to standard workflow; Average time to transfer completion; Percentage of transfers completed in time period; Percentage of transfers with receiving provider notified of patient arrival; Staff survey assessing adequacy of transfer communication |
550-bed academic, tertiary care center with 13 medical and surg. ACUs + 80 adult critical care beds across 4 adult ICUs | Pre-survey: 41 physicians 2 PAs 115 nurses Post-survey: 43 physicians 123 nurses |
| Hemingway et al. (2015) | Assess Perioper. Services safety initiatives: Changing processes for safety reporting and performance improvement plans Adding resources and nurses’ roles, Creating communication strategies around adverse safety events |
Custom staff survey to understand OR safety culture | Massachusetts General Hospital, Boston | 79 RNs, surg. technologist, OR assistants, operational associates |
| Lozito et al. (2018) | Assess a Good Catch Campaign designed to improve perioperative safety culture including: Formal education about good catch reporting; Standardized event reporting; Debriefing sessions for interprofessional discussions of actual events or near misses |
Number of good catch reports Participation in and scores from AHRQ Hospital Survey on Patient Safety Culture |
249-bed acute care community teaching hospital in Pennsylvania | Nurses, surg. technologists, anesth. care providers, PAs, quality director and coordinator, surgeons and others: 2014: 58; 2015:35; 2016: 71 |
| Odell et al. (2019) | Assess safety culture and its associations with surgical outcomes after: Participation in the American College of Surgeons’ NSQIP Engaging surgeon champions Supporting QI team with formal QI education, external QI coaches, and surgeon mentors Sharing outcomes benchmark data |
Modified Safety Attitudes Questionnaire Postoperative patient outcomes |
49 adult Illinois Surgical Quality Improvement Collaborative (ISQIC) hospitals | 103 hospital administrators 131 physicians 17 PA/nurse practitioner 460 nurses 108 quality improvement team members |
| Pimentel et al. (2021) | Identify variability in safety climate between groups of perioperative staff, if any existed | AHRQ Hospital Survey on Patient Safety Culture | Brigham and Women’s Hospital, a academic tertiary medical center, 793 beds | 78 surgery attendings 46 surgery residents 68 anesth. attendings 46 anesth. residents 141 nurses 23 surgery techs |
| Putnam et al. (2014) | Develop and assess interventions to improve safety culture, local engagement of stakeholders, and comprehension of the WHO’s Surgical Safety checklist: Modified WHO’s Surgical Safety checklist Pediatric OR safety council Safety workshops: Culture of safety and high-reliability organizations Error identification and effective communication Stakeholder audit and feedback |
Safety Attitudes Questionnaire Checklist adherence |
Children’s Memorial Hermann Hospital academic, 240-bed children’s hospital within tertiary center | Unspecified number of perioper., direct care providers completed Safety Attitudes Questionnaire |
| Putnam et al. (2015) | Compare safety culture, teamwork, and metrics of speaking up between two groups: Surgeons, anesthesiologists, and perioper. nurses in workshops addressing communication & safety culture Surg. residents completing safety curriculum |
Safety Attitudes Questionnaire | University of Texas Health Science Center at Houston (Children’s hospital) | 48 surg. residents 63 perioper. staff (surgeons, anesthesiologist, ‘direct care providers’) |
| Scherer & Fitzpatrick (2008) | Compare physician and RN perceptions of patient safety after implementing the Joint Commission’s patient safety recommendations for verification of correct patient, procedure, side, and site for patients undergoing surgery | AHRQ Hospital Survey on Patient Safety Culture | 174-bed community hospital/ perioper. area | 40 surgeons + anesthesiologists 43 nurses |
| Wright, Polivka, & Abusalem (2021) | Examine relationships between perioper. nurse experience, engagement, and OR safety culture Examine if perioper. nurse experience and engagement predict OR safety culture Determine if OR culture of safety scores differ based on CNOR certification status |
Utrecht Work Engagement Scale – 9 item version; Modified Safety Attitudes Questionnaire −41 of 60 items |
Eligible perioperative nurses from local AORN chapter | 96 perioper. nurses |
| Wright, Polivka, & Clark (2022) | Explore normalization of deviance in OR Identify reasons for normalization of deviance Identify factors that protect against normalization of deviance. |
Custom interview questions about normalization of deviance | Perioper. Nurses in midwestern metropolitan area | 10 perioperative nurse |
| Zingiryan et al. (2017) | Implementation of WHO Surgery Safety Checklist to decrease 9 complications in perioper. morbidity/morality (mortality, wound dehiscence, sepsis, respiratory failure, venous thromboembolism, postoper. hemorrhage or hematoma, retained foreign body, transfusion reaction, and death among surg. inpatients with serious treatable complications) | Custom questions to assess attitudes towards the WHO Surgery Safety Checklist Complication rates for 9 complications |
University of Vermont Medical Center | 59 surgeons 33 surg. residents 37 anesthesiologists 13 anesth. residents 9 nurse anesthetists 54 OR nurse 5 scrub technicians 19 OB/GYN attendings 9 OB/GYN resident 17 other |
Abbreviations: AHRQ, Agency for Healthcare Research and Quality; anesth., anesthesia; CNOR, Certified Perioperative Nurse; ICU, intensive care unit; NSQIP, National Surgical Quality Improvement Program; OB/GYN, obstetrics and gynecology; OR, operating room; pa, perioperative; perioper, perioperative; surg, surgery; Univ, university.
The majority of the studies included multiple professional roles in the set of participants. One study included only anesthesiologists18. Two studies only included nurses 17 19. Two were unclear about the role of the participants (one mentioned selected staff20 and one mentioned perioperative direct care providers21). One study included hospital administrators as participants16. Two studies included workers with safety and/quality improvement experience16 22.
Measures
Table 2 summarizes the measures and instruments used in the reviewed studies.
Measures of clinical outcomes
Two studies considered outcomes measures. Odell et al.16 included postoperative patient outcomes. Zingiryan et al.23 considered complication rates for mortality, wound dehiscence, sepsis, respiratory failure, venous thromboembolism, postoperative hemorrhage or hematoma, retained foreign body, transfusion reaction, and death among surgical inpatients with serious treatable complications.
Measures of behavioral norms
Three studies specifically considered process and adherence measures to determine whether employees follow recommended procedures. Falcone et al.20, Halvorson et al.24, and Putnam et al.21 measured adherence to the recommended workflow. Halvorson et al. 24 added more detailed process measures in addition to step completion including time to complete and percentage of completions.
Goldhaber-Fiebert et al.18 focused on cognitive aids to support behavioral norms and their adoption. The Post-implementation Emergency Manual survey included 13 pre-implementation survey questions about attitudes toward cognitive aids plus nine questions regarding EM implementation and clinical use during critical events. The survey also addressed the enabling factor of training.
Measures from standard instruments
Eight included studies used one instrument that has been applied to research in other domains beyond perioperative care and a ninth 17 applied two instruments:
AHRQ’s Surveys on Patient Safety Culture™ (SOPS®) Hospital Survey25: Lozito, et al.22, 26, 27
Safety Attitudes Questionnaire (SAQ)28: Carney et al. 15, Odell et al. 16, Wright, Polivka, & Abusalem17, Putnam et al., 201421, Putnam et al., 2015 29
Safety Organizing Scale (SOS)30 : 14
Utrecht Work Engagement Scale (UWES) 31 32: Wright, Polivka, & Abusalem17
On the AHRQ instrument, 24 questions address patient safety. One question is a free response question about patient safety in general. Five questions address the unit (group) level: one question requests a rating of the unit’s patient safety and four address unit level enacting behaviors via review of work processes, treatment of staff suggestions, and evaluation of patient safety interventions. Fourteen questions address enacting behaviors related to error and near miss reporting, openness of communication, analysis, and the response to errors. Three questions address enacting behaviors related to teamwork (team effectiveness, behavior, and helping other team members during busy times) and another three probe specific team processes (transfer of information during transitions of care). Three questions address enabling factors of leadership and management participation in patient safety initiatives. One question addresses leadership and management priorities regarding patient safety (providing adequate resources). Related to staffing resources, two questions address having adequate staff and the use of temporary workers and two questions about workload (hours worked, pace of work). One question addresses leadership and management expectations about workload (expectations about work faster during busy times). The instrument includes work and experience questions (position, job responsibilities, and background experience).
The SAQ has longer and shorter forms but generally includes one question asking whether the respondent would feel safe being treated at the location as a patient. Several questions address enacting behaviors: error and near miss reporting, openness and pathways of communication about errors and other patient safety concerns, and the culture of feedback and response to errors (i.e., the culture in this [clinical area] makes it easy to learn from the errors of others). One question addresses team processes and another addresses teamwork to support the employee when busy. One question addresses the ability to ask questions when not understanding. Two questions probe having adequate information to complete work tasks. Regarding enabling factors, one question addresses leadership and management participation in patient safety efforts. One question addresses staffing. The SAQ includes one question about the adequacy of employee training. The instrument includes one human resources related question (about dealing with problem employees) and another about hospital administration supporting daily efforts. The SAQ survey includes four questions about job satisfaction and morale. Four questions probe the respondent’s understanding of the effect of context on human performance:
I am more likely to make errors in tense or hostile situations.
I am less effective at work when fatigued.
Fatigue impairs my performance during emergency situation
When my workload becomes excessive, my performance is impaired.
The 9-question SOS includes two questions about error reporting and response (e.g., we talk about mistakes and ways to learn from them). It includes seven questions related to teamwork and team processes (e.g., “when giving report to an oncoming nurse, we usually discuss what to look out for” and “we discuss our unique skills with each other so we know who on the unit has relevant specialized skills and knowledge”).
The UWES is focused specifically on individual level enabling factors surrounding work engagement. It has short and longer forms. The questions address the worker’s levels of energy and mental resilience. The instrument also probes the worker’s relationship toward the work regarding dedication, inspiration, and pride. It also probes work engagement regarding challenge and concentration.
Measures from custom instruments
Five included studies used custom instruments. As mentioned above, some studies addressed adherence to a protocol. Halvorson et al. 24 executed a five question pre-/post-implementation survey regarding adherence to a standardized transfer workflow.
Regarding the enacting behaviors, Hemingway et al. 33 executed a staff survey with four questions related to error reporting and response. On an employee engagement survey, Falcone et al. 20 included one question about others’ grace and gratitude in response to safety concerns in addition to one on a climate of trust in the work area.
Regarding enabling factors that create the context for norms, values, and assumptions to develop, Wright et al. 19 executed twelve-question interviews regarding personnel and management practices, and employee engagement as well as safety concerns.
The Zingiryan et al. 23 survey included 28 questions that spanned enacting behaviors (e.g., “I receive feedback about problems or mistakes that were identified in the checklist debriefing” and “When a patient safety event is reported, it feels like the problem is addressed, not the person”) and enabling factors (e.g., “The actions of the OR nursing and physician leadership teams show that patient safety is a top priority”).
Measures used to assess participation in safety processes
One study addressed participation in patient safety processes. Lozito et al. 22 focused on participation in as well as the scores from the AHRQ survey. In addition, the authors investigated the number of good catch reports submitted, a measure that addresses participation in the reporting process.
Baseline safety culture studies in the perioperative environment
Three studies addressed collecting baseline data with no interventions mentioned. Pimentel et al.26 were interested in characterizing variability in safety climate between groups of perioperative staff, if any existed. Analysis of AHRQ survey data from 431 surgeons, anesthesiologists, nurses, and technicians indicated variability in perioperative patient safety climate across survey dimensions, professional roles, and levels of training. For example, surgery attending physicians reported significantly higher composite average dimension scores than attending anesthesiologists, nurses, and technicians. Physicians reported the lowest scores for frequency of event reporting while this dimension was highest for nurses. Nurses and technicians reported feedback and communication about errors as well as hospital management support for safety as their groups’ two lowest ranking dimension scores.
Wright, Polivka, & Abusalem17 examined a) relationships between perioperative nurse experience, engagement, and OR safety culture, b) if perioperative nurse experience and engagement predict OR safety culture, and c) if OR culture of safety scores differ based on Certified Perioperative Nurse (CNOR) certification status. Based on data from 96 nurses, perioperative nurses who held CNOR certification had significantly higher culture of safety scores compared with others.
Wright, Polivka, & Clark19 were focused on a contributor to lack of protocol adherence by perioperative nurses. In particular, they focused on normalization of deviance where workers fail to adhere to standard performance before such performance becomes an accepted norm. Based on data from ten nurses, they determined that normalization of deviance results from productivity pressures, generalized complacency, complacency related experience, social pressures, and negative acculturation. They found that nurse engagement and having supportive managerial relationships can protect against normalization of deviance.
Intervention studies
A range of interventions were addressed in twelve studies.
Bundles and other multi-components interventions
Some multi-component interventions were focused on safety culture. Hemingway et al.33 described safety initiatives with limited evaluation. The authors present a set of a Perioperative Services department’s safety initiatives to enhance safety culture. As is more typical, modified procedures were introduced. Enacting behavior related components included enhanced electronic safety reporting system, a system of safety behavior auditing and feedback, facility-wide dissemination of safety issues, and debriefing of safety reports. Enabling factor related components includes additional safety and quality nursing positions and modified policies. The authors presented select survey results. Regarding enacting behaviors, the majority of RNs, surgical technologists, OR assistants, and operational associates answered negatively to the question, “I feel free to question the decision or actions of those with more authority.” Also, regarding norms, close to half stated that they would not speak up if they saw something negatively affecting patient safety.
Falcone et al.20 assess an integrated set of perioperative safety initiatives including enabling factors such as new safety missions and tenets highlighting being “one team” for safety, multidisciplinary safety training and safety culture champion teams trained on coaching skills and safety processes as well as enacting behaviors such as new safety processes with standard training, monthly pulse surveys with feedback for safety concerns, an intraoperative huddle process to improve intraoperative communication and situation awareness, and clear pathways for resolution of safety concerns. Based on a review of episodes of retained foreign bodies at the study institution, there was an initiative on prevention of retained foreign objects. They found that by coaching on the processes and safety culture specifics, the champions aided the implementation of the new safety processes. The pulse surveys, communications, and staff behavior also helped with sustainment.
Lozito et al. 22 address enacting behaviors (standardized event reporting and debriefing sessions for interprofessional discussions of actual events or near misses) related to a “good catch” initiative designed to improve perioperative safety culture. Enabling factors included formal education about good catch reporting. The intervention yielded a significant increase in the number of reported good catches during the six-month post-implementation period. Results using the AHRQ survey indicated better scores in five areas: communication openness, feedback and communication about error, frequency of event reporting, nonpunitive response to error, and organizational learning and continuous improvement.
Odell et al. 16 assessed safety culture and its associations with surgical outcomes after participation in the American College of Surgeons’ National Surgical Quality Improvement Program (NSQIP) 34, engaging surgeon champions, supporting quality improvement (QI) teams (with formal QI education, external QI coaches, and surgeon mentors), and sharing outcomes benchmark data. Compared with the other areas, OR safety culture scores were the highest while hospital management ratings were the lowest. Hospital administrators provided higher ratings of perceptions of safety culture as compared to physicians, advanced practice providers, and nurses. Administrators were more likely to rate teamwork as a weakness while physicians, advanced practice providers, and nurses tended to rate teamwork as a strength. Positive SAQ ratings were significantly associated with lower risk of postoperative morbidity and death or serious morbidity.
Putnam et al. 21 assessed checklist adherence and perspectives on safety culture after the implementation of a modified WHO’s Surgical Safety checklist coupled with safety workshops addressing safety culture and error reporting as well as effective communication and with stakeholder audits and feedback. Surgical residents completed safety curriculum. Checklist adherence significantly improved after each interventional period. Perioperative direct care providers, circulating nurses and scrub technicians’ SAQ ratings improved in safety culture, teamwork, speaking up, safety rounds, and other aspects of the safety culture.
One intervention assessed safety culture but the intervention itself addressed clinical practice. Barr et al.14 assessed safety culture, ICU team collaboration, and work environment factors associated with ICU Liberation (ABCDEF) Bundle on Pain, Agitation, Delirium, Immobility, and Sleep 35 guidelines implementation in hospitals in Michigan with adult ICUs. They compared physician and nurse leadership agreement around ICU organizational characteristics and bundle implementation. They found that bundle implementation varied significantly across ICUs and that better work environment scores as measured by higher SOS mean score and/or a higher composite collaborative work environment domain score were significantly associated with implementation of the majority of bundle elements.
Checklists and cognitive aids
Four studies focus on work performance interventions such as checklists and other cognitive aids. Goldhaber-Fiebert et al. 18 developed and executed surveys to assess perspectives on OR safety culture regarding cognitive aid use specifically before and after the implementation of an emergency manual for perioperative critical events 36. The emergency manuals had been placed in ORs and associated training provided. Anesthesia resident attitudes towards the use of emergency manuals improved post-implementation. In the sustainment phase, they indicated that emergency manuals helped the team deliver better care to patients.
Halvorson et al.24 discussed a key stakeholder-developed standardized care transition workflow (transfer process for transfers from ICUs to acute care units). An associated structured handoff checklist supported performance. Survey data assessed the adequacy of transfer communication.
Carney et al. 15 assessed teamwork differences between perioperative nurses and surgeons after medical team training developed by the National Center for Patient Safety (NCPS) 37 and implementation of the Surgical Safety checklist. They found that nurses and surgeons rated the communication and collaboration they experience with nurses as relatively high. However, surgeons rated the communication and collaboration they experienced with other surgeons as relatively high, but nurses rated the communication and collaboration they experienced with surgeons as relatively low. In addition on five of the six teamwork climate ratings, surgeons had a significantly more favorable perception than nurses.
Zingiryan et al. 23 analyzed post WHO Surgery Safety Checklist implementation. They reported no significant decrease in any of the nine complications (mortality, wound dehiscence, sepsis, respiratory failure, venous thromboembolism, postoperative hemorrhage or hematoma, retained foreign body, transfusion reaction, and death among surgical inpatients with serious treatable complications). They also examined OR staff (nurses, surgeons, anesthesiologists, and OB/GYN physicians) attitudes regarding how implementation of the WHO Surgery Safety Checklist affected team dynamics and patient safety. There was overall agreement that the SSC improved communication, safety, and prevented errors in the operating room. Nurses and surgeons disagreed regarding whether all three parts of the SSC were always completed.
Scherer & Fitzpatrick 27 compared physician and RN perceptions of patient safety after implementing the Joint Commission’s patient safety recommendations for verification of correct patient, procedure, side, and site for patients undergoing surgery. Nurses provided significantly higher safety culture ratings as compared with physicians with respect to feedback and communication about error as well as to supervisor expectations and actions promoting safety.
Training
Putnam et al. 29 presented comparisons of safety attitudes for perioperative and surgery personnel regarding safety culture and teamwork, and metrics associated with speaking up. Surgeons, anesthesiologists, and perioperative nurses participated in workshops aimed at enhancing communication and safety culture. The general surgery residents completed an online safety curriculum only. A higher percentage of perioperative personnel perceived significantly better safety culture than the surgical residents.
Discussion
This work focused on understanding how studies in the perioperative environment address understanding, assessing, and improving safety culture. In addition to addressing perceptions of safety climate and outcomes measures, the analysis leveraged consideration of enabling factors that create conditions conducive for safe behavioral norms, values, and assumptions and enacting behaviors that support observing and learning from behaviors in the work environment.
The perioperative environment includes a wide range of team members from a disparate set of disciplines including surgeons, anesthesiologists, certified registered nurse anesthetists, circulating nurses, surgical techs, respiratory therapists, and more. Some studies failed to make clear what were the disciplinary areas of the participants. In addition, not all studies made clear what level of training the participants had achieved. While some studies included a range of health care disciplinary perspectives, only one study included hospital administrators as participants 16 and only two included quality improvement professionals 16 22. Considering the organizational level for patient safety initiatives, such roles are relevant in the participant cohorts. In order to address safety culture issues across the organization and group levels as well as to consider experience, the perioperative environment safety literature would benefit from studies that recruit, collection data, and report results from a broader participant base including multi-site studies.
Based on the reviewed studies, there is no consensus on what dependent measures to include in safety culture studies. Studies tend to collect perceptions of safety climate. If interventions are part of a study, then measures related to the perceptions of the interventions may also be collected. Measures of adherence to recommended procedures, with or without the benefit of a cognitive aid and/or training, provide process measures that can augment the collection of clinical outcome data.
For organizations that implement support for engaging in behaviors that prevent, respond to, or resolve safety issues, collecting related behavioral data supports understanding their effects. Some of the reviewed studies collected data related to communication and information exchange between individuals, teams and groups, and management and workers. Measures that address sharing and discussing safety information coupled with the existence of conversations about what improvements can be made to enhance safety can shed light on the extent to which communications can be effectively attended to as well as whether issues surrounding openness of communication may need to be investigated38.
Data related to teamwork and collaboration shed light on how well teams work together but also about support and backup. The perioperative environment requires task switching during high workload periods. The studies including nurses as participants probe concepts related to team members being able to anticipate or at least be aware of other member’s load in order to help when necessary. This need for nurses to support one another is critical and should be considered with respect to staffing plans in order to avoid missed nursing care 39.
Information related to just culture40 41 is important for understanding whether workers can and will engage with incident reporting and addressing errors and near misses or whether they will encounter or perceive they will encounter punitive behaviors. Studies appear to be more likely to address the punitive side of the coin but there is opportunity to investigate perceptions of offering praise, recognition, or other incentives to improve safety.
Studies that focus on the individual and group (unit) level should also collect measures associated with the organizational level. Partly this is critical because administrative leaders allocate resources and therefore greatly impact whether safety initiatives can be executed. In addition, workers are influenced by management’s commitment to safety as expressed by their actions and attitudes42.
Limitation of this work
In terms of limitations, it is possible relevant research was not identified with our search terms and we only reviewed publications in English from settings within the United States. For example, the use of “patient safety” instead of “safety culture” may have yielded relevant papers. In addition, considering terms to augment the concept of perioperative, such as surgery or anesthesia, may have returned relevant manuscripts.
Conclusion
This work investigated measures used to assess safety culture in the perioperative environment. Based on the reviewed manuscripts, there is no consensus on what dependent measures to include in safety culture studies. In addition to perceptions of safety climate and outcome measures, study investigators are encouraged to collect and analyze data about engaging in behaviors that prevent, respond to, or resolve safety issues, and related factors that support understanding their effects. In addition, they are encouraged to consider focusing on measures at the individual, team and organizational level.
Key points:
Improving the safety of patient care is a top priority in the perioperative environment in order to minimize preventable deaths, post-surgical complications, and preventable adverse events.
While there is an increasing interest in patient safety and in transforming safety culture in the perioperative environment, it is not clear what methods are being used to understand, assess, and influence safety culture and climate.
There is no consensus on what dependent measures to include in perioperative safety culture studies.
Clinics Care Points.
Measurement of safety climate is a point in time characterization of perceptions and attitudes while safety culture of an organization is the product of individual and group values, attitudes, perceptions, competencies, and patterns of behavior that determine the commitment to, and the style and proficiency of, an organization’s health and safety management.
Assessment of patient safety initiatives to support improving safety culture should consider the use of validated instruments.
In order to generalize and to compare improvements across work contexts and health systems, standard measures should be use.
Patient safety initiatives to support improving safety culture should include the range of clinical perspectives for which initiatives propose to have impact.
Patient safety initiatives require a range of supporting activities and resources for adoption and sustainment.
Acknowledgements
The National Heart, Lung, and Blood Institute (NHLBI) of the United States National Institutes of Health funded this study in part through an investigator-initiated research grant (1R01HL153735-01; PI: M. Lane-Fall). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NHLBI.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure:
Conflict of Interest Disclosures: None.
References
- 1.Anderson O, Davis R, Hanna GB, & Vincent CA (2013). Surgical adverse events: a systematic review, The American Journal of Surgery, 206 (2), 253–262. [DOI] [PubMed] [Google Scholar]
- 2.Bates DW, Levine DM, Salmasian H, Syrowatka A, Shahian DM, Lipsitz S, … & Mort E (2023). The safety of inpatient health care. New England Journal of Medicine, 388(2), 142–153. [DOI] [PubMed] [Google Scholar]
- 3.Dobson GP (2020). Trauma of major surgery: A global problem that is not going away. International Journal of Surgery, 81, 47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lawson EH, Hall BL, Louie R, Ettner SL, Zingmond DS, Han L, … & Ko CY (2013). Association between occurrence of a postoperative complication and readmission: implications for quality improvement and cost savings. Annals of Surgery, 258(1), 10–18. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong BA, Dutescu IA, Nemoy L, Bhavsar E, Carter DN, Ng KD, Boet S, Trbovich P, & Palter V (2022). Effect of the surgical safety checklist on provider and patient outcomes: a systematic review. BMJ Quality & Safety, 31(6), 463–478. [DOI] [PubMed] [Google Scholar]
- 6.Westman M, Takala R, Rahi M, & Ikonen TS (2020). The need for surgical safety checklists in neurosurgery now and in the future-A systematic review. World Neurosurgery, 134, 614–628.e3. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization (n.d.). WHO Surgical Safety Checklist https://www.who.int/teams/integrated-health-services/patient-safety/research/safe-surgery/tool-and-resources
- 8.Zohar D. (1980). Safety climate in industrial organizations: Theoretical and applied implications. Journal of Applied Psychology, 65, 96–102. [PubMed] [Google Scholar]
- 9.Bisbey TM, Kilcullen MP, Thomas EJ, Ottosen MJ, Tsao K, & Salas E (2021). Safety culture: An integration of existing models and a framework for understanding its development. Human Factors, 63(1), 88–110. [DOI] [PubMed] [Google Scholar]
- 10.Arksey H, O’Malley L (2005). Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 8(1):19–32 [Google Scholar]
- 11.U.S. Government Publishing Office (2005). 119 Stat. 424 - Patient Safety and Quality Improvement Act of 2005. July 29, 2005. https://www.govinfo.gov/content/pkg/STATUTE-119/html/STATUTE-119-Pg424.htm
- 12.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elo S, & Kyngäs H (2008). The qualitative content analysis process .Journal of Advanced Nursing, 62(1), 107–115. [DOI] [PubMed] [Google Scholar]
- 14.Barr J, Ghaferi AA, Costa DK, Hedlin HK, Ding VY, Ross C, Pun BT, Watson SR, Asch SM. (2020). Organizational characteristics associated with ICU Liberation (ABCDEF) Bundle implementation by adult ICUs in Michigan. Crit Care Explor, 2(8), e0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carney BT, West P, Neily J, Mills PD, & Bagian JP (2010). Differences in nurse and surgeon perceptions of teamwork: implications for use of a briefing checklist in the OR. AORN J, 91(6), 722–729. [DOI] [PubMed] [Google Scholar]
- 16.Odell DD, Quinn CM, Matulewicz RS, Johnson J, Engelhardt KE, Stulberg JJ, Yang AD, Holl JL, Bilimoria KY (2019). Association between hospital safety culture and surgical outcomes in a statewide surgical quality improvement collaborative. Journal of the American College of Surgeons, 229(2), 175–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wright MI, Polivka B, & Abusalem S (2021). An examination of factors that predict the perioperative culture of safety. AORN Journal, 113(5), 465–475. [DOI] [PubMed] [Google Scholar]
- 18.Goldhaber-Fiebert SN, Pollock J, Howard SK, & Bereknyei Merrell S (2016). Emergency manual uses during actual critical events and changes in safety culture from the perspective of anesthesia residents: A pilot study. Anesth Analg, 123(3), 641–649. [DOI] [PubMed] [Google Scholar]
- 19.Wright MI, Polivka B, & Clark P (2022). Exploring normalization of deviance among perioperative registered nurses in the operating room. Western Journal of Nursing Research, 44(2), 116–124 [DOI] [PubMed] [Google Scholar]
- 20.Falcone RA, Simmons J, Carver AM, Mullett B, Kotagal M, Lin E, Muething S, von Allmen D. (2021). Perioperative safety: Engage, integrate, empower, sustain to eliminate patient safety events. Pediatric Quality & Safety, 6(6), e495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Putnam LR, Levy SM, Sajid M, Dubuisson DA, Rogers NB, Kao LS, Lally KP, Tsao K (2014). Multifaceted interventions improve adherence to the surgical checklist. Surgery, 156(2):336–44. [DOI] [PubMed] [Google Scholar]
- 22.Lozito M, Whiteman K, Swanson-BiearmanW B, Barkhymer M, & Stephens K (2018). Good Catch Campaign: Improving the perioperative culture of safety. AORN Journal, 107(6), 705–714. [DOI] [PubMed] [Google Scholar]
- 23.Zingiryan A, Paruch JL, Osler TM, & Hyman NH (2017). Implementation of the surgical safety checklist at a tertiary academic center: Impact on safety culture and patient outcomes. American Journal of Surgery, 214(2), 193–197. [DOI] [PubMed] [Google Scholar]
- 24.Halvorson S, Wheeler B, Willis M, Watters J, Eastman J, O’Donnell R, & Merkel M (2016). A multidisciplinary initiative to standardize intensive care to acute care transitions. International Journal for Quality in Health Care, 28(5), 615–625. [DOI] [PubMed] [Google Scholar]
- 25.Agency for Healthcare Research and Quality (n.d.). Hospital Survey on Patient Safety Culture https://www.ahrq.gov/sops/surveys/hospital/index.html
- 26.Pimentel MPT, Choi S, Fiumara K, Kachalia A, & Urman RD (2021). Safety culture in the operating room: Variability among perioperative healthcare workers. Journal of Patient Safety, 17(6), 412–416. [DOI] [PubMed] [Google Scholar]
- 27.Scherer D, & Fitzpatrick JJ (2008). Perceptions of patient safety culture among physicians and RNs in the perioperative area. AORN Journal, 87(1), 163–175. [DOI] [PubMed] [Google Scholar]
- 28.Sexton JB, Helmreich RL, Neilands TB, Rowan K, Vella K, Boyden J, Roberts PR, & Thomas EJ (2006). The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Services Research, 6, 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Putnam LR, Levy SM, Kellagher CM, Etchegaray JM, Thomas EJ, Kao LS, Lally KP, & Tsao K (2015). Surgical resident education in patient safety: where can we improve? Journal of Surgical Research, 199(2), 308–313 [DOI] [PubMed] [Google Scholar]
- 30.Vogus TJ, & Sutcliffe KM (2007). The Safety Organizing Scale: development and validation of a behavioral measure of safety culture in hospital nursing units. Medical Care 45(1), 46–54. [DOI] [PubMed] [Google Scholar]
- 31.Schaufeli WB, Bakker AB, and Salanova M (2006). The measurement of work engagement with a short questionnaire: a cross–national study. Educ. Psychol. Measure 66, 701–716. [Google Scholar]
- 32.Schaufeli WB, Shimazu A, Hakanen J, Salanova M, and De Witte H (2017). An ultra–short measure for work engagement: the UWES–3 validation across five countries. Eur. J. Psychol. Assess 1–15. [Google Scholar]
- 33.Hemingway MW, O’Malley C, & Silvestri S (2015). Safety culture and care: a program to prevent surgical errors. AORN J, 101(4), 404–415. [DOI] [PubMed] [Google Scholar]
- 34.Shiloach M, Frencher SK, Steeger JE, Rowell KS, Bartzokis K, Tomeh MG, Richards KE, Ko CY, & Hall BL (2010). Toward robust information: Data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program, Journal of the American College of Surgeons, 210(1), 6–16. [DOI] [PubMed] [Google Scholar]
- 35.Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJC, PandharipandeW PP, Watson PL, Weinhouse GL, Nunnally ME, Rochwerg B, Balas MC, van den Boogaard M, Bosma KJ, Brummel NE, Chanques G, Denehy L, Drouot X, Fraser GL, Harris JE, Joffe AM, … Alhazzani W (2018). Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Critical Care Medicine, 46(9), e825–e873. [DOI] [PubMed] [Google Scholar]
- 36.Stanford Anesthesia Cognitive Aid Group (n.d.). Stanford Emergency Manual for perioperative critical events. http://emergencymanual.stanford.edu
- 37.Dunn EJ, Mills PD, Neily J, Crittenden MD, Carmack AL, & Bagian JP (2007). Medical team training: applying crew resource management in the Veterans Health Administration. Joint Commission Journal on Quality and Patient Safety, 33(6), 317–325. [DOI] [PubMed] [Google Scholar]
- 38.Chen IC, & Li HH (2010). Measuring patient safety culture in Taiwan using the Hospital Survey on Patient Safety Culture (HSOPSC). BMC Health Services Research, 10, 152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lake ET, Germack HD, & Viscardi MK (2016). Missed nursing care is linked to patient satisfaction: a cross-sectional study of US hospitals. BMJ Quality & Safety, 25(7), 535–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reason J, (1997). Managing the risks of organisational accidents. Aldershot: Ashgate. [Google Scholar]
- 41.Marx D (2001). Patient safety and the “just culture”: A primer for healthcare executives. New York: Columbia University. [Google Scholar]
- 42.Singer SJ, Molina G, Li Z, Jiang W, Nurudeen S, Kite JG, Edmondson L, Foster R, Haynes AB, & Berry WR (2016). Relationship between operating room teamwork, contextual factors, and safety checklist performance. Journal of the American College of Surgeons, 223(4), 568–580.e2. [DOI] [PubMed] [Google Scholar]


