Abstract
Ageing is a complex biological process associated with increased morbidity and mortality. Nine classic, interdependent hallmarks of ageing have been proposed involving genetic and biochemical pathways that collectively influence ageing trajectories and susceptibility to pathology in humans. Ageing skeletal muscle undergoes profound morphological and physiological changes associated with loss of strength, mass, and function, a condition known as sarcopenia. The aetiology of sarcopenia is complex and whilst research in this area is growing rapidly, there is a relative paucity of human studies, particularly in older women. Here, we evaluate how the nine classic hallmarks of ageing: genomic instability, telomere attrition, epigenetic alterations, loss of proteostasis, deregulated nutrient sensing, mitochondrial dysfunction, cellular senescence, stem cell exhaustion, and altered intercellular communication contribute to skeletal muscle ageing and the pathophysiology of sarcopenia. We also highlight five novel hallmarks of particular significance to skeletal muscle ageing: inflammation, neural dysfunction, extracellular matrix dysfunction, reduced vascular perfusion, and ionic dyshomeostasis, and discuss how the classic and novel hallmarks are interconnected. Their clinical relevance and translational potential are also considered.
Keywords: hallmarks of ageing, sarcopenia, skeletal muscle
Introduction
Hallmarks have been traditionally used as organising principles to identify distinctive characteristics or underlying biological causes of a process such as ageing in many human tissues and animal models [1–3] and disease [4,5]. Nine unifying hallmarks of biological ageing, termed primary, antagonistic, or integrative hallmarks, have been proposed involving genetic and biochemical pathways that collectively influence ageing trajectories and susceptibility to pathology in humans [1]. These are genomic instability, telomere attrition, epigenetic alteration, loss of proteostasis (primary), deregulated nutrient sensing, mitochondrial dysfunction, cellular senescence (antagonistic), stem cell exhaustion, and altered intercellular communication (integrative). Recent addition of new hallmarks such as compromised autophagy, chronic inflammation, and dysbiosis [2,3], altered mechanical properties and splicing dysregulation [3,6] emphasises the complexity of the ageing process. As originally proposed, experimental manipulation of these hallmarks may either accelerate or ameliorate mammalian ageing [1,2]. Hallmarks have been used as a contextual framework to classify the multiplicity of mechanisms governing normal ageing in tissues and body systems [7,8] and they have been mapped to age-related diseases [4,9].
This review investigates the relevance of the hallmarks of ageing to the specific situation of ageing skeletal muscle and sarcopenia, a condition characterised by progressive and generalised loss of skeletal muscle strength, mass, and function [10,11]. Here we give a broad overview of the main mechanisms that are likely to drive the pathophysiology of sarcopenia in normal skeletal muscle of ageing women and men in the context of these hallmarks. This focus on human rather than animal skeletal muscle biology also allows consideration of the clinical relevance and translational potential of hallmarks for sarcopenia.
Specifically, this review addresses the following four objectives to:
Evaluate the nine classic hallmarks of ageing and highlight five novel hallmarks potentially most relevant for ageing skeletal muscle and sarcopenia in humans
Highlight the existence of large literature involving animal studies and a relative paucity of human studies particularly in older women
Emphasise the interconnectedness of hallmarks and need for interdisciplinary approach to integrate biology of ageing muscle
Identify clinical relevance and translational potential of hallmarks for sarcopenia.
The review has three main parts. The first and second parts (Human skeletal muscle and ageing and Hallmarks of ageing in skeletal muscle and sarcopenia) address objectives 1 and 2, and the third part (Clinical relevance and translational potential) discusses objectives 3 and 4, followed by Conclusions.
Human skeletal muscle and ageing
Maintaining skeletal muscle health in terms of muscle strength, mass, and function (physical performance) [12], is a prerequisite to increase the healthspan [13,14]. Skeletal muscle comprises approximately 40% of total human body mass and is a complex tissue [15] that serves multiple functions, from main mechanistic contraction for movement, to thermogenesis and metabolism [16].
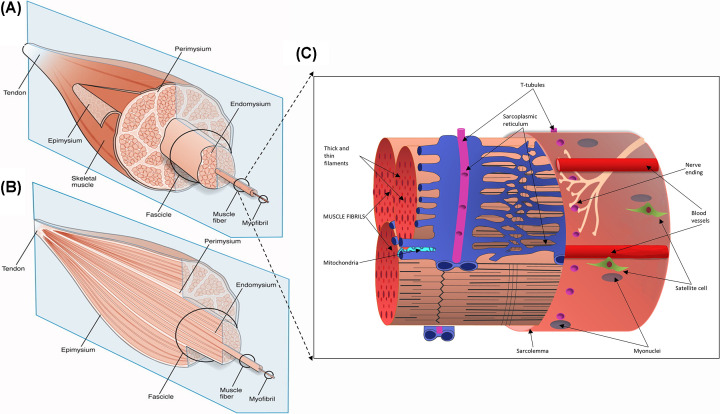
Skeletal muscle tissue consists of long contractile multinucleated myofibres filled with specialised contractile proteins organised into sarcomeres, with invaginations of the plasma membrane (sarcolemma), known as T-tubules to facilitate rapid and coordinated conversion of excitation into contraction, and mitochondria tethered at sites of high energy need. Each myofibre is connected to a nerve via the neuromuscular junction (NMJ) to stimulate myofibre contraction and there is a rich vascular supply with a network of capillaries around the myofibres (Figure 1). Specialised extracellular matrix (ECM) rich in laminins, known as the basal lamina (or basement membrane) is in intimate contact with the sarcolemma of each myofibre. In mature muscles, mononucleated muscle precursor cells called satellite cells are located on the myofibre surface between the sarcolemma and basal lamina [16,17] (Figure 1): these cells are responsible for muscle regeneration following necrosis resulting from injury. Other mononucleated interstitial cells include fibroblasts, adipocytes, and mesenchymal stem cells, surrounded by complex ECM molecules.
Figure 1. Schematic diagram of skeletal muscle tissue and of a single muscle fibre organisation.
Panels (A,B) present schematic diagrams of the skeletal muscle tissue and muscle extracellular matrix (ECM)-tendon organisation. The muscle ECM is categorised into epimysium (a layer surrounding the entire muscle), perimysium (a layer surrounding muscle fascicles or the muscle fibre bundles, which are further grouped together to form the muscle tissue), and endomysium (a basal lamina that is in intimate contact with individual myofibres). In the longitudinal section of the muscle (panel B), the endomysium is enclosed within the fascicles, whereas the perimysium is presented continuously with the tendon. Panel (C) represents a single myofibre comprised of the myofibrils organised into sarcomeres enclosed in the sarcolemma. The sarcoplasmic reticulum entangles the fibrils, and the transverse (T) tubules intersect them. Mitochondria are secured near the T-tubules to sarcoplasmic reticulum junction and (or) are found in subsarcolemmal regions. Along the length of the myofibres are nerves (attached at the NMJ) and capillaries (often near satellite cells).
Panels A and B from Gillies, A.R. and Lieber, R.L. (2011) Structure and function of the skeletal muscle extracellular matrix. Muscle Nerve 44, 318–331. Panel C was adapted from [15] and used with the permission of Wiley.
Most adult human muscles are a mixture of slow-twitch type 1 (oxidative) and fast-twitch type 2 myofibres (glycolytic) [18] (Figure 2A), with the myofibre type being primarily defined by a motor nerve (motorneuron) activity [19]. Slow and fast myofibres differ by their contractile, biochemical, and metabolic phenotypes, contributing to the heterogeneity of over 600 muscles in the human body that differ in their architecture and function [16,18–25].
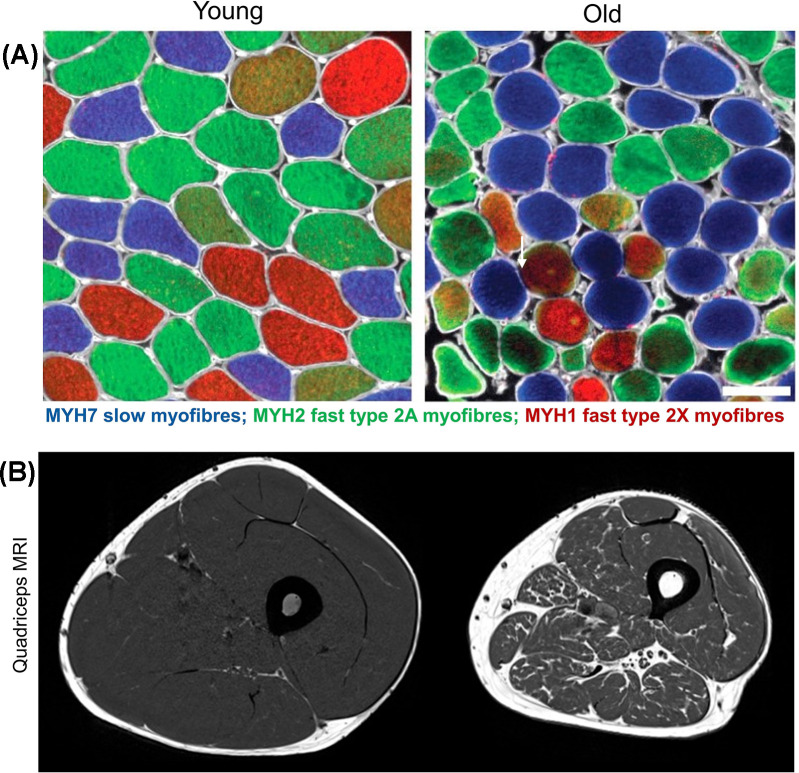
Figure 2. Comparison of skeletal muscle morphology and architecture in young and old adults.
Panel (A) depicts representative cross-sections of the vastus lateralis (VL) muscle biopsies from young (left; aged ∼24 years) and old (right; aged ∼70 years) healthy, active men, immuno-stained with antibodies specific to adult myosin heavy chain (MYH) isoforms: blue (anti-MYH7, slow type 1 myofibres), green (anti-MYH2, fast type 2A myofibres), and red (anti-MYH1, fast type 2X myofibres) (scale bar: 100 μm). Compared with the relatively uniform size of myofibres in young muscles (left; Panel A), the main features of old muscle are a wider range (variability) of size and shapes especially in type 2 myofibres (right; Panel (A), white arrow). Panel (B) shows a magnetic resonance imaging (MRI) of human thigh with area of quadriceps muscle (grey) and surrounding fatty tissue (white) in young (left) compared with loss of muscle mass in older men (right).
Panel (A) from [38] was used with the permission from Cell Press. Panel (B) from Herrmann, M., Engelke, K., Ebert, R., Müller-Deubert, S., Rudert, M., Ziouti, F. et al. (2020) Interactions between Muscle and Bone-Where Physics Meets Biology. Biomolecules10, 432, with permission from MDPI.
Age-related decrease in muscle mass and strength starts around the fourth decade of life [26–28], and accelerates in later life [26,29]. Estimates from longitudinal studies of adults (aged ≥75 years) show annual loss in muscle mass of 0.64–0.70% in men and 0.80–0.98% in women, with an even steeper decline in muscle strength of 3–4% in men and 2.5–3% women [29]. Skeletal muscle is malleable organ responsive to intrinsic and extrinsic stimuli such as exercise, diet, and inflammation across the lifecourse [22,26–29]: sarcopenia is characterised by a decline in muscle mass and function beyond the normal clinically defined cut-offs [10,11,28]. Magnetic resonance imaging (MRI) of old human thighs (vastus lateralis, VL) shows decreased lean muscle mass and replacement of muscle tissue by fat (Figure 2B), which accounts for deterioration of muscle quality and function in sarcopenia. However, the age-related changes are not uniform across all muscles and the extent of sarcopenia varies between muscles in different locations with different function [25].
At the cellular level, some key features of skeletal muscle ageing are increased myofibre variability and decreased myofibre cross-sectional area (atrophy), as demonstrated by analyses of biopsied muscle tissue sections (Figure 2A); also net loss of myofibre numbers [23,30,31] (reviewed in [32–35]) and functional denervation of myofibres caused by destabilisation of NMJs [23,36]. To this end, fast type myofibres are more affected compared with slow, a phenomenon known as preferential atrophy and loss of type 2 myofibres [35]; many of these fast myofibres become denervated and are re-innervated by slow motorneurons, so they survive but lose their original identity [22–25,30–38]. We consider that loss of motor-innervation is a hallmark of skeletal muscle ageing [37] (see Hallmark: Neural dysfunction). Additionally, single-myofibre proteomics reveal metabolic changes in fast, but not slow, myofibres in old versus young men [38]) (see Hallmark: Deregulated nutrient sensing).
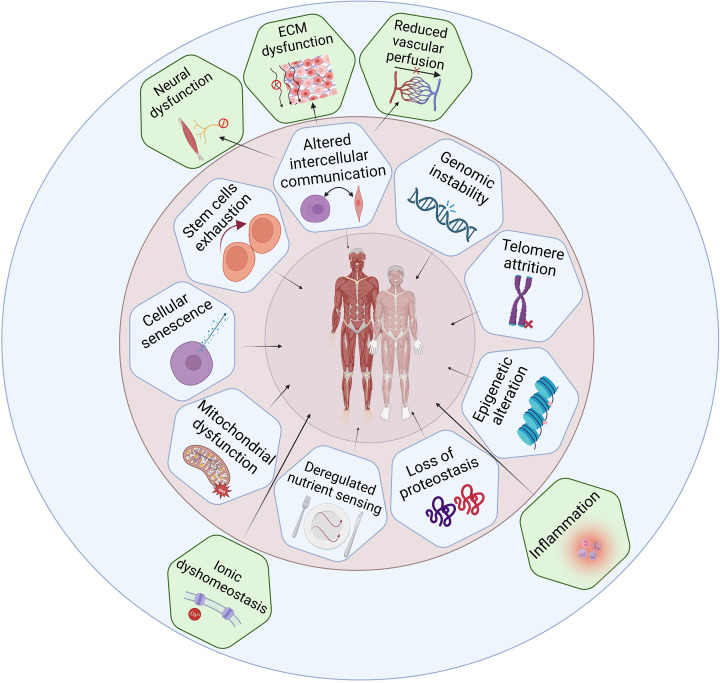
The mechanisms underlying sarcopenia in ageing human muscles are complex [14,39–41] and the interconnectedness of cellular components and body systems, sex-specific differences, and cross-species comparison makes understanding the predominant driving mechanisms challenging [42,43]. Here we evaluate the relevance to ageing skeletal muscle and sarcopenia for each of the classic nine hallmarks of ageing [1] and suggest five novel skeletal muscle-specific hallmarks (Figure 3).
Figure 3. Hallmarks of ageing as applied to human skeletal muscle.
Hallmarks of ageing were evaluated for their involvement in skeletal muscle ageing and sarcopenia. The nine classic hallmarks [1] are depicted in the inner (pink) circle. The outer (blue) circle highlights potential new hallmarks of skeletal muscle ageing and sarcopenia. Created with BioRender.com.
Hallmarks of ageing in skeletal muscle and sarcopenia
Genomic instability
The accumulation of genetic damage caused by endogenous and environmental factors is a key feature of ageing and age-related disease [44,45] inversely associated with the lifespan in mammals [46]. This manifests in various forms, including somatic mutations (e.g., point mutations, translocations and deletions occurring in nuclear and mitochondrial (mt) DNA), telomere shortening, and chromosomal aneuploidy. Loss of heterochromatin, resulting in de-repression and activation of retrotransposon activity is another consequence of ageing potentially leading to somatic mutations [47,48]. DNA damage that escapes the DNA damage detection or subsequent illigitimate repair -the machinery of which also becomes error-prone with age [49] -and activation of repressed genome elements, may cause detrimental changes in gene transcription and translation, resulting in dysfunctional cells that, if not cleared, contribute to dyshomeostasis of tissues and organs. Here, we briefly discuss the relevance of nuclear and mtDNA alterations and activation of retrotransposable elements (RTEs) in human skeletal muscle with ageing.
Threre are many factors that contribute to DNA damage in old tissues, including skeletal muscle, but the direct correlation to ageing is not fully elucidated (reviewed in [50]). Reactive oxygen species (ROS) such as free radicals are regarded as a major cause of damage to DNA (nuclear and mitochondrial) and also proteins, lipids and other cell components (reviewed in [51]) in skeletal muscles. ROS are naturally produced during muscle metabolism, contraction, regeneration, inflammation, and hypoxia [50,52]. Damaged DNA can contribute to muscle ageing by altering gene expression and inducing cellular senescence (see Hallmark: Cellular senescence). Evidence for other types of DNA damage, however, in ageing and sarcopenic skeletal muscle is limited. In an early study of 66 adults aged 25–93 years (47% women) 8-hydroxy-2-deoxyguanosine, a marker of oxidative DNA damage was substantially increased in VL and vastus medialis muscle with age [53]. Oxidatively damaged DNA can block transcription, decrease protein synthesis and degradation, and attenuate synthesis of key muscle proteins (e.g., actin and myosin), consequently decreasing muscle strength and function (reviewed in [50,54]).
It is well established that chemotherapy and radiation cause excessive DNA damage in cancer and normal cells triggering mutagenesis, senescence, and apoptosis (reviewed in [55]). Chemotherapy may further contribute to DNA oxidation and damage by increasing ROS and oxidative stress in ageing muscle [56]. Studies with middle aged and older cancer patients undergoing antineoplastic treatments for various cancers have observed exacerbated loss of muscle mass (cancer cachexia) and increased risk of sarcopenia (loss of muscle mass and function) by not fully understood mechanisms (reviewed in [56,57]). However, reports also show muscle gain or no change in muscle mass in subpopulation of cancer patients with stable clinical course of the disease [56,58], including older patients [58]. Taken together, these examples indicate a complex relationship between DNA damaging oncologic agents, cancer cachexia and sarcopenia in cancer patients.
Mitochondrial DNA represents 0.93% of total DNA in human skeletal muscle (reviewed in [59]). An increase in deletions and point mutations in mtDNA in post-mitotic tissues such as skeletal muscle has been observed during normal ageing in studies with bulk muscle tissue (reviewed in [60]) [61,62] and in myofibres [63]. Histochemical analyses of 12 VL muscle biopsies from men and women aged 49–92 years, showed that older muscles have higher number of myofibres with electron transport system (ETS) enzymatic abnormalities and respiratory chain deficiency (from 6% to 31%) [63]. Notably, all myofibres with the ETS abnormalities were harbouring mtDNA-deletion mutations as shown by polymerase-chain reaction (PCR) [63]. Another study used high-throughput droplet digital PCR for quantification of mtDNA deletion frequency in 14 VL muscle biopsies from men aged 20–80 years [61] and found a 98-fold increase of these deletions between the youngest and the oldest age [61]. A follow-up study by the same group showed an 18-fold increase (from 0.008 to 0.15%; 10.4%/year) in deletions from ages 50–86 years in men and women, which correlated with a lower physical performance [62].
Another ultra-sensitive high-throughput mtDNA deletion detection method called LostArc [59] was developed to assess the full deletion spectrum across the mtDNA genome of myofibres in VL muscle in individuals aged 17-93 years. This showed that, while mtDNA levels and copy numbers are not affected by age, deletion rates increase with age favouring genes that support electron transport and the oxidative phosphorylation (OXPHOS) in older adults and sparing those involved in mtDNA replication [59]. However, mtDNA ablations (the deleted mtDNA fraction) varied by age and increased linearly after age 60, possibly contributing to mitochondrial dysfunction in older muscles [59].
Taken together, destabilisation of the mitochondrial genome observed in ageing skeletal muscle may lead to dysfunctional ETS, focal respiratory chain deficiency, decline in energy production and myofibre atrophy [64] and thus contribute to sarcopenia. Decline in mitochondrial function as a hallmark of skeletal muscle ageing is discussed further in Hallmark: Mitochondrial dysfunction.
Increasing evidence suggets that transposons (retrotransposable elements, RTEs), genetic sequences that can move within the genome, play a role in ageing and age-related diseases in eukaryotes [47,65,66]. The human genome comprises 35% of RTEs; the activation of a small sub-set of those that are functionally active in adult human somatic tissue appears to be harmful and may promote age-related phenotypes [66–68]. RTEs act by triggering DNA damage, mutagenesis, aberrant transcription, alternative splicing, genomic instability, innate immune response, and inflammation [47,69–71]. To counteract their activity, organisms have developed several mechanisms for silencing active RTEs such as DNA methylation, histone modification, and RNA silencing pathways [65,70,72].
The only active RTE in the human genome are LINE1 (long-interspersed element), which comprises 17% of the human genome [65]. Activation of LINE1 has been shown in senescent human fibroblasts in vitro [48], and old rodent tissues, including skeletal muscle [73,74]. Studies that describe activity of RTEs in human muscle ageing are limited (reviewed in [75]). One human study showed de-repression of LINE1 and the resulting increase in LINE1 mRNA VL muscle biopsies in 13 older men and women aged (58 ± 8 years), compared with 15 younger participants (aged 23 ± 3 years) [76]. In the context of ageing, increased LINE1 mRNA expression results in cytoplasmic accumulation (rather than retrotrasposition) of LINE1 cDNA and this, in turn, induces type-1 interferon (IFN-I) response and activation of pro-inflammatory pathways (inflammaging) in mice [73]. To this end, increased interferon-responsive genes and inflammation are a shared feature of ageing skeletal muscles, as well as other tissues, in rodents [77,78] and with some markers also observed in humans [6]. One study in humans proposed that LINE1 expression in skeletal muscles may be suppressed by exercise [75] but these initial findings require further confirmation.
In summary, emerging evidence from human studies indicates that oxidative damage to nuclear DNA, mtDNA alterations and transposons may play a role in muscle ageing and possibly sarcopenia by promoting mitochondrial dysfunction and inflammation, and cellular senescence.
Telomere attrition
Telomere dynamics are proposed as a vital component of human ageing [79] characterised by a progressive shortening of telomeres (repetitive DNA sequences at the ends of chromosomes) in dividing cells, which triggers a DNA damage signal response and replicative senescence in vitro [79,80]. Telomere lengths (TLs) have been studied across human [81,82] and rodent tissues [83] and often in comparison with blood cells (leukocytes), which are used as a reference for TLs of the entire organism and a biomarker of ageing [84]. Although human blood samples are relatively easy to obtain to measure leukocyte TLs, compared with (invasive) muscle biopsies (to measure TLs in myofibres, satellite cells, or muscle-associated mononucleated cells), the leukocyte TLs cannot be considered a meaningful biological marker for a multidimensional age-related condition such as sarcopenia [85]. Also, there is a great heterogeneity in (leukocyte) TLs at the intracellular, intercellular, and individual level established using various techniques [86], with no standardised protocol and hight intra- and inter-laboratory technical variations [87].
Human studies of skeletal muscle telomere dynamics with ageing are less comprehensive and overall show relative TL stability in myonuclei with age [81,88,89], and malleability to environmental factors (e.g., longer telomeres being associated with higher levels of physical activity compared with a sedentary lifestyle) [90,91]. Inter-individual telomere variability in muscle as a minimally proliferative tissue appears to be established largely in early life during the normal growth phase [92,93], but this conclusion needs to consider which specific cells these data relate to (as listed above). For example, the TLs of satellite cells decrease during the first two decades of human life (a period of muscle growth), while TLs in myonuclei remains constant from birth to 86 years, indicating stability and very low turnover [88].
In the Genotype-Tissue Expression (GTEx) project, TL analyses of over 20 tissue types from 952 individuals aged 20–70 years revealed high inter-individual variability in TLs in most tissues with ageing, except in skeletal muscle. However, when leukocyte TLs were used as a reference of the entire body TL, they correlated moderately with TLs of most tissues (r range 0.15-0.37) [81]. A comparative study of telomere attrition in the minimally proliferative (fat, muscle) and maximally proliferative (skin, leukocytes) tissues from racially diverse samples of men and women aged 19–77 years, observed comparable age-dependent telomere attrition rates per year [92]. Although TLs were the longest in muscle and shortest in leukocytes, they still correlated between the tissues [92]. In another study involving young and old healthy men (aged 18–87 years), TLs in muscle and leukocytes were correlated across the lifecourse (r = 0.26) [94]. Individuals with longer leukocyte telomeres had longer muscle telomeres. Taken together, these studies infer early life origins of the TL differences across the tissues and suggest a shared endogenous mechanisms of TL regulation.
Currently, it is not known whether muscle telomere dynamics associate with muscle strength and mass during ageing, since sarcopenia has been mostly explored in relation to leukocyte TLs in human studies. The results from the studies using leukocyte TLs as a reference for myofibre TLs are inconsistent and warrant further investigation [84,95] to clarify whether skeletal muscle telomere attrition plays any role in muscle ageing and sarcopenia.
Epigenetic alteration
Somatic cells are susceptible to epigenetic modifications, that change gene expression without modifying the base genetic code. DNA methylation and histone acetylation are the most studied epigenetic modifications, the former being well described in ageing skeletal muscle in bulk tissue [96–99]. Epigenetic changes are interconnected with other hallmarks of ageing and can lead to dysregulated nutrient sensing, mitochondrial dysfunction, and cellular senescence (discussed in [1,2]).
An altered epigenetic landscape in aged human skeletal muscle was first described by Zykovich et al. [96] using a genome-wide study of DNA methylation. DNA methylation arrays containing 450,000 CpG sites revealed hypermethylation across the genome in muscles from older men (aged 68–89 years) compared with younger men (aged 18–27 years). Over 5900 CpG sites were differentially methylated (dmCpG) between the groups, of which 92% were hypermethylated. The hypermethylation sites were under-represented in promoter regions and over-represented within the gene bodies (the central and 3′ regions), especially in genes that guide the formation of the NMJ. 500 CpG sites were able to distinguish between old and young muscle, creating the first epigenetic clock of muscle ageing.
A human muscle-specific epigenetic clock was then generated from 682 skeletal muscle samples and 12 independent methylome datasets (aged 18–89 years, 22% women, 99% white). This showed that the methylation status of 200 CpG sites can predict muscle chronological age [97]. Exploration of DNA methylation patterns revealed 180 differentially methylated regions (DMRs) with advancing age, equally balanced between hyper- and hypomethylation. A further update of the muscle epigenetic clock involved a large-scale epigenome-wide association study (EWAS) meta-analysis of skeletal muscle ageing from 10 studies and 908 muscle methylomes (men and women aged 19–89 years). The study identified over 6700 DMRs spanning >6300 unique genes involved in muscle structure development, contraction, and calcium transport regulation [98]. Global hypermethylation of human skeletal muscle with ageing and methylation patterns have been further confirmed in a large study involving 850,000 CpG sites in muscle tissue and isolated heterogenous muscle-derived human primary cells (HDMCs) from old (mean age 83 years) and young adults (mean age 27 years) [99]. Enriched hypermethylation in old muscle tissue was observed for various cellular pathways (e.g., mitogen-activated protein kinase [MAPK], phosphatidylinositol3-AKT-protein kinase B-mammalian target of rapamycin [PI3K-AKT-mTOR], and p53 signalling), axon-guidance, and Hippo-signalling pathway (proposed to control muscle mass and function [100]). Differential methylation analysis showed marked hypermethylation of the HOX genes (developmental regulatory and musculoskeletal patterning genes [101]) only in old human muscle tissue and cells [99].
The relationship between muscle methylome and sarcopenia have been investigated in a cohort of 83 older men (mean age: 76 years) from the Hertfordshire Sarcopenia Study (HSS) and HSS extension (14% with sarcopenia). The dmCpGs associated with sarcopenia were enriched in genes linked to myotube fusion (e.g., homophilic cell adhesion via plasma membrane adhesion molecules), oxidative phosphorylation, and voltage-gated calcium channels [102]. There was an overlap in the number of dmCpGs associated with sarcopenia and muscle mass, plus sarcopenia and muscle function (strength and gait speed) [102]. The results suggest that epigenetic alteration of specific genes may contribute to impaired muscle function in older men; yet to be confirmed in larger studies of older women [103,104].
Taken together, these results (mainly for older men), confirm DNA methylation of tissue-specific genes in skeletal muscle and their association with muscle characteristics, with flexibility of the muscle epigenetic landscape revealed by increasing detail in methylome sequencing and powerful EWAS meta-analyses and yet to be determined at single-cell resolution [105]. These data strongly support epigenetic alterations as a hallmark of ageing associated with sarcopenia; however, epigenetic studies of sarcopenia in older women are lacking.
Loss of proteostasis
A balanced process of protein synthesis and degradation controls myofibre size, protein content and protein renewal. Extensive literature suggests a decline in protein homeostasis (or proteostasis) as a hallmark of ageing and age-associated disease [1,2,9,106–108]. Dysregulation of proteostasis leading to myofibre atrophy and accumulation of misfolded and aggregated proteins has been relatively well studied in ageing rodents, with limited studies in humans [6,109–111]. These studies suggest a very complex mis-regulation of many aspects of proteostasis in old muscles.
An extensive discovery study that compared the proteome from VL muscles of healthy men and women (aged 20–87 years), found that the abundance of ribosomal proteins and chaperones decreases with ageing [6]. Depletion of ribosomal proteins may result in lower protein synthesis, protein turnover, and, ultimately, a failure to replace damaged contractile machinery, while a decrease in chaperones may result in diminished chaperone-mediated autophagy [6].
One key pathway that controls protein homeostasis in skeletal muscle is the AKT-mTOR complex 1 (mTORC1) pathway, which is dysregulated in old muscle. As discussed below, age-related dysregulation of this pathway has been widely studied in rodents, while human data are limited. In healthy muscles, activation of AKT downstream of anabolic factor receptors, such as insulin-like growth factor 1 (IGF-1), stimulates the mTORC1-dependent protein synthesis [112]. Paradoxically, at least in rodents, mTORC1 is hyperactivated in old muscles [113–116]. Such an increase in mTORC1 signalling is associated with progression of sarcopenia in rats and occurs in parallel with elevated markers of muscle protein ubiquitination and suppressed markers of autophagy [113–116]. To this end, therapeutic inhibition of mTORC1 signalling with rapamycin or its analogue (Everolimus) attenuates age-related loss of muscle mass and function in rodents [115,116]. Human data reporting the status of AKT/mTORC1 signaling in sarcopenia is limited, due to the paucity of standardised clinical studies. However, early clinical studies suggest that the AKT/mTORC1 pathway may also be mis-regulated in old human muscles [117,118], possibly with low efficiency of AKT signalling [117] and increased basal levels of phosphorylated mTORC1 and its downstream target S6K1 [118], these data being consistent with evidence in rodent sarcopenia.
Thus loss of proteostasis is endorsed as a strong hallmark of sarcopenia in rodents, with limited but emerging evidence in humans.
Inflammation
Low-grade chronic inflammation present during ageing also contributes to disturbed proteostasis and muscle atrophy. As mentioned above, age-related activation of RTEs and genomic instability may trigger an innate immune response, and inflammation. Intrinsic age-related dysregulation of the inflammatory system, and other cells of the innate immune response, affects many cellular events [119–121]. Transcriptomic and proteomic data from human and rodent muscles identify upregulated proinflammatory pathways as major hallmarks of ageing muscle [6,77,78,113,122,123]. Discovery proteomics in human muscles show that age increases expression of nuclear factor kappa-B (NF-κB) activators and decreased expression of NF-κB attenuators [6]. Increased inflammatory signalling may be one of the drivers of disturbed proteostasis in sarcopenia, since pro-inflammatory cytokines activate the NF-κB pathway to induce protein degradation via the ubiquitin–proteasomal pathway in humans and rodents [124] (reviewed in [125]). A study of 71 Brazilian community-dwelling older women (age range 66–96 years), that measured cytokines in blood as biomarkers of inflammation, showed highest blood levels of IL8, sTNFr-1, and sTNFr-2 for the more advanced sarcopenia [126].
Such age-related chronic inflammation is associated with increased ROS that can cause reversable and irreversible oxidation of DNA, proteins and lipids and other cellular components, with adverse effects on many tissues [51,52,127]. As a vicious cycle, damaged organelle macromolecules accumulate in aged cells and contribute to a pro-inflammatory state [120]. Indeed, a classic biomarker of ageing is lipofuscin that can provide a lifetime history of exposure to chronic oxidative stress: lipofuscin is an autofluorescent product of irreversibly oxidised macromolecules that accumulate in post-mitotic cells such as ageing human skeletal muscles [128].
Reactive oxygen species (ROS) are generated in several compartments and organelles within the muscle cells, including mitochondria, sarcoplasmic reticulum, and sarcolemma, and increased levels are strongly associated with inflammation. Under normal physiological conditions, ROS modulate many normal biological processes such as signal transduction, cell proliferation, stimulation of antioxidant systems, and apoptosis [50]. However, high levels of ROS can result in dysregulation of signalling pathways and oxidative damage to mitochondria, proteins, lipids, RNA and DNA in muscle cells, contributing to muscle atrophy and sarcopenia [52,129], with sustained inflammation and increased ROS implicated in many age-related disorders [51].
Increased chronic pro-inflammatory signalling in old muscles, may result from failing mitochondria quality control [130] (see Hallmark: Mitochondrial dysfunction) that is strongly linked to many age-related disorders [51], increased pro-inflammatory cells (see Immunoageing, part of Hallmark: Altered intercellular communication), and atrophic myofibres may also contribute; further studies are required to clarify these mechanisms. Additionally, as discussed above, de-repression of chromatin which results in exposure and activation of retrotransposons may partially be responsible for driving innate immune response and inflammation in old muscles [73,74].
In conclusion, this pro-inflammatory environment is endorsed as a moderate and emerging hallmark of skeletal muscle ageing and potentially sarcopenia in humans, as it may disrupt various aspects of organ homeostasis and function (see also Immunoageing), with a complex mis-regulation of many interconnected pathways.
Deregulated nutrient sensing
A nutrient is a substance used by an organism to grow, survive, and reproduce. They include energy-providing macronutrients (e.g., carbohydrates, proteins, fats) and micronutrients (e.g., vitamins, minerals) required for metabolic and physiological functions. There is a preferential atrophy of fast-twitch glycolytic (type 2X) myofibres with age [31,33,131–135], which accounts for the age-related reduction in human thigh muscle lean cross-sectional area [31,134]. Fast-twitch glycolytic myofibre atrophy also occurs in states of actual or perceived nutrient scarcity (e.g., starvation, cancer, and diabetes mellitus) [132,136] suggesting that deregulated nutrient sensing is an important hallmark of skeletal muscle ageing.
Insulin stimulates glucose uptake into myofibres, and low muscle mass is a risk factor for insulin resistance [137]. Glucose transporter (GLUT) 4 is the main insulin-regulated transporter in adult skeletal muscle [138] regulated by a complex process involving AKT activation (phosphorylation) [139]. Elevated basal mTORC1 activity [115,117] that inhibits AKT activation via a negative feedback loop may contribute to mis-regulated AKT signalling in old muscle. This could help explain the right-shift in insulin-glucose-dose-response curve with age (i.e., a greater insulin concentration is required for the same degree of glucose uptake) [140]. Skeletal muscle is responsible for 80% of postprandial glucose uptake [141], thus a right-shift in this relationship may account for a significant proportion of insulin resistance [142]. In fact, reduced skeletal muscle glucose uptake can precede Type 2 diabetes onset by 10–20 years [143]. However, the relationship between insulin resistance and skeletal muscle is bidirectional: older adults with sarcopenia have an increased risk of developing diabetes, whilst adults with diabetes have an increased risk of sarcopenia [144]. This relationship is emphasised by a study in 72-year-old men and women where reduction of daily activity for 2 weeks impaired insulin sensitivity and reduced leg lean mass [145] -an effect which persisted for two weeks after return to habitual activity [146].
Slow type 1 myofibres mainly use lipid as a fuel. Muscle lipid accumulation is associated with sarcopenia and has been linked with insulin resistance and mitochondrial dysfunction although the exact mechanisms remain unclear. Although some of this lipid accumulation is likely due to inactivity rather than ageing per se [147], the preferential oxidation of serum-free fatty acids, instead of intramyocellular lipid as well as larger lipid droplets that are not associated with mitochondria, are differences that persist when activity levels are controlled for [148–150]. Highly trained individuals also exhibit increased muscle lipid, but droplets tend to be smaller and associated with mitochondria [149]. This suggests the relation of lipid droplets to mitochondria as well as their absolute quantity is important.
As well as insulin resistance and increased lipids, older muscles display anabolic resistance; this term describes reduced protein synthesis in response to amino acids, insulin, and exercise triggers [151–154]. Although basal muscle protein synthesis seems not to be affected by age, response of old muscles to infused amino-acid-glucose mix is blunted [118].
It is possible that at least some of the age-related deficit in response to amino acid infusion is due to impaired vascularisation rather than contractile protein synthesis. When amino acid infusion is combined with sodium nitroprusside to induce local vasodilation, there is no longer an age difference in protein synthesis [155,156]. This implies that reduced skeletal muscle capillary density, and compromised endothelial wall function are two likely contributors [132].
AMP-activated protein kinase (AMPK) is an energy sensor protein that switches cell pathways between anabolism (protein and lipid syntheses) and catabolism (e.g., protein breakdown) in response to the intracellular AMP/ATP ratio or by phosphorylation. In a study of human twins, genetic factors had little effect on AMPK expression [157]. However, the expression the AMPK complex activated during exercise (α2β2γ3) was higher in fast-twitch fibres, higher in men (than women) and reduced with age [157]. This myofibre-type specific reduction with age accords with a rodent study that examined the contraction-evoked effects on AMPK activation in fast- and slow-twitch myofibres [158].
Overall, there is moderate evidence that altered nutrient sensing is a hallmark of skeletal muscle ageing and sarcopenia, linked with diabetes in a bidirectional manner in humans.
Mitochondrial dysfunction
Mitochondria are derived from early endosymbiotic bacteria. They are the main source of cellular energy, and have many other roles including hormone production, calcium buffering, and generation of ROS [159]. However, under pathological conditions mitochondria may produce excess or altered ROS, damaging cellular components (e.g., proteins, lipids, nucleic acids) and contributing to cellular and systemic inflammatory responses [159–162]. There is also emerging evidence that mitochondria may be key players in cellular senescence and the senescence-associated secretory phenotype (SASP) [163] (see Hallmark: Cellular senescence).
Decline in mitochondrial function appears to be a prominent hallmark of loss of skeletal muscle mass and function with ageing and inactivity [164] and is one of the few hallmarks directly linked to functional decline [165,166]. An increase in the number of COX− myofibres with age is a consistent finding in human skeletal muscle and correlates with accumulation of mtDNA mutations [54,167,168] (see Hallmark: Genomic instability). Above the age of 40 years, up to five COX− myofibres are considered within normal limits, while under 40 years these indicate pathology [168,169]. However, controversy exists regarding whether the reduced mitochondrial oxidative capacity is explained by reduced mitochondrial volume alone [149,170], or a deficit in oxidative capacity, in addition to reduced mitochondrial number/volume [171,172]. Genome-wide transcriptomic analyses show down-regulation of transcriptional signature of genes linked to mitochondrial proteostasis and function, in sarcopenic muscles of rats [77,113] and humans [122,160]. Sarcopenic individuals of different ethnicities demonstrate a decline in transcriptional signature of mitochondrial function [172]. Notably, transcriptional down-regulation of gene pathways linked with mitochondrial function (tricarboxylic acid (TCA) cycle, oxidative phosphorylation, mitochondrial respiration) have the strongest association with human muscle mass and function [172]. Congruent with gene expression data, discovery proteomics from skeletal muscles from people aged 20–87 years showed an age-related decrease in proteins related to energetic metabolism, including those related to the TCA cycle, mitochondria respiration, and glycolysis [6].
In terms of a link with inflammation, analyses of 669 adults from the Baltimore Longitudinal Study of Ageing showed association between low mitochondrial oxidative capacity and markers of chronic systemic inflammation [160], suggesting that damaged mitochondrial DNA (see Hallmark: Genomic instability) and excess production of ROS by dysfunctional mitochondria could trigger inflammation [160]. To this end, levels of circulating cell-free mtDNA were found to be an independent risk factor for sarcopenia [173].
Clearance of damaged and dysfunctional mitochondria via autophagy/mitophagy may be impaired in old skeletal muscles because of a compromised catabolic process [174] that may also contribute to inflammation [120]. Sustained activation of the mTORC1 signalling in sarcopenic skeletal muscles has been suggested as a mechanism that inhibit mitochondrial turnover (clearance) via supressing autophagy [175]. However, while activation of the mTORC1 signalling and benefits of pharmacological inhibition of this pathway in old muscles has been relatively well studied in rodents [115,116], human data are lacking.
Interestingly, healthy old muscles can also carry healthy mitochondria, with mitochondrial content and mitochondrial respiratory function preserved in skeletal muscles of 85+ year old men and women who were healthy, active and did not have a deficit in muscle strength [176]. Therefore, it is not clear if mitochondrial decline causes sarcopenia or is a result of sarcopenia [161]. However, decline in mitochondrial function is certainly a feature of sarcopenic muscle, and inactivity (which increases with age), and is likely a significant contributor to mitochondrial demise, since exercise improves oxidative capacity independent of age [177].
Cellular senescence
Cellular senescence represents a state of permanent cell cycle arrest in response to various stressors. Senescent cells arise via different senescence programs, including replicative senescence (i.e., telomere shortening), DNA damage-induced senescence, oncogenic stimulation, mitochondrial dysfunction-associated senescence, and oxidative stress-induced senescence [178,179]. Senescent cells accumulate with ageing and disease, in mitotic and post-mitotic human and animal tissues [180,181] hampering their regenerative capacity [123] and promoting disease development. Senescent cells secrete a range of extracellular modulators such as cytokines, chemokines, growth factors, and extracellular matrix degrading proteins termed SASP [182–184], which contribute to systemic dysfunction in ageing and disease [179,183]. Senescent cells are highly heterogenous at the transcriptomic level [123], and their identification and quantification remain difficult because of their scarcity [123] in the absence of a universal senescence marker [179,185]. Nonetheless, the presence of senescent cells has been described in multiple human tissues and implicated in the pathogenesis of several age-related diseases [181]. In animal models, the clearance of senescent cells has been shown to improve the ageing phenotype and alleviate age-related pathologies [186,187].
There is little information for human skeletal muscle in vivo, regarding the extent that senescent cells and SASP accumulate in post-mitotic myonuclei of myofibres, satellite cells, and other mitotic interstitial cells, and how they might contribute to muscle ageing and sarcopenia. Some observations in aged murine models with several markers of cellular senescence have been replicated in human studies, whereas others have not (reviewed in [188]). Early reports of bulk muscle tissue showed an increase in mRNA levels of the senescence-associated genes involved in cell cycle arrest/DNA damage (i.e., p21CIP1 and p53) in older women aged 65–71 years [189]. Cultured human myoblasts did not show elevated senescence markers p16INK4a, senescence-associated β-galactosidase (SA-β-Gal) (a marker of lysosomal overload), and DNA damage response marker γH2A.X [190] with ageing as observed in rodent studies [188]. Also, skeletal muscle transcriptome in the GESTALT study of bulk muscle tissue from 53 healthy humans (aged 22–83 years) showed differential expression of mRNA encoding proteins of cellular senescence, but not p16INK4a protein [191], a primary mediator of cell-cycle arrest and a promoter of cellular senescence [192].
Studies using bulk muscle tissue fail to determine the spatial distribution of the signal across different cell-types. This was addressed recently in a comprehensive assessment of young and aged mice and 52 human muscle biopsies (including 22 older adults aged 69.8 years) [193] with spatially resolved methods of single myofibres [194]; and also in a lifecourse study of 40 middle-aged and older adults [195]. qPCR revealed increased p16INK4a and p21CIP1 mRNA expression in older human muscle compared to young, which were negatively associated with muscle oxidative capacity, maximum oxygen consumption, and strength (leg extension) [193]. Immunohistochemistry staining revealed higher frequency of p16INK4a-positive nuclei (within and outside human myofibres) and higher frequency of γH2A.X staining colocalising to telomeres (i.e., telomere-associated DNA damage foci or TAF) [193]. Senescence markers HMGB1 (High Mobility Group Box 1), TAF, and Lamin B1 were associated with muscle mass and function in the lifecourse study and observed to be stronger in women than in men [195]. Taken together, the results revealed the core elements of the senescence programme in aged human muscle decline, with implications for muscle quality and function [193,195].
A combination of single-cell transcriptomics and a senescence-cell enrichment sorting protocol [123] detected a new senescence-cell niche comprised of three main cell populations (satellite cells, fibroadipogenic progenitors, and myeloid cells) in regenerating muscles after experimental injury, for young (3–6 months) and old (>28 months) mice. Also, human muscles in vivo with damaged areas (aged 69–85 years) were characterised by upregulated cellular stress pathways (oxidative and metabolic) and downregulated DNA-damage and mitochondrial response pathways implicated in inflammation and fibrosis [123]. These senescent cells and their inflammatory secretome can blunt muscle regeneration in vivo after experimental injury in young and old mice [123].
The role of SASP proteins in human muscle ageing was investigated in the LIFE study of over 1,300 older women and men aged 70–89 with sedentary lifestyle and the risk of mobility disability (Short Physical Performance Battery [SPPB] score 7–10). The top 10 SASP proteins in blood (e.g., actin A, VEGFA, IL15, IL6, and MMP7) were inversely associated with disability and the SPPB score and its individual components [196]. These SASP biomarkers had superior predictive power for poor physical performance (SPPB ≤7), slow gait speed (≤0.8 m/s), low muscle strength (grip strength <16 kg [women], <27 kg [men]), compared with models with only age, sex, race, and BMI [196].
In summary, the results of these studies indicate that senescent cells and SASP may contribute to muscle ageing and poor muscle function in older sedentary adults; however, a direct association with sarcopenia is unclear as a basis for senescence to be explored as a possible therapeutic target (reviewed in [197,198]).
Stem cell exhaustion
The main myogenic stem cells of interest in skeletal muscle are a sub-population of satellite cells. Satellite cells give rise to myoblasts during regeneration, they are a heterogeneous population, and the proposal that some intrinsic decline in satellite cell function contributes to human sarcopenia has attracted much attention, with many controversies (reviewed in [199,200]).
The proposed role for satellite cells during sarcopenia assumes that there is extensive intrinsic myonecrosis and regeneration occurring in normal human muscles throughout life: yet this does not seem to be the case. It is widely recognised that regeneration of normal human muscles is of vital importance in response to myonecrosis that usually results from major accidental damage, surgery, or experimental injury. However, in most human muscles (in the absence of major injury, or excessive exercise), it appears that intrinsic myonecrosis is a rare event during activities of normal daily life, even in response to strenuous exercise (reviewed in [22,201]), as discussed below.
Low myonuclei turnover and intrinsic myonecrosis throughout life
Human skeletal muscle is a relatively stable tissue with little turnover of post-mitotic myonuclei because TLs in these myonuclei remains almost constant from birth to 86 years [88]. This conclusion is supported by radioisotope labelling of nuclei in human muscles [202] and comprehensively reviewed in [203,204] (see Hallmark: Telomere attrition). Compelling evidence for minimal turnover of myonuclei throughout the lifespan comes from experiments in mice where satellite cells were eliminated from all muscles of young adult mice, with no subsequent impact on manifestation of sarcopenia in very old sedentary mice [205], indicating no requirement for adult myofibre size maintenance [206]. This conclusion implies no regular satellite cell-dependent regeneration in these ageing mice, and thus no intrinsic incidence of myonecrosis.
For human muscles across the lifespan, there does not appear to be histological evidence of intrinsic myonecrosis reported [207], although this may be hard to encounter in small muscle biopsies [208] (Figure 2). Morphological changes in very old muscles, such as small myofibres and central myonuclei, may have been mis-interpreted as resulting from regeneration (with assumed prior myonecrosis); instead, they are more likely to result from other changes during ageing such as atrophy, denervation, and myofibre splitting [201]. Further histological investigations would be useful to provide direct evidence of the incidence of myonecrosis in normal ageing muscles of human and other species and in response to damaging exercise.
Capacity for muscle regeneration and satellite cells myogenesis in older adults
Because it is difficult to induce myonecrosis in human muscles in vivo even when applying damaging eccentric exercise (reviewed in [22]), a group in Copenhagen established an experimental model to induce myonecrosis/regeneration in humans in response to physiological overload using electrically stimulated eccentric contractions [209]. When they compared the response of muscles from young (20–31 years) and older men (60–73 years) [210], muscle regeneration was similar in both groups; thus these in vivo studies emphasise that myonecrosis (and hence the need for regeneration) is rare in healthy ageing human muscle in response to normal daily activities including exercise. This study used heathy older individuals, with only minor deficits in muscle function [210]: thus it is hard to determine whether a similar competent regenerative capacity would be evident in muscles of very old adults with clinically diagnosed sarcopenia [211].
Old human satellite cells retain an excellent intrinsic capacity for myogenesis, which was confirmed by an in vivo study that transplanted human muscles (from cadavers) into immunodeficient mice, and there was no measurable difference in regeneration observed across the range of ages up to 78 years [212]. However, it is increasingly recognised that age-related progressive detrimental changes in the extrinsic environment, including altered inflammation and increasing fibrosis, can result in delayed kinetics of regeneration and impaired muscle formation in very old hosts [123,207,213,214].
Other roles for satellite cells in muscle ageing
Since a major role for satellite cells in the context of necrosis/regeneration does not appear to be supported for sarcopenia, this raises the issue of other possible roles for satellite cells in sarcopenia; such as satellite cell activation in response to transient contractile muscle damage, without fusion to the myofibre [210]: the consequences of this transient activation of satellite cells are not yet understood (reviewed in [22]). The experiment by Fry et al. [205] suggests that satellite cells might modify the ECM and reduce fibrosis, and there is increasing evidence to support some role for activated (and possibly quiescent) ‘non-fusing’ satellite cells for cross-talk with ECM and other components of muscle tissue [206]. Satellite cells are now known to communicate with myofibres, fibroblasts [206], and vascular endothelial cells [215], and other cellular components of muscle tissue with signalling that can involve NMJ [216], biomechanical interactions with the ECM and cilia on satellite cells [217], and the release of small extracellular vesicles (exosomes) [206]. The contribution of such cross-signalling involving satellite cells, to modulation of muscle homeostasis throughout the lifespan and sarcopenia remains to be determined.
In conclusion, while stem cells are of major importance during development for constructing skeletal muscles, evidence for a key role of myogenic stem cells in maintaining normal muscle mass throughout life is lacking, and stem cell exhaustion does not appear to be a relevant hallmark for sarcopenia.
Altered intercellular communication
Intercellular communication that includes systemic interconnectivity and important signalling between myofibres and other cellular components is the last of the classic nine hallmarks of ageing. Here we discuss extrinsic (outside the myofibres) factors that impact muscle ageing: immunoageing, neuronal dysfunction, extracellular matrix dysfunction, and reduced vascular perfusion. Another vital intrinsic component of myofibres ionic dyshomeostasis is also described.
Immunoageing
Age-related changes in inflammatory cells (inflammageing), and other immune cells are all covered by the term immunoageing. There are many systemic changes in the immune system with ageing with one striking aspect being exacerbation of a pro-inflammatory environment, associated with increased ROS (see Hallmark: Inflammation). Adverse effects of immunoageing on skeletal muscles are demonstrated by muscle wasting (atrophy), discussed previously (see Hallmark: Inflammation). Atrophy also occurs in response to cancer cachexia, that is increased in old mice (compared with young), and further exacerbated by anti-cancer therapies; which is ameliorated by immunomodulation of old macrophages [218], and improved recovery after disuse atrophy in old mice [219]. Similar adverse effects of immunoageing, and the benefits of immunomodulation, are evident for the kinetics of muscle regeneration after experimental injury in old mice [214,220].
Regeneration of old nerves is also impaired because of defective response of Schwann cells attributed to immunoageing, especially hyperinflammation, since the microenvironment of old uninjured nerves is characterised by chronic macrophage infiltration with elevated expression of cytokines, pro-inflammatory markers [221] and oxidative stress with irreversible oxidation of macromolecules [222]. A comprehensive review emphasises that immunoageing has major adverse effects on many aspects of regeneration after experimental injury of old muscles [223]; although intrinsic necrosis/regeneration in healthy muscles with ageing is not a regular occurrence. While there is strong evidence for immunoageing in animals and human, the evidence for broad immunoageing as a hallmark of human sarcopenia is overall moderate.
Neural dysfunction
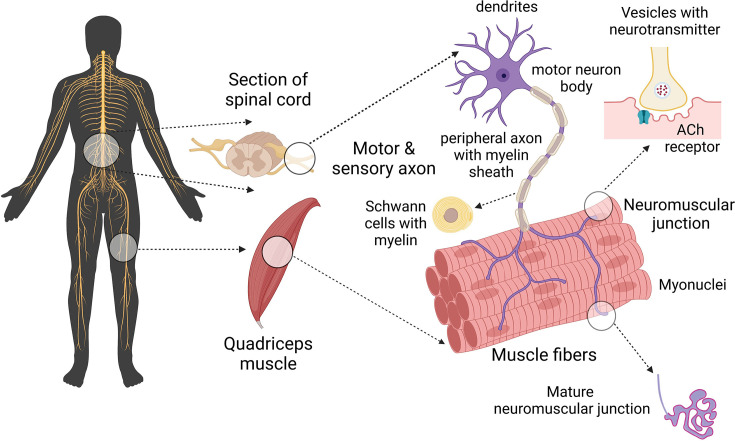
Efficient transmission of electrical signals via the motor neuron-skeletal muscle connection is critical for normal function of skeletal human muscle (Figure 4). There is very strong evidence of age-related changes in neuronal systems associated with loss of function and mass of old human muscles [224,225]. Major age-related changes in skeletal muscles of older humans, including loss of muscle mass (Figure 2), along with shifts in myofibre type were discussed briefly (see Human skeletal muscles and ageing [22–25,30–38]): the fast-to-slow myofibre transitions during ageing are further supported by proteomic studies [226]. The associated neuronal changes are extensive and include: demyelination of axons caused by oxidative damage to proteins and lipids [227], axonal atrophy, with altered ECM including increased collagen around nerves, loss of motor units, increase in motor unit size, with reduction in motor unit discharge rate, and motor unit remodelling [228,229].
Figure 4. Key components of motor unit and neuromuscular junction.
Schematic diagram of the motorneuron-skeletal muscle connection that is critical for the transfer of electrical signals for myofibre contraction. The motorneuron cell body in the spinal cord, sends an electrical signal down the motorneuron axon to the NMJ on the surface of an individual myofibre. The pre-synaptic nerve terminal release vesicles containing the neurotransmitter acetylcholine, this binds to receptors on the post-synaptic folds on the myofibre surface (sarcolemma). This signal is transferred along the myofibre surface and then into the T-tubules to initiate contraction. In mature human NMJs, the post-synaptic junction on each myofibre forms complex folds, a typical form of mature NMJ (in red; bottom right). The NMJ is innervated by a single motor axon (in purple; bottom right). Created with BioRender.com.
ACh receptor, acetylcholine receptor.
Also well documented are progressive age-related changes in NMJ morphology, including alterations at the pre-synaptic and post-synaptic membranes and terminal Swann cells, with modified transmission of the electric signal through the NMJs [230]. In contrast to rodent studies where there is extensive evidence of NMJ remodelling throughout life, relatively little is known about human NJMs (Figure 4), that are smaller and differ morphologically compared with rodent NMJs. The only comprehensive human study showed no evidence of morphological changes across the lifecourse for NMJs on peroneus longus muscles [231], with conflicting observations for other studies on intercostal muscles (discussed in [230]): differences in the extent of sarcopenia between these specific muscles may contribute to such discrepancies. However, there is strong evidence from many human studies that myofibre denervation likely contributes to the decline in physical function in sarcopenia via different mechanisms, including breakdown of the NMJ affecting a single myofibre, or death of a motorneuron leading to denervation or loss of all myofibres in that motor unit [232], or myofibre atrophy contributing to the NMJ breakdown and subsequent denervation. There is selective loss of large fast motorneurons (that innervate fast-twitch myofibres), with re-innervation of these ‘intact denervated’ myofibres by collateral sprouting of slow motorneurons throughout life (reviewed in [225,233]). Such remodelling indicates adaptation and a homeodynamic response to ageing, rather than homeostasis [234].
Confusion can arise when interpreting histological changes evident in normal old human muscles, such as atrophy of fast type 2X myofibres, small diameter myofibres and altered shape of myofibres with central myonuclei, which in other situations are attributed to regenerated muscles, since it seems likely that these may instead result from progressive denervation, atrophy, increasing fibrosis and splitting of myofibres due to remodelling [23,201,207,208,235].
Ageing also adversely affects the function of muscle spindles, small sensory organs within muscles (proprioceptors) that have a marked impact on gait, balance, and frailty [236]. Recent studies show that ageing reduces the sensory excitatory feedback from muscle spindles to motoneurons in the spinal cord, to compromise motorneuron function, with adverse effects on locomotion; demonstrated in mice initially and recently in old primates and humans [237,238]. Exercise has benefits on these age-related changes [239,240].
There is increasing recognition of the benefits of physical exercise on molecular markers of NMJ stability and myofibre denervation (reviewed in [241]) and neural markers such as motor unit discharge rate [242] in healthy older adults. Importantly, physical exercise is one of the few interventions that can prevent and mitigate sarcopenia (reviewed in [243–245]), with the adverse effects of sedentary behaviour emphasised [246].
Despite extensive evidence of neural dysfunction as a hallmark of human sarcopenia, it remains unclear whether sarcopenia is initiated and driven primarily by changes in nerves, or by myofibres, or both [247]. In humans, there is evidence that alteration in peripheral and central motor neuron excitability and changes in conduction velocity precede neuronal loss [248–251], but how these changes relate to simultaneous changes occurring within human muscle has, to our knowledge, not been explored. A lifecourse approach with a particular focus on the age around which muscle mass and different aspect of neuronal function first starts to decline [26] is needed to disentangle the relative contribution of nerves and myofibre to skeletal muscle ageing and sarcopenia.
Extracellular matrix dysfunction
The ECM that surrounds each myofibre and the whole muscle, is of crucial importance for skeletal muscle function (Figure 1). Basement membrane is specialised laminin-rich ECM in intimate contact with the myofibre surface (sarcolemma) which transfers and integrates the force, generated by contractile proteins within the myofibre, across the sarcolemma and out to strong collagens in the interstitial ECM compartment, to move parts of the body [252]. The ECM also plays major roles in muscle formation and regeneration (reviewed in [253,254]).
Complex changes in ECM gene expression across the lifespan are a feature of skeletal muscle in ageing rodents [113,255], and many differences in ECM composition are described for human and rodent muscles during ageing (reviewed in [256]). Analyses of ECM gene expression in muscles of young and older men (aged 70 years), showed changes in transcriptome of collagen I and some matrix metalloproteases (MMPs) and their inhibitors (involved in ECM remodelling), which were marked with age and in response to exercise [257]. ECM changes in older muscles, nerves and other tissues are widely reported in humans and animals, including higher collagen content and increased oxidation (glycation) and crosslinking, with decreased collagen turnover (reviewed [258]) that contributes to impaired function of old muscles [259]. Consequently, ageing is associated with pronounced interstitial muscle fibrosis and increasing ‘stiffness’ (i.e., reduced elasticity). Such altered stiffness affects biomechanistic, mechanotransduction and function, and can also impair myogenesis [22]. The complexity of changes in many ECM proteins and their turnover in response to different forms of exercise, unloading, and ageing in human muscles is the focus of a recent review [260]. Increased fibrosis also impairs myogenesis and re-innervation of nerves, with major implications for the efficacy of regeneration in old humans and animals [253].
Consistent reports state that the age-related loss of muscle mass alone cannot account for the extent of decline of muscle strength: across the neuromuscular system there is extensive remodelling with age, which involves muscles (with changes in architecture and pennation), fascia, and the central and peripheral nervous systems [256]. The altered architecture of old tendons may also contribute to altered biomechanics of contraction, as shown by a doubling in length of the myotendinous junction region with an increase in proximal tendon length (31%) for old mouse soleus muscles [261]. Further analyses of many muscles for mice aged 6–32 months emphasise that such ECM tendon remodelling and shortened myofibres (rather than myofibre loss) appear to play a role in the loss of both mass and function in sarcopenia [262]. Such observations emphasise the broad impact of age-related ECM remodelling in the context of sarcopenia which needs further investigations in human studies.
Reduced vascular perfusion
The dense capillary network surrounding skeletal muscle is dynamic-during muscle contraction blood flow can increase up to 100-fold and delivers oxygen and nutrients whilst removing waste products and heat [263]. There is a close anatomical association between capillaries and satellite cells [264], with more capillaries and satellite cells in slow type 1 myofibres (more reliant on oxidative metabolism) compared with fast type 2 myofibres [265]. Studies in young and old men (aged about 24 and 67 years) show that in old muscles the satellite cells of type 2 (fast) myofibres were located at a greater distance from the nearest capillary, and that a single bout of exercise increased the extent of capillarisation, decreased the distance between capillaries and satellite cells and increased satellite cell activation; demonstrating some of the many benefits of exercise on old muscles [266]. Increased skeletal muscle capillarisation is associated with increased muscle mass [267] and improved insulin sensitivity in men [268]. Despite the increased muscle mass, increased skeletal muscle capillarisation was not associated with greater post-absorptive muscle protein synthesis in older men [267]. However, increased skeletal muscle capillarisation is associated with a faster walking speed and less difficulty with daily activities in men and women [269]. Interestingly, sarcopenic subjects have reduced capillary contacts and a reduced capillary to myofibre ratio, with some evidence that the reduction in myofibre capillary contacts occurs prior to or simultaneously with (but not after) loss of muscle mass [270]. The lower capillary density in type 2 myofibres probably contributes to their increased vulnerability to age-related microvascular dysfunction [271].
In summary, human studies demonstrate that reduced myofibre vascular perfusion is an important hallmark of age-related decline in skeletal muscles, and potentially sarcopenia.
Ionic dyshomeostasis
Skeletal muscle contraction and ionic homeostasis are the major energy expenditures for myofibres, with each accounting for approximately 50% of ATP use [272]. Dysregulated calcium (Ca2+) homeostasis is one of the hallmarks of neuronal ageing [273] and there is evidence from several of the epigenetic (see Hallmark: Epigenetic alterations) and other physiological studies that it plays a role in skeletal muscle functional decline with age [274,275].
Skeletal muscle contraction and relaxation relies on massive Ca2+ efflux from the sarcoplasmic reticulum (SR) via ryanodine receptors (RyR1) and subsequent reuptake of Ca2+ into the SR by the SR Ca2+ pump. With age, RyR1 becomes progressively oxidated and nitrosylated causing Ca2+ leak and consequent SR Ca2+ store depletion and muscle weakness [274–276]. Mitochondria are tethered to the SR in the region of RyR1 [277] and SR Ca2+ efflux via RyR1 triggers mitochondrial ATP synthesis [278]. However, chronic RyR1 Ca2+ leak causes mitochondrial overload and dysfunction as evidenced by the cores (regions lacking mitochondria) that characterise RyR1 myopathies in humans. Although studies in human muscle are limited, in mouse models increased mitochondrial ROS production accelerates RyR1 Ca2+ leak [279], and RyR1 mutation causing Ca2+ leak impairs oxidative phosphorylation [280] -showing further evidence of the bidirectional link between RyR1 and mitochondria.
Skeletal muscle is critical for whole body ionic homeostasis. Extracellular K+ makes up approximately 2% of the total body K+ store [281] and of the 98% of K+ that is intracellular, approximately 80% is in skeletal muscle [281]. Maintenance of this transmembrane K+ gradient is performed by activity of the Na+/K+ pump and accounts for approximately 7% of skeletal muscle ATP use [282]. Maintenance of the Na+/K+ transmembrane gradient is critical for the initiation and propagation of an action potential.
However, there is evidence in humans that intramuscular Na+ increases with age [282–284] whilst intramuscular K+ decreases [284] thus reducing the transmembrane Na+/K+ gradient. A reduction of the transmembrane Na+/K+ gradient would be expected to depolarise skeletal muscle resting membrane potential and reduce excitability (the ability to generate and propagate action potentials). There is evidence of depolarisation of skeletal muscle resting membrane potential with age in humans [285,286] as well as reduced skeletal muscle excitability with age in rodents and humans [286–289].
As well as being central to muscle excitability, the transmembrane sodium gradient is important for a wide number of co-transporters [290,291]. The impact on molecules that rely on the Na+ transmembrane gradient for co-transport (e.g., amino acid transporters or insulin-independent glucose transporters) has, to our knowledge, not been directly explored. However, several studies from independent groups have found a greater accumulation of H+ and inorganic phosphate ions in older skeletal muscle from men and women following exercise [292–295]. This was not due to a deficit in ATP production [293] nor a deficit in perfusion [292]. Therefore, the mechanism of this proton and inorganic phosphate accumulation is not known. We speculate that it may be of relevance that two out of the three transporters that can extrude H+ from skeletal muscle are sodium dependent and bicarbonate import relies on the sodium gradient [296]. The wider impact of alterations in ionic homeostasis remains to be determined but is worth pursuing as a potentially tractable mechanism contributing to sarcopenia.
Clinical relevance and translational potential
The clinical relevance and translational potential of the proposed hallmarks of ageing skeletal muscle can only be realised by the field within a context of understanding the findings from human and animal studies to date. This review has sought to enable this through describing the nine classic hallmarks of ageing as first described by Lopez-Ortin et al. [1] and five novel hallmarks in the context of human skeletal muscle ageing and sarcopenia (Figure 3). We summarise the likely relevance of these hallmarks for normal ageing human skeletal muscle in Figure 5. This information is combined with text that comments on the implications for sarcopenia, based on early studies that did not differentiate between healthy ageing and sarcopenia, and more recent studies that made these distinctions based on clinical definitions of sarcopenia [10,11].
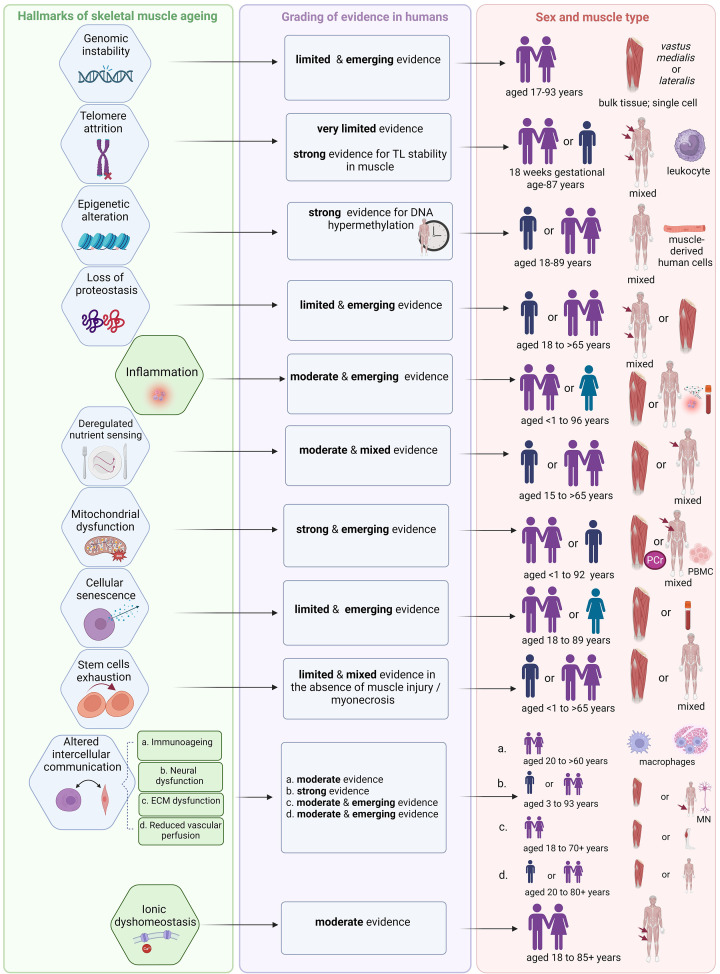
Figure 5. Summary of evidence from human studies for each hallmark of ageing applied to skeletal muscle.
For each of the nine classic (blue) and five novel hallmarks of ageing (green), the strength of evidence for human skeletal muscle ageing is graded in the middle column and depicted in the end column according to the sex (with age range) and type of muscle (vastus lateralis or mixed) most used in these studies. While specific data are available and emerging for some of these hallmarks in the context of sarcopenia (see individual Hallmark sections) these data are limited. Because of the relative paucity of studies for women and for investigating sex-specific differences across the lifespan for hallmarks of ageing, possible sex-related differences could not be determined at this time. For example, out of six individual studies included for Hallmark: Cellular senescence, only one feasibility pilot study explored senescence markers in men and women separately [195]. Moreover, consensus on clinical diagnosis of sarcopenia is still emerging: consequently, earlier studies likely included sarcopenic individuals who were not diagnosed as such. Therefore, at this stage, it is appropriate to evaluate the hallmarks based on evidence for normal ageing human muscle. This provides the background for progression of sarcopenia (as an adverse manifestation of normal ageing) [10,11] and, in limited cases, provides direct evidence of involvement of a hallmark in sarcopenia. Created with BioRender.com.
ECM, extracellular matrix; MN, motor neuron; PBMC, peripheral blood mononuclear cells; PCr, phosphocreatine by 31P magnetic resonance spectroscopy; TL, telomere length.
As indicated in Figure 5, the body of evidence to support loss of proteostasis, deregulated nutrient sensing, and mitochondrial dysfunction as major hallmarks of skeletal muscle ageing, is large and persuasive in animals, and limited, moderate and strong, respectively in humans. There is overall moderate evidence for the role of altered intercellular communication in skeletal muscle ageing in humans that, because of its complexity covering factors extrinsic to myofibres, we subdivided into immunoageing (includes inflammation), neural dysfunction, extracellular matrix dysfunction and reduced vascular perfusion. Evidence for the role of extracellular matrix dysfunction and reduced vascular perfusion is moderate but remain largely underexplored in individuals with diagnosed sarcopenia. Neural dysfunction has a strong role in human muscle ageing with some evidence that resilience to sarcopenia has a neural basis [228]: however, better understanding of changes in women is needed (Figure 5). Ionic dyshomeostasis is a novel hallmark, with moderate and emerging evidence from human studies of its involvement in skeletal muscle ageing but no evidence of its role in sarcopenia. The evidence for genomic instability and cellular senescence was limited but, especially in the latter case, has gained attention. Evidence for DNA hypermethylation (epigenetic alteration) in ageing human muscle was strong. However, the evidence for telomere attrition and stem cell exhaustion as key hallmarks of ageing in skeletal muscle is limited and weak.
This review includes a large body of literature investigating the role of the hallmarks of ageing in skeletal muscle and we make four key observations which potentially limit the clinical and translational potential. Firstly, although there is an abundance of superb scientific study in various animal models, there is a relative paucity of work confirming its translation into humans -this needs to be a priority. Secondly, there is a lack of diversity in the human participants of research studies for example characterised by under-representation of women. Thus, sex differences in the hallmarks of ageing in skeletal muscle and their role in the development of sarcopenia in men and women are outstanding questions and a priority for future work. Thirdly, few studies use a lifecourse approach involving participants across all ages with most human studies simply comparing young and old. To identify mechanisms and develop therapies for sarcopenia, the lifecourse approach adds a unique value for advancing translational research [42] (reviewed in [297]).
Impact of exercise and nutrition
Despite the intense research into molecular targets and potential drug candidates for sarcopenia using in vivo and in vitro models [298], the only intervention in human studies that has shown translational potential for sarcopenia [299], by possibly attenuating several hallmarks of ageing, is exercise [300–303]. Many reviews support the pleiotropic and system-wide benefits of regular exercise (both aerobic and resistance), with the potential to counteract age-related diseases, including sarcopenia, by ameliorating hallmarks of ageing [300–303]. Although the relationship between exercise and the hallmarks of skeletal muscle ageing is outside the scope of this review, several pertinent observations are highlighted here. These include studies showing malleability of telomeres in myonuclei due to exercise (i.e., endurance exercise and strength training) [89,90], benefits of exercise on molecular markers of NMJ stability and myofibre denervation (i.e., life-long endurance and resistance exercise) [241], ionic homeostasis (i.e., isometric contractions exercise) [292–295], favourable ECM gene expression involved in ECM remodelling (different resistance exercise modalities) [257], protein turnover [260] and capillarisation, and satellite cell activation in response to exercise in older muscles (i.e., resistance exercise, sedentary versus physically active lifestyle) [265]. Although these studies varied by the type of exercise, duration and intensity of exercise programmes, and the terms used to define self-reported physical activity (thus preventing any meaningful in-depth evaluation of their differential effects on the hallmarks of ageing), they all endorse translational benefits of exercise for better muscle ageing. Exercise has the potential to target multiple hallmarks of skeletal muscle ageing and is the only intervention shown to prevent and mitigate sarcopenia in humans (reviewed in [243–245]) [299].
Evidence from human randomised controlled trials has been accumulating for the beneficial effects of nutritional supplements such as whey protein (with or without vitamin D) [304] and omega-3 fatty acid supplementations [305] in muscle function in older adults with frailty and sarcopenia. There is a vast literature investigating various combined interventions of exercise and nutritional supplements and future work needs to determine how these might ameliorate hallmarks of ageing [306] in the context of skeletal muscle. Another promising area or research related to nutrition includes the gut and microbiome dysbiosis [2] during skeletal muscle ageing [307]. Valuable studies in mice show that changes in the gut microbiome via bacteria depletion, faecal transplantation, and various supplements (e.g., probiotics, prebiotics, and short-chain fatty acids) directly affect muscle phenotypes. Mechanistic studies in mice reveal that these treatments may ameliorate different cellular mechanisms and hallmarks of ageing (e.g., mitochondrial dysfunction, lipid oxidation, inflammation, and muscle fatigue). However, human data related to the role of microbiome and skeletal muscle mass and function have been inconsistent [307] and little is known yet about how the gut microbiome may regulate muscle with ageing.
Intercellular connectivity
Although each hallmark is distinct, they are intricately linked and often influence each other creating a network of interactions that drive the ageing process (Figure 3). The interconnectedness, integration, and entanglement of hallmarks of ageing has been discussed in detail in López-Otín et al. landmark papers [1,2]. Recent evidence about causes of mammalian ageing using a system termed ‘ICE’ (inducible changes to the epigenome) in animal models revealed that the cellular response to double-strand DNA breaks erode the epigenetic landscape and advance ageing via other mechanisms (hallmarks), including senescence and DNA methylation [308]. Here we briefly highlight the following hallmark interconnectedness relevant for skeletal muscle ageing. For example, genomic instability can lead to mitochondrial dysfunction which impairs oxidative phosphorylation, impacting the ability to maintain ionic homeostasis and, therefore, neural signalling. Circulating mtDNA released by damaged mitochondria may drive chronic inflammation. Such inflammation is exacerbated by senescent cells that secrete pro-inflammatory factors-triggered by cytosolic mtDNA [163] -further driving senescence and oxidative stress. Also of increasing interest is wider interconnectivity between skeletal muscles and the brain via circulating systemic factors produced by contracting muscles, with links between sarcopenia and many aspects of cognitive dysfunction [166,309,310]. These diverse examples emphasize the interconnectedness of the hallmarks of ageing muscle and sarcopenia, and the complexity and multifaceted nature of the ageing process.
Consensus definition of sarcopenia
Progress in clinical and translational research for sarcopenia depends not only on synthesising and recognising the interconnectedness of cellular and molecular findings from representative human studies across the lifecourse but requires an agreed consensus definition of sarcopenia [311]. Recent meta-analysis of observational studies revealed seven definitions and diagnostic criteria for sarcopenia, the European Working Group on Sarcopenia in Older People (EWGSOP) being one of them [312]; and the Global Leadership Initiative in Sarcopenia (GLIS) aims to develop a single clear definition of sarcopenia that can be utilised worldwide [12]. A single clinical definition of sarcopenia could facilitate human studies that employ a lifecourse approach and involve diverse participants. Such studies, focussed on the most promising hallmarks with strongest human evidence (Figure 5) will be key to realise the clinical relevance and translational potential of hallmarks research linked to ageing skeletal muscle and sarcopenia.
Conclusions
This review provides a broad overview of the importance of hallmarks of ageing to the specific situation of human skeletal muscle and their implications for sarcopenia. We conclude that there is strong evidence for epigenetic alteration, mitochondrial dysfunction, neural dysfunction, and moderate evidence for inflammation, deregulated nutrient sensing, immunoaging, ECM dysfunction, and reduced vascular perfusion as hallmarks for skeletal muscle ageing, with their relevance for sarcopenia evolving.
We recognise that many human studies use only one muscle source (vastus lateralis), and we highlight the low representation of older women. We discuss the interconnectedness of these hallmarks mirrored in the complexity of skeletal muscle ageing and pathophysiology of sarcopenia. This intricate linkage provides the opportunity to identify their translational potential by targeting several hallmarks simultaneously with anti-ageing interventions, with exercise as an exemplar.
Acknowledgements
AG, KS, and AAS would like to acknowledge the support from the National Institute for Health and Care Research (NIHR) Newcastle Biomedical Research Centre (BRC). The views expressed are those of the authors and not necessarily those of the National Institute for Health and Care Research, United Kingdom. We would like to thank Ryan White (Regeneron Pharmaceutical, USA) and Sulev Kõks (Perron Institute, Western Australia) for their advice on the Genomic instability and Epigenetic changes hallmarks, respectively.
Abbreviations
- Ach
acetylcholine
- AKT
AKT-protein kinase B
- AMPK
AMP-activated protein kinase
- ATP
adenosine triphosphate
- BMI
body mass index
- Ca2+
calcium ion
- COX
cytochrome c oxidase-negative
- CpG
5′-C[cytosine]-phosphate-G[quinine]-3′
- dmCpG
differentially methylated CpG
- DMR
differentially methylated regions
- ECM
extracellular matrix
- ETS
electron transport system
- EWAS
epigenome-wide association study
- EWGSOP
The European Working Group on Sarcopenia in Older People
- GLIS
The Global Leadership Initiative in Sarcopenia
- GLUT1
Glucose transporter 1
- GLUT4
Glucose transporter 4
- GTEx
The Genotype-Tissue Expression project
- H+
hydrogen ion
- HDMC
muscle-derived human primary cell
- HOX
homeotic genes
- HSS
The Hertfordshire Sarcopenia Study
- ICE
inducible changes to the epigenome
- IFN-1
type-1 interferon
- IGF-1
insulin-like growth factor 1
- IL15
interleukin 15
- IL6
interleukin 6
- IL8
interleukin 8
- IMCL
intramyocellular lipids
- K+
potassium ion
- LINE-1
long-interspersed element 1
- MAPK
mitogen-activated protein kinase
- MMP7
matrix metalloproteinase-7
- MMP
matrix metalloproteinase
- MRI
magnetic resonance imaging
- mtDNA
mitochondrial DNA
- mTOR
mammalian target of rapamycin
- mTORC1
mammalian target of rapamycin complex 1
- MYH1
myosin heavy chain isoform 1
- MYH2
myosin heavy chain isoform 2
- MYH7
myosin heavy chain isoform 7
- Na+
sodium ion
- NF-κB
nuclear factor kappa-light-chain-enhancer of activated B cells
- NMJ
neuromuscular junction
- OXPHOS
oxidative phosphorylation
- PCR
polymerase chain reaction
- PI3K
phosphatidylinositol 3 kinase
- qPCR
quantitative polymerase chain reaction
- ROS
reactive oxygen species
- RTE
retrotransposable element
- RyR1
ryanodine receptor 1
- S6K1
ribosomal protein S6 kinase β-1
- SA-β-Gal
senescence-associated β-galactosidase
- SASP
senescence-associated secretory phenotype
- SPPB
short physical performance battery
- SR
sarcoplasmic reticulum
- sTNFr1
soluble tumor necrosis factor receptor-1
- sTNFr2
soluble tumor necrosis factor receptor-2
- T-tubules
transverse tubules
- TAF
telomere-associated DNA damage foci
- TCA
tricarboxylic acid
- TLs
telomere lengths
- VEGFA
vascular endothelial growth factor A
Data Availability
This is a narrative review and not an original research paper.
Competing Interests
A.G., K.S., M.G., and A.A.S. declare no competing interests associated with the manuscript. T.S. is an employee of Regeneron and holds stock in Regeneron.
Funding
The authors declare that there are no sources of funding to be acknowledged.
Open Access
Open access for this article was enabled by the participation of Newcastle University in an all-inclusive Read & Publish agreement with Portland Press and the Biochemical Society under a transformative agreement with JISC.
CRediT Author Contribution
Antoneta Granic: Conceptualization, Investigation, Visualization, Writing—original draft, Writing—review & editing. Karen Suetterlin: Investigation, Writing—original draft, Writing—review & editing. Tea Shavlakadze: Investigation, Writing—original draft, Writing—review & editing. Miranda D. Grounds: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. Avan A. Sayer: Conceptualization, Investigation, Writing—original draft, Writing—review & editing.
References
- 1.López-Otín C., Blasco M.A., Partridge L., Serrano M. and Kroemer G. (2013) The hallmarks of aging. Cell 153, 1194–1217 10.1016/j.cell.2013.05.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.López-Otín C., Blasco M.A., Partridge L., Serrano M. and Kroemer G. (2023) Hallmarks of aging: An expanding universe. Cell 186, 243–278 10.1016/j.cell.2022.11.001 [DOI] [PubMed] [Google Scholar]
- 3.Schmauck-Medina T., Molière A., Lautrup S., Zhang J., Chlopicki S., Madsen H.B.et al. (2022) New hallmarks of ageing: a 2022 Copenhagen ageing meeting summary. Aging 14, 6829–6839 10.18632/aging.204248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fraser H.C., Kuan V., Johnen R., Zwierzyna M., Hingorani A.D., Beyer A.et al. (2022) Biological mechanisms of aging predict age-related disease co-occurrence in patients. Aging Cell 21, e13524 10.1111/acel.13524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanahan D. and Weinberg R.A. (2011) Hallmarks of cancer: the next generation. Cell 144, 646–674 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 6.Ubaida-Mohien C., Lyashkov A., Gonzalez-Freire M., Tharakan R., Shardell M., Moaddel R.et al. (2019) Discovery proteomics in aging human skeletal muscle finds change in spliceosome, immunity, proteostasis and mitochondria. eLife 8, e49874 10.7554/eLife.49874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mattson M.P. and Arumugam T.V. (2018) Hallmarks of brain aging: adaptive and pathological modification by metabolic states. Cell Metab. 27, 1176–1199 10.1016/j.cmet.2018.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meiners S., Eickelberg O. and Königshoff M. (2015) Hallmarks of the ageing lung. Eur. Respir. J. 45, 807–827 10.1183/09031936.00186914 [DOI] [PubMed] [Google Scholar]
- 9.Wilson D.M. 3rd, Cookson M.R., Van Den Bosch L., Zetterberg H., Holtzman D.M. and Dewachter I. (2023) Hallmarks of neurodegenerative diseases. Cell 186, 693–714 10.1016/j.cell.2022.12.032 [DOI] [PubMed] [Google Scholar]
- 10.Cruz-Jentoft A.J., Bahat G., Bauer J., Boirie Y., Bruyère O., Cederholm T.et al. (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48, 16–31 10.1093/ageing/afy169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cruz-Jentoft A.J. and Sayer A.A. (2019) Sarcopenia. Lancet 393, 2636–2646 10.1016/S0140-6736(19)31138-9 [DOI] [PubMed] [Google Scholar]
- 12.Cawthon P.M., Visser M., Arai H., Ávila-Funes J.A., Barazzoni R., Bhasin S.et al. (2022) Defining terms commonly used in sarcopenia research: a glossary proposed by the Global Leadership in Sarcopenia (GLIS) Steering Committee. Eur. Geriatr. Med. 13, 1239–1244 10.1007/s41999-022-00706-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McLeod M., Breen L., Hamilton D.L. and Philp A. (2016) Live strong and prosper: the importance of skeletal muscle strength for healthy ageing. Biogerontology 17, 497–510 10.1007/s10522-015-9631-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tieland M., Trouwborst I. and Clark B.C. (2018) Skeletal muscle performance and ageing. J. Cachexia Sarcopenia Muscle. 9, 3–19 10.1002/jcsm.12238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mukund K. and Subramaniam S. (2020) Skeletal muscle: A review of molecular structure and function, in health and disease. Wiley Interdiscip. Rev. Syst. Biol. Med. 12, e1462 10.1002/wsbm.1462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frontera W.R. and Ochala J. (2015) Skeletal muscle: a brief review of structure and function. Calcif. Tissue Int. 96, 183–195 10.1007/s00223-014-9915-y [DOI] [PubMed] [Google Scholar]
- 17.Giordani L., He G.J., Negroni E., Sakai H., Law J.Y.C., Siu M.M.et al. (2019) High-dimensional single-cell cartography reveals novel skeletal muscle-resident cell populations. Mol. Cell 74, 609.e6–621.e6 10.1016/j.molcel.2019.02.026 [DOI] [PubMed] [Google Scholar]
- 18.Murgia M., Nogara L., Baraldo M., Reggiani C., Mann M. and Schiaffino S. (2021) Protein profile of fiber types in human skeletal muscle: a single-fiber proteomics study. Skelet. Muscle. 11, 24 10.1186/s13395-021-00279-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schiaffino S. and Reggiani C. (2011) Fiber types in mammalian skeletal muscles. Physiol. Rev. 91, 1447–1531 10.1152/physrev.00031.2010 [DOI] [PubMed] [Google Scholar]
- 20.Talbot J. and Maves L. (2016) Skeletal muscle fiber type: using insights from muscle developmental biology to dissect targets for susceptibility and resistance to muscle disease. Wiley Interdiscip. Rev. Dev. Biol. 5, 518–534 10.1002/wdev.230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schiaffino S. (2010) Fibre types in skeletal muscle: a personal account. Acta Physiol. 199, 451–463 10.1111/j.1748-1716.2010.02130.x [DOI] [PubMed] [Google Scholar]
- 22.Lloyd E.M., Pinniger G.J., Murphy R.M. and Grounds M.D. (2023) Slow or fast: Implications of myofibre type and associated differences for manifestation of neuromuscular disorders. Acta Physiol. (Oxf.) e14012 10.1111/apha.14012 [DOI] [PubMed] [Google Scholar]
- 23.Andersen J.L. (2003) Muscle fibre type adaptation in the elderly human muscle. Scand. J. Med. Sci. Sports 13, 40–47 10.1034/j.1600-0838.2003.00299.x [DOI] [PubMed] [Google Scholar]
- 24.Nygaard E. and Sanchez J. (1982) Intramuscular variation of fiber types in the brachial biceps and the lateral vastus muscles of elderly men: how representative is a small biopsy sample? Anat. Rec. 203, 451–459 10.1002/ar.1092030404 [DOI] [PubMed] [Google Scholar]
- 25.Kirkeby S. and Garbarsch C. (2000) Aging affects different human muscles in various ways. An image analysis of the histomorphometric characteristics of fiber types in human masseter and vastus lateralis muscles from young adults and the very old. Histol. Histopathol. 15, 61–71 [DOI] [PubMed] [Google Scholar]
- 26.Dodds R.M., Syddall H.E., Cooper R., Kuh D., Cooper C. and Sayer A.A. (2016) Global variation in grip strength: a systematic review and meta-analysis of normative data. Age Ageing 45, 209–216 10.1093/ageing/afv192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nair K.S. (2005) Aging muscle. Am. J. Clin. Nutr. 81, 953–963 10.1093/ajcn/81.5.953 [DOI] [PubMed] [Google Scholar]
- 28.Sayer A.A., Robinson S.M., Patel H.P., Shavlakadze T., Cooper C. and Grounds M.D. (2013) New horizons in the pathogenesis, diagnosis and management of sarcopenia. Age Ageing 42, 145–150 10.1093/ageing/afs191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mitchell W.K., Williams J., Atherton P., Larvin M., Lund J. and Narici M. (2012) Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front. Physiol. 3, 260 10.3389/fphys.2012.00260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coggan A.R., Spina R.J., King D.S., Rogers M.A., Brown M., Nemeth P.M.et al. (1992) Histochemical and enzymatic comparison of the gastrocnemius muscle of young and elderly men and women. J. Gerontol. 47, B71–B76 10.1093/geronj/47.3.B71 [DOI] [PubMed] [Google Scholar]
- 31.Nilwik R., Snijders T., Leenders M., Groen B.B., van Kranenburg J., Verdijk L.B.et al. (2013) The decline in skeletal muscle mass with aging is mainly attributed to a reduction in type II muscle fiber size. Exp. Gerontol. 48, 492–498 10.1016/j.exger.2013.02.012 [DOI] [PubMed] [Google Scholar]
- 32.Brunner F., Schmid A., Sheikhzadeh A., Nordin M., Yoon J. and Frankel V. (2007) Effects of aging on Type II muscle fibers: a systematic review of the literature. J. Aging Phys. Act 15, 336–348 10.1123/japa.15.3.336 [DOI] [PubMed] [Google Scholar]
- 33.Deschenes M.R. (2004) Effects of aging on muscle fibre type and size. Sports Med. (Auckland, N.Z.) 34, 809–824 10.2165/00007256-200434120-00002 [DOI] [PubMed] [Google Scholar]
- 34.Wilkinson D.J., Piasecki M. and Atherton P.J. (2018) The age-related loss of skeletal muscle mass and function: Measurement and physiology of muscle fibre atrophy and muscle fibre loss in humans. Ageing Res. Rev. 47, 123–132 10.1016/j.arr.2018.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lexell J. and Downham D. (1992) What is the effect of ageing on type 2 muscle fibres? J. Neurol. Sci. 107, 250–251 10.1016/0022-510X(92)90297-X [DOI] [PubMed] [Google Scholar]
- 36.Jolesz F. and Sreter F.A. (1981) Development, innervation, and activity-pattern induced changes in skeletal muscle. Annu. Rev. Physiol. 43, 531–552 10.1146/annurev.ph.43.030181.002531 [DOI] [PubMed] [Google Scholar]
- 37.Deschenes M.R. (2011) Motor unit and neuromuscular junction remodeling with aging. Curr. Aging Sci. 4, 209–220 10.2174/1874609811104030209 [DOI] [PubMed] [Google Scholar]
- 38.Murgia M., Toniolo L., Nagaraj N., Ciciliot S., Vindigni V., Schiaffino S.et al. (2017) Single muscle fiber proteomics reveals fiber-type-specific features of human muscle aging. Cell Rep. 19, 2396–2409 10.1016/j.celrep.2017.05.054 [DOI] [PubMed] [Google Scholar]
- 39.Dao T., Green A.E., Kim Y.A., Bae S.J., Ha K.T., Gariani K.et al. (2020) Sarcopenia and muscle aging: a brief overview. Endocrinol. Metab. (Seoul) 35, 716–732 10.3803/EnM.2020.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aversa Z., Zhang X., Fielding R.A., Lanza I. and LeBrasseur N.K. (2019) The clinical impact and biological mechanisms of skeletal muscle aging. Bone 127, 26–36 10.1016/j.bone.2019.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wiedmer P., Jung T., Castro J.P., Pomatto L.C.D., Sun P.Y., Davies K.J.A.et al. (2021) Sarcopenia - Molecular mechanisms and open questions. Ageing Res. Rev. 65, 101200 10.1016/j.arr.2020.101200 [DOI] [PubMed] [Google Scholar]
- 42.Dodds R.M., Hurst C., Hillman S.J., Davies K., Roberts L., Aspray T.J.et al. (2022) Advancing our understanding of skeletal muscle across the lifecourse: Protocol for the MASS_Lifecourse study and characteristics of the first 80 participants. Exp. Gerontol. 166, 111884 10.1016/j.exger.2022.111884 [DOI] [PubMed] [Google Scholar]
- 43.Xie W.Q., He M., Yu D.J., Wu Y.X., Wang X.H., Lv S.et al. (2021) Mouse models of sarcopenia: classification and evaluation. J. Cachexia Sarcopenia Muscle. 12, 538–554 10.1002/jcsm.12709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schumacher B., Pothof J., Vijg J. and Hoeijmakers J.H.J. (2021) The central role of DNA damage in the ageing process. Nature 592, 695–703 10.1038/s41586-021-03307-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yousefzadeh M., Henpita C., Vyas R., Soto-Palma C., Robbins P. and Niedernhofer L. (2021) DNA damage-how and why we age? eLife 10, e62852 10.7554/eLife.62852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cagan A., Baez-Ortega A., Brzozowska N., Abascal F., Coorens T.H.H.et al. (2022) Somatic mutation rates scale with lifespan across mammals. Nature 604, 517–524 10.1038/s41586-022-04618-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.De Cecco M., Criscione S.W., Peterson A.L., Neretti N., Sedivy J.M. and Kreiling J.A. (2013) Transposable elements become active and mobile in the genomes of aging mammalian somatic tissues. Aging 5, 867–883 10.18632/aging.100621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.De Cecco M., Ito T., Petrashen A.P., Elias A.E., Skvir N.J., Criscione S.W.et al. (2019) L1 drives IFN in senescent cells and promotes age-associated inflammation. Nature 566, 73–78 10.1038/s41586-018-0784-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bétermier M., Bertrand P. and Lopez B.S. (2014) Is non-homologous end-joining really an inherently error-prone process? PLos Genet. 10, e1004086 10.1371/journal.pgen.1004086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bou Saada Y., Zakharova V., Chernyak B., Dib C., Carnac G., Dokudovskaya S.et al. (2017) Control of DNA integrity in skeletal muscle under physiological and pathological conditions. Cell. Mol. Life Sci. 74, 3439–3449 10.1007/s00018-017-2530-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maldonado E., Morales-Pison S., Urbina F. and Solari A. (2023) Aging hallmarks and the role of oxidative stress. Antioxidants (Basel) 12, 651 10.3390/antiox12030651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jackson M.J., Pollock N., Staunton C., Jones S. and McArdle A. (2022) Redox control of signalling responses to contractile activity and ageing in skeletal muscle. Cells 11, 1698 10.3390/cells11101698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mecocci P., Fanó G., Fulle S., MacGarvey U., Shinobu L., Polidori M.C.et al. (1999) Age-dependent increases in oxidative damage to DNA, lipids, and proteins in human skeletal muscle. Free Radic. Biol. Med. 26, 303–308 10.1016/S0891-5849(98)00208-1 [DOI] [PubMed] [Google Scholar]
- 54.Vermeij W.P., Hoeijmakers J.H. and Pothof J. (2016) Genome integrity in aging: human syndromes, mouse models, and therapeutic options. Annu. Rev. Pharmacol. Toxicol. 56, 427–445 10.1146/annurev-pharmtox-010814-124316 [DOI] [PubMed] [Google Scholar]
- 55.Niedernhofer L.J., Gurkar A.U., Wang Y., Vijg J., Hoeijmakers J.H.J. and Robbins P.D. (2018) Nuclear genomic instability and aging. Annu. Rev. Biochem. 87, 295–322 10.1146/annurev-biochem-062917-012239 [DOI] [PubMed] [Google Scholar]
- 56.Bozzetti F. (2020) Chemotherapy-induced sarcopenia. Curr. Treat. Options Oncol. 21, 7 10.1007/s11864-019-0691-9 [DOI] [PubMed] [Google Scholar]
- 57.Pedrosa M.B., Barbosa S., Vitorino R., Ferreira R., Moreira-Gonçalves D. and Santos L.L. (2023) Chemotherapy-induced molecular changes in skeletal muscle. Biomedicines 11, 905 10.3390/biomedicines11030905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Prado C.M., Sawyer M.B., Ghosh S., Lieffers J.R., Esfandiari N., Antoun S.et al. (2013) Central tenet of cancer cachexia therapy: do patients with advanced cancer have exploitable anabolic potential? Am. J. Clin. Nutr. 98, 1012–1019 10.3945/ajcn.113.060228 [DOI] [PubMed] [Google Scholar]
- 59.Lujan S.A., Longley M.J., Humble M.H., Lavender C.A., Burkholder A., Blakely E.L.et al. (2020) Ultrasensitive deletion detection links mitochondrial DNA replication, disease, and aging. Genome Biol. 21, 248 10.1186/s13059-020-02138-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kadenbach B., Münscher C., Frank V., Müller-Höcker J. and Napiwotzki J. (1995) Human aging is associated with stochastic somatic mutations of mitochondrial DNA. Mutat. Res. 338, 161–172 10.1016/0921-8734(95)00021-W [DOI] [PubMed] [Google Scholar]
- 61.Herbst A., Lee C.C., Vandiver A.R., Aiken J.M., McKenzie D., Hoang A.et al. (2021) Mitochondrial DNA deletion mutations increase exponentially with age in human skeletal muscle. Aging Clin. Exp. Res. 33, 1811–1820 10.1007/s40520-020-01698-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Herbst A., Prior S.J., Lee C.C., Aiken J.M., McKenzie D., Hoang A.et al. (2021) Skeletal muscle mitochondrial DNA copy number and mitochondrial DNA deletion mutation frequency as predictors of physical performance in older men and women. Geroscience 43, 1253–1264 10.1007/s11357-021-00351-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bua E., Johnson J., Herbst A., Delong B., McKenzie D., Salamat S.et al. (2006) Mitochondrial DNA-deletion mutations accumulate intracellularly to detrimental levels in aged human skeletal muscle fibers. Am. J. Hum. Genet. 79, 469–480 10.1086/507132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McKenzie D., Bua E., McKiernan S., Cao Z., Aiken J.M. and Wanagat J. (2002) Mitochondrial DNA deletion mutations: a causal role in sarcopenia. Eur. J. Biochem. 269, 2010–2015 10.1046/j.1432-1033.2002.02867.x [DOI] [PubMed] [Google Scholar]
- 65.Gorbunova V., Seluanov A., Mita P., McKerrow W., Fenyö D., Boeke J.D.et al. (2021) The role of retrotransposable elements in ageing and age-associated diseases. Nature 596, 43–53 10.1038/s41586-021-03542-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Burns K.H. (2020) Our conflict with transposable elements and its implications for human disease. Annu. Rev. Pathol. 15, 51–70 10.1146/annurev-pathmechdis-012419-032633 [DOI] [PubMed] [Google Scholar]
- 67.Fröhlich A., Pfaff A.L., Bubb V.J., Kõks S. and Quinn J.P. (2022) Characterisation of the function of a SINE-VNTR-Alu Retrotransposon to modulate isoform expression at the MAPT locus. Front. Mol. Neurosci. 15, 815695 10.3389/fnmol.2022.815695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kõks S., Pfaff A.L., Singleton L.M., Bubb V.J. and Quinn J.P. (2022) Non-reference genome transposable elements (TEs) have a significant impact on the progression of the Parkinson's disease. Exp. Biol. Med. (Maywood) 247, 1680–1690 10.1177/15353702221117147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hsu P.S., Yu S.H., Tsai Y.T., Chang J.Y., Tsai L.K., Ye C.H.et al. (2021) More than causing (epi)genomic instability: emerging physiological implications of transposable element modulation. J. Biomed. Sci. 28, 58 10.1186/s12929-021-00754-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Goodier J.L. (2016) Restricting retrotransposons: a review. Mob. DNA 7, 16 10.1186/s13100-016-0070-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Warkocki Z. (2023) An update on post-transcriptional regulation of retrotransposons. FEBS Lett. 597, 380–406 10.1002/1873-3468.14551 [DOI] [PubMed] [Google Scholar]
- 72.Osipovich A.B., Dudek K.D., Trinh L.T., Kim L.H., Shrestha S., Cartailler J.P.et al. (2023) ZFP92, a KRAB domain zinc finger protein enriched in pancreatic islets, binds to B1/Alu SINE transposable elements and regulates retroelements and genes. PLos Genet. 19, e1010729 10.1371/journal.pgen.1010729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Simon M., Van Meter M., Ablaeva J., Ke Z., Gonzalez R.S., Taguchi T.et al. (2019) LINE1 derepression in aged wild-type and SIRT6-deficient mice drives inflammation. Cell Metab. 29, 871.e5–885.e5 10.1016/j.cmet.2019.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mumford P.W., Romero M.A., Osburn S.C., Roberson P.A., Vann C.G., Mobley C.B.et al. (2019) Skeletal muscle LINE-1 retrotransposon activity is upregulated in older versus younger rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 317, R397–R406 10.1152/ajpregu.00110.2019 [DOI] [PubMed] [Google Scholar]
- 75.Romero M.A., Mumford P.W., Roberson P.A., Osburn S.C., Young K.C., Sedivy J.M.et al. (2022) Translational Significance of the LINE-1 Jumping Gene in Skeletal Muscle. Exerc. Sport Sci. Rev. 50, 185–193 10.1249/JES.0000000000000301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Roberson P.A., Romero M.A., Osburn S.C., Mumford P.W., Vann C.G., Fox C.D.et al. (2019) Skeletal muscle LINE-1 ORF1 mRNA is higher in older humans but decreases with endurance exercise and is negatively associated with higher physical activity. J. Appl. Physiol. (1985) 127, 895–904 10.1152/japplphysiol.00352.2019 [DOI] [PubMed] [Google Scholar]
- 77.Shavlakadze T., Morris M., Fang J., Wang S.X., Zhu J., Zhou W.et al. (2019) Age-related gene expression signature in rats demonstrate early, late, and linear transcriptional changes from multiple tissues. Cell Rep. 28, 3263.e3–3273.e3 10.1016/j.celrep.2019.08.043 [DOI] [PubMed] [Google Scholar]
- 78.Shavlakadze T., Xiong K., Mishra S., McEwen C., Gadi A., Wakai M.et al. (2023) Age-related gene expression signatures from limb skeletal muscles and the diaphragm in mice and rats reveal common and species-specific changes. Skelet. Muscle 13, 11 10.1186/s13395-023-00321-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shay J.W. and Wright W.E. (2005) Senescence and immortalization: role of telomeres and telomerase. Carcinogenesis 26, 867–874 10.1093/carcin/bgh296 [DOI] [PubMed] [Google Scholar]
- 80.Shay J.W. and Wright W.E. (2019) Telomeres and telomerase: three decades of progress. Nat. Rev. Genet. 20, 299–309 10.1038/s41576-019-0099-1 [DOI] [PubMed] [Google Scholar]
- 81.Demanelis K., Jasmine F., Chen L.S., Chernoff M., Tong L., Delgado D.et al. (2020) Determinants of telomere length across human tissues. Science 369, eaaz6876 10.1126/science.aaz6876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dlouha D., Maluskova J., Kralova Lesna I., Lanska V. and Hubacek J.A. (2014) Comparison of the relative telomere length measured in leukocytes and eleven different human tissues. Physiol. Res. 63, S343–S350 10.33549/physiolres.932856 [DOI] [PubMed] [Google Scholar]
- 83.Semeraro M.D., Almer G., Renner W., Gruber H.J. and Herrmann M. (2022) Telomere length in leucocytes and solid tissues of young and aged rats. Aging 14, 1713–1728 10.18632/aging.203922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kirk B., Kuo C.L., Xiang M. and Duque G. (2022) Associations between leukocyte telomere length and osteosarcopenia in 20,400 adults aged 60 years and over: Data from the UK Biobank. Bone 161, 116425 10.1016/j.bone.2022.116425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lorenzi M., Bonassi S., Lorenzi T., Giovannini S., Bernabei R. and Onder G. (2018) A review of telomere length in sarcopenia and frailty. Biogerontology 19, 209–221 10.1007/s10522-018-9749-5 [DOI] [PubMed] [Google Scholar]
- 86.Ishikawa N., Nakamura K., Izumiyama-Shimomura N., Aida J., Matsuda Y., Arai T.et al. (2016) Changes of telomere status with aging: An update. Geriatr. Gerontol. Int. 16, 30–42 10.1111/ggi.12772 [DOI] [PubMed] [Google Scholar]
- 87.Martin-Ruiz C.M., Baird D., Roger L., Boukamp P., Krunic D., Cawthon R.et al. (2015) Reproducibility of telomere length assessment: an international collaborative study. Int. J. Epidemiol. 44, 1673–1683 10.1093/ije/dyu191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Decary S., Mouly V., Hamida C.B., Sautet A., Barbet J.P. and Butler-Browne G.S. (1997) Replicative potential and telomere length in human skeletal muscle: implications for satellite cell-mediated gene therapy. Hum. Gene Ther. 8, 1429–1438 10.1089/hum.1997.8.12-1429 [DOI] [PubMed] [Google Scholar]
- 89.Ponsot E., Lexell J. and Kadi F. (2008) Skeletal muscle telomere length is not impaired in healthy physically active old women and men. Muscle Nerve 37, 467–472 10.1002/mus.20964 [DOI] [PubMed] [Google Scholar]
- 90.Arsenis N.C., You T., Ogawa E.F., Tinsley G.M. and Zuo L. (2017) Physical activity and telomere length: Impact of aging and potential mechanisms of action. Oncotarget 8, 45008–45019 10.18632/oncotarget.16726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sellami M., Bragazzi N., Prince M.S., Denham J. and Elrayess M. (2021) Regular, intense exercise training as a healthy aging lifestyle strategy: preventing DNA damage, telomere shortening and adverse DNA methylation changes over a lifetime. Front Genet. 12, 652497 10.3389/fgene.2021.652497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Daniali L., Benetos A., Susser E., Kark J.D., Labat C., Kimura M.et al. (2013) Telomeres shorten at equivalent rates in somatic tissues of adults. Nat. Commun. 4, 1597 10.1038/ncomms2602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sabharwal S., Verhulst S., Guirguis G., Kark J.D., Labat C., Roche N.E.et al. (2018) Telomere length dynamics in early life: the blood-and-muscle model. FASEB J. 32, 529–534 10.1096/fj.201700630r [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hiam D., Smith C., Voisin S., Denham J., Yan X., Landen S.et al. (2020) Aerobic capacity and telomere length in human skeletal muscle and leukocytes across the lifespan. Aging 12, 359–369 10.18632/aging.102627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Meyer A., Salewsky B., Spira D., Steinhagen-Thiessen E., Norman K. and Demuth I. (2016) Leukocyte telomere length is related to appendicular lean mass: cross-sectional data from the Berlin Aging Study II (BASE-II). Am. J. Clin. Nutr. 103, 178–183 10.3945/ajcn.115.116806 [DOI] [PubMed] [Google Scholar]
- 96.Zykovich A., Hubbard A., Flynn J.M., Tarnopolsky M., Fraga M.F., Kerksick C.et al. (2014) Genome-wide DNA methylation changes with age in disease-free human skeletal muscle. Aging Cell 13, 360–366 10.1111/acel.12180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Voisin S., Harvey N.R., Haupt L.M., Griffiths L.R., Ashton K.J., Coffey V.G.et al. (2020) An epigenetic clock for human skeletal muscle. J. Cachexia Sarcopenia Muscle. 11, 887–898 10.1002/jcsm.12556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Voisin S., Jacques M., Landen S., Harvey N.R., Haupt L.M., Griffiths L.R.et al. (2021) Meta-analysis of genome-wide DNA methylation and integrative omics of age in human skeletal muscle. J. Cachexia Sarcopenia Muscle. 12, 1064–1078 10.1002/jcsm.12741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Turner D.C., Gorski P.P., Maasar M.F., Seaborne R.A., Baumert P., Brown A.D.et al. (2020) DNA methylation across the genome in aged human skeletal muscle tissue and muscle-derived cells: the role of HOX genes and physical activity. Sci. Rep. 10, 15360 10.1038/s41598-020-72730-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Watt K.I., Goodman C.A., Hornberger T.A. and Gregorevic P. (2018) The Hippo Signaling Pathway in the Regulation of Skeletal Muscle Mass and Function. Exerc. Sport Sci. Rev. 46, 92–96 10.1249/JES.0000000000000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Noordermeer D., Leleu M., Splinter E., Rougemont J., De Laat W. and Duboule D. (2011) The dynamic architecture of Hox gene clusters. Science 334, 222–225 10.1126/science.1207194 [DOI] [PubMed] [Google Scholar]
- 102.Antoun E., Garratt E.S., Taddei A., Burton M.A., Barton S.J., Titcombe P.et al. (2022) Epigenome-wide association study of sarcopenia: findings from the Hertfordshire Sarcopenia Study (HSS). J. Cachexia Sarcopenia Muscle. 13, 240–253 10.1002/jcsm.12876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.He L., Khanal P., Morse C.I., Williams A. and Thomis M. (2019) Differentially methylated gene patterns between age-matched sarcopenic and non-sarcopenic women. J. Cachexia Sarcopenia Muscle. 10, 1295–1306 10.1002/jcsm.12478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.He L., Khanal P., Morse C.I., Williams A. and Thomis M. (2020) Associations of combined genetic and epigenetic scores with muscle size and muscle strength: a pilot study in older women. J. Cachexia Sarcopenia Muscle. 11, 1548–1561 10.1002/jcsm.12585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Trapp A., Kerepesi C. and Gladyshev V.N. (2021) Profiling epigenetic age in single cells. Nat. Aging 1, 1189–1201 10.1038/s43587-021-00134-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kaushik S. and Cuervo A.M. (2015) Proteostasis and aging. Nat. Med. 21, 1406–1415 10.1038/nm.4001 [DOI] [PubMed] [Google Scholar]
- 107.Ross C.A. and Poirier M.A. (2004) Protein aggregation and neurodegenerative disease. Nat. Med. 10, S10–S17 10.1038/nm1066 [DOI] [PubMed] [Google Scholar]
- 108.Soto C. and Pritzkow S. (2018) Protein misfolding, aggregation, and conformational strains in neurodegenerative diseases. Nat. Neurosci. 21, 1332–1340 10.1038/s41593-018-0235-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ayyadevara S., Balasubramaniam M., Suri P., Mackintosh S.G., Tackett A.J., Sullivan D.H.et al. (2016) Proteins that accumulate with age in human skeletal-muscle aggregates contribute to declines in muscle mass and function in Caenorhabditis elegans. Aging 8, 3486–3497 10.18632/aging.101141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Fernando R., Drescher C., Nowotny K., Grune T. and Castro J.P. (2019) Impaired proteostasis during skeletal muscle aging. Free Radic. Biol. Med. 132, 58–66 10.1016/j.freeradbiomed.2018.08.037 [DOI] [PubMed] [Google Scholar]
- 111.Paez H.G., Pitzer C.R. and Alway S.E. (2023) Age-related dysfunction in proteostasis and cellular quality control in the development of sarcopenia. Cells 12, 249 10.3390/cells12020249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Condon K.J. and Sabatini D.M. (2019) Nutrient regulation of mTORC1 at a glance. J. Cell Sci. 132, jcs222570 10.1242/jcs.222570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ibebunjo C., Chick J.M., Kendall T., Eash J.K., Li C., Zhang Y.et al. (2013) Genomic and proteomic profiling reveals reduced mitochondrial function and disruption of the neuromuscular junction driving rat sarcopenia. Mol. Cell. Biol. 33, 194–212 10.1128/MCB.01036-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.White Z., White R.B., McMahon C., Grounds M.D. and Shavlakadze T. (2016) High mTORC1 signaling is maintained, while protein degradation pathways are perturbed in old murine skeletal muscles in the fasted state. Int. J. Biochem. Cell 78, 10–21 10.1016/j.biocel.2016.06.012 [DOI] [PubMed] [Google Scholar]
- 115.Joseph G.A., Wang S.X., Jacobs C.E., Zhou W., Kimble G.C., Tse H.W.et al. (2019) Partial inhibition of mTORC1 in aged rats counteracts the decline in muscle mass and reverses molecular signaling associated with sarcopenia. Mol. Cell. Biol. 39, e00141–e00219 10.1128/MCB.00141-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ham D.J., Börsch A., Chojnowska K., Lin S., Leuchtmann A.B., Ham A.S.et al. (2022) Distinct and additive effects of calorie restriction and rapamycin in aging skeletal muscle. Nat. Commun. 13, 2025 10.1038/s41467-022-29714-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Léger B., Derave W., De Bock K., Hespel P. and Russell A.P. (2008) Human sarcopenia reveals an increase in SOCS-3 and myostatin and a reduced efficiency of Akt phosphorylation. Rejuvenation Res. 11, 163B–175B 10.1089/rej.2007.0588 [DOI] [PubMed] [Google Scholar]
- 118.Markofski M.M., Dickinson J.M., Drummond M.J., Fry C.S., Fujita S., Gundermann D.M.et al. (2015) Effect of age on basal muscle protein synthesis and mTORC1 signaling in a large cohort of young and older men and women. Exp. Gerontol. 65, 1–7 10.1016/j.exger.2015.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bauer M.E. and de la Fuente M. (2016) The role of oxidative and inflammatory stress and persistent viral infections in immunosenescence. Mech. Ageing Dev. 158, 27–37 10.1016/j.mad.2016.01.001 [DOI] [PubMed] [Google Scholar]
- 120.Ferrucci L. and Fabbri E. (2018) Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat. Rev. Cardiol. 15, 505–522 10.1038/s41569-018-0064-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhang X., Li H., He M., Wang J., Wu Y. and Li Y. (2022) Immune system and sarcopenia: Presented relationship and future perspective. Exp. Gerontol. 164, 111823 10.1016/j.exger.2022.111823 [DOI] [PubMed] [Google Scholar]
- 122.Su J., Ekman C., Oskolkov N., Lahti L., Ström K., Brazma A.et al. (2015) A novel atlas of gene expression in human skeletal muscle reveals molecular changes associated with aging. Skelet. Muscle 5, 35 10.1186/s13395-015-0059-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Moiseeva V., Cisneros A., Sica V., Deryagin O., Lai Y., Jung S.et al. (2023) Senescence atlas reveals an aged-like inflamed niche that blunts muscle regeneration. Nature 613, 169–178 10.1038/s41586-022-05535-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Cai D., Frantz J.D., Tawa N.E. Jr, Melendez P.A., Oh B.C., Lidov H.G.et al. (2004) IKKbeta/NF-kappaB activation causes severe muscle wasting in mice. Cell 119, 285–298 10.1016/j.cell.2004.09.027 [DOI] [PubMed] [Google Scholar]
- 125.Egerman M.A. and Glass D.J. (2014) Signaling pathways controlling skeletal muscle mass. Crit. Rev. Biochem. Mol. Biol. 49, 59–68 10.3109/10409238.2013.857291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.da Costa Teixeira L.A., Avelar N.C.P., Peixoto M.F.D., Parentoni A.N., Santos J.M.D., Pereira F.S.M.et al. (2023) Inflammatory biomarkers at different stages of Sarcopenia in older women. Sci. Rep. 13, 10367 10.1038/s41598-023-37229-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Meng S.J. and Yu L.J. (2010) Oxidative stress, molecular inflammation and sarcopenia. Int. J. Mol. Sci. 11, 1509–1526 10.3390/ijms11041509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hütter E., Skovbro M., Lener B., Prats C., Rabøl R., Dela F.et al. (2007) Oxidative stress and mitochondrial impairment can be separated from lipofuscin accumulation in aged human skeletal muscle. Aging Cell 6, 245–256 10.1111/j.1474-9726.2007.00282.x [DOI] [PubMed] [Google Scholar]
- 129.Marzetti E., Calvani R., Cesari M., Buford T.W., Lorenzi M., Behnke B.J.et al. (2013) Mitochondrial dysfunction and sarcopenia of aging: from signaling pathways to clinical trials. Int. J. Biochem. Cell Biol. 45, 2288–2301 10.1016/j.biocel.2013.06.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Picca A., Lezza A.M.S., Leeuwenburgh C., Pesce V., Calvani R., Bossola M.et al. (2018) Circulating mitochondrial DNA at the crossroads of mitochondrial dysfunction and inflammation during aging and muscle wasting disorders. Rejuvenation Res. 21, 350–359 10.1089/rej.2017.1989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Cheema N., Herbst A., McKenzie D. and Aiken J.M. (2015) Apoptosis and necrosis mediate skeletal muscle fiber loss in age-induced mitochondrial enzymatic abnormalities. Aging Cell 14, 1085–1093 10.1111/acel.12399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Dowling P., Gargan S., Swandulla D. and Ohlendieck K. (2023) Fiber-type shifting in sarcopenia of old age: proteomic profiling of the contractile apparatus of skeletal muscles. Int. J. Mol. Sci. 24, 2415 10.3390/ijms24032415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Larsson L., Sjödin B. and Karlsson J. (1978) Histochemical and biochemical changes in human skeletal muscle with age in sedentary males, age 22–65 years. Acta Physiol. Scand. 103, 31–39 10.1111/j.1748-1716.1978.tb06187.x [DOI] [PubMed] [Google Scholar]
- 134.Sundberg C.W., Hunter S.K., Trappe S.W., Smith C.S. and Fitts R.H. (2018) Effects of elevated H+ and Pi on the contractile mechanics of skeletal muscle fibres from young and old men: implications for muscle fatigue in humans. J. Physiol. 596, 3993–4015 10.1113/JP276018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wang Y. and Pessin J.E. (2013) Mechanisms for fiber-type specificity of skeletal muscle atrophy. Curr. Opin. Clin. Nutr. Metab. Care 16, 243–250 10.1097/MCO.0b013e328360272d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Matsakas A. and Patel K. (2009) Skeletal muscle fibre plasticity in response to selected environmental and physiological stimuli. Histol. Histopathol. 24, 611–629 [DOI] [PubMed] [Google Scholar]
- 137.Srikanthan P. and Karlamangla A.S. (2011) Relative muscle mass is inversely associated with insulin resistance and prediabetes. Findings from the third National Health and Nutrition Examination Survey. J. Clin. Endocrinol. Metab. 96, 2898–2903 10.1210/jc.2011-0435 [DOI] [PubMed] [Google Scholar]
- 138.Merz K.E. and Thurmond D.C. (2020) Role of Skeletal muscle in insulin resistance and glucose uptake. Compr. Physiol. 10, 785–809 10.1002/cphy.c190029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.van Dam E.M., Govers R. and James D.E. (2005) Akt activation is required at a late stage of insulin-induced GLUT4 translocation to the plasma membrane. Mol. Endocrinol. 19, 1067–1077 10.1210/me.2004-0413 [DOI] [PubMed] [Google Scholar]
- 140.Chia C.W., Egan J.M. and Ferrucci L. (2018) Age-related changes in glucose metabolism, hyperglycemia, and cardiovascular risk. Circ. Res. 123, 886–904 10.1161/CIRCRESAHA.118.312806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Thiebaud D., Jacot E., DeFronzo R.A., Maeder E., Jequier E. and Felber J.P. (1982) The effect of graded doses of insulin on total glucose uptake, glucose oxidation, and glucose storage in man. Diabetes 31, 957–963 10.2337/diacare.31.11.957 [DOI] [PubMed] [Google Scholar]
- 142.DeFronzo R.A. and Tripathy D. (2009) Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care 32, S157–S163 10.2337/dc09-S302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Warram J.H., Martin B.C., Krolewski A.S., Soeldner J.S. and Kahn C.R. (1990) Slow glucose removal rate and hyperinsulinemia precede the development of type II diabetes in the offspring of diabetic parents. Ann. Intern. Med. 113, 909–915 10.7326/0003-4819-113-12-909 [DOI] [PubMed] [Google Scholar]
- 144.Mesinovic J., Zengin A., De Courten B., Ebeling P.R. and Scott D. (2019) Sarcopenia and type 2 diabetes mellitus: a bidirectional relationship. Diab. Metab. Syndr. Obes. 12, 1057–1072 10.2147/DMSO.S186600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Breen L., Stokes K.A., Churchward-Venne T.A., Moore D.R., Baker S.K., Smith K.et al. (2013) Two weeks of reduced activity decreases leg lean mass and induces “anabolic resistance” of myofibrillar protein synthesis in healthy elderly. J. Clin. Endocrinol. Metab. 98, 2604–2612 10.1210/jc.2013-1502 [DOI] [PubMed] [Google Scholar]
- 146.McGlory C., von Allmen M., Stokes T. and Phillips S. (2016) Only Two weeks of physical inactivity induces insulin resistance and impairs glycemic control in older adults. FASEB J. 30, 734.2–734.2 [Google Scholar]
- 147.St-Jean-Pelletier F., Pion C.H., Leduc-Gaudet J.P., Sgarioto N., Zovilé I., Barbat-Artigas S.et al. (2017) The impact of ageing, physical activity, and pre-frailty on skeletal muscle phenotype, mitochondrial content, and intramyocellular lipids in men. J. Cachexia Sarcopenia Muscle 8, 213–228 10.1002/jcsm.12139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Chee C., Shannon C.E., Burns A., Selby A.L., Wilkinson D., Smith K.et al. (2016) Relative contribution of intramyocellular lipid to whole-body fat oxidation is reduced with age but subsarcolemmal lipid accumulation and insulin resistance are only associated with overweight individuals. Diabetes 65, 840–850 10.2337/db15-1383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Crane J.D., Devries M.C., Safdar A., Hamadeh M.J. and Tarnopolsky M.A. (2010) The effect of aging on human skeletal muscle mitochondrial and intramyocellular lipid ultrastructure. J. Gerontol. A Biol. Sci. Med. Sci. 65, 119–128 10.1093/gerona/glp179 [DOI] [PubMed] [Google Scholar]
- 150.Yoshiko A., Maeda H., Takahashi H., Koike T., Tanaka N. and Akima H. (2022) Contribution of skeletal muscle and serum lipids to muscle contraction induced by neuromuscular electrical stimulation in older individuals. Physiol. Rep. 10, e15236 10.14814/phy2.15236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Bosaeus I. and Rothenberg E. (2016) Nutrition and physical activity for the prevention and treatment of age-related sarcopenia. Proc. Nutr. Soc. 75, 174–180 10.1017/S002966511500422X [DOI] [PubMed] [Google Scholar]
- 152.Kumar V., Selby A., Rankin D., Patel R., Atherton P., Hildebrandt W.et al. (2009) Age-related differences in the dose-response relationship of muscle protein synthesis to resistance exercise in young and old men. J. Physiol. 587, 211–217 10.1113/jphysiol.2008.164483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Moore D.R. (2014) Keeping older muscle “young” through dietary protein and physical activity. Adv. Nutr. 5, 599S–607S 10.3945/an.113.005405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Wall B.T., Gorissen S.H., Pennings B., Koopman R., Groen B.B., Verdijk L.B.et al. (2015) Aging is accompanied by a blunted muscle protein synthetic response to protein ingestion. PloS ONE 10, e0140903 10.1371/journal.pone.0140903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Dillon E.L., Casperson S.L., Durham W.J., Randolph K.M., Urban R.J., Volpi E.et al. (2011) Muscle protein metabolism responds similarly to exogenous amino acids in healthy younger and older adults during NO-induced hyperemia. Am. J. Physiol. Regul. Integr. Comp. Physiol. 301, R1408–R1417 10.1152/ajpregu.00211.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Timmerman K.L., Lee J.L., Fujita S., Dhanani S., Dreyer H.C., Fry C.S.et al. (2010) Pharmacological vasodilation improves insulin-stimulated muscle protein anabolism but not glucose utilization in older adults. Diabetes 59, 2764–2771 10.2337/db10-0415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Mortensen B., Poulsen P., Wegner L., Stender-Petersen K.L., Ribel-Madsen R., Friedrichsen M.et al. (2009) Genetic and metabolic effects on skeletal muscle AMPK in young and older twins. Am. J. Physiol. Endocrinol. Metab. 297, E956–E964 10.1152/ajpendo.00058.2009 [DOI] [PubMed] [Google Scholar]
- 158.Ljubicic V. and Hood D.A. (2009) Diminished contraction-induced intracellular signaling towards mitochondrial biogenesis in aged skeletal muscle. Aging Cell 8, 394–404 10.1111/j.1474-9726.2009.00483.x [DOI] [PubMed] [Google Scholar]
- 159.Meyer A., Laverny G., Bernardi L., Charles A.L., Alsaleh G., Pottecher J.et al. (2018) Mitochondria: an organelle of bacterial origin controlling inflammation. Front. Immunol. 9, 536 10.3389/fimmu.2018.00536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Zampino M., Brennan N.A., Kuo P.L., Spencer R.G., Fishbein K.W., Simonsick E.M.et al. (2020) Poor mitochondrial health and systemic inflammation? Test of a classic hypothesis in the baltimore longitudinal study of aging GeroScience 42, 1175–1182 10.1007/s11357-020-00208-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Picca A., Calvani R., Bossola M., Allocca E., Menghi A., Pesce V.et al. (2018) Update on mitochondria and muscle aging: all wrong roads lead to sarcopenia. Biol. Chem. 399, 421–436 10.1515/hsz-2017-0331 [DOI] [PubMed] [Google Scholar]
- 162.Joseph A.M., Adhihetty P.J. and Leeuwenburgh C. (2016) Beneficial effects of exercise on age-related mitochondrial dysfunction and oxidative stress in skeletal muscle. J. Physiol. 594, 5105–5123 10.1113/JP270659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Victorelli S., Salmonowicz H., Chapman J., Martini H., Vizioli M.G., Riley J.S.et al. (2023) Apoptotic stress causes mtDNA release during senescence and drives the SASP. Nature 622, 627–636 10.1038/s41586-023-06621-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Grevendonk L., Connell N.J., McCrum C., Fealy C.E., Bilet L., Bruls Y.M.H.et al. (2021) Impact of aging and exercise on skeletal muscle mitochondrial capacity, energy metabolism, and physical function. Nat. Commun. 12, 4773 10.1038/s41467-021-24956-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Tian Q., Mitchell B.A., Zampino M., Fishbein K.W., Spencer R.G. and Ferrucci L. (2022) Muscle mitochondrial energetics predicts mobility decline in well-functioning older adults: The baltimore longitudinal study of aging. Aging Cell 21, e13552 10.1111/acel.13552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Tian Q., Bilgel M., Walker K.A., Moghekar A.R., Fishbein K.W., Spencer R.G.et al. (2023) Skeletal muscle mitochondrial function predicts cognitive impairment and is associated with biomarkers of Alzheimer's disease and neurodegeneration. Alzheimers Dement 19, 4436–4445 10.1002/alz.13388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Kopsidas G., Kovalenko S.A., Kelso J.M. and Linnane A.W. (1998) An age-associated correlation between cellular bioenergy decline and mtDNA rearrangements in human skeletal muscle. Mutat. Res. 421, 27–36 10.1016/S0027-5107(98)00150-X [DOI] [PubMed] [Google Scholar]
- 168.Pesce V., Cormio A., Fracasso F., Vecchiet J., Felzani G., Lezza A.M.et al. (2001) Age-related mitochondrial genotypic and phenotypic alterations in human skeletal muscle. Free Radic. Biol. Med. 30, 1223–1233 10.1016/S0891-5849(01)00517-2 [DOI] [PubMed] [Google Scholar]
- 169.Murgia M., Tan J., Geyer P.E., Doll S., Mann M. and Klopstock T. (2019) Proteomics of Cytochrome c oxidase-negative versus -positive muscle fiber sections in mitochondrial myopathy. Cell Rep. 29, 3825.e4–3834.e4 10.1016/j.celrep.2019.11.055 [DOI] [PubMed] [Google Scholar]
- 170.Lanza I.R., Larsen R.G. and Kent-Braun J.A. (2007) Effects of old age on human skeletal muscle energetics during fatiguing contractions with and without blood flow. J. Physiol. 583, 1093–1105 10.1113/jphysiol.2007.138362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Conley K.E., Jubrias S.A. and Esselman P.C. (2000) Oxidative capacity and ageing in human muscle. J. Physiol. 526, 203–210 10.1111/j.1469-7793.2000.t01-1-00203.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Migliavacca E., Tay S.K.H., Patel H.P., Sonntag T., Civiletto G., McFarlane C.et al. (2019) Mitochondrial oxidative capacity and NAD+ biosynthesis are reduced in human sarcopenia across ethnicities. Nat. Commun. 10, 5808 10.1038/s41467-019-13694-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Fan Z., Yang J.Y., Guo Y., Liu Y.X. and Zhong X.Y. (2022) Altered levels of circulating mitochondrial DNA in elderly people with sarcopenia: Association with mitochondrial impairment. Exp. Gerontol. 163, 111802 10.1016/j.exger.2022.111802 [DOI] [PubMed] [Google Scholar]
- 174.Aman Y., Schmauck-Medina T., Hansen M., Morimoto R.I., Simon A.K., Bjedov I.et al. (2021) Autophagy in healthy aging and disease. Nat. Aging 1, 634–650 10.1038/s43587-021-00098-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Guillén C. and Benito M. (2018) mTORC1 overactivation as a key aging factor in the progression to type 2 diabetes mellitus. Front. Endocrinol. 9, 621 10.3389/fendo.2018.00621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Dodds R.M., Davies K., Granic A., Hollingsworth K.G., Warren C., Gorman G.et al. (2018) Mitochondrial respiratory chain function and content are preserved in the skeletal muscle of active very old men and women. Exp. Gerontol. 113, 80–85 10.1016/j.exger.2018.09.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Irving B.A., Lanza I.R., Henderson G.C., Rao R.R., Spiegelman B.M. and Nair K.S. (2015) Combined training enhances skeletal muscle mitochondrial oxidative capacity independent of age. J. Clin. Endocrinol. Metab. 100, 1654–1663 10.1210/jc.2014-3081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Gorgoulis V., Adams P.D., Alimonti A., Bennett D.C., Bischof O., Bishop C.et al. (2019) Cellular senescence: defining a path forward. Cell 179, 813–827 10.1016/j.cell.2019.10.005 [DOI] [PubMed] [Google Scholar]
- 179.Hernandez-Segura A., Nehme J. and Demaria M. (2018) Hallmarks of cellular senescence. Trends Cell Biol. 28, 436–453 10.1016/j.tcb.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 180.van Deursen J.M. (2014) The role of senescent cells in ageing. Nature 509, 439–446 10.1038/nature13193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Tuttle C.S.L., Luesken S.W.M., Waaijer M.E.C. and Maier A.B. (2021) Senescence in tissue samples of humans with age-related diseases: A systematic review. Ageing Res. Rev. 68, 101334 10.1016/j.arr.2021.101334 [DOI] [PubMed] [Google Scholar]
- 182.Acosta J.C., Banito A., Wuestefeld T., Georgilis A., Janich P., Morton J.P.et al. (2013) A complex secretory program orchestrated by the inflammasome controls paracrine senescence. Nat. Cell Biol. 15, 978–990 10.1038/ncb2784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Lopes-Paciencia S., Saint-Germain E., Rowell M.C., Ruiz A.F., Kalegari P. and Ferbeyre G. (2019) The senescence-associated secretory phenotype and its regulation. Cytokine 117, 15–22 10.1016/j.cyto.2019.01.013 [DOI] [PubMed] [Google Scholar]
- 184.Kumari R. and Jat P. (2021) Mechanisms of cellular senescence: cell cycle arrest and senescence associated secretory phenotype. Front. Cell Developmental Biol. 9, 645593 10.3389/fcell.2021.645593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Roy A.L., Sierra F., Howcroft K., Singer D.S., Sharpless N., Hodes R.J.et al. (2020) A blueprint for characterizing senescence. Cell 183, 1143–1146 10.1016/j.cell.2020.10.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Baker D.J., Wijshake T., Tchkonia T., LeBrasseur N.K., Childs B.G., van de Sluis B.et al. (2011) Clearance of p16Ink4a-positive senescent cells delays ageing-associated disorders. Nature 479, 232–236 10.1038/nature10600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Xu M., Pirtskhalava T., Farr J.N., Weigand B.M., Palmer A.K., Weivoda M.M.et al. (2018) Senolytics improve physical function and increase lifespan in old age. Nat. Med. 24, 1246–1256 10.1038/s41591-018-0092-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Englund D.A., Zhang X., Aversa Z. and LeBrasseur N.K. (2021) Skeletal muscle aging, cellular senescence, and senotherapeutics: Current knowledge and future directions. Mech. Ageing Dev. 200, 111595 10.1016/j.mad.2021.111595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Welle S., Brooks A.I., Delehanty J.M., Needler N., Bhatt K., Shah B.et al. (2004) Skeletal muscle gene expression profiles in 20-29 year old and 65-71 year old women. Exp. Gerontol. 39, 369–377 10.1016/j.exger.2003.11.011 [DOI] [PubMed] [Google Scholar]
- 190.Dungan C.M., Peck B.D., Walton R.G., Huang Z., Bamman M.M., Kern P.A.et al. (2020) In vivo analysis of γH2AX+ cells in skeletal muscle from aged and obese humans. FASEB J. 34, 7018–7035 10.1096/fj.202000111RR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Tumasian R.A. 3rd, Harish A., Kundu G., Yang J.H., Ubaida-Mohien C., Gonzalez-Freire M.et al. (2021) Skeletal muscle transcriptome in healthy aging. Nat. Commun. 12, 014 10.1038/s41467-021-22168-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Coppé J.P., Rodier F., Patil C.K., Freund A., Desprez P.Y. and Campisi J. (2011) Tumor suppressor and aging biomarker p16(INK4a) induces cellular senescence without the associated inflammatory secretory phenotype. J. Biol. Chem. 286, 36396–36403 10.1074/jbc.M111.257071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Zhang X., Habiballa L., Aversa Z., Ng Y.E., Sakamoto A.E., Englund D.A.et al. (2022) Characterization of cellular senescence in aging skeletal muscle. Nat. Aging 2, 601–615 10.1038/s43587-022-00250-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Gurkar A.U., Gerencser A.A., Mora A.L., Nelson A.C., Zhang A.R., Lagnado A.B.et al. (2023) Spatial mapping of cellular senescence: emerging challenges and opportunities. Nat. Aging 3, 776–790 10.1038/s43587-023-00446-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Habiballa L., Hruby A., Granic A., Dodds R.M., Hillman S.J., Jurk D.et al. (2023) Determining the feasibility of characterising cellular senescence in human skeletal muscle and exploring associations with muscle morphology and physical function at different ages: findings from the MASS_Lifecourse Study. GeroScience 10.1007/s11357-023-00869-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Fielding R.A., Atkinson E.J., Aversa Z., White T.A., Heeren A.A., Achenbach S.J.et al. (2022) Associations between biomarkers of cellular senescence and physical function in humans: observations from the lifestyle interventions for elders (LIFE) study. GeroScience 44, 2757–2770 10.1007/s11357-022-00685-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Zhang L., Pitcher L.E., Yousefzadeh M.J., Niedernhofer L.J., Robbins P.D. and Zhu Y. (2022) Cellular senescence: a key therapeutic target in aging and diseases. J. Clin. Invest. 132, e158450 10.1172/JCI158450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Witham M.D., Granic A., Miwa S., Passos J.F., Richardson G.D. and Sayer A.A. (2023) New Horizons in cellular senescence for clinicians. Age Ageing 52, afad127 10.1093/ageing/afad127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Engquist E.N. and Zammit P.S. (2021) The Satellite Cell at 60: The Foundation Years. J. Neuromuscul. Dis. 8, S183–S203 10.3233/JND-210705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Sousa-Victor P., García-Prat L. and Muñoz-Cánoves P. (2022) Control of satellite cell function in muscle regeneration and its disruption in ageing. Nat. Rev. Mol. Cell Biol. 23, 204–226 10.1038/s41580-021-00421-2 [DOI] [PubMed] [Google Scholar]
- 201.Grounds M.D. (2014) The need to more precisely define aspects of skeletal muscle regeneration. Int. J. Biochem. Cell Biol. 56, 56–65 10.1016/j.biocel.2014.09.010 [DOI] [PubMed] [Google Scholar]
- 202.Spalding K.L., Bhardwaj R.D., Buchholz B.A., Druid H. and Frisén J. (2005) Retrospective birth dating of cells in humans. Cell 122, 133–143 10.1016/j.cell.2005.04.028 [DOI] [PubMed] [Google Scholar]
- 203.Snijders T., Aussieker T., Holwerda A., Parise G., van Loon L.J.C. and Verdijk L.B. (2020) The concept of skeletal muscle memory: Evidence from animal and human studies. Acta Physiol. (Oxf) 229, e13465 10.1111/apha.13465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Kirby T.J. and Dupont-Versteegden E.E. (2022) Cross Talk proposal: Myonuclei are lost with ageing and atrophy. J. Physiol. 600, 2077–2080 10.1113/JP282380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Fry C.S., Lee J.D., Mula J., Kirby T.J., Jackson J.R., Liu F.et al. (2015) Inducible depletion of satellite cells in adult, sedentary mice impairs muscle regenerative capacity without affecting sarcopenia. Nat. Med. 21, 76–80 10.1038/nm.3710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Murach K.A., Fry C.S., Kirby T.J., Jackson J.R., Lee J.D., White S.H.et al. (2018) Starring or Supporting Role? Satellite Cells and Skeletal Muscle Fiber Size Regulation Physiology (Bethesda). 33, 26–38 10.1152/physiol.00019.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Grounds M.D. (2014) Therapies for sarcopenia and regeneration of old skeletal muscles: more a case of old tissue architecture than old stem cells. Bioarchitecture 4, 81–87 10.4161/bioa.29668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Joyce N.C., Oskarsson B. and Jin L.W. (2012) Muscle biopsy evaluation in neuromuscular disorders. Phys. Med. Rehabil. Clin. North Am. 23, 609–631 10.1016/j.pmr.2012.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Crameri R.M., Aagaard P., Qvortrup K., Langberg H., Olesen J. and Kjaer M. (2007) Myofibre damage in human skeletal muscle: effects of electrical stimulation versus voluntary contraction. J. Physiol. 583, 365–380 10.1113/jphysiol.2007.128827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Karlsen A., Soendenbroe C., Malmgaard-Clausen N.M., Wagener F., Moeller C.E., Senhaji Z.et al. (2020) Preserved capacity for satellite cell proliferation, regeneration, and hypertrophy in the skeletal muscle of healthy elderly men. FASEB J. 34, 6418–6436 10.1096/fj.202000196R [DOI] [PubMed] [Google Scholar]
- 211.González-Blanco L., Bermúdez M., Bermejo-Millo J.C., Gutiérrez-Rodríguez J., Solano J.J., Antuña E.et al. (2022) Cell interactome in sarcopenia during aging. J. Cachexia Sarcopenia Muscle 13, 919–931 10.1002/jcsm.12937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Novak J.S., Mázala D.A.G., Nearing M., Hindupur R., Uapinyoying P., Habib N.F.et al. (2021) Human muscle stem cells are refractory to aging. Aging Cell 20, e13411 10.1111/acel.13411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Shavlakadze T., McGeachie J. and Grounds M.D. (2010) Delayed but excellent myogenic stem cell response of regenerating geriatric skeletal muscles in mice. Biogerontology 11, 363–376 10.1007/s10522-009-9260-0 [DOI] [PubMed] [Google Scholar]
- 214.Duong L., Radley H.G., Lee B., Dye D.E., Pixley F.J., Grounds M.D.et al. (2021) Macrophage function in the elderly and impact on injury repair and cancer. Immun. Ageing 18, 4 10.1186/s12979-021-00215-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Nederveen J.P., Betz M.W., Snijders T. and Parise G. (2021) The importance of muscle capillarization for optimizing satellite cell plasticity. Exerc. Sport Sci. Rev. 49, 284–290 10.1249/JES.0000000000000270 [DOI] [PubMed] [Google Scholar]
- 216.Larouche J.A., Mohiuddin M., Choi J.J., Ulintz P.J., Fraczek P., Sabin K.et al. (2021) Murine muscle stem cell response to perturbations of the neuromuscular junction are attenuated with aging. eLife 10, e66749 10.7554/eLife.66749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Ng D.C.H., Ho U.Y. and Grounds M.D. (2021) Cilia, centrosomes and skeletal muscle. Int. J. Mol. Sci. 22, 9605 10.3390/ijms22179605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Tomay F., Wells K., Duong L., Tsu J.W., Dye D.E., Radley-Crabb H.G.et al. (2018) Aged neutrophils accumulate in lymphoid tissues from healthy elderly mice and infiltrate T- and B-cell zones. Immunol. Cell Biol. 96, 831–840 10.1111/imcb.12046 [DOI] [PubMed] [Google Scholar]
- 219.Ferrara P.J., Yee E.M., Petrocelli J.J., Fix D.K., Hauser C.T., de Hart N.M.M.P.et al. (2022) Macrophage immunomodulation accelerates skeletal muscle functional recovery in aged mice following disuse atrophy. J. Appl. Physiol. 133, 919–931 10.1152/japplphysiol.00374.2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Zhang C., Cheng N., Qiao B., Zhang F., Wu J., Liu C.et al. (2020) Age-related decline of interferon-gamma responses in macrophage impairs satellite cell proliferation and regeneration. J. Cachexia Sarcopenia Muscle 11, 1291–1305 10.1002/jcsm.12584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Buttner R., Schulz A., Reuter M., Akula A.K., Mindos T., Carlstedt A.et al. (2018) Inflammaging impairs peripheral nerve maintenance and regeneration. Aging Cell 17, e12833 10.1111/acel.12833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Moreno-García A., Kun A., Calero O., Medina M. and Calero M. (2018) An Overview of the Role of Lipofuscin in Age-Related Neurodegeneration. Front. Neurosci. 12, 464 10.3389/fnins.2018.00464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Tidball J.G., Flores I., Welc S.S., Wehling-Henricks M. and Ochi E. (2021) Aging of the immune system and impaired muscle regeneration: A failure of immunomodulation of adult myogenesis. Exp. Gerontol. 145, 111200 10.1016/j.exger.2020.111200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Aagaard P., Suetta C., Caserotti P., Magnusson S.P. and Kjaer M. (2010) Role of the nervous system in sarcopenia and muscle atrophy with aging: strength training as a countermeasure. Scand. J. Med. Sci. Sports 20, 49–64 10.1111/j.1600-0838.2009.01084.x [DOI] [PubMed] [Google Scholar]
- 225.Larsson L., Degens H., Li M., Salviati L., Lee Y.I., Thompson W.et al. (2019) Sarcopenia: Aging-Related Loss of Muscle Mass and Function. Physiol. Rev. 99, 427–511 10.1152/physrev.00061.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Dowling P., Gargan S., Swandulla D. and Ohlendieck K. (2022) Proteomic profiling of impaired excitation-contraction coupling and abnormal calcium handling in muscular dystrophy. Proteomics 22, e2200003 10.1002/pmic.202200003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Deschenes M.R., Flannery R., Hawbaker A., Patek L. and Mifsud M. (2022) Adaptive remodeling of the neuromuscular junction with aging. Cells 11, 1150 10.3390/cells11071150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Piasecki M., Ireland A., Jones D.A. and McPhee J.S. (2016) Age-dependent motor unit remodelling in human limb muscles. Biogerontology 17, 485–496 10.1007/s10522-015-9627-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Sonjak V., Jacob K., Morais J.A., Rivera-Zengotita M., Spendiff S., Spake C.et al. (2019) Fidelity of muscle fibre reinnervation modulates ageing muscle impact in elderly women. J. Physiol. 597, 5009–5023 10.1113/JP278261 [DOI] [PubMed] [Google Scholar]
- 230.Taetzsch T. and Valdez G. (2018) NMJ maintenance and repair in aging. Curr. Opin. Physiol. 4, 57–64 10.1016/j.cophys.2018.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Jones R.A., Harrison C., Eaton S.L., Llavero Hurtado M., Graham L.C., Alkhammash L.et al. (2017) Cellular and molecular anatomy of the human neuromuscular junction. Cell Rep. 21, 2348–2356 10.1016/j.celrep.2017.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Jackson M.J. (2020) On the mechanisms underlying attenuated redox responses to exercise in older individuals: A hypothesis. Free Radic. Biol. Med. 161, 326–338 10.1016/j.freeradbiomed.2020.10.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Grosicki G.J., Zepeda C.S. and Sundberg C.W. (2022) Single muscle fibre contractile function with ageing. J. Physiol. 600, 5005–5026 10.1113/JP282298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Rattan S.I.S. (2020) Naive extrapolations, overhyped claims and empty promises in ageing research and interventions need avoidance. Biogerontology 21, 415–421 10.1007/s10522-019-09851-0 [DOI] [PubMed] [Google Scholar]
- 235.Pichavant C. and Pavlath G.K. (2014) Incidence and severity of myofiber branching with regeneration and aging. Skelet. Muscle 4, 9 10.1186/2044-5040-4-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Suetterlin K.J. and Sayer A.A. (2014) Proprioception: where are we now? A commentary on clinical assessment, changes across the life course, functional implications and future interventions Age Ageing 43, 313–318 10.1093/ageing/aft174 [DOI] [PubMed] [Google Scholar]
- 237.Krishnan V.S., Shavlakadze T., Grounds M.D., Hodgetts S.I. and Harvey A.R. (2018) Age-related loss of VGLUT1 excitatory, but not VGAT inhibitory, immunoreactive terminals on motor neurons in spinal cords of old sarcopenic male mice. Biogerontology 19, 385–399 10.1007/s10522-018-9765-5 [DOI] [PubMed] [Google Scholar]
- 238.Castro R.W., Lopes M.C., Settlage R.E. and Valdez G. (2023) Aging alters mechanisms underlying voluntary movements in spinal motor neurons of mice, primates, and humans. JCI Insight 8, e168448 10.1172/jci.insight.168448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Gillon A., Nielsen K., Steel C., Cornwall J. and Sheard P. (2018) Exercise attenuates age-associated changes in motoneuron number, nucleocytoplasmic transport proteins and neuromuscular health. GeroScience 40, 177–192 10.1007/s11357-018-0020-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Santuz A. and Akay T. (2023) Muscle spindles and their role in maintaining robust locomotion. J. Physiol. 601, 275–285 10.1113/JP282563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Soendenbroe C., Andersen J.L. and Mackey A.L. (2021) Muscle-nerve communication and the molecular assessment of human skeletal muscle denervation with aging. Am. J. Physiol. Cell Physiol. 321, C317–C329 10.1152/ajpcell.00174.2021 [DOI] [PubMed] [Google Scholar]
- 242.Kamen G. and Knight C.A. (2004) Training-related adaptations in motor unit discharge rate in young and older adults. J. Gerontol. A Biol. Sci. Med. Sci. 59, 1334–1338 10.1093/gerona/59.12.1334 [DOI] [PubMed] [Google Scholar]
- 243.O'Bryan S.J. and Hiam D. (2022) The benefits of physical activity on neuromuscular structure and function in old age. J. Physiol. 600, 2283–2285 10.1113/JP283102 [DOI] [PubMed] [Google Scholar]
- 244.Coletti C., Acosta G.F., Keslacy S. and Coletti D. (2022) Exercise-mediated reinnervation of skeletal muscle in elderly people: An update. Eur. J. Transl. Myol. 32, 10416 10.4081/ejtm.2022.10416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Coletta G. and Phillips S.M. (2023) An elusive consensus definition of sarcopenia impedes research and clinical treatment: A narrative review. Ageing Res. Rev. 86, 101883 10.1016/j.arr.2023.101883 [DOI] [PubMed] [Google Scholar]
- 246.Raffin J., de Souto Barreto P., Le Traon A.P., Vellas B., Aubertin-Leheudre M. and Rolland Y. (2023) Sedentary behavior and the biological hallmarks of aging. Ageing Res. Rev. 83, 101807 10.1016/j.arr.2022.101807 [DOI] [PubMed] [Google Scholar]
- 247.Pannérec A., Springer M., Migliavacca E., Ireland A., Piasecki M., Karaz S.et al. (2016) A robust neuromuscular system protects rat and human skeletal muscle from sarcopenia. Aging 8, 712–729 10.18632/aging.100926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Clark B.C. and Carson R.G. (2021) Sarcopenia and neuroscience: learning to communicate. Gerontol. A Biol. Sci. Med. Sci. 76, 1882–1890 10.1093/gerona/glab098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Jankelowitz S.K., McNulty P.A. and Burke D. (2007) Changes in measures of motor axon excitability with age. Clin. Neurophysiol. 118, 1397–1404 10.1016/j.clinph.2007.02.025 [DOI] [PubMed] [Google Scholar]
- 250.Tomlinson B.E. and Irving D. (1977) The numbers of limb motor neurons in the human lumbosacral cord throughout life. J. Neurol. Sci. 34, 213–219 10.1016/0022-510X(77)90069-7 [DOI] [PubMed] [Google Scholar]
- 251.Palve S.S. and Palve S.B. (2018) Impact of aging on nerve conduction velocities and late responses in healthy individuals. J. Neurosci. Rural. Pract. 9, 112–116 10.4103/jnrp.jnrp_323_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Grounds M.D., Sorokin L. and White J. (2005) Strength at the extracellular matrix-muscle interface. Scand. J. Med. Sci. Sports 15, 381–391 10.1111/j.1600-0838.2005.00467.x [DOI] [PubMed] [Google Scholar]
- 253.Grounds M.D. (2008) Complexity of extracellular matrix and skeletal muscle regeneration. In Skeletal muscle repair and regeneration. Advences in Muscle Research(Schiaffino S. and Partridge T., eds), pp. 269–302, Springer, Dordrecht: 10.1007/978-1-4020-6768-6_13 [DOI] [Google Scholar]
- 254.Csapo R., Gumpenberger M. and Wessner B. (2020) Skeletal muscle extracellular matrix - what do we know about its composition, regulation, and physiological roles? A narrative review Front. Physiol. 11, 253 10.3389/fphys.2020.00253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Barns M., Gondro C., Tellam R.L., Radley-Crabb H.G., Grounds M.D. and Shavlakadze T. (2014) Molecular analyses provide insight into mechanisms underlying sarcopenia and myofibre denervation in old skeletal muscles of mice. Int. J. Biochem. Cell Biol. 53, 174–185 10.1016/j.biocel.2014.04.025 [DOI] [PubMed] [Google Scholar]
- 256.Zullo A., Fleckenstein J., Schleip R., Hoppe K., Wearing S. and Klingler W. (2020) Structural and functional changes in the coupling of fascial tissue, skeletal muscle, and nerves during aging. Front. Physiol. 11, 592 10.3389/fphys.2020.00592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Gumpenberger M., Wessner B., Graf A., Narici M.V., Fink C., Braun S.et al. (2020) Remodeling the skeletal muscle extracellular matrix in older age-effects of acute exercise stimuli on gene expression. Int. J. Mol. Sci. 21, 7089 10.3390/ijms21197089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Kragstrup T.W., Kjaer M. and Mackey A.L. (2011) Structural, biochemical, cellular, and functional changes in skeletal muscle extracellular matrix with aging. Scand. J. Med. Sci. Sports 21, 749–757 10.1111/j.1600-0838.2011.01377.x [DOI] [PubMed] [Google Scholar]
- 259.Pavan P., Monti E., Bondí M., Fan C., Stecco C., Narici M.et al. (2020) Alterations of extracellular matrix mechanical properties contribute to age-related functional impairment of human skeletal muscles. Int. J. Mol. Sci. 21, 3992 10.3390/ijms21113992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Mavropalias G., Boppart M., Usher K.M., Grounds M.D., Nosaka K. and Blazevich A.J. (2023) Exercise builds the scaffold of life: muscle extracellular matrix biomarker responses to physical activity, inactivity, and aging. Biol. Rev. Camb. Philos. Soc. 98, 481–519 10.1111/brv.12916 [DOI] [PubMed] [Google Scholar]
- 261.Nielsen K.B., Lal N.N. and Sheard P.W. (2018) Age-related remodelling of the myotendinous junction in the mouse soleus muscle. Exp. Gerontol. 104, 52–59 10.1016/j.exger.2018.01.021 [DOI] [PubMed] [Google Scholar]
- 262.Lal N.N., Cornwall J. and Sheard P.W. (2021) Age-related structural changes show that loss of fibers is not a significant contributor to muscle atrophy in old mice. Exp. Gerontol. 156, 111618 10.1016/j.exger.2021.111618 [DOI] [PubMed] [Google Scholar]
- 263.Hendrickse P. and Degens H. (2019) The role of the microcirculation in muscle function and plasticity. J. Muscle Res. Cell Motil. 40, 127–140 10.1007/s10974-019-09520-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Barnouin Y., McPhee J.S., Butler-Browne G., Bosutti A., De Vito G., Jones D.A.et al. (2017) Coupling between skeletal muscle fiber size and capillarization is maintained during healthy aging. J. Cachexia Sarcopenia Muscle 8, 647–659 10.1002/jcsm.12194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Nederveen J.P., Betz M.W., Snijders T. and Parise G. (2021) The importance of muscle capillarization for optimizing satellite cell plasticity. Exerc. Sport Sci. Rev. 49, 284–290 10.1249/JES.0000000000000270 [DOI] [PubMed] [Google Scholar]
- 266.Nederveen J.P., Joanisse S., Snijders T., Ivankovic V., Baker S.K., Phillips S.M.et al. (2016) Skeletal muscle satellite cells are located at a closer proximity to capillaries in healthy young compared with older men. J. Cachexia Sarcopenia Muscle 7, 547–554 10.1002/jcsm.12105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Betz M.W., Aussieker T., Kruger C.Q., Gorissen S.H.M., van Loon L.J.C. and Snijders T. (2021) Muscle fiber capillarization is associated with various indices of skeletal muscle mass in healthy, older men. Exp. Gerontol. 143, 111161 10.1016/j.exger.2020.111161 [DOI] [PubMed] [Google Scholar]
- 268.Snijders T., Nederveen J.P., Verdijk L.B., Houben A.J.H.M., Goossens G.H., Parise G.et al. (2017) Muscle fiber capillarization as determining factor on indices of insulin sensitivity in humans. Physiol. Rep. 5, e13278 10.14814/phy2.13278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Nicklas B.J., Leng I., Delbono O., Kitzman D.W., Marsh A.P., Hundley W.G.et al. (2008) Relationship of physical function to vastus lateralis capillary density and metabolic enzyme activity in elderly men and women. Aging Clin. Exp. Res. 20, 302–309 10.1007/BF03324860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Prior S.J., Ryan A.S., Blumenthal J.B., Watson J.M., Katzel L.I. and Goldberg A.P. (2016) Sarcopenia Is Associated With Lower Skeletal Muscle Capillarization and Exercise Capacity in Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 71, 1096–1101 10.1093/gerona/glw017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Groen B.B., Hamer H.M., Snijders T., van Kranenburg J., Frijns D., Vink H.et al. (2014) Skeletal muscle capillary density and microvascular function are compromised with aging and type 2 diabetes. J. Appl. Physiol. 116, 998–1005 10.1152/japplphysiol.00919.2013 [DOI] [PubMed] [Google Scholar]
- 272.Barclay C.J., Woledge R.C. and Curtin N.A. (2007) Energy turnover for Ca2+ cycling in skeletal muscle. J. Muscle Res. Cell Motil. 28, 259–274 10.1007/s10974-007-9116-7 [DOI] [PubMed] [Google Scholar]
- 273.Mattson M.P. and Arumugam T.V. (2018) Hallmarks of Brain Aging: Adaptive and Pathological Modification by Metabolic States. Cell Metab. 27, 1176–1199 10.1016/j.cmet.2018.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Lamboley C.R., Wyckelsma V.L., Dutka T.L., McKenna M.J., Murphy R.M. and Lamb G.D. (2015) Contractile properties and sarcoplasmic reticulum calcium content in type I and type II skeletal muscle fibres in active aged humans. J. Physiol. 593, 2499–2514 10.1113/JP270179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Lamboley C.R., Wyckelsma V.L., McKenna M.J., Murphy R.M. and Lamb G.D. (2016) Ca(2+) leakage out of the sarcoplasmic reticulum is increased in type I skeletal muscle fibres in aged humans. J. Physiol. 594, 469–481 10.1113/JP271382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Andersson D.C., Betzenhauser M.J., Reiken S., Meli A.C., Umanskaya A., Xie W.et al. (2011) Ryanodine receptor oxidation causes intracellular calcium leak and muscle weakness in aging. Cell Metab. 14, 196–207 10.1016/j.cmet.2011.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Pietrangelo L., D'Incecco A., Ainbinder A., Michelucci A., Kern H., Dirksen R.T.et al. (2015) Age-dependent uncoupling of mitochondria from Ca2+ release units in skeletal muscle. Oncotarget 6, 35358–35371 10.18632/oncotarget.6139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Jouaville L.S., Pinton P., Bastianutto C., Rutter G.A. and Rizzuto R. (1999) Regulation of mitochondrial ATP synthesis by calcium: evidence for a long-term metabolic priming. Proc. Natl. Acad. Sci. U. S. A. 96, 13807–13812 10.1073/pnas.96.24.13807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Umanskaya A., Santulli G., Xie W., Andersson D.C., Reiken S.R. and Marks A.R. (2014) Genetically enhancing mitochondrial antioxidant activity improves muscle function in aging. Proc. Natl. Acad. Sci. U. S. A. 111, 15250–15255 10.1073/pnas.1412754111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Hanson M.G., Wilde J.J., Moreno R.L., Minic A.D. and Niswander L. (2015) Potassium dependent rescue of a myopathy with core-like structures in mouse. eLife 4, e02923 10.7554/eLife.02923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Cheng C.J., Kuo E. and Huang C.L. (2013) Extracellular potassium homeostasis: insights from hypokalemic periodic paralysis. Semin. Nephrol. 33, 237–247 10.1016/j.semnephrol.2013.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Dyke J.P., Meyring-Wösten A., Zhao Y., Linz P., Thijssen S. and Kotanko P. (2018) Reliability and agreement of sodium (23Na) MRI in calf muscle and skin of healthy subjects from the US. Clin. Imaging 52, 100–105 10.1016/j.clinimag.2018.07.010 [DOI] [PubMed] [Google Scholar]
- 283.Kopp C., Linz P., Dahlmann A., Hammon M., Jantsch J., Müller D.N.et al. (2013) 23Na magnetic resonance imaging-determined tissue sodium in healthy subjects and hypertensive patients. Hypertension 61, 635–640 10.1161/HYPERTENSIONAHA.111.00566 [DOI] [PubMed] [Google Scholar]
- 284.Simms H.S. and Stolman A. (1937) Changes in human tissue electrolytes in senescence. Science 86, 269–270 10.1126/science.86.2229.269 [DOI] [PubMed] [Google Scholar]
- 285.Forsberg A.M., Bergström J., Lindholm B. and Hultman E. (1997) Resting membrane potential of skeletal muscle calculated from plasma and muscle electrolyte and water contents. Clin. Sci. (Lond.) 92, 391–396 10.1042/cs0920391 [DOI] [PubMed] [Google Scholar]
- 286.Lee J.H.F., Boland-Freitas R. and Ng K. (2018) Sarcolemmal excitability changes in normal human aging. Muscle Nerve 57, 981–988 10.1002/mus.26058 [DOI] [PubMed] [Google Scholar]
- 287.Chugh D., Iyer C.C., Wang X., Bobbili P., Rich M.M. and Arnold W.D. (2020) Neuromuscular junction transmission failure is a late phenotype in aging mice. Neurobiol. Aging 86, 182–190 10.1016/j.neurobiolaging.2019.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Padilla C.J., Harrigan M.E., Harris H., Schwab J.M., Rutkove S.B., Rich M.M.et al. (2021) Profiling age-related muscle weakness and wasting: neuromuscular junction transmission as a driver of age-related physical decline. GeroScience 43, 1265–1281 10.1007/s11357-021-00369-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Suetterlin K.J., Tan S.V., Mannikko R., Phadke R., Orford M., Eaton S.et al. (2021) Ageing contributes to phenotype transition in a mouse model of periodic paralysis. JCSM Rapid Commun. 4, 245–259 10.1002/rco2.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Clausen T. (2003) Na+-K+ pump regulation and skeletal muscle contractility. Physiol. Rev. 83, 1269–1324 10.1152/physrev.00011.2003 [DOI] [PubMed] [Google Scholar]
- 291.Gagnon K.B. and Delpire E. (2021) Sodium transporters in human health and disease. Front. Physiol. 11, 588664 10.3389/fphys.2020.588664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Layec G., Trinity J.D., Hart C.R., Le Fur Y., Zhao J., Reese V.et al. (2018) Impaired muscle efficiency but preserved peripheral hemodynamics and mitochondrial function with advancing age: evidence from exercise in the young, old, and oldest-old. J. Gerontol. A Biol. Sci. Med. Sci. 73, 1303–1312 10.1093/gerona/gly050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Sundberg C.W., Prost R.W., Fitts R.H. and Hunter S.K. (2019) Bioenergetic basis for the increased fatigability with ageing. J. Physiol. 597, 4943–4957 10.1113/JP277803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Sundberg C.W., Hunter S.K., Trappe S.W., Smith C.S. and Fitts R.H. (2018) Effects of elevated H+ and Pi on the contractile mechanics of skeletal muscle fibres from young and old men: implications for muscle fatigue in humans. J. Physiol. 596, 3993–4015 10.1113/JP276018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Sundberg C.W., Kuplic A., Hassanlouei H. and Hunter S.K. (2018) Mechanisms for the age-related increase in fatigability of the knee extensors in old and very old adults. J. Appl. Physiol. (1985) 125, 146–158 10.1152/japplphysiol.01141.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Aalkjær C. and Nielsen O.B. (2018) The ins and outs of acid-base transport in skeletal muscle. J. Gen. Physiol. 150, 3–6 10.1085/jgp.201711955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Dodds R. and Aihie Sayer A. (2021) A lifecourse approach to sarcopenia. In Sarcopenia(Cruz-Jentoft A.J. and Morley J.E., eds), pp. 77–93, Wiley Blackwell; 10.1002/9781119597896.ch8 [DOI] [Google Scholar]
- 298.Mankhong S., Kim S., Moon S., Kwak H.B., Park D.H. and Kang J.H. (2020) Experimental models of sarcopenia: bridging molecular mechanism and therapeutic strategy. Cells 9, 1385 10.3390/cells9061385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Shen Y., Shi Q., Nong K., Li S., Yue J., Huang J.et al. (2023) Exercise for sarcopenia in older people: a systematic review and network meta-analysis. J. Cachexia Sarcopenia Muscle 14, 1199–1211 10.1002/jcsm.13225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Distefano G. and Goodpaster B.H. (2018) Effects of exercise and aging on skeletal muscle. Cold Spring Harb. Perspect. Med. 8, a029785 10.1101/cshperspect.a029785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Garatachea N., Pareja-Galeano H., Sanchis-Gomar F., Santos-Lozano A., Fiuza-Luces C., Morán M.et al. (2015) Exercise attenuates the major hallmarks of aging. Rejuvenation Res. 18, 57–89 10.1089/rej.2014.1623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Goh J., Wong E., Soh J., Maier A.B. and Kennedy B.K. (2023) Targeting the molecular and cellular pillars of human aging with exercise. FEBS J. 290, 649–668 10.1111/febs.16337 [DOI] [PubMed] [Google Scholar]
- 303.Rebelo-Marques A., De Sousa Lages A., Andrade R., Ribeiro C.F., Mota-Pinto A., Carrilho F.et al. (2018) Aging hallmarks: the benefits of physical exercise. Front. Endocrinol. (Lausanne) 9, 258 10.3389/fendo.2018.00258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Nasimi N., Sohrabi Z., Nunes E.A., Sadeghi E., Jamshidi S., Gholami Z.et al. (2023) Whey protein supplementation with or without vitamin D on sarcopenia-related measures: a systematic review and meta-analysis. Adv. Nutr. 14, 762–773 10.1016/j.advnut.2023.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Cornish S.M., Cordingley D.M., Shaw K.A., Forbes S.C., Leonhardt T., Bristol A.et al. (2022) Effects of omega-3 supplementation alone and combined with resistance exercise on skeletal muscle in older adults: a systematic review and meta-analysis. Nutrients 14, 2221 10.3390/nu14112221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Shannon O.M., Ashor A.W., Scialo F., Saretzki G., Martin-Ruiz C., Lara J.et al. (2021) Mediterranean diet and the hallmarks of ageing. Eur. J. Clin. Nutr. 75, 1176–1192 10.1038/s41430-020-00841-x [DOI] [PubMed] [Google Scholar]
- 307.Liu C., Cheung W.H., Li J., Chow S.K., Yu J., Wong S.H.et al. (2021) Understanding the gut microbiota and sarcopenia: a systematic review. J. Cachexia Sarcopenia Muscle 12, 1393–1407 10.1002/jcsm.12784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Yang J.H., Hayano M., Griffin P.T., Amorim J.A., Bonkowski M.S., Apostolides J.K.et al. (2023) Loss of epigenetic information as a cause of mammalian aging. Cell 186, 305.e27–326.e27 10.1016/j.cell.2022.12.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Arosio B., Calvani R., Ferri E., Coelho-Junior H.J., Carandina A., Campanelli F.et al. (2023) Sarcopenia and Cognitive Decline in Older Adults: Targeting the Muscle-Brain Axis. Nutrients 15, 1853 10.3390/nu15081853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Han X., Ashraf M., Tipparaju S.M. and Xuan W. (2023) Muscle-brain crosstalk in cognitive impairment. Front. Aging Neurosci. 15, 1221653 10.3389/fnagi.2023.1221653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Coletta G. and Phillips S.M. (2023) An elusive consensus definition of sarcopenia impedes research and clinical treatment: A narrative review. Ageing Res. Rev. 86, 101883 10.1016/j.arr.2023.101883 [DOI] [PubMed] [Google Scholar]
- 312.Carvalho do Nascimento P.R., Bilodeau M. and Poitras S. (2021) How do we define and measure sarcopenia? A meta-analysis of observational studies Age Ageing 50, 1906–1913 10.1093/ageing/afab148 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This is a narrative review and not an original research paper.