Abstract
Little is known about the impact of sociocultural stressors such as acculturative stress on self-rated health among Hispanics. We aimed to examine (a) associations between acculturative stress and self-rated health, and (b) the moderating effects of the community of settlement (i.e., Maricopa County, AZ and Miami-Dade County, FL) and social support on the association between acculturative stress and self-rated health. A hierarchical multiple regression model and moderation analyses were conducted using a cross-sectional sample of 200 Hispanic emerging adults from Arizona and Florida. Findings indicate that higher levels of pressure to acculturate are associated with lower levels of self-rated health. Community of settlement functioned as a moderator whereby pressure to acculturate was only associated with lower levels of self-rated health in Maricopa County. Lastly, a three-way interaction indicated that emotional social support mitigated the association between pressure to acculturate and self-rated health in Maricopa County. This study highlights the importance of accounting for community of settlement when examining associations between acculturative stress and health-related outcomes. A finding that may have implications for interventions is that social support may help to counteract the effects of acculturative stress.
Keywords: Acculturation stress, Coping, Stress buffering, Perceive health, Latinos
Introduction
Self-rated health is a measure of perceived health status that serves as a valid and reliable indicator of mortality, chronic disease, and objective assessments of health status (e.g., medical diagnoses, biomarkers), including among Hispanic populations (inclusive of Latino/Latina/Latinx) [1–3]. While higher levels of psychological stress have been linked with poorer self-rated health [4], little is known about sociocultural stressors that are relevant to Hispanics, and their respective associations with self-rated health.
Research on self-rated health merits attention, particularly among emerging adulthood, a period roughly spanning the ages of 18–25, given that clinical endpoints (e.g., chronic disease) at this developmental stage are rare [5]. Emerging adulthood is often challenging and stressful due to multiple developmental psychosocial transitional factors, including changes in autonomy, developmental tasks, and social roles [6, 7]. This period may be particularly difficult for Hispanic emerging adults because many encounter sociocultural stressors (e.g., acculturative stress, ethnic discrimination) that may increase their risk of developing adverse health outcomes over the lifecourse [8–10].
To better understand self-rated health among Hispanic emerging adults, our study aimed to examine (a) associations between components of acculturative stress and self-rated health, and (b) the extent to which social support and community of settlement (i.e., Miami-Dade County, Florida and Maricopa County, Arizona) may operate as moderators of these focal associations. Our examination of these aims is guided by an integrated approach that includes the Stress Buffering Model and the Contextual Model of Acculturative Stress. The Stress Buffering Model proposes that higher levels of social support may help mitigate the effects of stressors (i.e., acculturative stress) on health-related outcomes (i.e., self-rated health) [11] and the Contextual Model of Acculturative Stress suggests that contextual factors, such as the community of settlement, may influence levels of acculturative stress [12].
Acculturative Stress
Acculturative stress, a multidimensional construct, encompasses the stress response stemming from negotiating and adjusting to perceived cultural incompatibilities when interacting with the receiving culture (i.e., U.S. culture) and the heritage culture (i.e., Hispanic culture) [13, 14]. Two indicators of acculturative stress are “pressure to acculturate,” which refers to the perceived pressure to accept American cultural standards, and “pressure against acculturation,” which refers to the perceived pressure from individuals of the heritage culture to prevent inheriting American cultural values or becoming Americanized [14]. A growing body of evidence indicates that acculturative stress adversely influences health outcomes (e.g., mental, physical health) and the well-being of Hispanics [15–17]. For example, higher levels of acculturative stress have been associated with higher depressive symptoms [18–20]. However, research on acculturative stress and self-rated health among Hispanics is scarce. We found two studies that appeared to examine this relationship; however, our review of these articles found that thay examined ethnic discrimination [21] and migration-related stress [22] rather than acculturative stress. As a result, our study may be the first study that examines the association between acculturative stress and self-rated health among Hispanics.
Community of Settlement
Environmental factors, such as the community of settlement, where an individual resides (e.g., Miami-Dade County, Maricopa County), may have a direct impact on the levels of acculturative stress and their respective effects on health-related outcomes. According to the Contextual Model of Acculturative Stress, the community of settlement (region of residence) directly influences the association between the level of acculturative stress and psychological distress [12]. This relationship may be partly caused by the way residents are expected to act in the community where they live [23]. Additionally, the community of settlement may also moderate the associations between acculturative stress and health-related outcomes.
For instance, one study found that Hispanic youth in North Carolina were more likely than Hispanic youth in Los Angeles to report symptoms of depression and anxiety [24]. An explanation for this finding is that the Hispanic population of North Carolina is smaller than that of California. Thus, North Carolina’s Hispanic youth may not perceive social acceptance in their communities based on their ethnicity. Our study might have similar findings as in Maricopa County, 31% of the population is Hispanic, compared to 69% in Miami-Dade County [25, 26]. The cultural and economic ties between Miami-Dade County and Latin America distinguish it from Maricopa County as the “Gateway to the Americas” [27]. Because of this, there may be differences in Hispanic attitudes, ethnic density, public policy, and resources [28, 29]. To our knowledge, no research has studied the impact of this unique social context on acculturative stress and self-rated health among Hispanics of any age group.
Social Support
Social support, a multidimensional construct, describes an individual’s social network and the degree to which members of the social network serve particular functions like providing guidance or showing empathy [30, 31]. Research has found that higher levels of social support are associated with better health-related outcomes, including self-rated health [32]. This association is explained in part by the Stress Buffering Model which posits that social support mitigates the adverse effects of stressors (e.g., acculturative stress) on health-related outcomes (e.g., self-rated health). Extant research on relations between acculturative stress, social support, and mental health support this model [10, 33–35]. Despite evidence that social support improves health outcomes, studies have not examined the moderating effects of social support on the association between acculturative stress and self-rated health among Hispanics.
Present Study
Guided by the Stress Buffering Model, the Contextual Model of Acculturative Stress, and existing literature, the following hypotheses were developed. Hypothesis one higher levels of pressure to acculturate and pressure against acculturation will respectively be associated with lower self-rated health. Hypothesis two the community of settlement will moderate respective associations among pressure to acculturate and pressure against acculturation with self-rated health. Due to the smaller Hispanic population in Maricopa County, compared to Miami-Dade County we expect that the adverse association between pressure to acculturate and self-rated health will be stronger among participants in Maricopa County. By contrast, the association between pressure against acculturation and self-rated health will be stronger among participants in Miami-Dade County. Hypothesis three, higher levels of emotional social support and tangible social support will mitigate the respective associations among pressure to acculturate and pressure against acculturation with self-rated health.
We will conduct posthoc analyses to test three-way interactions between respective components of acculturative stress, respective components of social support, and community of settlement (e.g., pressure to acculturate, emotional social support, and community of settlement). However, given the scarcity of literature, we are not proposing specific directional hypotheses.
Methods
Procedure and Participants
The present study was approved by the Institutional Review Board of Florida International University. We utilized data from a cross-sectional study with a sample of 200 participants from the Project on Health among Emerging Adult Latinos (Project HEAL). Quota sampling was used to recruit a convenience sample of participants using in-person, posting flyers, and targeted emails. Inclusion criteria for participants included being between the age of 18 and 25, self-identifying as Hispanic, ability to read English, and currently residing in Maricopa County, AZ or Miami-Dade County, FL. Participants provided informed consent to participate in the study by signing an electronic informed consent form. All measures in the survey were conducted in English. The survey took approximately 50 min to complete, and participants were compensated with a $30 electronic Amazon gift card. More details on the procedures for Project HEAL are published elsewhere [36].
Measures
Demographic Questionnaire
The following sociodemographic variables were included as dichotomous covariates: gender (0 = men, 1 = women), community of settlement (0 = Miami-Dade County, FL, 1 = Maricopa County, AZ), partner status (0 = single, 1 = has a partner), nativity (0 = immigrant, 1 = non-immigrant), Hispanic heritage group (0 = other Hispanics, 1 = Mexican heritage), student status (0 = current college student, 1 = non-college student), and employment status (0 = unemployed, 1 = employed). Age and financial strain (1 = has more money than needed, 2 = just enough money for needs, 3 = not enough money to meet needs) were also included as covariates. These variables were included in the regression analyses to control for potential confounding effects [37–39].
Self-rated Health
General self-rated health status was assessed with a question retrieved from the Short-form Health Survey [40]. The question was, “Generally speaking, how would you describe your health status?” and used a five-point Likert-type scale (1 = poor, 5 = excellent). This single item is a valid and strong predictor of morbidity and mortality [2] and has also been widely used in epidemiological studies in the U.S. with diverse populations, including Hispanic populations [21, 41, 42].
Acculturative Stress
Two components of self-reported acculturative stress were measured with the Multidimensional Acculturative Stress Inventory (MASI) [14]. Pressure to acculturate (e.g., “I feel uncomfortable when others expect me to know American ways of doing things”) was measured with the corresponding seven-item subscale of the MASI. Pressure against acculturation (e.g., “I have had conflicts with others because I prefer American customs over Latino ones”) was measured with the corresponding four-item subscale of the MASI. Participants responded using a five-point Likert-type scale (1 = not at all stressful, 5 = extremely stressful). Otherwise, they indicated “This did not occur in the past year,” which was recorded as a score of zero. Higher mean scores indicate higher levels of acculturative stress for each respective subscale.
Social Support
Two dimensions of social support were measured using the Medical Outcomes Study Social Support Survey (MOSSSS) [43]. Perceived tangible social support (e.g., Someone to help you if you were confined to bed) and emotional social support (e.g., Have someone to turn to for suggestions about how to deal with a personal problem) were measured with the corresponding four-item subscale of the MOSSSS. Participants responded using a five-point Likert-type scale (1 = none of the time, 5 = all of the time). Higher mean scores indicate higher levels of social support for each respective subscale.
Statistical Analysis Plan
The main effects of the predictor variables on self-rated health were estimated using hierarchical multiple regression (HMR). In a specified order, predictor variables were entered into the HMR model so that each block of predictors contributed to the explanatory variance of the outcome variable (i.e., self-rated health) after having controlled for the variance explained by the previous block of variables [44]. PROCESS v3.2 for SPSS [45] was used to test moderation by (a) estimating the interaction term between focal predictors (e.g., acculturative stress) and the moderating variable (e.g., community of settlement), and (b) estimating the conditional effects on self-rated health. The moderation analyses controlled for all the variables included in the HMR model.
Results
Frequencies, proportions, means, and standard deviations for all study variables are presented by community of settlement in Table 1. Bivariate correlations for all study variables are presented in Table 2.
Table 1.
Descriptive statistics for study variables (n = 200)
| Variable | Maricopa County 99 (49.5) | Miami-Dade County 101 (50.5) | |
|---|---|---|---|
| n (%) | n (%) | χ2 | |
| Gender | 0.50 | ||
| Women | 53 (53.5) | 49 (48.5) | |
| Men | 46 (46.5) | 52 (51.5) | |
| Partner Status | 1.05 | ||
| Single | 67 (67.7) | 75 (74.3) | |
| Has Partner | 32 (32.3) | 26 (25.7) | |
| Nativity | 23.48** | ||
| Immigrant | 14 (14.1) | 46 (45.5) | |
| U.S.-Born | 85 (85.9) | 55 (54.5) | |
| Hispanic Heritage | 146.21** | ||
| Mexican | 86 (86.9) | 2 (2.0) | |
| Other Hispanic Heritage | 13 (13.1) | 99 (98.0) | |
| Student Status | 0.06 | ||
| Current College Student | 68 (68.7) | 71 (70.3) | |
| Non-College Student | 31 (31.3) | 30 (29.7) | |
| Employment Status | 31.43** | ||
| Employed | 94 (94.9) | 63 (62.4) | |
| Unemployed | 5 (5.1) | 38 (37.6) |
| M (SD) | M (SD) | t value | α | |
|---|---|---|---|---|
| Age | 21.67 (1.91) | 20.94 (2.20) | − 2.49** | |
| Financial strain | 2.34 (.61) | 2.26 (.58) | − 1.03 | |
| Tangible social support | 3.72 (1.09) | 4.21 (.91) | 3.51*** | 0.91 |
| Emotional social support | 4.08 (.84) | 4.13 (.97) | .40 | 0.89 |
| Pressure to acculturate | 2.27 (1.29) | 1.71 (1.29) | − 3.08** | 0.91 |
| Pressure against acculturation | 1.51 (1.22) | 1.10 (1.18) | − 2.40** | 0.86 |
| Self-rated health | 3.31 (1.00) | 3.84 (.94) | 3.87*** |
p ≤ .05,
p ≤ .01,
p ≤ .001, α = Cronbach’s alpha reliability coefficient
Table 2.
Bivariate correlations for study variables (n = 200)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | – | |||||||||||||
| 2. Gender | − 0.05 | – | ||||||||||||
| 3. Community of Settlement | 0.17* | 0.05 | – | |||||||||||
| 4. Partner Status | 0.24** | 0.01 | 0.07 | – | ||||||||||
| 5. Nativity | 0.08 | 0.14* | 0.34** | − 0.01 | – | |||||||||
| 6. Hispanic Heritage | 0.23** | 0.02 | 0.86** | 0.06 | 0.32** | – | ||||||||
| 7. Student Status | 0.30** | − 0.01 | 0.02 | 0.01 | − 0.11 | 0.01 | – | |||||||
| 8. Employment Status | 0.27** | 0.05 | 0.40** | 0.09 | 0.16* | 0.37** | 0.24** | – | ||||||
| 9. Financial Strain | − 0.02 | 0.10 | 0.07 | 0.03 | 0.02 | 0.06 | − 19** | 0.02 | – | |||||
| 10. Tangible Support | − 0.06 | − 0.01 | − 0.24** | − 0.01 | − 0.14* | − 0.18** | 0.04 | − 0.08 | − 0.08 | – | ||||
| 11. Emotional Support | − 0.01 | 0.16* | − 0.03 | 0.08 | − 0.12 | 0.05 | 0.08 | 0.09 | − 0.10 | 0.61** | – | |||
| 12. Pressure to Acculturate | − 0.11 | 0.17* | 0.21** | − 0.02 | 0.12 | 0.19** | − 0.21** | − 0.01 | 0.09 | − 0.03 | 0.05 | – | ||
| 13. Pressure against Acculturation | − 0.06 | − 0.07 | 0.17* | − 0.04 | 0.11 | 0.15* | − 0.12 | 0.01 | 0.08 | − 0.09 | − 0.04 | 0.61** | – | |
| 14. Self-rated Health | 0.08 | −0.09 | − 0.27** | 0.04 | − 0.17* | − 0.21** | 0.14 | − 0.01 | − 0.25** | 0.10 | 0.16* | − 0.29** | − 0.19** | – |
p ≤ .05,
p ≤ .01
Table 3 presents all regression coefficients from the HMR model. Results indicate that 21.8% of the variance in self-rated health was explained by all predictor variables entered in the HMR model. The first predictor block included demographic variables and explained 16.0% of the variance in self-rated health, R2 = 0.160, F (9, 190) =4.01, p < 0.001. The second block added components of social support, which explained 2.0% of the variance in self-rated health, ΔR2 = 0.020, F (2, 188) = 2.42, p > 0.05. The third and final block added components of acculturative stress, which explained 3.8% of the variance in self-rated health, ΔR2 = 0.038, F (1, 186) = 4.50, p = 0.01.
Table 3.
Hierarchical multiple regression model with self-rated health as the outcome (n = 200)
| Variable | Model 1 |
Model 2 |
Model 3 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| b | SE | β | b | SE | β | b | SE | β | |
| Block 1 | |||||||||
| Age | 0.04 | 0.04 | 0.08 | 0.04 | 0.04 | 0.09 | 0.04 | 0.04 | 0.07 |
| Gender | − 0.09 | 0.14 | − 0.05 | − 0.16 | 0.14 | − 0.08 | − 0.10 | 0.14 | − 0.05 |
| Community of settlement | − 0.59 | 0.26 | − 0.30* | − 0.55 | 0.27 | − 0.27* | − 0.47 | 0.26 | − 0.24 |
| Partner status | 0.08 | 0.15 | 0.04 | 0.04 | 0.15 | 0.02 | 0.04 | 0.15 | 0.02 |
| Nativity | − 0.17 | 0.16 | − 0.08 | − 0.12 | 0.16 | − 0.06 | − 0.12 | 0.16 | − 0.05 |
| Hispanic heritage | 0.05 | 0.26 | 0.03 | − 0.04 | 0.26 | − 0.02 | − 0.02 | 0.26 | − 0.01 |
| Student status | 0.10 | 0.16 | 0.05 | 0.09 | 0.16 | 0.04 | 0.02 | 0.16 | 0.01 |
| Employment status | 0.22 | 0.19 | 0.09 | 0.17 | 0.19 | 0.07 | 0.15 | 0.18 | 0.06 |
| Financial strain | − 0.37 | 0.12 | − 0.22** | − 0.34 | 0.12 | − 0.20** | − 0.33 | 0.11 | − 0.20** |
| Block 2 | |||||||||
| Tangible social support | − 0.10 | 0.09 | − 0.10 | − 0.10 | 0.08 | − 0.10 | |||
| Emotional social support | 0.21 | 0.10 | 0.19* | 0.22 | 0.10 | 0.20* | |||
| Block 3 | |||||||||
| Pressure to acculturate | − 0.16 | 0.07 | − 0.21* | ||||||
| Pressure against acculturation | 0.01 | 0.07 | 0.01 | ||||||
R2 = 16.0% for Block 1, ΔR2 change = 2.0% for Block 2, ΔR2 change = 3.8% for Block 3
b unstandardized coefficient, SE standard error, β standardized coefficient
p ≤ 0.05,
p ≤ 0.01,
≤ 0.001
Moderation Analyses
Moderation analyses, corresponding with hypothesis two, indicated that the community of settlement had a statistically significant interaction with pressure to acculturate in relation to self-rated health (β =− 0.40, p = 0.004). Conditional effects across participants show that higher levels of pressure to acculturate were associated with lower self-rated health among participants in Maricopa County (β = − 0.42, p ≤ 0.001), but not Miami-Dade County (β = − 0.02, p > 0.05). This moderating effect is demonstrated in Fig. 1. Community of settlement also had a statistically significant interaction with pressure against acculturation in relation to self-rated health (β = − 0.38, p = 0.004). However, the conditional effects between participants in Maricopa County (β = − 0.18, p > 0.05) and Miami-Dade County (β = 0.20, p > 0.05) were not statistically significant.
Fig. 1.
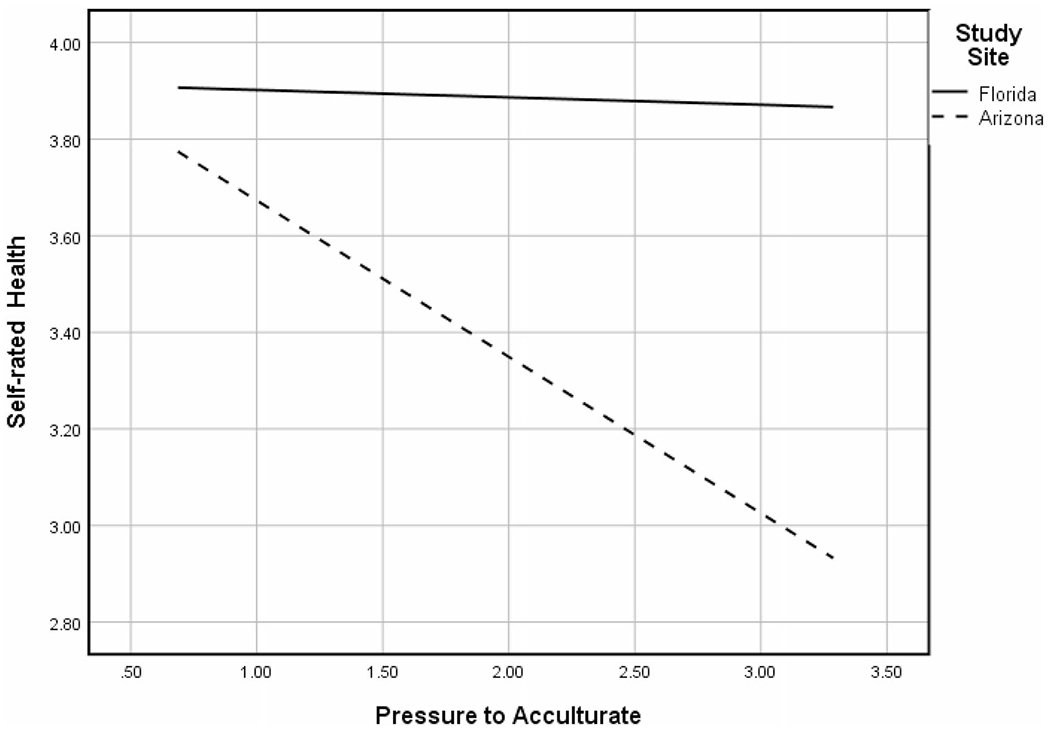
Two-way interaction with community of settlement moderating the association between pressure to acculturate and self-rated health
Moderation analyses, corresponding with hypothesis three, indicated that emotional social support did not moderate respective associations between pressure to acculturate (β = 0.07, p > 0.05) or pressure against acculturation (β = − 0.01, p > 0.05) in relation to self-rated health. Similarly, tangible social support did not moderate respective associations between pressure to acculturate (β = 0.10, p > 0.05) or pressure against acculturation (β = 0.10, p > 0.05) in relation to self-rated health.
Lastly, three-way interactions were tested between respective components of acculturative stress, social support, and community of settlement. Results indicate there was a statistically significant three-way interaction between pressure to acculturate, the community of settlement, and emotional social support in relation to self-rated health (β = 0.29, p = 0.03) (Fig. 2). Conditional effects among participants in Maricopa County indicate that pressure to acculturate had the strongest association with self-rated health at low levels (1 SD below the mean) of emotional social support (β = − 0.68, p < 0.001), followed by the mean level of emotional social support (β = − 0.43, p < 0.001). The conditional effect between pressure to acculturate and self-rated health at high levels (1 SD above the mean) of emotional social support was not statistically significant (β = − 0.19, p > 0.05). None of the conditional effects between pressure to acculturate and self-rated health were statistically significant among participants in Miami-Dade County. All three-way interactions between respective components of acculturative stress, social support, and the community of settlement were not statistically significant.
Fig. 2.
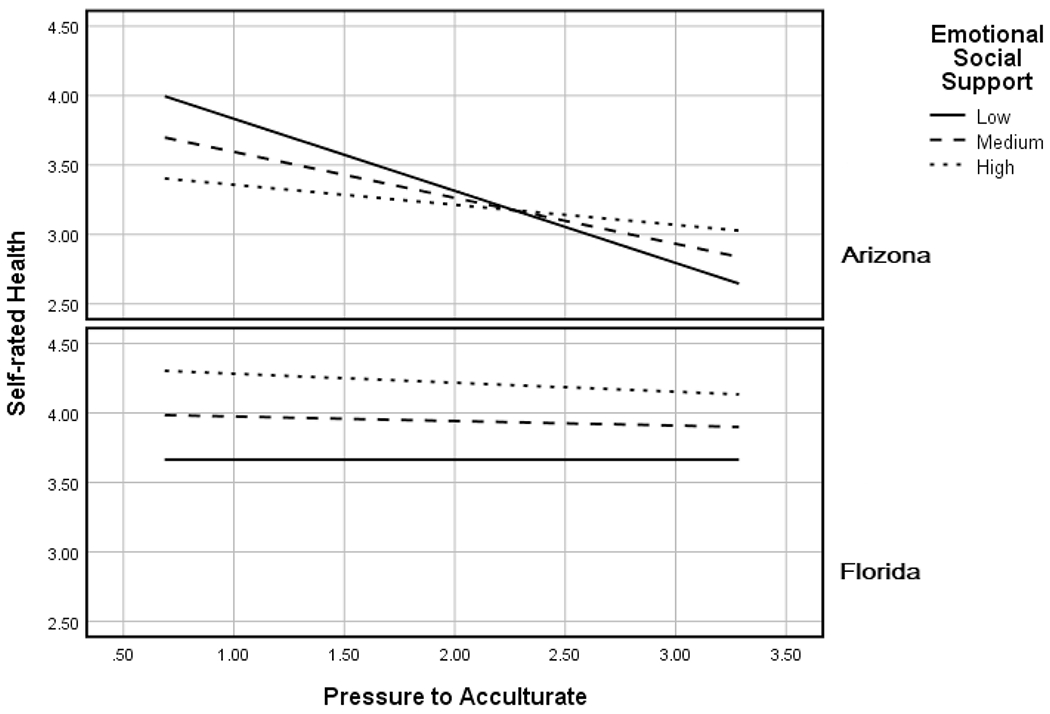
Three-way interaction with community of settlement and emotional social support moderating the association between pressure to acculturate and self-rated health
Discussion
The current study extends research on self-rated health among Hispanics by examining acculturative stress, community of settlement, and social support. Our first hypothesis was partially supported. Results indicated that higher levels of pressure to acculturate were associated with a lower level of self-rated health, but no significant association was found between pressure against acculturation and self-rated health. This finding suggests that the pressure to adopt mainstream U.S. customs may be stressful for some Hispanic emerging adults and may contribute to an individual’s health by impacting the physiological responses (e.g., elevated blood pressure, cortisol secretions) [46] whereas the pressure to maintain traditional Hispanic culture may not be deemed distressing in relation to self-rated health. Reducing acculturative stress may help avoid or delay the onset of poor health consequences, such as chronic diseases, later in life. However, longitudinal studies controlling for other factors are required to further understand this association.
Our data also partially supported our second hypothesis, which suggests that the community of settlement moderated associations between acculturative stress and self-rated health. We found that higher levels of pressure to acculturate were associated with a lower level of self-rated health among participants in Maricopa County, but not in Miami-Dade County. These findings could be explained in part because of the low ethnic density in Maricopa County compared to Miami-Dade county. As a minority population in Maricopa County, Hispanics may experience higher levels of cultural incongruence, which can result in poorer health-related outcomes. Empirical evidence suggests that pressure to acculturate may increase as a function of the social context of the community of settlement [47]. Alternatively, previous research has shown that community of settlement can be beneficial for people to mitigate not only stress but also to promote healthy behaviors. For example, researchers have found that living in a community with a high ethnic density of Hispanics protects Hispanic adolescents from engaging in substance use [48]. Further, research on ethnic density has found lower rates of cancer and cardiovascular disease among Hispanics living in more ethnically dense communities [49].
We did not find a statistically significant direct association between tangible social support and self-rated health. Nonetheless, we found that higher emotional social support was positively associated with self-rated health. It is possible that the non-significant association between tangible social support and self-rated health is partly due to the age of our participants. Emerging adults are generally healthy and less likely to need or think about tangible support to promote better health, compared to older people. Among emerging adults, emotional social support may be more important and relevant to health [33]. Further research is needed to identify if the sources of social support (e.g., family vs. friends), and the quality of social support moderate the association between acculturative stress and self-rated health along with the types of social support.
The three-way interaction between pressure to acculturate, the community of settlement, and emotional social support with self-rated health was statistically significant only among the participants in Maricopa County. It is possible that in communities that are not as ethnically dense, emotional social support plays a larger role in self-rated health compared to areas that are more ethnically dense. As such, low levels of emotional social support might pose unique challenges and opportunities for improving the self-rated health of the Hispanic population within Maricopa County. However, in Miami-Dade County, emotional social support might not have much influence on pressure to acculturate, given that the community of settlement is predominantly Hispanic and immigrants. Arguably, Hispanics in Miami-Dade County can live and function within their society without feeling much pressure to acculturate compared to Hispanics in Maricopa County. Our study did not find any significant associations between pressure against acculturation, the community of settlement, and components of social support with self-rated health.
A possible explanation could be attributed to differences in population demographics of the two counties, the current political landscape, local policies, and variation to accessibility to resources [47, 50], which could account for the differences observed. This could alleviate the pressure to acculturate for Hispanics within Miami-Dade County. On the other hand, Hispanics in Maricopa County might need higher levels of emotional social support to compensate for the sociopolitical context.
Considering the observational nature of our study it is premature to implement intervention strategies to target the adverse association between acculturative stress and self-rated health. However, if future studies replicate our findings healthcare providers in facilities that serve a high proportion of Hispanic patients may consider using brief screening measures for acculturative stress [51]. If an individual reports difficulties with acculturative stress additional assessments such as the Coping with Acculturative Stress Scale can be used to better determine what coping resources may be most beneficial for that person [52]. Lastly, consistent with the Stress Buffering Model and our findings [30], enhancing an individual’s level of emotional support may help weaken the adverse association between acculturative stress and self-rated health.
The contributions of this study to the literature should be interpreted with its limitations. First, measures used in this study were self-reported which might introduce error and social desirability bias. Second, due to the cross-sectional study design, causal relationships or temporality could not be established. Third, the generalizability of study findings is restricted due to our sample size and non-probability sampling. The study population is Hispanic yet, the survey was conducted in English, which might compromise the generalizability. Furthermore, Hispanics may experience acculturative stress differently based on demographic factors such as Hispanic heritage group and/or generation status [53]. However, our sample is not large enough to detect sub-group variations.
Conclusions
To our knowledge, this is the first study that empirically establishes evidence describing the association between acculturative stress and self-rated health among Hispanic emerging adults or in any age group. Our study highlights the importance of accounting for the role of social context (e.g., community of settlement) when examining associations of acculturative stress with health-related outcomes. In addition, our findings suggest that some forms of social support may mitigate the adverse association between acculturative stress and self-rated health. This is a finding that may have implications for health interventions targeting acculturative stress. Our data indicate the social context also plays a role in who may benefit most from coping resources such as emotional social support.
Acknowledgements
Preparation of this article was supported by the National Institute on Alcohol Abuse and Alcoholism [K01 AA025992]. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health. The authors would like to acknowledge Carlos Estrada and Irma Beatriz Vega de Luna for their work in recruiting participants.
Footnotes
Conflict of interest All authors declare that they have no conflicts of interest and do not have any financial disclosures to report.
References
- 1.Benyamini Y Why does self-rated health predict mortality? An update on current knowledge and a research agenda for psychologists. New York: Taylor & Francis; 2011. [DOI] [PubMed] [Google Scholar]
- 2.Bombak AE. Self-rated health and public health: a critical perspective. Front Public Health. 2013;1:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finch BK, et al. Validity of self-rated health among Latino (a) s. Am J Epidemiol. 2002;155(8):755–9. [DOI] [PubMed] [Google Scholar]
- 4.Oh SH, Kim JS. Importance of lifestyle, stress, and chronic diseases in self-rated health of Korean doctors. J Korean Med Assoc. 2020;63(9):566. [Google Scholar]
- 5.Sokol R, et al. Variability in self-rated health trajectories from adolescence to young adulthood by demographic factors. Prev Med. 2017;105:73–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arnett JJ, Žukauskienė R, Sugimura K. The new life stage of emerging adulthood at ages 18–29 years: Implications for mental health. The Lancet Psychiatry. 2014;1(7):569–76. [DOI] [PubMed] [Google Scholar]
- 7.Patton GC, et al. Our future: a Lancet commission on adolescent health and wellbeing. The Lancet. 2016;387(10036):2423–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cano MÁ, et al. Exposure to ethnic discrimination in social media and symptoms of anxiety and depression among Hispanic emerging adults: examining the moderating role of gender. J Clin Psychol. 2020;77:571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rahman A, et al. Ethnic discrimination and psychological stress among Hispanic emerging adults: Examining the moderating effects of distress tolerance and optimism. Int J Intercult Relat. 2022;86:217–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crockett LJ, et al. Acculturative stress, social support, and coping: relations to psychological adjustment among Mexican American college students. Cultur Divers Ethnic Minor Psychol. 2007;13(4):347. [DOI] [PubMed] [Google Scholar]
- 11.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310. [PubMed] [Google Scholar]
- 12.Bekteshi V, Van Hook M. Contextual approach to acculturative stress among Latina immigrants in the US. J Immigr Minor Health. 2015;17:1401–11. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez N, et al. Validation of the multidimensional acculturative stress inventory on adolescents of Mexican origin. Psychol Assess. 2015;27(4):1438. [DOI] [PubMed] [Google Scholar]
- 14.Rodriguez N, et al. Development of the multidimensional acculturative stress inventory for adults of Mexican origin. Psychol Assess. 2002;14(4):451. [PubMed] [Google Scholar]
- 15.Torres L, Driscoll MW, Voell M. Discrimination, acculturation, acculturative stress, and Latino psychological distress: a moderated mediational model. Cultur Divers Ethnic Minor Psychol. 2012;18(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. J Health Soc Behav. 2000;41:295–313. [PubMed] [Google Scholar]
- 17.D’Anna-Hernandez KL, Aleman B, Flores A-M. Acculturative stress negatively impacts maternal depressive symptoms in Mexican-American women during pregnancy. J Affect Disord. 2015;176:35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCord AL, Draucker CB, Bigatti S. Cultural stressors and depressive symptoms in Latino/a adolescents: an integrative review. J Am Psychiatr Nurses Assoc. 2019;25(1):49–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Castellanos R, Acculturative Stress and Depression among Latinos/As: Investigating the Role of Neighborhood Context. 2017. [Google Scholar]
- 20.Driscoll MW, Torres L. Acculturative stress and Latino depression: the mediating role of behavioral and cognitive resources. Cultur Divers Ethnic Minor Psychol. 2013;19(4):373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Finch BK, Vega WA. Acculturation stress, social support, and self-rated health among Latinos in California. J Immigr Health. 2003;5(3):109–17. [DOI] [PubMed] [Google Scholar]
- 22.Panchang S, et al. Self-rated health, gender, and acculturative stress among immigrants in the US: New roles for social support. Int J Intercult Relat. 2016;55:120–32. [Google Scholar]
- 23.Berry JW, Sam DL. The Cambridge handbook of acculturation psychology. Cambridge: Cambridge University Press; 2006. [Google Scholar]
- 24.Potochnick S, Perreira KM, Fuligni A. Fitting in: the roles of social acceptance and discrimination in shaping the daily psychological well-being of Latino youth. Soc Sci Q. 2012;93(1):173–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.U.S. Census Bureau. American Community Survey 1-year estimates, Maricopa County. 2019. [cited 2022; Available from: https://censusreporter.org/profiles/05000US04013-maricopa-county-az/.
- 26.U.S. Census Bureau. American Community Survey 1-year estimates, Miami-Dade County. 2019; Available from: https://censusreporter.org/profiles/05000US12086-miami-dade-county-fl/.
- 27.National Tour Association. Miami—the gateway to the Americas. 2004; Available from: https://ntaonline.com/miami-the-gateway-to-the-americas/.
- 28.Cano MÁ, et al. Depressive symptoms and externalizing behaviors among Hispanic immigrant adolescents: examining longitudinal effects of cultural stress. J Adolesc. 2015;42:31–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lawton KE, Gerdes AC. Acculturation and Latino adolescent mental health: integration of individual, environmental, and family influences. Clinical Child Family Psychol Rev. 2014;17(4):385–98. [DOI] [PubMed] [Google Scholar]
- 30.Cohen S Social relationships and health. Am Psychol. 2004;59(8):676. [DOI] [PubMed] [Google Scholar]
- 31.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–14. [DOI] [PubMed] [Google Scholar]
- 32.Gorman BK, Sivaganesan A. The role of social support and integration for understanding socioeconomic disparities in self-rated health and hypertension. Soc Sci Med. 2007;65(5):958–75. [DOI] [PubMed] [Google Scholar]
- 33.Cano MÁ, et al. Depressive symptoms and resilience among Hispanic emerging adults: examining the moderating effects of mindfulness, distress tolerance, emotion regulation, family cohesion, and social support. Behav Med. 2020;46(3–4):245–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barrera M, Garrison-Jones C. Family and peer social support as specific correlates of adolescent depressive symptoms. J Abnorm Child Psychol. 1992;20(1):1–16. [DOI] [PubMed] [Google Scholar]
- 35.Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull. 1996;119(3):488. [DOI] [PubMed] [Google Scholar]
- 36.Cano MÁ, et al. Alcohol use severity among Hispanic emerging adults: examining the roles of bicultural self-efficacy and acculturation. Addict Behav. 2020;108:106442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Angel RJ, et al. Financial strain and health among elderly Mexican-origin individuals. J Health Soc Behav. 2003;44:536–51. [PubMed] [Google Scholar]
- 38.Dominguez K, et al. Vital signs: leading causes of death, prevalence of diseases and risk factors, and use of health services among Hispanics in the United States—2009–2013. MMWR Morb Mortal Wkly Rep. 2015;64(17):469. [PMC free article] [PubMed] [Google Scholar]
- 39.Savoy EJ, et al. Financial strain and self-rated health among black adults. Am J Health Behav. 2014;38(3):340–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ware JE Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. [DOI] [PubMed] [Google Scholar]
- 41.Krieger N, et al. Racial discrimination, psychological distress, and self-rated health among US-born and foreign-born Black Americans. Am J Public Health. 2011;101(9):1704–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Subramanian SV, Huijts T, Avendano M. Self-reported health assessments in the 2002 World Health Survey: how do they correlate with education? Bull World Health Organ. 2010;88:131–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moser A, et al. The eight-item modified medical outcomes study social support survey: psychometric evaluation showed excellent performance. J Clin Epidemiol. 2012;65(10):1107–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. London: Psychology press; 2014. [Google Scholar]
- 45.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: Guilford publications; 2017. [Google Scholar]
- 46.Morris MC, et al. Cortisol reactivity to experimentally manipulated psychosocial stress in young adults at varied risk for depression. Depress Anxiety. 2014;31(1):44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Berry JW, Annis RC. Acculturative stress: the role of ecology, culture and differentiation. J Cross Cult Psychol. 1974;5(4):382–406. [Google Scholar]
- 48.Kulis S, et al. Neighborhood effects on youth substance use in a southwestern city. Sociol Perspect. 2007;50(2):273–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alvarez KJ, Levy BR. Health advantages of ethnic density for African American and Mexican American elderly individuals. Am J Public Health. 2012;102(12):2240–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stepick A, Dutton Stepick C, Vanderkooy P. Becoming American. In: Schwartz SJ, Luyckx K, Vignoles VL, editors. Handbook of identity theory and research. New York: Springer;2011. p. 867–93. [Google Scholar]
- 51.Torres CA, Crowther MR, Brodsky S. Addressing acculturative stress in psychotherapy: a case study of a Latino man overcoming cultural conflicts and stress related to language use. Clin Case Stud. 2017;16(3):187–99. [Google Scholar]
- 52.Castro-Olivo SM, et al. Development and validation of the Coping With Acculturative Stress in American Schools (CASAS-A) Scale on a Latino adolescent sample. Assess Eff Interv. 2014;40(1):3–15. [Google Scholar]
- 53.Cano M, et al. Experiences of ethnic discrimination among US Hispanics: Intersections of language, heritage, and discrimination setting. Int J Intercult Relat. 2021;84:233–50. [DOI] [PMC free article] [PubMed] [Google Scholar]


