Abstract
Aim:
Young adults (ages 18–35) are underrepresented in lifestyle interventions for people with serious mental illness (SMI), such as schizophrenia, bipolar disorder, and severe depression, and little is known about factors influencing their engagement in these programs. This qualitative study examined factors affecting engagement among young adults with SMI who were enrolled in a lifestyle intervention trial at community mental health centers.
Methods:
Seventeen young adults with SMI participated in this qualitative study. Participants were drawn from a 12-month randomized controlled trial (n=150) comparing an in-person group lifestyle intervention augmented with mobile health technology (PeerFIT) to one-on-one personalized remote health coaching (BEAT) using purposive sampling. The 17 participants completed semi-structured qualitative interviews at post-intervention to explore their perceived benefits of the intervention and factors impacting engagement. We used a team-based descriptive qualitative approach to code transcripts and identify themes in the data.
Results:
Participants across both interventions reported experiencing improved ability to engage in health behavior change. Participants described managing psychosocial stressors and family and other responsibilities that limited their ability to attend in-person PeerFIT sessions. The remote and flexible BEAT remote health coaching intervention appeared to facilitate engagement even in the context of challenging life circumstances.
Conclusions:
Remotely delivered lifestyle interventions can facilitate engagement among young adults with SMI navigating social stressors.
Keywords: Digital health, exercise, nutrition, schizophrenia, bipolar disorder, depression
Introduction
People with serious mental illness (SMI), including schizophrenia, bipolar disorder, and major depression, have a cardiovascular mortality rate more than twice that of the overall population (Correll et al., 2017; Olfson et al., 2015; Saha et al., 2007). Increased prevalence of cardiovascular risk factors and behaviors, including diabetes, hypertension, obesity, smoking, sedentary behavior, and poor diet are present early in the course of mental illness (Correll et al., 2014; Correll et al., 2010; McCloughen et al., 2016). Although behavioral lifestyle interventions adapted for persons with SMI have shown efficacy in randomized controlled trials (Bartels et al., 2013; Bartels et al., 2015; Cabassa et al., 2021; Daumit et al., 2013), young adults ages 18 to 35 with SMI have been underrepresented in these studies (Naslund et al., 2017). Furthermore, while prior studies have explored correlates of lifestyle intervention engagement among middle-aged adults with SMI (Tuda et al., 2022), little is known about the factors that influence engagement in lifestyle interventions among young adults with SMI. Given the increased risk for obesity in young adulthood and decline in health-promoting behaviors (Kwan et al., 2012; Laska et al., 2012; Nelson et al., 2008), identifying effective strategies for engaging this group in lifestyle interventions is critical to prevent chronic and disabling physical disease.
Engaging young adults in behavioral interventions that promote weight loss in the overall population has been a challenge (Brokaw et al., 2015; LaRose et al., 2016). Data pooled from three behavioral weight loss trials for overweight and obese adults showed that young adults aged 18–35 years represented 7% of the sample, attended significantly fewer sessions than middle-aged adults and were less likely to be retained for study assessments (Gokee-LaRose et al., 2009). Multiple factors contribute to a young person’s willingness to engage in structured behavioral programs that promote weight loss and physical activity, including time and costs of programs and conflicts with work and school responsibilities (Lanoye et al., 2016; LaRose et al., 2016). Mental health symptoms, substance use, social isolation and lack of family involvement are predictors of disengagement from mental health services among persons with SMI (Dixon et al., 2016; Kreyenbuhl et al., 2009), which may create additional barriers to participating in lifestyle programs for young adults.
Much of what is known about motivation to adopt healthy eating and physical activity behaviors among young people has been discovered through research in the overall population. The motivating factors for weight loss and physical activity among young adults identified in the literature include physical appearance, peer influences, and social inclusion and connection (Ashton et al., 2015; Larose et al., 2013). Based on these preferences and the unique challenges of living with SMI, our team developed and evaluated PeerFIT, an in-person group lifestyle intervention (including exercise and lifestyle education sessions) augmented with mobile health (mHealth) technology (Aschbrenner et al., 2018). We evaluated PeerFIT against Basic Education and Activity Tracking (BEAT), a one-on-one personalized remote health coaching intervention, in the Fit Forward Trial, a 12-month randomized controlled trial (RCT) of 150 young adults with SMI. Primary findings (Aschbrenner et al., 2021) did not indicate superiority of one intervention over the other and participants in both conditions experienced significant improvements in cardiovascular disease risk reduction (i.e., clinically significant weight loss of 5% from baseline or clinically significant improvements in fitness, reflected as an increase of >50 meters on the six minute walk test from baseline). Yet, intervention attendance was significantly higher in BEAT (70%) compared to PeerFIT (22% for exercise sessions; 26% for lifestyle sessions). Therefore, exploring the factors that contributed to these disparate attendance rates could inform future tailoring and delivery of lifestyle interventions for young adults with SMI. The purpose of this qualitative study was to identify factors impacting lifestyle intervention engagement from the perspective of young adults with SMI enrolled in the Fit Forward trial.
Methods
Study Overview
The protocol for the Fit Forward Trial has been published (Aschbrenner et al., 2018) and the trial was registered on clinicaltrials.gov (NCT02815813). Briefly, the study was a two-arm RCT conducted in four community mental health centers located in the northeastern U.S. The study evaluated the effectiveness of PeerFIT compared to BEAT on cardiovascular risk reduction. All participants gave written informed consent after receiving a complete description of the study, and institutional review boards at Dartmouth College, the Massachusetts Department of Mental Health, and the State of New Hampshire Department of Health and Human Services approved the study.
Participants
Participants in the Fit Forward Trial were young adults aged 18 to 35 with a chart verified diagnosis of SMI receiving services at community mental health centers and who were overweight or obese defined as having a body mass index of ≥25 kg/m2. Participants obtained medical clearance from their primary care provider to participate in the study prior to randomization (See Aschbrenner et al., 2021 for exclusion criteria).
Interventions
Mental health or fitness professionals with a minimum of a bachelor’s degree served as lifestyle coaches for both PeerFIT and BEAT interventions. They received training and supervision from members of the research team. Both interventions were delivered in two phases over 12 months: 1) intensive phase (Months 1–6); and 2) maintenance phase (Months 7–12).
PeerFIT.
PeerFIT was a 12-month in-person group lifestyle intervention with mHealth adapted from the Diabetes Prevention Program (Diabetes Prevention Program Research Group, 2012). Lifestyle coaches provided intensive, ongoing contact with participants to help them achieve and maintain their weight loss and physical activity goals. PeerFIT’s intensive phase consisted of twice weekly in-person group sessions: 24 group lifestyle sessions and 24 exercise group sessions. PeerFIT participants also received Fitbit devices, access to a private Facebook group, a digital scale, and 2–3 weekly text messages from the lifestyle coach. These digital components promoted peer-to-peer support for health behavior change and encouraged self-monitoring of physical activity and body weight. The intensive phase was followed by a six-month maintenance phase during which lifestyle sessions were discontinued (all other components remained accessible).
BEAT.
BEAT was a 12-month one-on-one personalized remote coaching intervention that included once monthly telephone coaching calls, 2–3 weekly text messages from the coach with reminders and encouragement, and wearable activity devices (i.e., Fitbits) to promote self-monitoring of physical activity. During the intensive phase, coaches delivered six monthly 30-minute telephone coaching calls as well as weekly text messages. Lifestyle coaching calls were discontinued during the maintenance phase with all other components still accessible.
Qualitative Interviews
Sampling Approach.
As participants completed their 12-month outcome assessment and completed the study, our team used purposive sampling to invite 10 participants categorized as high and low intervention engagers stratified by intervention type (Palinkas et al., 2015). For the PeerFIT intervention, high engagers were defined as participants who attended 50% or more of the weekly lifestyle and exercise sessions offered during the 6-month intensive phase of the study, whereas low engagers were defined as participants who attended less than 50% of the weekly lifestyle and exercise sessions offered during the same period. For the comparison condition (BEAT), high engagers were defined as those participants who attended 50% or more of the monthly telephone coaching calls offered during the 6-month intensive phase of the study, whereas low engagers were defined as those who attended less than 50% of the monthly telephone coaching calls offered during the same period. These definitions for high vs. low engagers were selected given that a range of prior lifestyle intervention studies have observed significant positive relationships between participant engagement (e.g., attending classes or intervention sessions) and achieving health behavior changes, including in lifestyle intervention studies among adults with SMI (Green et al., 2015; Porter et al., 2020; Thomson et al., 2015). Research staff invited 10 participants in each category (i.e., high vs. low engager) across intervention type using a list generated by the data manager to participate in a 30-minute telephone based qualitative interview to learn about their experiences with the intervention. Seventeen participants agreed to participate in the qualitative interviews of which 10 were from PeerFIT (6 high engagers, 4 low engagers) and seven were from BEAT (6 high engagers, 1 low engager). Participants received $50 for participating in the telephone interviews, which were audio recorded for transcription with their permission.
Interview Guide.
The semi-structured interviews explored participants’ experience with the interventions centered around the domains of feasibility, acceptability, and perceived benefits. Questions included on the interview guide covered participants’ enjoyment (“What did you like the most/least about the intervention?), ease of use (“Tell me about the parts of the program that were easiest/most difficult to use”), helpfulness (“What parts of the program were the most helpful?”), and views of intervention components (e.g., “What did you think about the number of sessions?”).
Data Analysis
Qualitative interview transcripts were analyzed using a team-based descriptive approach (Colorafi & Evans, 2016). Three members of the study team independently read and coded all transcripts. The researchers applied descriptive codes from a preliminary codebook developed by the principal investigator and added new codes as they were identified in the data (Miles et al., 2013). The team met after coding sets of three transcripts to compare consistency of code application. Any discrepancies in coding were discussed at team meetings until consensus was reached. When all transcripts were coded, the team evaluated the usefulness of the codes and refined the code list by eliminating codes and adding new codes identified and agreed upon by the team. The team arrived at a final set of codes organized into themes corresponding to three domains for each intervention: (1) barriers to intervention engagement, (2) facilitators of engagement, and (3) perceived benefits of the intervention.
Results
Participants
Participants in the qualitative interviews were, on average, 29 years old, primarily female (82%), White (77%), and unmarried (82%) with a high school education or higher (77%). Just under half (47%) of the sample identified as Hispanic and just over half (52%) were living independently. Most participants (88%) were not working and had at least weekly in-person contact with their parents. Participants had psychiatric diagnoses of schizophrenia-spectrum disorders (41%), mood disorders (41%), or posttraumatic stress disorder (18%) and the majority (77%) were taking antipsychotic medications. These characteristics are generally consistent with the larger sample from the parent RCT (Aschbrenner et al., 2021) except for gender, race, and ethnicity in which this sample had a higher proportion of female, White, and Hispanic participants.
Barriers to Engagement
PeerFIT.
Participants expressed that it was difficult to attend scheduled in-person exercise and lifestyle sessions due to competing demands and responsibilities (e.g., childcare, appointments, work). Psychosocial stressors related to housing and finances were described as barriers to engagement. One participant shared the impact of life circumstances on their ability to attend PeerFIT sessions:
“Then like I missed some groups because I was living in a place that was transitional living for families. Kicking us out with no notice.” – Participant 1
In addition to logistical and psychosocial challenges related to attending in-person groups, participants expressed difficulties with being able to fully engage in the exercise sessions due to physical limitations. One participant shared their struggles with the exercise sessions:
“The only thing that was difficult was for me to do certain exercises. It was-- yoga was a little hard for me, and a couple of things was hard for me, the pushups and stuff.” – Participant 2
BEAT.
As engagement in BEAT was high and the intervention sample consisted of primarily high engagers, barriers to engagement were not consistently identified across interviews.
Facilitators of Engagement
PeerFIT.
Overall, participants found the communication and coaching style helpful for engaging in PeerFIT. Specifically, participants expressed that the coaches were encouraging, motivating, and supportive. Participants also shared that it was helpful to talk with coaches about challenges that arose during the course of the study that could impact engagement (e.g., new job that conflicted with groups, anxiety). Coaches were able to discuss strategies for overcoming these challenges to maximize engagement. Taken together, coaches’ ability to provide encouragement and support while acknowledging the overall context that the person is navigating (e.g., personal stressors) was important for facilitating engagement.
BEAT.
Participants found the flexibility of the BEAT intervention helpful for being able to engage in the intervention. One participant shared how they were able to engage despite having multiple additional responsibilities:
“Because I have so many appointments and so much daily stuff in life plus a son, I didn’t have time to go to groups and all that so doing it this way, it was so much easier where I knew I’d be able to participate and still text and do all that and talk to [my son] and then talk to you guys.” – Participant 3
Additionally, BEAT participants enjoyed communicating with the coach and found their coaching style supportive, non-judgmental, and motivating. These positive qualities promoted engagement in the intervention.
Perceived Benefits
PeerFIT.
Participants reported that the peer-to-peer support increased their self-confidence and was helpful in facilitating health behavior changes. One participant shared their perspective on how peer-to-peer support was beneficial:
“Like it’s not just get fit and get healthy. It’s socializing and getting to know people in the same boat and just very supportive and nonjudgmental type of environment. You’re getting more than just exercise and fitness out of it, you know?” – Participant 4
BEAT.
Participants found that they became more aware of their health behaviors through BEAT, particularly by using the Fitbit for tracking sleep, weight, and steps. Participants also shared that their engagement in BEAT and communication with the BEAT coaches helped them pay greater attention to their eating habits and exercise (Figure 1).
Figure 1.
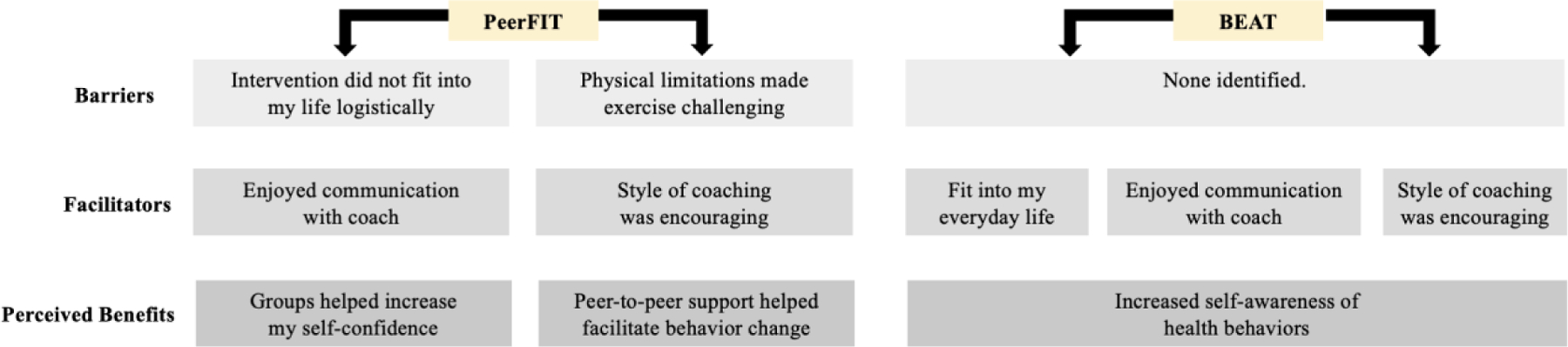
Themes corresponding to domains of barriers, facilitators, and perceived benefits by intervention type
Discussion
This qualitative study examined factors influencing engagement in lifestyle interventions for young adults with SMI in the context of an RCT that evaluated PeerFIT, an in-person group program with mHealth compared to BEAT, a one-on-one personalized remote health coaching program. We explored themes corresponding to the domains of barriers to engagement, facilitators of engagement, and perceived benefits of the programs within each intervention. Results highlighted perceived benefits of both PeerFIT and BEAT, particularly with regard to awareness and capacity to engage in health behavior change. The findings also showed that young adults with SMI face several personal and psychosocial challenges that interfere with intervention engagement but that these barriers may be overcome through supportive coaching, problem-solving, and flexible remote intervention delivery.
Consistent with the goals of the lifestyle interventions, participants in PeerFIT and BEAT perceived benefits to their awareness and ability to increase their physical activity and improve their nutrition. While both interventions involved coaching support that facilitated health behavior change, PeerFIT capitalized on peer-to-peer support in particular. PeerFIT participants found that peer-to-peer support from group sessions both led to improved self-confidence and was helpful for facilitating lifestyle changes. Group-based exercise interventions have been shown to be feasible and acceptable in young people with psychosis (Shannon et al., 2020). Further, these types of programs may be especially valuable given that individuals with SMI experience high levels of loneliness, and both loneliness and lack of support are barriers to health behavior intervention engagement (Firth et al., 2016; Fortuna et al., 2022; Roberts & Bailey, 2011). Thus, group-based designs and embedded peer-to-peer support appear to be critical ingredients for improving confidence and health behavior change in young adults with SMI.
Despite these perceived benefits, barriers to engagement were particularly salient for participants randomized to PeerFIT. Specifically, the reported challenges of attending in-person lifestyle and exercise sessions due to responsibilities and stressors (e.g., work, childcare, appointments, unstable housing) likely explain the low attendance rates observed in the parent RCT (Aschbrenner et al., 2021). Much of the existing research on barriers to engagement in exercise and lifestyle programs in the SMI population has focused on psychological reasons (e.g., low mood, mental health symptoms, stress) for low adherence (Firth et al., 2016; Roberts & Bailey, 2011). Our findings highlighted how social determinants of health (SDOH) impact engagement in lifestyle interventions for young adults with SMI, particularly for the in-person PeerFIT program. Evidence has shown that SDOH, such as financial and housing instability and low access to resources, disproportionately affect individuals with SMI and negatively impact mental health (Alegría et al., 2018; Compton & Shim, 2015). It may be that young adults with SMI have difficulty engaging in lifestyle interventions due to synergistic effects of psychological stressors and SDOH. As such, consideration of the array of challenges affecting young adults with SMI should be considered when designing lifestyle interventions for this group.
The combination of flexibility and supportive, one-on-one, remote coaching provided in BEAT appeared to promote engagement even among participants navigating social stressors. Future iterations of BEAT may specifically examine the role of SDOH in behavior change interventions to help participants manage these challenges while making positive changes to their health behavior. For example, BEAT coaches could be trained to connect participants with childcare and housing-related supports and resources while promoting increased physical activity. Further, it may be possible for BEAT coaches to promote improved nutrition while simultaneously assessing access to healthy food options and connecting participants to local, affordable resources. BEAT has the potential to serve as an effective lifestyle intervention for young adults with SMI that considers the context in which they live and addresses relevant SDOH for this population.
The study was limited in the small sample size of 17 participants. Further, although the recruitment of low engagers for this qualitative study was a strength, the sample primarily consisted of high engagers, particularly in BEAT. Thus, it is possible there were barriers to engagement with BEAT that were not captured through our interviews. Our study focused on factors affecting engagement from participant perspectives, thereby highlighting a need for future work to consider factors that affect maintenance of outcomes, as well as perspectives from multiple stakeholders on implementation outcomes of lifestyle interventions at the provider, community, and facility levels. The sample also was primarily female and White, which limits generalizability to participants of other genders and racial backgrounds. Despite these limitations, this study adds important insights on barriers and facilitators to engagement in lifestyle interventions for the young adult population with SMI.
Acknowledgments
This study was funded by the National Institute of Mental Health (R01 MH-110965) awarded to K. Aschbrenner. Dr. Browne is supported by a VA Rehabilitation Research and Development Career Development Award (IK1RX003904). Dr. Cabassa is supported by P50MH115843. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the United States Government or Department of Veterans Affairs.
Footnotes
Conflicts of Interest
All authors declare that they have no conflicts of interest.
Data Availability Statement
The data that support the findings of this study will be available upon request through the National Institute of Mental Health Data Archive (NDA; https://nda.nih.gov/) once the parent study is complete.
References
- Alegría M, NeMoyer A, Falgàs Bagué I, Wang Y, & Alvarez K (2018). Social determinants of mental health: where we are and where we need to go. Current Psychiatry Reports, 20(11), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aschbrenner KA, Naslund JA, Gorin AA, Mueser KT, Browne J, Wolfe RS, Xie H, & Bartels SJ (2021). Group lifestyle intervention with mobile health for young adults with serious mental illness: A randomized controlled trial. Psychiatric Services, appi.ps.2021000. 10.1176/appi.ps.202100047 [DOI] [PMC free article] [PubMed]
- Aschbrenner KA, Naslund JA, Gorin AA, Mueser KT, Scherer EA, Viron M, Kinney A, & Bartels SJ (2018). Peer support and mobile health technology targeting obesity-related cardiovascular risk in young adults with serious mental illness: Protocol for a randomized controlled trial. Contemporary Clinical Trials, 74, 97–106. 10.1016/j.cct.2018.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashton LM, Hutchesson MJ, Rollo ME, Morgan PJ, Thompson DI, & Collins CE (2015). Young adult males’ motivators and perceived barriers towards eating healthily and being active: A qualitative study. International Journal of Behavioral Nutrition and Physical Activity, 12(1), 1–10. 10.1186/s12966-015-0257-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels Pratt SI, Aschbrenner KA, Barre LK, Jue K, Wolfe RS, ... & Naslund JA, S. J. (2013). Clinically significant improved fitness and weight loss among overweight persons with serious mental illness. Psychiatric Services, 64(8), 729–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels SJ, Pratt SI, Aschbrenner KA, Barre LK, Naslund JA, Wolfe R, Xie H, McHugo GJ, Jimenez DE, Jue K, Feldman J, & Bird BL (2015). Pragmatic replication trial of health promotion coaching for obesity in serious mental illness and maintenance of outcomes. American Journal of Psychiatry, 172(4), 344–352. 10.1176/appi.ajp.2014.14030357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brokaw SM, Carpenedo D, Campbell P, Butcher MK, Furshong G, Helgerson SD, ..., & Workgroup, M. C. D. and D. P. (2015). Effectiveness of an adapted diabetes prevention program lifestyle intervention in older and younger adults. Journal of the American Geriatrics Society, 63(6), 1067–1074. [DOI] [PubMed] [Google Scholar]
- Cabassa LJ, Stefancic A, Lewis-Fernández R, Luchsinger J, Weinstein LC, Guo S, Palinkas L, Bochicchio L, Wang X, O’Hara K, Blady M, Simiriglia C, & McCurdy MM (2021). Main outcomes of a peer-led healthy lifestyle intervention for people with serious mental illness in supportive housing. Psychiatric Services, 72(5), 490–497. 10.1176/appi.ps.202000304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colorafi KJ, & Evans B (2016). Qualitative descriptive methods in health science research. Health Environments Research & Design Journal, 9(4), 16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, & Shim RS (2015). The social determinants of mental health. Focus, 13(4), 419–425. [Google Scholar]
- Correll CU, Robinson DG, Schooler NR, Brunette MF, Mueser KT, Rosenheck RA, ..., & Kane JM (2014). Cardiometabolic risk in patients with first-episode schizophrenia spectrum disorders baseline results from the RAISE-ETP study. JAMA Psychiatry, 71(12), 1350–1363. 10.1001/jamapsychiatry.2014.1314 [DOI] [PubMed] [Google Scholar]
- Correll Christoph U., Druss BG, Lombardo I, O’Gorman C, Harnett JP, Sanders KN, Alvir JM, & Cuffel BJ (2010). Findings of a U.S. national cardiometabolic screening program among 10,084 psychiatric outpatients. Psychiatric Services, 61(9), 892–898. 10.1176/ps.2010.61.9.892 [DOI] [PubMed] [Google Scholar]
- Correll Christoph U., Solmi M, Veronese N, Bortolato B, Rosson S, Santonastaso P, Thapa-Chhetri N, Fornaro M, Gallicchio D, Collantoni E, Pigato G, Favaro A, Monaco F, Kohler C, Vancampfort D, Ward PB, Gaughran F, Carvalho AF, & Stubbs B (2017). Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry, 16(2), 163–180. 10.1002/wps.20420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daumit Dickerson FB, Wang NY, Dalcin A, Jerome GJ, Anderson CA, ... & Oefinger M, G. L. (2013). A behavioral weight-loss intervention in persons with serious mental illness. New England Journal of Medicine, 368(17), 1594–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon LB, Holoshitz Y, & Nossel I (2016). Treatment engagement of individuals experiencing mental illness: review and update. World Psychiatry, 15(1), 13–20. 10.1002/wps.20306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, & Vancampfort D, J. (2016). Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis. Psychological Medicine, 46(14), 2869–2881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortuna KL, Ferron J, Bianco CL, Santos MM, Williams A, Williams M, Mois G, & Pratt SI (2022). Loneliness and its association with health behaviors in people with a lived experience of a serious mental illness. Psychiatric Quarterly, 92(1), 101–106. 10.1007/s11126-020-09777-8.Loneliness [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gokee-LaRose J, Gorin AA, Raynor HA, Laska MN, Jeffery RW, Levy RL, & Wing RR (2009). Are standard behavioral weight loss programs effective for young adults? Journal of Obesity, 33(12), 1374–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green CA, Yarborough BJH, Leo MC, Yarborough MT, Stumbo SP, Janoff SL, Perrin NA, Nichols GA, & Stevens VJ (2015). The STRIDE weight loss and lifestyle intervention for individuals taking antipsychotic medications: A randomized trial. American Journal of Psychiatry, 172(1), 71–81. 10.1176/appi.ajp.2014.14020173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group, D. P. P. (DPP) R. (2012). The Diabetes Prevention Program (DPP) description of lifestyle intervention. Diabetes Care, 25(12), 2165–2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreyenbuhl J, Nossel IR, & Dixon LB (2009). Disengagement from mental health treatment among individuals with schizophrenia and strategies for facilitating connections to care: A review of the literature. Schizophrenia Bulletin, 35(4), 696–703. 10.1093/schbul/sbp046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwan MY, Cairney J, Faulkner GE, & Pullenayegum EE (2012). Physical activity and other health-risk behaviors during the transition into early adulthood: A longitudinal cohort study. American Journal of Preventive Medicine, 42(1), 14–20. [DOI] [PubMed] [Google Scholar]
- Lanoye A, Gorin AA, & LaRose JG (2016). Young adults’ attitudes and perceptions of obesity and weight management: implications for treatment development. Current Obesity Reports, 5(1), 14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaRose JG, Guthrie KM, Lanoye A, Tate DF, Robichaud E, Caccavale LJ, & Wing RR (2016). A mixed methods approach to improving recruitment and engagement of emerging adults in behavioural weight loss programs. Obesity Science and Practice, 2(4), 341–354. 10.1002/osp4.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larose JG, Leahey TM, Hill JO, & Wing RR (2013). Differences in motivations and weight loss behaviors in young adults and older adults in the national weight control registry. Obesity, 21(3), 449–453. 10.1002/oby.20053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laska MN, Pelletier JE, Larson NI, & Story M (2012). Interventions for weight gain prevention during the transition to young adulthood: A review of the literature. Journal of Adolescent Health, 50(4), 324–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCloughen A, Foster K, Kerley D, Delgado C, & Turnell A (2016). Physical health and well-being: Experiences and perspectives of young adult mental health consumers. International Journal of Mental Health Nursing, 25(4), 299–307. 10.1111/inm.12189 [DOI] [PubMed] [Google Scholar]
- Miles M, Huberman A, & Saldaña J (2013). Qualitative Data Analysis: A Methods Sourcebook Sage Publications. [Google Scholar]
- Naslund JA, Aschbrenner KA, Scherer EA, Pratt SI, & Bartels SJ (2017). Health promotion for young adults with serious mental illness. Psychiatric Services, 68(2), 137–143. 10.1176/appi.ps.201600091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson MC, Story M, Larson NI, Neumark-Sztainer D, & Lytle LA (2008). Emerging adulthood and college-aged youth: An overlooked age for weight-related behavior change. Obesity, 16(10), 2205–2211. 10.1038/oby.2008.365 [DOI] [PubMed] [Google Scholar]
- Olfson M, Gerhard T, Huang C, Crystal S, & Stroup TS (2015). Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry, 72(12), 1172–1181. [DOI] [PubMed] [Google Scholar]
- Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, & Hoagwood K (2015). Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health and Mental Health Services Research, 42(5), 533–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter KJ, Thomson JL, & Zoellner JM (2020). Predictors of engagement and outcome achievement in a behavioural intervention targeting sugar-sweetened beverage intake among rural adults. Public Health Nutrition, 23(3), 554–563. 10.1017/S1368980019003392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts SH, & Bailey JE (2011). Incentives and barriers to lifestyle interventions for people with severe mental illness: A narrative synthesis of quantitative, qualitative and mixed methods studies. Journal of Advanced Nursing, 67(4), 690–708. 10.1111/j.1365-2648.2010.05546.x [DOI] [PubMed] [Google Scholar]
- Saha S, Chant D, & McGrath J (2007). A systematic review of mortality in schizophrenia: Is the differential mortality gap worsening over time? Archives of General Psychiatry, 64(10), 1123–1131. 10.1001/archpsyc.64.10.1123 [DOI] [PubMed] [Google Scholar]
- Shannon A, McGuire D, Brown E, & O’Donoghue B (2020). A systematic review of the effectiveness of group-based exercise interventions for individuals with first episode psychosis. Psychiatry Research, 293(June), 113402. 10.1016/j.psychres.2020.113402 [DOI] [PubMed] [Google Scholar]
- Thomson JL, Tussing-Humphreys LM, Goodman MH, & Zoellner JM (2015). Engagement indicators predict health changes in a lifestyle intervention. American Journal of Health Behavior, 39(3), 409–420. 10.5993/AJHB.39.3.13 [DOI] [PubMed] [Google Scholar]
- Tuda D, Stefancic A, Hawes M, Wang X, Guo S, & Cabassa LJ (2022). Correlates of Attendance in a Peer-Led Healthy Lifestyle Intervention for People with Serious Mental Illness Living in Supportive Housing. Community Mental Health Journal, 58(4), 761–769. 10.1007/s10597-021-00881-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study will be available upon request through the National Institute of Mental Health Data Archive (NDA; https://nda.nih.gov/) once the parent study is complete.


