Abstract
A novel distraction technique is described for total hip arthroplasty in symptomatic high hip dislocation (Crowe IV) combining an intramedullary motorized lengthening nail with a pelvic support plate to gradually stretch hip soft tissues (distalization) and performing total hip arthroplasty with the cup in the primary acetabulum. Twelve patients (15 hips) were identified in a retrospective study via chart review. Medical records and radiographs were reviewed for details of the initial case parameters, surgical details, magnitude of distalization, duration of treatment, outcomes, and complications. Followed by an average of 67.4 mm of distalization, nearly anatomical cup placement, and equal leg length were achieved in all patients. During distalization, pain level was low with acceptable range of motion. One unplanned surgery and no complications with long-term sequelae occurred.
Keywords: High luxation of the hip, Chronic hip dislocation, Total hip arthroplasty, Distraction nail, Gradual distalization
Introduction
Symptomatic high hip dislocation, classified as Crowe type IV [1] developmental dysplasia of the hip (DDH), presents an orthopedic challenge [2,3]. Patients become symptomatic when the proximally migrated hip becomes stiff or painful. Limb length discrepancy contributes to lumbar spine degenerative change, long limb arthropathy, and even short limb knee and foot symptoms. The length discrepancy is further worsened by adduction and flexion contractures (Fig. 1). Treatment options that exist to this point include: (i) arthrodesis; (ii) total hip arthroplasty (THA) in conjunction with femoral shortening [[4], [5], [6]]; and (iii) THA after gradual distalization with an external skeletal fixator [7]. Each of these techniques has advantages and disadvantages [8]. The most commonly performed procedure, acute femoral shortening in combination with THA, treats the joint itself but leaves the patient with significant limb length discrepancy. The purpose of this report is to describe the initial results of a novel two-stage all-internal technique using an internal motorized lengthening nail (IMN) for gradual distalization of the femur, followed by THA. Our investigation took the form of a retrospective study across 2 institutions and was institutional review board-approved. Patients with symptomatic high hip dislocation (Crowe type IV [1]) that were treated in a two-stage procedure using an IMN together with a customized pelvic support plate (PSP) between 2015 and 2020 were identified via chart review. Baseline demographic data, clinical data of treatment, and outcome data with complications were obtained. Radiographs for all patients were reviewed. Patients at both institutions had provided prospective consent for inclusion in the retrospective study.
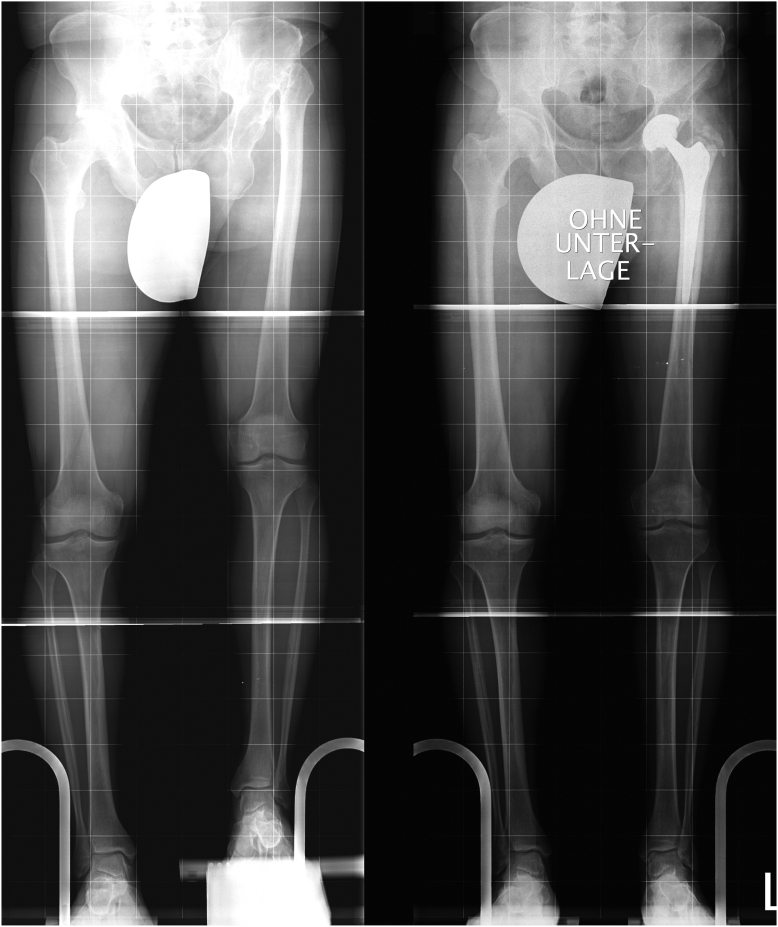
Figure 1.
Proximal migration of the hip joint and adduction contracture.
Surgical technique
A standard IMN Fitbone (Orthofix, Italy) and a custom-designed PSP was used as a base for femoral distraction in all patients. The PSP consists of a triangular plate-like base with 3 hemispherical cavity with polyethylene insert (Fig. 2) for articulation with a temporary 22-mm spherical head. An attached metal half-ring constrains the head, preventing dislocation, and allows range of motion of 30 degrees in all directions matched with an adapter allows attachment of the head to the IMN. Activation of the IMN is achieved by an external transmitter to a subcutaneous receiver by radiofrequency power. For final THA, an acetabular component used was a conventional Pinnacle Press fit cup (Depuy, IN, USA) and, in most cases, an Alloclassic SL cementless stem (Zimmer Biomet, IN, USA).
Figure 2.
Pelvic support plate (PSP).
The treatment was performed in 2 stages (Fig. 3).
Figure 3.
Sequence of treatment (1. initial finding, 2. start of distalization 3. end of distalization, 4. THA).
Stage 1
The patient is positioned lateral decubitus after general or spinal anesthesia and antibiotic prophylaxis given. An adductor tendon release is performed via a percutaneous small dissection using a hook knife until abduction of 30 degrees is achieved. Posterolateral exposure of the hip is preferred, as posterolateral acetabular augmentation may be necessary. Hip joint capsulotomy, femoral neck osteotomy, and identification of the true acetabulum are performed with reaming in the usual fashion. If more than 1 cm of the cup is uncovered, a solid graft formed from the resected femoral head is shaped and secured with screw fixation. A metal support, such as tantalum wedge, is never used. The acetabular cup is impacted and is routinely fixed with 2 or 3 screws to provide ideal stability. The abductor musculature proximal to the true acetabulum is split, periosteum is elevated, and the PSP is positioned (Fig. 4) 5-7 cm proximal to the upper border of the newly implanted acetabular component, oriented 30° to the frontal and sagittal plane, and secured bicortically with screws to the ilium. Rigid reaming of the proximal femur is performed to a diameter of 9 mm distally, preventing interference of future stem stability. The adapter and head are attached to a trial femoral nail inserted into the proximal femur and reduced into the PSP by lateral elevation and inward rotation of the leg. If reduction without tension and satisfactory stability is achieved, the trial nail is replaced by the definitive IMN (Fitbone TAA 0960) (Orthofix, Italy). The constraining half-ring is then attached via 2 screws, and the distal interlocking screw of the nail is inserted with perfect circle free-hand technique. A subcutaneous pocket is developed for the transceiver, which is placed into the pocket and attached to the IMN. An intraoperative test is performed to ensure motor function of the IMN.
Figure 4.
PSP in place.
Distraction begins immediately after surgery at a rate of 3 mm/day for 1 week, 2 mm/day for 1 week, and then 1 mm/day until the tip of the greater trochanter has moved 10-15 mm distal to the center of the acetabular cup as assessed on anterior-posterior radiograph (Fig. 5). The lengthening is stopped by the presence of neurologic signs and slowed by neurologic symptoms. Weight bearing of up to 20 kg is allowed on the operated leg. X-rays and exam are conducted weekly. The lengthening stops when the target position of the trochanter tip is 10-15 mm beyond the center of the final cup location. A one-to-two-week period allows further soft tissue accommodation to the new length.
Figure 5.
Thirthy-eight years, female (Case #10) sequence of distalization.
Stage 2
The second stage of treatment begins with exposure through the previous posterolateral approach, cautiously noting that all tissues, particularly the abductor musculature, will now be under increased tension. The constraining half-ring mechanism, PSP, antenna, and IMN are removed in that order. The femur is now broached in the usual fashion, allowing for implantation of a cementless femoral stem. Attention is being paid to the site of previous reaming and interlocking screw fixation in order to minimize the risk of fracture. Definitive Polyethylene liner and femoral head are implanted after trialing. If the cup size was 46 mm or less, we would use a 22 mm head and liner. In all other cases, larger heads were used but never more than 28 mm.
Results
Twelve patients (15 hips) were identified in whom two-stage hip distalization and THA had been performed. Mean age at initial surgery was 39.9 (15-67) years. In all cases, the etiology of hip dislocation was congenital hip dysplasia. The period of hip distalization (soft tissue lengthening) is managed (except in case 1) on an outpatient basis with an average inpatient stay of 8.4 days (3-14) following stage one and 6.6 (2-13) days following stage 2. Time between surgical stages averaged 73.4 days (30-98). In 3 bilateral patients, distalization was performed sequentially resulting in a temporary limb length discrepancy after the first side, which resolved after treatment of the second side, overall increasing the patient’s height. In 3 patients, prophylactic cerclage cabling of the proximal femur was performed due to concern about fracture on stem insertion.
Acetabular component position
In the group of 9 unilateral patients, acetabular component was positioned (relative to the craniocaudal position of the unaffected hips center of rotation) within 5 mm in 7 hips. In the group of the bilateral distalization, difference in acetabular component cranio-caudal location averaged 3.7 mm.
Limb length difference
Preoperatively, all patients had pain and severely compromised gait. Bilateral pathology and subsequent treatment occurred in 3 patients. In the 9 unilaterally affected patients, 81.8% of limb length difference resulted from proximal femoral migration (ΔS1 and ΔL, see Table 1). Mean preoperative limb length discrepancy was 66 mm (56-80) and postoperative 7.7 mm (0-19). Residual limb length discrepancy can be attributed to bone length segment differences, as reported in Table 1. One patient (9) had limb length discrepancy of 22 mm after bilateral distalization and THA and was shortened on the longer femur and stabilized with a retrograde femoral nail. Near equalization of limb length discrepancy resulted in functional and cosmetic improvement for patients (Figure 6, Figure 7).
Table 1.
Case report of treatment.
| Case | Side | Age [y] | Sex | Δ S 1 [mm] | Δ L [mm] | Distalization [mm] | Δ S 2 [mm] | Δ Cup [mm] | TBS [d] | Inpat. 1 [d] | Inpat. 2 [d] | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | R | 29 | f | −58 | −11 | +49 | −2 | 0 | 42 | 51 | ||
| 2 | R | 24 | m | −65 | −15 | +65 | −11 | +2 | 56 | 10 | 8 | |
| 3 | L | 31 | f | −70 | −7 | +60 | −12 | 0 | 30 | 7 | 8 | Nerve palsy |
| 4 | L | 15 | f | −56 | −7 | +53 | −7 | +6 | 70 | 7 | 6 | |
| 5 | L | 53 | m | −60 | −16 | +55 | 0 | 0 | 84 | 8 | 6 | |
| 6 | L | 23 | m | −58 | −21 | +80 | +2 | −11 | 70 | 6 | 5 | |
| 7 | R | 67 | f | −79 | −22 | +60 | −19 | −9 | 84 | 14 | 13 | Fracture |
| 8 | R | 62 | f | −80 | −1 | +60 | −15 | 0 | 57 | 3 | 2 | |
| 9 | L | 35 | f | 0 | 0 | +78 | 0 | 0 | 84 | 8 | 5 | |
| 9 | R | 36 | f | −7 | −3 | +75 | −5 | +3 | 92 | 5 | 7 | Fracture |
| 10 | L | 37 | f | −9 | −2 | +86 | 0 | 0 | 91 | 12 | 7 | |
| 10 | R | 38 | f | 0 | 0 | +75 | 0 | +1 | 98 | 8 | 7 | |
| 11 | L | 60 | f | 0 | 0 | +75 | 0 | 0 | 84 | 9 | 6 | |
| 11 | R | 60 | f | −6 | −3 | +80 | 0 | +7 | 82 | 7 | 6 | Screw loosening |
| 12 | L | 43 | f | −67 | −7 | +60 | −2 | +5 | 77 | 13 | 7 |
Patient 9, 10 and 11 were treated bilateral.
Δ S 1/2 – Leg Length difference as measured by distance anterior superior iliac spine to level of ankle joint, affected side minus unaffected side.
Δ L – Leg length difference as measured from tip of greater trochanter to level of ankle joint, affected side minus unaffected side.
Δ Cup - Difference in caudocranial position of center of rotation, of replaced hip minus contralateral hip.
TBS, Time between surgical stages.
Figure 6.
Fifty-three years, male (Case #5) before and after treatment.
Figure 7.
Fifty-three years, male (Case #5) clinical result.
Functional outcomes
Preoperative and 2-year postoperative gait videos were reviewed. Preoperative videos were notable for uni- or bilateral Trendelenburg gait, in addition to gait changes related to limb length discrepancy and hip stiffness. Three months after second-stage treatment, gait improved in all patients. Two-year videos demonstrated ongoing Trendelenburg gait in 1 of 9 monolateral patients, while others had near-normal gait. Of the 3 bilateral patients, 2 of them retained mild, single-sided Trendelenburg gait.
In 10 patients, mean pain level was documented on a visual analog scale (0 = no pain, 10 = unable to move) with an average of 5.9 preoperatively and 1.2 at examination 3 months after THA. Health-related quality of life (SF-36) score was available for 8 patients pre- and post-treatment. The mean physical component summary increased by 35% (standard deviation 9.8, P = .003) and the mean mental component summary increased by 17% (standard deviation 11.0, P = .04), corresponding to an improvement in health-related quality of life. Figure 8 shows that the summary values after surgery are close to the German population sample [9].
Figure 8.

Physical and mental component summary before and after treatment.
Complications
In all cases, distraction took place as planned. Instability and dislocation of the head has never been a problem. Temporary sciatic neuropraxia occurred in one case (#3); in retrospect, intraoperative distalization when implanting the IMN was done with too much tension. The PSP loosened in one patient (#11) and was revised to achieve an acceptable screw fixation. Two patients (#7, #9) sustained a fracture of the proximal femur during stem insertion at the second surgery, managed with cerclage wires in one case and cerclage wires and long-stemmed component in the other with no long-term sequela.
Discussion
The incidence of chronic proximal hip dislocation secondary to untreated DDH (Crowe IV DDH) [1] has decreased in developed countries since the introduction of screening programs [10] for hip dysplasia in infants. Patients affected commonly demonstrate a short leg gait, Trendelenburg limping, and pelvic obliquity. They may complain of hip pain, back pain, fatigue, limp, and cosmetic dissatisfaction with the condition.
Arthrodesis of the hip joint compromises activities of daily living while sitting, standing, and walking. Degenerative change of the lumbar spine results from hyperlordosis and pelvic obliquity. Performing THA by placing the cup proximal to the primary acetabulum does not provide long-term cup stability, as the bone stock at this level is poor and does not have the geometric shape for cup stability [11].
The primary goal for THA must be to position the cup in the location of the primary acetabulum, with or without reconstruction of the acetabular roof. Reduction of the proximal femur, greater trochanter, and the gluteus medius muscle into the appropriate position requires distalizing these structures 4-8 cm without damage to them and the sciatic nerve.
Acute distraction of the hip by more than 2 cm is associated with a high risk of sciatic nerve injury [12]. The majority of sciatic nerve palsies may not resolve [13]. Previous studies have described safe lengthening thresholds of between 2.7 and 5.4 cm [14]. Farrell et al. noted an average of just 1.7 cm of lengthening in patients with nerve palsy where that was deemed to be the causative factor [13]. Additionally, recent study has demonstrated changes in sciatic nerve motor evoked potentials with an average of just 14.9 mm of acute lengthening (or 3% of femoral length) [15].
Segmental resection of the proximal femur to acutely distalize the trochanter region reduces the risk of damaging the sciatic nerve but results in scarring, muscular dysfunction, and persistent shortening. Ahmed et al. published a retrospective study of 13 patients (14 hips) with Crowe IV DDH who underwent THA and simultaneous subtrochanteric osteotomy at a mean age of 37 years [16]. All osteotomies were united, with no sciatic nerve injuries noted; however, there was a revision rate of 14%. Wang et al. reported a series of 76 hips in 62 patients with Crowe IV DDH with a mean age of 38.8 years [17]. Mean limb length discrepancy prior to treatment was 4.3 cm, and after treatment it was 1.0 cm. They reported 2 cases of transient nerve palsy, 1 case of nonunion, and 4 cases of intraoperative fracture. A long stem THA was used, with the medial gluteus muscle stretched or lengthened acutely. With this technique, even if later lengthening of the distal femur is performed [18], the result is not a physiological approach to the muscles.
Gradual lengthening with an external fixator presents a risk of iliac pin loosening, patient discomfort, and pin site sepsis leading to prosthetic infection. Lai et al. used an external fixator for iliofemoral distraction in 56 patients with unilateral Crowe IV DDH, followed by THA [19]. Anatomical cup placement without femoral shortening was achieved, but 6 patients required revision due to pin loosening. Cup revision was required in 9 cases. Holinka et al. reported use of a monolateral external fixator with 2 pin site infections and one temporary peroneal nerve palsy. Three cups required revision surgery in 2 of their patients [7].
The first case reported of gradual distraction with an IMN was performed in 2003 in Munich. This successful procedure was published as case report in 2005 [20]. However, the early versions of customized PSP resulted in a small range of motion during distalization and high pain levels and did not offer a breakthrough.
Summary
The goal of our study was to evaluate the use of an IMN in combination with a PSP with gradual distalization of the femur to a physiologic level, adapted to the specific situation of high hip dislocation. Summarizing the most common problems of chronically dislocated hips, they are addressed by continuous distalization in a most physiological approach. Using an IMN avoids the disadvantage of external fixation and allows anatomical cup placement and even more correction of limb length discrepancies. In our small series, the major goals were reached, and no permanent sciatic nerve palsy or infection occurred. Compared to other techniques with 2 stages to restore the hip physiologically and compensate for the limb length discrepancy all internally, the costs are not higher. We recognize the learning curve intrinsic to this first consecutive group of patients, as well as the lack of a comparative control group. We emphasize avoiding intraoperative sciatic nerve tension during hip reduction and carefully inserting the stem into the femur to avoid shaft fracture. On the one hand, the technique requires expert skills for difficult hip arthroplasty in often osteopenic bone, as well as skills for managing gradual implantable limb lengthening. On the other hand, it offers THA for patients with symptomatic high hip dislocation in a more physiological, all internal way.
Conflicts of interest
S. Morrison is paid for educational talks for Orthofix LLC (Italy). M. Dahl is a paid consultant for Stryker and NuVasive and receives IP royalties from Stryker. R. Baumgart receives royalties from Orthofix and paid consultant for Orthofix and Implantcast; all other authors declare no potential conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2023.101257.
Appendix A. Supplementary data
References
- 1.Crowe J.F., Mani V.J., Ranawat C.S. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61:15–23. [PubMed] [Google Scholar]
- 2.Liu R.Y., Bai C.Y., Song Q.C., Dang X.Q., Wu Y.J., Wang K.Z. Partial greater trochanter osteotomy for hip reduction in total hip arthroplasty for high dislocated hip: a preliminary report. BMC Musculoskelet Disord. 2014;15:293. doi: 10.1186/1471-2474-15-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Starker M., Bischof F., Lindenfeld T. Versorgung der hohen Hüftluxation (Crowe-IV-Hüfte) mit einer zementfreien Individualendoprothese und z-förmiger subtrochantärer Femurverkürzung. Zeitschrift fur Orthopadie und Unfallchirurgie. 2011;149:518–525. doi: 10.1055/s-0031-1280029. [DOI] [PubMed] [Google Scholar]
- 4.Król R., Rojewski M., Kamiński A., Popławski T. Operative tactics and results of treatment of patients with coxarthrosis secondary to congenital high luxation of hip joints. Ortop Traumatol Rehabil. 2007;9:604–611. [PubMed] [Google Scholar]
- 5.Zeng W.N., Liu J.L., Wang F.Y., Zhang X., Fan H.Q., Chen G.X., et al. Total hip arthroplasty for patients with Crowe type IV developmental dysplasia of the hip: Ten years results. Int J Surg. 2017;42:17–21. doi: 10.1016/j.ijsu.2017.04.029. [DOI] [PubMed] [Google Scholar]
- 6.Vreim Holm A.G., Terjesen T., Reikerås O. Subtrochanteric shortening and uncemented arthroplasty in hips with high dislocation - a cohort study with 13-30 years follow-up. J Orthop. 2019;16:80–85. doi: 10.1016/j.jor.2018.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holinka J., Pfeiffer M., Hofstaetter J.G., Lass R., Kotz R.I., Giurea A. Total hip replacement in congenital high hip dislocation following iliofemoral monotube distraction. Int Orthop. 2011;35:639–645. doi: 10.1007/s00264-010-1001-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guo R., Chen J.Y., Zhang G., Zhou Y., Chen J., Chai W. Calculation method to predict postoperative limb length in patients undergoing THA following developmental dysplasia of hips. BMC Musculoskelet Disord. 2019;20:513. doi: 10.1186/s12891-019-2903-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bellach B.-M., Ellert U., Radoschewski M. Der SF-36 im Bundes-Gesundheitssurvey. Bundesgesundheitsbl - Gesundheitsforsch - Gesundheitsschutz. 2000;43:210–216. [Google Scholar]
- 10.Graf R. Classification of hip joint dysplasia by means of sonography. Arch Orthop Trauma Surg (1978) 1984;102:248–255. doi: 10.1007/BF00436138. [DOI] [PubMed] [Google Scholar]
- 11.Munigangaiah S., O'Dwyer S., Masterson E. Uncemented total hip arthroplasty in osteoarthritis of hip secondary to low and high dislocated hips: a mid-term follow-up study. J Nat Sci Biol Med. 2016;7:136–142. doi: 10.4103/0976-9668.184699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hofstätter J., Dominkus M. Endoprothetische Versorgung der sekundären Dysplasiecoxarthrose bei kongenitaler Hüftluxation. JATROS Orthopädie Traumatologie Rheumatologie. 2017;22:22–24. [Google Scholar]
- 13.Farrell C.M., Springer B.D., Haidukewych G.J., Morrey B.F. Motor nerve palsy following primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2619–2625. doi: 10.2106/JBJS.C.01564. [DOI] [PubMed] [Google Scholar]
- 14.Higuchi Y., Hasegawa Y., Ishiguro N. Leg lengthening of more than 5 cm is a risk factor for sciatic nerve injury after total hip arthroplasty for adult hip dislocation. Nagoya J Med Sci. 2015;77:455–463. [PMC free article] [PubMed] [Google Scholar]
- 15.Bayram S., Akgül T., Özmen E., Kendirci A.Ş., Demirel M., Kılıçoğlu Ö.İ. Critical limit of lower-extremity lengthening in total hip arthroplasty: an intraoperative neuromonitorization study. J Bone Joint Surg Am. 2020;102:664–673. doi: 10.2106/JBJS.19.00988. [DOI] [PubMed] [Google Scholar]
- 16.Ahmed E., Ibrahim E.-G., Ayman B. Total hip arthroplasty with subtrochanteric osteotomy in neglected dysplastic hip. Int Orthop. 2015;39:27–33. doi: 10.1007/s00264-014-2554-0. [DOI] [PubMed] [Google Scholar]
- 17.Wang D., Li L.-L., Wang H.-Y., Pei F.-X., Zhou Z.-K. Long-term results of cementless total hip arthroplasty with subtrochanteric shortening osteotomy in Crowe type IV developmental dysplasia. J Arthroplasty. 2017;32:1211–1219. doi: 10.1016/j.arth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 18.Harkin E., Rozbruch S.R., Liskutin T., Hopkinson W., Bernstein M. Total hip arthroplasty and femoral nail lengthening for hip dysplasia and limb-length discrepancy. Arthroplast Today. 2018;4:279–286. doi: 10.1016/j.artd.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lai K.-A., Liu J., Liu T.-K. Use of iliofemoral distraction in reducing high congenital dislocation of the hip before total hip arthroplasty. J Arthroplasty. 1996;11:588–593. doi: 10.1016/s0883-5403(96)80114-8. [DOI] [PubMed] [Google Scholar]
- 20.Baumgart R., Krammer M., Winkler A., Hinterwimmer S., Muensterer O., Mutschler W. Reduction of high dislocation of the hip using a distraction nail before arthroplasty. J Bone Joint Surg Br. 2005;87:565–567. doi: 10.1302/0301-620X.87B4.16080. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.