Abstract
Background
Leg length discrepancy (LLD) is a common complication after total hip arthroplasty (THA) leading to significant morbidity and dissatisfaction for patients. A popular system for robotic arm-assisted THA utilizes preoperative computed tomography (CT) scans for surgical planning. Accurate measurement of leg length is crucial for restoring appropriate patient anatomy during the procedure. This study investigates the interobserver and interlandmark reliability of 3 different pelvic landmarks for measuring preoperative LLD.
Methods
We compiled preoperative pelvic CT scans from 99 robotic arm-assisted THAs for osteoarthritis. Radiologic leg length measurement was performed using the robotic arm-assisted THA application by 2 orthopaedic residents using reference lines bisecting the following pelvic landmarks: the anterior superior iliac spines, acetabular teardrops, and most inferior aspect of the ischial rami.
Results
On multivariate analysis, there was no significant difference found (P value = .924) for leg length measurement based on the 3 different pelvic anatomical landmarks. Leg length measurements showed interobserver reliability with significant Pearson correlation coefficients (r = 1.0, 0.94, 0.96, respectively) and nonsignificant differences in LLD means between subjects on paired sample (P value = .158, .085, 0.125, respectively) as well as between landmarks on pairwise comparison.
Conclusions
The 3 pelvic landmarks used in this study can be used interchangeably with the lesser trochanter as the femoral reference point to evaluate preoperative LLD on pelvic CT in patients undergoing robotic-arm assisted THA. This study is the first of its kind to evaluate the interobserver and interlandmark reliability of anatomical landmarks on pelvic CT scans and suggests interchangeability of 3 pelvic landmarks for comparing leg length differences.
Keywords: Leg length discrepancy, Total hip arthroplasty, Mako robotic-assisted total hip arthroplasty, Pelvic landmark
Introduction
Clinically significant leg length discrepancy (LLD) is among the most common causes of patient dissatisfaction after total hip arthroplasty (THA) with an incidence rate up to 50% [1,2]. Excessive LLD can lead to decreased hip stability [3] and patient dissatisfaction [2,4], as well as increased back pain or sciatica [5,6], gait disorders [7], and litigation [[8], [9], [10]].
Accurate measurement of LLD therefore represents an important component of the approach to preoperative planning in THA. Several techniques, both radiological and clinical, have been developed for this purpose, with the most common clinical technique being the tape measure method (anterior superior iliac spine to medial malleolus) and the most common radiological technique being full-length standing anterior-posterior radiograph [11,12]. When LLD is related to disease of the pelvis, hip, or proximal femur, as in hip osteoarthritis, measurement can be performed on anterior-posterior pelvic imaging using pelvic and femoral landmarks alone. Common femoral reference points include the center or tip of the femoral head or the most medial prominence of the lesser trochanter. Common pelvic landmarks include the inferior end of the acetabular teardrop, the caudal end of the ischial tuberosity, and the anterior superior iliac spine (ASIS) as described and used by many authors [[13], [14], [15], [16], [17], [18], [19], [20]]. Prior investigations have resulted in contradictory evidence regarding the reliability of each of these landmarks for use in accurately determining LLD using plain radiographs [13,18,19], but similar investigations have not been performed using computed tomography (CT) scans for pelvic imaging.
Some robotic arm-assisted THA systems require a CT scan for preoperative planning, and LLD measurement can be performed on these scans using the aforementioned landmarks. Being CT based, this specific platform may provide a more accurate means to measure leg length differences as compared to traditional radiograph-based methods. [[21], [22], [23]]. The goal of this study was to compare the reliability of 3 commonly used pelvic reference landmarks in accurately measuring LLD as measured using a CT-based 3-dimensional capable templating software. Our null hypothesis was that there is no difference between the LLD as measured by the pelvic landmarks described.
Material and methods
Institutional review board approval was obtained prior to the initiation of the study. A retrospective review was performed on 105 consecutive patients who underwent robotic arm-assisted THA (Mako robotic arm-assisted total hip, Stryker, Mahwah, New Jersey USA) with preoperative pelvic CT at a full-service hospital in the Midwestern United States between August 2018 and March 2021. The sample size of this study was derived through power analysis, and represented every patient that underwent THA with the Mako system from a single provider during the stated time period. Supine CT images were taken during preoperative planning in accordance with the THA CT scanning protocol per manufacturer recommendations. Images were stored as Digital Imaging and Communications in Medicine (DICOM file) on a Picture Archiving and Communication System (Agfa HealthCare, Mortsel, Belgium). Images were then imported into the MAKOplasty Total Hip Application for segmentation, landmark identification, and preoperative leg length measurement.
Inclusion criteria included all patient ages, all sex categorizations, unilateral arthroplasty for any surgical indication, and no patient with clinically detectable active infection. Six patients had current or prior pathology that affected the anatomical landmarks making them ineligible for the study. Thus, 99 of the 105 images met the inclusion criteria for analysis.
Radiologic leg length measurement was performed using the CT-based Total Hip Application by 2 independent orthopaedic residents who were blinded to each other’s work. For each image set, reference lines were drawn at 3 anatomic landmarks of the pelvis: (1) The ASIS-ASIS line, connecting the centers of bilateral ASISs; 2) the interteardrop line, connecting the caudal margin of the bilateral acetabular teardrops, and 3) the bi-ischial line, connecting the caudal margin of the bilateral ischial tuberosities. Radiological leg lengths were calculated by the software as the distance between each pelvic reference line and a single femoral reference point, the most prominent tip of the lesser trochanter. LLD was calculated by the Total Hip Application planning page by subtracting the operative leg length from the nonoperative leg length. The workflow of pelvic and femoral landmark selection is depicted in Figure 1, Figure 2, respectively. The LLD measurement process is displayed in Figure 3, Figure 4, Figure 5. A positive LLD value was reported when the operated limb was longer than the contralateral side, while a negative value indicated the opposite. Radiological measures were reported with a 1-mm precision scale.
Figure 1.
Pelvic landmark selection workflow on CT image; ASIS landmark. Selection is made on transverse (a), coronal (c), and sagittal (d) views with 3D composite representation (b). CT, computed tomography; 3D, 3-dimensional.
Figure 2.
Femoral landmark selection workflow on CT image; Lesser trochanter landmark. Selection is made on transverse (a), coronal (c), and sagittal (d) views with 3D composite representation (b). CT, computed tomography; 3D, 3-dimensional.
Figure 3.
Leg length discrepancy (LLD) measurement using ASIS-ASIS line (arrowhead) and lesser trochanters (arrows). ASIS, anterior superior iliac spine.
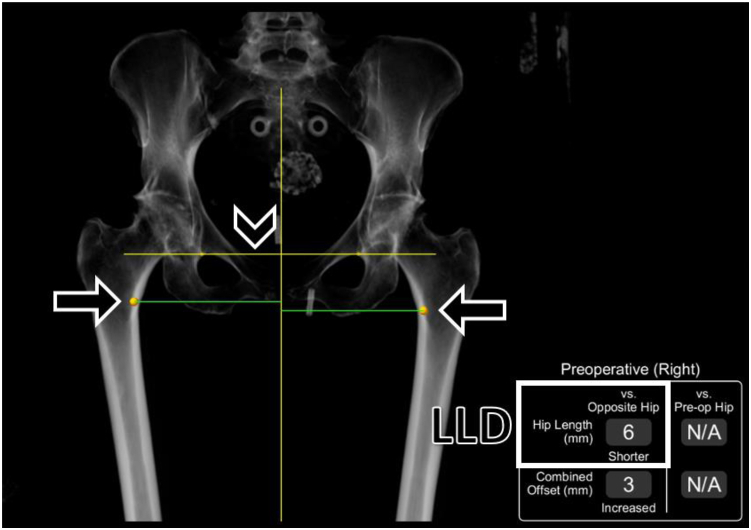
Figure 4.
Leg length discrepancy (LLD) measurement using interteardrop line (arrowhead) and lesser trochanters (arrows).
Figure 5.
Leg length discrepancy (LLD) measurement using bi-ischial line (arrowhead) and lesser trochanters (arrows).
Statistical analyses were conducted using the SPSS Statistics, version 28 (IBM, Armonk, New York). Descriptive statistics provided in Table 1 are mean with standard deviation. Pearson correlation coefficient and paired t-test were used to examine the interobserver consistency of the 2 reviewers. The differences among the leg length measurements based on 3 different pelvic anatomical landmarks (ASIS-ASIS line, interteardrop line, and bi-ischial line) were tested by repeated-measure analysis of variance. All the analytical results were considered to be significant when P values were less than or equal to .05.
Table 1.
Descriptive statistics of LLD measurements in the study population.
| Pelvic landmark | Total | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| ASIS-ASIS line | 99 | −4.616 | 6.5776 | −49 | 8 |
| Interteardrop line | 99 | −4.525 | 6.8922 | −54.5 | 9 |
| Bi-ischial line | 98a | −4.582 | 7.4053 | −49 | 7.5 |
LLD, leg length discrepancy; SD, standard deviation; ASIS, anterior superior iliac spine.
One patient’s bi-ischial line value was not measured by one of the reviewers.
Results
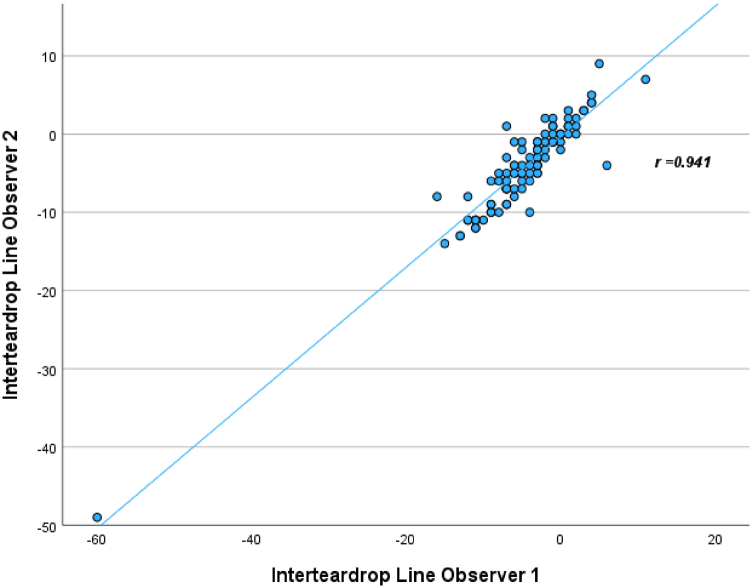
On multivariate analysis, there was no significant difference found (P-value = .924) for leg length measurement based on the 3 different pelvic anatomic landmarks (ASIS-ASIS line, interteardrop line, and bi-ischial line) as reported in Table 2. The leg length measurements from both reviewers were consistent with significant Pearson correlation coefficient (r = 1.0, 0.94, 0.96, respectively), as seen in Figure 6, Figure 7, Figure 8 and nonsignificant differences in means (P value = .158, .085, 0.125, respectively), as seen in Table 3. Finally, nonsignificant differences were found through pairwise comparison between each of the pelvic landmarks as reported in Table 4. The null hypothesis was not rejected.
Table 2.
Multivariate statistical analysis results.
| Three pelvic landmarks | Value | F | Hypothesis df | Error df | P value |
|---|---|---|---|---|---|
| Pillai’s Trace | 0.002 | 0.080 | 2.00 | 96.00 | .924 |
| Wilks’ Lambda | 0.998 | 0.080 | 2.00 | 96.00 | .924 |
| Hotelling’s Trace | 0.002 | 0.080 | 2.00 | 96.00 | .924 |
| Roy’s Largest Root | 0.002 | 0.080 | 2.00 | 96.00 | .924 |
Figure 6.
Linear regression of interobserver LLD measurement using the ASIS-ASIS line with Pearson correlation coefficient. ASIS, anterior superior iliac spine; LLD, leg length discrepancy.
Figure 7.
Linear regression of interobserver LLD measurement using the Interteardrop line with Pearson correlation coefficient. LLD, leg length discrepancy.
Figure 8.
Linear regression of interobserver LLD measurement using the Bi-ischial line with Pearson correlation coefficient. LLD, leg length discrepancy.
Table 3.
Paired samples statistical analysis results.
| Pelvic landmark pair (observer 1 vs 2) | Mean difference | SD | SEM | 95% confidence interval of the difference |
t | df | P value | |
|---|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||||
| ASIS-ASIS line | −0.020 | 0.141 | 0.014 | −0.048 | 0.008 | −1.421 | 98 | .158 |
| Interteardrop line | −0.444 | 2.544 | 0.256 | −0.952 | 0.063 | −1.738 | 98 | .085 |
| Bi-ischial line | −0.306 | 1.960 | 0.198 | −0.699 | −0.087 | −1.546 | 97a | .125 |
SD, standard deviation; SEM, standard error of the mean; ASIS, anterior superior iliac spine.
One patient’s bi-ischial line value was not measured by one of the reviewers.
Table 4.
Pairwise comparison statistical analysis results.
| Pelvic landmark 1 | Pelvic landmark 2 | Mean difference | SEM | 95% confidence interval of the difference |
P value | |
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||
| ASIS-ASIS line | Interteardrop line | −0.133 | 0.336 | −0.799 | 0.534 | .694 |
| Bi-ischial line | −0.092 | 0.495 | −1.074 | 0.891 | .853 | |
| Interteardrop line | ASIS-ASIS line | 0.133 | 0.336 | −0.534 | 0.799 | .694 |
| Bi-ischial line | 0.041 | 0.394 | −0.741 | 0.823 | .918 | |
| Bi-ischial line | ASIS-ASIS line | 0.092 | 0.495 | −0.891 | 1.074 | .853 |
| Interteardrop line | −0.041 | 0.394 | −0.823 | 0.741 | .918 | |
SEM, standard error of the mean; ASIS, anterior superior iliac spine.
Discussion
LLDs are very common in the general population with LLDs of up to 10 mm existing in 60%-95% of the population. However, not all patients with LLDs present with symptoms or functional deficits [24]. Typically, LLDs less than 5 mm are asymptomatic, whereas LLDs that are greater than 2 cm are nearly always symptomatic [9,24]. LLD-associated symptoms following THA can include back pain, gait disorders, dislocation, and neuritis [6,7,25].
LLDs can be found postoperatively in up to 50% of THA patients, and this is one of the leading causes of patient dissatisfaction after a THA [1,2]. According to the American Association of Hip and Knee Surgeons, LLD was the second highest cause for malpractice lawsuits against orthopaedic surgeons in 2007 [9,10]. Some experts recommend that surgeons avoid LLDs greater than 1 cm when performing THA [24]. Since LLDs can impact a patient’s overall satisfaction and functionality, efforts to reduce the incidence of symptomatic postoperative LLD are an important avenue of study.
Robotic assistance has been shown to help reduce LLD in patients undergoing THA [[21], [22], [23]]. As arthroplasty technology evolves, investigations to validate various landmarks and compare them to each other in addressing LLD become important. This study was an attempt to compare 3 landmarks and their contributions in the analysis of LLD.
Accurate leg length measurement is highly dependent on imaging modality. Measurements can be distorted on plain film by factors such as magnification, distance from the radiograph source to the cassette, or pelvic rotation [9,26]. Historical attempts to correct for these variables include full-length imaging techniques such as the orthoroentgenogram, teleoroentgenogram, and CT scanogram, which have been shown to be more reliable and accurate than standard plain films [14,26]. However, these modalities involve greater radiation exposure than is necessary when comparing preoperative and postoperative images of patients undergoing THA, where potential changes in the leg length occur only within the operative site about the hip and pelvis. CT scan with digital localization image has been shown to be an even more reliable imaging modality, but is infrequently used due to cost, inconvenience, and radiation exposure concerns [26]. However, these drawbacks are obviated for patients receiving robotic THA as the use of the robotic targeting system requires a preoperative CT scan. Patient positioning appears to have little effect on measurement; it has been demonstrated that weight-bearing imaging modalities do not differ significantly from supine modalities when measuring leg length [[26], [27], [28]]. Measurements based on supine CT scan theoretically eliminate projection inaccuracies seen with plain films in patients with contractures at the hip or knee.
Various authors have argued for the reliability of each of the landmarks used in the present study. The interteardrop line has been found to be the most reliable pelvic landmark when comparing plain films to “True LLD” (ie, LLD as measured by block testing or tape measure), and it has been demonstrated that the vertical position of the teardrop points is not affected significantly by the rotation of the pelvis [18,29]. However, recent investigations have conversely found that in suboptimal radiographs, such as some intraoperative plain films, relationships between classically used landmarks such as the pelvic teardrops may be distorted. In this case, the obturator foramen was found to be the most reliable landmark resistant to these distortion effects, and the teardrops were the least reliable [9]. Other investigators have concluded that measuring from the inferior aspect of the ischial tuberosities to the most prominent medial point on the lesser trochanter is the superior method for measuring LLD but still experienced large error margins [13].
The present study revealed a trend, as demonstrated by a Pearson correlation coefficient of 1, that interobserver reliability was highest when measuring LLD using the ASIS-ASIS line as the pelvic landmark. However, this finding did not achieve statistical significance (P-value = .158). As no significant difference was found between measurements of LLD, the present study serves as evidence that each of these pelvic landmarks are equally reliable when assessing LLD on CT imaging. Although the measurements were performed by residents trained through instruction by a single attending surgeon, we believe that the interobserver findings support that the measurement were taken correctly and consistently. To better understand the effect of levels of experience on measurement, future methodology can include multiple observers with different levels of experience to increase the power of interobserver findings. It is possible that no significant difference was seen because most of the subjects included in this study had preoperative differences of less than 10 mm with all landmarks. Patients with more coronal obliquity of the pelvis (whether related to a flexion contracture of an arthritic hip or a spinopelvic deformity) who consequently have more significant differences in preoperative leg length may have a greater degree of variability in the LLD measurements obtained using the 3 methods.
The current study is limited by the lack of comparative clinical measurements of subjects’ True LLD as it has been shown that LLD as measured by pelvic landmarks on plain radiograph differs significantly from True LLD (as measured by block testing or tape measure) [18,19]. The findings of this study are exclusively applicable to preoperative pelvic CT scans, and further study is required to understand the applicability with plain radiographs, or in the setting of intraoperative and postoperative imaging. The findings are also limited to the particular technology and software used in the analysis and may not be generalizable to other technologies or clinical situations. Furthermore, other literature has determined that True LLD correlates more accurately to patient perception of LLD than LLD as measured by CT scanogram [30]. As these questions have not been assessed when using standard CT scans, comparison of LLD as measured in the current study to clinical measurements of True LLD represents a clinically important avenue of future investigation.
Conclusions
From this study, we propose that most of the time, in routine total hip arthroplasty cases, any of the 3 pelvic landmarks assessed (ASIS-ASIS line, interteardrop line, and bi-ischial line) can be used interchangeably with the lesser trochanter as the femoral reference point to evaluate preoperative LLD on pelvic CT in patients undergoing robotic-arm-assisted THA. This investigation is the first of its kind which studies the interobserver and interlandmark reliability of anatomical landmarks on pelvic CT scans and provides valuable information for optimizing the accuracy of radiological leg length measurement.
Conflicts of interest
Tarek A. Taha reports having stock or stock options in Monogram Orthopaedics (Investor). All other authors declare no potential conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2023.101252.
Appendix A. Supplementary data
References
- 1.Djerf K., Wahlstrom O. Total hip replacement comparison between the McKee-Farrar and Charnley prostheses in a 5-year follow-up study. Arch Orthop Trauma Surg. 1986;105:158–162. doi: 10.1007/BF00433934. [DOI] [PubMed] [Google Scholar]
- 2.Ranawat C.S. The pants too short, the leg too long. Orthopedics. 1999;22:845–846. doi: 10.3928/0147-7447-19990901-16. [DOI] [PubMed] [Google Scholar]
- 3.Woo R.Y., Morrey B.F. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]
- 4.Kayani B., Pietrzak J., Donaldson M.J., Konan S., Haddad F.S. Treatment of limb length discrepancy following total hip arthroplasty. Br J Hosp Med. 2017;78:633–637. doi: 10.12968/hmed.2017.78.11.633. [DOI] [PubMed] [Google Scholar]
- 5.Friberg O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine. 1983;8:643–651. doi: 10.1097/00007632-198309000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Mihalko W.M., Phillips M.J., Krackow K.A. Acute sciatic and femoral neuritis following total hip arthroplasty. A case report. J Bone Joint Surg Am. 2001;83:589–592. doi: 10.2106/00004623-200104000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Rösler J., Perka C. The effect of anatomical positional relationships on kinetic parameters after total hip replacement. Int Orthop. 2000;24:23–27. doi: 10.1007/s002640050006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hofmann A.A., Skrzynski M.C. Leg-length inequality and nerve palsy in total hip arthroplasty: a lawyer awaits. Orthopedics. 2000;23:943–944. doi: 10.3928/0147-7447-20000901-20. [DOI] [PubMed] [Google Scholar]
- 9.Tsang H., Bouz T., Kwan K., French M. The intraoperative pelvic radiograph during total hip arthroplasty: is it reliable to estimate leg length? Arthroplast Today. 2022;16:9–14. doi: 10.1016/j.artd.2022.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Upadhyay A., York S., Macaulay W., McGrory B., Robbennolt J., Bal B.S. Medical malpractice in hip and knee arthroplasty. J Arthroplasty. 2007;22(6 Suppl 2):2–7. doi: 10.1016/j.arth.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Alfuth M., Fichter P., Knicker A. Leg length discrepancy: a systematic review on the validity and reliability of clinical assessments and imaging diagnostics used in clinical practice. PLoS One. 2021;16 doi: 10.1371/journal.pone.0261457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pettit M.H., Kanavathy S., McArthur N., Weiss O., Khanduja V. Measurement techniques for leg length discrepancy in total hip arthroplasty: a systematic review of reliability and validity. J Arthroplasty. 2022;37:2507–2516.e11. doi: 10.1016/j.arth.2022.05.029. [DOI] [PubMed] [Google Scholar]
- 13.Heaver C., St Mart J.P., Nightingale P., Sinha A., Davis E.T. Measuring limb length discrepancy using pelvic radiographs: the most reproducible method. HIP Int. 2013;23:391–394. doi: 10.5301/hipint.5000042. [DOI] [PubMed] [Google Scholar]
- 14.Kjellberg M., Al-Amiry B., Englund E., Sjödén G.O., Sayed-Noor A.S. Measurement of leg length discrepancy after total hip arthroplasty. The reliability of a plain radiographic method compared to CT-scanogram. Skeletal Radiol. 2012;41:187–191. doi: 10.1007/s00256-011-1166-7. [DOI] [PubMed] [Google Scholar]
- 15.Patel S.R., Toms A.P., Rehman J.M., Wimhurst J. A reliability study of measurement tools available on standard picture archiving and communication system workstations for the evaluation of hip radiographs following arthroplasty. J Bone Joint Surg Am. 2011;93:1712–1719. doi: 10.2106/JBJS.J.00709. [DOI] [PubMed] [Google Scholar]
- 16.Mahmood S.S., Al-Amiry B., Mukka S.S., Baea S., Sayed-Noor A.S. Validity, reliability and reproducibility of plain radiographic measurements after total hip arthroplasty. Skeletal Radiol. 2015;44:345–351. doi: 10.1007/s00256-014-2055-7. [DOI] [PubMed] [Google Scholar]
- 17.McWilliams A.B., Grainger A.J., O’Connor P.J., Redmond A.C., Stewart T.D., Stone M.H. Assessing reproducibility for radiographic measurement of leg length inequality after total hip replacement. HIP Int. 2012;22:539–544. doi: 10.5301/HIP.2012.9751. [DOI] [PubMed] [Google Scholar]
- 18.Meermans G., Malik A., Witt J., Haddad F. Preoperative radiographic assessment of limb-length discrepancy in total hip arthroplasty. Clin Orthop Relat Res. 2011;469:1677–1682. doi: 10.1007/s11999-010-1588-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tipton S.C., Sutherland J.K., Schwarzkopf R. The assessment of limb length discrepancy before total hip arthroplasty. J Arthroplasty. 2016;31:888–892. doi: 10.1016/j.arth.2015.10.026. [DOI] [PubMed] [Google Scholar]
- 20.Reina-Bueno M., Lafuente-Sotillos G., Castillo-Lopez J.M., Gomez-Aguilar E., Munuera-Martinez P.V. Radiographic assessment of lower-limb discrepancy. J Am Podiatr Med Assoc. 2017;107:393–398. doi: 10.7547/15-204. [DOI] [PubMed] [Google Scholar]
- 21.Sugano N. Computer-assisted orthopaedic surgery and robotic surgery in total hip arthroplasty. Clin Orthop Surg. 2013;5:1. doi: 10.4055/cios.2013.5.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taha T.A., Bejcek C. Robotic arm–assisted total hip arthroplasty to correct leg length discrepancy in a patient with spinopelvic obliquity. Arthroplast Today. 2020;6:784–791. doi: 10.1016/j.artd.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu S., Bernardo L., Yew K., Pang H. Robotic-arm assisted direct anterior total hip arthroplasty; improving implant accuracy. Surg Technol Int. 2020;38:347–352. doi: 10.52198/21.STI.38.OS1368. [DOI] [PubMed] [Google Scholar]
- 24.O’Brien S., Kernohan G., Fitzpatrick C., Hill J., Beverland D. Perception of imposed leg length inequality in normal subjects. HIP Int. 2010;20:505–511. doi: 10.1177/112070001002000414. [DOI] [PubMed] [Google Scholar]
- 25.Desai A.S., Dramis A., Board T.N. Leg length discrepancy after total hip arthroplasty: a review of literature. Curr Rev Musculoskelet Med. 2013;6:336–341. doi: 10.1007/s12178-013-9180-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sabharwal S., Kumar A. Methods for assessing leg length discrepancy. Clin Orthop Relat Res. 2008;466:2910–2922. doi: 10.1007/s11999-008-0524-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cleveland R.H., Kushner D.C., Ogden M.C., Herman T.E., Kermond W., Correia J.A. Determination of leg length discrepancy. A comparison of weight-bearing and supine imaging. Invest Radiol. 1988;23:301–304. doi: 10.1097/00004424-198804000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Guggenberger R., Pfirrmann C.W.A., Koch P.P., Buck F.M. Assessment of lower limb length and alignment by biplanar linear radiography: comparison with supine CT and upright full-length radiography. Am J Roentgenol. 2014;202:W161–W167. doi: 10.2214/AJR.13.10782. [DOI] [PubMed] [Google Scholar]
- 29.Goodman S.B., Adler S.J., Fyhrie D.P., Schurman D.J. The acetabular teardrop and its relevance to acetabular migration. Clin Orthop Relat Res. 1988;236:199–204. [PubMed] [Google Scholar]
- 30.Harris I., Hatfield A., Walton J. Assessing leg length discrepancy after femoral fracture: clinical examination or computed tomography? ANZ J Surg. 2005;75:319–321. doi: 10.1111/j.1445-2197.2005.03349.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.