Abstract
Purpose:
The purpose of this systematic literature review was to explore studies that report the experiences of adolescents, their families, and health care professionals of adolescents’ transition to self-management of type 1 diabetes (T1DM).
Methods:
SocINDEX, PsycInfo, APA PsycArticles, and MEDLINE electronic databases were searched. Studies reporting on experiences of transition to self-management of T1DM for adolescents, their parents, siblings, and health care professionals published between January 2010 amd December 2021 were included. The Mixed Methods Appraisal Tool guided trustworthiness and relevance of selected studies.
Results:
A total of 29 studies met the inclusion criteria. Findings indicate that adolescents’ experiences of transitioning to self-management of T1DM are interconnected with the supports provided by others (eg, family, teachers, friends). Considering interdependence and collective lived experiences is essential to developing effective and personalized family, peer, and social interventions to facilitate transition and to avoid negative outcomes in later life. The renegotiation of roles within the network of supports that impact adolescents’ transition and adolescents’ self-negotiation have been neglected.
Conclusion:
Transition to self-management of T1DM is a dynamic and iterative process comprising of continuous shifts between interdependence and independence, making it challenging for all involved. A number of research gaps and avenues for future research are outlined.
Type 1 diabetes (T1DM) is a predominantly childhood-onset chronic condition that results in a lifelong dependence on exogenous insulin. Maintaining optimal glycemic targets (A1C) requires onerous monitoring of blood glucose levels, balancing insulin requirements with carbohydrate intake and exercise, and multiple daily insulin injections. The incidence rate of T1DM, particularly in children and adolescents, has dramatically increased worldwide, with nearly 98 200 developing T1DM each year under 15 years old, increasing to approximately 128 900 under 20 years old. 1
Adolescence is an important milestone with an increased desire for autonomy in multiple areas of life. However, due to the complexity and unpredictability of T1DM, adolescents experience tensions between expectations and their capacity to become fully independent, which conflicts with their sense of autonomy. 2 Transition to self-management of T1DM during adolescence has been described as a multidimensional and evolving process, with parents and health care professionals gradually shifting and sharing day-to-day T1DM responsibilities and decision-making with adolescents, with the final goal of achieving full autonomy. 3 Characterizing and understanding the end-to-end collaborative trajectory between adolescents, their families, and health care professionals is challenging, and the various levels of interaction are poorly described in existing literature.
Navigating the turbulence of developmental, illness-factors, situational and organizational (health care) life transitions, and a mix of biopsychosocial factors associated with adolescence, can present significant challenges and barriers for successfully transitioning to self-management of T1DM. 4 This can result in deterioration of glycemic control, and may partly explain the observation that adolescents have highest AIC levels when compared across the lifespan. 5 As described in past research,6,7 transition to self-management cannot be seen independently from constructs such as empowerment and autonomy. Empowerment is a transactional and developmental process that may be essential to facilitating autonomy.6,8,9 Autonomy results from being empowered and pertains to the capacity of independent decision-making and initiative in which adolescents gradually separate from parental and other influences, and build the skills required for adulthood. In addition, the end stages of the transition to self-management of T1DM can occur in parallel with the transfer from pediatric care services to adult care services. During this time, patient care moves from their established health care team or clinic to another, consequently increasing the burden of self-management for adolescents with T1DM. However, transition of autonomy and transfer of care need to be considered as two distinct and separate constructs within the T1DM literature.
Suboptimal T1DM management can accelerate short- and long-term life-threatening complications, including diabetic ketoacidosis, severe hypoglycaemia, 10 cognitive function decline, visual impairment and blindness, kidney failure, 11 loss of consciousness, 12 and premature mortality. 13 Importantly, the risk of developing these complications appears to be cumulative. Periods of unsafe glycemic control in T1DM, as can occur in adolescence, will have a detrimental effect on lifelong outcomes, and this is termed “metabolic memory.” 14 Although the multiple dimensionality of the various transitions experienced by adolescents with T1DM have been acknowledged, including transitioning to adulthood, 15 beginning college, 16 entering the workforce, 17 accommodating new diabetes technology, 18 and transferring to adult care services, 19 the transition to self-management of T1DM within and beyond the family is not fully understood. Therefore, focusing on optimizing this transition will reduce complications in later life and improve future health outcomes at a population level. However, little is known regarding exactly how adolescents, their families, and their caregivers should navigate this transition and the role that health care professionals might play in this process.
The aim of this study was to conduct a systematic literature review of qualitative, quantitative, and mixed-methods research across social science, psychology, and health care literature domains in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines 20 to explore adolescents’ experiences of the transition to self-management of T1DM. This review also examined studies that report the experiences of their families and health care professionals regarding adolescents’ transition to self-management of T1DM. The key objective was to inform family, practitioner, and professional decision-making, policy, and practice through developing a comprehensive understanding of the barriers and facilitators of this transition. The guiding research question for this study adopted elements of the patient/problem, intervention, comparison and outcome (PICO) 21 process and was structured as follows: How do adolescents (P) with T1DM (I), their families, and medical professionals experience transition (O) to self-management of T1DM?
Methods
A systematic review of peer-reviewed literature in the social science (SocINDEX), psychology (PsycInfo, APA PsycArticles), and health care (MEDLINE) databases published in the English language between January 2010 and December 2021 was conducted. Although studies from all countries were considered for a global understanding of adolescents’ transition to self-management of T1DM, limited resources for translation compelled the authors to restrict to studies published in the English language. Evidence suggests that the exclusion of non-English studies has minimal impact on systematic review outcomes.22-24 Studies using quantitative, qualitative, and mixed-methods approaches were included. Zotero was used to organize the results from each database and to remove duplicates. A total of 1787 articles resulted from the database searches. A narrative synthesis using the Guidance on the Conduct of Narrative Synthesis in Systematic Reviews 25 was undertaken due to the degree of heterogeneity between studies. This approach was not a linear process but an iterative one, therefore relationships within and between studies were explored until finalized themes emerged to fully interpret the data.26,27
Search Strategy
The search strategy aimed to synthesize the literature related to the experiences of transition to self-management of T1DM directly experienced by adolescents and indirectly experienced by their parents, siblings, and health care professionals. Search terms were hierarchically structured and combined variations with Boolean connectors (“AND,” “OR”) of the following keywords: (autonomy) transition, type 1 diabetes, and self-management. The search was undertaken in November 2021 and last updated in January 2023. In compliance with PRISMA guidelines for reproducibility of this review, Table 1 shows a comprehensive example of the search string applied at SocINDEX database. The study protocol was not registered. For the study protocol, refer to the Supplemental Material.
Table 1.
Search String Applied to SocINDEX Database
| Search No. | Query |
|---|---|
| 4 | S1 AND S2 AND S3 |
| 3 | TI ( (self* OR manag* OR care* OR decision*) ) OR AB ( (self* OR manag* OR care* OR decision*) ) |
| 2 | TI ( (diabetes* OR “type 1 diabetes*”) ) OR AB ( (diabetes* OR “type 1 diabetes*”) ) |
| 1 | TI ( (autonomy OR transition*) ) OR AB ( (autonomy OR transition*) ) |
Abbreviations: S1, Search 1; S2, Search 2; S3, Search 4.
Eligibility Criteria
Mixed-study reviews are relevant to better understanding and exploring complex and context-sensitive topics, 28 such as transitions. Therefore, qualitative, quantitative, and mixed-methods research that reported on adolescents’, parents’, siblings’, and health care professionals’ experiences of transition to self-management of T1DM were included. Considering that the age of the transition to self-management for adolescents with T1DM can vary, age ranges between 3 and 40 years old were chosen to ensure that experiences before, during, or after transition were captured. Following agreement among all authors on the inclusion and exclusion criteria, identified studies were transferred to Zotero for further assessment. A screening process was undertaken to identify eligible articles following the removal of duplicates (n = 282). Abstracts and titles (n = 1505) were screened, and irrelevant studies were discarded. Remaining articles were retrieved in full text format, and the same criteria was applied. Reasons for exclusion were documented. Discrepancies among authors were resolved by consensus.
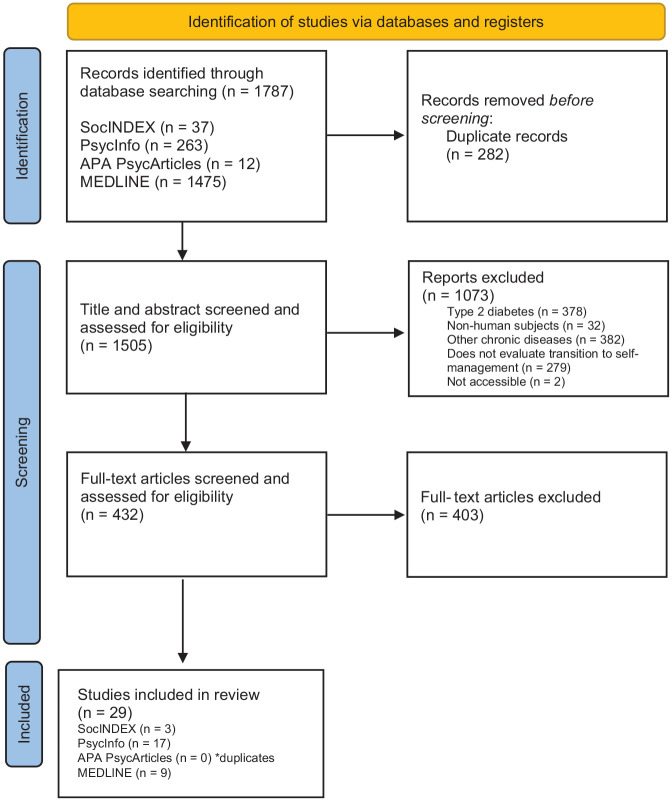
Articles were selected for inclusion if they were (1) scholarly peer-reviewed articles published in English between 2010 and 2021 and (2) included data pertaining to experiences of transition to self-management of T1DM. Studies were excluded if (1) there was no evidence in the title or abstract that the study was related to the transition from parental management to self-management, (2) the study investigated experiences of other chronic conditions, (3) the study did not use human subjects, and (4) the aim of the study was to evaluate life transitions. Table 2 summarizes the inclusion and exclusion criteria utilized. A data collection form was used to extract the information from the studies. The following study characteristics were collected: (a) author’s last name(s) and year published, (b) aim of the research, (c) research method, (d) sample size, and (e) study findings. A total of 29 articles were considered eligible for the review (see Figure 1 for PRISMA flow diagram).
Table 2.
Inclusion and Exclusion Criteria
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Publication type | Scholarly peer-reviewed journals | Not subject to peer review |
| Methods/design | Qualitative Quantitative Mixed method |
N/A |
| Language | English | Study titles and abstracts in languages other than English |
| Populations | Adolescents with type 1 diabetes and their parents/guardians, siblings, and health care professionals All ages |
Other chronic or long-term disease/illness Not human subjects |
| Published date | 2010 to 2021 | N/A |
| Other reasons | N/A | Duplicates Evaluates life transitions Does not contain data pertaining to lived experiences Full text not available |
Figure 1.
PRISMA flow diagram representing article identification and selection process.
Critical Appraisal
Selected studies underwent a critical appraisal for further comprehensive assessment of trustworthiness, relevance, and quality. The critical appraisal of the qualitative (n = 23), quantitative (n = 5), and mixed-methods (n = 1) selected studies was informed by the guidance of the Mixed Methods Appraisal Tool (MMAT),28,29 a single quality appraisal tool for systematic mixed-studies reviews. Trustworthiness and relevance of studies were determined by individual components that involved initial screening questions and sets of 6 quality appraisal questions to each appropriate research design, allowing for consideration of the unique characteristics of each study to be taken into consideration. The quality appraisal was undertaken to aid the interpretation of findings and to assist in determining the strength of the conclusions drawn. The critical appraisal showed that 28 of 29 studies were of high quality with a score of 3 or more. A detailed assessment of the quality of each study using the MMAT is provided in the Supplemental Material. None of the studies were excluded based on the results of the quality assessment as per MMAT recommendations. 29
Data Synthesis
Due to the heterogeneity between selected studies, findings were synthesized into themes using a narrative synthesis, which is commonly used to evaluate evidence across multiple disciplinary fields. 30 Selected studies were compared and summarized. Narrative synthesis guidance informed the reflected themes identified to produce an in-depth understanding of the transition from parental management to self-management of T1DM.25-27
Results
Included and categorized studies are shown in Tables 3 and 4, respectively, in which findings are detailed and relationships between themes are explored. Following the 10-year time frame recommendation for researching contemporary experiences, 31 studies were published between January 2010 and December 2021. Different settings, study designs, and sampling methods characterized these studies. Studies originated from the United States (n = 15), Denmark (n = 4), Sweden (n = 2), Brazil (n = 1), Canada (n = 1), Ireland (n = 1), Italy (n = 1), South Africa (n = 1), Taiwan (n = 1), and United Kingdom (n = 1). The data reported in each study were collected via semistructured interviews (n = 12), measures of self-management questionnaires (n = 2), a combination of interviews and focus groups (n = 2), workshops (n = 2), online surveys (n = 2), database search (n = 2), questionnaire with interviews (n = 1), semistructured interviews with photo elicitation (n = 1), visual storytelling (n = 1), in-depth interviews (n = 1), intensive interviews and internet communication (n = 1), journaling (n = 1), and path analysis (n = 1). Sixteen studies explored adolescents’ experiences of transition to self-management of T1DM4,18,32-45, and 9 studies included adolescent and parental experiences, predominantly mothers.46-54 Siblings’ experiences were considered in 1 study, 55 and 3 studies focused exclusively on parental experiences.56-58 None of the studies included health care professionals’ experiences.
Table 3.
Selected Articles Summarized
| Authors | Study aims/objective | Methodology | Population | Findings related to transition to self-management of T1DM |
|---|---|---|---|---|
| Babler and Strickland 32 (2015) | Gain a greater understanding of adolescent’s experiences of living with T1DM | In-depth interviews | 15 participants age 11-15 y | Parental nagging is barrier to a successful transition, whereas a trusting parent-adolescent relationship decreases conflict. |
| Bekker et al 56 (2019) | Explore how parents make meaning of living with a child with T1DM | Semistructured interviews | 9 mothers of children 12-18 y | Empowering adolescents to transition to self-management and live a healthy life adds meaning to parents’ lives. |
| Castensøe-Seidenfaden et al 46 (2017) | Explore the experiences of adolescents and their parents living with T1DM | Visual storytelling | 9 participants age 15-19 y | Parents are key in supporting adolescents’ transition to self-management, but they often experience anxiety and frustration. |
| Chiang et al 33 (2020) | Explore the life experiences of patients with T1DM who transition from adolescence into adulthood in Taiwan | Semistructured interviews | 14 participants age 16-25 y | Transition is a period that is characterized by interdependent relationships. |
| Chilton and Pires-Yfantouda 34 (2015) | Understand how adolescents adapt to their self-management requirements from diagnosis to the point of successful self-management | Semistructured interviews | 13 participants age 13-17 y | Successful transition to self-management correlates with reaching blood glucose targets, independence, and taking ownership and responsibility, factors that are associated with a strong sense of independence. |
| Collet et al 35 (2018) | Analyze the needs of preadolescents with T1DM | Semistructured interviews | 9 participants age 10-14 y | Emotional overload weakens transition to self-management. Adolescents must develop self-efficacy, self-awareness, and self-perception to confidently manage T1DM. |
| Dashiff et al 36 (2011) | Describe the experiences of parents of adolescents with T1DM in transitioning diabetes self-management to their adolescent | Semistructured interviews | 40 parents of children age 16-18 y | Parents’ negative experiences involving struggle, frustration, and worry can inhibit their adolescents’ transition to self-management. Reminders, positive recognition, and granting freedom can support transition to self-management, whereas scolding, judging, checking, nagging, and becoming emotional can hinder it. |
| Fornasini et al 47 (2020) | Synthesize what is known about the consequences of T1DM onset for families | Database search | Children age 3-18 y | Parents share educational responsibilities for teaching T1DM plans, with mothers having a predominant role and fathers often absent. |
| Goethals et al 48 (2020) | Examine the role of autonomy-supportive communication by providers and parents and how they interact in the prediction of diabetes outcomes | Questionnaire | 135 participants age 11-18 y, 171 mothers, and 121 fathers | Autonomy-supportive communication by health care professionals and parents are associated with better engagement in the transition to self-management of T1DM. |
| Goethals et al 54 (2021) | Assess the changes in perceived readiness for independent self-care in teens with T1DM from both teens’ and parents’ perspectives | Questionnaire and interview | 178 participants age 13-17.5 y, 178 parents | Adolescents feel more ready for transition to self-management than parents perceive, but this readiness doesn’t immediately translate to better self-care and optimal A1C. |
| Hanna and Hansen 37 (2020) | Insight into understanding T1DM self-management among emerging adults experiencing transitions | Semistructured interview | 25 participants age 19-26 y | Social support, stress, conduciveness of environment, stigma, and self-reliance were identified as influential factors to T1DM management. |
| Hanna et al 49 (2013) | Explore parental diabetes-specific autonomy support experienced by adolescents with T1DM and their parents | Path analysis | 89 participants age 12-18 y | Parents’ autonomy-supportive approach to T1DM management is crucial for adolescents to accept sharing of diabetes tasks. Both parents’ and adolescents’ perspectives are important to consider. |
| Holtz et al 50 (2020) | Explore adolescents’ and their parents’ perspectives on the transition from parent management to team management of T1DM | Semistructured interviews | 12 participants age 13-22 y, 9 parents | Resources, such as parent involvement, communication with health care professionals, education, and social support, to address perceived fears should be the focus for developing interventions that aim to increase coping skills during transition. |
| Ingersgaard et al 38 (2021) | Explore young peoples’ perceptions of living with T1DM | Workshops | 19 participants age 15-25 y | Transition leads to family conflict because parental involvement may be perceived as intrusive, not collaborative. This may harm T1DM care, reducing engagement and optimal A1C targets. |
| Kelly et al 39 (2018) | Examine how “transition readiness” skills develop from relationship processes with parents, friends, and health care providers | Surveys | 242 participants age 17.77 y, on average | Relationships with health care professionals and friends may facilitate transition skills for adolescents. |
| Miller et al 51 (2013) | Investigate the relation of changes in executive functioning to changes in diabetes self-management of youth with T1DM and their maternal caregivers | Quantitative | Children age 9-11 y | Positive changes in behaviors may enhance self-management of T1DM during transition. |
| Overgaard et al 55 (2020) | Explore daily life with T1DM in families with an adolescent with T1DM | Workshops | 20 participants age 8-18 y, 29 parents, 10 siblings | Three themes characterized family life during the transition to self-management of T1DM: perpetual challenges, diverse worries, and diabetes autonomy. All family members’ lives were affected by these aspects, but to varying degrees. |
| Pals et al 18 (2021) | Explore how children with T1DM perceive, make sense of, and handle diabetes technologies in their everyday lives | Semistructured interviews with photo elicitation | 18 participants age 10-14 y | T1DM technology creates tensions regarding dependence and independence and control. |
| Pihlaskari et al 40 (2018) | Examine longitudinal associations of perceived diabetes-specific peer support for adolescents during transition | Surveys | 211 participants age 17.77 y, on average | T1DM peer support in high school predicted better engagement across time. |
| Pritlove et al 41 (2020) | Explore the experiences, perspectives, and needs of parents of emerging adults living with T1DM during the transition phase | Semistructured interviews | 16 parents of children age 18-24 y | Parents stay involved during the transition to self-management during emerging adulthood, causing a renegotiation of responsibilities that can be challenging and provoke fear and worry. |
| Ramchandani et al 42 (2019) | Explore developmental, situational, and organizational challenges experienced by emerging adults with T1DM | Focus groups and interviews | 21 participants age 18-29 y | Finding balance between T1DM and life, desire for T1DM control, hidden burden of T1DM, and desire for a connection with health care professionals are challenges adolescents faced during transition to self-management. |
| Rasmussen et al 4 (2011) | Identify life transitions likely to impact diabetes self-care among young adults with T1DM and their coping strategies during transition events | Semistructured interviews | 20 participants age 18-38 y | Strategic thinking and planning transition to self-management by self-negotiation, managing T1DM with past experience, connecting with others with T1DM, actively seeking information, and putting T1DM into perspective were used by study participants. |
| Smaldone and Ritholz 57 (2011) | Explore perceptions of psychosocial adaptations in parenting children with T1DM | Semistructured interviews | 14 parents of adolescents with T1DM diagnosed at age ≤5 y | Developmentally appropriate delegation of responsibility and support for adolescents in the transition to self-management should occur through ongoing conversations while still under parental guidance. |
| Sparud-Lundin et al 52 (2010) | Explore the meaning of interactions with and supports of self-management from parents and other significant others for young adults with T1DM | Intensive interviews and internet communication | 13 participants age 20-22 y, 13 parents | Transition is a relational and reflexive process leading to ongoing redefinition of relationships and identity. Parents were perceived as the most reliable supporters compared to partners, siblings, and other significant others. |
| Strand et al 43 (2019) | Explore how adolescents perceive the transition from being dependent on their parents to managing their own diabetes | Semistructured interviews | 18 participants age 16-18 y | Adolescents want to self-manage T1DM, but they need more knowledge, skills, and support from parents, friends, and health care professionals because the transition process is burdensome. |
| Sullivan-Bolyai et al 53 (2014) | Describe the perspectives of teens and their parents about self-management of T1DM | Focus groups and interviews | 10 participants age 13-17 y, 13 parents | Guidance in partnership should be positive and encouraging, aiming for interdependence, where the goal is “striking a balance but still in the driver’s seat.” |
| Tomette et al 58 (2020) | Examine parental and caregiver distress among families caring for children with T1DM as the child transitions into emerging adulthood | Semistructured interviews | 19 parents/caregivers of adolescents age 19.2 y, on average | The effects of the transition to self-management are detrimental not only to the adolescent well-being but also to their parents and other family caregivers. |
| Trudeau et al 44 (2019) | Describe the gradual shift of developmentally appropriate tasks and experiences over the transition from parental management to shared management to interdependent management | Journaling | 2 participants age 18-19 y | With parents serving as diabetes self-management coaches to adolescents, an interdependent relationship is built. |
| Tuohy et al 45 (2019) | Meta-synthesis of the experiences and perceptions of self-management of T1DM children and young people | Database search | Children age 8-18 y | The role of others in promoting transition of self-management responsibilities and their reactions can impact the success of the transition and the individual’s perceived control of T1DM. |
Abbreviation: T1DM, type 1 diabetes.
Table 4.
Summary Table of Themes and Subthemes
| Theme | Subtheme including article from which data were retrieved |
|---|---|
| Theme 1: Devolved agency | Accommodating normalcy through self-invisibility4,15,25-28,31,34,35,37-39,44,49
Rehearsal and preparation26,30,35,37,47 |
| Theme 2: Relational autonomy | Interdependencies15,25,26,28,29,31,33,34,36-40,42,45,46,48,50,51 |
The selected studies (n = 29) that examined the experiences of transition to self-management of T1DM for adolescents, parents, siblings, and health care professionals are summarized in Table 3. Recurrent core themes identified as effective ways to understand and ease the transition to self-management of T1DM were devolved agency and relational autonomy. Studies were included in more than 1 theme.
Devolved Agency
This theme relates to having ownership over one’s self-management, based on factual and experiential knowledge that facilitates meaningful choices in life. Agency embodies the dynamic and complex nature of personal development construct through self-negotiation59,60 during the transition to self-management of T1DM, specifically the significant differences in management decisions and practices by adolescents, their families, and health care professionals. This reflects on adolescents’ key decision-making and problem-solving abilities that personalize and enhance the transition from parental management so they may direct their self-management, a process that is intuitive and gradually learned. The concept of agency assumes significance when taking into account the many factors that impact the transition to self-management of T1DM. Adolescents’ autonomy conflicts with a target-driven medical culture that can place unrealistic expectations on maintenance of A1C levels and less focus on supporting agency.4,18,33-35,37,38,41-46,51,54,56 A high level of agency was shown to have strong implications on successful self-management of T1DM, specifically when adolescents integrate the condition within their identity without letting it dominate their lives.34,35,38,42,43,45,46,51,56 Two key subthemes emerge in relation to how adolescents obtain ownership over their own self-management: accommodating normalcy through self-invisibility and rehearsal and preparation.
Accommodating normalcy through self-invisibility
In accordance with diabetes language recommendations, 61 the term “normalcy” in the context of this review refers to the desire to live as a person without diabetes. This includes not being restricted by diabetes management routines (eg, balancing carbohydrate intake during social contexts) and being treated equally to peers without diabetes. 62 One of the motivating factors that appears to influence optimal transition to self-management of T1DM is achieving a balance between normalcy and self-management requirements, a key aspect of which is acceptance of the condition. Normalcy and acceptance of T1DM were reported in 7 studies to play an important part of overcoming the barriers that accompany the transition from parental management to self-management of T1DM as it encourages adolescents to maintain a high level of autonomy.4,18,32,35,38,42,44,45,56 Participants in 9 studies reported employing various methods gained through dedicated trial and error to avoid the psychological burden of this transition, for example, sacrificing perfect A1C over other daily momentary priorities.4,18,33-35,41,42,44,46,51 Accommodating normalcy through making T1DM temporarily “invisible” is highlighted by adolescents’ and parents’ decision to maintain elevated blood glucose levels in certain situations. Adolescents admitted to purposely allowing their blood glucose levels to be elevated in situations such as partying, work responsibilities, driving a car, and practicing a sport, as reported in the study conducted by Ramchandani et al. 42 Parents also encouraged and justified these types of decisions even though many feared that adequate help would not be available from those around the adolescent if needed. 46 Therefore, agency allows for decision-making capacities that minimizes the impact of the transition to self-management of T1DM on the adolescents’ life in certain situations, such as accommodating adolescents’ “fitting in” or assimilating with their peers and social contexts.38,42,43,46,56
Rehearsal and preparation
Rehearsal and preparation refers to gradual introductions of T1DM management requirements as a strategy to support and facilitate the transition to self-management. Although the awareness and desire to leave behind parental and professional management of T1DM may be prompted by developmental changes associated with life transitions, early preparation with encouragement from a significant network of support (ie, family members, friends, work colleagues, and significant others) is required for a successful transition to occur.33,37,44 In 3 studies, a network of support was discussed positively and negatively in association with transition to self-management of T1DM.33,37,42 An early evolving sense of agency over the management of T1DM can benefit adolescents, whereas those who lack agency may experience depression, stress, and anxiety. 46 Trudeau et al 44 found that adolescents and their family members would implement hypothetical situations, “what-if scenarios,” for example, from early diagnosis of T1DM. These are situations that may occur while the adolescent is away from home and were reviewed so the adolescent can gradually develop the agency necessary for the near future. This provides safe opportunities for agency development so the adolescents can be prepared for potential emergencies and develop their own strategies as they transition to self-management. Rehearsal and preparation for transition should begin in early T1DM diagnosis, keeping in mind age-appropriate developmental stages and individualized skills, as suggested through this finding. Goethals et al 54 discussed that although early preparation may facilitate transition from parental management, it does not ensure that A1C targets will be attained over time. While parents acknowledged their child’s increasing agency, many instances of interdependence, where adolescents manage T1DM with parental and medical professional guidance as needed, were described. This led to the next theme, which was emphasized across various studies: relational autonomy, where the formation of agency identities (eg, adolescent’s belief in their capacities) is manifested within networks of support.
Relational Autonomy
The transition to self-management of T1DM can be seen from a relational perspective, where the experiences of transition for adolescents, their families, and health care professionals are interconnected and interdependent. Relational autonomy states that adolescents live in contexts where they are embedded in networks of support, referring to social networks that are central to adolescents’ developmental advance, and challenges the concept of autonomy.63,64 In the context of this review, this theme relates to parents’ continuous role of overseeing T1DM management while promoting that adolescents take on primary responsibility for management plans, often referred to as interdependence and shared responsibility.18,32,33,35,36,38,40,41,43,44,46,47,49,52,53,55,57,58
Interdependencies
As adolescents move toward self-management of T1DM, interdependence was presented as an antecedent to full autonomy.18,44,47,49 This implies that full unsupported independence in terms of T1DM is the goal, particularly from a medical perspective. However, Sullivan-Bolyai et al 53 argued that the goal for a successful transition to take place should be interdependence rather than independence. Interdependence was defined in other included studies as teamwork, partnership, co-management, and collaborative practice, with parents perceived as the most reliable guides.45,52,55,57 Adolescents’ perspectives on the transition to self-management of T1DM revealed that although adolescents wanted to independently manage their diabetes and were aware of their abilities, they required ongoing guidance and support.43,52 Although there is a lack of studies regarding interdependence in the transition to self-management, findings from Hanna et al 49 showed interdependence to be essential in preparing for transition from early diagnosis. On the other hand, Trudeau et al 44 argued that interdependence is a goal for late adolescence, although early preparation is encouraged. Despite contradictions regarding when interdependence occurs in the 2 included studies mentioned here, age is not addressed in previous literature regarding networks of support as a significant factor in the improvement of A1C levels during the transition to self-management.65,66
The transition to self-management of T1DM has proven to be a negotiated process between adolescents and parents based on parents’ perceptions of adolescents’ agency in all aspects of their lives. Gender also appears to be a dimension that has an impact41,44,45 and is an important factor in adolescents’ agency during life transitions.60,67,68 While parents and adolescents recognize the importance of interdependence, many expressed that gender may intersect with interdependence, specifically for young men.41,42 Participants from studies conducted by Pritlove et al 41 and Ramchandani et al 42 highlighted that young men could be more vulnerable to unsafe T1DM self-management due to social constructions of masculinity. Barriers to fully acknowledge interdependence include masculinized identity of being tough, in command, and self-reliant. 41
Adolescent and parent participants also reported that management of T1DM was a shared responsibility of supportive collaboration, where final decisions are made by adolescents.33,41,44,55 Shared responsibility between adolescents and parents leads to desirable self-management of T1DM, defined here as a process that includes both medical and positive psychological outcomes, such as higher quality of life and satisfaction, which suggests that greater parental support is fundamental for adolescents’ transition to self-management and autonomy development.39,46-49,65,69 Compared to adolescents with parental support, Fornasini et al 47 reported worse self-management of T1DM among adolescents with less parental support. Considering this within the family setting, Hanna et al 49 tested the importance of parental support and shared responsibility in interdependence for T1DM management. Findings show that parental support is essential to shared responsibility and may promote adolescents’ acceptance of interdependence while encouraging the transition to self-management of T1DM.35,45,48,49 Adolescent and parent participants agree with the findings mentioned, however excessive parental support has a detrimental effect on adolescents’ ability to self-manage.32,49 To avoid this, shared responsibility should be appropriate and allow for adolescents to build trust and reduce the need for parental support and oversight.
Findings also reported that shared responsibility and the use of technology are integral factors that facilitate interdependence.33,41,44,55 Thus, adolescents are also interdependent on several technologies that contribute to a sense of autonomy in their everyday lives.42,44,50 Technology plays a key role in supporting adolescent agency, but it also contributes to conflict and tensions in interdependence due to the opportunities that technology creates for ongoing parental monitoring. 18 Discrepant perspectives regarding these conflicts may reflect adolescents’ desired autonomy.18,36,45,49 Adolescents experience mixed emotions regarding A1C levels being monitored by parents, such as relief, security, and resentment due to continuous monitoring, access to blood glucose levels, and having to explain why they did not achieve A1C targets, which may be due to various unexplainable factors such as mood. Whereas for parents, monitoring of A1C entails reaching targets rather than meeting adolescents’ specific emotional needs at the time.18,42,47,50 The increasing use of continuous glucose monitor technology has enabled parents to monitor their child’s real-time glycemic control. However, it remains unclear whether this is a facilitator or barrier for the transition to self-management.
Four studies reported the transition to self-management of T1DM to be primarily a family affair rather than a medical one.38,47,53,55 This may explain the lack of studies (n = 0) in this review that explored health care professionals’ perspectives of this transition. Overgaard et al 55 found that many studies have not examined the perspectives of siblings, including an existing lack of role clarification, which has often resulted in siblings being overlooked during the transition to self-management. The analysis from Overgaard et al 55 shows that the transition to self-management of T1DM can be disruptive and challenging for all family members in varying degrees and ways, including siblings. Although not included in the search string of this systematic literature review, 9 studies have analyzed interdependence in the context of others included in the adolescents’ networks of support, such as school nurse, peers, significant others, internet-based peers, and extended family.37,39,40,43-45,50,52,53,57
Discussion
In this systematic literature review, we identified themes that are significant to the transition to self-management of T1DM. The study focused on examining the available evidence concerning adolescents’ experiences of this transition and the experiences of their parents, siblings, and health care professionals. To achieve this, a narrative synthesis was undertaken. Few studies (n = 29) met the inclusion criteria, emphasizing the paucity of research on effective approaches to supporting and facilitating this transition. Devolved agency and relational autonomy emerge as essential antecedents of the transition to self-management of T1DM, which echoes the definition of the transition to self-management by Karlsson et al 70 (p565) as a “hovering between individual actions and support of others.” It also aligns with the definition of healthy transitions by Meleis et al, 71 which are characterized as achieving a subjective sense of well-being, mastery, and well-being of interpersonal relationships. Critically, findings indicate that the transition to self-management does not anticipate that A1C targets are attained; rather, it strives to resist the medical systems’ pressure and to focus instead on achieving better quality of life for adolescents.
Many adolescents desire to lead their life similar to peers without T1DM during the transition to self-management. 72 The reality of daily living, however, is interfered with by the ever-present requirements of T1DM. Adolescents and their families therefore engage in a delicate balancing act between these requirements and leading a healthy life by allowing the adolescents’ devolved agency to accommodate normalcy and a sense of self. Frustrations with striving for normalcy have been identified as one of the most difficult barriers to successful transition. 42 The fear of diabetes-related stereotypes and not fitting in with peers combined with the ongoing burden of T1DM management can lead to a sense of disruption and create barriers for adolescents seeking to live a balanced life. Findings from this review show that accommodating normalcy is attainable through age-appropriate devolved agency in the negotiation of situations that may be deemed important to the adolescent. In line with this finding, Spaans et al 73 suggests that adolescents are better prepared for the transition to self-management once a certain level of agency has been established to the satisfaction of their families and health care professionals as well.
This review found that rehearsal and preparation for the transition to self-management should be tailored to the adolescents’ needs and comfort level.4,74 Preparation for transition should begin as early as diagnosis because it allows adolescents to develop agency in many factors that influence self-management of T1DM rather than just at the time of transition. Previous research on the transfer from pediatric to adult care services, which often occurs in parallel to the transition from parental management to self-management, has also found that rehearsal and preparation is a useful strategy to improve self-management competencies through awareness of the condition and its potential outcomes. 75 Future research should explore and identify concrete strategies developed by adolescents and their available networks of support that may facilitate rehearsal and preparation for this transition while also undergoing a set of other life transitions.
A key finding from this review shows that the transition to self-management is considered a family affair.38,47,53,55 This often entails conscious efforts from networks of support to increase adolescents’ autonomy in self-management while anticipating psychosocial adaptations that may occur. Networks of support are vital in facilitating effective communication with adolescents, shared decision-making, and a supportive environment, ultimately contributing to a successful transition. Discussions concerning the impact of overprotection from networks of support, particularly parental support, on the quality of life of adolescents are recommended. Drawing on this finding, it appears that overprotection can hinder adolescents’ autonomy and lead to a decreased quality of life. Thus, open discussions about the effects of overprotection can help create an optimal environment that will encourage transition to self-management and promote adolescents’ overall well-being.
Aiming toward interdependence, rather than independence, has proven crucial to avoid negative consequences, such as deteriorating A1C.76-79 Findings from this review suggest that interdependence may be more beneficial in facilitating the transition to self-management of T1DM. Consistent with the current finding, Farthing et al 66 showed that although adolescents age and mature, an interdependent approach rather than an independent endeavor is necessary from early diagnosis of T1DM to prepare for transition. Interdependence in self-management of T1DM occurs in the context of everyday social relations where “individuals influence each other’s outcomes in the course of their interaction.” 80 (p3) This concept differs from the fully independent approach employed by the health care system in the transition to self-management. As such, health care professionals should consider adopting an interdependent approach in supporting adolescents living with T1DM and their families. The study by Weissberg-Benchell et al 78 concluded that adolescents who were fully independent made more errors in managing T1DM than those who were interdependent. Thus, responsibilities and obligations with networks of support should be renegotiated in a flexible way to avoid the extremes of overprotection or lack of involvement during transition. Future research should further investigate the concept of interdependencies within networks of support in the transition to self-management of T1DM because it has been shown to facilitate and ease the transition for adolescents and their families.
Limitations
Although the findings of this systematic literature review suggest important factors that may facilitate and ease the transition from parental management to self-management of T1DM, a few limitations do exist. First, factors including A1C measurements, age of diagnosis, family composition, socioeconomic status, and insurance coverage were not available in all the studies. Most studies did not assess self-management responsibilities performed by the adolescents and those by their parents or caregivers. Second, the search string of this review did not include experiences of all members of the adolescents’ network of support, such as extended family, school teachers and nurses, friends, and significant others. Finally, only peer-reviewed studies in the English language were included.
Conclusion
In conclusion, this review highlights the importance of agency and relational autonomy factors as adolescents transition from parental management to self-management of T1DM. The transition was shown to be complex due to a combination of factors associated with developmental life transitions. The findings reported to have implications for further research are accommodating normalcy through self-invisibility, rehearsal and preparation, and interdependencies in the transition to self-management. This review focuses directly on adolescents’ with T1DM, their families, and health care professionals’ experiences of transition; however, future research should focus on the experiences of all associated in the adolescents’ network of support.
Supplemental Material
Supplemental material, sj-docx-1-tde-10.1177_26350106231206779 for Adolescents’ Experiences of Transition to Self-Management of Type 1 Diabetes: Systematic Review and Future Directions by Paula Leocadio, Carol Kelleher, Eluska Fernández and Colin P. Hawkes in The Science of Diabetes Self-Management and Care
Footnotes
There are no relevant conflicts of interest.
Funding: The authors wish to acknowledge Cork University Hospital Charity (CUH Charity) for funding this research, an organization which actively supports life-saving and life-changing services for patients. Further acknowledgment to the Department of Management and Marketing at Cork University Business School (CUBS), University College Cork (UCC) and the School of Applied Social Studies, UCC, for additional PhD scholarship support.
ORCID iDs: Paula Leocadio  https://orcid.org/0000-0002-1379-2006
https://orcid.org/0000-0002-1379-2006
Colin P. Hawkes  https://orcid.org/0000-0001-6484-0445
https://orcid.org/0000-0001-6484-0445
Supplemental Material: Supplemental material is available online with this article.
Contributor Information
Paula Leocadio, Department of Management and Marketing, University College Cork, Cork, Ireland.
Carol Kelleher, Department of Management and Marketing, University College Cork, Cork, Ireland.
Eluska Fernández, School of Applied Social Studies, University College Cork, Cork, Ireland.
Colin P. Hawkes, Department of Paediatrics and Child Health, University College Cork, Cork, Ireland; INFANT Research Centre, University College Cork, Cork, Ireland; Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, United States.
References
- 1. Patterson CC, Karuranga S, Salpea P, et al. Worldwide estimates of incidence, prevalence and mortality of type 1 diabetes in children and adolescents: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107842. doi: 10.1016/j.diabres.2019.107842 [DOI] [PubMed] [Google Scholar]
- 2. Kelly CS, Berg CA. Close relationships and diabetes management across the lifespan: the good, the bad, and autonomy. J Health Psychol. 2021;26(2):226-237. doi: 10.1177/1359105318805815 [DOI] [PubMed] [Google Scholar]
- 3. Schilling LS, Dixon JK, Knafl KA, et al. A new self-report measure of self-management of type 1 diabetes for adolescents. Nurs Res. 2009;58(4):228-236. doi: 10.1097/NNR.0b013e3181ac142a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rasmussen B, Ward G, Jenkins A, King SJ, Dunning T. Young adults’ management of type 1 diabetes during life transitions. J Clin Nurs. 2011;20(13-14):1981-1992. doi: 10.1111/j.1365-2702.2010.03657.x [DOI] [PubMed] [Google Scholar]
- 5. Hermann JM, Miller KM, Hofer SE, et al. The Transatlantic HbA1c gap: differences in glycaemic control across the lifespan between people included in the US T1D Exchange Registry and those included in the German/Austrian DPV registry. Diabet Med. 2020;37(5):848-855. doi: 10.1111/dme.14148 [DOI] [PubMed] [Google Scholar]
- 6. Funnell MM, Anderson RM. Empowerment and self-management of diabetes. Clin Diabetes. 2004;22(3):123-127. doi: 10.2337/diaclin.22.3.123 [DOI] [Google Scholar]
- 7. Brown SA. Interventions to promote diabetes self-management: state of the science. Diabetes Educ. 1999;25(suppl 6):52-61. doi: 10.1177/014572179902500623 [DOI] [PubMed] [Google Scholar]
- 8. Nguyen T, Henderson D, Stewart D, Hlyva O, Punthakee Z, Gorter JW. You never transition alone! Exploring the experiences of youth with chronic health conditions, parents and healthcare providers on self-management. Child Care Health Dev. 2016;42(4):464-472. doi: 10.1111/cch.12334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sattoe JNT, van Staa A, Hilberink SR, eds. Self-Management of Young People With Chronic Conditions: A Strength-Based Approach for Empowerment and Support. Springer International Publishing; 2021. doi: 10.1007/978-3-030-64293-8 [DOI] [Google Scholar]
- 10. Fritsch M, Rosenbauer J, Schober E, et al. Predictors of diabetic ketoacidosis in children and adolescents with type 1 diabetes. Experience from a large multicentre database. Pediatr Diabetes. 2011;12(4, pt 1):307-312. doi: 10.1111/j.1399-5448.2010.00728.x [DOI] [PubMed] [Google Scholar]
- 11. Zhang L, Krzentowski G, Albert A, Lefebvre PJ. Risk of developing retinopathy in Diabetes Control and Complications Trial type 1 diabetic patients with good or poor metabolic control. Diabetes Care. 2001;24(7):1275-1279. doi: 10.2337/diacare.24.7.1275 [DOI] [PubMed] [Google Scholar]
- 12. Duca LM, Wang B, Rewers M, Rewers A. Diabetic ketoacidosis at diagnosis of type 1 diabetes predicts poor long-term glycemic control. Diabetes Care. 2017;40(9):1249-1255. doi: 10.2337/dc17-0558 [DOI] [PubMed] [Google Scholar]
- 13. Laing SP, Jones ME, Swerdlow AJ, Burden AC, Gatling W. Psychosocial and socioeconomic risk factors for premature death in young people with type 1 diabetes. Diabetes Care. 2005;28(7):1618-1623. doi: 10.2337/diacare.28.7.1618 [DOI] [PubMed] [Google Scholar]
- 14. Thomas MC. Glycemic exposure, glycemic control, and metabolic karma in diabetic complications. Adv Chronic Kidney Dis. 2014;21(3):311-317. doi: 10.1053/j.ackd.2014.03.004 [DOI] [PubMed] [Google Scholar]
- 15. Insabella G, Grey M, Knafl G, Tamborlane W. The transition to young adulthood in youth with type 1 diabetes on intensive treatment. Pediatr Diabetes. 2007;8(4):228-234. doi: 10.1111/j.1399-5448.2007.00266.x [DOI] [PubMed] [Google Scholar]
- 16. Ersig AL. An exploratory study: transition to adulthood for college students with type 1 diabetes and their parents. J Pediatr Nurs. 2019;46:12-17. doi: 10.1016/j.pedn.2019.01.008 [DOI] [PubMed] [Google Scholar]
- 17. Rasmussen B, O’Connell B, Dunning P, Cox H. Young women with type 1 diabetes’ management of turning points and transitions. Qual Health Res. 2007;17(3):300-310. doi: 10.1177/1049732306298631 [DOI] [PubMed] [Google Scholar]
- 18. Pals RAS, Hviid P, Cleal B, Grabowski D. Demanding devices—living with diabetes devices as a pre-teen. Soc Sci Med. 2021;286:114279. doi: 10.1016/j.socscimed.2021.114279 [DOI] [PubMed] [Google Scholar]
- 19. Garvey KC, Beste M, Luff D, Atakov-Castillo A, Wolpert H, Ritholz M. Experiences of health care transition voiced by young adults with type 1 diabetes: a qualitative study. Adolesc Health Med Ther. 2014;5:191-198. doi: 10.2147/AHMT.S67943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. The BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stillwell SB, Fineout-Overholt E, Melnyk BM, Williamson KM. Evidence-based practice, step by step: asking the clinical question: a key step in evidence-based practice. Am J Nurs. 2010;110(3):58-61. doi: 10.1097/01.NAJ.0000368959.11129.79 [DOI] [PubMed] [Google Scholar]
- 22. Morrison A, Polisena J, Husereau D, et al. The effect of English-language restriction on systematic review-based meta-analysis: a systematic review of empirical studies. Int J Technol Assess Health Care. 2012;28(2):138-144. doi: 10.1017/S0266462312000086 [DOI] [PubMed] [Google Scholar]
- 23. Hartling L, Featherstone R, Nuspl M, Shave K, Dryden DM, Vandermeer B. Grey literature in systematic reviews: a cross-sectional study of the contribution of non-English reports, unpublished studies and dissertations to the results of meta-analyses in child-relevant reviews. BMC Med Res Methodol. 2017;17(1):64. doi: 10.1186/s12874-017-0347-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nussbaumer-Streit B, Klerings I, Dobrescu AI, et al. Excluding non-English publications from evidence-syntheses did not change conclusions: a meta-epidemiological study. J Clin Epidemiol. 2020;118:42-54. doi: 10.1016/j.jclinepi.2019.10.011 [DOI] [PubMed] [Google Scholar]
- 25. Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews. Published January 4, 2006:92. Accessed July 10, 2022. http://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf
- 26. Clarke V, Braun V. Thematic analysis. J Posit Psychol. 2017;12(3):297-298. doi: 10.1080/17439760.2016.1262613 [DOI] [Google Scholar]
- 27. Clarke V, Braun V. Toward good practice in thematic analysis: avoiding common problems and be(com)ing a knowing researcher. Int J Transgender Health. 2023;24(1):1-6. doi: 10.1080/26895269.2022.2129597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Booth A, Sutton A, Papaioannou D. Systematic Approaches to a Successful Literature Review. 2nd ed. Sage; 2016. [Google Scholar]
- 29. Hong QN, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). J Eval Clin Pract. 2018;24(3):459-467. [DOI] [PubMed] [Google Scholar]
- 30. Madden A, Bailey C, Alfes K, Fletcher L. Using narrative evidence synthesis in HRM research: an overview of the method, its application, and the lessons learned. Hum Resour Manage. 2018;57(2):641-657. doi: 10.1002/hrm.21858 [DOI] [Google Scholar]
- 31. Cronin P, Ryan F, Coughlan M. Undertaking a literature review: a step-by-step approach. Br J Nurs. 2008;17(1):38-43. doi: 10.12968/bjon.2008.17.1.28059 [DOI] [PubMed] [Google Scholar]
- 32. Babler E, Strickland CJ. Moving the journey towards independence: adolescents transitioning to successful diabetes self-management. J Pediatr Nurs. 2015;30(5):648-660. doi: 10.1016/j.pedn.2015.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chiang YT, Yu HY, Lo FS, et al. Emergence of a butterfly: the life experiences of type 1 diabetes Taiwanese patients during the 16-25 years old transition period. Int J Qual Stud Health Well-Being. 2020;15(1):1748362. doi: 10.1080/17482631.2020.1748362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chilton R, Pires-Yfantouda R. Understanding adolescent type 1 diabetes self-management as an adaptive process: a grounded theory approach. Psychol Health. 2015;30(12):1486-1504. doi: 10.1080/08870446.2015.1062482 [DOI] [PubMed] [Google Scholar]
- 35. Collet N, Batista AFMB, Nóbrega VMD, Souza MHDN, Fernandes LTB. Self-care support for the management of type 1 diabetes during the transition from childhood to adolescence. Rev Esc Enferm U P. 2018;52:e03376. doi: 10.1590/S1980-220X2017038503376 [DOI] [PubMed] [Google Scholar]
- 36. Dashiff C, Riley BH, Abdullatif H, Moreland E. Parents’ experiences supporting self-management of middle adolescents with type 1 diabetes mellitus. Pediatr Nurs. 2011;37(6):304-310. [PubMed] [Google Scholar]
- 37. Hanna KM, Hansen JR. Habits and routines during transitions among emerging adults with type 1 diabetes. West J Nurs Res. 2020;42(6):446-453. doi: 10.1177/0193945919882725 [DOI] [PubMed] [Google Scholar]
- 38. Ingersgaard MV, Hoeeg D, Willaing I, Grabowski D. An exploratory study of how young people experience and perceive living with type 1 diabetes during late adolescence and emerging adulthood. Chronic Illn. 2021;17(4):475-492. doi: 10.1177/1742395319886487 [DOI] [PubMed] [Google Scholar]
- 39. Kelly CS, Berg CA, Ramsey MA, et al. Relationships and the development of transition readiness skills into early emerging adulthood for individuals with type 1 diabetes. Child Health Care. 2018;47(3):308-325. doi: 10.1080/02739615.2017.1354294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pihlaskari AK, Wiebe DJ, Troxel NR, Stewart SM, Berg CA. Perceived peer support and diabetes management from adolescence into early emerging adulthood. Health Psychol. 2018;37(11):1055-1058. doi: 10.1037/hea0000662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pritlove C, Markowitz B, Mukerji G, Advani A, Parsons JA. Experiences and perspectives of the parents of emerging adults living with type 1 diabetes. BMJ Open Diabetes Res Care. 2020;8(1):e001125. doi: 10.1136/bmjdrc-2019-001125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ramchandani N, Way N, Melkus GD, Sullivan-Bolyai S. Challenges to diabetes self-management in emerging adults with type 1 diabetes. Diabetes Educ. 2019;45(5):484-497. doi: 10.1177/0145721719861349 [DOI] [PubMed] [Google Scholar]
- 43. Strand M, Broström A, Haugstvedt A. Adolescents’ perceptions of the transition process from parental management to self-management of type 1 diabetes. Scand J Caring Sci. 2019;33(1):128-135. doi: 10.1111/scs.12611 [DOI] [PubMed] [Google Scholar]
- 44. Trudeau B, Trudeau C, Polfuss ML, Sullivan-Bolyai S. A developmental milestones map of type 1 diabetes self-management transition from parents to adolescents. Diabetes Spectr Publ Am Diabetes Assoc. 2019;32(1):21-29. doi: 10.2337/ds18-0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tuohy E, Rawdon C, Gallagher P, et al. Children and young people’s experiences and perceptions of self-management of type 1 diabetes: a qualitative meta-synthesis. Health Psychol Open. 2019;6(2):2055102919877105. doi: 10.1177/2055102919877105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Castensøe-Seidenfaden P, Teilmann G, Kensing F, Hommel E, Olsen BS, Husted GR. Isolated thoughts and feelings and unsolved concerns: adolescents’ and parents’ perspectives on living with type 1 diabetes—a qualitative study using visual storytelling. J Clin Nurs. 2017;26(19-20):3018-3030. doi: 10.1111/jocn.13649 [DOI] [PubMed] [Google Scholar]
- 47. Fornasini S, Miele F, Piras EM. The consequences of type 1 diabetes onset on family life. An integrative review. J Child Fam Stud. 2020;29(5):1467-1483. doi: 10.1007/s10826-019-01544-z [DOI] [Google Scholar]
- 48. Goethals ER, Jaser SS, Verhaak C, et al. Communication matters: the role of autonomy-supportive communication by health care providers and parents in adolescents with type 1 diabetes. Diabetes Res Clin Pract. 2020;163:108153. doi: 10.1016/j.diabres.2020.108153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hanna KM, Dashiff CJ, Stump TE, Weaver MT. Parent–adolescent dyads: association of parental autonomy support and parent–adolescent shared diabetes care responsibility. Child Care Health Dev. 2013;39(5):695-702. doi: 10.1111/j.1365-2214.2012.01373.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Holtz BE, Mitchell KM, Holmstrom AJ, et al. Teen and parental perspectives regarding transition of care in type 1 diabetes. Child Youth Serv Rev. 2020;110:104800. doi: 10.1016/j.childyouth.2020.104800 [DOI] [Google Scholar]
- 51. Miller MM, Rohan JM, Delamater A, et al. Changes in executive functioning and self-management in adolescents with type 1 diabetes: a growth curve analysis. J Pediatr Psychol. 2013;38(1):18-29. doi: 10.1093/jpepsy/jss100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Sparud-Lundin C, Öhrn I, Danielson E. Redefining relationships and identity in young adults with type 1 diabetes. J Adv Nurs. 2010;66(1):128-138. doi: 10.1111/j.1365-2648.2009.05166.x [DOI] [PubMed] [Google Scholar]
- 53. Sullivan-Bolyai S, Bova C, Johnson K, et al. Engaging teens and parents in collaborative practice: perspectives on diabetes self-management. Diabetes Educ. 2014;40(2):178-190. doi: 10.1177/0145721713520568 [DOI] [PubMed] [Google Scholar]
- 54. Goethals ER, Volkening LK, Tinsley L, Laffel LM. Ready or not? Greater readiness for independent self-care predicts better self-management but not HbA1c in teens with type 1 diabetes. Diabet Med J Br Diabet Assoc. 2021;38(5):e14507. doi: 10.1111/dme.14507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Overgaard M, Lundby-Christensen L, Grabowski D. Disruption, worries and autonomy in the everyday lives of adolescents with type 1 diabetes and their family members: a qualitative study of intrafamilial challenges. J Clin Nurs. 2020;29(23-24):4633-4644. doi: 10.1111/jocn.15500 [DOI] [PubMed] [Google Scholar]
- 56. Bekker CI, Deacon E, Segal D. Meaning in life experienced by parents of children living with diabetes. Health Psychol Open. 2019;6(1):205510291983222. doi: 10.1177/2055102919832221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Smaldone A, Ritholz MD. Perceptions of parenting children with type 1 diabetes diagnosed in early childhood. J Pediatr Health Care. 2011;25(2):87-95. doi: 10.1016/j.pedhc.2009.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Tomette A, Henderson JN, Hass A, Carson LD, King K. Parental stress as a child with diabetes transitions from adolescence to emerging adulthood. J Patient Exp. 2020;7(3):365-371. doi: 10.1177/2374373519842963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Vijayaraghavan J, Vidyarthi A, Livesey A, et al. Strengthening adolescent agency for optimal health outcomes. BMJ. 2022;379:e069484. doi: 10.1136/bmj-2021-069484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Schoon I, Heckhausen J. Conceptualizing individual agency in the transition from school to work: a social-ecological developmental perspective. Adolesc Res Rev. 2019;4(2):135-148. doi: 10.1007/s40894-019-00111-3 [DOI] [Google Scholar]
- 61. Dickinson JK, Guzman SJ, Maryniuk MD, et al. The use of language in diabetes care and education. Diabetes Care. 2017;40(12):1790-1799. doi: 10.2337/dci17-0041 [DOI] [PubMed] [Google Scholar]
- 62. Freeborn D, Dyches T, Roper SO. Lessons learned from a life with type 1 diabetes: adult perspectives. Diabetes Spectr. 2017;30(3):188-194. doi: 10.2337/ds16-0032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Varga SM, Zaff JF. A new framework to advance understanding of relationships and youth development. Published 2017:14. Accessed September 16, 2022. https://americaspromise.org/resources/defining-webs-support-new-framework-advance-understanding-relationships-and-youth/
- 64. Varga SM, Zaff JF. Webs of support: an integrative framework of relationships, social networks, and social support for positive youth development. Adolesc Res Rev. 2018;3(1):1-11. doi: 10.1007/s40894-017-0076-x [DOI] [Google Scholar]
- 65. Anderson BJ, Holmbeck G, Iannotti RJ, et al. Dyadic measures of the parent–child relationship during the transition to adolescence and glycemic control in children with type 1 diabetes. Fam Syst Health. 2009;27:141-152. doi: 10.1037/a0015759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Farthing P, Bally JMG, Leurer MD, Holtslander L, Nour MA, Rennie D. Managing the unmanageable through interdependence in adolescents living with type 1 diabetes and their parents: a constructivist grounded theory. J Pediatr Nurs. 2022;67:e191-e200. doi: 10.1016/j.pedn.2022.07.016 [DOI] [PubMed] [Google Scholar]
- 67. Hurault JC, Broc G, Crône L, Tedesco A, Brunel L. Measuring the sense of agency: a French adaptation and validation of the sense of agency scale (F-SoAS). Front Psychol. 2020;11:584145. doi: 10.3389/fpsyg.2020.584145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Nunes F, Mota CP, Schoon I, Ferreira T, Matos PM. Sense of personal agency in adolescence and young adulthood: a preliminary assessment model. Personal Individ Differ. 2022;196:111754. doi: 10.1016/j.paid.2022.111754 [DOI] [Google Scholar]
- 69. Vesco AT, Anderson BJ, Laffel LMB, Dolan LM, Ingerski LM, Hood KK. Responsibility sharing between adolescents with type 1 diabetes and their caregivers: importance of adolescent perceptions on diabetes management and control. J Pediatr Psychol. 2010;35(10):1168-1177. doi: 10.1093/jpepsy/jsq038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Karlsson A, Arman M, Wikblad K. Teenagers with type 1 diabetes—a phenomenological study of the transition towards autonomy in self-management. Int J Nurs Stud. 2008;45(4):562-570. doi: 10.1016/j.ijnurstu.2006.08.022 [DOI] [PubMed] [Google Scholar]
- 71. Meleis AI, Sawyer LM, Im EO, Messias DAKH, Schumacher K. Experiencing transitions: an emerging middle-range theory. Adv Nurs Sci. 2000;23(1):12-28. doi: 10.1097/00012272-200009000-00006 [DOI] [PubMed] [Google Scholar]
- 72. Sanders T, Elliott J, Norman P, Johnson B, Heller S. Disruptive illness contexts and liminality in the accounts of young people with type 1 diabetes. Sociol Health Illn. 2019;41(7):1289-1304. doi: 10.1111/1467-9566.12906 [DOI] [PubMed] [Google Scholar]
- 73. Spaans EAJM, Kleefstra N, Groenier KH, Bilo HJG, Brand PLP. Adherence to insulin pump treatment declines with increasing age in adolescents with type 1 diabetes mellitus. Acta Paediatr. 2020;109(1):134-139. doi: 10.1111/apa.14931 [DOI] [PubMed] [Google Scholar]
- 74. Schmidt S, Herrmann-Garitz C, Bomba F, Thyen U. A multicenter prospective quasi-experimental study on the impact of a transition-oriented generic patient education program on health service participation and quality of life in adolescents and young adults. Patient Educ Couns. 2016;99(3):421-428. doi: 10.1016/j.pec.2015.10.024 [DOI] [PubMed] [Google Scholar]
- 75. van Staa AL, Jedeloo S, van Meeteren J, Latour JM. Crossing the transition chasm: experiences and recommendations for improving transitional care of young adults, parents and providers: crossing the transition chasm. Child Care Health Dev. 2011;37(6):821-832. doi: 10.1111/j.1365-2214.2011.01261.x [DOI] [PubMed] [Google Scholar]
- 76. Anderson BJ, Auslander WF, Jung KC, Miller JP, Santiago JV. Assessing family sharing of diabetes responsibilities. J Pediatr Psychol. 1990;15(4):477-492. doi: 10.1093/jpepsy/15.4.477 [DOI] [PubMed] [Google Scholar]
- 77. Anderson B, Ho J, Brackett J, Finkelstein D, Laffel L. Parental involvement in diabetes management tasks: relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. J Pediatr. 1997;130(2):257-265. doi: 10.1016/S0022-3476(97)70352-4 [DOI] [PubMed] [Google Scholar]
- 78. Weissberg-Benchell J, Glasgow AM, Tynan WD, Wirtz P, Turek J, Ward J. Adolescent diabetes management and mismanagement. Diabetes Care. 1995;18(1):77-82. doi: 10.2337/diacare.18.1.77 [DOI] [PubMed] [Google Scholar]
- 79. Wysocki T, Taylor A, Hough BS, Linscheid TR, Yeates KO, Naglieri JA. Deviation from developmentally appropriate self-care autonomy: association with diabetes outcomes. Diabetes Care. 1996;19(2):119-125. doi: 10.2337/diacare.19.2.119 [DOI] [PubMed] [Google Scholar]
- 80. Kelley HH, Holmes JG, Kerr NL, Reis HT, Rusbult CE, Van Lange PAM. An Atlas of Interpersonal Situations. Cambridge University Press; 2001. doi: 10.1017/CBO9780511499845 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-tde-10.1177_26350106231206779 for Adolescents’ Experiences of Transition to Self-Management of Type 1 Diabetes: Systematic Review and Future Directions by Paula Leocadio, Carol Kelleher, Eluska Fernández and Colin P. Hawkes in The Science of Diabetes Self-Management and Care