Abstract
This study aimed to provide a comprehensive understanding of the influence of hearing loss on social participation in older adults and including its facilitators and barriers. Following the rigorous methodological framework of scoping studies, nine multidisciplinary databases were searched with 44 keywords. Published mainly in the last decade, 41 studies using primarily a quantitative cross-sectional design were selected. Older adults with hearing loss have been found to have difficulty maintaining relationships and social activities. While social support and engaged-coping strategies were major facilitators of social participation, barriers included greater hearing loss, communication difficulties, comorbidities and reduced mental health. To better promote the social participation of older adults, early detection of hearing loss, holistic assessment, and interprofessional collaboration must be considered. Future research is necessary to better address the stigma related to hearing loss in older adults and challenges of early detection, and to propose innovative solutions to develop interprofessional collaboration.
Keywords: presbycusis, engagement, holistic, interprofessional collaboration, detection, stigma
Introduction
Representing 0.7 billion worldwide in 2019, the number of people aged 65 and older is expected to reach 1.5 billion by 2050 (United Nations [UN], 2019). Increasingly prevalent and affecting almost one older adult out of three (World Health Organization [WHO], 2016), hearing loss has significant consequences in aging societies. Hearing loss is associated with social isolation (Chen, 1994; Palmer et al., 2019), decreased self-esteem (Chen, 1994), depressive symptoms, cognitive and functional decline, and a higher risk of falling (Lopez et al., 2011; Viljanen et al., 2009). In addition to its impacts on the physical, cognitive, mental, and social skills (Cacchione, 2014), uncorrected hearing loss often leads to a significant withdrawal from social activities. A decrease in social activities can affect the quality of life of older adults (Arlinger, 2003; Heine & Browning, 2002), as well as their mental health and well-being (Heine & Browning, 2002). Social participation represents the “person’s involvement in activities that provided interactions with others in community life and in important shared spaces, evolving according to available time and resources, and based on the societal context and what individuals want and is meaningful to them” (Levasseur et al., 2022, p. 8). It is associated with improved health (Gilmour, 2012), well-being (Litwin & Shiovitz-Ezra, 2006), decreased depressive symptoms (Byers et al., 2012), cognitive (Zunzunegui et al., 2003) and functional decline (Avlund et al., 2004), medication use, health service utilization (Bath & Gardiner, 2005), and mortality risk (Gilmour, 2012). Social participation is a key determinant of healthy aging and quality of life, including for older adults with hearing loss.
Levasseur and colleagues (2006) identified five older adults with disabilities quality of life attributes: (i) a sense of satisfaction with life; (ii) a state of physical, psychological, social, and spiritual well-being; (iii) a satisfactory functional state, evidenced by the presence of adaptive behaviors; (iv) a sense of control over one’s life; and (v) the achievement of meaningful occupations, which represents ‘the social, psychological, and spiritual fulfillment of the individual’. The importance of social participation, interactions and networks were also highlighted as factors improving quality of life (Schalock, 2004). Considering that these factors are especially influenced by hearing loss and to improve support of older adults with this condition, it is essential to better understand their social participation and identify its facilitators and barriers.
Although studies have shown that hearing loss influenced social participation in older adults, mixed findings were reported regarding the extent of its impact and the associated factors. While many studies agree that hearing loss in older adults increases the risk of reduced social participation, there is no consensus on the extent of this restriction. According to few studies, no difference was observed in the social participation of older adults with and without hearing loss. Based on these heterogeneous findings, the factors that may explain restriction in social participation of older adults with hearing loss are diverse and occasionally contradictory. Such restriction could be explained by communication impairments (Heine & Browning, 2004; Jang et al., 2003), or fatigue related to the increased cognitive load due to compensation for hearing loss (Arlinger, 2003). One study found that age is the main factor restricting social participation, not hearing impairment (Clark et al., 1999). The influence of hearing loss on social participation could also be related to depressive symptoms (Andrade et al., 2017), low self-esteem (Mikkola et al., 2016; Palmer et al., 2019), or evolution in the support network but no consensus was found on how and which networks were affected (Heffernan et al., 2016; Mikkola et al., 2016; Palmer et al., 2019). According to one study, hearing loss did not affect the quantity but the quality of older adults’ social interactions (Cruice et al., 2005), and a small network might not mean that the person was isolated (Sung et al., 2016). Other studies have highlighted the functional impact of hearing loss, which can lead to a decreased functional independence and restricted social participation in older adults (Gopinath, Schneider, McMahon, et al., 2012; Mikkola et al., 2016). Finally, hearing loss had a differential impact on social participation regarding older women and men, with no consensus on which gender is more influenced (Mick et al., 2014; Pronk et al., 2013; Ramage-Morin, 2016).
Although a growing body of scientific literature examining the impacts of hearing loss on social participation of older adults has been observed since 2010, to our knowledge, no review specific to this topic have been carried out. Among previous reviews, the most recent was published in 2012 (Ciorba et al.), which related to the quality of life of older adults with hearing loss. Since studies were mainly quantitative cross-sectional and defined social participation differently, heterogeneous results complexified integration of knowledge specific to the social participation of older adults with hearing loss. A rigorous, integrative, and comprehensive portrait about social participation of older adults with hearing loss is needed. A systematic integration of results from previous studies is also required to better identify the available evidence, knowledge gaps and future research opportunities (Arksey & O’Malley, 2005; Munn et al., 2018). This study thus aimed to provide a comprehensive and integrated understanding of the influence of hearing loss on social participation in older adults, including its facilitators and barriers. Such understanding may ultimately lead to recommendations to support decisions and the development of innovative interventions, clear guidelines, and best practices regarding social participation in older adults with hearing loss.
Methods
The methodological framework for scoping studies presented by Levac and colleagues in 2010, based on the original methodology of Arksey and O’Malley (2005), was used to synthesize and disseminate current knowledge on the influence of hearing loss on social participation in older adults. This framework consisted of five stages: (1) formulate the research question by clarifying and linking the purpose and research question, (2) identify relevant studies by balancing feasibility with breadth and comprehensiveness, (3) select research using an iterative team approach to study the selections and data extraction, (4) chart the data incorporating numerical summary and qualitative thematic analysis, (5) collate, summarize and report the results, including the implications for policy, practice or research (Levac et al., 2010). To ensure high rigor and replicability, the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) was followed.
Identifying the Research Questions
Three questions were specifically addressed:
1) How does hearing loss influence social participation in older adults?
2) What individual and environmental factors influence the social participation of older adults with hearing loss, and how, i.e. are they facilitators or barriers?
3) What are the recommendations to promote social participation of older adults with hearing loss including knowledge gaps and future research opportunities?
Identifying et Selecting Relevant Studies
Nine multidisciplinary databases in aging and health science (Abstract in social gerontology, Academic search complete, Ageline, APA PsycInfo, CINAHL, Medline, Pubmed, Scopus, SocIndex) were searched using 44 keywords related to social participation, older adults, and hearing loss. These keywords were identified through a search in dictionaries, thesauri, and previous scoping including similar concepts (Courtin & Knapp, 2017; David & Werner, 2016; Levasseur et al., 2022), and validated by a documentalist (Table 1). Studies published in French or English until December 2022 were targeted.
Table 1.
Keywords and Research Strategy.
| Keywords (44) | 1. Participation sociale OR social participation OR social engagement OR social involvement OR social activit* OR participation OR social network* OR social relationship* OR activit* OR social interaction* OR quality of life OR psychosocial OR social functioning OR social disengagement OR loneliness OR social isolation |
| 2. Age* OR aine* OR geronto* OR older adult* OR older people OR elder* OR geriatr* OR aging | |
| 3. Deficien* auditi* OR perte auditive OR difficult* auditiv* OR sourd* OR surd* OR hard of hearing OR hearing impair* OR hearing disabilit* OR hearing loss OR hearing difficult* OR deaf* OR presbyacousie OR presbycusis OR hearing OR sensory loss OR auditory disablement OR hearing status OR communication impairment* OR sensory impairment* OR difficult* communicating |
Research strategy: 1 AND 2 AND 3.
The selection of relevant literature was limited, but not exclusive (retained if results were specific to older adults with disabilities, including older adults with hearing loss), to studies that addressed social participation or psychosocial or behavioral issues of older adults with hearing loss. Due to the challenge of fully considering cultural differences in social participation in national contexts, studies conducted in cultures considerably different from western countries (i.e., China, Japan, Colombia) were excluded. Also, the selected study involved exclusively people living in the community, whose daily functioning, support, and opportunities for participation are different from those of older adults living in a residence. Finally, studies involving only older adults with dual sensory loss (i.e., vision and hearing loss) were excluded.
Two authors (APC & THTN) separately screened the studies. Following PRISMA guideline, the studies were firstly screened by title, abstract and then by full-text based on inclusion and exclusion criteria to determine eligibility (Moher et al., 2009). They regularly met during the screening and selection process to discuss about the eligibility of studies. Due to time constraints (Arksey & O’Malley, 2005), except google scholar, websites were excluded.
Charting the Data, and Collating, Summarizing, and Reporting Results
As suggested by Arksey and O’Malley (2005), the first step involved to record the following information in a data charting form: (a) author(s), year of publication, study location, (b) aim(s) of the study, (c) research methodology, (d) sample size and description, (e) outcome measures, (f) important results, (g) recommendations. A thematic content analysis was then conducted using the Human Development Model – Disability Creation Process (HDM-DCP). This model illustrates the dynamics between personal and environmental factors that influence a person’s social participation (Fougeyrollas, 2019). This model ensures a comprehensive understanding of older adults, their hearing loss and social participation based on the interaction of their personal and environmental factors. The HDM-DCP operationalized social participation through the accomplishment of two categories of life habits: daily and social activities (Fougeyrollas et al., 2019). The influence of hearing loss on older adults' social participation, facilitators and barriers to their social participation, and recommendations on how to promote this health determinant were analysed with the help of NVivo 12.
Results
Studies Characteristics
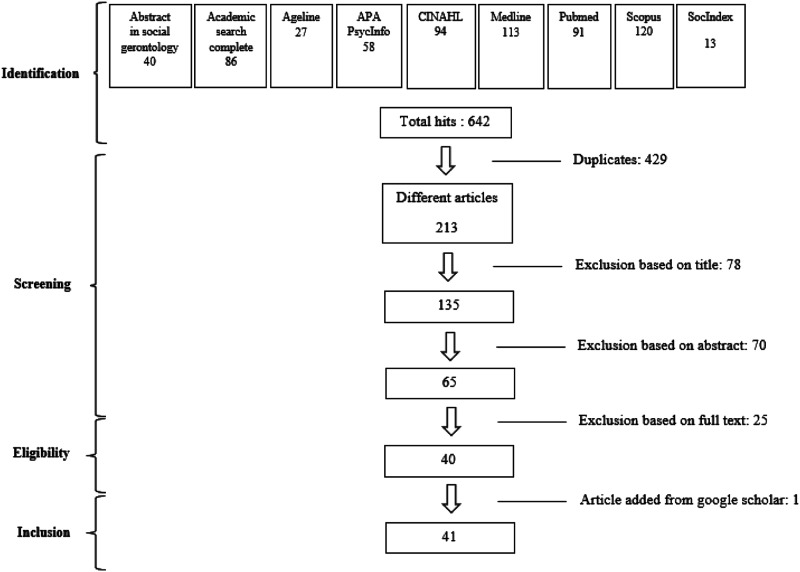
Of the 640 papers retrieved from the databases, 40 met the inclusion criteria and one was added through the extended search strategy in Google scholar using three keywords (social participation - older adult - hearing loss; Figure 1). Except for one thesis, all selected articles were issued in peer-reviewed journals. Published from 2000 to 2022 (see Appendix), most papers were from the last decade (number and proportion of papers: 32/41; 78.1%) with the most prolific year being 2016 (7; 17.1%). Most studies had been carried out in North America (16; 39.0%), but others in Europe (15; 36.6%) and Oceania (10; 24.4%). Majority of studies were quantitative (35; 85.4%), four qualitative (4; 9.7%) and two used a mixed approach (2; 4.9%). Cross-sectional design was mostly used (31; 75.6%). Finally, almost half of studies (19; 46.3%) did not provide a detailed description of their sample.
Figure 1.
Flow chart.
When specified (36/41; 87.8%), the mean age was above 65 for almost all studies (33/36; 91.7%). A majority (24/41; 58.5%) involved a sample of more than 150 persons. While two-third (26) of the studies had participants completing an audiometric assessment, i.e., reported the degree of hearing loss, in about a quarter (11; 26.8%) only a self-assessment of hearing loss was performed. Such assessment involved mainly answering questions related to the use of hearing aids and hearing difficulties in noisy environments. The majority (26, 63.4%) of studies specified the hearing assistive devices used by their participants. Different dimensions of social participation were used in the selected studies such as engagement, social activities, instrumental activities, social interactions (Levasseur et al., 2022). 44 different questionnaires were identified in 33 studies (80.5%) and targeted various related concepts, in addition to social participation (12; 29.3%) itself, such as: quality of life (11; 26.8%), mental status (9; 22.0%), communication (7; 17.1%), coping (4; 9.8%), and satisfaction toward an intervention (1; 2.4%). These questionnaires estimated the frequency of participation in different social activities (i.e., volunteering, education, hobbies, religion, shopping), participation restrictions, types of interactions, as well as the description of the social network (i.e., size, availability). For studies not using questionnaires, structured or semi-structured interviews were used.
In most of the studies (25/41; 61.0%), participants were predominantly female. In eight of them (19.5%), they represented more than 60% of the participants. Majority (24; 58.5%) of studies reported participants’ health information (i.e., self-rated perceived health, comorbidities, functional limitations). Some studies provided information on marital status (18; 43.9%), education (23; 56.1%), household income (13; 31.7%), and occupational status (7; 17.1%). When specified (13/41; 31.7%), the sample was predominantly Caucasian (13/13; 100%).
Social Participation
Of the 17 factors associated with social participation, 5 (29.4%) related to daily activities and 12 (70.6%) to social roles (Table 2). The majority (15; 88.2%) were barriers to social participation such as communication difficulties that negatively influenced involvement particularly in group activities, but also in formal encounters with, for example, a health care professional or a new person who is unaware of that person’s hearing loss. In a study exploring the psychosocial experiences of adults with hearing loss, a participant with sudden-onset hearing loss, stated, “I just wanted to be on my own and [with] people that I knew… I was frightened to meet new people because you don’t know how they speak” (Heffernan et al., 2016, p. S7). Difficulties identified in activities of daily living (ADLs; i.e., getting ready, walking) and instrumental activities of daily living (IADLs; i.e., household chores, shopping, entertaining guest) represented another barrier to social participation. While support from family and friends has been identified as a key facilitator to social participation, older adults with hearing loss seems to have difficulty in maintaining frequent meetings with friends (Table 2). A participant in a study that examined the subjective experience related to personal relationships and social interactions of older adults with hearing loss put it this way, “I see people less than before. They are still my friends; I just see them less. I get so frustrated” (Krawczyk, 2001, p. 36). Lack of empathy from others and miscommunication due to hearing loss can deteriorate relationships with loved ones, which might negatively influence social participation of older adults. Hearing loss might also result in a withdrawal of meaningful activities, either recreational, religious, educational, or professional.
I am part of the prayer ministry team a couple of weeks ago I said: ‘I am really going to have to come off it’…because I can’t do it. I cannot hear what people want prayer for […] it is…something else that is stripped away…it is not just your hearing that you have lost; it is a lot of other things you have lost as well. (Heffernan et al., 2016, p. S7).
Table 2.
Synthesis of Factors Positively (+) or Negatively (−) Influencing with Social Participation in Older Adults with Hearing Loss.
| Factors | Facilitator or Barrier | Frequency (%; n = 41) | |
|---|---|---|---|
| By Factors | Total | ||
| Participation | 11 (26.8) | ||
| • Daily activities | 10 (24.4) | ||
| Communication | 8 (19.5) | ||
| • Communication difficulties | (−) Dalton et al., 2003; Heffernan et al., 2016; Strawbridge et al., 2000; Sung et al., 2016 | 4 (9.8) | |
| Group conversations | (−) Fowler et al., 2022; Heffernan et al., 2016; Hickson et al., 2008; Hickson et al., 2014 | 4 (9.8) | |
| Formal interactions or with new people | (−) Fowler et al., 2022; Heffernan et al., 2016 | 2 (4.9) | |
| • Use of telecommunication | |||
| Telephone | (−) Fowler et al., 2022; Heffernan et al., 2016 | 2 (4.9) | |
| Internet | (+) Simpson et al., 2018 | 1 (2.4) | |
| Difficulties in ADLs & IADLs a | (−) Dalton et al., 2003; Gopinath, Schneider, McMahon, et al., 2012; Liljas et al., 2016; Strawbridge et al., 2000 | 4 (9.8) | 4 (9.8) |
| • Social activities | 7 (17.1) | ||
| Interpersonal relationships | 6 (14.6) | ||
| • Affective relationships | |||
| Difficulties to maintain friendships or romantic relationship | (−) Fowler et al., 2022; Heffernan et al., 2016; Krawczyk, 2001; Mikkola et al., 2015; Palmer et al., 2019 | 5 (12.2) | |
| • Social relationships | |||
| Difficulties in establishing relationships with colleagues | (−) Heffernan et al., 2016 | 1 (2.4) | |
| • Lack of empathy from those around | (−) Fowler et al., 2022; Hickson et al., 2008 | 2 (4.9) | |
| Community and spiritual life | 2 (4.9) | ||
| • Restriction of participation in recreational and community activities | (−) Heffernan et al., 2016 | 1 (2.4) | |
| • Withdrawal from religious activities | (−) Heffernan et al., 2016; Krawczyk, 2001 | 2 (4.9) | |
| Education | 1 (2.4) | ||
| • Restriction of participation in educational activities | (−) Heffernan et al., 2016 | 1 (2.4) | |
| Employment | 2 (4.9) | ||
| • Restriction of participation in working life | (−) Fowler et al., 2022; Heffernan et al., 2016 | 2 (4.9) | |
| Recreation | 4 (9.8) | ||
| • Withdrawal from leisure activities | (−) Fowler et al., 2022; Heffernan et al., 2016; Krawczyk, 2001; Mikkola et al., 2016 | 4 (9.8) | |
| Personal factors | 36 (87.8) | ||
| • Identity factors | 12 (29.3) | ||
| Sociodemographic characteristics | 11 (26.8) | ||
| • < 80 years old | (−) Gopinath, Schneider, McMahon, et al., 2012; Mick et al., 2014; Sung et al., 2016; Zhang et al., 2016 | 4 (9.8) | |
| • Being a woman | (−) Hickson et al., 2008; Mick et al., 2014; b Ramage-Morin, 2016; c (+) Zhang et al., 2016 | 4 (9.8) | |
| • Being in couple | (+) Lazzarotto et al., 2018; Ramage-Morin, 2016; Simpson et al., 2018; (−) Pronk et al., 2013 | 4 (9.8) | |
| • Being single (including divorced or widowed) | (−) Huang et al., 2021; Pronk et al., 2014. d | 2 (4.9) | |
| • Higher level of education | (+) Lazzarotto et al., 2018; Ramage-Morin, 2016. e | 2 (4.9) | |
| Personal identity characteristics | 1 (2.4) | ||
| • Extraversion | (+) Jang et al., 2003 | 1 (2.4) | |
| • Organic systems | 6 (14.6) | ||
| • Comorbidities | (−) Lazzarotto et al., 2018; Moser et al., 2017; Pronk et al., 2013; Simpson et al., 2018; Solheim et al., 2011 | 5 (12.2) | |
| • Dual sensory loss (hearing & vision loss) | (−) Lazzarotto et al., 2018; Ramage-Morin, 2016; f Zhang et al., 2016 | 3 (7.3) | |
| • Capabilities | 34 (82.9) | ||
| Intellectual activities | 2 (4.9) | ||
| • Negative representations of hearing loss | (−) Fowler et al., 2022; Heffernan et al., 2016 | 2 (4.9) | |
| Language | 5 (12.2) | ||
| • Comprehension difficulties | (−) Fowler et al., 2022; Krawczyk, 2001; Polku et al., 2016 | 3 (7.3) | |
| Whispering | (−) Gopinath, Hickson, et al., 2012; Krawczyk, 2001 | 2 (4.9) | |
| • Acquisition of communication related skills (lip reading, sign language…) | (+) Kerr & Stephens, 2000; Krawczyk, 2001 | 2 (4.9) | |
| Behavior | 20 (48.8) | ||
| • Negative emotions (anxiety, embarrassment, loss of self-esteem…) | (−) Fowler et al., 2022; Gopinath, Hickson, et al., 2012; Heffernan et al., 2016; Hickson et al., 2008; Krawczyk, 2001; Lazzarotto et al., 2016; Lazzarotto et al., 2018; Palmer et al., 2019; Polku et al., 2016; Strawbridge et al., 2000; Sung et al., 2016 | 11 (26.8) | |
| • Engaged coping | (+) Convery et al., 2019; Fowler et al., 2022; Heffernan et al., 2016; Jones et al., 2019; Kerr & Stephens, 2000; Krawczyk, 2001; Lazzarotto et al., 2016; Lazzarotto et al., 2018; Lazzarotto et al., 2019; Moser et al., 2017 | 10 (24.4) | |
| • Good cognition status | (+) Jang et al., 2003; Ramage-Morin, 2016 | 2 (4.9) | |
| • Depressive symptoms | (−) Andrade et al., 2017; Fowler et al., 2022; Hay-McCutcheon et al., 2018; Palmer et al., 2019; Strawbridge et al., 2000; Strawbridge et al., 2000; Sung et al., 2016 | 6 (14.6) | |
| • High daily stress | (−) Ramage-Morin, 2016 | 1 (2.4) | |
| • Fear of falling | (−) Ramage-Morin, 2016 | 1 (2.4) | |
| Motor activity | 7 (17.1) | ||
| • Functional limitations | (−) Gopinath, Schneider, McMahon, et al., 2012; Mikkola et al., 2016; Morgan et al., 2002; Palmer et al., 2019; Ramage-Morin, 2016; Schneider et al., 2010; Strawbridge et al., 2000 | 7 (17.1) | |
| Sense & perception | 21 (51.2) | ||
| • Greater hearing loss | (−) Andrade et al., 2017; Dalton et al., 2003; Goman et al., 2021 g ; Gopinath, Schneider, Hickson., et al., 2012; Hickson et al., 2008; Huang et al., 2021; Jang et al., 2003; Mikkola et al., 2015; Pronk et al., 2013; Ramage-Morin, 2016; Schneider et al., 2010; Shukla et al., 2021; Simpson et al., 2018; Solheim et al., 2011; Strawbridge et al., 2000; Sung et al., 2016; Zhang et al., 2016 | 18 (43.9) | |
| • Difficulties in spatial hearing | (−) Fowler et al., 2022; Krawczyk, 2001; Polku et al., 2016 | 3 (7.3) | |
| • Incontinence | (−) Ramage-Morin, 2016. f | 1 (2.4) | |
| Protection & resistance | 1 (2.4) | ||
| • Pain | (−) Ramage-Morin, 2016 | 1 (2.4) | |
| Environmental factors | 16 (39.0) | ||
| ➢ Social factors | 8 (19.5) | ||
| Socio-health system | 7 (17.1) | ||
| • Community services including support groups | (+) Fowler et al., 2022; Krawczyk, 2001; Schneider et al., 2010 | 3 (7.3) | |
| • Support from rehabilitation professionals | (+) Kerr & Stephens, 2000 | 1 (2.4) | |
| • Social support | (+) Fowler et al., 2022; Kerr & Stephens, 2000; Krawczyk, 2001; Lazzarotto et al., 2016; Moser et al., 2017 | 5 (12.2) | |
| • Large social networks | (+) Jang et al., 2003 | 1 (2.4) | |
| Social norms | 3 (7.3) | ||
| • Ageism | (−) Fowler et al., 2022; Krawczyk, 2001; Raymond & Lantagne Lopez, 2020 | 3 (7.3) | |
| • Lack of inclusion | (−) Fowler et al., 2022; Raymond & Lantagne Lopez, 2020 | 2 (4.9) | |
| • Responsibility for social participation rests with older adults with hearing loss | (−) Raymond & Lantagne Lopez, 2020 | 1 (2.4) | |
| ➢ Physical factors | 12 (29.3) | ||
| • Noisy environments | (−) Fowler et al., 2022; Heffernan et al., 2016; Hickson et al., 2008; Krawczyk, 2001; Mikkola et al., 2015; Pronk et al., 2014 | 6 (14.6) | |
| • Use of hearing aids | (+) Fowler et al., 2022; Gopinath, Schneider, Hickson, et al., 2012; Heffernan et al., 2016; h Ishigami et al., 2021; Krawczyk, 2001; i Pronk et al., 2014; Raymond & Lantagne Lopez, 2020; Weinstein et al., 2016 | 8 (19.5) | |
| • Technical aids (teletext, loop system…) | (+) Kerr & Stephens, 2000; Krawczyk, 2001 | 2 (4.9) | |
| • Living in rural communities | (−) Hay-McCutcheon et al., 2018. j | 1 (2.4) | |
| Total | 13 (+); 36 (−) | ||
aActivities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs).
bOnly for 60- to 69-year-old women.
cExcept for women who were single or living alone.
dFor older persons who had recently (within the past 3-4 years) lost their partner from the household.
eFor men.
fFor women.
gOnly for mental activities.
hBut hearing aids have their limitations.
iWhether people are comfortable wearing their hearing aids.
jRegarding positive social interactions.
Being in a relationship might encourage social participation, although there was no consensus (Table 2), depending on the type of relationship or personal factors of individuals such as gender.
Personal and Environmental Characteristics
Personal Factors
Socio-demographic characteristics, behavioral skills and the severity of older adults’ hearing loss were factors identified as negatively influencing their social participation (Table 2). Being younger (<80) and a women aged 60 to 69 were found to be among the older adults with hearing loss who experienced more isolation. While being extroverted was found to be positive for social engagement, older adults with hearing loss experiencing depressive symptoms or having negative representations of their condition will induce a greater risk of restriction in social participation (Table 2). Older adults had to negotiate their hearing loss in the context of a broader societal stigma that influenced their own view of this impairment. An older Irishman, when asked about his perspective on the impact of hearing loss on his social functioning, replied:
But I always thought of it as old person’s disease, and I can remember people had these great big hearing aids, and they had the thing in the pocket, and the last thing I wanted … you know, ‘Oh, I don’t want to wear a hearing aid.’ You just … you just sort of think no, it makes you look really impaired. It’s got kind of a social stigma to it. (Fowler et al., 2022, p. 2014).
In addition, according to the study from Heffernan and colleagues exploring psychosocial experiences of older adults with hearing loss, one participant expressed that his or her hearing loss reduced his/her sentiment of competence and authority: “I have always been… ever so efficient and capable and, you know, running things and organising things but because of my hearing, all that has gone” (Heffernan et al., 2016, p. S6).
Although good mental health and cognitive function can prevent social isolation, greater hearing loss was the most mentioned barrier (21; 51.2%) to social participation. In the presence of comorbidities or a visual impairment, the risk of social isolation also increased. Older adults with comprehension difficulties associated with the hearing might feel embarrassed, anxious and less confident, as reported by a participant describing his personal relationships and social interactions:
I no longer take the initiative in a conversation. I sit back and try to understand what is being said. Because I am afraid I might not have understood what was said, I am afraid I might be totally off the track when responding. So I have begun to say less and less. (Krawczyk, 2001, p. 35).
With engaged-coping, older adults can however develop new communication strategies and skills that might help them overcome the difficulties associated with their hearing loss and improve their social participation and quality of life, as described by a participant who is determined to continue his/her daily life despite his/her hearing loss: “you either concentrate on the negative side of it…Or you say, ‘Well, that is how it is. Now let’s get on with it’…Which sounds terribly pompous and flag-waving but…you effectively do that” (Heffernan et al., 2016, p. S8). Older adults with hearing loss might as well face functional limitations that negatively influence their mobility and participation. Hearing loss also causes difficulties with spatial hearing, which can range from an inconvenience, e.g., not being able to hear the phone ring, to a real danger, e.g., not being able to locate the noise of a car. In a study of the social functioning of older people with hearing loss, one participant addressed the difficulties of spatial hearing by describing the lack of accommodations in public places:
And we never hear public announcements – train stations, airports, anywhere. Well, you have to go and find a noticeboard or something like that, you know. Most places have monitors now, with times and directions on them. Well, you’re always last to leave the boat (laughs). You’re watch… you’re watching other people moving, and then you decide it’s time to get up. (Fowler et al., 2022, p. 2017).
Facing this insecurity, older adults with hearing loss may reduce their area of mobility and, consequently, their opportunities to participate socially.
Environmental Factors
The physical and social aspects of the environment are also critical in enabling participation of older adults with hearing loss. One study found that older adults living in rural communities, where access to hearing healthcare may be poor, experienced fewer positive social interactions than their urban counterparts (Table 2). At the level of the socio-health system, support from community services and rehabilitation professionals as well as having a large social network is among facilitators in assisting older adults to participate socially (Table 2). Support groups were also appreciated, as for this participant who reported an increase in new relationships as a result of his active participation in a hearing loss support group: “It helps me to be with other people who also can’t hear too good. I have learned from them that it is ok to speak up and tell people when I can’t hear or understand” (Krawczyk, 2001, p. 37). Such adaptive social environment is helpful, as opposed to noisy environments in which older adults with hearing loss are not comfortable, as emphasized by one participant who had to give up actively participating in such environments: “I don’t like large meetings. The background noise is too confusing. When I have to attend meetings with my husband, I turn my hearing aids way down or off and pretend that I can hear what is going on” (Krawczyk, 2001, p. 39). Many older adults with hearing loss end up avoiding noisy environments (Table 2), thereby reducing their social participation, more out of obligation than choice: “I attend fewer movies. The sound is too loud. I can turn my hearing aid down but then I miss what is being said. If my friends want to go to the movies, I usually stay home” (Krawczyk, 2001, p. 36). To adapt, some older adults choose to wear hearing aids which, despite their limitations, foster social participation. Others use assistive devices such as teletext, pagers, or colored alarms to maintain their independence.
Despite these accommodations, older adults with hearing loss experience several social challenges that impeded their ability to engage in society. Indeed, although the rhetoric around people with impairments is to encourage inclusion, the reality of participation in organization for older adults is different on the field. Opportunities for participation are not always tailored to the needs of older adults with hearing loss with, for example, an inadequate telephone registration system. Some people seem to think that older adults having disabilities are the only responsible for their social participation and must know their limitations and adapt their activities to their abilities. Finally, because of ageism, representations of young and fit older adults are prioritized, not the inclusion of people with disabilities, such as having hearing loss.
Recommendations
Authors of most papers (32; 78.0%) made recommendations in their discussion for preventing the negative consequences of hearing loss by preserving the engagement and quality of life of older adults. These recommendations concerned three steps of clinical practice: prevention, assessment, and intervention.
Because hearing loss in older adults has important negative biopsychosocial consequences, it is essential to develop prevention campaigns about hearing loss and regularly detect this condition in the population (Andrade et al., 2017; Dalton et al., 2003; Gopinath et al., 2012; Lazzarotto et al., 2018; Pronk et al., 2014; Strawbridge et al., 2000; Zhang et al., 2016).
In addition to prevention, and since the severity of hearing loss is a major barrier to social participation in older adults (Dalton et al., 2003; Lazzarotto et al., 2019; Schneider et al., 2010; Strawbridge et al., 2000), the importance of early detection was frequently highlighted. Among the 24 (58.5%) papers advising assessment in older adults, more than half (14; 58.3%) recommended enriching the evaluation of hearing loss with a biopsychosocial tool to better understand and support this condition and its impact on their daily lives (Gopinath, Hickson, Schneider, et al., 2012; Gopinath, Schneider, Hickson, et al., 2012; Hay-McCutcheon et al., 2018; Heffernan et al., 2016; Hickson et al., 2008; Jang et al., 2003; Krawczyk, 2001; Lazzarotto et al., 2016; 2018; 2019; Morgan et al., 2002; Pronk et al., 2013; Ramage-Morin, 2016; Solheim et al., 2011). Lazzarotto and colleagues (2019) explained that assessment focusing on symptoms does not fully represent how an individual’s condition impact on his or her daily life, compared to the necessary combination of physiological and functional tools with subjective questionnaire exploring the influence of hearing loss in the lives of older adults. Rather than only measuring hearing loss, a complementary assessment of handicap’s situation related to hearing loss should be carried out using questionnaires such as the Hearing Handicap Questionnaire (HHQ; Hickson et al., 2008), the Quantified Denver Scale (QDS; Hickson et al., 2008) or the Hearing Handicap Inventory for the Elderly (HHIE; Gopinath, Hickson, et al., 2012; Gopinath, Schneider, Hickson, et al., 2012). When examining the effects of hearing loss on the psychosocial health of older adults, Pronk and colleagues (2013) emphasized the importance of considering differences, such as living in a rural or urban environment (Hay-McCutcheon et al., 2018), or gender (Ramage-Morin, 2016). A systematic assessment of coping also helps to identify older adults with unhealthy strategies so that professional support can be tailored (Lazzarotto et al., 2016; 2019). As it is critical for social participation, mental health should be assessed, especially in older adults at higher risk of depression (Morgan et al., 2002). Such holistic evaluation will foster adaptive support and appropriate interdisciplinary interventions and collaboration according to the older adult’s profile.
Most (27; 65.9%) papers provided recommendations for interventions maintaining or improving social participation in older adults with hearing loss (Table 3). Almost all recommendations resulted from the authors interpretation (identified by * in Table 3), whereas only one study was evidence-based (identified by + in Table 3). This highlights the lack of evidence related to interventions aiming to maintain or improve social participation of older adults with hearing loss. According to the types of rehabilitation interventions proposed by McColl and Law (2013), these recommendations focused either on the individual (training, skill development, and education) or his/her environment (environmental modification, support provision, and support enhancement; McColl & Law, 2013). To help older adults with hearing loss adapt to their condition and prevent isolation, many authors recommend training with audiological rehabilitation such as audiological training (Gopinath, Schneider, Hickson, et al., 2012; Mikkola et al., 2015; Solheim et al., 2011). Audiological training is an intervention designed to maximize the use of an individual’s residual hearing through listening practice to improve related skills and speech comprehension. It often follows a structured hierarchy of listening activities that become increasingly difficult with each training session [i.e., multiple repetitions of sounds; progressively difficult exercises from coarse (acoustically different sounds to fine (acoustic properties) discriminations (Tye-Murray et al., 2012). The active involvement of caregivers in the rehabilitation process should also be encouraged to improve the social participation and quality of life of older adults with hearing loss (Gopinath, Hickson, Schneider, et al., 2012; Lazzarotto et al., 2019; Moser et al., 2017). Because of their positive impact on social participation, interventions that target’s new skills development such as engaging in appropriate coping strategies for both older adults with hearing loss and their caregivers should be prioritized (Lazzarotto et al., 2016; 2019; Moser et al., 2017). Appropriate use of hearing aids or other assistive listening devices may also be beneficial (Ishigami et al., 2021; Schneider et al., 2010; Weinstein et al., 2016), as well as the use of the Internet for non-verbal communication (Ramage-Morin, 2016; Simpson et al., 2018). Convery and his colleagues (2019) have shown that developing self-management skills for hearing loss in older adults can improve their social participation. Among educative interventions, the recommendations mainly concerned transmission of knowledge about the nature of the hearing impairment (Gopinath, Hickson, Schneider, et al., 2012; Moser et al., 2017), promotion of the use of assistive devices (Dalton et al., 2003; Gopinath, Schneider, Hickson, et al., 2012; Weinstein et al., 2016) and enhancing social self-efficacy and self-esteem (Andrade et al., 2017; Kerr & Stephens, 2000; Palmer et al., 2019). The variety and scope of these clinical areas require interdisciplinary intervention and collaboration.
Table 3.
Synthesis of Recommendations (*) and Interventions Without Conclusive Results (?) or Positively (+) Influencing with Social Participation in Older Adults with Hearing Loss.
For the environment, the recommendations mainly targeted developing the support from the relatives and interprofessional collaboration. According to Moser and collaborators (2017), social support was the strongest predictor of quality of life in older adults, especially in the psychological and social domains. Support and information, whether provided by significant others or by audiologists, must be adapted to the person, i.e., require taking the time necessary to properly know the older adults, understand their context and advise them according to their life project and, when needed, within an interprofessional collaboration (Lazzarotto et al., 2019). Specialized hearing care should also be offered to older adults living in areas with poor access to health system through community workers, telehealth, or support groups (Hay-McCutcheon et al., 2018). To facilitate participation, the representations and behaviors of relatives, organizations and public authorities must also be less stigmatizing and more inclusive (Lazzarotto et al., 2018; Raymond & Lantagne Lopez, 2020).
Discussion
This study aimed to provide a comprehensive understanding of the influence of hearing loss on social participation in older adults, including its facilitators and barriers. The results shown that older adults with hearing loss have difficulty maintaining their relationships and tend to withdraw from social activities that are important to them. This scoping review highlighted that social support, engaged coping strategies, and the use of hearing aids were the primary facilitators of social participation among older adults with hearing loss. Conversely, greater hearing loss, communication difficulties, co-morbidities and reduced mental health were the main barriers identified. To better promote the social participation of this population, it is necessary to promote early detection of hearing loss, holistic assessment and interprofessional collaboration.
The importance of a holistic assessment was also highlighted a decade ago in a previous review (Ciorba et al., 2012). From evaluation to intervention and including rehabilitation, such assessment is also coherent with recommendations from Heine and Browning literature review (2002). Despite this review published 20 years ago and clinical guidelines emphasized consideration of the psychosocial consequences of hearing loss, practice-based studies have shown that audiologists rarely carried out a holistic assessment (Bennett, Barr, et al., 2021). As discussed in at least two studies (Bennett, Donaldson, et al., 2021; Pryce et al., 2016), psychosocial impacts are sometimes difficult to target during appointments with the audiologist, either because of time constraints or because the professionals do not feel sufficiently competent to assess and intervene accordingly. Nevertheless, the majority of audiologists seem to be aware of the importance of psychosocial impacts of hearing loss and desire to develop their skills to better assess and intervene (Bennett, Kelsall-Foreman, et al., 2021). Furthermore, despite evidence-based approaches in assessing the psychosocial effects of hearing loss, a study of 65 international audiologists found that they primarily use informal, non-standardized measurement tools (Bennett, Barr, et al., 2021). Even though audiologists are developing their practice, it is not possible to rely solely on one category of professionals for a holistic assessment and intervention, it is and therefore essential to develop interprofessional collaboration.
Being in a greater number on the field and having often developed a trust relationship with their patients, physicians and advanced practice nurses are often in a strategic position to provide early detection of hearing loss. Physician and advanced practice nurses could also provide holistic intervention and follow-up in partnership with other professionals, such as audiologists, psychologists, occupational therapists, or social workers. However, most countries face a significant shortage of health and social professionals (WHO, 2016). Because of this shortage and limited professional skills, training and development of new intervention protocols remains a challenge. According to a study published in 2009, many physicians do not detect hearing loss due to a lack of time or knowledge about measurement tools such as the Hearing Handicap Inventory for Elderly-Screening (HHIE-S; Tomioka et al., 2013), which patients can answer alone in the waiting room (Johnson et al., 2009). Awareness and skills’ training should thus not only target audiologists and physicians, but all professionals that work with older adults and have an impact on at least one of the individual or environmental factors highlighted in this review as influencing their social participation.
Since greater hearing loss is one of the major obstacles to their social participation (Andrade et al., 2017; Shukla et al., 2021), the bigger challenge remains to identify older adults with hearing loss as early as possible. Despite its prevalence, older adults with hearing loss await an average of 7 years before seeking for help (Hearing Loss Association of America, 2018) and only one individual out of five who might benefit from treatment is actually being seen by professionals (Davis et al., 2007). Help-seeking has been shown to occur at critical times, such as when discomfort and stress of hearing loss become highly prominent (Davis et al., 2007; Southall et al., 2010). Older adults seem to accept hearing loss as an inconvenience of the aging process (Clements, 2018), and for those who want to reduce its negative impact, the stigma associated with this condition remains a significant barrier to seek for help (David et al., 2018; Wallhagen, 2010). According to Clements (2018), when being exposed to potential stigmatization, the individuals evaluate this situation as a threat to their social identity and therefore tend to deny it. These stigmas include looking old, stupid, cognitively impaired, and less capable (Clements, 2018; Southall et al., 2010; Wallhagen, 2010). Hearing aids are also often described as ugly and associated with being old (Bennett et al., 2022; Clements, 2018). Campaigns promoting hearing aids that are almost invisible can unfortunately increase stigmatization (Clements, 2018). To reduce the delay in seeking for assistance in older adults with hearing loss, it is necessary to modify societal norms with efficacious public education strategies (Chundu et al., 2020).
Strengths and Limitations
Following a rigorous framework and multidisciplinary database research, this study provides a comprehensive understanding of the influence of hearing loss on social participation in older adults and identified facilitators and barriers at the individual and environmental levels. Due to financial and time constraints, it is possible that some relevant studies may not have been identified, especially from the gray literature. In accordance with the framework followed, this scoping study did not assess the quality of the studies, but all selected articles were published in peer-reviewed journals. Finally, the use of multiple scales might also have influenced the interpretation of results.
Conclusion
This scoping review aimed to provide a comprehensive understanding of the influence of hearing loss on social participation in older adults, including its facilitators and barriers. The results highlighted the difficulties that most older adults with hearing loss faced in their social participation, particularly in maintaining relationships and significant social activities. The major facilitators identified were social support, engaged coping strategies, and the use of hearing aids. In contrast, greater hearing loss, communication difficulties, co-morbidities and reduced mental health were the main barriers reported. Early detection of hearing loss, holistic assessment, and interdisciplinary intervention and collaboration remain the key recommendations in promoting social participation for older adults with hearing loss. The stigma of hearing loss in society as well as the shortage of personnel in many social and health care professions remains the major challenges in improving social participation of older adults with hearing loss. As social participation is a key determinant of well-being and health and the prevalence of hearing loss is increasingly important in aging societies, it is necessary to better assess and intervene accordingly. Future research is needed to address the issues and consequences related to the stigma of hearing loss. Similarly, it is essential to explore the challenges faced by professionals in early detection and to identify innovative solutions to expand screening, holistic assessment, intervention, and interprofessional collaboration to join the global movement for Healthy Aging.
Acknowledgments
We wish to thank Miguel Escobar documentalist at Université de Sherbrooke for his help in refining our research strategy.
Author Biographies
Agathe Chaintré Prieur is a master student in gerontology at School of Social Work, Faculty of Letters and Social Sciences, Université de Sherbrooke. Agathe Prieur Chaintré is a nurse by training who has worked with older adults in France.
Yves Couturier is affiliated with the Social Work Department at the Université de Sherbrooke (Canada). His research expertise is related to integrated services, interprofessional collaboration, and sociology of professional practices in the field of health and social services.
T.H. Trang Nguyen is a master student in gerontology at School of Social Work, Faculty of Letters and Social Sciences, Université de Sherbrooke.
Mélanie Levasseur is an occupational therapist, director of research and full professor at the School of Rehabilitation of the Université de Sherbrooke, and a researcher at the Research Centre on Aging. Her research program targets the development and evaluation of a continuum of innovative interventions to promote the social participation of older adults.
Appendix.
Table A1.
Characteristics of the Articles on Social Participation of Older Adults with Hearing Loss.
| Author(s) | Year | Region | Design | Sample [Size; Mean Age (Range)] | Objective | |
|---|---|---|---|---|---|---|
| [1] | Andrade et al | 2017 | Europe | Longitudinal, prospective correlational, data from the Survey of health, ageing and retirement in Europe (SHARE) | 10 088; 69 (50+) | Investigate how hearing loss difficulties are related to depression and social activities using a sample of 10 countries |
| [2] | Convery et al | 2018 | Oceania | Cross-sectional, correlational | 37; 74 (52–83) | Investigate the associations between self-reported hearing loss, self-management and hearing aid benefit and satisfaction |
| [3] | Dalton et al | 2003 | North America | Cross-sectional, correlational, data from the 5-year follow-up of the epidemiology of hearing loss study (EHLS-2) | 2688; 69 (53–97) | Investigate the impact of hearing loss on quality of life in a large population of older adults |
| [4] | Fowler et al | 2022 | Europe | Qualitative, constructivist grounded theory, individual interviews | 6; 75 (64–85) | Explore social functioning and engagement in older adults with age-related hearing loss who used hearing aids or cochlear implants |
| [5] | Goman et al | 2021 | North America | Longitudinal, quasi-experimental (test at baseline session -retest at 6 months follow up session) | 40; 77 (70–84) | Evaluate a hearing loss intervention versus an aging education intervention on activity engagement in the aging and cognitive health evaluation in elders pilot (ACHIEVE-P) |
| [6] | Gopinath, Hickson, et al | 2012 | Oceania | Longitudinal, correlational, data from 2 waves (1997–99 & 2002–04) of the blue mountains hearing study | 811; 49+ (T0) | Assess both cross-sectional and longitudinal associations between measured hearing impairment and self-perceived hearing handicap, and health outcomes (comorbidities, functional and cognitive decline, self-rated health, and well-being) |
| [7] | Gopinath, Schneider, Hickson, et al | 2012 | Oceania | Longitudinal, prospective correlational, data from 2 waves (1997–99 & 2002–04) of the blue mountains hearing study | 829; 67 | Determine the prospective association between measured hearing impairment, self-reported hearing handicap and hearing aid use with quality of life |
| [8] | Gopinath, Schneider, McMahon, et al | 2012 | Oceania | Cross-sectional, correlational, data from the 10 years follow-up (2002–04) of the blue mountains hearing study | 1572; 74 | Assess the associations between hearing impairment with activity limitations as assessed by the activities of daily living (ADL) scale |
| [9] | Hay-McCutcheon et al. | 2018 | North America | Cross-sectional, correlational | 80; 70 (60+) | Explore the extent to which hearing loss affected positive social interactions in older adults living in rural and urban communities |
| [10] | Heffernan et al., 2016 | 2016 | Europe | Qualitative, deductive thematic analysis, individual semi-structed interviews, 2 groups: Adults with mild-moderate hearing loss & hearing healthcare professionals | 25 (+9 hearing healthcare professionals); 69 (20–91) | Explore the psychosocial experiences of adults with hearing loss using the self-regulatory model as a theoretical framework |
| [11] | Hickson et al | 2008 | Oceania | Cross-sectional, Descriptive/correlational, participants were a subset of subjects from the University of Queensland’s active communication education program | 178; 74 (53–94) | Investigate: (i) The associations between measured hearing impairment and self-reported hearing and communication difficulties (i.e., activity limitations, participation restrictions), health-related quality of life and wellbeing in community-based older australians; and (ii) the influence of age, gender, living situation and hearing aid use on these associations |
| [12] | Huang et al | 2020 | North America | Cross-sectional, correlational, data from wave 2 (2010–11) of the National Social Life, Health and Aging Project | 3196; 73 (62–91) | (i) Investigate the associations between functional hearing and loneliness and (ii) assess effect modification by age, sex, and marital status |
| [13] | Ishigami et al | 2020 | North America | Cross-sectional, descriptive, baseline data (2010–15) from the Canadian longitudinal study on aging | 51 338; 60 (45–85) | Describe the profile of assistive device users in Canada regarding socio-demographic and health factors as well as socials, including social participation |
| [14] | Jang et al | 2003 | North America | Cross-sectional, descriptive/correlational, sample from the Charlotte County healthy aging study | 425; 72 (60–84) | Examine the comparative roles of vision and hearing in different aspects of older individuals’ lives |
| [15] | Jayakody et al | 2020 | Oceania | Qualitative, community conversation, groups of five participants to discuss three open-ended questions | 40; (60+) | Identify the views of the community members when designing an online community using Facebook to support the psychosocial well-being of hearing- impaired older adults |
| [16] | Jones et al | 2019 | North America | Cross-sectional, 10-week prospective single-blind pilot RCT of interactive group auditory rehabilitation (GAR; control) versus GAR + interactive socialisation/health education (SHE) & strengthening exercises | 66; 74 (65+) | Explore the impact of a group exercise and socialisation/health education intervention and group auditory rehabilitation on physical function and loneliness among older adults with hearing loss |
| [17] | Kerr & Stephens | 2000 | Europe | Mixed, (QUAL) open-ended questionnaire (to list positive experiences due to their hearing loss) while waiting for (QUAN) the doctor (where participants were asked to rate how helpful they found each positive experience they listed) or a hearing testing | 207; 63 | Understand the nature and function of positive experiences in living with auditory disablement |
| [18] | Krawczyk | 2001 | North America | Qualitative (thesis), phenomenology, individual semi-structured interviews | 15; 80 (66–100) | Explore acquired hearing loss in seniors as a risk factor for a decline in the psychosocial functioning within that population |
| [19] | Lazzarotto et al | 2016 | Europe | Cross-sectional, descriptive/correlational, dyads were recruited in a French preventive health center | 88 (44 dyads); patients 71 (57–93), caregivers 64 (19–87) | Determine whether quality of life of patients and caregivers is influenced by coping strategies implemented either by themselves or their relatives |
| [20] | Lazzarotto et al | 2018 | Europe | Cross-sectional, descriptive/correlational, performed in a French preventive health center | 51; 71 (66–79) | Assess the associations between psycho-behavioral determinants and quality of life in individuals with age-related hearing loss |
| [21] | Lazzarotto et al | 2019 | Europe | Cross-sectional, descriptive/correlational, dyads were recruited in a French preventive health center | 896 (448 dyads); patients 70 (66–77), caregivers 69 (63–76) | Examine, in a sample of patient-caregiver dyads in the specific context of age-related hearing loss, whether the quality of life of patients and caregivers is influenced by the coping processes they use from a specific actor–partner interdependence model (APIM) |
| [22] | Liljas et al | 2016 | Europe | Longitudinal, descriptive/correlational, sample of British men followed up for 2 years for disability and 10 years for mortality | 3981; 72 (63–85 in 2003) | Examine the associations between hearing impairment and risk of incident disability and all-cause mortality |
| [23] | Mick et al | 2014 | North America | Cross-sectional, descriptive/correlational, data from the 1999 to 2006 cycles of the National Health and Nutrition Examination Survey (NHNES) | 860 (60–69) + 593 (70–84); (60–84) | Determine if age-related hearing loss is associated with social isolation and whether factors such as age, gender, income, race, or hearing aid use moderated this association |
| [24] | Mikkola et al | 2014 | Europe | Cross-sectional, descriptive/correlational, data from the Life Space Mobility in Old Age (LISPE) | 848; 81 (75–90) | Investigate whether hearing difficulty is associated with objective and perceived participation in social and leisure activities outside the home in older adults |
| [25] | Mikkola et al | 2015 | Europe | Longitudinal, descriptive/correlational, data from the life space mobility in old age (LISPE) | 767; 81 (75–90) | Investigate whether self-reported hearing problems are associated with time spent out-of-home and withdrawal from a leisure activity among older adults |
| [26] | Morgan et al | 2002 | Oceania | Cross-sectional, descriptive/correlational, participants were a subset of 250 subjects who had taken part in the University of Queensland’s longitudinal “keep on talking” program | 93; 72 (59–96) | Investigate the impact of hearing impairment on the quality of life of older australians |
| [27] | Moser et al | 2017 | Europe | Cross-sectional, descriptive/correlational | 65; 72 (55–75+) | Explore the influence of hearing problems, various coping strategies, and perceived social support on quality of life |
| [28] | Palmer et al | 2019 | North America | Cross-sectional, prospective correlational, participants recruited from the communication, health, aging, relationship types and support study | 240; 73 (65–94) | Examine whether the severity of a communication impairment was associated with a range of social measures and to examine the association between these characteristics and psychological well-being |
| [29] | Polku et al | 2016 | Europe | Cross-sectional, correlational, data from a second follow up of the Life Space Mobility in Old Age (LISPE) and a new sub-study (Hearing, cognition, and well-being) | 706; 82 (76–91) | Assess the associations between different domains of quality of life, perceived hearing difficulties in various everyday situations, and audiometrically measured hearing level among community dwelling older adults |
| [30] | Pronk et al | 2013 | Europe | Longitudinal, descriptive/correlational, data from the Longitudinal Aging Study Amsterdam (LASA; covering 4 years of follow-up) | 996 (self-report analyses) and 830 (speech-in-noise test analyses); 74 (63–93) | (i) Determine the longitudinal associations between baseline hearing status and 4-year follow-up depression and loneliness in an older population and (ii) investigate possible differences across subgroups (i.e., men, partner in the household, one or more chronic disease(s)) in these associations |
| [31] | Pronk et al | 2014 | Europe | Longitudinal, descriptive/correlational, data from the Longitudinal Aging Study Amsterdam (LASA; covering 3 to 7 years of follow-up) | 1178; (57–85+) | Investigate whether the rate of decline in older adults’ hearing status is associated with the rate of decrease in their psychosocial health and explore moderation by baseline hearing status, health-related factors, and sociodemographic factors |
| [32] | Ramage-Morin | 2016 | North America | Cross-sectional, descriptive/correlational, data from 2008/2009 Canadian Community Health Survey-Healthy Aging (CCHS-HA) | 30 176; 60 | Examine the prevalence of hearing difficulties and social isolation, and associations between them when controlling for sociodemographic factors, functional limitations, incontinence, and fear of falling |
| [33] | Raymond & Lantagne Lopez | 2020 | North America | Mixed, phase 1 (QUAL): Focus groups using 2 scenarios to be analyzed, phase 2 (QUAN): Questionnaire survey developed from the results of phase 1 | 40 for phase one (38 focus group +2 individual interviews) 86 for the questionnaire; focus groups: 39-: 18%, 40–59: 23%, 60–74: 48%, 75+: 13%/questionnaire: 39-: 10%, 40–59: 32%, 60–74: 40%, 75+: 18% | Document the social representations that exist within seniors’ organizations regarding participation by older adults with impairments |
| [34] | Schneider et al | 2010 | Oceania | Longitudinal, correlational, data from the Blue Mountains Hearing Study (BMHS) | 2 956, 1 457 at the 5-year follow-up; 69 | Estimate the cross-sectional and longitudinal impact of hearing loss on use of community support services and reliance on non-spouse family/friends among older adults |
| [35] | Shukla et al | 2021 | North America | Cross-sectional, descriptive/correlational, data from the 2015 Medicare Current Beneficiaries Survey (MCBS) | 1009; 64-: 16.14%, 65–74: 49.60%, 75+: 34.26% | Investigate the independent association between functional hearing loss and social engagement in a nationally representative sample of older adults |
| [36] | Simpson et al | 2018 | Oceania | Cross-sectional, correlational | 65; 65–70: 26%, 71–80: 34%, 81+: 40% | Examine the associations between self-reported loneliness and internet use in hearing aid wearers aged 65 years and over |
| [37] | Solheim et al | 2011 | Europe | Cross-sectional, descriptive/correlational, participants recruited from a hospital waiting list for outpatient hearing aid fitting | 84; 65–92 (less than 80: 51.2%, more than 80: 48.8%) | Assess the daily life consequences of hearing loss in older adults and to explore the influences of hearing loss, subjective assessment of health and general life satisfaction, gender, age, and marital status |
| [38] | Strawbridge et al | 2000 | North America | Longitudinal, correlational, data from the Alameda County study (began in 1965, with follow-up in 1974, 1983, 1994 & 1995) | 2461; 65 (50–102) | Determine whether functional and psychosocial outcomes associated with hearing impairment are a direct result or stem from prevalent comorbidity |
| [39] | Sung et al | 2015 | North America | Cross-sectional, descriptive/correlational, participants from the Studying Multiple Outcomes After Aural Rehabilitative Treatment (SMART) | 145; 50–94 (50–59: 14.6%, 60–69: 34.5%, 70–79: 29%, 80+: 21.9%) | Determine factors associated with loneliness in older adults presenting for hearing loss treatment |
| [40] | Weinstein et al | 2016 | North America | Cross-sectional, quasi-experimental, test at the hearing aid fitting, retest at 1-week & 4- to 6- week follow-up | 40; 80 (62–92) | Investigate the buffering effects of hearing aid use on perceived social and emotional loneliness |
| [41] | Zhang et al | 2016 | Oceania | Cross-sectional, descriptive/correlational, baseline data from the Brief Risk Identification of Geriatric Health Tool (BRIGHT) | 3817; 80 (61–98) | Establish associations between sensory-related disability and quality of life |
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Agathe Prieur Chaintré is supported by a salary award from the Université de Sherbrooke, Canada; and the Coopérative Funéraire de l’Estrie, Canada. Mélanie Levasseur is a Fonds de la recherche du Québec Santé Senior Researcher (#298996, 2021-2025).
ORCID iD
Mélanie Levasseur https://orcid.org/0000-0002-5914-0708
References
- Andrade C. C., Pereira C. R., Silva P. A. D. (2017). The silent impact of hearing loss: Using longitudinal data to explore the effects on depression and social activity restriction among older people. Ageing and Society, 38(12), 2468–2489. 10.1017/S0144686X17000708 [DOI] [Google Scholar]
- Arksey H., O’Malley L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Arlinger S. (2003). Negative consequences of uncorrected hearing loss—A review. International Journal of Audiology, 42(sup2), 17–20. 10.3109/14992020309074639 [DOI] [PubMed] [Google Scholar]
- Avlund K., Lund R., Holstein B. E., Due P. (2004). Social relations as determinant of onset of disability in aging. Archives of Gerontology and Geriatrics, 38(1), 85–99. 10.1016/j.archger.2003.08.003 [DOI] [PubMed] [Google Scholar]
- Bath P. A., Gardiner A. (2005). Social engagement and health and social care use and medication use among older people. European Journal of Ageing, 2(1), 56–63. 10.1007/s10433-005-0022-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett R. J., Barr C., Montano J., Eikelboom R. H., Saunders G. H., Pronk M., Preminger J. E., Ferguson M., Weinstein B., Heffernan E., van Leeuwen L., Hickson L., Timmer B. H. B., Singh G., Gerace D., Cortis A., Bellekom S. R. (2021). Identifying the approaches used by audiologists to address the psychosocial needs of their adult clients. International Journal of Audiology, 60(2), 104–114. 10.1080/14992027.2020.1817995 [DOI] [PubMed] [Google Scholar]
- Bennett R. J., Donaldson S., Kelsall-Foreman I., Meyer C., Pachana N. A., Saulsman L., Eikelboom R. H., Bucks R. S. (2021). Addressing emotional and psychological problems associated with hearing loss: Perspective of consumer and community representatives. American Journal of Audiology, 30(4), 1130–1138. 10.1044/2021_AJA-21-00093 [DOI] [PubMed] [Google Scholar]
- Bennett R. J., Kelsall-Foreman I., Donaldson S., Olaithe M., Saulsman L., Badcock J. C. (2021). Exploring current practice, knowledge, and training needs for managing psychosocial concerns in the audiology setting: Perspectives of audiologists, audiology reception staff, and managers. American Journal of Audiology, 30(3), 557–589. 10.1044/2021_AJA-20-00189 [DOI] [PubMed] [Google Scholar]
- Bennett R. J., Saulsman L., Eikelboom R. H., Olaithe M. (2022). Coping with the social challenges and emotional distress associated with hearing loss: A qualitative investigation using Leventhal’s self-regulation theory. International Journal of Audiology, 61(5), 353–364. 10.1080/14992027.2021.1933620 [DOI] [PubMed] [Google Scholar]
- Byers A. L., Vittinghoff E., Lui L.-Y., Hoang T., Blazer D. G., Covinsky K. E., Ensrud K. E., Cauley J. A., Hillier T. A., Fredman L., Yaffe K. (2012). Twenty-year depressive trajectories among older women. Archives of General Psychiatry, 69(10), 1073–1079. 10.1001/archgenpsychiatry.2012.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacchione P. Z. (2014). Sensory impairment: A new research imperative. Journal of Gerontological Nursing, 40(4), 3–5. 10.3928/00989134-20140306-01 [DOI] [PubMed] [Google Scholar]
- Chen H.-L. (1994). Hearing in the elderly: Relation of hearing loss, loneliness, and self-esteem. Journal of Gerontological Nursing, 20(6), 22–28. 10.3928/0098-9134-19940601-07 [DOI] [PubMed] [Google Scholar]
- Chundu S., Manchaiah V., Han W., Thammaiah S., Ratinaud P., Allen P. M. (2020). Social representation of “hearing loss” among people with hearing loss: An exploratory cross-cultural study. Journal of the American Academy of Audiology, 31(10), 725–739. 10.1055/s-0040-1719127 [DOI] [PubMed] [Google Scholar]
- Ciorba A., Bianchini C., Pelucchi S., Pastore A. (2012). The impact of hearing loss on the quality of life of elderly adults. Clinical Interventions in Aging, 7, 159–163. 10.2147/CIA.S26059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark M. S., Bond M. J., Sanchez L. (1999). The effect of sensory impairment on the lifestyle activities of older people. Australasian Journal on Ageing, 18(3), 124–129. APA PsycInfo. 10.1111/j.1741-6612.1999.tb00112.x [DOI] [Google Scholar]
- Clements C. (2018). Why do older adults delay in seeking help for hearing loss. Journal of Otolaryngology-ENT Research, 3(4), 00070. 10.15406/joentr.2015.03.00070 [DOI] [Google Scholar]
- Convery E., Keidser G., Hickson L., Meyer C. (2019). The relationship between hearing loss self-management and hearing aid benefit and satisfaction. American Journal of Audiology, 28(2), 274–284. 10.1044/2018_AJA-18-0130 [DOI] [PubMed] [Google Scholar]
- Courtin E., Knapp M. (2017). Social isolation, loneliness and health in old age: A scoping review. Health & Social Care in the Community, 25(3), 799–812. CINAHL Plus with Full Text. 10.1111/hsc.12311 [DOI] [PubMed] [Google Scholar]
- Cruice M., Worrall L., Hickson L. (2005). Personal factors, communication and vision predict social participation in older adults. Advances in Speech Language Pathology, 7(4), 220–232. 10.1080/14417040500337088 [DOI] [Google Scholar]
- Dalton D. S., Cruickshanks K. J., Klein B. E. K., Klein R., Wiley T. L., Nondahl D. M. (2003). The impact of hearing loss on quality of life in older adults. The Gerontologist, 43(5), 661–668. 10.1093/geront/43.5.661 [DOI] [PubMed] [Google Scholar]
- David D., Werner P. (2016). Stigma regarding hearing loss and hearing aids: A scoping review. Stigma and Health, 1(2), 59–71. APA PsycArticles. 10.1037/sah0000022 [DOI] [Google Scholar]
- David D., Zoizner G., Werner P. (2018). Self-stigma and age-related hearing loss: A qualitative study of stigma formation and dimensions. American Journal of Audiology, 27(1), 126–136. 10.1044/2017_AJA-17-0050 [DOI] [PubMed] [Google Scholar]
- Davis A., Smith P., Ferguson M., Stephens D., Gianopoulos I. (2007). Acceptability, benefit and costs of early screening for hearing disability: A study of potential screening tests and models. Health Technology Assessment, 11(42).1–294. 10.3310/hta11420 [DOI] [PubMed] [Google Scholar]
- Heffernan E., Coulson N. S., Henshaw H., Barry J. G., Ferguson M. A. (2016). Understanding the psychosocial experiences of adults with mild-moderate hearing loss: An application of Leventhal’s self-regulatory model. International Journal of Audiology, 55 Suppl 3(Suppl 3), S3–S12. 10.3109/14992027.2015.1117663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fougeyrollas P., Boucher N., Edwards G., Grenier Y., Noreau L. (2019). The disability creation process model: A comprehensive explanation of disabling situations as a guide to developing policy and service programs. Scandinavian Journal of Disability Research, 21(1), 25–37. Article 1. 10.16993/sjdr.62 [DOI] [Google Scholar]
- Fowler E., Woodside J. V., Kee F., Loughrey D., Lawlor B., McHugh Power J. (2022). Reconnecting to others: Grounded theory of social functioning following age-related hearing loss. Ageing and Society, 42(9), 2008–2025. 10.1017/s0144686x20001853 [DOI] [Google Scholar]
- Gilmour H. (2012). Social participation and the health and well-being of canadian seniors. Health Reports, 23(4), 23–32. [PubMed] [Google Scholar]
- Goman A. M., Gao T., Betz J., Reed N. S., Deal J. A., Lin F. R. (2021). Association of hearing loss with physical, social, and mental activity engagement. Seminars in Hearing, 42(1), 59–65. 10.1055/s-0041-1726001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gopinath B., Hickson L., Schneider J., McMahon C. M., Burlutsky G., Leeder S. R., Mitchell P. (2012). Hearing-impaired adults are at increased risk of experiencing emotional distress and social engagement restrictions five years later. Age and Ageing, 41(5), 618–623. 10.1093/ageing/afs058 [DOI] [PubMed] [Google Scholar]
- Gopinath B., Schneider J., Hickson L., McMahon C. M., Burlutsky G., Leeder S. R., Mitchell P. (2012). Hearing handicap, rather than measured hearing impairment, predicts poorer quality of life over 10 years in older adults. Maturitas, 72(2), 146–151. 10.1016/j.maturitas.2012.03.010 [DOI] [PubMed] [Google Scholar]
- Gopinath B., Schneider J., McMahon C. M., Teber E., Leeder S. R., Mitchell P. (2012). Severity of age-related hearing loss is associated with impaired activities of daily living. Age and Ageing, 41(2), 195–200. 10.1093/ageing/afr155 [DOI] [PubMed] [Google Scholar]
- Hay-McCutcheon M. J., Reed P. E., Cheimariou S. (2018). Positive social interaction and hearing loss in older adults living in rural and urban communities. Journal of Speech, Language, and Hearing Research: JSLHR, 61(8), 2138–2145. 10.1044/2018_JSLHR-H-17-0485 [DOI] [PubMed] [Google Scholar]
- Hearing Loss Association of America [HLAA] . (2018). Do you think you have a hearing loss? HLAA. https://www.hearingloss.org/wp-content/uploads/HLAA_DoYouThinkYouHave_Hearing-Loss.pdf?pdf=DoYouThink [Google Scholar]
- Heine C., Browning C. J. (2002). Communication and psychosocial consequences of sensory loss in older adults: Overview and rehabilitation directions. Disability and Rehabilitation, 24(15), 763–773. 10.1080/09638280210129162 [DOI] [PubMed] [Google Scholar]
- Heine C., Browning C. J. (2004). The communication and psychosocial perceptions of older adults with sensory loss: A qualitative study. Ageing and Society, 24(1), 113–130. 10.1017/S0144686X03001491 [DOI] [Google Scholar]
- Hickson L., Allen J., Beswick R., Fulton M., Wolf D., Worrall L., Scarinci N. (2008). Relationships between hearing disability, quality of life and wellbeing in older community-based Australians. Australian and New Zealand Journal of Audiology, 30(2), 99–112. 10.1375/audi.30.2.99 [DOI] [Google Scholar]
- Huang A. R., Deal J. A., Rebok G. W., Pinto J. M., Waite L., Lin F. R. (2021). Hearing Impairment and Loneliness in Older Adults in the United States. Journal of Applied Gerontology, 40(10), 1366–1371. [DOI] [PubMed] [Google Scholar]
- Ishigami Y., Jutai J., Kirkland S. (2021). Assistive device use among community-dwelling older adults: A profile of canadians using hearing, vision, and mobility devices in the Canadian longitudinal study on aging. Canadian Journal on Aging, 40(1), 23–38. 10.1017/S0714980819000692 [DOI] [PubMed] [Google Scholar]
- Jang Y., Mortimer J. A., Haley W. E., Small B. J., Chisolm T. E. H., Graves A. B. (2003). The role of vision and hearing in physical, social, and emotional functioning among older adults. Research on Aging, 25(2), 172–191. 10.1177/0164027502250019 [DOI] [Google Scholar]
- Johnson C. E., Danhauer J. L., Bennett M., Harrison J. (2009). Systematic review of physicians’ knowledge of, participation in, and attitudes toward hearing and balance screening in the elderly population. Seminars in Hearing, 30(03), 193–206. 10.1055/s-0029-1225404 [DOI] [Google Scholar]
- Jones C. A., Siever J., Knuff K., Van Bergen C., Mick P., Little J., Jones G., Murphy M.-A., Kurtz D., Miller H. (2019). Walk, talk and listen: A pilot randomised controlled trial targeting functional fitness and loneliness in older adults with hearing loss. BMJ Open, 9(4). e026169. 10.1136/bmjopen-2018-026169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr P., Stephens D. (2000). Understanding the nature and function of positive experiences in living with auditory disablement. Scandinavian Journal of Disability Research, 2(1), 21–38. 10.1080/15017410009510750 [DOI] [Google Scholar]
- Krawczyk C. S. (2001). Effects of acquired hearing loss on the psychosocial functioning of seniors. UMI Dissertation Services, ProQuest Information and Learning. https://search.ebscohost.com/login.aspx?direct=true&db=gnh&AN=908495&site=ehost-live [Google Scholar]
- Lazzarotto S., Baumstarck K., Loundou A., Hamidou Z., Aghababian V., Leroy T., Auquier P. (2016). Age-related hearing loss in individuals and their caregivers: Effects of coping on the quality of life among the dyads. Patient Preference and Adherence, 10, 2279–2287. 10.2147/PPA.S112750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazzarotto S., Baumstarck K., Moheng B., Leroy T., Auquier P. (2018). Determinants of the quality of life of the hearing-impaired elderly. Sante Publique (Vandoeuvre-Les-Nancy, France), 30(6), 811–820. 10.3917/spub.187.0811 [DOI] [PubMed] [Google Scholar]
- Lazzarotto S., Martin F., Saint-Laurent A., Hamidou Z., Aghababian V., Auquier P., Baumstarck K. (2019). Coping with age-related hearing loss: Patient-caregiver dyad effects on quality of life. Health and Quality of Life Outcomes, 17(1), 86. 10.1186/s12955-019-1161-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levac D., Colquhoun H., O’Brien K. K. (2010). Scoping studies: Advancing the methodology. Implementation Science: IS, 5(1), 69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levasseur M., Lussier-Therrien M., Biron M. L., Raymond É., Castonguay J., Naud D., Fortier M., Sévigny A., Houde S., Tremblay L. (2022). Scoping study of definitions of social participation: Update and co-construction of an interdisciplinary consensual definition. Age and Ageing, 51(2), afab215. 10.1093/ageing/afab215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levasseur M., Tribble D. S.-C., Desrosiers J. (2006). Analyse du concept qualité de vie dans le contexte des personnes âgées avec incapacités physiques. Canadian Journal of Occupational Therapy, 73(3), 163–177. 10.2182/cjot.05.0013 [DOI] [PubMed] [Google Scholar]
- Liljas A. E. M., Wannamethee S. G., Whincup P. H., Papacosta O., Walters K., Iliffe S., Lennon L. T., Carvalho L. A., Ramsay S. E. (2016). Hearing impairment and incident disability and all-cause mortality in older British community-dwelling men. Age and Ageing, 45(5), 661–666. 10.1093/ageing/afw080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litwin H., Shiovitz-Ezra S. (2006). The association between activity and wellbeing in later life: What really matters? Ageing and Society, 26(2), 225–242. 10.1017/S0144686X05004538 [DOI] [Google Scholar]
- Lopez D., McCaul K. A., Hankey G. J., Norman P. E., Almeida O. P., Dobson A. J., Byles J. E., Yeap B. B., Flicker L. (2011). Falls, injuries from falls, health related quality of life and mortality in older adults with vision and hearing impairment—Is there a gender difference? Maturitas, 69(4), 359–364. 10.1016/j.maturitas.2011.05.006 [DOI] [PubMed] [Google Scholar]
- McColl M. A., Law M. (2013). Interventions affecting self-care, productivity, and leisure among adults: A scoping review. OTJR: Occupation, Participation and Health, 33(2), 110–119. 10.3928/15394492-20130222-01 [DOI] [PubMed] [Google Scholar]
- Mick P., Kawachi I., Lin F. R. (2014). The association between hearing loss and social isolation in older adults. Otolaryngology-Head and Neck Surgery: Official Journal of American Academy of Otolaryngology-Head and Neck Surgery, 150(3), 378–384. 10.1177/0194599813518021 [DOI] [PubMed] [Google Scholar]
- Mikkola T. M., Polku H., Portegijs E., Rantakokko M., Tsai L.-T., Rantanen T., Viljanen A. (2016). Self-reported hearing is associated with time spent out-of-home and withdrawal from leisure activities in older community-dwelling adults. Aging Clinical and Experimental Research, 28(2), 297–302. 10.1007/s40520-015-0389-1 [DOI] [PubMed] [Google Scholar]
- Mikkola T. M., Portegijs E., Rantakokko M., Gagné J.-P., Rantanen T., Viljanen A. (2015). Association of self-reported hearing difficulty to objective and perceived participation outside the home in older community-dwelling adults. Journal of Aging and Health, 27(1), 103–122. 10.1177/0898264314538662 [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G., PRISMA Group . (2009). Preferred reporting Items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. 10.1371/journal.pmed1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan A., Hickson L., Worrall L. (2002). The impact of hearing impairment on quality of life of older people. Asia Pacific Journal of Speech, Language and Hearing, 7(1), 39–53. 10.1179/136132802805576562 [DOI] [Google Scholar]
- Moser S., Luxenberger W., Freidl W. (2017). The influence of social support and coping on quality of life among elderly with age-related hearing loss. American Journal of Audiology, 26(2), 170–179. 10.1044/2017_AJA-16-0083 [DOI] [PubMed] [Google Scholar]
- Munn Z., Peters M. D. J., Stern C., Tufanaru C., McArthur A., Aromataris E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18(1), 143. 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer A. D., Carder P. C., White D. L., Saunders G., Woo H., Graville D. J., Newsom J. T. (2019). The impact of communication impairments on the social relationships of older adults: Pathways to psychological well-being. Journal of Speech, Language, and Hearing Research: JSLHR, 62(1), 1–21. 10.1044/2018_JSLHR-S-17-0495 [DOI] [PubMed] [Google Scholar]
- Polku H., Mikkola T. M., Rantakokko M., Portegijs E., Törmäkangas T., Rantanen T., Viljanen A. (2016). Hearing and quality of life among community-dwelling older adults. The Journals of Gerontology: Series B: Psychological Sciences and Social Sciences, 73(3), 543–552. 10.1093/geronb/gbw045 [DOI] [PubMed] [Google Scholar]
- Pronk M., Deeg D. J. H., Kramer S. E. (2013). Hearing status in older persons: A significant determinant of depression and loneliness? Results from the longitudinal aging study amsterdam. American Journal of Audiology, 22(2), 316–320. 10.1044/1059-0889(2013/12-0069) [DOI] [PubMed] [Google Scholar]
- Pronk M., Deeg D. J. H., Smits C., Twisk J. W., van Tilburg T. G., Festen J. M., Kramer S. E. (2014). Hearing loss in older persons: Does the rate of decline affect psychosocial health? Journal of Aging and Health, 26(5), 703–723. 10.1177/0898264314529329 [DOI] [PubMed] [Google Scholar]
- Pryce H., Hall A., Laplante-Lévesque A., Clark E. (2016). A qualitative investigation of decision making during help-seeking for adult hearing loss. International Journal of Audiology, 55(11), 658–665. 10.1080/14992027.2016.1202455 [DOI] [PubMed] [Google Scholar]
- Ramage-Morin P. L. (2016). Hearing difficulties and feelings of social isolation among Canadians aged 45 or older. Health Reports, 27(11), 3–12. [PubMed] [Google Scholar]
- Raymond É., Lantagne Lopez M. (2020). Participation of people with impairments in seniors’ organizations: Conditions and limitations on inclusion. The Gerontologist, 60(6), 1126–1136. 10.1093/geront/gnaa011 [DOI] [PubMed] [Google Scholar]
- Schalock R. L. (2004). The concept of quality of life: What we know and do not know. Journal of Intellectual Disability Research: JIDR, 48(Pt 3), 203–216. 10.1111/j.1365-2788.2003.00558.x [DOI] [PubMed] [Google Scholar]
- Schneider J., Gopinath B., Karpa M. J., McMahon C. M., Rochtchina E., Leeder S. R., Mitchell P. (2010). Hearing loss impacts on the use of community and informal supports. Age and Ageing, 39(4), 458–464. 10.1093/ageing/afq051 [DOI] [PubMed] [Google Scholar]
- Shukla A., Cudjoe T. K. M., Lin F. R., Reed N. S. (2021). Functional hearing loss and social engagement among medicare beneficiaries. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 76(1), 195–200. 10.1093/geronb/gbz094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson A., Clarke S., Šarkić B., Smullen J. B., Pereira C. J. (2018). Internet usage and loneliness in older hearing aid wearers. Canadian Journal of Speech-Language Pathology and Audiology, 42(1), 69–79. [Google Scholar]
- Solheim J., Kværner K. J., Falkenberg E.-S. (2011). Daily life consequences of hearing loss in the elderly. Disability and Rehabilitation, 33(23–24), 2179–2185. 10.3109/09638288.2011.563815 [DOI] [PubMed] [Google Scholar]
- Southall K., Gagné J.-P., Jennings M. B. (2010). Stigma: A negative and a positive influence on help-seeking for adults with acquired hearing loss. International Journal of Audiology, 49(11), 804–814. 10.3109/14992027.2010.498447 [DOI] [PubMed] [Google Scholar]
- Strawbridge W. J., Wallhagen M. I., Shema S. J., Kaplan G. A. (2000). Negative consequences of hearing impairment in old age: A longitudinal analysis. The Gerontologist, 40(3), 320–326. 10.1093/geront/40.3.320 [DOI] [PubMed] [Google Scholar]
- Sung Y., Li L., Blake C., Betz J., Lin F. R. (2016). Association of hearing loss and loneliness in older adults. Journal of Aging and Health, 28(6), 979–994. 10.1177/0898264315614570 [DOI] [PubMed] [Google Scholar]
- Tomioka K., Ikeda H., Hanaie K., Morikawa M., Iwamoto J., Okamoto N., Saeki K., Kurumatani N. (2013). The Hearing Handicap Inventory for Elderly-Screening (HHIE-S) versus a single question: Reliability, validity, and relations with quality of life measures in the elderly community, Japan. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 22(5), 1151–1159. 10.1007/s11136-012-0235-2 [DOI] [PubMed] [Google Scholar]
- Tye-Murray N., Sommers M. S., Mauzé E., Schroy C., Barcroft J., Spehar B. (2012). Using patient perceptions of relative benefit and enjoyment to assess auditory training. Journal of the American Academy of Audiology, 23(8), 623–634. 10.3766/jaaa.23.8.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations . (2019). World population aging. United Nations. [Google Scholar]
- Viljanen A., Kaprio J., Pyykko I., Sorri M., Pajala S., Kauppinen M., Koskenvuo M., Rantanen T. (2009). Hearing as a predictor of falls and postural balance in older female twins. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 64A(2), 312–317. 10.1093/gerona/gln015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallhagen M. I. (2010). The stigma of hearing loss. The Gerontologist, 50(1), 66–75. 10.1093/geront/gnp107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein B. E., Sirow L. W., Moser S. (2016). Relating hearing aid use to social and emotional loneliness in older adults. American Journal of Audiology, 25(1), 54–61. Article 1. 10.1044/2015_AJA-15-0055 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2016). Global strategy on human resources for health: Workforce 2030. World Health Organization. https://apps.who.int/iris/handle/10665/250368 [Google Scholar]
- Zhang S., Moyes S., McLean C., Searchfield G., Welch D., Jacobs R., Kerse N. (2016). Self-reported hearing, vision and quality of life: Older people in New Zealand. Australasian Journal on Ageing, 35(2), 98–105. 10.1111/j.1741-6612.2012.00627.x [DOI] [PubMed] [Google Scholar]
- Zunzunegui M.-V., Alvarado B. E., Del Ser T., Otero A. (2003). Social networks, social integration, and social engagement determine cognitive decline in community-dwelling Spanish older adults. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 58(2), S93–S100. 10.1093/geronb/58.2.S93 [DOI] [PMC free article] [PubMed] [Google Scholar]