Abstract
Weight recurrence after one-anastomosis gastric bypass (OAGB), the third most common metabolic and bariatric surgery performed worldwide, is observed in a subset of patients due to the chronic, progressive nature of obesity. Endoscopic revision of the OAGB (ER-OAGB) through full-thickness suturing to reduce the gastrojejunal anastomosis and gastric pouch is a potential alternative to surgical revision. Here, we present a case series of ER-OAGB and long-term nutritional support at two international centers with expertise in bariatric endoscopy. Data were retrospectively evaluated from a prospectively maintained database. The primary outcome was total body weight loss (TBWL) at 12 months. Secondary outcomes included TBWL at 3, 6, and 15 months; excess weight loss (EWL) at 3, 6, 12, and 15 months; frequency of new/worsening symptoms of gastroesophageal reflux disease (GERD); and the frequency of serious adverse events. In this series, 17 adults (70.6% female, mean age 46.8 years, mean BMI 39.1 kg/m2) successfully underwent ER-OAGB an average of 8 years (range 2–21 years) after OAGB for a mean weight recurrence of 43.2% (range 10.9–86.9%). TBWL from ER-OAGB was 9.7 ± 1.8% at 3 months, 13.4 ± 3.5% at 6 months, 18.5 ± 2.1% at 12 months, and 18.1 ± 2.2% at 15 months. EWL from ER-OAGB was 30.5 ± 14.7% at 3 months, 42.6 ± 16.2% at 6 months, 54.2 ± 11.3% at 12 months, and 54.2 ± 11.7% at 15 months. There were no instances of new/worsening GERD symptoms or serious adverse events. In this small series of adults who experienced weight recurrence after OAGB, ER-OAGB facilitated safe and clinically meaningful weight loss, without new or worsening GERD symptoms, when performed by experienced bariatric endoscopists in concert with longitudinal nutritional support.
Keywords: case series, endoscopic revision, one-anastomosis gastric bypass, weight recurrence
Plain Language Summary
Endoscopic revision of one-anastomosis gastric bypass for weight recurrence
The one-anastomosis gastric bypass (OAGB) is now the third most commonly performed metabolic and bariatric surgery worldwide. As with other weight loss surgeries, the OAGB is associated with weight recurrence over time that prompts patients to seek further treatment; however, revisional surgeries are known to carry increased risk. The endoscopic revision of the OAGB (ER-OAGB) is an incisionless technique that reduces the gastrojejunal anastomosis and gastric pouch to facilitate weight loss after weight recurrence in OAGB. Here, we showed in a series of 17 adults that the ER-OAGB safely helped patients lose over 18% of their body weight within the year following their revision.
Introduction
Developed by Dr. Robert Rutledge in 1997 as a primary metabolic and bariatric surgery, the one-anastomosis gastric bypass (OAGB), formerly called the ‘mini gastric bypass’, involves the creation of a long, sleeve-like gastric pouch that is connected via a wide, 4–5 cm anastomosis to the uninterrupted jejunum approximately 150–200 cm distal to the ligament of Treitz.1–3 Compared to the Roux-en-Y gastric bypass (RYGB), the OAGB is faster, less technically challenging, and facilitates easier postoperative evaluation of both jejunal limbs.4–6 The OAGB has become the third most common bariatric surgery performed worldwide, and in May 2022, the American Society for Metabolic and Bariatric Surgery officially endorsed the surgery. 7 With this endorsement and the rising rate of global obesity, implementation of OAGB is anticipated to increase within the United States and worldwide.
As obesity is a chronic, progressive, relapsing disorder, weight recurrence following metabolic and bariatric surgery is common and expected. 8 Meta-analyses suggest that at least 7% of post-OAGB patients undergo surgical revision for insufficient weight loss response, 6 and weight recurrence comprises approximately 11–34% of cases undergoing revisional surgery after OAGB.9–12 Nevertheless, these interventions – which include conversion to RYGB or biliopancreatic limb elongation – carry heightened risk compared to the original surgery,6,9 in keeping with revisions of other metabolic and bariatric surgeries.13,14 As risk aversion is a formidable barrier for patients seeking surgical forms of weight loss, there is a growing need for safe, minimally invasive tools to address postsurgical weight recurrence as OAGB rates increase in the United States,15,16
Transoral outlet reduction (TORe) using the Overstitch endoscopic suturing system (Apollo Endosurgery, Austin, TX, USA) is FDA-authorized to treat weight recurrence after RYGB in adults with a BMI between 30 and 50 kg/m2. TORe involves full-thickness suturing of the gastrojejunal anastomosis (GJA), which is often dilated in patients with weight recurrence, to provide further restriction of the gastric outlet to promote satiety.17,18 Accordingly, reduction of the GJA in OAGB is a potential target to promote weight loss. A second endoscopic target for weight recurrence after OAGB is full-thickness suturing of the long sleeve-like gastric pouch, as has been successfully performed for weight recurrence following vertical sleeve gastrectomy19,20 and which comports with weight loss success from surgical resizing of a dilated gastric pouch after OAGB. 21
GJA and gastric pouch reduction may allow endoscopic revision of OAGB (ER-OAGB) (Figure 1) to halt and reverse weight recurrence and its associated detrimental metabolic, psychosocial, and economic effects.22–24 To date, ER-OAGB for weight recurrence has not been described in the literature. Further, there are OAGB-specific concerns that restriction of the GJA and/or pouch may be detrimental to pouch clearance and thus promote debilitating symptoms of gastroesophageal reflux from either biliary or gastric acid origin.2,12,25–28 To address these knowledge gaps, we present a case series of 17 adult patients who underwent ER-OAGB at two centers with expertise in bariatric endoscopy to highlight the clinical efficacy and safety of this novel approach in the outpatient setting.
Figure 1.

Endoscopic revision of the one-anastomosis gastric bypass (ER-OAGB). As indicated by the arrows, the components of ER-OAGB include circumferential narrowing of the gastrojejunal anastomosis (inset) and reduction of the sleeve-like gastric pouch, both through full-thickness endoscopic suturing.
Methods
Data were retrospectively analyzed from two prospectively maintained center-specific databases of patients who underwent ER-OAGB for the primary indication of weight recurrence. The study was granted an Institutional Review Board exemption (WCG IRB, Puyallup, WA, USA). The reporting of this study conforms to the Case Report (CARE) Guidelines. 29
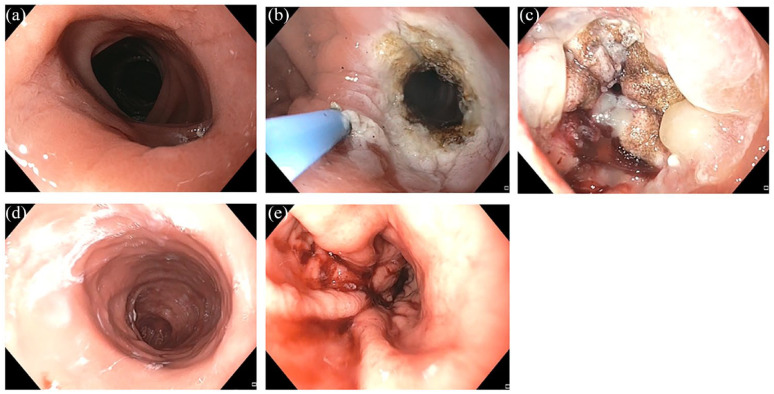
All procedures were performed under general anesthesia on an outpatient basis by one of two experienced bariatric endoscopists (AH, CM) using a dual-channel therapeutic endoscope (FUJIFILM Medical Systems, Lexington, MA, USA) and the Overstitch endoscopic suturing system (Apollo Endosurgery, Inc., Austin, Texas, USA). Six ER-OAGB cases were performed by CM and 11 by AH at their respective institutions. Prior to ER-OAGB, an endoscopic evaluation with a single-channel gastroscope was performed to assess the gastric pouch and the GJA for size, health, and presence of pathology (including stoma and pouch dilation). Pouch length was measured via standard scope markings, and GJA diameter was estimated visually relative to the endoscope and/or endoscopic tools, as is standard practice in TORe.30,31 If present, visible surgical material was removed from the GJA with forceps and/or endoscopic scissors. If no contraindications to ER-OAGB were identified, gastric tissue surrounding the GJA was circumferentially ablated using argon plasma coagulation (80 W, 1.2 L/min) for a golden-brown effect approximately 5–10 mm in width. A dual-channel therapeutic gastroscope equipped with Overstitch endoscopic suturing system was then used to perform a purse-string outlet reduction as described previously. 32 Outlet reduction was performed with suture tightening over a through-the-scope fluid-filled balloon inserted through the GJA for a consistent final outlet diameter. Further reduction of the dilated gastric pouch was then performed with a series of U-shaped sutures rows placed sequentially from the GJA to the proximal gastric pouch. The endoscopic view of procedural steps is shown in Figure 2. All patients were discharged home same-day and enrolled in a comprehensive lifestyle and nutrition program that included regular follow-up with registered dietitians.
Figure 2.
Steps of ER-OAGB. (a) Gastrojejunostomy (outlet) before revision. (b) Argon plasma coagulation of outlet. (c) Purse-string suture of outlet. (d) Gastric pouch before revision and (e) Endoscopic suturing to narrow pouch.
ER-OAGB, endoscopic revision of OAGB; OAGB, one-anastomosis gastric bypass.
Calculations:
- Total body weight loss (TBWL) = (weight at time of intervention – weight at time point)/weight at time of intervention × 100
- Excess weight loss (EWL) = (weight at time of intervention − weight for BMI of 25)/weight at time of intervention × 100
- Weight recurrence = (weight at time of ER-OAGB − nadir weight after OAGB)/(weight at time of OAGB − nadir weight after OAGB) ×100.
The primary outcome was TBWL at 12 months. Secondary outcomes were technical feasibility (defined as the ability to complete the procedure with reduction of the GJA and gastric pouch); suture number; TBWL at 3, 6, and 15 months; EWL at 3, 6, 12, and 15 months; improvement, worsening or de novo symptoms of gastroesophageal reflux disease (GERD) following ER-OAGB by 12 months (per patient report of symptoms); and safety. Patients were monitored for adverse events throughout the follow-up period, which were graded according to standard definitions. 33 Baseline comorbidities were based on presence of medication used to treat the respective condition; hemoglobin A1c ⩾ 6.5% (type 2 diabetes mellitus); controlled attenuation parameter ⩾248 dB/m via transient elastography (hepatic steatosis); and/or diagnosis from another physician. Continuous variables were reported as means ± standard deviation or ranges, and categorical variables as frequencies and percentages, unless otherwise specified.
Results
A total of 17 patients (70.6% female, mean age 46.8 years, mean BMI 39.1 kg/m2) underwent ER-OAGB from June 2020 to September 2021. Patient characteristics are shown in Table 1. At the time of ER-OAGB, patients had the following obesity-associated comorbidities: hypertension (n = 7), type 2 diabetes mellitus (n = 4), and hepatic steatosis (n = 9). The average time from initial OAGB to ER-OAGB was 8 years (range 2–21 years), with an average weight recurrence at the time of ER-OAGB of 43.2% (range 10.9–86.9%) from post-OAGB nadir. The mean procedure duration was 23 min. All procedures included one purse-string suture, with an average of 2 (range 1–5) sutures for pouch reduction. Technical success was 100%. There were no instances of gastrogastric fistula identified during ER-OAGB. Patient follow-up rates at 3, 6, 12, and 15 months were 94.1% (16/17), 94.1% (16/17), 100% (12/12), and 62.5% (5/8), respectively. TBWL was 18.5 ± 2.1% at 12 months. Overall TBWL trajectory from time of OAGB to 15 months after ER-OAGB is show in Figure 3. As demonstrated in this figure, patients re-approached their post-OAGB weight nadir following ER-OAGB. EWL at 3, 6, 12, and 15 months after ER-OAGB was 30.5 ± 14.7%, 42.6 ± 16.2%, 54.2 ± 11.3%, and 54.2 ± 11.7%, respectively. Data on GERD at baseline and 12 months were available for 12 (70.6%) subjects. Of these, three (25.0%) had GERD at the time of ER-OAGB. At 12 months, GERD symptoms resolved in 2 of the 3 subjects and remained unchanged in 1 of the 3 subjects. There were no reported instances of new or worsening GERD. There were no serious adverse events for any patient during the study duration. Immediate postprocedural symptoms following ER-OAGB are similar to those observed following TORe in RYGB – namely, 1–2 days of mild cramping and substernal pressure/dyspepsia.
Table 1.
Cohort characteristics. Values are presented as median (range) or mean ± standard deviation.
| Patient characteristic | Value |
|---|---|
| Age at time of ER-OAGB (years) | 46 (range 37–71) |
| No. female (%) | 12 (70.6) |
| BMI at time of ER-OAGB (kg/m2) | 39.1 ± 6.6 |
| Total body weight loss from OAGB to post-OAGB weight nadir (%) | 35.9 ± 10.7 |
| Excess weight loss from OAGB to post-OAGB weight nadir (%) | 77.9 ± 24.3 |
| Time from OAGB to ER-OAGB (years) | 8 (range 2–21) |
| Weight recurrence from post-OAGB weight nadir (%) | 43.2 ± 23.4 |
| Comorbidities at time of ER-OAGB, n (%) | |
| Hypertension | 7 (41.2) |
| Type 2 diabetes mellitus | 4 (23.5) |
| Hepatic steatosis | 9 (52.9) |
BMI, body mass index; ER-OAGB, endoscopic revision of one-anastomosis gastric bypass; OAGB, one-anastomosis gastric bypass.
Figure 3.
Weight Loss trajectory before and after ER-OAGB. Mean TBWL over time from original OAGB and from ER-OAGB are shown at corresponding time points.
ER-OAGB, endoscopic revision of one-anastomosis gastric bypass; OAGB, one-anastomosis gastric bypass; TBWL, total body weight loss.
Discussion
Consistent with the paradigm of obesity as a chronic, progressive disorder, OAGB appears to be subject to the same challenges of weight recurrence observed in other metabolic and bariatric surgeries,6,34,35 a phenomenon associated with recrudescence of comorbidities, increased health care cost, and diminished quality of life.22–24,36 Given the rising rates of both obesity and implementation of OAGB, there is a need for minimally invasive revisional therapies for weight recurrence, which may reduce the need for riskier revisional surgeries or life-long anti-obesity pharmacotherapy.37–39 This is the first account documenting the clinical efficacy and safety of full-thickness suturing post-OAGB to treat weight recurrence.
Patients undergoing ER-OAGB experienced similar weight loss to that observed in patients who underwent TORe and endoscopic revisions of sleeve gastrectomy at our centers, as well as similar to those observed in the published literature on these procedures18,19 – namely, modest compared to the initial surgery but satisfying weight loss and safety thresholds outlined in expert-level recommendations for adoption of a novel endobariatric therapy 40 and likely sufficient to improve weight-related medical comorbidities that may accompany weight recurrence. 41 In ER-OAGB, it is unclear whether GJA or pouch reduction contributes more significantly to the degree of weight loss, as both anatomical features can contribute to weight recurrence after metabolic bariatric surgery.42,43 Nevertheless, we suspect tissue ablation with the purse-string approach to GJA narrowing is preferable to tissue ablation alone or interrupted suture technique, as was shown with TORe.32,44 We also suspect that the specific suture pattern of the gastric pouch is less consequential, as it does not appear to be a major determinant of weight loss in the analogous gastric imbrication of endoscopic sleeve gastroplasty. 45 Though none were encountered in this series, as with TORe, gastrogastric fistula must be managed as part of a revision for weight management after OAGB, and this can be attempted endoscopically.46,47
A major concern of OAGB is the risk of GERD, which is observed in 5–10% of patients after OAGB and leads to revision in 2–3%.2,12,28 Historically, the prevailing speculation was that reflux was primarily biliary in nature, owing to surgical technique.27,48 While transient biliary reflux has been demonstrated after OAGB, 26 further study has demonstrated nearly equal frequency of acid reflux. 25 To manage GERD, there is consensus among experts that the gastric pouch should be as long as permitted by the patient’s anatomy, while also avoiding practices that may contribute to impaired pouch clearance of food contents, bile, or acid – such as creating an overly narrowed pouch or GJA. 2 Accordingly, many experts construct the GJA with a diameter between 40 and 50 mm, 2 and in series of patients with more narrowed GJA, there were increased reports of GERD.49,50
In the present series of ER-OAGB, both the pouch and GJA were intentionally narrowed, anatomical modifications that are hypothesized to impede pouch clearance. In this manner, it may be surprising that no patient in this series described new or worsening GERD. The reasons for this are not clear. There are OAGB surgical techniques that ostensibly help prevent reflux of both acid and bile that are unrelated to the modification from ER-OAGB – such as resection of gastric tissue (diminishing acid), as well as dependent-placement and latero-lateral construction of the GJA (attenuating bile reflux). 25 An alternative explanation is that these ER-OAGB modifications are, in some ways, protective against reflux. First, the gastric pouch is exposed to transient, physiologic biliary flow due to lack of a sphincter, and narrowing of the GJA may generate an anatomical barrier. 25 Second, the elasticity of gastric tissue can lead to pouch dilation over time, especially if involving the greater curvature, and this can lead to meal stagnation3,28 – a phenomenon potentially mediated by pouch reduction. Finally, GERD is a comorbidity associated with increased abdominal pressure from central adiposity, and thus, weight loss observed in this case series may itself be a protective factor against GERD. 51 Ultimately, improvement in or worsening of GERD is likely to be multifactorial with ER-OAGB, and future study may include pH-impedance testing to help inform appropriate patient selection based on type and severity of reflux, as has been done to guide surgical revision of OAGB. 28
This case series suggests that ER-OAGB can serve as a promising weight loss tool for patients with weight recurrence after OAGB wishing to avoid surgical revision or long-term anti-obesity pharmacotherapy. However, given the small size of this cohort, further validation is needed to confirm the efficacy and safety of this technique, including the frequency of outlet stenosis, which is observed in approximately 3–4% of patients undergoing the analogous TORe procedure, but which was not observed here. 44 Additionally, further study could expand on this series’ limitations through thorough and objective assessment of the effects of ER-OAGB on weight-related medical conditions and GERD (from bile or acid). Still, given that TORe has FDA authorization for patients with weight recurrence after RYGB, OAGB use is increasing, and there is growing interest from physicians and patients in endobariatric therapies, it stands to reason that patients will seek out ER-OAGB in increasing numbers. Centers offering endobariatric therapies, especially revisional procedures, should be prepared to encounter such patients.
Supplemental Material
Supplemental material, sj-jpg-1-cmg-10.1177_26317745231210120 for Endoscopic revision of one-anastomosis gastric bypass (ER-OAGB) for weight recurrence: a case series of 17 adults by Daniel B. Maselli, Anna C. Hoff, Ashley Kucera, Areebah Waseem, Chase Wooley, Lauren L. Donnangelo, Brian Coan and Christopher E. McGowan in Therapeutic Advances in Gastrointestinal Endoscopy
Acknowledgments
None.
Footnotes
ORCID iD: Daniel B. Maselli  https://orcid.org/0000-0002-8605-6966
https://orcid.org/0000-0002-8605-6966
Contributor Information
Daniel B. Maselli, True You Weight Loss, Atlanta, GA, USA
Anna C. Hoff, Clinica Angioskope, Sao Paulo, Brazil
Ashley Kucera, True You Weight Loss, Cary, NC, USA.
Areebah Waseem, True You Weight Loss, Cary, NC, USA.
Chase Wooley, True You Weight Loss, Cary, NC, USA.
Lauren L. Donnangelo, True You Weight Loss, Atlanta, GA, USA
Brian Coan, True You Weight Loss, Cary, NC, USA.
Christopher E. McGowan, Medical Director and Research Director, True You Weight Loss, 2001 Weston Parkway, Cary, NC 27513, USA.
Declarations
Ethics approval and consent to participate: The study followed the ethical principles outlined in the Declaration of Helsinki and is consistent with the Good Clinical Practices recommendation. The study was granted an Institutional Review Board exemption (WCG IRB, Puyallup, WA). Informed consent was obtained from all individual participants included in the study.
Consent for publication: All individual participants consented to have their de-identified data published in a scientific journal.
Author contributions: Daniel B. Maselli: Data curation; Formal analysis; Writing – original draft; Writing – review & editing.
Anna C. Hoff: Data curation; Investigation; Writing – review & editing.
Ashley Kucera: Data curation; Methodology.
Areebah Waseem: Data curation; Writing – original draft; Writing – review & editing.
Chase Wooley: Data curation; Formal analysis; Writing – review & editing.
Lauren L. Donnangelo: Writing – review & editing.
Brian Coan: Writing – review & editing.
Christopher E. McGowan: Conceptualization; Data curation; Formal analysis; Investigation; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The following authors are or previously have been consultants for Apollo Endosurgery (Austin, TX, USA), which is the manufacturer of the endoscopic suturing device used for ER-OAGB: Daniel B. Maselli, MD; Anna C. Hoff. MD, MSc; Christopher E. McGowan, MD, MSCR, AGAF, FASGE.
Availability of data and materials: Data used in preparation of this manuscript can be made available upon request.
References
- 1. Chaim EA, Ramos AC, Cazzo E. Mini-gastric bypass: description of the technique and preliminary results. Arq Bras Cir Dig 2017; 30: 264–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mahawar KK, Parmar C, Graham Y. One anastomosis gastric bypass: key technical features, and prevention and management of procedure-specific complications. Minerva Chir 2019; 74: 126–136. [DOI] [PubMed] [Google Scholar]
- 3. Mahawar KK. Key features of an ideal one anastomosis/mini-gastric bypass pouch. Obes Surg 2017; 27: 1630–1631. [DOI] [PubMed] [Google Scholar]
- 4. Lee WJ, Ser KH, Lee YC, et al. Laparoscopic Roux-en-Y vs. Mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg 2012; 22: 1827–1834. [DOI] [PubMed] [Google Scholar]
- 5. Rheinwalt KP, Plamper A, Rückbeil MV, et al. One anastomosis gastric bypass-mini-gastric bypass (OAGB-MGB) versus Roux-en-Y gastric bypass (RYGB)-a mid-term cohort study with 612 patients. Obes Surg 2020; 30: 1230–1240. [DOI] [PubMed] [Google Scholar]
- 6. Khrucharoen U, Juo YY, Chen Y, et al. Indications, operative techniques, and outcomes for revisional operation following mini-gastric bypass-one anastomosis gastric bypass: a systematic review. Obes Surg 2020; 30: 1564–1573. [DOI] [PubMed] [Google Scholar]
- 7. Haddad A, Bashir A, Fobi M, et al. The IFSO worldwide one anastomosis gastric bypass survey: techniques and outcomes? Obes Surg 2021; 31: 1411–1421. [DOI] [PubMed] [Google Scholar]
- 8. Bray GA, Kim KK, Wilding JPH, et al. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev 2017; 18: 715–723. [DOI] [PubMed] [Google Scholar]
- 9. Musella M, Vitiello A, Susa A, et al. Revisional surgery after one anastomosis/minigastric bypass: an Italian multi-institutional survey. Obes Surg 2022; 32: 256–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Voon K, Huang CK, Patel A, et al. Conversion of one-anastomosis gastric bypass (OAGB) to Roux-en-Y gastric bypass (RYGB) is effective in dealing with late complications of OAGB: experience from a tertiary bariatric center and literature review. J Metab Bariatr Surg 2021; 10: 32–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lee WJ, Lee YC, Ser KH, et al. Revisional surgery for laparoscopic minigastric bypass. Surg Obes Relat Dis 2011; 7: 486–491. [DOI] [PubMed] [Google Scholar]
- 12. Chevallier JM, Arman GA, Guenzi M, et al. One thousand single anastomosis (omega loop) gastric bypasses to treat morbid obesity in a 7-year period: outcomes show few complications and good efficacy. Obes Surg 2015; 25: 951–958. [DOI] [PubMed] [Google Scholar]
- 13. Shimizu H, Annaberdyev S, Motamarry I, et al. Revisional bariatric surgery for unsuccessful weight loss and complications. Obes Surg 2013; 23: 1766–1773. [DOI] [PubMed] [Google Scholar]
- 14. Mahawar KK, Graham Y, Carr WR, et al. Revisional Roux-en-Y gastric bypass and sleeve gastrectomy: a systematic review of comparative outcomes with respective primary procedures. Obes Surg 2015; 25: 1271–1280. [DOI] [PubMed] [Google Scholar]
- 15. Imbus JR, Voils CI, Funk LM. Bariatric surgery barriers: a review using Andersen’s model of health services use. Surg Obes Relat Dis 2018; 14: 404–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wharton S, Serodio KJ, Kuk JL, et al. Interest, views and perceived barriers to bariatric surgery in patients with morbid obesity. Clin Obes 2016; 6: 154–160. [DOI] [PubMed] [Google Scholar]
- 17. Vargas EJ, Bazerbachi F, Rizk M, et al. Transoral outlet reduction with full thickness endoscopic suturing for weight regain after gastric bypass: a large multicenter international experience and meta-analysis. Surg Endosc 2018; 32: 252–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jirapinyo P, Kumar N, AlSamman MA, et al. Five-year outcomes of transoral outlet reduction for the treatment of weight regain after Roux-en-Y gastric bypass. Gastrointest Endosc 2020; 91: 1067–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Maselli DB, Alqahtani AR, Abu Dayyeh BK, et al. Revisional endoscopic sleeve gastroplasty of laparoscopic sleeve gastrectomy: an international, multicenter study. Gastrointest Endosc 2021; 93: 122–130. [DOI] [PubMed] [Google Scholar]
- 20. de Moura DTH, Barrichello S, Jr, de Moura EGH, et al. Endoscopic sleeve gastroplasty in the management of weight regain after sleeve gastrectomy. Endoscopy 2020; 52: 202–210. [DOI] [PubMed] [Google Scholar]
- 21. Faul A, Chevallier JM, Poghosyan T. Dilated gastric pouch resizing for weight loss failure after one anastomosis gastric bypass. Obes Surg 2019; 29: 3406–3409. [DOI] [PubMed] [Google Scholar]
- 22. Sheppard CE, Lester EL, Chuck AW, et al. The economic impact of weight regain. Gastroenterol Res Pract 2013; 2013: 379564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sjöström L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. New Engl J Med 2004; 351: 2683–2693. [DOI] [PubMed] [Google Scholar]
- 24. Voorwinde V, Steenhuis IHM, Janssen IMC, et al. Definitions of long-term weight regain and their associations with clinical outcomes. Obes Surg 2020; 30: 527–536. [DOI] [PubMed] [Google Scholar]
- 25. Nehmeh WA, Baratte C, Rives-Lange C, et al. Acid reflux is common in patients with gastroesophageal reflux disease after one-anastomosis gastric bypass. Obes Surg 2021; 31: 4717–4723. [DOI] [PubMed] [Google Scholar]
- 26. Saarinen T, Räsänen J, Salo J, et al. Bile reflux scintigraphy after mini-gastric bypass. Obes Surg 2017; 27: 2083–2089. [DOI] [PubMed] [Google Scholar]
- 27. Musella M, Vitiello A. The eternal dilemma of the bile into the gastric pouch after OAGB: do we need to worry? Obes Surg 2021; 31: 426–427. [DOI] [PubMed] [Google Scholar]
- 28. Tarhini A, Rives-Lange C, Jannot AS, et al. One-anastomosis gastric bypass revision for gastroesophageal reflux disease: long versus short biliopancreatic limb Roux-en-Y gastric bypass. Obes Surg 2022; 32: 970–978. [DOI] [PubMed] [Google Scholar]
- 29. Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Glob Adv Health Med 2013; 2: 38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Brunaldi VO, Peixoto de Oliveira GH, Kerbage A, et al. Long-term follow-up after transoral outlet reduction following Roux-en-Y gastric bypass: back to stage 0? Endosc Int Open 2023; 11: E538–E545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Galvao Neto M, Brunaldi VO, Grecco E, et al. Good clinical practices on argon plasma coagulation treatment for weight regain associated with dilated gastrojejunostomy following Roux-en-Y gastric bypass: a Brazilian-modified delphi consensus. Obes Surg 2022; 32: 273–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schulman AR, Kumar N, Thompson CC. Transoral outlet reduction: a comparison of purse-string with interrupted stitch technique. Gastrointest Endosc 2018; 87: 1222–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 2010; 71: 446–454. [DOI] [PubMed] [Google Scholar]
- 34. Maciejewski ML, Arterburn DE, Van Scoyoc L, et al. Bariatric surgery and long-term durability of weight loss. JAMA Surg 2016; 151: 1046–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cooper TC, Simmons EB, Webb K, et al. Trends in weight regain following Roux-en-Y gastric bypass (RYGB) bariatric surgery. Obes Surg 2015; 25: 1474–1481. [DOI] [PubMed] [Google Scholar]
- 36. Istfan NW, Lipartia M, Anderson WA, et al. Approach to the patient: management of the post–bariatric surgery patient with weight regain. J Clin Endocrinol Metab 2021; 106: 251–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mechanick JI, Apovian C, Brethauer S, et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures – 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg Obes Relat Dis 2020; 16: 175–247. [DOI] [PubMed] [Google Scholar]
- 38. Brethauer SA, Kothari S, Sudan R, et al. Systematic review on reoperative bariatric surgery: American society for metabolic and bariatric surgery revision task force. Surg Obes Relat Dis 2014; 10: 952–972. [DOI] [PubMed] [Google Scholar]
- 39. Himpens J, Coromina L, Verbrugghe A, et al. Outcomes of revisional procedures for insufficient weight loss or weight regain after Roux-en-Y gastric bypass. Obes Surg 2012; 22: 1746–1754. [DOI] [PubMed] [Google Scholar]
- 40. ASGE/ASMBS Task Force on Endoscopic Bariatric Therapy. A pathway to endoscopic bariatric therapies. Surg Obes Relat Dis 2011; 7: 672–682. [DOI] [PubMed] [Google Scholar]
- 41. Ryan DH, Yockey SR. Weight loss and improvement in comorbidity: differences at 5%, 10%, 15%, and over. Curr Obes Rep 2017; 6: 187–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Roberts K, Duffy A, Kaufman J, et al. Size matters: gastric pouch size correlates with weight loss after laparoscopic Roux-en-Y gastric bypass. Surg Endosc 2007; 21: 1397–1402. [DOI] [PubMed] [Google Scholar]
- 43. Bonaldi M, Rubicondo C, Giorgi R, et al. Re-sleeve gastrectomy: weight loss, comorbidities and gerd evaluation in a large series with 5 years of follow-up. Updates Surg 2023; 75: 959–965. [DOI] [PubMed] [Google Scholar]
- 44. Jaruvongvanich V, Vantanasiri K, Laoveeravat P, et al. Endoscopic full-thickness suturing plus argon plasma mucosal coagulation versus argon plasma mucosal coagulation alone for weight regain after gastric bypass: a systematic review and meta-analysis. Gastrointest Endosc 2020; 92: 1164–1175.e6. [DOI] [PubMed] [Google Scholar]
- 45. Espinet-Coll E, Nebreda-Durán J, Galvao-Neto M, et al. Suture pattern does not influence outcomes of endoscopic sleeve gastroplasty in obese patients. Endosc Int Open 2020; 8: E1349–E1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ribeiro-Parenti L, De Courville G, Daikha A, et al. Classification, surgical management and outcomes of patients with gastrogastric fistula after Roux-en-Y gastric bypass. Surg Obes Relat Dis 2017; 13: 243–248. [DOI] [PubMed] [Google Scholar]
- 47. Dolan RD, Jirapinyo P, Maahs ED, et al. Endoscopic closure versus surgical revision in the management of gastro-gastric fistula following Roux-en-Y gastric bypass. Endosc Int Open 2023; 11: E629–E634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. M’Harzi L, Chevallier JM, Certain A, et al. Long-term evaluation of biliary reflux on esogastric mucosae after one-anastomosis gastric bypass and esojejunostomy in rats. Obes Surg 2020; 30: 2598–2605. [DOI] [PubMed] [Google Scholar]
- 49. Shenouda MM, Harb SE, Mikhail SAA, et al. Bile gastritis following laparoscopic single anastomosis gastric bypass: pilot study to assess significance of bilirubin level in gastric aspirate. Obes Surg 2018; 28: 389–395. [DOI] [PubMed] [Google Scholar]
- 50. Doulami G, Triantafyllou S, Albanopoulos K, et al. Acid and nonacid gastroesophageal reflux after single anastomosis gastric bypass. An objective assessment using 24-hour multichannel intraluminal impedance-pH metry. Surg Obes Relat Dis 2018; 14: 484–488. [DOI] [PubMed] [Google Scholar]
- 51. Singh S, Sharma AN, Murad MH, et al. Central adiposity is associated with increased risk of esophageal inflammation, metaplasia, and adenocarcinoma: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 2013; 11: 1399–1412.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-jpg-1-cmg-10.1177_26317745231210120 for Endoscopic revision of one-anastomosis gastric bypass (ER-OAGB) for weight recurrence: a case series of 17 adults by Daniel B. Maselli, Anna C. Hoff, Ashley Kucera, Areebah Waseem, Chase Wooley, Lauren L. Donnangelo, Brian Coan and Christopher E. McGowan in Therapeutic Advances in Gastrointestinal Endoscopy