Abstract
Fetus in fetu is an uncommon medical anomaly characterized by the presence of a malformed fetus within the body of a living twin. Although the retroperitoneum is the most typical location, occurrences in the sacrococcygeal and dorsolumbar regions are rare. Ongoing debates center around its embryopathogenesis, debating whether it is a highly specialized teratoma or a result of parasitic twinning in a monozygotic monochorionic diamniotic pregnancy. Notably, distinguishing factors such as vertebral bodies and limbs are pivotal in discerning FIF from teratomas. Diagnostic imaging techniques are integral for preoperative diagnosis, with histopathological examination confirming the condition’s presence
Keywords: fetus in fetu, CT, MRI, teratoma, myelomeningocele
Introduction
Fetus in fetu (FIF) is an exceptionally rare pathological condition characterized by the presence of a malformed fetal structure within the body of a living twin. 1 FIF is a congenital anomaly arising from abnormal embryonic development in a diamniotic monochorionic and monozygotic twin setting, where the parasitic twin develops abnormally within the host twin’s body. While accurate preoperative diagnosis can be based on radiological findings in some cases, in others, diagnosis is only confirmed through surgical intervention. The classification of FIF as a distinct entity or as a highly specialized teratoma remains a subject of debate. Notably, only a few cases, including those in the sacrococcygeal and thoracolumbar regions, have been documented.1,2 In this report, we present an unusual case of FIF accompanied by spinal dysraphism in the dorsolumbar region, emphasizing the essential role of computed tomography (CT) and magnetic resonance imaging (MRI) in both diagnosis and evaluation.
Case Report
A female patient, aged 6 months, presented with a history of a gradually enlarging mass located in the dorsolumbar region. The infant was delivered at full term via normal vaginal delivery, weighing 2980 g at birth. Upon physical examination, the mass exhibited a firm, smooth texture and was non-painful, displaying a lower limb-like structure (Figure 1). Laboratory tests yielded unremarkable findings, and tumor markers, including β-HCG, AFP, and CEA, fell within the reference range.
Figure 1.
Clinical photogram showed a mass similar to a lower limb-like structure in the back of the girl.
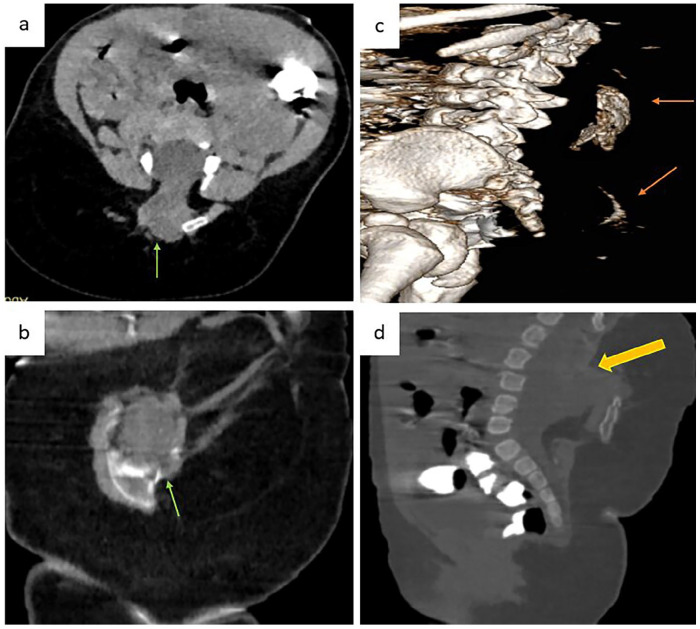
Computed tomography (CT) revealed a complex mass with a bony structure reminiscent of a hip bone and femur (Figure 2a, b, and c). The mass exhibited both cystic and solid components. Additionally, examination unveiled a spinal dorsolumbar dysraphism in the host, along with continuous adipose tissue within the epidural space connected to the mass (Figure 2d).
Figure 2.
(a-c) Axial, coronal and sagittal 3D CT images showed a mass (green arrow) with bony structure (orange arrow). (d) Axial bone reconstruction shows dorso-lumbar spinal dysraphism communicating with the mass (yellow arrow).
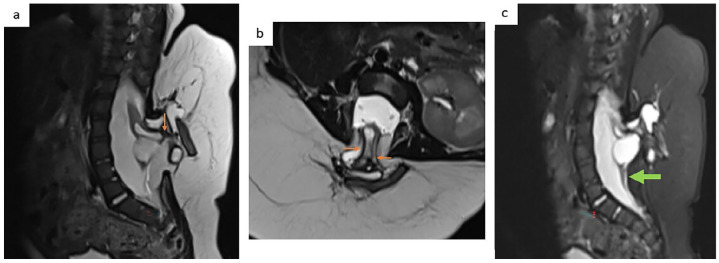
Magnetic resonance imaging (MRI) with T1 and T2 sequences (with and without fat suppression) disclosed a shared column between the mass and the host, highlighting a spinal defect in the posterior elements extending from D11 to L5. Notably, the mass was linked to the dilated thoracolumbar canal of the host, encompassing several nerve roots. This configuration resulted in a myelomeningocele with a tethered cord, with the conus medullaris terminating at the level of the fourth lumbar vertebra (see Figure 3). The filum terminale displayed thickening due to a filar lipoma and had been displaced into the sacral canal (Figure 4).
Figure 3.
(a-c) Axial and sagittal T2WI (with and without fat suppression) show that both share the same column with a spinal defect of the posterior elements from T12 to L5 onward, with nerve roots involvement compatible (orange arrows) with a myelomeningocele. Conus medullaris (green arrow).
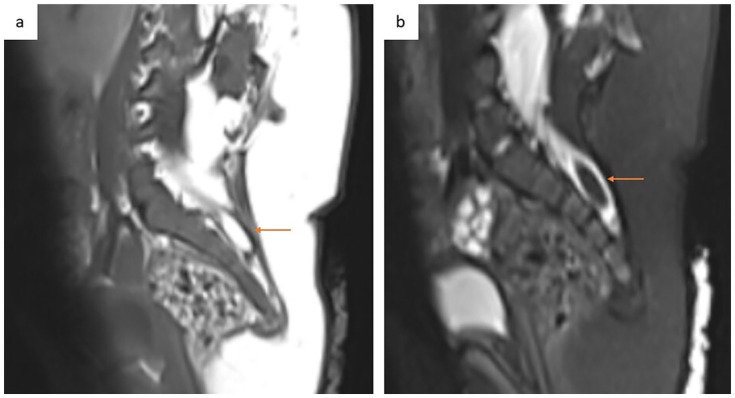
Figure 4.
(a and b) Sagittal T1WI and T2WI-FS show thickened filum terminale with filar lipoma dragged posterior in the sacral canal (orange arrows).
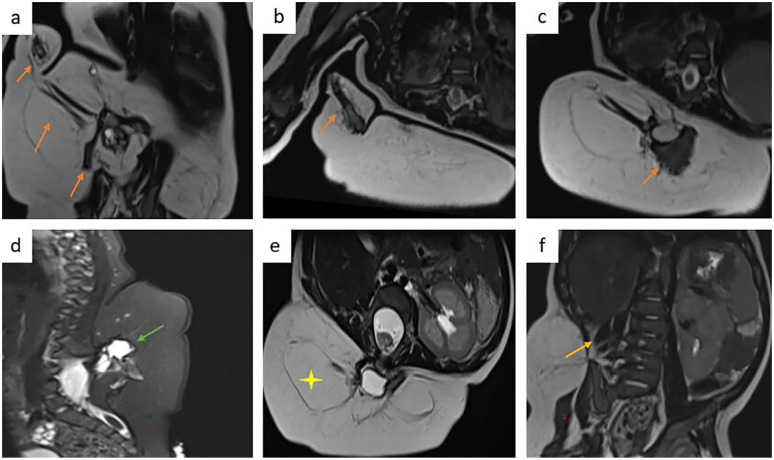
Furthermore, MRI imaging showcased the mass’s bone structure resembling that of a hip bone, femur, tibia, fibula, and phalanx (Figure 5a, b, and c), in addition to cystic lesions. Soft tissue components reminiscent of skeletal muscle were observed around joints, alongside bones and abundant subcutaneous adipose tissue (Figures 5d and e). Notably, associated right kidney agenesis was also apparent (Figure 5f).
Figure 5.
Coronal and axial T2WI (with and without fat suppression) showed mass with bony structure resembling hip bone, the femur, the tibia, the fibula and a phalanx (a-c) and with cystic lesions (d) soft tissue components similar to skeletal muscle around joints and abundant percutaneous adipose tissue (e). Right kidney agenesis (f).
A preoperative diagnosis of FIF was made and the discussion of neurosurgical intervention is ongoing; because the challenge in our case is the presence of myelomeningocele with a lack of cases describing this correlation in the scientific literature.
Discussion
Fetus in fetu (FIF) is typically identified during infancy, with the majority of cases being diagnosed before the age of 18 months. However, there have been instances of asymptomatic cases with delayed presentations, and notably, the oldest reported patient with FIF was a 47-year-old man.
Fetus in fetu (FIF) exhibits a male predominance, with a male-to-female ratio of 2:1. Most patients with FIF present with an abdominal mass within their first year of life. Nonetheless, it has been documented in various other locations, including the cranial cavity, oral cavity, neck, mediastinum, back, sacrococcygeal region, and even within the scrotum. 3
The precise embryogenesis of fetus in fetu (FIF) remains a subject of debate. Some researchers propose that FIF arises due to abnormal embryonic development within a diamniotic monochorionic twin pregnancy. In this scenario, a monozygotic twin with malformations becomes enclosed within the body of the other twin. Conversely, some experts classify it as a highly organized teratoma.
Typically, FIF cases involve a single fetus within the host, as in our case. However, there have been documented instances of multiple fetuses in fetu, ranging from 2 to 5 within a single host. The objective of this case report is to provide a detailed description of the characteristic computed tomography (CT) and magnetic resonance imaging (MRI) findings associated with this unusual and intriguing condition. 3
Various organ systems can be present within these fetuses. The vertebral column and limbs are 2 frequently observed organs. The ribs, central nervous systems, gastrointestinal tracts, vessels, and rarely thymic tissues can also be seen, among other organs. 3
The size and weight of FIF can vary, primarily depending on the blood supply, which is most commonly derived from the abdominal wall plexus. 3 In our case, the FIF has both nervous and vascular connections with the host, resulting in a larger size and better-developed features.
Because the majority of cases are in the abdomen, the symptoms of FIF are primarily caused by its mass impact and include abdominal distension, dysphagia, emesis, feeding problems, and jaundice. There have also been reports of dyspnea brought on by the tumor compressing the lung and neurological symptoms linked to intracranial FIF. Our case remained asymptomatic because the mass was located in the dorsolumbar region and was predominantly exophytic.
Imaging plays a crucial role in the preoperative diagnosis and follow-up of FIF. Radiographs are adequate when identifying vertebral columns and bony structures, such as limb bones. Ultrasonography is also valuable, serving as the primary imaging modality for prenatal and postnatal diagnosis due to its lack of ionizing radiation and convenience. 1
CT, especially with 3D reconstruction techniques, excels in displaying the vertebral column, limb buds with long bones, and various components like soft tissue, fat, and cysts within the mass. Additionally, contrast-enhanced CT can reveal feeding arteries and draining veins associated with FIF, offering insights into its relationship with adjacent organs and structures. 1
MRI, on the other hand, is a versatile tool for visualizing the intricate components of FIF. It boasts excellent soft tissue resolution and the ability to provide multiplanar imaging.
This entity differs from teratomas because they are an accumulation of pluripotential cells in which there is no organogenesis or vertebral segmentation. However, the current literature has described cases where both conditions are found to coexist. The distinguishing sign to differentiate a fetus in fetu from a teratoma is the presence of a separate vertebral column. The presence of vertebrae in FIF signifies an organized embryological development that involves the development of the notochord, the precursor of vertebral bones, during the primitive streak stage. In contrast, teratomas develop due to disorganized and uncontrolled pluripotent cell replication, and thus, vertebral segmentation and organogenesis are typically absent. 4 To classify a mass as FIF, it must exhibit one of the following features: a mass enclosed within a distinct sac, partially or completely covered by skin, and anatomical features that are recognizable to the naked eye. Additionally, it should be attached to the host by a pedicle containing a few relatively large blood vessels
It’s crucial to differentiate between FIF and teratoma due to the slight risk of malignancy associated with retroperitoneal teratomas. In contrast, FIF is almost always benign, with only one reported case of malignancy. Clinically, FIF can be distinguished from a teratoma by the presence of vertebrae and limbs. 2
Given that FIF grows in parallel with its host, surgical excision remains the primary treatment for this condition. with the removal of the fetus with its capsule. The prognosis of FIF is favorable in the most of the cases. However, a major coincidence of neurosurgical involvement like in our case has been the presence of meningocele, with a lack of cases describing this correlation in the scientific literature. The success of the resection is related to a multidisciplinary surgical intervention. 2 In our case, the participation of the pediatric neurosurgery team is fundamental for the patient’s prognosis due to their intervention in the closure of the thoracolumbar myelomeningocele.
Even though the different parts of FIF are developed, malignant transformation is still probable. After FIF resection, malignant change was noted. Therefore, careful clinical observation is required following surgery. Alpha-fetoprotein (AFP) or Beta-human chorionic gonadotropin (Beta-HCG) levels should be assessed in conjunction with imaging to identify any early indications of malignancy in the patient. 2
Conclusion
Fetus in fetu (FIF), an unusual congenital anomaly, predominantly manifests in the pediatric population. When FIF presents as an exophytic mass within the thoracolumbosacral region, patients might exhibit an absence of noticeable symptoms. The advancement of prenatal diagnostic methods has led to an enhanced detection rate for FIF, aided by the widespread utilization of imaging technologies. Notably, as exemplified in our case, magnetic resonance imaging (MRI) assumes a crucial role in unveiling potential anomalies associated with the sacral canal and conus medullaris in the host. The multidisciplinary approach and intervention of the pediatric neurosurgery specialty were of great importance since intervening on the associated neural tube.
Acknowledgments
We extend our heartfelt appreciation to our esteemed professors and dedicated colleagues whose invaluable contributions were instrumental in the culmination of this study.
Footnotes
Author Contributions: All authors contributed to this work.All authors have read and approved the final version of the manusctipt.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Ethical approval was not required for this case report since it is deemed not to constitute research at our institution.
Informed Consent: As for consent, the patient’s parent had provided written informed consent for the publication of her information.
Trial Registration: Not applicable.
Guarantor of Submission: The corresponding author is the guarantor of submission.
ORCID iDs: Meriem Zhim  https://orcid.org/0009-0006-4609-5297
https://orcid.org/0009-0006-4609-5297
Khadija Laasri  https://orcid.org/0000-0002-9766-4887
https://orcid.org/0000-0002-9766-4887
Amine Naggar  https://orcid.org/0000-0003-4841-0423
https://orcid.org/0000-0003-4841-0423
Soufiane Rostoum  https://orcid.org/0000-0003-2597-2626
https://orcid.org/0000-0003-2597-2626
References
- 1. Lu T, Ma J, Yang X. A rare case of fetus in fetu in the sacrococcygeal region: CT and MRI findings. BMC Pediatr. 2021;21:575. doi: 10.1186/s12887-021-03063-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cantarero MC, Osejo Cantarero A, Mendieta LR. The first case of fetus in Fetu in Nicaragua: the management experience of the Pediatric Neurosurgery Team. Cureus. 2023;15(1):e33835. doi: 10.7759/cureus.33835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sitharama SA, Jindal B, Vuriti MK, et al. Fetus in fetu: case report and brief review of literature on embryologic origin, clinical presentation, imaging and differential diagnosis. Pol J Radiol. 2017;82:46-49. doi: 10.12659/PJR.899956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jihwaprani MC, Mousa AA, Mohamed AA, Alkouz Y, Bahlawan IH. Fetus-in-fetu: a differential diagnosis of neonatal fetiform encysted abdominal mass. Cureus. 2023;15(1):e33725. doi: 10.7759/cureus.33725 [DOI] [PMC free article] [PubMed] [Google Scholar]