Abstract
Background:
Utilization of an emergency department (ED) visit for anterior cruciate ligament (ACL) injury is associated with high cost and diagnostic unreliability.
Hypothesis:
Patients initially evaluated at an ED for an ACL injury would be more likely to be from a lower income quartile, use public insurance, and experience a delay in treatment.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Patients in the Rhode Island All Payers Claims Database who underwent ACL reconstruction (ACLR) between 2012 and 2021 were identified using the Current Procedure Terminology (CPT) code 29888. Patients were stratified into 2 cohorts based on CPT codes for ED or in-office services within 1 year of ACLR. A chi-square analysis was used to test for differences between cohorts in patient and surgical characteristics. Multivariable linear and logistic regression were used to determine how ED evaluation affected timing and outcome variables.
Results:
While adjusting for patient and operative characteristics, patients in the ED cohort were more likely to have Medicaid (29% vs 12.5%; P < .001) and be in the lowest income quartile (44.6% vs 32.1%; P < .001). ED visit and Medicaid status were associated with increased time to (1) diagnostic magnetic resonance imaging, adding 7.97 days on average (95% CI, 4.14-11.79 days; P < .001) and 8.40 days (95% CI, 3.44-13.37 days; P = .001), respectively; and (2) surgery, adding 20.30 days (95% CI, 14.10-26.49 days; P < .001) and 12.88 days (95% CI, 5.15-20.60 days; P = .001), respectively. Patients >40 years who were evaluated in the ED were 2.5 times more likely to require subsequent ACLR (odds ratio, 2.50 [95% CI, 1.01-6.21]; P = .049).
Conclusion:
In this study, patients who visited the ED within 1 year before ACLR were more likely to have a lower income, public insurance, increased time to diagnostic imaging, and increased time to surgery, as well as decreased postoperative physical therapy use and increased subsequent ACLR rates in the 40-49 years age-group.
Keywords: anterior cruciate ligament, emergency department utilization, knee, socioeconomic disparities
Anterior cruciate ligament (ACL) injuries are among the most common ligament injuries, with a reported incidence between 100,000 and 200,000 injuries in the United States each year. 10 Delays in ACL reconstruction (ACLR) surgery leave patients susceptible to knee instability, osteoarthritis, and secondary injuries—such as medial and lateral meniscal tears, contralateral ACL injury, and chondral lesions.5,12
The utility of an emergency department (ED) visit in the setting of an acute ACL injury has recently been questioned. 16 Patients with an acute ACL injury are often under significant duress with considerable pain and swelling in the affected knee. It is easy to understand the impetus for patients to visit the ED to receive a diagnosis and early treatment. Unfortunately, it has been previously shown that ED providers do not diagnose these injuries accurately. 1 In addition, ED visits have been found to add a mean of US$4857 in cost to ACL injury care despite reduced diagnostic accuracy. 16
A previous study has found that patients with public insurance have a greater propensity to utilize the ED after a musculoskeletal injury. 6 The reasoning behind this for Medicaid patients is likely multifactorial but related in part to difficulty with booking timely appointments in an orthopaedic office. 21 Another contributing factor may be the longer wait times for magnetic resonance imaging (MRI) experienced by patients with Medicaid and other public insurance plans. 3 Some have also posited that lower health literacy among patients with public insurance plans may lead to overutilization of ED. 22 Considering these socioeconomic factors, the ED may be perceived as the sole access point for some patients into orthopaedic subspecialty care.
This study aimed to determine whether initial presentation to the ED after an ACL injury led to differences in time to care, utilization of postsurgical care, and postsurgical outcomes—such as a subsequent ACLR. We hypothesized that patients who initially presented to the ED would more likely be from a lower income quartile, use public insurance, and experience a delay in treatment.
Methods
Data Source
The Rhode Island All-Payer Claims Database (APCD) was utilized in this study. The APCD contains all health care insurance payment information for all people with health insurance in Rhode Island. Variables in this database include patient and provider characteristics, medical services utilized, ED visits, pharmacy claims, Current Procedural Terminology (CPT) codes, and International Classification of Disease, Ninth and Tenth Revisions (ICD-9 and ICD-10, respectively). This dataset does not include information on patients without health insurance, as well as claims by insurance companies with <3000 members. According to the Kaiser Family Foundation, 4.8% of Rhode Island’s population was uninsured in 2020. Therefore, data from about 95% of Rhode Islanders are included in this database. The protocol for this study received institutional review board approval.
Patient Selection
All patients in the APCD with a CPT code of 29888 (arthroscopically aided ACLR) between January 1, 2012, and December 31, 2021, were selected. The earliest ACLR claim for patients with multiple ACLRs was selected. Patients were divided into 2 cohorts—1 group initially presented to the ED for care (ED group) and 1 group initially presented to an office provider for care (non-ED group). The ED group was determined by identifying CPT codes for ED services for a musculoskeletal knee ICD-9 or ICD-10 code related to ACL injury within 1 year before their ACLR. The non-ED group was similarly identified using CPT codes for an office visit related to ACL, meniscal, or unspecified knee ligament injury within 1 year before their ACLR. Patients whose earliest evaluation was beyond 1 year before the ACLR were excluded to more confidently ensure that the evaluation for a knee injury was associated with the ACL injury. Patients >65 years, with Medicare, and with multiligamentous knee injuries—as defined by CPT codes 27405, 27427, and 29889 on the same day as ACLR—were excluded. A full list of the utilized ICD-9, ICD-10, and CPT codes for patient identification is presented in Appendix Table A1.
In total, 2226 patients with isolated ACLR or ACLR with meniscal repair were identified. Of these patients, 658 patients (29.6%) had a knee injury diagnosis in the ED within 1 year of ACLR (ED cohort), while 1568 patients (70.4%) had an ICD diagnosis of ACL tear, unspecified ligament sprain, or meniscal tear from an in-office visit (non-ED cohort). A full description of the inclusion and exclusion criteria is shown in Figure 1.
Figure 1.
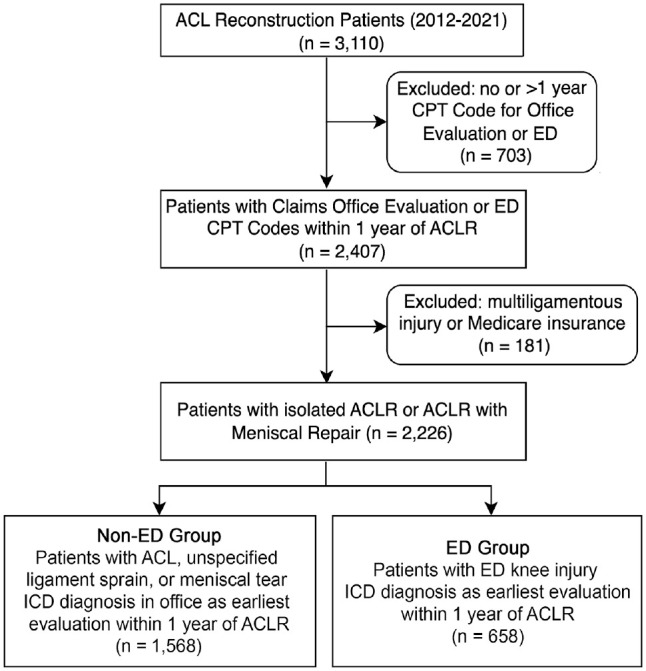
Flowchart of patient enrollment. ACLR, anterior cruciate ligament reconstruction; CPT, Current Procedural Terminology; ED, emergency department; ICD, International Classification of Diseases.
Statistical Analysis
A chi-square analysis with Bonferroni post hoc testing was used to test for differences in patient characteristics between the ED and non-ED groups. Multivariable linear regression models with time to surgery and time to MRI (CPT code, 73721) as outcome variables were used to model how much time to care an ED visit added while controlling for patient characteristics and operative variable differences between the groups. Multivariable logistic regression models were used to determine differences in the subsequent ACLR rate and use of physical therapy (PT) after surgery (CPT code, 97110). The following variables were used in the regression models: patient age, sex, income quartile of the patient’s ZIP code (according to 2020 US census data), insurance, concomitant meniscal repair, and allograft. Income quartiles were stratified as follows: quartile 1 (Q1) = < US$70,728; Q2 = US$70,728 to US$85,866; Q3 = US$85,867 to US$103,955, and Q4 = ≥ US$103,956. Age-groups were defined as follows: 10-19; 20-29; 30-39; 40-49; 50-59; and 60-64 years. Concomitant meniscal repair was determined by CPT codes 29882 and 29883 on the same day as the ACLR. The use of an allograft was defined by Healthcare Common Procedure Coding System codes C1762, C1763, and C1776 on the same day as the ACLR. Analysis was performed using Stata Version 16.0 (StataCorp) and R (Version 3.6.2; www.cran.r-project.org). Values of P < .05 were considered statistically significant.
Results
Across all included patients (N = 2226), 54% were men (95% CI, 51.9%-56.1%), the mean age was 28.9 years (95% CI, 28.4-29.4 years), and 17.4% of patients had Medicaid (95% CI, 15.8%-19%). Patients in the ED cohort (n = 658) were more likely to have Medicaid (29% vs 12.5%; P < .001), be in the lowest income quartile (Q1; 44.6% vs 32.1%; P < .001), and be <20 years old (34.8% vs 29.3%; P = .001) (Table 1). No significant difference was found in rates of concomitant meniscal repair or allograft use between the 2 cohorts (P = .150 and P = .210, respectively). In addition, no significant difference was found between the 2 groups with regard to patient sex (P = .802).
Table 1.
Characteristics of Patients With Non-ED Versus ED Evaluation of Knee Injury Within 1 Year of ACLR a
| Characteristic | Non-ED (n = 1568) | ED (n = 658) | P |
|---|---|---|---|
| Sex | .802 | ||
| Male | 844 (53.8) | 358 (54.4) | |
| Female | 722 (46.2) | 300 (45.6) | |
| Age-group, y | .001 | ||
| 10-19 | 459 (29.3) | 229 (34.8) | |
| 20-29 | 427 (27.2) | 197 (29.9) | |
| 30-39 | 280 (17.9) | 116 (17.6) | |
| 40-49 | 280 (17.9) | 87 (13.2) | |
| 50-59 | 101 (6.4) | 26 (4) | |
| 60-64 | 21 (1.3) | 3 (0.5) | |
| Insurance | <.001 | ||
| Commercial | 1372 (87.5) | 467 (71) | |
| Medicaid | 196 (12.5) | 191 (29) | |
| Income quartile b | <.001 | ||
| Q1 (<US$70,728) | 496 (32.1) | 290 (44.6) | |
| Q2 (US$70,728-US$85,866) | 469 (30.3) | 180 (27.7) | |
| Q3 (US$85,867-US$103,955) | 354 (22.9) | 112 (17.2) | |
| Q4 (≥US$103,956) | 228 (14.7) | 68 (10.5) |
Data are reported as n (%). Percentages are presented as within-column percentages.
Bold P values indicate statistically significant differences between groups (P < .05). ACLR, anterior cruciate ligament reconstruction; ED, emergency department; Q, quartile.
As determined by ZIP code.
Overall, the mean time to surgery was 72.98 days (95% CI, 70.18-75.79 days), and the mean time to MRI was 18.03 days (95% CI, 16.17-19.89 days) in the entire cohort. The mean time to surgery was found to be significantly longer in the ED cohort (88.01 days vs 66.68 days; P < .001) and in Medicaid patients (88.96 vs 69.62 days; P < .001). In patients aged <20 years, the difference was more pronounced, with the mean time to surgery significantly longer for ED patients (80.29 vs 53.08 days; P < .001) and Medicaid patients (77.36 vs 58.42 days; P < .001). Patients in the lowest income quartile (Q1) had the longest mean time to surgery (80.27 days; 95% CI, 75.41-85.13 days) compared with Q2 (73.68 days; 95% CI, 68.47-78.88 days), Q3 (67.34 days; 95% CI, 61.35-73.33 days), and Q4 (62.41 days; 95% CI, 55.19-69.63 days). The youngest patients—the 10-19 years age-group—had the shortest mean time to surgery of 62.14 days (95% CI, 57.50-66.77 days). This was compared with 72.41 days (95% CI, 67.52-77.30 days) in the 20-29 years age-group; 80.35 days (95% CI, 73.28-87.42 days) in the 30-39 years age-group; 83.84 days (95% CI, 76.04-91.64 days) in the 40-49 years age-group; 78.96 days (95% CI, 66.04-91.88 days) in the 50-59 years age-group; and 79.75 days (95% CI, 48.66-110.84 days) in the 60-64 years age-group.
Results of the multivariable linear regression regarding the effect of patient and surgical characteristics on time to ACLR are shown in Table 2. Male sex, age-group, ED utilization, and Medicaid status were significant predictors of longer time to ACLR. Initial diagnosis at the ED was significantly associated with time to surgery, adding 20.30 additional days on average (95% CI, 14.10-26.49 days; P < .001). Similarly, Medicaid status added a mean of 12.88 days before ACLR (95% CI, 5.15-20.60 days; P = .001). The highest income quartile (Q4) and concomitant meniscal repair were significant predictors of shorter time to ACLR. Patients in Q4 had a shorter duration between diagnosis and surgery, averaging 11.57 fewer days (95% CI, −20.70 to −2.44 days; P = .013). In addition, patients undergoing concomitant meniscal repair with ACLR had surgery 10.87 days earlier on average (95% CI, −17.84 to −3.89 days; P = .002).
Table 2.
Results of Multivariable Linear Regression of Time to ACLR a
| Parameter | Time to ACLR, d (95% CI) | P |
|---|---|---|
| Sex | ||
| Female | Referent | |
| Male | 7.47 (1.86 to 13.08) | .009 |
| Age-group, y | ||
| 10-19 | Referent | |
| 20-29 | 9.25 (1.97 to 16.53) | .013 |
| 30-39 | 16.31 (8.01 to 24.61) | <.001 |
| 40-49 | 24.31 (15.78 to 32.85) | <.001 |
| 50-59 | 19.47 (6.67 to 32.27) | .003 |
| 60-64 | 23.86 (−3.12 to 50.85) | .083 |
| Insurance | ||
| Commercial | Referent | |
| Medicaid | 12.88 (5.15 to 20.60) | .001 |
| Income quartile b | ||
| Q1 (<US$70,728) | Referent | |
| Q2 (US$70,728-US$85,866) | −2.45 (−9.49 to 4.60) | .496 |
| Q3 (US$85,867-US$103,955) | −6.02 (−13.86 to 1.81) | .132 |
| Q4 (≥US$103,956) | −11.57 (−20.70 to −2.44) | .013 |
| ED visit | ||
| Non-ED group | Referent | |
| ED group | 20.30 (14.10 to 26.49) | <.001 |
| Allograft use | ||
| No allograft | Referent | |
| Allograft | −7.72 (−18.22 to 2.79) | .150 |
| Meniscus | ||
| No repair | Referent | |
| Concomitant repair | −10.87 (−17.84 to −3.89) | .002 |
Bold P values indicate statistical significance (P < .05). ACLR, anterior cruciate ligament reconstruction; ED, emergency department; Q, quartile.
As determined by ZIP code.
Furthermore, ED diagnosis and Medicaid status were found to be significant predictors of increased time to diagnostic imaging while controlling for other factors; patients in the ED cohort waited 7.97 days more on average before imaging (95% CI, 4.14 to 11.79 days; P < .001), and Medicaid status similarly added 8.40 days (95% CI, 3.44 to 13.37 days; P = .001). Q3 income status was found to be a significant predictor of decreased time to imaging—7.63 days less on average (95% CI, −12.88 to −2.38 days; P = .004); Q4 status also decreased time to imaging by 5.30 days but did not reach significance (95% CI, −11.43 to −0.84 days; P = .091). ED patients aged <20 years were found to have significantly longer wait times for imaging (26.41 vs 11.74 days; P < .001).
Multivariable logistic regressions were generated to determine the effect of certain patient and surgical factors on subsequent ACLR and PT use. Advancing age was the only patient factor found to affect the odds of subsequent ACLR, with the 10-19 years age-group as the referent group. Decreased odds of subsequent surgery were found for patients aged 20-29 years (odds ratio [OR], 0.49 [95% CI, 0.33-0.73]; P = .001), 30-39 years (OR, 0.41 [95% CI, 0.25-0.68]; P = .001), 40-49 years (OR, 0.36 [95% CI, 0.21-0.63]; P < .001), and 50-59 years (OR, 0.18 [95% CI, 0.06-0.59]; P = .005). Patients aged >40 years who used the ED were 2.5 times more likely to require subsequent ACLR (OR, 2.50 [95% CI, 1.01-6.21]; P = .049). Within this older population, patients in income Q1 were 10 times more likely to undergo subsequent ACLR than those in Q3 (Q1 as referent group; OR, 0.101 [95% CI, 0.0125-0.808]; P = .031).
Medicaid status was found to be the only significant predictor of PT use postoperatively; patients on Medicaid demonstrated decreased odds of attending PT sessions (OR, 0.759 [95% CI, 0.59-0.97]; P = .031). When the population was further stratified to isolate patients on Medicaid and in the lowest income quartile, patients visiting the ED first had significantly decreased odds of using PT after surgery (OR, 0.54 [95% CI, 0.31-0.95]; P = .033).
Discussion
In this study, patients with Medicaid and those with lower incomes were more likely to visit the ED for knee-related issues before an ACLR. Our study additionally found that an ED visit, Medicaid status, and being from a lower income quartile were all predictive of increased time to diagnostic imaging and surgery. This finding reflects other studies from the pediatric literature, including a retrospective cohort study of 127 patients by Patel et al, 19 in which patients with government-assisted insurance plans received MRIs 41 days later than patients with commercial insurance and went to surgery almost 3 months later (174.6 vs 90.4 days). We are not aware of an established relationship between insurance or income status and delays to diagnosis or ACLR in the adult population; this study suggests that the same delays may affect the adult population with ACL injury. Given that there is an established association between delay in surgery and concomitant chondral and meniscal injuries, these delays in care may have important clinical consequences.4,17 One recent retrospective cohort study by Chava et al 7 determined that Medicaid patients had lower International Knee Documentation Committee scores as well as decreased rates of return to play as compared with privately insured patients. Given the nature of the present study, it is impossible to know exactly what may have led to delays in care; however, 1 study by Baraga et al 3 examining this issue in Florida found that system-related factors such as lack of access to specialized care accounted for the majority of care delay. Unfortunately, our study does not contain data on patient-related factors such as health literacy or other social determinants of health (SDOH); nonetheless, given that Medicaid status has previously been linked to lower health literacy, this important variable may also be at play. 2
Additionally, younger patients were the most likely age-group to visit the ED before ACLR. While ACL injury in the adult population can sometimes be treated nonoperatively based on desired activity level and other patient factors, this is generally not the case in physically active pediatric patients. 9 Newman et al 17 found that younger age, noncommercial insurance status, and decreased household income were associated with a significantly greater risk of delayed surgery in a retrospective review of 272 pediatric patients who underwent ACLR. As expected, the youngest cohort of patients in this study had the shortest time to surgery which reflects the clinical imperative for ALCR in the pediatric population as well as the shared decision-making approach that typically occurs in the adult population.
Patients aged >40 years who initially presented to the ED were 2.5 times more likely to require subsequent surgery. Patients in the lowest (Q1) income quartile were 10 times more likely to have a subsequent procedure than their counterparts in Q3. However, no significant differences were found in patients aged <20 years. The need for subsequent surgery is a clinically significant adverse outcome after ACLR. In a case-control study from California, Gallo et al 11 similarly reported an increased risk of revision or contralateral ACLR in publicly insured patients aged >30 years and decreased risk in publicly insured patients aged <21 years. The data demonstrating delays in diagnosis and surgery indicate that patients with initial ED presentation and lower income may experience unfavorable outcomes secondary to delays in appropriate treatment. Targeted patient educational materials in the ED for the >40 years age-group might aid in reducing these disparities by bridging the gaps in the clinical understanding of diagnosis and the need for intervention. ED providers should also be educated to provide diagnostic accuracy to this vulnerable population.
Medicaid patients and those who visited the ED preoperatively were also less likely to utilize PT postoperatively. Multiple prospective cohort studies have demonstrated that postoperative PT adherence is linked with higher return to sports and favorable patient-reported knee outcome scores.8,15 The inverse relationship between Medicaid and PT use appears to be multifactorial. One cross-sectional study in Massachusetts found that only half of PT clinics accept Medicaid, while 96% accept private insurance, leading to care delays. 20 When Medicaid patients find a PT clinic, they often experience delays in progress and return to sports and fewer overall visits. 13 Unfortunately, the present study could not shed light on how a preoperative ED visit may have affected outcomes. There was no significant association between a preoperative ED visit and a need for subsequent ACLR surgery. Decreased postoperative PT use hints at poorer outcomes for patients who visited the ED preoperatively; nonetheless, this relationship will need to be investigated further in future studies.
Limitations
This study is not without important limitations. First is the lack of certainty that patients with preoperative knee-related ED visits presented secondary to an ACL rupture. While most of these patients did not receive a diagnosis of ACL sprain, we know that the diagnostic value of an ED visit after ACL rupture is very low.14,16,18 It is possible that patients presented to the ED for a non-ACL-related knee issue in the year before ACLR, leading to improper stratification of patients. Second, there is also a concern that patterns from the health care landscape in Rhode Island might not be generalizable to other locales; however, sampling a large statewide population affords a degree of external validity. Regarding internal validity, when using a claims-based database, one must always consider the possibility of coding errors or billing differences between providers that may compromise the validity of potential findings. Finally, this study primarily used income and Medicaid status as markers of SDOH. Unfortunately, the database lacked enough consistent descriptive data on race, educational level, and occupation status to consider the effect of these important SDOH indicators. In addition, given that ICD-9 codes do not reveal laterality, we were unfortunately unable to confirm whether subsequent surgeries were ipsilateral revision surgeries or contralateral ACLRs.
Conclusion
In this study, patients who visited the ED within 1 year before ACLR surgery were more likely to have a lower income, public insurance, increased time to diagnostic imaging, and increased time to surgery, as well as decreased postoperative PT use and increased subsequent ACLR rates in the 40-49 years age-group. Future research efforts should focus on resolving system-related care inequities at a policy level while mitigating patient-related factors with enhanced patient education and support.
Acknowledgments
Data for this study were obtained through an approved request to the APCD administered by the Rhode Island Department of Health (RIDOH). Data were obtained between 2011 and 2021. The RIDOH is not responsible for the authors’ analysis, opinions, and conclusions contained in this document.
Appendix Table A1.
ICD-9, ICD-10, and CPT Codes Used for Patient Identification Queries a
| Diagnosis/Procedure | Codes |
|---|---|
| ED visit | 99281, 99292, 99283, 99284, 99285 |
| Office visit | 99202, 99203, 99204, 99205, 99212, 99213, 99214, 99215 |
| ACL/meniscal injury | 7170:7179, 8360:8362, 8442, 8449, S83501:S83519, M2320:M2336, M2360:M2361, M2390:M2392 |
| Knee injury | 7170, 7171, 7172, 7173, 7174, 71740, 71741, 71742, 71743, 71749, 7175, 7176, 7177, 7178, 71781, 71782, 71783, 71784, 71785, 71789, 7179, 71826, 71836, 71846, 71876, 71886, 71906, 71916, 71926, 71946, 71966, 71986, 71996, 836, 8360, 8361, 8362, 8363, 8364, 8365, 83650, 83651, 83652, 83653, 83654, 83659, 8366, 83660, 83661, 83662, 83663, 83664, 83669, 8442, 8448, 8449, 9241, 92411, M172, M173, M1730, M1731, M1732, M23000, M23001, M23002, M23003, M23004, M23005, M23006, M23007, M23009, M23011, M23012, M23019, M23021, M23022, M23029, M23031, M23032, M23039, M23041, M23042, M23049, M23051, M23052, M23059, M23061, M23062, M23069, M23200, M23201, M23202, M23203, M23204, M23205, M23206, M23207, M23209, M23211, M23212, M23219, M23221, M23222, M23229, M23231, M23232, M23239, M23241, M23242, M23249, M23251, M23252, M23259, M23261, M23262, M23269, M23300, M23301, M23302, M23303, M23304, M23305, M23306, M23307, M23309, M23311, M23312, M23319, M23321, M23322, M23329, M23331, M23332, M23339, M23341, M23342, M23349, M23351, M23352, M23359, M23361, M23362, M23369, M2340, M2341, M2342, M2350, M2351, M2352, M23601, M23602, M23609, M23611, M23612, M23619, M23621, M23622, M23629, M23631, M23632, M23639, M23641, M23642, M23649, M23671, M23672, M23679, M238X1, M238X2, M238X9, M2390, M2391, M2392, M24361, M24362, M24369, M24461, M24462, M24469, M24561, M24562, M24569, M25061, M25062, M25069, M25261, M25262, M25269, M25361, M25362, M25369, M25461, M25462, M25469, M25561, M25562, M25569, M25661, M25662, M25669, M25861, M25862, M25869, S8000:S8012, S830:S839, S898:S899 |
ACL, anterior cruciate ligament; CPT, Current Procedural Terminology; ED, emergency department; ICD, International Classification of Diseases.
Footnotes
Final revision submitted June 8, 2023; accepted June 20, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: The project described was supported by Institutional Development Award Number U54GM115677 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds Advance Clinical and Translational Research (Advance-CTR). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. B.D.O. has received consulting fees from Linvatec, CONMED, Mitek, Miach, DePuy Synthes Products, Vericel, MTF Biologics, and Medical Device Business Services; royalties from Linvatec and CONMED; honoraria from Vericel; and stock options from Vivorte Inc; and is a paid associate editor for the American Journal of Sports Medicine. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Lifespan Research Protection Office (ref No. 217919).
References
- 1. Allott NEH, Banger MS, McGregor AH. Evaluating the diagnostic pathway for acute ACL injuries in trauma centres: a systematic review. BMC Musculoskelet Disord. 2022;23(1):649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Andrus MR, Roth MT. Health literacy: a review. Pharmacotherapy. 2002;22(3):282-302. [DOI] [PubMed] [Google Scholar]
- 3. Baraga MG, Smith MK, Tanner JP, Kaplan LD, Lesniak BP. Anterior cruciate ligament injury and access to care in South Florida: does insurance status play a role? J Bone Joint Surg Am. 2012;94(24):e183. [DOI] [PubMed] [Google Scholar]
- 4. Bram JT, Talathi NS, Patel NM, DeFrancesco CJ, Striano BM, Ganley TJ. How do race and insurance status affect the care of pediatric anterior cruciate ligament injuries? Clin J Sport Med. 2020;30(6):e201-e206. [DOI] [PubMed] [Google Scholar]
- 5. Brambilla L, Pulici L, Carimati G, et al. Prevalence of associated lesions in anterior cruciate ligament reconstruction: correlation with surgical timing and with patient age, sex, and body mass index. Am J Sports Med. 2015;43(12):2966-2973. [DOI] [PubMed] [Google Scholar]
- 6. Capp R, Rooks SP, Wiler JL, Zane RD, Ginde AA. National study of health insurance type and reasons for emergency department use. J Gen Intern Med. 2014;29(4):621-627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chava NS, Fortier LM, Verma N, et al. Patients with Medicaid insurance undergoing anterior cruciate ligament reconstruction have lower postoperative International Knee Documentation Committee scores and are less likely to return to sport than privately insured patients. Arthrosc Sports Med Rehabil. 2022;4(4):e1457-e1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Della Villa F, Andriolo L, Ricci M, et al. Compliance in post-operative rehabilitation is a key factor for return to sport after revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(2):463-469. [DOI] [PubMed] [Google Scholar]
- 9. Dingel A, Aoyama J, Ganley T, Shea K. Pediatric ACL tears: natural history. J Pediatr Orthop. 2019;39(6)(suppl 1):S47-S49. [DOI] [PubMed] [Google Scholar]
- 10. Evans J, Nielson J l. Anterior cruciate ligament knee injuries. In: StatPearls. StatPearls Publishing; 2023. [Google Scholar]
- 11. Gallo MC, Bolia IK, Jalali O, et al. Risk factors for early subsequent (revision or contralateral) ACL reconstruction: a retrospective database study. Orthop J Sports Med. 2020;8(2):2325967119901173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Granan LP, Bahr R, Lie SA, Engebretsen L. Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears: a cohort study based on the Norwegian National Knee Ligament Registry. Am J Sports Med. 2009;37(5):955-961. [DOI] [PubMed] [Google Scholar]
- 13. Greenberg E, Butler L, Giampetruzzi N, et al. Differences in the course of rehabilitation and outcomes for publicly insured pediatric patients after anterior cruciate ligament reconstruction. Phys Ther Sport. 2022;58:52-57. [DOI] [PubMed] [Google Scholar]
- 14. Guillodo Y, Rannou N, Dubrana F, Lefèvre C, Saraux A. Diagnosis of anterior cruciate ligament rupture in an emergency department. J Trauma. 2008;65(5):1078-1082. [DOI] [PubMed] [Google Scholar]
- 15. Han F, Banerjee A, Shen L, Krishna L. Increased compliance with supervised rehabilitation improves functional outcome and return to sport after anterior cruciate ligament reconstruction in recreational athletes. Orthop J Sports Med. 2015;3(12):2325967115620770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Li LT, Chuck C, Bokshan SL, Owens BD. Increased total cost and lack of diagnostic utility for emergency department visits after ACL injury. Orthop J Sports Med. 2021;9(5):23259671211006711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Newman JT, Carry PM, Terhune EB, et al. Delay to reconstruction of the adolescent anterior cruciate ligament: the socioeconomic impact on treatment. Orthop J Sports Med. 2014;2(8):2325967114548176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Parwaiz H, Teo AQA, Servant C. Anterior cruciate ligament injury: a persistently difficult diagnosis. Knee. 2016;23(1):116-120. [DOI] [PubMed] [Google Scholar]
- 19. Patel AR, Sarkisova N, Smith R, Gupta K, VandenBerg CD. Socioeconomic status impacts outcomes following pediatric anterior cruciate ligament reconstruction. Medicine. 2019;98(17):e15361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rogers MJ, Penvose I, Curry EJ, DeGiacomo A, Li X. Medicaid health insurance status limits patient accessibility to rehabilitation services following ACL reconstruction surgery. Orthop J Sports Med. 2018;6(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shi W, Anastasio A, Guisse NF, et al. Impact of insurance and practice type on access to orthopaedic sports medicine. Orthop J Sports Med. 2020;8(7):2325967120933696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Taubman SL, Allen HL, Wright BJ, Baicker K. Oregon’s health insurance experiment. Science (1979). 2014;343(6168):263-268. [DOI] [PMC free article] [PubMed] [Google Scholar]


