Abstract
Background:
No consensus currently exists among orthopaedic surgeons regarding the benefits of hip orthosis after routine hip arthroscopy.
Purpose:
To compare patient-reported outcome measures (PROMs) and reoperation rates between patients who were braced versus those who were not braced after routine hip arthroscopy.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A retrospective review was conducted of 193 patients who underwent hip arthroscopy for femoroacetabular impingement (FAI) from January 1, 2018, to December 31, 2021, by 2 orthopedic surgeons at a single institution. Patients before July 1, 2019, were immobilized in a hip orthosis after hip arthroscopy (braced group; n = 101), whereas those after July 1, 2019, were not (nonbraced group; n = 92). Baseline PROMs (visual analog scale for pain, modified Harris Hip Score, Single Assessment Numeric Evaluation, and Veterans Rand 12-Item Health Survey [VR-12] Physical Component Summary and Mental Component Summary) were obtained for all patients and were repeated postoperatively at 2 weeks, 4 weeks, 3 months, 6 months, 1 year, and 2 years. The study groups were compared to evaluate differences in PROMs over time and 2-year postoperative reoperation rates. Group comparisons were also stratified by patient sex.
Results:
There were no significant differences on any PROM between the braced and nonbraced cohorts at any timepoint. There were also no significant group differences in reoperation rates, with 8 braced patients (7.9%) undergoing reoperation and 1 nonbraced patient (2.3%) undergoing reoperation (P = .208). In the sex-stratified analyses, nonbraced male patients had significantly higher VAS pain and lower VR-12 Mental Component Summary scores at 6 months postoperatively compared with braced male patients (P = .043 and .026, respectively).
Conclusion:
The study findings suggested that the use of an orthosis after routine hip arthroscopy for FAI does not improve patient-reported outcomes or negatively affect the 2-year reoperation rate. Postoperative bracing increases perioperative cost, and by foregoing routine bracing, patients may avoid the morbidity associated with wearing a brace for a prolonged period.
Keywords: clinical assessment/grading scales, hip arthroscopy, hip femoroacetabular impingement, physical therapy/rehabilitation
Hip arthroscopy has become an increasingly utilized procedure to correct intra- and extra-articular pathologies of the hip. 10 The number of hip arthroscopies performed in the United States (US) increased by 250% between 2007 and 2011, 12 and the number of hip arthroscopies performed in the US has continued to increase dramatically over the past decade due to further improvements in arthroscopic technology and technique. 8 The need for quality and comprehensive knowledge surrounding preoperative, intraoperative, and postoperative management of hip arthroscopy patients is important to optimize patient outcomes. 3
One essential aspect to successful patient outcomes after hip arthroscopy is successful postoperative management. Evidence-based literature surrounding postoperative management after hip arthroscopy is limited, so postoperative protocols are often based on known tissue healing properties, patient tolerance, and clinician experience. 17 The use of a hip orthosis is 1 common postoperative practice. One study examining the surgical practices of high-volume hip arthroscopy surgeons found that 59.2% of these surgeons prescribed a hip brace for some or all patients after hip arthroscopy. However, some surgeons in the cohort used the brace in only the case of specific procedures such as a labral repair, capsular plication, or gluteus repair. 7 Another study examining the rehabilitation practices after hip arthroscopy of orthopaedic surgeons in North America found that bracing was used in 54.8% of protocols and was used for a median 2-week duration (range, 1 to 6 weeks). Rationales provided by physicians for bracing include normalization of gait pattern while walking, hip protection, prevention of abduction and flexion/extension, and nighttime protection. 2
No consensus exists among orthopaedic surgeons regarding the benefits of postoperative hip orthoses in routine hip arthroscopy. In this study, we aimed to analyze postoperative patient-reported outcome measures (PROMs) and reoperation rates after hip arthroscopy in braced versus nonbraced patients compared with preoperative baseline values.
Methods
Study Participants
International review board approval was obtained for the study protocol, and all included participants provided written informed consent. From March 1, 2018, to June 30, 2022, a total of 375 patients underwent hip arthroscopy for FAI by 2 orthopedic surgeons (S.M. and J.P.S.) at a single institution. Hip arthroscopy was indicated in patients who failed to have satisfactory improvement in hip pain and function with at least 3 months of nonoperative management, including at least 6 weeks of physical therapy, nonsteroidal anti-inflammatory drugs, and activity modification. All 375 patients had enrolled in the Surgical Outcome System (SOS) to collect PROM data preoperatively and postoperatively.
The inclusion criteria for this study were patients who (1) received routine hip arthroscopy, defined as acetabuloplasty, femoroplasty, and labral repair with a Current Procedural Terminology (CPT) code 29914, 29915, 29916; and (2) completed PROMs preoperatively and at least 1 timepoint postoperatively. Capsular closure was performed routinely in all operations in both cohorts. Exclusion criteria were (1) any patient who did not complete preoperative PROM data or at least 1 timepoint of postoperative PROM data, (2) patients who underwent additional procedures (aside from hip arthroscopy) on the day of surgery, (3) patients who received a labral debridement (CPT code 29862), and (4) patients having a 29999 CPT code associated with their surgical procedure. A CPT code of 29999 was used as a surrogate for additional procedures performed alongside routine hip arthroscopy defined previously. These procedures included gluteus medius and minimus repairs, core muscle repairs, iliotibial band recession or elongation, iliopsoas fractional lengthening, trochanteric bursectomy, subspine decompression, acetabular microfracture, and capsular plication or augmentation. These patients were excluded, as they underwent different bracing protocols than our target population.
In anticipation for this study, the 2 surgeons involved had set a cutoff date of July 1, 2019, to forego hip bracing after routine hip arthroscopy. Hip arthroscopy patients who underwent surgery before July 1, 2019, were immobilized in a hip orthosis (braced group) whereas those who underwent surgery after July 1, 2019, were not (nonbraced group). The hip bracing protocol before July 1, 2019, consisted of 3 weeks of postoperative bracing. Brace settings allowed for 0 to 90° of flexion and no abduction. Patients were partial weightbearing and used crutches during this period. A similar physical therapy protocol was utilized in both cohorts.
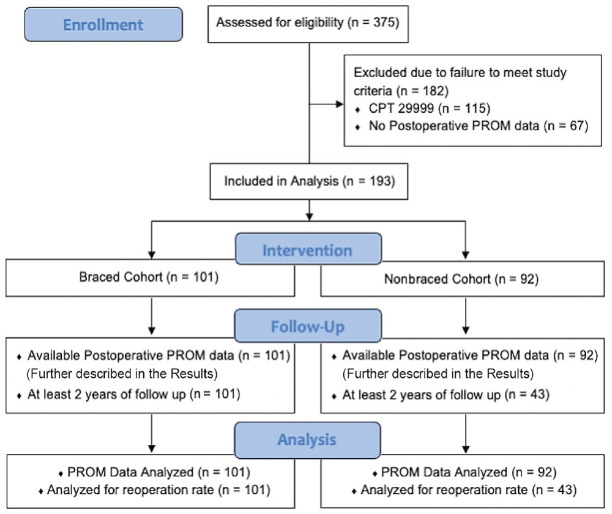
All 375 patient charts were reviewed via the SOS by 2 authors (D.W. and J.E.). After chart review, 115 patients were excluded due to a CPT code of 29999. This left 261 patients, of whom 67 were excluded due to incomplete PROM data in the SOS, leaving 193 active study participants. There were 101 patients in the braced group and 92 patients in the nonbraced group (Figure 1).
Figure 1.
CONSORT flowchart diagram of patient enrollment. CPT, current procedural terminology; PROM, patient-reported outcome measures.
Data Collection
Patient demographics including sex, age, body mass index (BMI), and the preoperative radiographic parameters of lateral center-edge angle (LCEA) and alpha angle were collected. PROM scores were collected at baseline and postoperatively using the SOS and included the visual analog scale (VAS) for pain, modified Harris Hip Score (mHHS), Single Assessment Numeric Evaluation (SANE) hip scores, and the Veterans Rand 12-Item Health Survey (VR-12) Physical Component Summary (PCS) and Mental Component Summary (MCS). VAS pain was recorded at 2 weeks, 4 weeks, 3 months, 6 months, 1 year, and 2 years. The mHHS and SANE was recorded at 3 months, 6 months, 1 year, and 2 years. VR-12 PCS and VR-12 MCS were recorded at 6 months, 1 year, and 2 years. This was in accordance with the standard PROM collection protocol.
The rates of and reasons for reoperation in both groups were also evaluated. A reoperation was defined as a second ipsilateral hip procedure occurring within 2 years of the index procedure. Reoperation was indicated in patients who failed to have sufficient improvement in hip pain and function despite an extended course of postoperative rehabilitation following the primary procedure (Table 1). Only patients with at least 2 years of follow-up data (all 101 patients in the braced group, 43 patients in the nonbraced group; Figure 1) were included in the analysis of reoperation rate.
Table 1.
Indications for Primary Hip Arthroscopy and Reoperation a
| Procedure | Indications |
|---|---|
| Primary hip arthroscopy | Patients without satisfactory improvement in hip pain and function after at least 3 months of nonoperative management, including at least 6 weeks of PT, NSAIDs, and activity modification |
| Reoperation | Patients without sufficient improvement in hip pain and function despite an extended course of postoperative rehabilitation |
NSAIDs, nonsteroidal anti-inflammatory drugs; PT, physical therapy.
Statistical Analysis
Statistical analysis was performed to evaluate age, sex, BMI, and preoperative radiographic differences between the braced and nonbraced groups. Comparisons of categorical demographics between the study groups were assessed using the chi-square test. Normality of all study outcome measures was assessed using the Shapiro-Wilk test. Independent comparisons of PROM scores between the groups at each timepoint were performed using the t test or Wilcoxon rank-sum test depending on normality. The Fisher exact test was used to compare the rate of reoperation between the 2 cohorts. A separate sex-stratified group comparison of PROM scores and reoperation rates was also conducted. Statistical significance was set at P < .05 for all analyses. Statistical analyses were performed using R (R Foundation for Statistical Computing) and Excel (Microsoft).
Power Analysis
A power analysis was conducted to determine the minimum sample sizes needed to reach 80% statistical power at a significance of P < .05 for 2-tailed comparisons. For each outcome measure, a literature review was conducted to identify the minimum clinically important difference (MCID) to serve as the basis for determining the relevant effect size. Table 2 summarizes the MCID values used for the power analysis and resulting sample size estimations for each PROM.11,13,15,18
Table 2.
MCID Values From Previous Studies Used for Power Analyses a
| PROM | MCID | Study | Minimum Sample Size per Group |
|---|---|---|---|
| VAS pain | 1.5 | Martin et al (2019) 13 | 35 |
| mHHS | 7.9 | Nwachukwu et al (2018) 15 | 65 |
| SANE | 17.2 b | Lau et al (2019) 11 | 23 |
| VR-12 PCS | 16.0 b | Sugarman et al (2021) 18 | 7 |
| VR-12 MCS | 1.7 b | Sugarman et al (2021) 18 | 611 |
MCS, Mental Component Summary; mHHS, modified Harris Hip Score; PCS, Physical Component Summary; PROM, patient-reported outcome measure; SANE, Single Assessment Numeric Evaluation; VAS, visual analog scale; VR-12, Veterans Rand 12-Item Health Survey.
Value was derived from mean preoperative to postoperative changes.
Results
Patient Characteristics and Preoperative Radiographic Parameters
Table 3 summarizes the patient characteristics and preoperative radiographic parameters of the braced and nonbraced cohorts. There were no significant group differences regarding sex distribution, age, or BMI. Regarding preoperative radiographic parameters, the nonbraced cohort had a higher mean LCEA compared with the braced cohort (35.1° ± 8.5° vs 32.9° ± 6.1°, respectively; P = .043).
Table 3.
Patient Characteristics and Preoperative Radiographic Parameters a
| Characteristic | Braced Group (n = 101) |
Nonbraced Group (n = 92) |
P |
|---|---|---|---|
| Sex | .418 | ||
| Female | 67 (66.3) | 66 (71.7%) | |
| Male | 34 (33.6%) | 26 (28.3%) | |
| Age, y | 33.2 ± 13.0 | 30.2 ± 11.5 | .085 |
| BMI | 28.9 ± 6.0 | 28 ± 6.2 | .501 |
| Preoperative radiographic parameter | |||
| Alpha angle, deg | 63.2 ± 12.7 | 62.0 ± 10.1 | .211 |
| LCEA, deg | 32.9 ± 6.1 | 35.1 ± 8.5 | .043 |
Data are reported as mean ± SD or n (%). BMI, body mass index; LCEA, lateral center-edge angle.
PROM Availability
Minimum sample sizes with 80% power were achieved for some but not all PROMs. Table 4 summarizes the sample sizes for the PROM data at each timepoint.
Table 4.
PROM Data Availability According to Timepoint a
| Postoperative | |||||||
|---|---|---|---|---|---|---|---|
| Preoperative | 2 weeks | 4 weeks | 3 months | 6 months | 1 year | 2 years | |
| Braced group | |||||||
| VAS pain | 101 | 95 | 96 | 85 | 75 | 78 | 75 |
| mHHS | 100 | NA | NA | 84 | 75 | 78 | 75 |
| SANE | 100 | NA | NA | 84 | 75 | 78 | 75 |
| VR-12 PCS | 101 | NA | NA | NA | 84 | 75 | 78 |
| VR-12 MCS | 101 b | NA | NA | NA | 75 b | 78 b | 75 b |
| Nonbraced group | |||||||
| VAS pain | 92 | 81 | 73 | 68 | 58 | 53 | 32 b |
| mHHS | 92 | NA | NA | 68 | 58 b | 53 b | 32 b |
| SANE | 92 | NA | NA | 68 | 53 | 53 | 32 |
| VR-12 PCS | 92 | NA | NA | NA | 58 | 53 | 32 |
| VR-12 MCS | 92 b | NA | NA | NA | 58 b | 53 b | 32 b |
MCS, Mental Component Summary; mHHS, modified Harris Hip Score; NA, not applicable; PCS, Physical Component Summary; PROM, patient-reported outcome measure; SANE, Single Assessment Numeric Evaluation; VAS, visual analog scale; VR-12, Veterans Rand 12-Item Health Survey.
Sample size was below the estimated 80% power level.
PROM Data
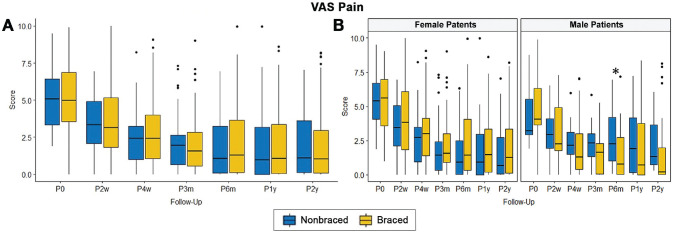
The PROM results for nonbraced and braced groups in both the overall and sex-based analyses are shown in Figures 2 to 5. With respect to VAS pain scores, in the overall analysis, there were no significant differences at any follow-up point between nonbraced and braced groups. In the sex-based analysis, nonbraced males reported significantly higher VAS pain at 6 months postoperatively compared with braced males (P = .043) (Figure 2B); however, the sample size at this timepoint was below the minimum threshold to achieve 80% statistical power.
Figure 2.
Comparison of VAS pain scores (A) overall and (B) stratified by patient sex between the nonbraced and braced groups at each follow-up point. *Statistically significant difference between groups (P < .05). The middle horizontal line of the box indicates the median, the top and bottom of the box indicate the upper and lower quartiles, the upper and lower error bars indicate the maximum and minimum values, and the dots indicate statistical outliers. m, month; p, postoperative; VAS, visual analog scale; w, week; y, year.
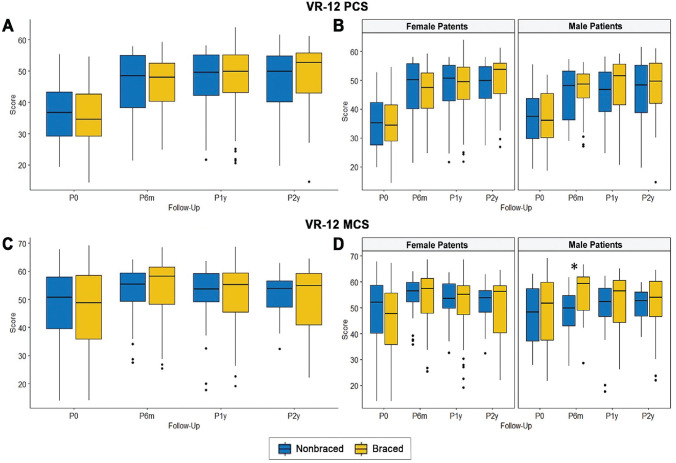
Figure 5.
Comparison of VR-12 PCS scores and MCS scores (A and C) overall and (B and D) stratified by patient sex between the nonbraced and braced groups at each follow-up point. *Statistically significant difference between groups (P < .05). The middle horizontal line of the box indicates the median, the top and bottom of the box indicate the upper and lower quartiles, the upper and lower error bars indicate the maximum and minimum values, and the dots indicate statistical outliers. m, month; MCS, Mental Component Summary; p, postoperative; PCS, Physical Component Summary; VR-12, veterans Rand 12-item; w, week; y, year.
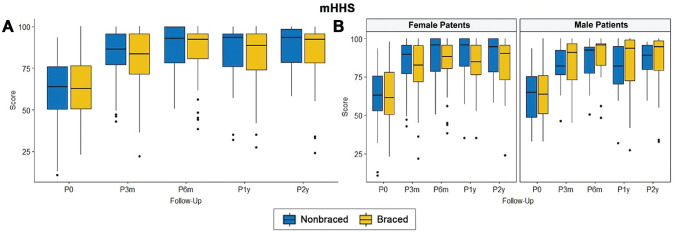
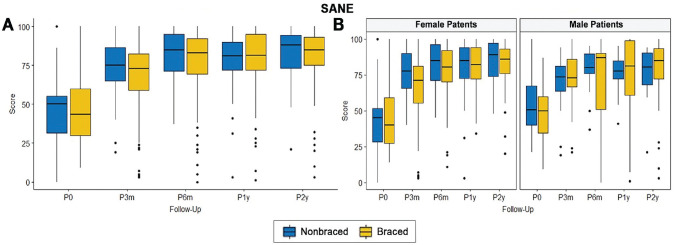
Regarding the mHHS and SANE, there were no significant differences between the nonbraced and braced groups at any follow-up point, in both the overall and sex-based analyses (Figures 3 and 4).
Figure 3.
Comparison of (mHHS) (A) overall and (B) stratified by patient sex between the nonbraced and braced groups at each follow-up point. The middle horizontal line of the box indicates the median, the top and bottom of the box indicate the upper and lower quartiles, the upper and lower error bars indicate the maximum and minimum values, and the dots indicate statistical outliers. mHHS, modified Harris Hip Scores; m, month; p, postoperative; w, week; y, year.
Figure 4.
Comparison of SANE scores (A) overall and (B) stratified by patient sex between the nonbraced and braced groups at each follow-up point. The middle horizontal line of the box indicates the median, the top and bottom of the box indicate the upper and lower quartiles, the upper and lower error bars indicate the maximum and minimum values, and the dots indicate statistical outliers. m, month; p, postoperative; SANE, single assessment numeric evaluation; w, week; y, year.
There were no significant group differences in VR-12 PCS scores at any follow-up in both the overall and sex-based analyses. Regarding the VR-12 MCS, in the sex-based analysis, nonbraced males reported significantly lower VR-12 MCS scores at 6 months postoperatively (P = .026) (Figure 5D); however, the sample size at this timepoint was below the minimum threshold to achieve 80% statistical power.
Reoperation Data
All patients with at least 2 years of follow-up (n = 144) were analyzed for reoperation. All primary procedures in this cohort were routine hip arthroscopy for FAI defined as acetabuloplasty, femoroplasty, and labral repair. Table 5 summarizes the demographics, preoperative radiographic parameters, and reoperation procedures in the braced and nonbraced patients with follow-up data. There were no significant differences between the cohorts.
Table 5.
Patient Characteristics, Preoperative Radiographic Parameters, and Reoperation Rates of Patients With 2-Year Follow-up Data a
| Characteristic | Braced Group (n = 101) |
Nonbraced Group (n = 43) |
P |
|---|---|---|---|
| Sex | .185 | ||
| Female | 67 (66.3) | 33 (76.7%) | |
| Male | 34 (33.6%) | 10 (23.3%) | |
| Age, y | 33.2 ± 13.0 | 29.6 ± 10.7 | .131 |
| BMI, kg/m2 | 28.9 ± 6.0 | 28.5 ± 6.2 | .686 |
| Preoperative radiographic parameter | |||
| Alpha angle, deg | 63.2 ± 12.7 | 62.0 ± 10.2 | .685 |
| LCEA, deg | 32.9 ± 6.1 | 34.4 ± 6.9 | .211 |
| Reoperations | 8 (7.9%) | 1 (2.3%) | .208 |
| Type of reoperation, n | NA | ||
| Revision labral repair | 5 | 1 | |
| Labral reconstruction | 1 | 0 | |
| Iliopsoas lengthening | 1 | 0 | |
| Lysis of adhesions | 1 | 0 | |
| Total hip arthroplasty | 0 | 0 |
Data are shown as n (%) or mean ± SD unless otherwise indicated. BMI, body mass index; LCEA, lateral center-edge angle; NA, not applicable.
In the braced cohort, 8 of 101 patients (7.9%) underwent a reoperation, while 1 of 43 patients (2.3%) in the nonbraced cohort underwent a reoperation. Of the braced group, 5 of the revision procedures were labral rerepairs, 1 was a labral reconstruction, 1 was iliopsoas fractional lengthening, and 1 was a lysis of adhesions. These revisions occurred at durations of 7, 8, 9, 13, 15, 15, 16, and 18 months after the index procedure. For the nonbraced cohort, the singular revision procedure was a labral rerepair. This occurred 12 months after the index procedure. No reoperation consisted of a total hip arthroplasty in either cohort. No significant group difference in the reoperation rates was detected (Table 5). As no male patients in our cohort underwent reoperation, only female patients were included in the sex-stratified analysis. Of the female patients, 8/67 (11.9%) underwent reoperation in the braced cohort while 1 of 33 (3.0%) underwent reoperation in the nonbraced cohort. No significant difference in the reoperation rate between the braced and nonbraced females was detected (P = .265).
Discussion
The findings of this study suggested that postoperative hip bracing has no significant impact on postoperative PROMs. The nonbraced cohort reported equitable values for every PROM at every measured timepoint after hip arthroscopy for FAI when compared with the braced cohort at the same postoperative timepoints. This indicates that the use of a hip orthosis after hip arthroscopy may not provide added benefit as it relates to improvement in PROM values for up to 2 years after arthroscopy. The postoperative PROM data showed that nonbraced males may experience slightly higher VAS pain scores and slightly lower VR-12 MCS scores compared with braced males at 6 months postoperatively; however, sample sizes at this timepoint were below the minimum threshold identified to achieve 80% statistical power based on previous literature. We interpreted this as an uncertain finding and suggest that further research is needed to investigate the clinical efficacy of this potential difference.
The rate of reoperation was shown to not be significantly different in the braced versus nonbraced cohorts for 2 years after hip arthroscopy. The 2-year reoperation rate for this study was 6.25%, with a 7.2% reoperation rate in the braced group and 2.3% reoperation rate in the nonbraced group. Previous studies of hip arthroscopy have reported reoperation rates of 1.4% to 5.31% after hip arthroscopy procedures, with 86% of revisions occurring within 18 months.5,19,20 Overall, it was shown in this study that postoperative hip bracing has no effect on the reoperation rate after arthroscopy.
The use of a hip brace after arthroscopy can be associated with increased morbidity for the patient as adverse effects have been reported with brace wear. Newcomb et al 14 examined the effects of hip bracing as a conservative treatment for patients with FAI and found that the use of a brace did not reduce pain or increase PROMs after 4 weeks of daily use, but all patients in the study reported at least 1 adverse effect related to use of the brace. Knee irritation of the braced leg, slipping of the brace, brace-related discomfort during or after brace wear, and contralateral hip pain were the adverse effects reported most frequently in the study. The use of a hip brace also increases perioperative costs. Each hip brace utilized in this study costs over US$1500, increasing costs for both the patient and the health system. Considering the added perioperative cost and risk of adverse effects for the patient with the use of a hip brace, surgeons should consider whether the use of a brace postoperatively is truly necessary.
Overall, the findings of this study can be used to guide clinical decision-making as it relates to the use of a postoperative hip orthosis in the setting of routine hip arthroscopy for FAI. This paper has demonstrated that hip bracing may not provide clinical benefit and, therefore, foregoing its use may help to reduce perioperative cost and limit the adverse effects associated with long-term use. There is still a paucity of literature surrounding postoperative rehabilitation protocols after hip arthroscopy, especially as it relates to the use of a brace. 6 Studies with a more robust sample size, longer follow-up, and a more diverse array of measures of clinical benefit and patient satisfaction could allow for more adequate knowledge of the significance and long-term effects of the use of a hip brace, or lack thereof, after hip arthroscopy.
Strengths and Limitations
One strength of this study is the sex-stratified analysis of both cohorts. Flores et al 4 suggested that women and men experience equitable recovery, similar postoperative PROMs, and similar rates of reoperation after hip arthroscopy. However, previous studies have suggested that women may experience worse preoperative hip function, worse patient-reported outcome scores, and higher rates of reoperation relative to men undergoing similar hip arthroscopy procedures.5,9 Another study by Beck et al 1 suggested that women may achieve higher postoperative values for mHHS after hip arthroscopy. Stratifying our data by sex helps to parse out any disparities in postoperative PROMs that could be due to gender related differences. In our study, it was discovered that nonbraced males reported worse postoperative outcomes in 2 measures, VAS pain and VR-12 MCS; however, sample sizes were limited. This could be due to the differences in postoperative recovery between men and women after hip arthroscopy; however, it is difficult to draw any assumptions based on these 2 datapoints. Second, all reoperations in our cohort were in female patients. Sardana et al 16 suggested that female patients more commonly undergo revision hip arthroscopy relative to male patients. Further research may be needed to elucidate discrepancies that may exist in the rates of reoperation based on gender.
One limitation of this study is the lack of literature available clearly defining the MCID for the PROMs utilized in this study as they relate to hip arthroscopy. Several of the MCIDs utilized in this study had to be determined based on pre and postoperative values reported in hip arthroscopy studies with similar patient populations. Accurate MCID is essential to determining statistical power and validity of statistical significance. Future research is needed to more adequately define MCID for SANE, VR-12 MCS, and VR-12 PCS after hip arthroscopy in the general population to better utilize these values to determine significance in clinical research. Another limitation was that it was not randomized but rather a timepoint was chosen for the change in clinical care of using a brace. This could possibly affect the outcomes since the surgeons would have had more experience with nonbraced patients. In addition, all patients in this study underwent hip arthroscopy for FAI; therefore, the results of this study may not translate to other diagnoses or arthroscopy procedures. The low follow-up at the 2-year timepoint in the nonbraced cohort is another limitation. Greater long-term follow-up in the nonbraced group would help to better power the findings of this study and allow for a better analysis of reoperation. A final limitation to this study was the lack of robust preoperative data defining risk in each cohort. Radiographic information such as the LCEA and Alpha Angle were collected, but more extensive preoperative information, such as range of motion or Tönnis grade, could better define the risk for poor outcomes in each cohort and allow for a further subanalysis of the use of a brace in high-risk populations, such as those with hypermobility, Ehlers-Danlos syndrome, or borderline dysplasia. Further prospective research examining these preoperative risk factors is needed.
Conclusion
The study findings suggested that the use of an orthosis after routine hip arthroscopy for FAI does not improve patient-reported outcomes or negatively impact the reoperation rate. Postoperative bracing increases perioperative cost, and, by foregoing routine bracing, patients may avoid the morbidity associated with wearing a brace for a prolonged period.
Footnotes
Final revision submitted June 7, 2023; accepted June 20, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: I.G. has received education payments from Titan Surgical and CGG Medical and hospitality payments from Zimmer Biomet Holdings. B.V. has received consulting fees from International Life Sciences, education payments from Titan Surgical and DePuy Synthes, and hospitality from Novastep. P.S. has received nonconsulting fees from Arthrex, education payments from Titan Surgical and Arthrex, consulting fees from Vericel, and hospitality payments from Zimmer Biomet Holdings. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from The University of Kansas Medical Center (ref No. STUDY00143689).
References
- 1. Beck EC, Drager J, Nwachukwu BU, Jan K, Rasio J, Nho SJ. Gender and age-specific differences observed in rates of achieving meaningful clinical outcomes 5-years after hip arthroscopy for femoroacetabular impingement syndrome. Arthroscopy. 2021;37(8):2488-2496.e2481. PMID: 33677021. [DOI] [PubMed] [Google Scholar]
- 2. Cvetanovich GL, Lizzio V, Meta F, et al. Variability and comprehensiveness of North American online available physical therapy protocols following hip arthroscopy for femoroacetabular impingement and labral repair. Arthroscopy. 2017;33(11):1998-2005. PMID: 28969949. [DOI] [PubMed] [Google Scholar]
- 3. Domb BG, Sgroi TA, VanDevender JC. Physical therapy protocol after hip arthroscopy: clinical guidelines supported by 2-year outcomes. Sports Health. 2016;8(4):347-354. PMC4922519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Flores SE, Chambers CC, Borak KR, Zhang AL. Is there a gender gap in outcomes after hip arthroscopy for femoroacetabular impingement? Assessment of clinically meaningful improvements in a prospective cohort. Orthop J Sports Med. 2020;8(7):2325967119900561. PMC7361492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Frank RM, Lee S, Bush-Joseph CA, Salata MJ, Mather RC, III, Nho SJ. Outcomes for hip arthroscopy according to sex and age: a comparative matched-group analysis. J Bone Joint Surg Am. 2016;98(10):797-804. PMID: 27194489. [DOI] [PubMed] [Google Scholar]
- 6. Grzybowski JS, Malloy P, Stegemann C, Bush-Joseph C, Harris JD, Nho SJ. Rehabilitation following hip arthroscopy - a systematic review. Front Surg. 2015;2:21. PMC4443726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gupta A, Suarez-Ahedo C, Redmond JM, et al. Best practices during hip arthroscopy: aggregate recommendations of high-volume surgeons. Arthroscopy. 2015;31(9):1722-1727. PMID: 25980403. [DOI] [PubMed] [Google Scholar]
- 8. Jamil M, Dandachli W, Noordin S, Witt J. Hip arthroscopy: indications, outcomes and complications. Int J Surg. 2018;54(Pt B):341-344. PMID: 28823795. [DOI] [PubMed] [Google Scholar]
- 9. Joseph R, Pan X, Cenkus K, Brown L, Ellis T, Di Stasi S. Sex differences in self-reported hip function up to 2 years after arthroscopic surgery for femoroacetabular impingement. Am J Sports Med. 2016;44(1):54-59. PMC5142445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kandil A, Safran MR. Hip arthroscopy: a brief history. Clin Sports Med. 2016;35(3):321-329. PMID: 27343387. [DOI] [PubMed] [Google Scholar]
- 11. Lau BC, Scribani M, Lassiter T, Wittstein J. Correlation of Single Assessment Numerical Evaluation Score for Sport and Activities of Daily Living to Modified Harris Hip Score and Hip Outcome Score in patients undergoing arthroscopic hip surgery. Am J Sports Med. 2019;47(11):2646-2650. PMID: 31348867 [DOI] [PubMed] [Google Scholar]
- 12. Marin-Peña O, Tey-Pons M, Perez-Carro L, et al. The current situation in hip arthroscopy. EFORT Open Rev. 2017;2(3):58-65. PMC5420826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Martin RL, Kivlan BR, Christoforetti JJ, et al. Minimal clinically important difference and substantial clinical benefit values for a pain visual analog scale after hip arthroscopy. Arthroscopy. 2019;35(7):2064-2069. PMID: 31208920. [DOI] [PubMed] [Google Scholar]
- 14. Newcomb NRA, Wrigley TV, Hinman RS, et al. Effects of a hip brace on biomechanics and pain in people with femoroacetabular impingement. J Sci Med Sport. 2018;21(2):111-116. PMID: 29074345. [DOI] [PubMed] [Google Scholar]
- 15. Nwachukwu BU, Chang B, Rotter BZ, Kelly BT, Ranawat AS, Nawabi DH. Minimal clinically important difference and substantial clinical benefit after revision hip arthroscopy. Arthroscopy. 2018;34(6):1862-1868. [DOI] [PubMed] [Google Scholar]
- 16. Sardana V, Philippon MJ, de Sa D, et al. Revision hip arthroscopy indications and outcomes: a systematic review. Arthroscopy. 2015;31(10):2047-2055. PMID 26033461. [DOI] [PubMed] [Google Scholar]
- 17. Stalzer S, Wahoff M, Scanlan M. Rehabilitation following hip arthroscopy. Clin Sports Med. 2006;25(2):337-357,x. PMID: 16638496. [DOI] [PubMed] [Google Scholar]
- 18. Sugarman EP, Birns ME, Fishman M, et al. Does capsular closure affect clinical outcomes in hip arthroscopy? A prospective randomized controlled trial. Orthop J Sports Med. 2021;9(5):2325967120963110. PMC8120543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Truntzer JN, Hoppe DJ, Shapiro LM, Abrams GD, Safran M. Complication rates for hip arthroscopy are underestimated: a population-based study. Arthroscopy. 2017;33(6):1194-1201. PMID: 28259588. [DOI] [PubMed] [Google Scholar]
- 20. West CR, Bedard NA, Duchman KR, Westermann RW, Callaghan JJ. Rates and risk factors for revision hip arthroscopy. Iowa Orthop J. 2019;39(1):95-99. PMC6604537. [PMC free article] [PubMed] [Google Scholar]