Abstract
Pandemics are complex events requiring a coordinated, global response. The response to the pandemic exposed vulnerabilities in system preparedness.
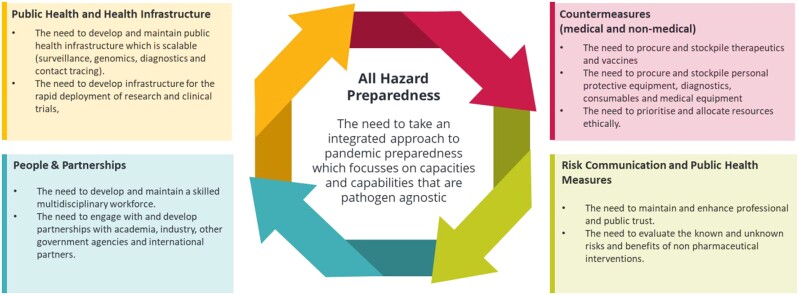
Lessons arising from the COVID-19 pandemic are characterized by four broad themes: (i) investment in public health and health infrastructure, (ii) countermeasures (medical and non-medical), (iii) risk communication and public health measures and (iv) investment in people and partnerships.
Learning from the COVID-19 pandemic identifies an approach that focusses on capacities and capabilities that are pathogen agnostic, ensuring that we can respond to diverse emerging infectious disease threats will be essential. The lessons learned from previous and ongoing infectious disease outbreaks should be kept under constant review, in line with technological and scientific advances, to improve our ability to detect, mitigate and respond to new and emerging threats.
Background
The response to the COVID-19 pandemic required a coordinated, global, whole-system response which exposed vulnerabilities in system preparedness. A report by the United Nations Environment Programme (UNEP) and International Livestock research Institute describes how COVID-19 is part of a growing trend of emerging zoonoses1 and while we cannot perfectly predict the characteristics of what the next pandemic might look like, it is a case of when and not if, a future pandemic will occur. It is imperative therefore that strategic and operational resilience is built into public health activities to enable the successful mitigation of the impact of future pandemics on the global population.
Pandemics are complex events that involve both political and health aspects. The focus of public health during a pandemic is to identify and contain the spread of the disease and to provide medical care to those who become infected. However, pandemics also have political dimensions due to the significant and widespread disruption to the economy, including interruptions to trade, supply chains and travel increasing social inequality and causing strained international relations.
The response to pandemics often involves coordination between health and political authorities, as well as collaboration across national and international borders. Governments play a critical role in developing policies and allocating resources to respond to pandemics, including funding for research and development, healthcare infrastructure and emergency response systems.
An integrated approach to pandemic preparedness—informed by learning from the response to the COVID-19 pandemic—focussing on capacities and capabilities that are pathogen agnostic and that can respond to any pathogen will be essential.
The key learning identified from the COVID-19 pandemic can be characterized by four broad themes: (i) investment in public health and health infrastructure, (ii) countermeasures (medical and non-medical); (iii) risk communication and public health measures and (iv) investment in people and partnerships (Figure 1).
Figure 1.
All-Hazard Preparedness: an integrated approach to pandemic preparedness that focusses on capacities and capabilities that are pathogen agnostic. This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
Public health and health infrastructure
The COVID-19 pandemic has shown the importance of investing in healthcare infrastructure.
A strong and effective public health infrastructure is essential not only to respond to emerging crises, but to detect and prevent them from developing in the first place. The response to the COVID-19 pandemic illustrated the importance of having the ability to mobilize and scale surveillance, genomics and research capabilities. This capability allowed the prevalence of the virus to be tracked across the UK, the detection of new variants and in turn, the analysis of both transmissibility and severity. Taken together, the overall impact that different waves and variants have on communities, and how it affects different social, ethnic and age groups could be understood. Without them, the ability to make timely and informed public health interventions would have been severely hampered.
Lesson 1: the need to develop and maintain public health and health infrastructure that is scalable (surveillance, genomics, diagnostics and contact tracing)
Surveillance
Effective surveillance systems are vital in controlling infectious disease outbreaks. The COVID-19 pandemic highlighted the importance of surveillance systems in detecting and monitoring the spread of a novel virus in real time. Examination of how COVID-19 surveillance was optimized can be used to maintain and improve surveillance for other infectious diseases.
The digitalization and data management electronic medical records, and online surveillance systems allowed for the rapid reporting of cases and contact tracing,2 determining the health impact to understand hospitalizations and deaths, and perform real-time vaccine effectiveness studies.3
First, molecular testing was used to rapidly detect and confirm cases of COVID-19.4 The development of rapid diagnostic tests enabled widespread testing, which allowed for the identification of cases and isolation of infected individuals.5 This technique enabled the identification of COVID-19 variants and their geographic spread.6
Furthermore, the UK developed national community and health care worker surveillance studies,7–9 regularly testing cohorts that provided valuable information to answer important questions including age profiles of those acquiring infection and their symptom profile, understanding the durability of the immune response and providing rapid assessments on the impact of vaccines.
The ability to answer the key questions on disease severity, transmission and the impact of interventions is essential and the ability to scale studies that can answer these questions in real time will be critical for future epidemics and pandemics.10
Genomics
In addition, the use of genomic sequencing allowed for the tracking of the spread of COVID-19.11 Some genomic sequencing was available from an early stage of the pandemic and, following the research funding provided to the COVID-19 Genomics UK consortium (COG-UK), retrospective analysis of incursions into the UK could be performed. By March 2021, the UK provided close to 50% of the world’s registered output in genomic sequencing of SARS-CoV-2. This genomic surveillance, sequencing and genotyping provided the ability to track and monitor the emergence of new variants, support research on vaccine and therapeutic effectiveness and support international collaboration and planning.12
The role of genomics in underpinning the efforts to understand and control future outbreaks is clear, but there is a need to develop and invest in the technology and infrastructure to collect genomic data and associated metadata at speed. New technologies in sequencing and bioinformatics have emerged in recent years, with some countries making major strides in establishing and strengthening their capacities and capabilities, this needs to continue and to be combined with clinical, epidemiological and other multi-source data to: identify emerging pathogens, or changes in recognized pathogens; understand pathogen characteristics and the potential biological impact, develop specific diagnostics, therapeutics and vaccines; and to inform public health measures by understanding disease transmission.
Ability to develop, validate and scale diagnostic testing
There needs to be investment in laboratory infrastructure to support rapid and accurate diagnosis of infectious diseases, including the development of metagenomics to detect the unknown emerging pathogens13 and development of rapid diagnostic tests to enable widespread testing.14,15
In January 2020, generic coronavirus assays developed post SARS were used to identify the potential new virus. The development of the specific assay occurred rapidly after the publication of the genome in January 2020.16 However, the ability to scale this diagnostic test to the allow the early identification and isolation of infected individuals, to control the spread of the virus, was slow and hindered the ability to identify individuals and isolate their contacts.
As capacity scaled, including the use of lateral flow rapid diagnostic tests, this allowed the detection of asymptomatic individuals, provided robust contact tracing and even provided novel methods to test individuals to release from isolation early or avoid isolation through daily or regular testing.17–22 Moreover, the development of rapid diagnostic tests has enabled quick and efficient testing at point-of-care settings, such as clinics, schools and workplaces. These tests provide results within minutes, allowing for immediate identification of infected individuals and isolation to prevent further transmission.23 Studies demonstrated that these tests could be rapidly deployed in the community, with results within 30 min and while sensitivity was lower than the gold-standard PCR, the ability to repeat them and to detect those with higher viral loads provided huge additional value over laboratory assays.24–26
Diagnostic tests have also played a crucial role in monitoring the effectiveness of vaccination programmes. Regular testing of vaccinated individuals has allowed for the identification of breakthrough infections and the implementation of appropriate measures to prevent further spread.27
Several studies have demonstrated the effectiveness of diagnostic tests in reducing COVID-19 transmission. A study conducted in the UK found that regular testing of healthcare workers reduced the risk of transmission by identifying asymptomatic cases and preventing outbreaks.28,29 Another study conducted in South Korea found that widespread testing and contact tracing measures were effective in controlling the spread of the virus.30
Optimally, in the future, we will need to be able to have sufficient equipment, consumables and staff trained to scale diagnostic testing to deliver large scale PCR tests per day within days to weeks of a pandemic declaration before the availability and validation of rapid diagnostic tests. Stockpiles of generic diagnostic tests would protect against lack of resilience in supply chains.
Contact tracing
Contact tracing is a critical component of infectious disease control, through identifying, monitoring, providing health information about the relevant infection and potentially isolating individuals who have been in contact with a case of infectious diseases. It enables chains of transmission to be broken. Traditional interview-based techniques are time consuming and during the COVID-19 pandemic, digital techniques were used by requesting cases to provide contact information and contact details through web-based forms that could allow automation and rapid information to be given to contacts. However, many contacts that individuals may have had on public transport, the work environment or in other public spaces will be unknown. The deployment of COVID app tools, using Google and Apple’s Bluetooth exposure notification platform allowed the notification of a potential high-risk contact and allowed those individuals to follow the relevant public health advice for their location. In England, such a tool was rolled out in late 2020 and was estimated to have saved 100 000 lives in its first year of use.31
Lesson 2: the need to develop infrastructure for the rapid deployment of research and clinical trials
Many WHO member states implemented the First Few X (FFX) enhanced surveillance protocol32 to investigate the clinical and epidemiological characteristics of at least the first 100 confirmed COVID-19 cases and their close contacts. These studies provided useful evidence for generating case definitions and informed modelling studies of the likely burden of COVID-19.33
During the COVID-19 pandemic, many thousand studies of therapeutics were initiated, however, many were underpowered to reach a primary outcome. The RECOVERY trial,34 using a multi-arm pragmatic adaptive trial design has been able to recruit more than 45 000 patients and determine the effectiveness (or not) of many drugs; it also used easily available end points that are available in clinical records to reduce the burden of data collection. In future, an anticipatory rather than reactive approach to pragmatic large scale clinical trial design and testing could improve regulatory approval processes, participant recruitment and operationalization.35
Animal studies were an important contribution to understanding the disease process, early therapeutic and vaccine studies across a range of variants. Maintaining the capability and reserve capacity to use animal models will be essential understand disease virulence, improve vaccine development and understand the biological response to therapeutics and vaccines.
Finally, international research consortia such as The International Severe Acute Respiratory and Emerging Infection Consortium have proved their ability to provide the operational capabilities to conduct clinical research in the context of an emerging infection, including the COVID-19 pandemic,36 the monkeypox outbreak37 and acute hepatitis of unknown aetiology in children.38 It will be important that infrastructures such as this are maintained and developed to provide the capabilities to respond to future emerging outbreaks.
All-hazard preparedness for an emerging health threat should include the development and maintenance of ‘sleeper’ studies and protocols that can be rapidly deployed to allow a range of information to be collected for new and emerging threats. This will enable the rapid generation of new knowledge to address the most important questions between and during epidemics and maximize the availability of clinical information through clinical characterization. There is an additional need to be able to rapidly evaluate the impact of non-pharmaceutical interventions. This will require dedicated funding and the ability to rapidly resource these initiatives.
Countermeasures (medical and non-medical)
Procuring medical supplies and ethical resource allocation thereafter needs to be a central consideration in all-hazard preparedness.
Lesson 3: the need to procure and stockpile therapeutics, vaccines, personal protective equipment, diagnostics, consumables and medical equipment
Procurement of essential medical supplies amid an evolving pandemic is difficult due to globally competitive supply chains.39 A pathogen specific approach to stockpiling is neither cost-effective, nor ensures preparedness for a threat from an unexpected pathogen.
Striking the balance between preparedness for the most likely threats (influenza) and unexpected threats should involve the combination of epidemiological, medical and commercial approaches. This should have the aim of procuring pathogen agnostic supplies (personal protective equipment, antibiotics and antivirals) that are dynamic and consider the wider effects of a new infectious threat including laboratory consumables. Any stockpiling should be sustainable and involve periodic reviews and the dynamic use of supplies to ensure cost-effectiveness and avoid unnecessary waste.
Finally, in the event of the next pandemic, drug and vaccine discovery will be expensive, time consuming and laborious. All-hazard preparedness should include the implementation of robust horizon scanning, defined as the systematic identification and evaluation of signals of potential risks and mitigations, to identify credible and plausible therapeutics and vaccines that can be repurposed and stockpiled for emerging infections.
Risk communication and public health measures
Lesson 4: the need to maintain and enhance professional and public trust
Public trust and transparency
Trust is one of public health’s best prophylactics with evidence suggesting that trust in government is one of the biggest predictors of adherence to public and social measures and vaccine acceptance.40–42 In a fast-changing pandemic context, where there is evolving evidence and changing guidance, it is important to have the ability relay information rapidly and transparently. One way in which trust is harmed is if the reasons or ‘the science’ behind decision making processes are not sufficiently transparent, as this is unlikely to instil trust. The COVID-19 dashboard43 has been a major contribution to transparency in the UK’s approach to the COVID-19 pandemic, becoming an essential tool for many and recognized internationally. While ensuring to protect individual patient privacy, work should continue to ensure open data sharing globally in a timely manner to ensure rapid and informed decisions can be made that are proportional to the threat. Misinformation is defined by the inadvertent spread of misleading and false information, whereas disinformation reflects the deliberate and coordinated spread of misleading and false information.44 Both mis- and disinformation can undermine efforts to protect public health and efforts should be made during non-pandemic periods to combat mis/disinformation and to build trust with communities through:
engagement with stakeholder and advocacy groups,
actively publishing and sharing verified information, and
improving media and health literacy.
Professional communications
There are additional unique challenges to communicating with healthcare professionals during a pandemic, which includes the ability to rapidly disseminate more technical communications (such as the UK technical briefings for COVID45 and updated medical guidance). In the rapidly changing context of a pandemic, healthcare professionals may often access information from the same sources as the public at the same time. It is therefore important to:
ensure mechanisms and communication channels are in place to rapidly disseminate urgent public health messages and technical guidance, and
ensure healthcare professionals are aware of these communication channels.
Lesson 5: the need to evaluate the known and unknown risks and benefits of non-pharmaceutical interventions
Non-pharmaceutical interventions, also known as ‘public health and social measures’, refers to measures to reduce transmission that does not depend on drugs, vaccines or other medical countermeasures. Examples include the use of face coverings, social distancing and travel restrictions.
Behavioural and social science insights
During the COVID-19 pandemic it was important to conduct rapid research and evaluation to understand how the behaviour of the public and professional communities’ changes in response to the novel infectious disease threat. Developing behavioural insights to understand the possible public behaviour changes that could be expected in a future pandemic and the impact of these on key sectors should form a key component of all-hazard preparedness. In the UK, preparedness work had identified the need for this work prior to the COVID-19 pandemic46,47 and web-based surveys were successfully used to track behaviour and compliance with public health measures throughout the pandemic.48
Developing an understanding of behaviour change and compliance with public health measures in an emerging incident requires continuous analysis in the medium term to generate behavioural insights to improve our public health campaigns and risk communications. This will also be important to ensure that any future public health interventions are designed and optimized using evidence from the behavioural and social sciences, with their effectiveness systematically evaluated.
Health inequalities
Public health measures and the burden of infectious diseases tend to disproportionally affect the most vulnerable groups in society, and this was exemplified in the COVID-19 pandemic.49 There is a need to develop the foundational capabilities for ‘hyperlocal’ engagement that can be rapidly scaled to gather insight from the groups of society most impacted by health threats and the potential unintended consequences associated public health measures. All-hazard preparedness work should include an emphasis on the ability to target resources on populations who are harder to reach with specific equality programmes with partner and stakeholder organizations.
People and partnerships
Lesson 6: the need to develop and maintain a skilled multidisciplinary workforce
Skill mix
It is important to identify, prioritize, recruit and maintain the skill mix required to prevent, detect, respond and mitigate a variety of hazards. An all-hazard response requires:
Frontline healthcare workforce: hospital-based, community-based, health and justice system and local public health experts
Scientific workforce: including biomedical and clinical scientists, data scientists, modellers, economists, epidemiologists, behavioural scientists and policy experts
Expert enabling workforce: finance, commercial, policy, human resources, technology and communications experts
It is neither feasible nor pragmatic to have the full-complement of the workforce required to respond to a pandemic in non-pandemic periods. Models from other emergency response functions such as the fire service could be emulated; in England in 2021, 35% of firefighters, representing 28% of whole-time equivalent employment, were retained reservists.50 A surge staff capacity and capability that combines a small but highly skilled retained reserve with a larger, more flexible volunteer reserve capacity would improve all-hazard preparedness51 and could be built with academia and industry.
Exercise planning
The COVID-19 pandemic has been a key learning exercise in itself, with many key lessons for the management of future pandemics. It is important to recognize, however, that the response to any future pandemic will be dependent on the pathogen, organizational, societal and political changes, technological advances and medical advances.
As we move forward, it will be important to develop and deliver multi-organizational and multi-professional exercises for a variety of hazards that:
test the readiness of the healthcare and public health infrastructure and other response mechanisms,
identify gaps in preparedness and
improve coordination among different agencies and organizations for a variety of hazards.
Lesson 7: the need to engage with and develop partnerships with academia, industry, other government agencies and international partners
One Health
The drivers of pandemics are often also the drivers of climate change and biodiversity loss. A One Health approach—which unites experts from multiple disciplines (public health, animal health, plant health and the environment) and engages partners from academia, industry and governments—will be required to enhance preparedness, mitigate the threats from infectious hazards and deliver outcomes that improve the health of people, wildlife and the planet.
Recommendations by the UNEP address this, and include expanding scientific enquiry into zoonoses, regulating and monitoring traditional food markets, incentivizing the legal wildlife trade and animal husbandry to adopt zoonotic control measures, and radically transforming food systems.1 The risk crosses all disciplines and borders and, as such, it is a global challenge requiring international cooperation.
International cooperation and data sharing
The COVID-19 pandemic has highlighted the challenges and opportunities of our inter-connected world in responding to global crises. The rapid rollout COVID-19 testing infrastructure, vaccine development programmes and global research collaborations in the spirit of cooperation and rapid data sharing illustrates the remarkable progress that can be achieved when the entire scientific community, industry, academia and governments unite towards a common goal.
Building on and formalizing the international partnerships and collaborations formed during the COVID-19 response and advocating for timely and open data, information and biological material sharing will enhance all-hazard preparedness and resilience against the next infectious disease threat.
Conclusion
Future health threats to the UK will probably be from importation and as such, work should continue to build the capabilities to develop long-term threat assessments, promote international collaboration and epidemic intelligence scanning, and consider the use of anonymized border health surveillance activities such as pan-respiratory virus screening to detect emerging pathogens from countries where surveillance systems are less mature. As we move into a post-pandemic period, it will be important to refine all-hazard surveillance capabilities to predict, detect and develop understanding of future human health threats, not just domestically, but globally.
Achieving all-hazard preparedness means keeping plans under constant review and a commitment to building capabilities to improve our ability to detect, mitigate and respond to new and emerging threats. As we prepare for a future pandemic, which will look different from COVID-19, all-hazard preparedness plans should evolve in response to technological and scientific advancements, lessons learned from previous and ongoing infectious disease outbreaks and rigorous exercising to test our response mechanisms.
Acknowledgements
None.
Contributor Information
Neil Cunningham, Clinical and Public Health Group, United Kingdom Health Security Agency (UKHSA), London, UK.
Susan Hopkins, Clinical and Public Health Group, United Kingdom Health Security Agency (UKHSA), London, UK.
Funding
Open Access CC-BY-NC is sponsoring open access for this paper. This paper was published as part of a supplement financially supported by an educational grant from Roche Molecular Systems.
Transparency declarations
None.
References
- 1. United Nations Environment Programme and International Livestock Research Institute 2020 . Preventing the Next Pandemic: Zoonotic diseases and how to break the chain of transmission. https://www.unep.org/resources/report/preventing-future-zoonotic-disease-outbreaks-protecting-environment-animals-and, 2020.
- 2. Banskota S, Healy M, Goldberg EM. 15 Smartphone apps for older adults to use while in isolation during the COVID-19 pandemic. West J Emerg Med 2020; 21:514–25. 10.5811/westjem.2020.4.47372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lopez Bernal J, Andrews N, Gower Cet al. . Effectiveness of COVID-19 vaccines against the B.1.617.2 (Delta) variant. N Engl J Med 2021; 385:585–94. 10.1056/NEJMoa2108891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lescure FX, Bouadma L, Nguyen Det al. . Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect Dis 2020; 20:697–706. 10.1016/S1473-3099(20)30200-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kohmer N, Toptan T, Pallas Cet al. . The comparative clinical performance of four SARS-CoV-2 rapid antigen tests and their correlation to infectivity in vitro. J Clin Med 2021; 10:328. 10.3390/jcm10020328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang H, Miller JA, Verghese Met al. . Multiplex SARS-CoV-2 genotyping reverse transcriptase PCR for population-level variant screening and epidemiologic surveillance. J Clin Microbiol 2021; 59:e0085921. 10.1128/JCM.00859-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Riley S, Atchison C, Ashby Det al. . Real-time assessment of community transmission (REACT) of SARS-CoV-2 virus: study protocol. Wellcome Open Res 2021; 5: 200. 10.12688/wellcomeopenres.16228.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. ONS Coronavirus (COVID-19) Infection Survey 2022 . Antibody data by UK country and age in England from the Coronavirus (COVID-19) Infection Survey. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronaviruscovid19infectionsurveyantibodyandvaccinationdatafortheuk/24august2022, 2022.
- 9. UK Health Security Agency 2022 . SIREN study: Providing vital research into coronavirus (COVID-19) immunity and vaccine effectiveness nationally. https://www.gov.uk/guidance/siren-study, 2022.
- 10. Bhatia S, Imai N, Watson Oet al. . Lessons from COVID-19 for rescalable data collection. Lancet Infect Dis 2023; 23: e383–8. 10.1016/S1473-3099(23)00121-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lorenzo-Redondo R, Machado de Sant’Anna Carvalho A, Hultquist JFet al. . SARS-CoV-2 genomics and impact on clinical care for COVID-19. J Antimicrob Chemother 2023. [details to be added as this paper is in included in this supplement]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bou-Antoun S, Rokadiya S, Ashiru-Oredope Det al. . Considerations for antimicrobial resistance and stewardship of COVID-19 therapeutics. J Antimicrob Chemother 2023. [details to be added as this paper is in included in this supplement]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ko KKK, Chng KR, Nagarajan N. Metagenomics-enabled microbial surveillance. Nat Microbiol 2022; 7: 486–96. 10.1038/s41564-022-01089-w [DOI] [PubMed] [Google Scholar]
- 14. Rabe BA, Cepko C. SARS-CoV-2 detection using isothermal amplification and a rapid, inexpensive protocol for sample inactivation and purification. Proc Natl Acad Sci U S A 2020; 117:24450–8. 10.1073/pnas.2011221117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Peto T, UK COVID-19 Lateral Flow Oversight Team . COVID-19: rapid antigen detection for SARS-CoV-2 by lateral flow assay: a national systematic evaluation of sensitivity and specificity for mass-testing. EClinicalMedicine 2021; 36: 100924. 10.1016/j.eclinm.2021.100924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Carter LJ, Garner LV, Smoot JWet al. . Assay techniques and test development for COVID-19 diagnosis. ACS Cent Sci 2020; 6:591–605. 10.1021/acscentsci.0c00501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Leng T, Hill EM, Holmes Aet al. . Quantifying pupil-to-pupil SARS-CoV-2 transmission and the impact of lateral flow testing in English secondary schools. Nat Commun 2022; 13: 1106. 10.1038/s41467-022-28731-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. UK Government 2021 . Position statement regarding daily contact testing in schools from PHE and NHS Test and Trace. https://www.gov.uk/government/publications/daily-contact-testing-in-schools-statement-from-phe-and-nhs-tt-about-next-steps/position-statement-regarding-daily-contact-testing-in-schools-from-phe-and-nhs-test-and-trace, 2021.
- 19. UK Health Security Agency 2022 . Evaluation of daily testing for contacts of COVID-19 cases (DTCC). https://www.gov.uk/government/publications/daily-testing-of-contacts-of-covid-19-cases-evaluation, 2022.
- 20. Bays D, Whiteley T, Williams Het al. . Mitigating isolation: further comparing the effect of LFD testing for early release from self-isolation for COVID-19 cases. medRxiv (preprint)2022. 10.1101/2022.01.25.22269818 [DOI] [Google Scholar]
- 21. Bays D, Whitely T, Pindar Met al. . Mitigating isolation: the use of rapid antigen testing to reduce the impact of self-isolation periods. medRxiv (preprint)2021. 10.1101/2021.12.23.21268326 [DOI] [Google Scholar]
- 22. Hakki S, Zhou J, Jonnerby Jet al. . Onset and window of SARS-CoV-2 infectiousness and temporal correlation with symptom onset: a prospective, longitudinal, community cohort study. Lancet Respir Med 2022; 10:1061–73. 10.1016/S2213-2600(22)00226-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sharma A, Balda S, Apreja Met al. . COVID-19 diagnosis: current and future techniques. Int J Biol Macromol 2021; 193(Pt B):1835–44. 10.1016/j.ijbiomac.2021.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fowler T, Fellows A, MacIsaac Ret al. . The evaluation of a multi-day testing approach with antigen lateral flow devices for people eligible for community-based COVID-19 treatments. J Antimicrob Chemother 2023. [details to be added as this paper is in included in this supplement]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pekosz A, Parvu V, Li Met al. . Antigen-based testing but not real-time polymerase chain reaction correlates with severe acute respiratory syndrome coronavirus 2 viral culture. Clin Infect Dis 2021; 73:e2861–6. 10.1093/cid/ciaa1706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dinnes J, Sharma P, Berhane Set al. . Rapid, point-of-care antigen tests for diagnosis of SARS-CoV-2 infection. Cochrane Database Syst Rev 2022; 7: CD013705. 10.1002/14651858.CD013705.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tillett RL, Sevinsky JR, Hartley PDet al. . Genomic evidence for reinfection with SARS-CoV-2: a case study. Lancet Infect Dis 2020; 21: 52–8. 10.1016/S1473-3099(20)30764-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Adams ER, Ainsworth M, Anand Ret al. . National COVID testing scientific advisory panel. Antibody testing for COVID-19: a report from the national COVID scientific advisory panel. Wellcome Open Res 2020; 5: 139. 10.12688/wellcomeopenres.15927.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. UK Health Security Agency 2022 . NHS workforce repeat asymptomatic testing. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1150866/NHS-workforce-repeat-asymptomatic-testing-evaluation-report.pdf, 2022.
- 30. Park Y, Huh IS, Lee Jet al. . Seoul Metropolitan Government COVID-19 Rapid Response (SCoRR) team. Application of testing-tracing-treatment strategy in response to the COVID-19 outbreak in Seoul, Korea. J Korean Med Sci 2020; 35:e396. 10.3346/jkms.2020.35.e396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kendall M, Tsallis D, Wymant Cet al. . Epidemiological impacts of the NHS COVID-19 app in England and Wales throughout its first year. Nat Commun 2023; 14: 858. 10.1038/s41467-023-36495-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. World Health Organization 2019 . Coronavirus disease (COVID-19) technical guidance: the Unity studies: early investigation protocols. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/early-investigations, 2019.
- 33. Boddington NL, Charlett A, Elgohari Set al. . Epidemiological and clinical characteristics of early COVID-19 cases, United Kingdom of Great Britain and Northern Ireland. Bull World Health Organ 2021; 99:178–89. 10.2471/BLT.20.265603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Clinical Trials 2020 . Randomised Evaluation of COVID-19 Therapy (RECOVERY). https://clinicaltrials.gov/ct2/show/NCT04381936, 2020.
- 35. Horsley AR, Pearmain L, Knight Set al. . Large scale clinical trials: lessons from the COVID-19 pandemic. BMJ Open Respir Res 2022; 9: e001226. 10.1136/bmjresp-2022-001226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. International Severe Acute Respiratory and emerging Infection Consortium 2023 . COVID-19 Clinical Research Resources. https://isaric.org/research/covid-19-clinical-research-resources/, 2023.
- 37. International Severe Acute Respiratory and emerging Infection Consortium 2023 . Monkeypox Response. https://isaric.org/research/monkeypox-response/, 2023.
- 38. International Severe Acute Respiratory and Emerging Infection Consortium 2023 . Severe Acute Hepatitis. https://isaric.org/research/severeacutehepatitis/, 2023.
- 39. UK Health Security Agency 2022 . Technical report on the COVID-19 pandemic in the UK - Chapter 9: pharmaceutical interventions: therapeutics and vaccines. https://www.gov.uk/government/publications/technical-report-on-the-covid-19-pandemic-in-the-uk, 2022.
- 40. Wright L, Steptoe A, Fancourt D. Predictors of self-reported adherence to COVID-19 guidelines. A longitudinal observational study of 51,600 UK adults. Lancet Reg Health Eur 2021; 4: 100061. 10.1016/j.lanepe.2021.100061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Williams SN, Armitage CJ, Tampe Tet al. . Public perceptions of non-adherence to pandemic protection measures by self and others: a study of COVID-19 in the United Kingdom. PLoS ONE 2021; 16: e0258781. 10.1371/journal.pone.0258781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Burgess RA, Osborne RH, Yongabi KAet al. . The COVID-19 vaccines rush: participatory community engagement matters more than ever. Lancet 2021; 397: 8–10. 10.1016/S0140-6736(20)32642-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. UK Health Security Agency 2023 . COVID-19 Dashboardhttps://coronavirus.data.gov.uk/, 2023.
- 44. Felten C, Nelson A. Countering misinformation with lessons from public health. New Perspect Foreign Policy 2019; 18: 52. [Google Scholar]
- 45. UK Health Security Agency 2021 . Investigation of SARS-CoV-2 Variants. https://www.gov.uk/government/publications/investigation-of-sars-cov-2-variants-technical-briefings, 2021.
- 46. Rubin GJ, Bakhshi S, Amlot Ret al. . The design of a survey questionnaire to measure perceptions and behaviour during an influenza pandemic: the flu telephone survey template (FluTEST). Health Serv Delivery Res 2014; 2:1–125. 10.3310/hsdr02410 [DOI] [PubMed] [Google Scholar]
- 47. Simpson CR, Knight M, Beever Det al. . The UK's pandemic influenza research portfolio: a model for future research on emerging infections. Lancet Infect Dis 2019; 19:e295–300. 10.1016/S1473-3099(18)30786-2 [DOI] [PubMed] [Google Scholar]
- 48. Smith LE, Potts HWW, Amlôt Ret al. . Adherence to the test, trace, and isolate system in the UK: results from 37 nationally representative surveys. BMJ 2021; 372: n608. 10.1136/bmj.n608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Public Health England 2020 . Disparities in the risk and outcomes of COVID-19. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/908434/Disparities_in_the_risk_and_outcomes_of_COVID_August_2020_update.pdf, 2020.
- 50. UK Home Office 2021 . FIRE1101: Staff in post employed by fire and rescue authorities by headcount and full time equivalent by role and fire and rescue authority. https://www.gov.uk/government/statistical-data-sets/fire-statistics-data-tables#workforce-and-workforce-diversity, 2021.
- 51. Skittrall JP, Bentley N, Wreghitt Tet al. . Preparing for the next pandemic: reserve laboratory staff are crucial. BMJ 2022; 378: e072467. 10.1136/bmj-2022-072467 [DOI] [PubMed] [Google Scholar]