Summary
The South-East Asia Region (SEAR) adopted the goal of “measles and rubella elimination by 2023”. The goal was revised in 2019 to ‘measles and rubella elimination by 2023’ The strategies adopted to reach the goal included achieving ≥95% coverage with 2 doses of measles- and rubella-containing vaccine (MCV2; RCV2); establishing effective case-based surveillance supported by an accredited laboratory network; and implementing rapid response measures to control measles outbreaks. Of the 11 countries in the Region, to date five countries have eliminated measles and rubella and two more have controlled rubella. An estimated 242 million cases and 4.7 million deaths due to measles were averted between 2014 and 2022. The high-level political commitment, programmatic infrastructure and partnerships developed for the elimination of polio and maternal and neonatal tetanus played a critical role in this achievement. WHO, supported by key partners, provided technical support and strategic guidance for programmatic improvements, generated evidence to guide policy and strategic shifts, strengthened capacity of health workforce and conducted periodic programmatic reviews. However, unexpected occurrence of COVID-19 pandemic impacted vaccine coverage and quality of surveillance, thereby delaying achievement of the goal, and necessitating a revision of the target date of elimination.
Keywords: Measles, Rubella, Vaccination, Elimination, Vaccine preventable diseases
Search strategy.
This review draws from information already available with the WHO Offices as a part of this initiative. Additional sources of information were accessed through a literature search of available related articles, grey literature and library search on reports was conducted from publicly available sources. The primary databases employed were Medline through PubMed (https://pubmed.ncbi.nlm.nih.gov/), and World Health Organization (WHO) institutional repository for information sharing (IRIS) available online (https://apps.who.int/iris/). No attempt was made to obtain unpublished data, data unavailable in the public domain, or data available within specific institutions at the national, state or local level.
This study estimated measles deaths and cases averted during this period using the measles mortality model adopted by WHO-UNICEF. This model is rerun each year using the new and revised annual WHO-UNICEF estimates of national immunization coverage data as well as updated surveillance data. We used an updated (2021) data on case fatality from a recent systematic review and a suite of covariates with known relationships to case fatality in a Bayesian meta-regression modeling framework to produce estimates of measles case fatality ratios.1
Introduction
Measles, a single-stranded, RNA respiratory tract virus commonly found in children, is one of the most contagious disease of humans, especially in children.2 Before the introduction of measles vaccine in 1963, major epidemics occurred every 2–3 years with an estimated 30 million cases and more than 2 million deaths occurring globally each year due to measles, and more than 95% of individuals had been infected with measles virus by the age of 15 years.3 Similarly, Rubella virus is generally recognized as the most common infectious cause of birth defects, accounting for an estimated 100,000 infants born with congenital rubella syndrome (CRS) each year worldwide.4 For both these diseases, the primary strategy for prevention is vaccination.
While the average return on investment (ROI) from the childhood vaccination program with WHO recommended antigens is 44 times the cost of these programs, the highest returns are associated with averting measles, at 58 times the cost through two routine immunization doses. Additionally, the ROI is 2.02 times for rubella.5,6 The Immunization Agenda 2030 identifies measles vaccination coverage and incidence recorded by surveillance as tracer indicators to identify communities and population groups that are un- or under immunized.7 Measles vaccination coverage is also an important indicator for attaining the Sustainable Development Goal (SDG) 3.2 which specifically says, “By 2030, end preventable deaths of newborn babies and children under 5 years of age, with all countries aiming to reduce neonatal mortality to at least as low as 12 per 1000 live births and under-5 mortality to at least as low as 25 per 1000 live births”.8 Measles and rubella elimination and the entire immunization program is expected to have a positive impact on 14 out of the 17 SDGs.9
In 2013, following an extensive consultation and review of the benefits and the biologic, programmatic, and financial feasibility of measles and rubella elimination, the eleven Member States of the World Health Organization (WHO) South-East Asia Region (SEAR)e adopted the goal of measles elimination (absence of endemic measles cases for a period of ≥12 months) and rubella and congenital rubella syndrome control (95% reduction in disease incidence from the 2013 level) by 2020.10 At that time, no global goal for measles and rubella elimination existed; a situation that has remained unchanged.11 In 2014, to provide impetus toward achieving this goal, the South-East Asia Region declared measles elimination and rubella control as one of the Regional Flagship Priorities.12,13 In 2019, based on an in-depth independent review of the status of rubella control and a consultation with experts and Member States and taking the opportunity offered by measles elimination activities, the goal was revised to eliminating both measles and rubella (defined as for measles) by 2023.14 The strategies adopted to achieve the goal were:
-
1)
Achieving and maintaining ≥95% coverage with 2 doses of measles- and rubella-containing vaccine in every district through routine or supplementary immunization activities (SIAs)f;
-
2)
Developing and sustaining a sensitive and timely case-based surveillance system that met recommended performance indicators;
-
3)
Developing and maintaining an accredited laboratory network;
-
4)
Achieving timely identification, investigation and response to measles outbreaks; and
-
5)
Linking with other public health initiatives to achieve the preceding four strategies.15
The purpose of this article is to review the progress achieved in the measles and rubella elimination efforts in WHO South-East Asia Region and identify key facilitators and barriers for the progress.
Progress in measles/rubella vaccination during the last decade
During the decade, access to two doses of measles containing vaccine and at least one dose of rubella containing vaccine was greatly enhanced (Table 1).
Table 1.
Date of introduction of measles and rubella containing vaccines in SEAR Countries.
| Country | MCV1 | MCV2a | RCV1a | RCV2a |
|---|---|---|---|---|
| Bangladesh | 1979 | 2012 | 2012 | 2015 |
| Bhutan | 1979 | 2006 | 2006 | 2006 |
| DPR Korea | 1997 | 2008 | 2019 | 2019 |
| India | 1985 | 2010 | 2017 | 2017 |
| Indonesia | 1982 | 2003 | 2017 | 2017 |
| Maldives | 1983 | 2007 | 2007 | 2017 |
| Myanmar | 1987 | 2012 | 2015 | 2017 |
| Nepal | 1988 | 2015 | 2013 | 2015 |
| Sri Lanka | 1984 | 2001 | 1996 | 2001 |
| Thailand | 1984 | 1996 | 1986 | 1997 |
| Timor-Leste | 1982 | 2016 | 2016 | 2016 |
MCV1- first dose of measles containing vaccine; MCV2-second dose of measles containing vaccine; RCV1- first dose of rubella containing vaccine and RCV2-second dose of rubella containing vaccine.
Between 2013 and 2022, approximately 314 million children have been vaccinated with the first dose of measles containing vaccine (MCV1), 265 million with the second dose of measles containing vaccine (MCV2) and 187 million children with the first dose of rubella containing vaccine (RCV1) as a part of routine immunization activities.16 All countries in the Region conducted supplementary immunization activities (SIAs) with measles and/or rubella containing vaccine and more than 653 million children were vaccinated during these SIAs in various age groups.17,18
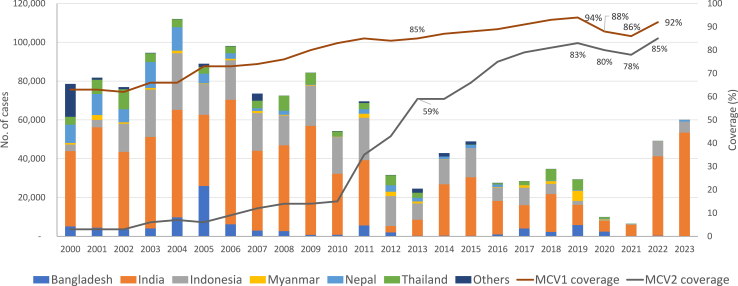
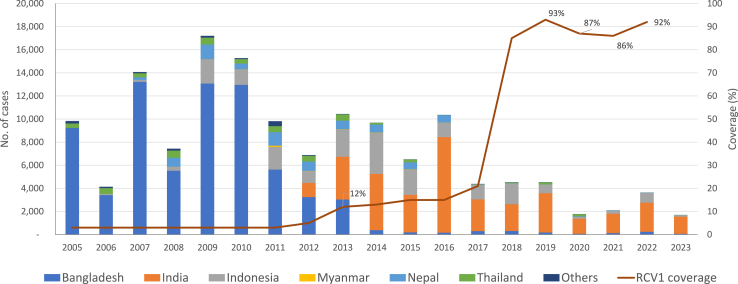
Coverage with MCV1 increased from 85% in 2013 to an all-time high of 94% in 2019. Similarly, the coverage of MCV2 was reported at 83% in 2019 compared to 59% in 2013. The coverage of RCV1 in 2019 was estimated at 93% compared to 12% in 2013.16 The Region was however significantly hit by the COVID-19 pandemic in 2020 and 2021 and observed a significant decline in coverages of measles and rubella containing vaccine.19 (Figs. 1 and 2) The Region reported an 8% decline in MCV1, 11% decline in MCV2 and a 7% decline in RCV1 coverage in 2021 compared with 2019. This was followed by a sharp recovery of MCV1 and MCV2 coverage in the Region in 2022, with the MCV1 coverage only 2% below the 2019 level, and the MCV2 coverage 2% above the 2019 level.16 A total of 49,201 suspected measles cases were reported in 2022 compared with 31,091 in 2020 and 69,207 in 2019.
Fig. 1.
Number of reported measles cases∗ and estimated percentage of children who received their first and second dose of measles-containing vaccine (MCV),† by country — World Health Organization (WHO) South-East Asia Region (SEAR), 2000–2023. Abbreviations: MCV1 = first dose of MCV in routine immunization; MCV2 = second dose of MCV in routine immunization. ∗Cases of measles reported to WHO and the United Nations Children’s Fund (UNICEF) through the Joint Reporting Form from WHO-SEAR. †Data are from WHO and UNICEF estimates for SEAR, available at http://immunizationdata.who.int. §Others include Bangladesh, Bhutan, DPR Korea, Maldives, Myanmar, Nepal, Sri Lanka, Timor-Leste.
Fig. 2.
Number of reported rubella cases∗ and estimated percentage of children who received their first dose of rubella vaccine (RCV),† by country — World Health Organization (WHO) South-East Asia Region (SEAR), 2005–2023. Abbreviations: MCV1 = first dose of MCV in routine immunization; MCV2 = second dose of MCV in routine immunization. ∗Cases of measles reported to WHO and the United Nations Children’s Fund (UNICEF) through the Joint Reporting Form from WHO-SEAR. †Data are from WHO and UNICEF estimates for SEAR, available at http://immunizationdata.who.int. §Others include Bangladesh, Bhutan, DPR Korea, Maldives, Myanmar, Nepal, Sri Lanka, Timor-Leste.
In 2013, all countries were conducting case-based surveillance which transformed to “Laboratory Supported Acute Fever and Rash Surveillance” by 2021. This effort was coupled with expansion of laboratory network from 23 laboratories in 2013 to 58 proficient laboratories in 2022 with at least 26 Measles-Rubella (MR) laboratories conducting both serology and Reverse Transcriptase - Polymerase Chain Reaction (RT-PCR) for measles and rubella and four laboratories including the Regional Reference Laboratory (RRL) in Bangkok, Thailand, also conducting viral genome sequencing.20 The sensitivity of measles and rubella surveillance as measured by the cardinal indicator of non-measles non-rubella discarded caseg rate per 100,000 population has increased from less than 0.5 is 2013 to around 3.79 in 2022—a more than seven-fold increase in the sensitivity of surveillance.21
By the end of 2021, the Region was no longer a major contributor to the global measles mortality burden. In 2014, the Region contributed to 40% (46,900 of total 114,900) of global measles deaths which reduced to 8% (10,230 of total 127,656) in 2021.22,23 The estimated annual number of deaths due to measles decreased by 78% (from 46,900 to 10,230 during the same period). Modeling data has estimated that cumulatively more than 242 million cases and more than 4.76 million deaths due to measles would have been averted due to vaccination during this period (Table 2).15,22,24, 25, 26
Table 2.
Estimated coveragea with the first and second dose of measles-containing vaccine (MCV), vaccination schedule,b number of reported measles cases,c and measles incidence,d,e by country — World Health Organization South-East Asia Region, 2003 and 2022.
| Country | 2003 |
2022 |
% change, 2003–2022 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| WHO/UNICEF estimated coveragea (%) |
MCV scheduleb |
No. reported measles cases (JRF)c | measles incidenced,e | WHO/UNICEF estimated coveragea (%) |
MCV scheduleb |
No. reported measles cases (JRF)c | Measles incidenced,e | MCV1 coverage | measles incidencee | |||||
| MCV1 | MCV2 | MCV1 | MCV2 | MCV1 | MCV2 | MCV1 | MCV2 | |||||||
| Bangladesh | 76 | —f | M-9 m | —f | 4067 | 30.2 | 97 | 93 | MR-9 m | MR-15 m | 311 | 1.8 | 28 | −94 |
| Bhutan | 88 | —f | M-9 m | —f | 0 | 0.0 | 97 | 97 | MMR-9 m | MMR-24 m | 7j | 0 | 10 | 0 |
| DPR Korea | 95 | —f | M-9 m | —f | 0 | 0.0 | 0k | 0k | MR-9 m | MR-15 m | 0 | 0 | −100 | 0 |
| India | 60 | —f | M-9 m | —f | 47,147 | 42.4 | 95 | 90 | MR-9 m | MR-16–24 m | 40,967 | 28.9 | 58 | −32 |
| Indonesia | 74 | 21g | M-9 m | M-7 yg | 24,457 | 111.0 | 84 | 67 | MR-9 m | MR-18 mh | 7704 | 28 | 14 | −75 |
| Maldives | 96 | —f | M-9 m | —f | 75 | 247.8 | 98 | 98 | MR-9 m | MMR-18 m | 0 | 0 | 2 | −100 |
| Myanmar | 80 | —f | M-9 m | —f | 830 | 17.2 | 75 | 90 | MR-9 m | MR-18 m | 10 | 0.2 | −6 | −99 |
| Nepal | 75 | —f | M-9 m | —f | 13,344 | 532.0 | 90 | 87 | MR-9 m | MR-15 m | 130 | 4.3 | 20 | −99 |
| Sri Lanka | 99 | 90 | M-9–12 mi | MR-3 y | 65 | 3.4 | 99 | 98 | MMR-9 m | MMR-3 y | 0 | 0.0 | 0 | −100 |
| Thailand | 96 | 92 | M-9 m | MMR-6 y | 4519 | 70.0 | 96 | 87 | MMR-9 m | MMR-1.5 y | 64 | 0.9 | 0 | −99 |
| Timor-Leste | 55 | —f | M-9 m | —f | 94 | 99.2 | 79 | 78 | MR-9 m | MR-18 m | 8j | 0 | 44 | −94 |
| Region overall | 66 | 6 | 94,598 | 57.4 | 92 | 85 | 49,201 | 23.8 | 39 | −59 | ||||
JRF = joint reporting form; m = months; M = measles; MCV = measles-containing vaccine; MR = measles-rubella; MMR = measles-mumps-rubella; UNICEF = United Nations Children’s Fund; y = years.
Data were from WHO and UNICEF estimates, 2020 revision (as of July 2021). Data available at http://immunizationdata.who.int.
As reported to WHO/UNICEF on JRFs for the year.
JRF was submitted to WHO and UNICEF by member states with the official immunization data and the number of measles cases in the country for the year.
Measles incidence is calculated based on the reported measles cases and population by member states through WHO/UNICEF JRF.
Cases per million population (excluding imported cases in countries verified to have eliminated measles).
MCV2 was not introduced into routine immunization.
Sub-national introduction in schools of West Java at age 7 years.
MCV third dose given in schools at grade 1.
Changed in 2011 from age 9 months to 9–12 months.
Imported or import related cases.
No vaccination conducted due to COVID-19 pandemic related barriers leading to vaccine stockout.
All countries in the region were endemic (continuous transmission of indigenous or imported cases that persists for ≥12 months in any defined geographical area) to measles and rubella in 2013. Following accelerated deployment of the elimination strategies, by October 2023, five countries—Bhutan, DPR Korea, Maldives, Sri Lanka and Timor-Leste were verified to have eliminated measles and rubella based on the verification framework developed by WHO.27,28 Two additional countries were verified to have controlled rubella and congenital rubella syndrome—Bangladesh and Nepal during this period.29, 30, 31
We discuss below enabling factors and challenges faced in this effort, however, much more remains to be done in reaching the ultimate target of elimination.
Enabling factors
The Region’s efforts over polio and maternal and neonatal tetanus elimination, and increases in routine immunization coverage, laid the foundations for establishing the goal of elimination of measles and rubella.32, 33, 34, 35, 36 The available infrastructure and capacity, especially for surveillance and vaccine deployment, were recalibrated for efficient implementation of regional strategy.37, 38, 39
Political and programmatic commitment
The Region, through its various regional committee resolutions expressed ownership and highest level of political commitment to achieve the goal of measles and rubella elimination in the context where there was no global goal to guide the program.9,13 Declaring measles and rubella elimination as a flagship programme underscored the commitment and gave additional impetus.12 This resulted in the development of a National Strategic Plan for measles and rubella elimination in each of the eleven Member States of the South-East Asia Region that provided the impetus for an accelerated implementation of activities as outlined in the results section.
Partnerships and collaborations
Much of the achievement of immunization in South-East Asia Region is a result of partnership that brought a range of stakeholders together – medical doctors, health workers, laboratory technicians, officials working in regulatory agencies, policymakers in health ministries, local partners, international agencies.37, 38, 39, 40 The Immunization task forces, or the immunization coordination committees created at all levels of administration in larger countries were utilized as oversight mechanisms for measles and rubella elimination. At subnational level, large countries activated or established multisectoral, intersectoral and cross-border collaborations created for previous elimination programs to enhance implementation of the strategies.41,42
Clear articulation of strategies and directives
‘The Strategic plan for measles elimination and rubella and congenital rubella syndrome control in the South-East Asia Region, 2014–2020’ and a costed ‘Strategic plan for measles and rubella elimination in WHO South-East Asia Region: 2020–2024’ developed during the period provided the strategic framework to the program and identified five key areas of focus for program implementation viz-immunization, surveillance, laboratory support, outbreak response and creating enabling environment through advocacy, enhanced program oversight and better program governance.14,43 The first document focused more on developing the systems and the processes and the second document focused more on innovative approaches to accelerating progress.
Technical leadership
The Regional and National Immunization Technical Advisory Groups provided overall technical leadership to the immunization program while the Regional Verification Commission for measles and rubella elimination (SEA-RVC), established in 2016, monitored the implementation of norms and standards through the process of in-depth country program evaluation, site visits, as well as the intensive review of the annual progress report submitted by the national verification committees applying the standard criteria laid out in the “Framework for verification of measles and rubella elimination”. This Framework was developed by WHO in 2016 and revised in 2020, in consultation with experts and Member States.27,28,44 The corresponding National Verification Committees (NVC) in the countries worked with respective governments to provide technical leadership and monitor progress towards the goal of measles and rubella elimination.29, 30, 31,45, 46, 47
A measles, rubella and congenital rubella syndrome surveillance guide was also developed in 2017 and updated in 2022 to support Member States to develop and implement elimination standard surveillance for measles and rubella.48
High quality operations including monitoring, evaluation and course corrections
The country teams of WHO and partners provided support to ensure high quality operations. This included ensuring guidance on establishing high quality vaccine supply chain, cold chain, safe injection practices, and waste management among various other measures. Significant focus was maintained on monitoring evaluation and course correction. Programmatic risk assessment for measles and rubella transmission was conducted periodically in all countries on an annual basis since 2017 and reviewed jointly by the national immunization programs and national verification committees to prioritize geographical areas and develop further strategies to mitigate the risk of measles and rubella transmission as well as to close the immunity gaps through vaccination activities.34
Periodic independent external evaluations were also conducted at regional and national level to inform timely course corrections.24, 25, 26 This included revising the goal of rubella control to rubella elimination; shifting the target date from 2019 to 2023; changing the case definition for suspected measles to a more sensitive syndromic approach of ‘Acute fever and rash surveillance’ and revision of the surveillance reporting sites in large countries involving more community informants.
Research and development
Several research studies to guide strategic interventions in the measles and rubella programme have been under implementation during the period. These include costing of measles and rubella elimination in the WHO South-East Asia Region; sero-surveys to assess the population immunity profile against measles and rubella for better targeting of SIAs in India and Nepal; assessment of other differential diagnoses of acute fever and rash to help determine if the current target of two non-measles, non-rubella fever and rash cases per 100,000 population needs revision; and development of rapid diagnostic test kit for measles and rubella.49 Emerging technologies like microarray patches for vaccine administration appear promising for operations of the future.
Challenges
The COVID-19 pandemic impacted the delivery of immunization and surveillance activities, posing significant challenges to achieve the measles and rubella elimination goal by 2023.50 Despite the challenges brought on by the pandemic, Bhutan, DPR Korea, Maldives, Sri Lanka and Timor-Leste sustained their measles elimination status while Maldives and Sri Lanka sustained their rubella elimination status.51
Significant challenges to achieve measles and rubella elimination in the Region remain irrespective of the pandemic, the greatest of which was to improve routine immunization programmes to 95% or more coverage with two doses of a measles-rubella containing vaccine in all districts of all countries. The un-evenness in vaccination coverage, due to operational issues as well as pockets of vaccine hesitancy remain a major challenge, especially in large countries of the Region. The accumulation of susceptible cohorts of children due to chronic gaps that further widened during the COVID-19 pandemic pose a risk of outbreaks of measles and rubella outbreaks. A root cause analysis of outbreaks conducted has demonstrated that these outbreaks have occurred because of failure to vaccinate due to either access issues or due to hesitancy to accept the vaccines by selected population groups, most of whom remain generally underserved for overall health services. Lack of awareness of benefits of vaccination campaigns is considered to have contributed to vaccine hesitancy. A similar approach to polio will be essential in the current situation for the special populations that remain hesitant to vaccination against measles and rubella.
Sensitivity of surveillance for measles and rubella remained sub-optimal in several endemic countries resulting in under reporting and underestimation of the disease burden. Of the measles outbreaks reported in the Region in 2022, only nearly half of these were responded with adequate immunization activities. Financial insufficiency and inadequate commitment for optimal implementation of key strategies at the sub-national level were major hindrances to achieve the 2023 target of measles and rubella elimination.52
Efforts were made to revive the coverage and surveillance through new and innovative ways including telephonic surveillance, virtual training and country-specific solutions were introduced to revitalize efforts.44,52 These efforts have resulted in a sharp recovery in immunization and surveillance performance, however an independent review commissioned to assess progress towards measles and rubella elimination by 2023 cautioned that the Region is off track to achieve the 2023 target and identified the need to revise the target date of measles and rubella elimination in consultation with global and regional experts, partners, and Member States.52
Way forward
Ensuring optimal implementation of key elimination strategies at accelerated pace remains a challenge, more so now with the COVID-19 pandemic and COVID-19 recovery phase that is likely to last for a couple of years. To accelerate progress and to sustain the gains, measles and rubella elimination activities should be optimally implemented through the primary health care (PHC) systems. Immunization programmes are an integral part of primary health care to achieve universal health coverage. Finally, the Region needs innovations to overcome vaccine delivery to areas with conflicts, migratory populations and specific populations with vaccine hesitancy. Measles and rubella elimination have their effect beyond immunization to overall child survival and development. Together we need to ensure that no child is left behind without the benefits of vaccination.
Contributors
Sunil Bahl and Sudhir Khanal were involved in the conceptualizing the paper and initial data analysis. Shahina Tabassum, Lucky Sangal, Jon Andrus, and Kumnuan Ungchusak were involved in the review of the draft manuscript, provide strategic comments and finalization of the manuscript.
Declaration of interests
SB, SK, LS are employees of WHO SEARO; ST, KU and JA are from South-East Asia Regional Verification Commission for Measles and Rubella Elimination. The views expressed in the submitted article are of the authors and not an official position of the institution to which they are affiliated. The authors were not precluded from accessing data in the study, and they accept responsibility to submit for publication. The authors declare no conflict of interest.
Acknowledgements
The authors would like to acknowledge the national immunization programs of ministries of health, in-country partners, the WHO and UNICEF country offices of the South-East Asia Region, UNICEF Regional Office for South-Asia.
SIAs generally are carried out using two target age ranges. An initial, nationwide catch-up SIA focuses on all children aged 9 months–14 years, with the goal of eliminating susceptibility to measles in the general population. Follow-up SIAs generally are conducted nationwide every 2–4 years and target children aged 9–59 months; their goal is to eliminate any measles-rubella susceptibility that has developed in recent birth cohorts and to protect children who did not respond to the first measles-rubella vaccination.
The WHO South-East Asia Region consists of Bangladesh, Bhutan, Democratic People’s Republic of Korea, India, Indonesia, Maldives, Myanmar, Nepal, Sri Lanka, Thailand, and Timor-Leste.
A suspected case of measles/rubella that has been investigated and discarded is termed a non-measles, nonrubella case if any of the following is true: An adequate specimen collected during the proper time period after the onset of rash has tested negative in a proficient laboratory; there is an epidemiological linkage to a laboratory-confirmed outbreak of another communicable disease that is not measles or rubella; another etiology has been confirmed, regardless of whether it meets the definition of an epidemiological linkage; and the case does not match the definition of a clinically compatible measles/rubella case.
References
- 1.Eilertson K.E., Fricks J., Ferrari M.J. Estimation and prediction for a mechanistic model of measles transmission using particle filtering and maximum likelihood estimation. Stat Med. 2019;38(21):4146–4158. doi: 10.1002/sim.8290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Measles vaccines: WHO position paper – April 2017 – note de synthèse de l’OMS sur les vaccins contre la rougeole – avril 2017. Wkly Epidemiol Rec Relevé Épidémiologique Hebd. 2017;92(17):205–227. https://apps.who.int/iris/handle/10665/255377 [cited 2022 Dec 14]; Available from: [PubMed] [Google Scholar]
- 3.Strebel P.M., Papania M.J., Fiebelkorn A.P., Halsey N.A. Vaccines. Sixth Ed. 2012. Measles vaccine; pp. 352–387.https://jhu.pure.elsevier.com/en/publications/measles-vaccine-4 [cited 2022 Dec 14]; Available from: [Google Scholar]
- 4.World Health Organization = Organisation mondiale de la Santé Rubella vaccines: WHO position paper – July 2020 – note de synthèse: position de l’OMS concernant les vaccins antirubéoleux. Wkly Epidemiol Rec Relevé Épidémiologique Hebd. 2020;95(27):306–324. https://apps.who.int/iris/handle/10665/332952 [cited 2022 Dec 14]; Available from: [Google Scholar]
- 5.Ozawa S., Clark S., Portnoy A., Grewal S., Brenzel L., Walker D.G. Return on investment from childhood immunization in low- and middle-income countries, 2011-20. Health Aff. 2016;35(2):199–207. doi: 10.1377/hlthaff.2015.1086. [DOI] [PubMed] [Google Scholar]
- 6.Sim S.Y., Watts E., Constenla D., Huang S., Brenzel L., Patenaude B.N. Costs of immunization programs for 10 vaccines in 94 low- and middle-income countries from 2011 to 2030. Value Health. 2021;24(1):70–77. doi: 10.1016/j.jval.2020.07.010. https://www.sciencedirect.com/science/article/pii/S109830152034393X [cited 2022 Dec 14]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Assembly 73. Global vaccine action plan: draft immunization vision and strategy: “Immunization agenda 2030”: report by the Director-General. World Health Organization; 2020. https://apps.who.int/iris/handle/10665/354893 [cited 2022 Dec 14]. Report No.: A73/7. Available from: [Google Scholar]
- 8.Transforming our world: the 2030 agenda for sustainable development | Department of Economic and Social Affairs. https://sdgs.un.org/2030agenda [cited 2022 Dec 14]. Available from:
- 9.Sustainable Development Goals. https://www.gavi.org/our-alliance/global-health-development/sustainable-development-goals [cited 2022 Dec 14]. Available from:
- 10.World Health Organization Regional Office for South-East Asia . WHO Regional Office for South-East Asia; 2013. SEA/RC66/R5 - Measles elimination and rubella/congential rubella syndrome control.https://apps.who.int/iris/handle/10665/128273 [cited 2022 Dec 14]. Report No.: SEA/RC66/R5. Available from: [Google Scholar]
- 11.World Health Organization . World Health Organization; 2013. Global vaccine action plan 2011-2020.https://apps.who.int/iris/handle/10665/78141 [cited 2022 Dec 14]. 148 pp. Available from: [Google Scholar]
- 12.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2022. Sustain Accelerate Innovate - South-East Asia: flagship priority programmes driving impact in countries for the health of billions.https://apps.who.int/iris/handle/10665/362030 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 13.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2020. Evaluation of implementation of regional flagship areas in the WHO South-East Asia Region 2014–2018.https://apps.who.int/iris/handle/10665/338722 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 14.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2019. Measles and rubella elimination by 2023.https://apps.who.int/iris/handle/10665/327923 [cited 2022 Dec 14]. Report No.: SEA/RC72/R3. Available from: [Google Scholar]
- 15.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2019. Strategic plan for measles and rubella elimination in WHO South-East Asia Region: 2020–2024.https://apps.who.int/iris/handle/10665/330356 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 16.WHO Immunization Data portal. https://immunizationdata.who.int/ [cited 2022 Dec 14]. Available from:
- 17.Progress toward measles elimination — South-East Asia region, 2003–2020 | MMWR. https://www.cdc.gov/mmwr/volumes/71/wr/mm7133a2.htm [cited 2022 Dec 14]. Available from: [DOI] [PMC free article] [PubMed]
- 18.Thapa A., Khanal S., Sharapov U., et al. Progress toward measles elimination - South-East Asia region, 2003-2013. MMWR Morb Mortal Wkly Rep. 2015;64(22):613–617. [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization Regional Office for South-East Asia Impact of the COVID-19 pandemic on immunization and surveillance of vaccine-preventable diseases in the WHO South-East Asia region. WHO South-East Asia J Public Health. 2021;10(Suppl 1):S1–S99. https://apps.who.int/iris/handle/10665/351482 ;10(3):1–3. [cited 2022 Dec 14]. Available from: [Google Scholar]
- 20.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2021. SEA region measles and rubella quarterly update Oct -Dec 2021.https://apps.who.int/iris/handle/10665/364212 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 21.World Health Organization Regional Office for South-East Asia SEA region measles and rubella quarterly update July -September 2022. 2022. https://apps.who.int/iris/handle/10665/364213 [cited 2022 Dec 14]. Available from:
- 22.World Health Organization = Organisation mondiale de la Santé Progress towards regional measles elimination – worldwide, 2000–2021 – progrès accomplis dans le monde en vue de l’élimination régionale de la rougeole, 2000-2021. Wkly Epidemiol Rec Relevé Épidémiologique Hebd. 2022;97(47):612–620. https://apps.who.int/iris/handle/10665/364733 [cited 2022 Dec 14]; Available from: [Google Scholar]
- 23.World Health Organization = Organisation mondiale de la Santé Progress towards regional measles elimination, worldwide, 2000–2014 = Progrès accomplis dans le monde en vue de l’élimination régionale de la rougeole, 2000-2014. Wkly Epidemiol Rec Relevé Épidémiologique Hebd. 2015;90(46):623–631. https://apps.who.int/iris/handle/10665/254526 [cited 2022 Dec 14]; Available from: [Google Scholar]
- 24.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2018. Midterm review of the “Strategic plan for measles elimination and rubella and congenital rubella syndrome control in the South-East Asia Region: 2014–2020”.https://apps.who.int/iris/handle/10665/279993 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 25.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2019. Joint national and international measles, rubella and congenital rubella syndrome programme review, Nepal 2019.https://apps.who.int/iris/handle/10665/332883 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 26.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2022. Review of progress and way forward on measles and rubella elimination activities in the WHO South-East Asia Region.https://apps.who.int/iris/handle/10665/352255 [cited 2022 Dec 14]. Report No.: SEA-Immun-135. Available from: [Google Scholar]
- 27.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2016. Guidelines on verification of measles elimination and rubella/congenital rubella syndrome control in the South-East Asia Region.https://apps.who.int/iris/handle/10665/255875 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 28.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2020. Framework for verification of measles and rubella elimination in the WHO South-East Asia Region.https://apps.who.int/iris/handle/10665/332737 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 29.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2017. Second Meeting of the South-East Asia Regional Verification Commission for Measles Elimination and Rubella/Congenital Rubella Syndrome Control: Colombo, Sri Lanka, 18–20 April 2017.https://apps.who.int/iris/handle/10665/277431 [cited 2022 Dec 14]. Report No.: SEA-IMMUN-113. Available from: [Google Scholar]
- 30.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2019. Fourth meeting of the WHO South-East Asia Regional Verification Commission for measles elimination and rubella/congenital rubella syndrome control Kathmandu, Nepal, 23–25 April 2019.https://apps.who.int/iris/handle/10665/331223 [cited 2022 Dec 14]. Report No.: SEA-Immun-130. Available from: [Google Scholar]
- 31.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2021. Sixth Meeting of the WHO South-East Asia Regional Verification Commission for measles and rubella.https://apps.who.int/iris/handle/10665/350119 [cited 2022 Dec 14]. Report No.: SEA-Immun-124. Available from: [Google Scholar]
- 32.Bahl S., Kumar R., Menabde N., et al. Polio-free certification and lessons learned--South-East Asia region, March 2014. MMWR Morb Mortal Wkly Rep. 2014;63(42):941–946. [PMC free article] [PubMed] [Google Scholar]
- 33.Kanu F.A., Yusuf N., Kassogue M., Ahmed B., Tohme R.A. Progress toward achieving and sustaining maternal and neonatal tetanus elimination - worldwide, 2000-2020. MMWR Morb Mortal Wkly Rep. 2022;71(11):406–411. doi: 10.15585/mmwr.mm7111a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2020. SEAR factsheet 2020: expanded programme on Immunization (EPI)https://apps.who.int/iris/handle/10665/336762 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 35.Meeting of the international task force for disease eradication, November 2015. https://www.who.int/publications-detail-redirect/WER9106 [cited 2022 Dec 14]. Available from: [PubMed]
- 36.World Health Organization Proceedings of the global technical consultation to assess the feasibility of measles eradication, 28-30 July 2010. J Infect Dis. 2011;204(Suppl 1):S4–S13. doi: 10.1093/infdis/jir100. [DOI] [PubMed] [Google Scholar]
- 37.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2017. Immunization achievements in South-East Asia: the platform for measles elimination.https://apps.who.int/iris/handle/10665/258759 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 38.Paudel K.P., Hampton L.M., Gurung S., et al. Adapting Nepal’s polio eradication programme. Bull World Health Organ. 2017;95(3):227–232. doi: 10.2471/BLT.16.173674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rodriguez D.C., Neel A.H., Mahendradhata Y., et al. The effects of polio eradication efforts on health systems: a cross-country analysis using the Develop-Distort Dilemma. Health Policy Plan. 2021;36(5):707–719. doi: 10.1093/heapol/czab044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2017. Lessons from the Big Six – closing the immunity gap for measles elimination and rubella/CRS control: New Delhi, India 31 January–02 February 2018.https://apps.who.int/iris/handle/10665/277429 [cited 2022 Dec 14]. Report No.: SEA-IMMUN-120. Available from: [Google Scholar]
- 41.Cintyamena U., Azizatunnisa’ L., Ahmad R.A., Mahendradhata Y. Scaling up public health interventions: case study of the polio immunization program in Indonesia. BMC Publ Health. 2021;21(1):614. doi: 10.1186/s12889-021-10647-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thacker N., Vashishtha V.M., Thacker D. Polio eradication in India: the lessons learned. Pediatrics. 2016;138(4) doi: 10.1542/peds.2016-0461. [DOI] [PubMed] [Google Scholar]
- 43.World Health Organization Regional Office for South-East Asia . WHO Regional Office for South-East Asia; 2015. Strategic plan for measles elimination and rubella and congenital rubella syndrome control in the South-East Asia Region, 2014-2020.https://apps.who.int/iris/handle/10665/205923 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 44.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2022. Thirteenth Meeting of the WHO South-East Asia Regional Immunization Technical Advisory Group: New Delhi, India, 17–19 August 2022.https://apps.who.int/iris/handle/10665/364534 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 45.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2016. First Meeting of the South-East Asia Regional Verification Commission for Measles Elimination and Rubella/Congenital Rubella Syndrome Control. 1–4 August 2016 WHO-SEARO, New Delhi, India.https://apps.who.int/iris/handle/10665/280122 [cited 2022 Dec 14]. Report No.: SEA-Immun-99. Available from: [Google Scholar]
- 46.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2018. Third Meeting of the South-East Asia Regional Verification Commission for Measles Elimination and Rubella/Congenital Rubella Syndrome Control: New Delhi, 31 July-2 August 2018.https://apps.who.int/iris/handle/10665/277455 [cited 2022 Dec 14]. Report No.: SEA-Immun-122. Available from: [Google Scholar]
- 47.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2020. Fifth meeting of the WHO South-East Asia regional verification commission for measles and rubella.https://apps.who.int/iris/handle/10665/338265 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 48.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2017. Surveillance guide for vaccine-preventable diseases in the WHO South-East Asia Region.https://apps.who.int/iris/handle/10665/277459 [cited 2022 Dec 14]. Available from: [Google Scholar]
- 49.The work of WHO in the South-East Asia region, report of the regional director, 1 January–31 December 2018. https://iris.who.int/handle/10665/327902%3famp%3border=desc%26query=The+Work+of+WHO+in+the+South-East+Asia+Region%2C+Report+of+the+Regional+Director%2C+1+January%E2%80%9331+December+2018%26rpp=10%26scope=%26sort_by=score%26search-result=true [cited 2022 Dec 14]. Available from:
- 50.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2021. Twelfth meeting of the WHO South-East Asia Regional Immunization Technical Advisory Group.https://iris.who.int/handle/10665/349583 License: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 51.World Health Organization Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2022. Seventh meeting of the WHO South-East Asia Regional Verification Commission for measles and rubella, Bali, Indonesia, 21–23 June 2022.https://apps.who.int/iris/handle/10665/360441 [cited 2022 Dec 14]. Report No.: SEA-Immun-136. Available from: [Google Scholar]
- 52.World Health Organization Regional Office for South-East Asia . 2021. WHO regional committee for South-East Asia: report of the seventy-fourth session, Nepal (virtual), 6-10 September 2021.https://apps.who.int/iris/handle/10665/355974 [cited 2022 Dec 14]. Report No.: SEA/RC74/21. Available from: [Google Scholar]