Summary
Health Emergency Risk Management (ERM) has become increasingly critical on the global stage, prompted by the escalating frequency and severity of natural disasters and disease outbreaks. This paper offers a comprehensive synthesis of the World Health Organization's (WHO) experiences in the South-East Asia Region during the period 2014–2023, shedding light on its efforts to manage health emergencies and enhance resilience. The South-East Asia Region's unique environmental and economic diversity exposes it to significant health risks, including emerging infectious diseases and their implications for development, particularly in low-income countries. Here we document the transition from reactive emergency responses to proactive preparedness, catalyzed by prioritizing ERM as one of the regional flagship priorities in 2014. Key components of this initiative included capacity-building, the establishment of the South-East Asia Regional Health Emergency Fund (SEARHEF), and the implementation of the International Health Regulations (IHR 2005). This synthesis highlights the region's achievements in event reporting, development of national actions plan, successful Early Warning, Alert, and Response System (EWARS) implementation, and improvements in core capacities under IHR (2005). It also underscores the challenges associated with cross-border data sharing and regional collaboration that could strengthen ERM and enhance readiness for effective synergistic response.
Keywords: South-East Asia Region, WHO, Disaster preparedness, Infectious diseases, Epidemic intelligence
Introduction
Health emergency risk management, in recent times, has been increasingly occupying the center stage of discussions around growth and development. Both resource-rich and resource-constrained countries are witnessing such a phenomenon alike. Worldwide natural disasters and emergencies occurring with increasing frequency over the last few decades, and their impact on health and development have conceivably served as the major driving force in this regard. Historically, since the beginning of farming by human civilizations, and more prominently with industrial revolution,1 the ecosystem of the planet earth has gradually been destabilized. Now there is a consensus that the resulting cumulative changes in weather and climate have negatively impacted upon global health through multiple direct and indirect pathways.2 Consequently, on one hand, while the indicators capturing exposure to such changes, and their impact at climate-health system interface are being critically examined for their relevance at global, regional and country level,3 on the other, interventions are being designed to remain prepared and mitigate the health risks as appropriate.
South-East Asia Region, due to its characteristic environmental, ecological and economic environment, merits due attention against this background. Notably, the region shoulders a great diversity of communicable diseases.4 For example, outbreaks of Nipah virus5 and artemisinin-resistant Plasmodium falciparum,6 both of which emerged in the region during the first decade of the current millennium received national, regional and international focus and new viral diseases such as severe acute respiratory syndrome and avian influenza A (caused by H5N1) attracted international investment. Noticeably, the burden of these emerging and re-emerging infectious diseases in countries of southeast Asia with lowest incomes comes with serious development implications. It is important to note that some of these diseases with pandemic potential adversely affect tourism industry, which serves as a major source of revenue generation in parts of southeast Asia. All these observations underline the importance of initiatives towards health emergency risk management and building resilience. However, coordination within the region and beyond has experienced some success7 and faced certain challenges.8
Prior to planned strategic collaboration within the region and beyond, the interventions were largely reactive in nature in response to regular occurrence of hazards such as flood, landslides, cyclone, and outbreaks of common diseases. Ebola outbreaks in African region in 2014–20159,10 and the concurrent enunciation of the Sendai Framework for Disaster Risk Reduction (2015–2030)11 resulted in policy level strategic re-thinking globally and in the Region–the new Health Emergencies Programme.12 We present here a synthesis of the lessons learnt by the World Health Organization (WHO) offices in the South East Asia Region. Health emergencies in this context encompass crises with public health consequences such as disease outbreaks, disasters, and humanitarian crises where the WHO plays an essential role in response and recovery. Eleven countries in South-East Asia–Bangladesh, Bhutan, Democratic Republic of Korea, India, Indonesia, Maldives, Myanmar, Nepal, Sri Lanka, Thailand and Timor-Leste (henceforth; ‘Region’)—constitute the Member States (MS) in this discussion. The WHO extended support towards health emergency risk management (ERM) in the Region with an overall goal to build core capacities for health security over the last two decades. In the process, while the International Health Regulations (IHR 2005),13 served as the driving force, initiatives in each of the MS were shaped by country specific leadership and priorities. Alongside the progress made, challenges faced in strengthening ERM policies and practices have also been highlighted, which could inform the way forward.
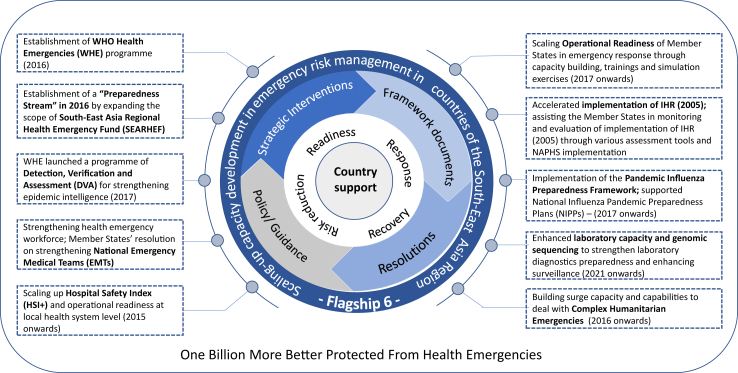
Considering the prevailing hazards, health risks, existing vulnerabilities, capacities and, increasing exposure of populations to a variety of emergency risks,14 in 2014, the WHO Regional Office for the South-East Asia along with the eleven Member States (MS) identified and prioritized eight regional flagship priority areas (Supplementary Figure S1). ‘Scaling-up capacity development in emergency risk management (ERM); as one of these priorities was termed as ‘Flagship 6’. Prioritization of the ERM as a regional flagship was preceded by the national level assessments of existing capacities in all MS in the Region from 2007 to 2012 using the WHO South-East Asia Region benchmarks for emergency preparedness and response framework with its standards and indicators.15 The benchmarks with a focus on legal, community, capacity building and early warning categories provided a comprehensive view of the emergency risk management in each country of the Region. It also provided a baseline for mapping of prevailing risks and hazards in each country.
Expanding the scope of an existing unique funding mechanism namely South-East Asia Regional Health Emergency Fund (SEARHEF)16 played a key role in the implementation. It is an operational fund established in 2008 as per the WHO Regional Committee decision by pooling a budget of US$ 1 million for each biennium from assessed contributions. The fund is designed to provide financial support for the first three months following a disaster that occurs in an affected country to support lifesaving health interventions and fill in critical gaps. Effective and efficient disbursement processes followed at the most critical initial 24 h after an emergency, which was an essential component of execution of emergency response.17 A Working Group constituted by the representatives from MS from the Region oversees the fund and decides on disbursement of it as a support to the affected country in immediate aftermath of an emergency.
Implementation process
Experiences gathered from the WHO supported initiatives have been presented in the following section under four subheadings namely a) Detection, Verification and Assessment, b) Early Warning Alert and Response System, c) Accelerated Implementation of International Health Regulation, and d) Good Practices from Countries in SEAR. Box 1 presents good practice-examples encompass health facility safety assessment, strengthening of emergency workforce through field epidemiology training, enhancement of laboratory capacity and development of mitigation strategy for influenza and other high threat pathogens. As can be identified from the domains enlisted above, the WHO-initiative in the SEAR under the aforementioned ‘flagship 6' covered different aspects starting with early detection of a threat and strengthening of laboratory and human capacity to moderation of impact of shock at health system interfaces.
Box 1. Good practices examples in scaling capacity development in emergency risk management in countries.
Health facility safety assessment
In 2019, the WHO Regional Office supported development of a mobile and web-enabled application for multi-hazards safety assessment and hospital preparedness. It was pilot-tested in four hub hospitals in Nepal, and later integrated into 25 hub hospital networks following capacity-building of the hospital staff. The app is adaptable in similar contexts in other countries of the Region. At the behest of the Ministry of Health and Population, Nepal; fire safety systems' functional assessment was conducted in selected health facilities including identification of gaps and needs on assessment of fire extinguishers and capacity to use them. These exercises in Nepal resulted in recommendations for improving building codes and fire safety systems’ monitoring in health facilities.
Health emergency workforce strengthening
The Field epidemiology training programme (FETPs) in the WHO South-East Asia Region, which was established in Thailand more than 40 years ago, as the first FETP outside of North America, with support from WHO and the U.S. Centres for Disease Control and Prevention (CDC). Subsequently, FETP was established in Indonesia in 1982, in India in 2001, and in Bangladesh in 2013. In 1996, the Regional FETP was established at India's National Institute of Communicable Diseases (now National Center for Disease Control), as the WHO collaborating Center for epidemiology and training. Among other countries, Nepal has formally started its FETP in 2023, where the first round of front-line course was completed in January 2023.
Enhanced laboratory capacity & genomic sequencing
Member States such as Bhutan, Nepal, Maldives, and Sri Lanka had limited molecular diagnostic laboratory capacity and were dependent on the WHO regional referral mechanisms for additional molecular testing, genomic sequencing, and virus isolation provided through India and Thailand. The COVID-19 pandemic triggered expansion of the laboratory systems and diagnostic capacities under compelling needs for early detection and monitoring of the virus, SARS-CoV-2. The testing capacity was expanded to the subnational level and by 2022 eight MS had developed in-country sequencing capacity of which six had established national networks for sequencing of SARS-CoV-2. This flagship also enabled setting up of an external quality assurance programme (EQAP) with the national laboratories from all MS during 2020–2021 for enhancing quality testing of SARS-CoV-2 infection. These national laboratories and over 1800 subnational laboratories from nine countries participated in the EQAP. A regional guidance to MS in the form of the “South-East Asia regional roadmap for diagnostic preparedness, integrated laboratory networking and genomic surveillance (2023–2027)” was provided.18
Pandemic influenza & other high threat pathohen mitigation strategy
The South-East Asia Region has successfully implemented the Global Influenza Strategy 2019–2030,19,20 the Pandemic Influenza Preparedness (PIP) Framework for sharing of influenza viruses and access to vaccines and other benefits.21 Member States were helped in developing, testing and updating national influenza pandemic preparedness plans (NIPPPs) using the WHO checklist for influenza preparedness planning (2005)22 and later through pandemic Influenza risk management.23,24 As a result, all eleven Member States have NIPPPs in implementation phase. There are presently ten influenza laboratories in the Region that have been recognized as national influenza centres within the Global Influenza Surveillance and Response System (GISRS) in eight countries.
Methods
We conducted a search for relevant articles, utilizing PubMed, WHO South-East Asia Journal of Public Health databases, and Google Scholar. The search terms used were “health emergencies,” “risk management,” “preparedness,” “response,” and “South-East Asia Region” for the period between 2000 and 2022. Additionally, we explored various publications from the WHO Regional Office of South-East Asia, including the published Regional Director's annual reports, reports and recommendations from the joint external evaluation of IHR, reports from relevant regional consultation meetings, and internal unpublished proceedings of the regional meetings. Only articles and documents written in English were considered for review. The final selection of references was based on their originality and relevance to the comprehensive scope of the present synthesis.
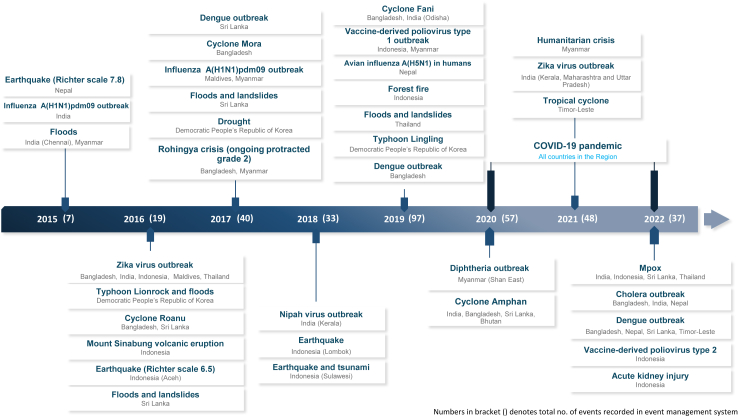
Detection, Verification & Assessment (Fig. 1)
Fig. 1.
Major public health events recorded in EMS in SEAR (1 January 2015–31 December 2022).
From 1st January 2014 to 31st December 2022, a total of 340 public health events in the Region were recorded in the event management system (EMS), and rapid risk assessments were conducted for 29 events. The number of events recorded per year gradually increased from 2 in 2014 to 97 in 2019 – an outcome of improved detection and reporting mechanisms because of sustained capacity building efforts on ERM in countries. The number of events reported decreased since 2020 due to prioritization around the COVID-19 pandemic. Among the 340 events in the Region since 2014, 47.8% were caused by infectious hazards, 35.4% were due to disasters, and 7.5% were outbreaks in animals.25
Epidemic intelligence from open sources (EIOS) was also introduced in the WHO-regional office in 2019 to further enhance the performance of event-based surveillance (EBS) for signal detection. Regional EBS screened over 1000 signals and detected over 150 events of public health significance in the year 2021 itself. From 2022 to early 2023, EIOS was introduced to the Ministry of Health in Bangladesh, Indonesia, Nepal, and Thailand as part of strengthening of EBS.
Early Warning, Alert & Response System (EWARS)
With the experience of implementing Early Warning, Alert and Response System (EWARS) in the aftermath of the Nepal earthquake in 2015, a mobile phone-based reporting system ‘EWARS in a box’ was developed. The ‘EWARS in a box’ was successfully implemented during Rohingya crisis emergency response operation in Cox's Bazar, Bangladesh in 2018. The evaluation of EWARS implementation, conducted in 2017, suggested that the system was a reliable one for rapid disease detection and response. Suggestions for improvement in data quality included increasing the frequency and quality of training, monitoring and feedback practices for users and the local team. Standardization of data collection forms and processes among the health centers operated by other health partners was recommended. Furthermore, as suggested by the evaluation, the integration of EWARS into the national health information systems is currently being explored.
Accelerated Implementation of IHR
The WHE has been assisting the Member States in monitoring and evaluation of implementation of IHR (2005) through self-assessment-based State Party Annual Reporting (SPAR); a mandatory tool and, voluntary tools such as Joint External Evaluation (JEE). Since 2016, there has been 100% reporting compliance to SPAR by all eleven Member States. In 2018, South-East Asia regional average core capacity was 56% (Global 61%), which further improved in 2022 to 64% (Global 64%). The highest average score was observed for surveillance followed by risk communication and health emergency management; augmented during COVID-19 response. The lowest score was reported for policies for chemical events management, legal and normative instruments to manage emergencies, and capacities to address food safety and radiation emergencies.
Seven Members developed, budgeted, and implemented the national action plans for health security (NAPHS) while Bangladesh NAPHS awaits high-level endorsement. The Universal Health and Preparedness Review (UHPR) is a recent and innovative approach in strengthening the national capacities for emergency preparedness and Thailand became one of the first countries to pilot this innovative approach globally in April 2022.
Good practice from countries in Southeast Asia
Box 1 presents select examples from countries in Southeast Asia. Rapid situation and response assessment with development of innovative intervention, strengthening of field epidemiology practices and diagnostic capacities across the region and enhancement of strategic capacity were prime considerations for selecting these examples. Fig. 2 depicts a comprehensive picture of the elements covered under ‘Flagship 6’.
Fig. 2.
Implementation elements under ‘Flagship 6’.
Discussion
Social, political and economic developments over the past few decades have resulted in substantial health gains in some countries in SEAR and smaller changes in others. The geology of the region, making it highly susceptible to earthquakes and tsunamis along with seasonal typhoons and floods increases health risks of the population from natural disasters and long-term effects of climate change, which encompass both non-communicable and communicable diseases. In such a situation, cooperation in the region around disaster preparedness and surveillance of and health system response to disease outbreaks offer obvious advantages as a public health strategy.26 In this context, the present synthesis provides evidence of a range of effective interventions implemented regionally pertaining to emergency preparedness and mitigation of impact of emerging and re-emerging diseases.
Member States, as described above, were supported by the WHO-Regional Office for SEAR through various regional level policies, technical and operational guidance, and frameworks with flexibility to adapt to country-contexts. High-level political commitments and increased investments by the Member States reflected through various resolutions also provided major strategic drives in strengthening the ERM in the Region. Importantly the WHE program leveraged the capacity building for health security under the IHR (2005) and improved capacities at national levels for epidemiological intelligence, laboratory diagnostics and capabilities for early detections and control of high-threat pathogens with advanced technological skills and competencies built over the last decade. An external evaluation conducted in July 2020 to assess the relevance, effectiveness, and efficiency of WHO's role in the progress and impact on the regional flagship areas during 2014–201827 underlined the same.
However, inadequate capacities for risk identification, community, and laboratory-based surveillance for timely notification under the IHR (2005) remained a weakness at primary healthcare levels. This weakness got accentuated and exposed during the COVID-19 pandemic with inability of WHO offices to come up with timely guidance on calibrating public health and social measures. A critical exploration of pandemic preparedness and responses at the global level had observations in consonance.26 It maintained that the global response was debilitated by shortage of timely action and investment. It has also been highlighted that overreliance on global security and hyper-focusing only on infectious disease response can distort the overall reality, which merits investment in early warning system and diagnostics to be concretely tied with26 strengthening of in-country health systems under universal health coverage (UHC).
Importantly, expanding the scope of an existing unique funding mechanism of WHO-SEAR served as an important mover of ‘Flagship 6’. However, in due course it was realized that the regional resource mobilization strategy should have been further improved through a comprehensive partner and donor landscaping; with periodic fund-mobilization meetings with the existing and potential partners.
Finally, non-availability of disaggregated data (age group, gender, disability etc) at country level on the impact of disaster and emergencies across populations and lack of sharing of public health data in the region appeared to be two key challenges requiring immediate attention. While public private-partnership and active engagement at the community level remain paramount in this regard in a country, the region requires exploring the range of factors affecting transfer, exchange and use of public health data and expertise across borders. Currently imbalances exist between national health systems and capacities that may affect cross-border data and information sharing. Establishment of good practice in the region would therefore require significant involvement of an independent third-party brokering organization or office, which will redress imbalances between country partners at different levels in the data sharing process, create meaningful communication channels and make the most of the shared information28 towards common public health good.
In conclusion, the key milestones achieved on strengthening ERM during the last decade facilitated Member States in shifting their focus from merely ‘investing into emergency response’ to ‘health emergency risk management’ through policy and strategic actions. The prioritized focus on health ERM adopted under the ‘flagship 6’ enabled MS in the Region to accelerate building IHR capacities on health risk assessment, epidemic and laboratory-based intelligence, and risk-informed readiness for effective emergency response.
Contributors
Singh PK, Salvador EC and Buddha N conceptualized and supervised the article, Bhola A and Sinha SK. reviewed the referenced literature under the agreed methods, synthesized the information while integrating the evidence into the first draft. Sinha SK. developed the infographics. Kato M, Wijesinghe PR, Samuel R, Naidoo D, Singh SK and Perera WLS. provided inputs over progress relevant to their subject areas and all co-authors reviewed a series of different versions of the draft manuscript. Bhola A and Sinha SK subsequently refined the revised versions to pre-final manuscript thereafter Salvador EC and Singh PK approved the manuscript for submission.
Declaration of interests
The authors are employed with WHO SEARO except AB and SS who were Ex-Consultants with WHO SEARO. The views expressed in the submitted article are of the authors and not an official position of the institution to which they are affiliated. The authors were not precluded from accessing data in the study, and they accept responsibility to submit for publication. The authors declare no conflict of interest.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lansea.2023.100304.
Appendix A. Supplementary data
Supplementary Figure S1.

References
- 1.Rossati A. Global warming and its health impact. Int J Occup Environ Med. 2017;8:7–20. doi: 10.15171/ijoem.2017.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haines A., Kovats R.S., Campbell-Lendrum D., Corvalan C. Climate change and human health: impacts, vulnerability and public health. Public Health. 2006;120:585–596. doi: 10.1016/j.puhe.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 3.Di Napoli C., McGushin A., Romanello M., et al. Tracking the impacts of climate change on human health via indicators: lessons from the Lancet countdown. BMC Public Health. 2022;22:663. doi: 10.1186/s12889-022-13055-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coker R.J., Hunter B.M., Rudge J.W., Liverani M., Hanvoravongachi P. Emerging infectious diseases in southeast Asia: regional challenges to control. Lancet. 2011;377:599–609. doi: 10.1016/s0140-6736(10)62004-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lo M.K., Rota P.A. The emergence of Nipah virus, a highly pathogenic paramyxovirus. J Clin Virol. 2008;43:396–400. doi: 10.1016/j.jcv.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Dondrop A.M., Yeung S., White L., et al. Artemisinin resistance: current status and scenarios for containment. Nat Rev Microbiol. 2010;8:272–280. doi: 10.1038/nrmicro2331. [DOI] [PubMed] [Google Scholar]
- 7.Lamy M., Phua K.H. Southeast Asian cooperation in health: a comparative perspective on regional health governance in ASEAN and the EU. Asia Eur J. 2012;10:233–250. doi: 10.1007/s10308-012-0335-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fidler D.P. Negotiating equitable access to influenza vaccines; global health diplomacy and the controversies surrounding avian influenza H5N1 and pandemic influenza H1N1. PLoS Med. 2010;7 doi: 10.1371/journal.pmed.1000247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ritchie H., Rosado P., Roser M. 2022. "Natural disasters".https://ourworldindata.org/natural-disasters OurWorldInData.org. Available at: [Online Resource] [Google Scholar]
- 10.Formetta G., Feyen L. Empirical evidence of declining global vulnerability to climate-related hazards. Glob Environ Change. 2019;57 doi: 10.1016/j.gloenvcha.2019.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sendai framework for disaster risk reduction 2015–2030. United Nations Office for Disaster Risk Reduction; Geneva: 2015. https://www.preventionweb.net/sendai-framework [Google Scholar]
- 12.Reform of WHO work in health emergency management. https://apps.who.int/iris/bitstream/handle/10665/252688/A69_30-en.pdf?sequence=1&isAllowed=y A69/30.
- 13.International health regulations (2005) 3rd ed. World Health Organization; Geneva: 2016. http://www.who.int/ihr/publications/9789241580496/en/ [Google Scholar]
- 14.SIMM, G Disaster response in Southeast Asia: the ASEAN agreement on disaster response and emergency management. Asian J Int Law. 2018;8(1):116–142. doi: 10.1017/S2044251316000205. [DOI] [Google Scholar]
- 15.World Health Organization, Regional Office for South-East Asia . World Health Organization. Regional Office for South-East Asia; 2021. Towards a safer future: learnings from a decade of public health emergencies in the South-East Asia Region.https://apps.who.int/iris/handle/10665/344735 [Google Scholar]
- 16.Regional Office for South-East Asia, World Health Organization . WHO Regional Office for South-East Asia; 2016. SEA/RC69/R6–expanding the scope of the South-East Asia regional health emergency fund (SEARHEF)https://apps.who.int/iris/handle/10665/250288 [Google Scholar]
- 17.WHO South-East Asia regional health emergency fund providing critical life-saving support. https://www.who.int/southeastasia/news/feature-stories/detail/WHO-South-East-Asia-Regional-Health-Emergency-Fund-providing-critical-life-saving-support Available at:
- 18.World Health Organization . World Health Organization; Geneva: 2019. Global influenza strategy 2019-2030.https://apps.who.int/iris/handle/10665/311184 Available at: [Google Scholar]
- 19.World Health Organization . World Health Organization; Geneva: 2011. Pandemic influenza preparedness framework for the sharing of influenza viruses and access to vaccines and other benefits.http://www.who.int/entity/influenza/resources/pip_framework/en/index.html Available at: [Google Scholar]
- 20.World Health Organization . World Health Organization; Geneva: 2018. Nipah research and development (R & D) roadmap.https://www.who.int/blueprint/priority-diseases/key-action/Nipah_Draft_Roadmap_publiccomment_MAY2018.pdf?ua=1 Available at: [Google Scholar]
- 21.Global Task Force on Cholera Control . World Health Organization; Geneva: 2017. Ending cholera: a global roadmap to 2030.https://www.who.int/cholera/publications/global-roadmap.pdf Available at: [Google Scholar]
- 22.World Health Organization . 2017. Pandemic Influenza risk management.https://apps.who.int/iris/handle/10665/259893 Geneva. Available at: [Google Scholar]
- 23.World Health Organization . World Health Organization; Geneva: 2018. Pandemic influenza preparedness (PIP) framework: partnership contribution (PC) preparedness high-level implementation plan II 2018—2023.https://www.who.int/publications/i/item/pip-pc-preparedness-high-level-implementation-plan-ii-2018-2023 Available at: [Google Scholar]
- 24.World Health Organization . 2005. WHO checklist for influenza pandemic preparedness planning.https://www.who.int/influenza/resources/documents/FluCheck6web.pdf?ua=1 Geneva. Available at: [Google Scholar]
- 25.Wijsinghe P.R., Ofrin R.H., Bhola A.K., Inbanathan F.Y., Bezbaruah S. Pandemic influenza preparedness in the WHO South-East Asia Region: a model for planning regional preparedness for other priority high-threat pathogens. WHO South-East Asia. J Public Health. 2020;9(1):43–49. doi: 10.4103/2224-3151.282995. https://apps.who.int/iris/handle/10665/331830 Available at: [DOI] [PubMed] [Google Scholar]
- 26.Chongsuvivatwong V., Phua K.H., Yap M.T., et al. Health and health-care systems in southeast Asia: diversity and transitions. Lancet. 2011;377:429–437. doi: 10.1016/S0140-6736(10)61507-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lal A.L., Chattu V.K., Erondu N.A., et al. Pandemic preparedness and response: exploring the role of universal health coverage within the global health security architecture. Lancet Glob Health. 2022;10:e1675–e1683. doi: 10.1016/S2214-109X(22)00341-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liverani M., Teng S., Le M.S., Coker R. Sharing public health data and information across borders: lessons from southeast Asia. Glob Health. 2018;14:94. doi: 10.1186/s12992-018-0415-0. [DOI] [PMC free article] [PubMed] [Google Scholar]