Noncommunicable diseases (NCDs) caused nearly two thirds of all deaths in countries of World Health Organization (WHO) South-East Asia Region (SE Asia Region) in 2021, with half of these deaths in the age group 30–69 years.1 Cardiovascular diseases (CVDs) (3.9 million), account for most NCD deaths, followed by cancers, chronic respiratory diseases and diabetes. Against the backdrop of the unfinished agenda on maternal and child health, and the re-emerging threat of communicable diseases, countries have taken up NCDs as a priority public health agenda. High level political advocacy accompanied by WHO guidance and tools including the NCD surveillance dashboard, have helped gather momentum and increase accountability for NCDs.2 The past decade has seen countries put in place policies, plans and programmes to reduce risk and manage NCDs.3 By 2021, ten countries had integrated national NCD action plans, committed to the SDG 3.4 target of 33.3% relative reduction of the probability of premature NCD mortality by 2030, and set time bound targets on NCD risk factors and management.2
While NCDs have received priority in terms of the political agenda and policies, progress in risk factor reduction and management of NCDs, except for tobacco, remains variable.3 Against the regional target of a 30% reduction in the age-standardized prevalence of tobacco use (smoked and smokeless) by 2025 relative to 2010, the region witnessed a declining trend and is on track to achieve an average reduction of almost 32% by 2025.4 More focus on reducing smokeless tobacco use and tackling new and emerging tobacco and nicotine products is needed.5 Alcohol consumption reduction and preventing unhealthy diets have seen lesser success.3 The relatively new focus on harms of unhealthy diets and alcohol, lack of strong political commitment of governments to overcome commercial influence to reduce the availability and the demand through evidence based fiscal and regulatory measures and the challenges to harness multi-sectoral support for recommended interventions, have limited the progress. Further efforts at targeted advocacy and evidence generation to foster multi-sectoral coordination, and reducing policy and enforcement gaps and addressing social and commercial determinants are critical.
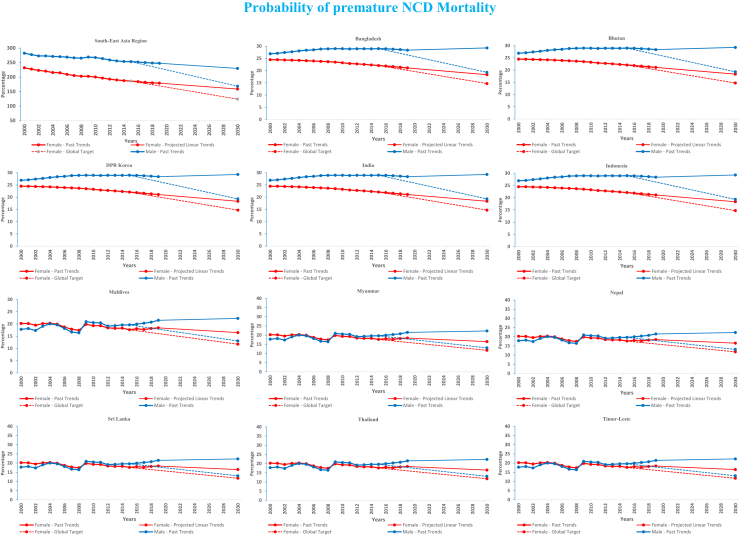
At the current rate of decline despite a small reduction of the projected premature mortality trends, the Region, except two countries is not expected to achieve the 2030 SDG 3.4 target (Fig. 1).3 Unless rectified, the substantial country health system gaps will cause further delays in reducing premature mortality.2 NCD management through primary health care (PHC) is the only way forward for countries with their limited health budgets and healthcare systems. While the WHO HEARTS technical package guides the scale up of hypertension and diabetes diagnosis and management,6 PHC systems that were designed for infectious diseases have not adequately adjusted to the increasing need for chronic care. They are not sufficiently equipped with the required guidelines, medicines, technology, skilled workforce and health information systems have hampered efforts to effectively cover and monitor NCD services.7
Fig. 1.
Probability of premature NCD mortality.
Source: SEARO NCD Dashboard (who.int).
The recent WHO country capacity survey reported that just 60% of countries in the Region reported availability of treatment guidelines for the 4 major NCDs-CVD, diabetes, cancer and chronic respiratory diseases.7 While 90% of countries reported availability of common medications in over 50% of institutions, several essential medicines, including sulphonylurea, insulin and steroid inhalers were limited.7 Just over 50% of countries reported general availability of essential technologies for early detection, diagnosis, and monitoring of NCDs in PHCs. The treatment gap and inadequate control among those on treatment are significant. The gaps, early detection and management of NCDs, and linkages with continued care need to be urgently addressed. A better skilled and appropriately trained workforce is vital to provide quality NCD services.7 Supplies/logistics must be reorganized to ensure essential medicines and diagnostics. Linking frontline NCD services to distant communities unable to access care is also important.
There are several successful country models to scale up and replicate. Bhutan’s Service with Care and Compassion Initiative screens everyone visiting health facilities for NCDs and covers home care, refill of medicines, reminder & follow-up for treatment & medication, referral and real-time monitoring.8 In 2018, India and Thailand accelerated hypertension control initiatives.9,10 By 2022, the India Hypertension Control Initiative had registered over 6 million people under treatment, with the quarterly cohort blood pressure control rates showing significant improvement. With Thailand’s initiative, approximately 50,000–70,000 patients are diagnosed with hypertension monthly, with improved blood pressure control rates at clinic level.10
The NCD implementation roadmap for accelerating prevention and control of NCDs in South-East Asia (2022–2030) aims to prioritize and accelerate the most impactful interventions, including digital solutions.11 Based on the roadmap, countries will focus on programmatic interventions. The SEAHEARTS initiative is a platform bringing together tobacco control, salt reduction, and elimination of trans-fatty acids along with improved hypertension and diabetes treatment coverage and control through PHC, supported by WHO and partners. Countries have also recently committed to placing one billion hypertensive and diabetes patients on standard care by 2025, which includes India’s commitment of 75 million people. Despite the challenges, this increased focus on NCD prevention and management will no doubt accelerate efforts to reach SDG 3.4 to save lives and ensure health for all in the region.
Contributors
AS, CV, NG, BG, PJ: conceptualization, literature search, figure, study design, data collection, analysis, interpretation and writing.
RA, SB, AB, SB, JK, PS, FAD, LD, NG, HK, FH, DJ, AAK, RL, PL, AMML, VM, MAF, ON, BN, CSP, PS, KT, CW, RP: review, data and information verification and editing.
Declaration of interests
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
The following authors are employees of WHO.
Angela de Silva; Cherian Varghese; Sadhana Bhagwat; Andrea Bruni; Sushera Bunleusin; Jagdish Kaur; Padmal de Silva; Farzana Akter Dorin; Bishnu Giri; Nalika Gunawardena; Fathimath Hudha; Dinesh Jeyakumaran; Pradeep Joshi; Ravivarman Lakshmanasamy; Pema Lethro; Aye Moe Moe Lwin; Virginie Mallawarachchi; Olivia Nieveras; Praveen Sinha; Razia Pendse.
References
- 1.World Health Organization . WHO South-East Asia Region; 2021. Noncommunicable diseases.https://www.who.int/southeastasia/health-topics/noncommunicable-diseases [Google Scholar]
- 2.World Health Organization . 2022. NCD dashboard. WHO South-East Asia Region.https://searncddashboard.searo.who.int/NCDMortality [Google Scholar]
- 3.World Health Organization . WHO; 2022. Noncommunicable diseases: progress monitor 2022.https://apps.who.int/iris/handle/10665/353048 [Google Scholar]
- 4.World Health Organization global report on trends in prevalence of tobacco use 2000-2025. 4th ed. World Health Organization; Geneva: 2021. [Google Scholar]
- 5.World Health Organization . WHO South-East Asia Region; 2022. Tobacco control in South-East Asia Region.https://www.who.int/southeastasia/health-topics/tobacco/tobacco-control-in-the-south-east-asia-region [Google Scholar]
- 6.World Health Organization . World Health Organization; Geneva: 2020. HEARTS technical package for cardiovascular disease management in primary health care: risk based CVD management. [Google Scholar]
- 7.World Health Organization . World Health Organization; Geneva: 2023. Assessing national capacity for the prevention and control of noncommunicable diseases: report of the 2021 global survey. [Google Scholar]
- 8.World Health Organization, Bhutan Evolving a people-centred approach to noncommunicable disease (NCD) services in Bhutan. https://www.who.int/southeastasia/news/feature-stories/detail/Evolving-a-people-centred-approach-to-noncommunicable-disease-NCD-services-in-Bhutan
- 9.ICMR. Ministry of Health and Family Welfare. Government of India. World Health Organization, India India hypertension control initiative 2021 progress report. https://www.who.int/southeastasia/internal-publications-detail/india-hypertension-control-initiative-(ihci)-2021
- 10.World Health Organization 2021. https://www.who.int/thailand/activities/reducing-cardiovascular-disease
- 11.World Health Organization . WHO SEARO; 2023. Implementation roadmap for accelerating the prevention and control of noncommunicable diseases in South-East Asia 2022–2030. [Google Scholar]