Abstract
Introduction
Mandibular abnormalities caused by ameloblastoma present significant surgical and reconstructive difficulties. This study investigates double barrel fibular bone graft to correct these abnormalities and improve mandibular function and appearance.
Case presentation
A 28-year-old male presented with a mandibular lump and facial asymmetry. The radiographic and histologic examination detected was subsequently diagnosed as ameloblastoma. After undergoing a hemi mandibulectomy procedure, a free vascularized fibular bone graft was harvested from the patient's left leg and transplanted to reconstruct the mandibular angle. The evaluation of the patient's functional outcomes was assessed utilising the University of Washington Quality of Life (UW-QOL) questionnaire. The patient UW – QOL Score has increased 62.5 pre-treatment to 93.75 post-treatment.
Discussion
The suggested strategy to treating aggressive ameloblastomas is radical surgery, involving the use of wide resection and following bone reconstruction. Vascularized grafts, including the double-barrel fibular bone graft, are usually preferred in relation to mandibular defect reconstruction for their ability to offer improved stability, height, and thickness, which enhances functional results. In contrast to conventional approaches, our case did not show any signs of facial deformities or bone resorption. The utilization of the vascularized fibular bone graft proved to be a valuable option for early rehabilitation in patients with mandibular continuity defects, offering promising outcomes in terms of patient well-being and quality of life. This final result provides proof supporting the potential of this technique for managing mandibular defects.
Conclusion
Double-barrel fibular bone grafts and dental rehabilitation can restore mandibular continuity defect from ameloblastoma.
Keywords: Mandibular continuity defects, Ameloblastoma, Double barrel fibular bone graft, Reconstructive plates, Case report
Highlights
-
•
Double-barrel vascularized fibular graft address mandibular defects in ameloblastoma patients.
-
•
Reconstruction plates improve mandibular stability and force distribution.
-
•
Double-barrel fibular graft helps maintain bone structure and improves oral functions.
1. Introduction
The mandible plays a crucial role in various vital functions, including airway protection, support for the tongue, articulation, speech, and facial aesthetics [1]. Ameloblastomas, although rare, can lead to severe impairments in these functions and significantly impact the quality of life of affected individuals. The treatment of mandibular continuity defects caused by ameloblastoma presents a difficult challenge that requires the use of a variety of surgical and restorative techniques. These tumours require extensive surgical intervention, which involves the complete removal of the tumour and substantial amounts of nearby bone tissue, leading to the appearance of mandibular defects. Several treatments are required to solve these defects, which cover non-vascularized and vascularized bone grafts as well as free flaps [2].
The use of a double-barrel fibular bone graft has become an effective method for treating certain mandibular defects. This technique utilises a vascularized fibular bone graft shaped into a double-barrel arrangement to treat mandibular continuity defects. This technique has been shown to effectively improve both the functional and aesthetic aspects of the mandible [[2], [3], [4]]. Additionally, the addition of dental prostheses improves both the aesthetic and functional aspects of the orofacial area [5]. This case report aims to evaluate the efficacy of double-barrel fibular bone grafts in a patient who received hemi-mandibulectomy for ameloblastoma treatment. The writing of this case report complied with the SCARE criteria [6].
2. Case presentation
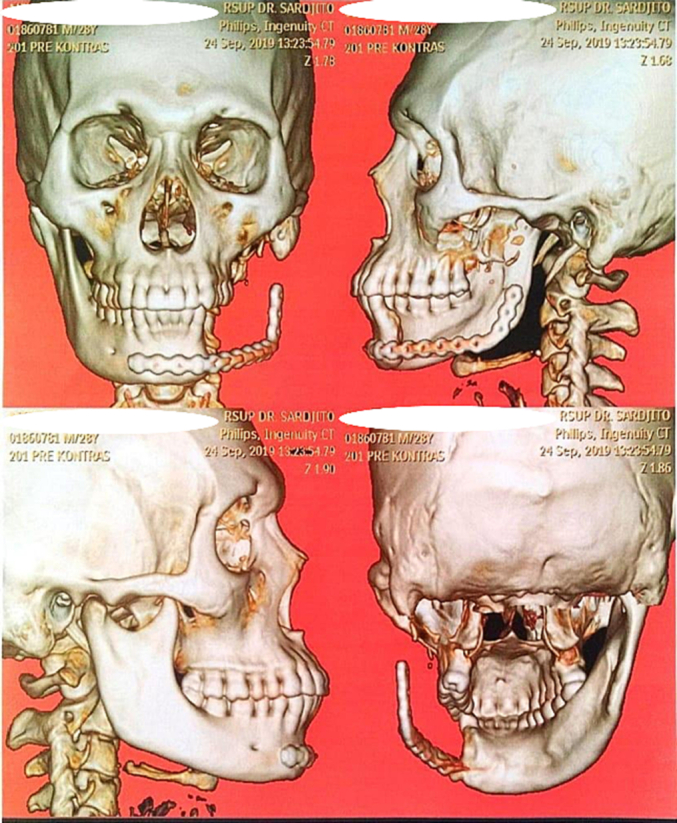
A male patient, aged 28, was observed to have a non-painful lump on the right cheek upon arrival at our medical facility. The symptoms had been present for approximately 1.5 years, leading to difficulties in speech and mastication. The patient reported no history of trauma or significant medical conditions. Upon physical examination, a palpable, firm mass was noted in the left mandibular angle, causing deviation of the jaw to the affected side. Intraoral examination revealed a non-tender, bony hard swelling with expansion of the buccal cortex. There was no evidence of ulceration or bleeding from the lesion. The results of plain radiography and a three-dimensional CT scan of the mandible (Fig. 1) revealed the presence of continuity defects that extended from the midline of the mandible to the condyle. Following these imaging studies, a biopsy examination was conducted, which confirmed the diagnosis as follicular and plexiform multicystic ameloblastoma (Fig. 1).
Fig. 1.
Pre-operative clinical pictures of ventral and lateral aspect of patient's mandible, observed to have a non-painful lump on the right cheek (A and B). Plain radiography of the mandible and three dimensional CT-Scan of the mandible that shows multicystic, soap-bubble like lesions, well-demarcated borders and no matrix calcification (C and D). Histopathological biopsy examination shows follicular and plexiform multicystic ameloblastoma (E).
The patient received a hemi-mandibulectomy procedure by the department of Oral and Maxillofacial Surgery, the condyle was disarticulated from the joint while preserving the articular disc, and a reconstruction plate with Orthognathic Supra Advancement (OSA) system was used to maintain the structure (Fig. 2). Subsequently, A one-year evaluation was carried out to confirm an absence of both infection and tumor recurrence. One year after the Hemimandibulectomy, the patient returned, complaining of facial asymmetry in the left angle of the mandible and sought consult with the Orthopedic Department for further management of the bone defect.
Fig. 2.
3D CT scan after the patient received a hemi-mandibulectomy procedure and followed by placement of Orthognathic Supra Advancement (OSA).
In order to address the issue, we conducted a collaborative procedure involving the orthopedic surgery and oral surgery departments to reconstruct the mandible using a fibular flap. The specialized orthopedic and oral surgeons spent 6 h performing the harvesting of the double vascularized fibular flap and the mandibular reconstruction. A 10 cm long vascularized fibular bone graft was harvested from the patient's left leg using a double-barrel technique (Fig. 3). The fibula was dissected from distal to proximal, with care taken to preserve a cuff of the flexor hallucis longus and tibialis posterior muscles located between the peroneal vessels and the posterior medial aspect of the fibula (Fig. 3). Subsequently, after the donor graft (double barrel vascularized fibular bone graft) was harvested, measurements of the distance between the defects (proximal to distal) were taken to predict the point of the mandibular angulus. Following the completion of these measurements, a transverse osteotomy was executed in the anterolateral facet of the fibular shaft, situated just beneath the entry point of the nutrient artery, resulting in the formation of a double-barrel construct, preserving the periosteal circulation of the bone. A bony bridge was preserved during the intervention, and the two segments of the fibula were stabilized using a reconstruction plate system (Fig. 4).
Fig. 3.
Schematic diagram of fibular osteotomy for harvesting double barrel fibular bone graft (A). The fibula that was dissected by the lateral approach, superior and inferior osteotomies then performed, keeping the medial aspect of the peroneal vessels (B and C). After isolation of the fibula on the peroneal vessel, the fibula may be removed. The length of each fibular struts measured by recipient bone defect and then cut by oscillating saw (D). The harvested free vascularized fibular graft with showing nutrient artery for its vascularization (E).
Fig. 4.
Fibular bone graft positioned in mandible and stabilized using a reconstruction plate system (A). Process of revascularization microvascular anastomosis of the peroneal artery with facial artery (B).
Following this, the fibular free bone graft was relocated to the target area. The graft was positioned to form the angulus of the mandible and was stabilized using a reconstruction plate system. Revascularization of the free vascularized fibular bone graft was accomplished through microvascular anastomosis. Specifically, the peroneal artery was anastomosed with the facial artery at the segmental defect site of the mandible. The masseter muscle was sutured to the angle of the reconstruction plate, securing the distal end into the glenoid fossa (Fig. 4). In the concluding step, dental implants were surgically placed in the distal region of the fibular arch and anterior maxilla to provide support for the dental prosthesis.
In addition to assessing the physical restoration of the mandible, we also evaluated the patient's postoperative quality of life using the University of Washington – Quality of Life (UW – QOL) questionnaire. The tool stated in this statement is an accepted instrument used to evaluate health-related quality of life in patients who are undergoing surgery for head and neck oncology, as well as those who are in the postoperative rehabilitation phase [7].
The patient's UW-QOL score showed significant enhancement from the preoperative assessment to the one-year follow-up, signifying a successful recovery not only in anatomical elements but also in functional and psychosocial fields [7]. The score increased from 62.5 pre-treatment to 93.75 post-treatment, indicating a significant improvement in the patient's quality of life (Table 1). This measure highlights the efficacy of the grafting method in facilitating patients' restoration of normal function and overall well-being. During the radiological examination, it was observed that the graft was appropriately positioned and no signs of graft resorption were detected (Fig. 5).
Table 1.
University of Washington – Quality of Life (UW – QOL) questionnaire. The score increased from 62.5 pre-treatment to 93.75 post-treatment, indicating a significant improvement in the patient's quality of life.
| UW – QOL scores | ||
|---|---|---|
| Pre | Post | |
| Pain | 75 | 100 |
| Appearance | 25 | 75 |
| Activity | 50 | 75 |
| Recreation | 50 | 100 |
| Swallowing | 75 | 100 |
| Chewing | 50 | 100 |
| Speech | 75 | 100 |
| Shoulder | 100 | 100 |
| Taste | 75 | 100 |
| Saliva | 75 | 100 |
| Mood | 50 | 100 |
| Anxiety | 50 | 75 |
| Overall mean | 62.5 | 93.75 |
Fig. 5.

Clinical evaluation after one year follow-up (A and B). Plain Radiology of the mandible after one year follow-up post operatively (C).
3. Discussion
The presence of mandibular bone defects poses a complex and challenging clinical dilemma, requiring the integration of various surgical and reconstructive techniques [8]. Using double-barrel fibular bone graft is considered a noteworthy surgical alternative for addressing mandibular continuity defects [[2], [3], [4]]. Subsequently, the method has gained widespread usage owing to its satisfactory dimensions, density, and favourable vascularization of the transplant. The utilization of a double-barrel configuration serves to augment the stability of the graft and mitigate the risk of fibular shaft collapse or fracture. Furthermore, maintaining the structural integrity of the bone placed between the two segments of the fibula is essential for ensuring proper occlusion, speech, and swallowing functions after the reconstruction process [2,3,5].
A key aspect of postoperative rehabilitation is restoring function and appearance after mandibular reconstruction. A double-barrel vascularized fibular bone graft from the patient's left leg proved in our case study had achieved a significant part achieving this goal. It proved successful in correcting the mandible's angle, a crucial element in oral functionality and aesthetics, in alongside correcting the mandibular continuity defect [9]. The graft's stability and effective integration were confirmed by radiological and clinical assessments done a year after surgery, showing the possibility of this approach for early rehabilitation in patients with mandibular continuity defects.
4. Conclusion
In conclusion, our case study highlights the valuable role of double-barrel fibular bone grafts in reconstructing the mandible post-ameloblastoma excision. The graft showcased impressive outcomes, with no evidence of resorption, significant functional improvements, and enhanced aesthetics a year after surgery. This approach holds promise as a swift rehabilitation option for mandibular continuity defects. Ongoing research is essential to validate these findings and further refine surgical techniques, ensuring the mitigation of potential complications at the donor site. Additional research is required to support these findings and improve surgical techniques in order to reduce complications related to the donor site.
Consent
We were able to obtain written informed consent from the patient (or their guardian or next of kin) for the publication of this case report and its accompanying images.
The head of our institution are also taking responsible that exhaustive attempts have been made to contact the family and that the paper has been sufficiently anonymised not to cause harm to the patient or their family. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
This case report doesn't require ethical approval based on our research ethics committee's institution. Our institution's ethics committee confirmed that this report aligns with routine clinical practice and doesn't involve experimental interventions or additional data collection.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author contribution
Conceptualization: M.M., M.B.L., M.R.Z., A.A.N.T., M.Y.Y.
Data Curation: M.M., M.B.L., M.R.Z. A.A.N.T.
Formal Analysis: M.M., M.B.L., M.R.Z., A.A.N.T., M.Y.Y.
Funding acquisition: Not applicable.
Investigation: M.M., M.B.L., M.R.Z., A.A.N.T., M.Y.Y.
Project Administration: M.M., M.B.L., M.R.Z. A.A.N.T.
Resources: M.M., M.B.L., M.R.Z. A.A.N.T.
Software: Not applicable.
Supervision: M.M., M.B.L., M.R.Z. A.A.N.T.
Validation: M.M., M.B.L., M.R.Z., A.A.N.T., M.Y.Y.
Visualization: M.M., M.B.L., M.R.Z., A.A.N.T., M.Y.Y.
Writing-original draft preparation: M.M., M.B.L., M.R.Z., A.A.N.T., M.Y.Y.
Writing-review and editing: M.M., M.B.L., M.R.Z., A.A.N.T., M.Y.Y.
All authors have read and agreed to the published version of the manuscript.
Guarantor
Meirizal.
Research registration number
This study is not “First In Man” studies.
Conflict of interest statement
The authors have no conflict of interest.
References
- 1.Chen J., Yin P., Li N., Wu L., Jian X., Jiang C. Functional mandibular reconstruction with double-barrel fibular flap and primary osseointegrated dental implants improve facial esthetic outcome. J. Oral Maxillofac. Surg. 2019;77:218–225. doi: 10.1016/j.joms.2018.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Kokosis G., Schmitz R., Powers D.B., Erdmann D. Mandibular reconstruction using the free vascularized fibula graft: an overview of different modifications. Arch. Plast. Surg. 2016;43:3–9. doi: 10.5999/aps.2016.43.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.He Y., Zhang Z.Y., Zhu H.G., Wu Y.Q., Fu H.H. Double-barrel fibula vascularized free flap with dental rehabilitation for mandibular reconstruction. J. Oral Maxillofac. Surg. 2011;69:2663–2669. doi: 10.1016/j.joms.2011.02.051. [DOI] [PubMed] [Google Scholar]
- 4.Shen Y., Guo X.H., Sun J., Li J., Shi J., Huang W., et al. Double-barrel vascularised fibula graft in mandibular reconstruction: a 10-year experience with an algorithm. J. Plast. Reconstr. Aesthet. Surg. 2013;66:364–371. doi: 10.1016/j.bjps.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Chang Y.M., Tsai C.Y., Wei F.C. One-stage, double-barrel fibula osteoseptocutaneous flap and immediate dental implants for functional and aesthetic reconstruction of segmental mandibular defects. Plast. Reconstr. Surg. 2008;122:143–145. doi: 10.1097/PRS.0b013e3181774135. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrab C., Mathew G., Kirwan A., Thomas A., et al. The SCARE 2020 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. 2020;84(1):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Ho J.-H. In: Encyclopedia of Quality of Life and Well-being Research. Michalos A.C., editor. Springer Netherlands; Dordrecht: 2014. University of Washington Quality of Life Questionnaire; pp. 6821–6824. [DOI] [Google Scholar]
- 8.Dandriyal R., Gupta A., Pant S., Baweja H. Surgical management of ameloblastoma: conservative or radical approach. Natl. J. Maxillofac. Surg. 2011;2:22. doi: 10.4103/0975-5950.85849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adham M., Musa Z., Atmodiwirjo P., Bangun K. Ameloblastoma: hemimandibulectomy and reconstruction with free fibular graft-a case report and review of the literature introduction case report. Int. J. Head Neck Sci. 2017;1:251–257. doi: 10.6696/IJHNS.2017.0104.07. [DOI] [Google Scholar]





