Abstract
Introduction
Acquired hemophilia type A is a rare autoimmune disease characterized by bleeding episodes ranging from mild to severe, leading to significant morbidity and mortality. One of the various presentations is compartment syndrome secondary to a spontaneous hematoma.
Case presentation
A 95-year-old woman arrived at the emergency department with a one-week history of progressive pain in the right leg, without a previous history of trauma. Upon physical examination, she presented tenderness, edema, and bruising on the posterior and lateral aspects of the right leg, without neurovascular deficits.
Ultrasound revealed a collection in the posterior compartment of the leg, consistent with a hematoma. Due to worsening clinical condition, urgent drainage and fasciotomy of the posterior and lateral compartments of the leg was performed. After 2 years of follow-up, the patient has shown favorable progression.
Discussion
Hematoma drainage and fasciotomy are the primary management approaches for compartment syndrome secondary to hematoma presence. This etiology should be suspected in patients diagnosed with hemophilia who present to the emergency department with acute limb pain of unclear origin. Treatment should focus on relieving compartment pressure, supplementing the deficient factor, and eradicating inhibitors. None of the globally reported cases present a scenario with such an elderly patient exhibiting positive outcomes.
Conclusion
Compartment syndrome secondary to a spontaneous hematoma in a patient with acquired hemophilia is a diagnosis associated with significant morbidity and mortality, necessitating urgent management to ensure appropriate progression. This requires a multidisciplinary approach to drain the hematoma and rectify the hematologic condition.
Keywords: Case report, Acquired hemophilia, Compartment syndrome, Surgical management
Highlights
-
•
Acquired hemophilia type A is a rare autoimmune disease characterized by bleeding episodes ranging from mild to severe.
-
•
A spontaneous hematoma can lead to the development of compartment syndrome.
-
•
Management consists in hematoma drainage, fasciotomy, and intra-compartmental fibrin sealant.
1. Introduction
Acquired hemophilia type A is a rare autoimmune disease that can occur in both male and female patients, predominantly affecting elderly individuals or women postpartum. Clinically, it is characterized by bleeding episodes ranging from mild, such as mucosal bleed, to severe, such as spontaneous hemarthrosis, leading to significant morbidity and mortality [1]. Literature reports have described cases of postpartum or elderly patients with fatal outcomes, as well as some with favorable outcomes. However, to the best of our knowledge, this specific scenario has not been described in an elderly patient surpassing 80 years of age with a favorable outcome [2,3].
In this article, we present a case of a 95-year-old patient with a history of acquired hemophilia type A who developed a spontaneous muscular hematoma in the leg, subsequently progressing to compartment syndrome with a favorable outcome, managed in an academic institution. This report shows the clinical evolution and the treatment provided, hopefully, illustrating and guiding other physicians in future events. This case report has been reported in line with SCARE criteria [4].
2. Presentation of case
A 95-year-old female patient with a history of hypertension, type 2 diabetes mellitus, and acquired hemophilia type A presented to the emergency department of a level IV institution with a one-week history of progressive and debilitating pain in the right leg, without a previous history of trauma. On physical examination, she had edema and bruising on the posterior and lateral aspects of the right leg and foot (Fig. 1), with tenderness on palpation of the posterior musculature. No distal neurovascular deficit was documented. Based on these findings, the presence of a hematoma was considered, and an ultrasound was requested to confirm the diagnosis, as well as hemoglobin levels, factor VIII levels, and the presence of factor VIII inhibitors.
Fig. 1.

Photograph illustrating the documented signs in the patient's right leg.
The ultrasound revealed a 200-cc collection in the posterior compartment of the leg, consistent with a hematoma (Fig. 2). The patient had an initial hemoglobin level of 9.9 g/dL with isolated prolonged partial thromboplastin time (49 s) and decreased factor VIII levels (25.7 %), confirming a reactivation of her hematologic condition. As a result, she was evaluated by the Orthopedics and Hematology services, who decided to initiate supplementation with activated recombinant factor VIII, monitor for bleeding and signs of compartment syndrome.
Fig. 2.
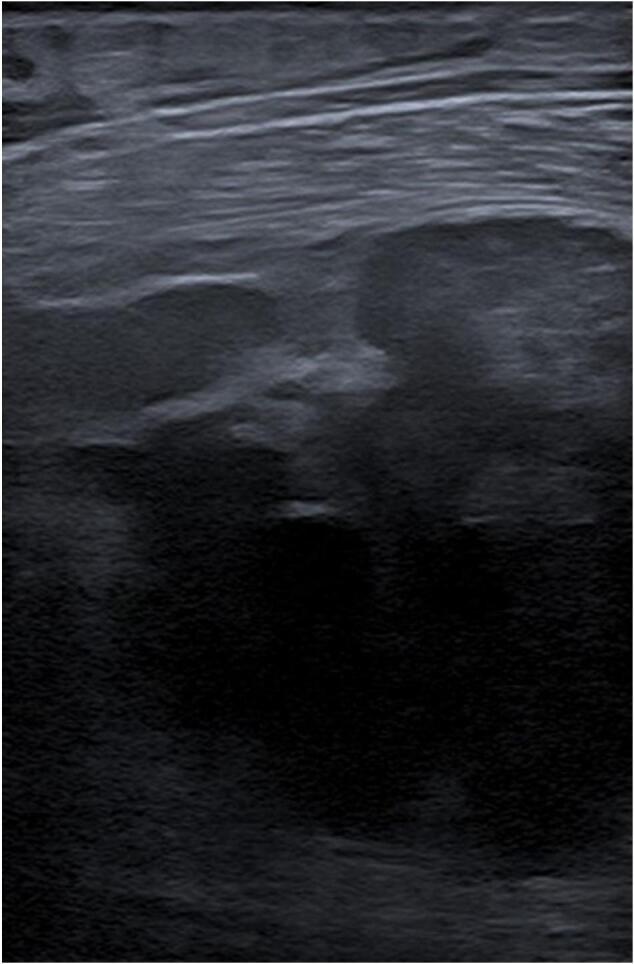
Ultrasound showing compartmentalized hematoma in the posterior compartment of the right leg.
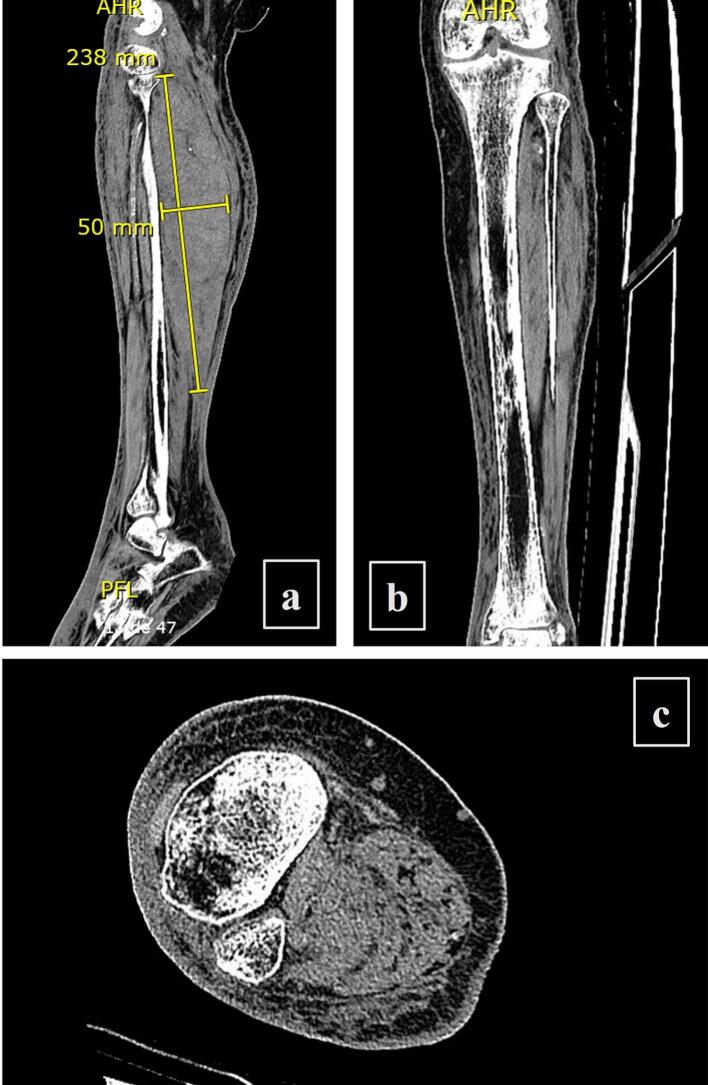
Approximately 48 h after admission, the patient experienced increased pain in her right leg, along with a deterioration in her level of consciousness, becoming somnolent, and exhibiting increased bruising and edema in the leg. Factor VIII levels were 20.4 % (previously 25.7 %), Hb: 8.3 g/dL (previously 9.9 g/dL), and PTT: 59 s (previously 49 s), indicating increased bleeding. During the daily evaluation by the orthopedics service, the patient reported pain with passive ankle dorsiflexion, and an increase in the size of the hematoma in the leg, leading to a diagnosis of compartment syndrome of the leg. An urgent intervention was deemed necessary, including hematoma drainage and fasciotomy of the posterior and lateral compartments of the leg. Prior to the surgery, a plain CT scan of the extremity was performed for surgical planning, and the patient's coagulation factors were stabilized by the Hematology service (Fig. 3).
Fig. 3.
(a) Sagittal, (b) coronal and (c) transversal plain leg CT scan showing hematoma in the posterior and lateral compartments measuring approximately 240 mm × 50 mm with a volume of 295 cm3.
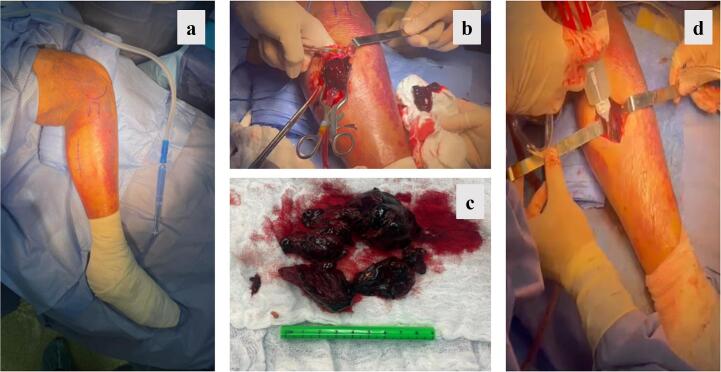
Ultimately, the patient underwent surgery 60 h after admission, during which a coagulated and compartmentalized hematoma was documented in the superficial and deep posterior compartments, with tension in the fascia at this level. Hematoma drainage, fasciotomy, and intra-compartmental fibrin sealant application were performed to control the bleeding prior to the primary closure of the wound. No vacuum device was used (Fig. 4).
Fig. 4.
(a) Marked surgical approach, (b) evidence of hematoma, (c) extracted hematoma, and (d) application of fibrin sealant in the right leg of the patient.
In the postoperative period, the patient exhibited a favorable clinical course. She regained her initial level of consciousness, experienced resolution of pain in her extremity, showed no neurological deficits, and had no new bleeding episodes. As a result, it was decided to discharge her from the institution after 96 h, with supplementation of factor VIII and prednisone 50 mg/day due to suspicion of factor VIII inhibitors, despite negative results during hospitalization.
2 years later, patient continues to be monitored in our institution and has shown a favorable progression without any new bleeding episodes, or adverse events.
3. Discussion
Acquired hemophilia type A is a rare disease, with an estimated incidence of 0.2 to 1.48 cases per million people per year. Approximately 50 % of cases are idiopathic, and it exhibits a bimodal presentation with one peak occurring before the age of 30, primarily in postpartum women, and another peak in patients over 65 years of age, with a 1:1 ratio between males and females [5].
In this condition, IgG autoantibodies are developed against factor VIII, resulting in decreased levels of factor VIII and the subsequent occurrence of mild hemostatic disorders, primarily involving mucocutaneous bleeding, as well as potentially life-threatening massive hemorrhages. It is generally estimated that the morbidity and mortality rates approach 40 %, which increase with delayed diagnosis or inadequate treatment [6].
The occurrence of muscular bleeding with subsequent increase in intra-compartmental pressure and the development of compartment syndrome is one of the possible catastrophic situations that can arise. In our literature review, we found cases of elderly patients who developed compartment syndrome in both upper and lower limbs, none of whom exceeded 90 years of age, and none with an early diagnosis and favorable outcome [[7], [8], [9]].
Diagnosis is usually made by finding isolated prolonged partial thromboplastin time (PTT), which prompts a mixing study to confirm the coagulation abnormality and simultaneously assess the presence of inhibitors through the Bethesda assay. It is important to note that the severity of bleeding is not correlated with factor VIII levels or inhibitor levels, as observed in our patient [1,6].
Treatment is based on controlling bleeding and eradicating the inhibitor. This is achieved with the use of bypassing agents such as recombinant factor VII and/or activated prothrombin complexes. Immunosuppression with steroids, cyclophosphamide, and even rituximab may be employed [10].
The development of compartment syndrome is one of the possible complications. The incidence is estimated at 3 per 100,000 individuals; however, it has not been specifically estimated in patients with acquired hemophilia. While it typically occurs secondary to high-energy fractures, it has also been widely reported in patients with hematologic disorders. Early treatment with fasciotomies, as performed in our patient, improves the prognosis of the affected limb [9,11].
4. Conclusion
The presence of compartment syndrome in patients with hematologic disorders necessitates clinical suspicion and early diagnosis to improve the prognosis of the affected limb and enhance patient survival. Treatment is aimed at relieving compartment pressure, as well as supplementing the deficient factor and eradicating inhibitors in cases such as acquired hemophilia type A. In the future a cohort study should be carried out to define factors related to poor prognosis in patients with acquired hemophilia.
Informed consent and ethics committee approval
Written informed consent was obtained from the patient's guardian for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request. Additionally, the final version of this manuscript was approved by the Ethical Committee of the Hospital Universitario Fundación Valle del Lili via Act Num. 11, 2023, Report case No. 669, IRB Approval No. 322–2023 on May 23, 2023.
Ethical approval
The final version of this manuscript was submitted to the institutional ethics committee and approved for submission via Act Num. 11, 2023, Report case No. 669, IRB Approval No. 322-2023 on May 23, 2023.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Guarantor
Paulo José Llinás H.
CRediT authorship contribution statement
Andrés Felipe Fonseca: Data collection and interpretation, writing
Gilberto Herrera: Study concept, data collection and interpretation, writing
Alejandro Gallego Álvarez: Data collection, writing
Paulo José Llinás: Study concept, data collection and interpretation, writing.
Declaration of competing interest
None.
Contributor Information
Andres Felipe Fonseca, Email: andres.fonseca@fvl.org.co.
Gilberto Antonio Herrera, Email: gilberto.herrera@fvl.org.co.
Alejandro Gallego, Email: alejandro.gallego.al@fvl.org.co.
Paulo J Llinas, Email: paulo.llinas@fvl.org.co.
References
- 1.García-Chávez J., Majluf-Cruz A. Hemofilia adquirida. Gac. Med. Mex. 2020;156(1):67–77. doi: 10.24875/GMM.19005469. [DOI] [PubMed] [Google Scholar]
- 2.Kaur K., Kalla A. A case of acquired hemophilia A in an elderly female. J. Community Hosp. Intern. Med. Perspect. 2018;8(4):237–240. doi: 10.1080/20009666.2018.1487246. (Internet) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gicart M., De Weweire A., Demulder A., De Wilde V. Acquired hemophilia A revealed by spontaneous bleeding in an 80-year-old man: a marginal diagnosis? Acta Clin. Belgica Int. J. Clin. Lab. Med. 2020;00(00):1–3. doi: 10.1080/17843286.2020.1768735. (Internet) [DOI] [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrab C., Mathew G., Kirwan A., Thomas A., et al. The SCARE 2020 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. 2020;84(1):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Webert K.E. Hemofilia a Adquirida Seminars 2012. Semin. Thromb. Hemost. 2012;38(7):735–741. doi: 10.1055/s-0032-1326779. [DOI] [PubMed] [Google Scholar]
- 6.Kruse-Jarres R., Kempton C.L., Baudo F., Collins P.W., Knoebl P., Leissinger C.A., et al. Acquired hemophilia A: updated review of evidence and treatment guidance. Am. J. Hematol. 2017;92(7):695–705. doi: 10.1002/ajh.24777. [DOI] [PubMed] [Google Scholar]
- 7.Pham T.V., Sorenson C.A., Nable J.V. Acquired factor VIII deficiency presenting with compartment syndrome. Am. J. Emerg. Med. 2014;32(2):195.e1–195.e2. doi: 10.1016/j.ajem.2013.09.022. (Internet) [DOI] [PubMed] [Google Scholar]
- 8.Lak M., Sharifian R.A., Karimi K., Mansouritorghabeh H. Acquired hemophilia A: clinical features, surgery and treatment of 34 cases, and experience of using recombinant factor VIIa. Clin. Appl. Thromb. 2010;16(3):294–300. doi: 10.1177/1076029608331227. [DOI] [PubMed] [Google Scholar]
- 9.Jentzsch T., Brand-Staufer B., Schäfer F.P., Wanner G.A., Simmen H.P. Illustrated operative management of spontaneous bleeding and compartment syndrome of the lower extremity in a patient with acquired hemophilia A: a case report. J. Med. Case Rep. 2014;8(1):1–7. doi: 10.1186/1752-1947-8-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tengborn L., Baudo F., Huth-Kühne A., Knoebl P., Lévesque H., Marco P., et al. Pregnancy-associated acquired haemophilia A: results from the European Acquired Haemophilia (EACH2) registry. BJOG Int. J. Obstet. Gynaecol. 2012;119(12):1529–1537. doi: 10.1111/j.1471-0528.2012.03469.x. [DOI] [PubMed] [Google Scholar]
- 11.Alidoost M., Conte G.A., Chaudry R., Nahum K., Marchesani D. A unique presentation of spontaneous compartment syndrome due to acquired hemophilia a and associated malignancy: case report and literature review. World J. Oncol. 2020;11(2):72–75. doi: 10.14740/wjon1260. [DOI] [PMC free article] [PubMed] [Google Scholar]