Abstract
Introduction
Embolization of the Middle Meningeal Artery (EMMA) is an emerging treatment option for patients with Chronic Subdural Haematoma (CSDH).
Questions
(1) Can EMMA change the natural history of untreated minimally symptomatic CSDH which do not require immediate evacuation? (2) What is the role of EMMA in the prevention of recurrence following surgical treatment? (3) Can the procedure be performed under local anaesthetic?
Material and methods
Systematic literature review. No randomised clinical trials available on EMMA for meta-analysis.
Results
Six unique large cohorts with more than 50 embolisations were identified (evidence: 3b-4). EMMA can control the progression of surgically naïve CSDH in 91.1–100% of the patients, in which haematoma expansion is halted, or the lesion decreases and resolves. Treatment failure requiring surgery occurs in 0–4.1% of the patients having EMMA as the primary and only treatment. Treatment failure requiring surgery goes up slightly to 6.8% if post-surgical patients are included. When EMMA is used as postsurgical adjunctive the risk of recurrence is 1.4–8.9% compared to 10–20% in surgical series. EMMA has minimal morbidity and it is feasible under local anaesthesia or slight sedation in the majority of cases.
Conclusion
There is cumulative low-quality evidence in the literature that EMMA may be able to modify the natural course of the disease. It appears effective in controlling progression of CSDHs in patients having it as a primary standing alone treatment and it reduces the risk of recurrence and the need for surgical intervention in refractory postsurgical cases or as a postsurgical adjunctive treatment with minimal morbidity (recommendation: C).
Keywords: Middle meningeal artery, Embolization, Therapeutic, Chronic subdural haematoma
Highlights
-
•
The literature on EMMA continues to grow based predominantly on non-randomised prospective or retrospective cohort studies.
-
•
There is cumulative low-quality evidence that EMMA is able to modify the natural course of the disease (Level of evidence: 3b-4).
-
•
EMMA appears effective in controlling progression of CSDHs as a primary standing alone treatment with minimal morbidity (level of recommendation: C).
-
•
If EMMA is used as postsurgical adjunctive recurrence is 1.4–8.9% compared to 10–20% in surgical series (level of recommendation: C).
1. Introduction
Embolization of the Middle Meningeal Artery (EMMA) is an emerging treatment option for patients with Chronic Subdural Haematoma (CSDH) (Starnoni et al., 2019). Early case reports and case series showed excellent results in terms of safety and efficacy and larger non-randomised studies suggest it can lower haematoma recurrence rates compared to conventional treatment, with equivalent morbidity (Srivatsan et al., 2019). Interest in this minimally invasive technique is growing and its use is spreading fast on the structure of already stablished interventional neuroradiology services (Martinez-Perez et al., 2020; Dicpinigaitis et al., 2021). We have previously reported the clinical outcomes of our early cohort which to our knowledge is the first group of patients in the UK to receive EMMA for CSDH (Mohamed et al., 2022).
There is renewed interest in the pathophysiology of this disease and how arterial embolization can change its natural course (Foreman et al., 2019). Observational studies on the natural history of CSDH have shown that about 40% of all patients may eventually recover on medical management without surgical intervention (Yang and Huang, 2017; Bender and Christoff, 1974). Therefore, conservative management is frequently advocated in asymptomatic cases with small collections and no mass effect. However, about 20% of those patients undergoing conservative management eventually deteriorate and require treatment (Bender and Christoff, 1974; Pichert and Henn, 1987). Surgical evacuation -via burr holes, twist drill craniostomy or craniotomy-is the most frequently used treatment (Holl et al., 2018). The rate of recurrence following surgical evacuation varies in the literature from 5 to 30% and further surgery is required in 10–20% of the cases (Mehta et al., 2018). A large prospective UK study showed that evacuation with two burr holes followed by temporary closed system drainage had the lowest rate of recurrence at 9% (Brennan et al., 2017). The use of dexamethasone has recently been shown in a large randomised clinical trial to produce fewer favourable outcomes than placebo, mainly due to more adverse events and despite a reduction in the need for an operation from 7.1% to 1.7% (Hutchinson et al., 2020). Similar results were obtained in a multicenter, open-label, controlled, noninferiority trial which was terminated early by the data and safety monitoring board owing to safety and outcome concerns in the dexamethasone group (Miah et al., 2023). Atorvastatin has also been trialled as a non-invasive treatment for CSDH. In a randomised clinical trial of 196 Chinese patients 11% of the patients who were taking atorvastatin and 23% of those who were taking placebo required surgery for an enlarging haematoma and/or a clinical deterioration (Jiang et al., 2018). Early data suggests that the clinical outcomes of EMMA may be superior to those of the currently used treatments described above.
1.1. Research questions
We have reviewed the published literature to answer the following questions:
-
−
Can EMMA change the natural history of untreated minimally symptomatic CSDH which do not require immediate evacuation?
-
−
What is the role of EMMA in the prevention of recurrence following surgical treatment?
-
−
What are the potential complications and can the procedure be performed under local anaesthetic to avoid the risk of general anaesthesia?
Ongoing randomised clinical trial were also reviewed and their design summarised to understand how future publications can help answer the questions above.
2. Materials and methods
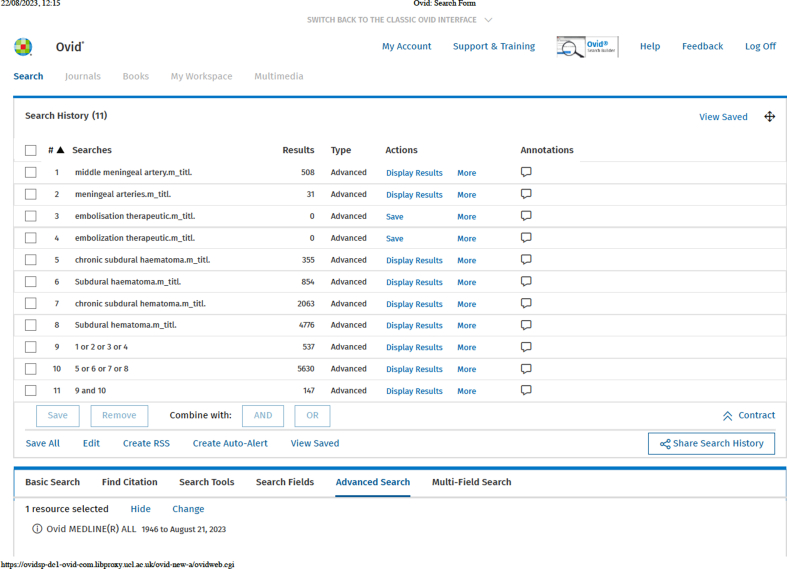
A literature search was performed to identify any studies reporting on the outcomes of EMMA for the treatment of CSDH. The PubMed database (US National Library of Medicine) was searched via the OVID platform (https://ovidsp.ovid.com) in August 2023 using the keywords: “middle meningeal artery” OR “meningeal arteries” OR “embolization therapeutic” OR “embolization therapeutic” AND “chronic subdural haematoma” OR “Subdural haematoma” OR “chronic subdural haematoma” OR “Subdural haematoma”. The search was limited to studies on adult humans, published at any time in English or Spanish language. The review was conducted and reported using the updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., 2021).
The PubMed search yielded one hundred and forty-seven (147) papers. The titles and abstracts of those articles were reviewed and forty-eight (48) non-related papers were excluded. Ninety-nine (99) papers were considered relevant to the subject. Eighteen (18) of them were letters to the editor, ten (10) were non-systematic reviews or commentary articles and eighteen (18) were miscellaneous papers reporting on a variety of issues other than treatment outcomes, such as anatomical descriptions, technical notes and imaging or pathophysiology studies. Those were also excluded. The remaining papers were twelve (12) systematic reviews, twenty-three (23) case reports or small case series with less than 10 patients, ten (10) case series with 10–50 patients undergoing EMMA and eight (8) larger case series -some with control groups-of more than 50 embolisations. These studies and their references were reviewed to answer the three questions above. No randomised clinical trials are available on EMMA to conduct meta-analysis. The papers reporting outcomes in series larger than 50 patients were appraised and summarised. This arbitrary threshold was established to avoid bias from studies reporting outcomes of small numbers. Data collected from the papers included the demographics and clinical characteristics of the patients and the radiological features of the CSDH treated, the details of the procedure including type of anaesthesia and outcomes including need for further treatment, recurrence rates and radiological outcomes. The levels of evidence and grades of recommendation of the Oxford Centre for Evidence-Based Medicine were used to rate the quality of evidence (Phillips et al., 2009).
The clinical trials database of the United States National Library of Medicine and National Institutes of Health (clinicaltrials.gov) was searched using the keywords “middle meningeal artery” AND “chronic subdural haematoma”. The methodology and study design of ongoing randomised clinical trials studying the use of EMMA for CSDH was reviewed and summarised.
3. Results
No randomised clinical trials are available on EMMA to conduct meta-analysis. We have identified six unique large cohorts with more than 50 embolisations which have been summarised in Table 1 (Ban et al., 2018; Link et al., 2019; Kan et al., 2021; Salem et al., 2023; Liu et al., 2023; Catapano et al., 2023). Two other large case series (Joyce et al., 2020; Nia et al., 2021) were excluded to avoid duplication as they essentially report on the same multi-centre cohort from the USA first described, in a more comprehensive manner, by Kan et al. The series by Salem et al. also comes from the same USA population but it is sufficiently bigger (530 vs 138 patients) for it to be regarded as a different cohort so it was included in our review.
Table 1.
Large case series with more than 50 MMA embolisations for CSDH.
| Study Country | Design | Number of patients | Patient characteristics | Procedure | Outcomes | Complications | Evidence/recommend |
|---|---|---|---|---|---|---|---|
|
Ban et al. (2018) South Korea |
Prospective non-randomised study with historical cohort | 72 consecutive patients Surgically naïve: 37.5% Adjunctive postsurgical: 62.5% Historical control: 469 patients Conservative: 14.3% Surgery: 85.7% |
Older than 20 y Haemispheric CSDHs Max thickness ≥10 mm Radiological mass effect No underlying cause Life expectancy >6 mo |
Polyvinyl alcohol (PVA) particles Under LA |
Treatment failure: Embolization group 1.4% Surgically naïve: 0% Adjunctive postsurgical: 2.2% Controls: 27.5% Surgical rescue: Embolization group 1.4% Controls: 18.8% |
No statistical difference in treatment related complications. 0% in EMMA group 4.3% in controls |
3b/C |
|
Link et al. (2019) USA |
Retrospective case series | 60 CSDHs Surgically naïve: 42 Recurrent postsurgical: 8 Adjunctive postsurgical: 10 |
Symptomatic adults Multiple comorbidities Aspirin 57% dual antiplatelets: 10%| Anticoagulation: 12% |
Polyvinyl alcohol (PVA) particles Most cases: light/no sedation Few under GA |
Non-adjunctive cases: Stable/decreased in size and able to avoid surgery: 91.1% Recurrence requiring surgery: 8.9% Resolution/reduction in size >50%: 68.9% |
3 unrelated mortalities No procedural complications |
4/C |
|
Kan et al. (2021) USA Also see: Joyce et al. (2020), Nia et al. (2021) |
Multi-centre prospective non-randomised case series 15 centers |
138 consecutive patients Bilateral interventions: 15 Total embolizations: 154 Primary treatment: 66.7% Previous surgery: 33.3% |
Median SDH thickness: 14 mm Antiplatelet: 30.4% Anticoagulation: 23.9% |
Particles: 70.2% Liquid: 25.3% GA: 46.1% |
Procedure successfully completed: 97.4% >50% thickness reduction: 70.8% Further CSDH treatment: 6.5% Primary treatment - stable/decreased in size and able to avoid surgery: 95.9% No difference between embolization materials |
16 complications Continued haematoma expansion: 6.5% Mortality: 4.4%, mostly unrelated |
4/C |
|
Salem et al. (2023) USA |
Multi-centre Retrospective 13 centers |
530 patients 636 MMA embolisations Stand-alone treatment: 50.4% Concurrent with surgery: 25.8% Prior surgical failure: 23.9% |
Median SDH thickness: 15 mm Antiplatelet: 31.3% Anticoagulation: 21.7% |
Particles: 14.8% Coils + particles: 39.9% Liquid: 36.7% Liquid and coils: 6.1% GA: 34% |
Median follow-up: 4.1 months Clinical failure: 6.8% Radiographic failure to reduce >50%: 26.3% |
Complication: 4.7% Worse SDH: 0.9% Stroke: 0.8% Visual loss: 0.8% Access site: 0.6% |
4/C |
|
Liu et al. (2023) China |
Retrospective case series | 53 patients MMA embolization alone: 31 MMA + burr hole irrigation: 22 |
Mean SDH thickness: 15.6 mm Mean MLS: 11.42 mm Antiplatelet or anticoagulation: 38.7% |
PVA Particles + liquid Majority under LA. Few under conscious sedation. |
1 relapse (EMMA alone): no surgery required Haematoma resolution: 50.9% at 4 months 90.6% at last radiologic follow-up No significant difference in haematoma absorption between EMMA alone and EMMA + irrigation at 6 months |
No procedural complications | 4/C |
|
Catapano et al. (2023) Arizona, USA |
Retrospective case series | 80 patients 98 CSDHs EMMA alone or adjunctive postsurgical |
Symptomatic patients CSDH width ≥8 mm Antiplatelet or anticoagulation: 49% |
Onyx: 89% Liquid or particles: 10% |
Significant reduction in haematoma volume and MLS in the immediate post-embolization period | Not reported | 4/C |
Three clinically distinct treatment subgroups are now well defined in the literature: the surgically naive, postsurgical adjunctive, and recurrent postsurgical patients (Matsumoto et al., 2018; Sioutas et al., 2023). The contribution of these three groups to the large case series are presented in Table 1, together with the characteristics of the patients and radiological characteristics of the haematomas included.
-
−
Can EMMA change the natural history of untreated minimally symptomatic CSDH which do not require immediate evacuation?
The progression of CSDH and need for surgery for the subgroup of patients having EMMA as a stand-alone treatment were reported in three of the studies summarised in Table 1. EMMA is able to control the progression of surgically naïve CSDH in 91.1–100% of the patients, in which haematoma expansion is halted, or the lesion decreases and resolves. Treatment failure requiring surgery occurs in 0–4.1% of the patients having EMMA as the primary and only treatment. These outcomes are consistently better than historical cohorts and control groups having conservative management which strongly suggests that EMMA can modify the course of the disease and alter the underlying pathophysiological processes that maintain CSDH.
-
−
What is the role of EMMA in the prevention of recurrence following surgical treatment?
When EMMA is used as a postsurgical adjunctive treatment the risk of recurrence varies between 1.4 and 8.9% and treatment failure requiring surgery goes up slightly to 6.8% when recurrent post-surgical patients are included. (Srivatsan et al., 2019). It is difficult to pool the outcomes for recurrent postsurgical patients as only one paper provided outcomes for that subgroup. However, recurrent postsurgical patients have been well represented in the case load since the early reports and the results appear consistently better than historical data for other treatment options (Martinez-Perez et al., 2020; Onyinzo et al., 2022).
-
−
What are the potential complications and can the procedure be performed under local anaesthetic to avoid the risk of general anaesthesia?
The most common complication is treatment failure, i.e. worsening of the haematoma with neurological deficit, which occurs in a small percentage of patients and generally require surgery as detailed in Table 1. Patients with enlarging haematomas after MMA who require rescue operation tend to have good outcomes after surgery but mortalities have also been described. Large case series have reported death in about 1% of the patients, mostly unrelated to the embolization procedure but in some cases involved pneumonia or other complications related to long inpatient stay (Kan et al., 2021). MMA rupture during the procedure and the development of extradural haematoma has been described (Mohamed et al., 2022).
Great attention has been given to anatomical variants and dangerous collateral vessels. Ophthalmic origin of the middle meningeal artery, as opposed to maxillary, has been described in up to 13.8% of patients with CSDH which is higher than the general population (Fantoni et al., 2020). Meningo-ophthalmic connections, i.e. anastomoses between the MMA and the ophthalmic artery, have been reported in 8.5% of cases and they must be actively sought to avoid vision loss secondary to occlusion of the central retinal artery, a branch of the ophthalmic artery (Kan et al., 2021). Inadvertent embolization of the recurrent meningeal artery may result in blindness or stroke and embolization of the petrosal branch of the MMA or the vasa nervorum of the facial nerve may result in facial palsy (Yu et al., 2016; Shotar et al., 2021b). Recommendations have changed over time from excluding those patients and offering them alternative treatments to ensuring embolization is distal to the origin of the anastomoses (Tempaku et al., 2015). Rarer complications such as dural arteriovenous fistula formation or abducens cranial nerve palsies have also been described (Raviskanthan et al., 2021; Shotar et al., 2021a; Piergallini et al., 2019; Yu et al., 2016).
Five out of six papers in Table 1 reported the kind of anaesthesia used for EMMA. The procedure was performed under local anaesthesia in all 72 patients reported by Ban et al., more than 50% of the cases in the USA-based series (Salem et al., 2023; Kan et al., 2021), and the majority of the patients in the cohort reported by Liu et al. (Table 1). It was done under light or no sedation in most cases treated by Link et al. The procedure described involves selective microcatheterization of the MMA with radial or femoral artery and the aim to embolize both distal branches which is achieved in 97.4% of the cases (Kan et al., 2021). Multiple embolization materials have been used including polyvinyl alcohol (PVA) particles, liquid embolic agents such as N-butyl-2- cyanoacrylate (NBCA), coils and gelatine sponge, alone or in combination. Liquid embolics can penetrate deeper into smaller vessels, including anastomoses with the intracranial circulation, and for this reason it has been suggested that large particles (above 150 μm) may be more appropriate. However, no difference has yet been found in terms of efficacy or complications between embolization materials (Kan et al., 2021).
-
−
Ongoing clinical trials
The clinicaltrials.gov search yielded 15 studies. Ten of them are Randomised Clinical Trials (RCT) and their design and current stage is summarised in Table 2. Nine of them are already recruiting patients and in total they will include more than 2500 patients in at least six countries. Some of the common inclusion criteria include: symptomatic patients, haemispheric haematoma of a considerable size (generally ≥10 mm) or causing mass effect, patients that have failed conservative management or require surgery, high risk of recurrence, mild to moderate disability and expected survival more than 6 months. The primary outcome is radiological in five of them, i.e. progression or recurrence, and composite, haematoma recurrence/progression or need for re-intervention, in the rest. Secondary outcomes include: hemorrhagic or ischemic complications, neurological deficits including blindness and facial nerve palsy, access-related complications, mortality, length of hospital stay, improvement on functional scores (mRS and National Institutes of Health Stroke Scale, NIHSS) and subgroup analyses are planned to determine if there is difference between embolization materials. All RCTs are expected to complete recruitment before 2025 and two have already passed their registered estimated date of completion. Two non-randomised trials (NCT04065113, NCT04500795) and three single arm non-randomised interventional studies (NCT03307395, NCT04095819, NCT04923984) are also in course.
Table 2.
Ongoing trials.
| Trial | Centre | Study design | Population | Intervention | Outcome/endpoint | Current stage |
|---|---|---|---|---|---|---|
| MMA embolization compared to Traditional Surgical Strategies to Treat CSDH. NCT04095819 |
Atlantic Health, New Jersey, US https://ClinicalTrials.gov/show/NCT04095819 |
Single centre randomized open-label trial with parallel assignment | 50 adult patients Symptomatic CSDH that have failed conservative management |
EMMA vs drainage of CSDH using craniotomy or Burr Hole | Size of SDH at 6 months | Recruiting Start: Sep 2019 EDC: Apr 2022 |
| Embolization of Middle Meningeal Artery in Chronic Subdural Haematoma (ELIMINATE). NCT04511572 |
Academisch Medisch Centrum, Universiteit van Amsterdam, Netherlands https://clinicaltrials.gov/ct2/show/NCT04511572 |
Multicenter, randomized controlled open-label superiority trial | 170 patients CSDH that require surgery |
EMMA within 72 h of standard surgical treatment vs surgery only. | Reoperation within 24 weeks | Recruiting Start: Aug 2020 EDC: Jul 2025 |
| Management of CSDH with or without EMMA - a Randomized Control Trial. NCT04750200 |
University of Manitoba, Canadahttps://clinicaltrials.gov/ct2/show/NCT04750200 | Open-label randomized control trial comparing | 200 symptomatic patients Clinical need of surgical drainage or medical management mRankin Scale of ≤2 at baseline CSDH thickness ≥10 mm |
Standard of care treatment (surgical drainage and/or medical management) with or without EMMA no later than 48 h. | Recurrence at 90-days | Recruiting Start: Feb 2021 EDC: Dec 2025 |
| Embolization of the MMA for the Prevention of CSDH Recurrence in High Risk Patients (EMPROTECT). NCT04372147 |
Assistance Publique, Hôpitaux de Paris, Francehttps://clinicaltrials.gov/ct2/show/NCT04372147 | Multicenter open label randomized controlled intention to treat trial | 342 adults operated for CSDH + high risk of recurrence: Chronic alcoholism, liver cirrhosis, antiplatelet, anticoagulant, thrombocytopenia or surgery without a drain | MMA embolization within 7 days of surgery vs standard medical care only | Recurrence at 6 months | Unknown Start: May 2020 EDC: Dec 2022 |
| MMA Embolization for the Treatment of Subdural Hematomas With TRUFILL® n-BCA (MEMBRANE). NCT04816591 |
Industry sponsored: Cerenovus, DePuy Synthes Products, Inc. New York and Morgantown, US https://clinicaltrials.gov/ct2/show/NCT04816591 |
Prospective, multi-center, open-label, randomized controlled study | 376 patients with previously untreated CSDH and pre-randomization mRS </ = 3 | Four arms: Surgery + Embolization Surgery Only Medical Management + Embolization Medical Management only |
Haematoma recurrence/progression or need for re-intervention | Recruiting Start: Mar 21 EDC: May 25 |
| Dartmouth Middle Meningeal Embolization Trial (DaMMET). NCT04270955 |
Dartmouth-Hitchcock Medical Center, New Hampshire, US https://clinicaltrials.gov/ct2/show/NCT04270955 |
Single Center Randomized Control Trial | 118 symptomatic or asymptomatic adults patients CSDH maximal thickness > 7 mm Non-focal: >50% of the convexity |
Embolization of the Middle Meningeal Artery vs Standard of care including possible surgical evacuation | Radiographic resolution of the haematoma | Recruiting Start: Mar 2021 EDC: Dec 2025 |
| The Onyx™ Trial For The Embolization Of The Middle Meningeal Artery For CSDH (OTEMACS). NCT04742920 |
Montpellier, France https://clinicaltrials.gov/ct2/show/NCT04742920 |
Prospective, randomised, open-label multicenter clinical trial with blinded endpoint evaluation | 440 symptomatic patients ≥18 y Non-focal CSDH >10 mm No significant disability (mRS ≤3) |
Surgical treatment plus adjuvant MMA Onyx™ non-adhesive liquid embolic agent embolization within 24 h vs surgical treatment alone | Recurrence and reintervention at 90 days and functional outcome | Recruiting Start: Feb 2021 EDC: Dec 2022 |
| The SQUID Trial for the Embolization of the Middle Meningeal Artery for Treatment of CSDH (STEM). NCT04410146 |
Industry sponsored: Balt USA. 26 sites in US, France, Germany and Spain. https://clinicaltrials.gov/ct2/show/NCT04410146 |
International, multi-center, prospective, randomized controlled trial | 228 patients ≥30 y Pre-morbid mRS 0-1 CSDH ≥10 mm greatest thickness Symptomatic and mass effect Radiological chronicity |
Standard Management (surgery or medical) with or without MMA embolization using SQUID non-adhesive liquid embolic agent | Residual/re-accumulation (≥10 mm), re-operation, new major stroke and death from neurological cause at 180 days | Active, not recruiting Start: Jun 2020 EDC: Aug 2024 |
| Embolization of the MMA With ONYX™ Liquid Embolic System for Subacute and CSDH (EMBOLISE). NCT04402632 |
Industry spondored: Medtronic Neurovascular Clinical Affairs. https://clinicaltrials.gov/ct2/show/NCT04402632 |
Randomised open label clinical trial with sequencial assignment | 600 participants Untreated CSDH Pre-morbid mRS ≤3 subacute or chronic SDH Normal MMA anatomy Able to stop anticoagulation |
Four arms: Evacuation only Evacuation + Embolization Observation only Embolization only |
Recurrence/progression requiring re-intervention at 90 days | Recruiting Start: Oct 2020 EDC: Aug 2024 |
| Endovascular Embolization for Chronic Subdural Hematomas Following Surgical Evacuation (endovascular). NCT04272996 |
Medical College of Georgia, Augusta University, US https://clinicaltrials.gov/ct2/show/NCT04272996 |
Randomised, open label clinical trial | 60 participants 18–90 yo CSDH that require surgical evacuation |
Evacuation of subdural hematomas and endovascular embolization of the MMA vs standard surgical evacuation alone | Radiographic recurrence at 3 months | Recruiting Start: Feb 2020 EDC: June 2024 |
4. Discussion
We have reviewed the literature regarding the use of MMA embolization for CSDH and summarised the clinical outcomes of more than 900 patients who have undergone this procedure within non-randomised prospective or retrospective cohort studies, Table 1. No randomised clinical trials are available on EMMA to conduct meta-analysis. The level of evidence derived from the available publications is low (3b-4) but multiple groups from different countries have showed that EMMA is effective in controlling progression of CSDHs in 91.1–100% of the patients having it as a primary standing alone treatment with 0–4.1% of them requiring surgery. This is better than failure rates reported for conservative management, atorvastatin, dexamethasone and surgery and a strong indication that EMMA is indeed able to modify the natural course of the disease. However, there is currently not strong enough evidence to recommend its use over other treatment options in patients who do not require immediate surgical evacuation.
A dramatic reduction in the risk of recurrence requiring further surgery has been described when EMMA is used in refractory cases or as a postsurgical adjunctive treatment (Table 1). This has been consistently described in all large case series and the investigators who designed currently ongoing clinical trials were aware that recurrence rate post-surgery is the primary outcome most likely to yield positive or statistically significant results. Eight out of ten RCTs currently recruiting patients include as part of their design a comparison of patients having surgical treatment with or without EMMA to examine the potential effect in recurrence rates. We suspect that a lower rate of recurrence after surgery or in refractory cases will be the key aspect supporting superiority of MMA above other treatments in clinical trials.
The neurosurgical community is already familiar with the scenario of endovascular treatment replacing surgery for pathologies that are traditionally treated with surgery as it happened with aneurysms. The less invasive nature of endovascular surgery gives it an innate advantage over surgery and comparable outcomes, as oppose to superiority, are enough to tilt the balance away from surgery. Local anaesthetic or light sedation were the preferred methods of anaesthesia in most large series published in the literature (Table 1). This favours the use of endovascular treatment over surgery in CSDH patients who are usually elderly with multiple comorbidities and would benefit from avoiding the risks of general anaesthesia.
Anticoagulation and antiplatelets can be continued or started sooner after EMMA compared to surgery, which is advantageous to a large part of the CSDH population (Dian et al., 2021). In the largest series reported in the literature, on admission 31.3% of the patients were on antiplatelet medications and 21.7% of them were on anticoagulation (Salem et al., 2023). Withholding these medications in patients with CSDH having conservative or surgical management increases their risk of cardiac or other thromboembolic complications and multiple groups now routinely continue antithrombotic medication in patients undergoing MMA embolization (Foreman et al., 2019). The cost benefit profile of MMA embolization has been examined with great interest and that is reflected in the design of ongoing clinical trials (Gilligan and Gologorsky, 2020; McCann et al., 2023). EMMA has been associated with lower total hospital cost compared to surgery and the lower cost is directly related to the decreased need for additional treatment interventions (Catapano et al., 2022). Most trials found through our clinicaltrials.gov search included a cost outcome measure. A potential disadvantage of EMMA compared to surgery is the need for repeated follow up imaging after treatment which most centers are likely to perform, at least until EMMA is fully stablished as a routine treatment. A previous randomized trial involving 361 patients showed that the use of routine CT after evacuation of a CSDH had no advantage over CT performed only in patients with clinical deterioration (Schucht et al., 2019). It is likely that this conclusion will also be reached for EMMA as more good quality data becomes available.
A potential shift from surgical to endovascular management of CSDH can have negative implications for neurosurgical training. Burr holes for CSDH tend to be one of the first procedures performed independently by junior neurosurgical trainees and they are particularly good for early training because they enable trainees to develop confidence, intraoperative decision making and core surgical skills with low risk. The emergence of EMMA for CSDH can worsen an already worrying trend towards less training opportunities for young surgeons.
There are limitations in the currently available outcome data and therefore in the conclusions that could be drawn from our literature review. Although most of the outcomes reported in large series was gathered prospectively the selection of patients undergoing MMA embolization was based on individual surgeon preference and this is likely to have introduced selection bias. There is also a large degree of heterogeneity in the patients selected for EMMA and it is not possible currently to confidently conclude which patients are most likely to benefit from this treatment. We expect that the conclusion of the ongoing RCTs, with their independent data collection and analysis mechanisms, will allow for strong levels of recommendation in terms of patient and treatment selection. It is unlikely that all questions will be answered by the trials but it is definitely a innovation in the neurosurgical field to have as many as ten RCTs simultaneously recruiting patients who have traditionally been under the neurosurgeons remit (Haldrup et al., 2021; Mori and Maeda, 2001). We look forward to learning how this subject will unfold and how it will change our practice.
5. Conclusions
EMMA is an emerging minimally invasive technique and there is strong indication from cumulative low-quality literature that EMMA is indeed able to modify the natural course of the disease. No randomised clinical trials are available on EMMA to conduct meta-analysis but it appears effective in controlling progression of CSDHs in patients having it as a primary standing alone treatment and it reduces the risk of recurrence and the need for surgical intervention in refractory postsurgical cases or as a postsurgical adjunctive treatment. EMMA has minimal morbidity and it is feasible under local anaesthesia or slight sedation in the majority of cases. Multiple randomised controlled clinical trials are currently being conducted to fully determine the efficacy and long-term outcomes of this treatment and their results are likely to change the current treatment paradigm of this disease.
Declaration of competing interest
I can confirm that the authors of this paper have not conflicts of interest to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bas.2023.102672.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
figs1.
References
- Ban S.P., Hwang G., Byoun H.S., Kim T., Lee S.U., Bang J.S., Han J.H., Kim C.Y., Kwon O.K., Oh C.W. Middle meningeal artery embolization for chronic subdural hematoma. Radiology. 2018;286(3):992–999. doi: 10.1148/radiol.2017170053. [DOI] [PubMed] [Google Scholar]
- Bender M.B., Christoff N. Nonsurgical treatment of subdural hematomas. Arch. Neurol. 1974;31(2):73–79. doi: 10.1001/archneur.1974.00490380021001. [DOI] [PubMed] [Google Scholar]
- Brennan P.M., Kolias A.G., Joannides A.J., Shapey J., Marcus H.J., Gregson B.A., Grover P.J., Hutchinson P.J., Coulter I.C., Collaborative B.N.T.R. The management and outcome for patients with chronic subdural hematoma: a prospective, multicenter, observational cohort study in the United Kingdom. J. Neurosurg. 2017:1–8. doi: 10.3171/2016.8.JNS16134.test. [DOI] [PubMed] [Google Scholar]
- Catapano J.S., Koester S.W., Hanalioglu S., Farhadi D.S., Naik A., Hartke J.N., Tunc O., Winkler E.A., Chang S.W., Lawton M.T., Jadhav A.P., Ducruet A.F., Albuquerque F.C. Middle meningeal artery embolization associated with reduced chronic subdural hematoma volume and midline shift in the acute postoperative period. J. Neurointerventional Surg. 2023 doi: 10.1136/jnis-2022-020054. [DOI] [PubMed] [Google Scholar]
- Catapano J.S., Koester S.W., Srinivasan V.M., Rumalla K., Baranoski J.F., Rutledge C., Cole T.S., Winkler E.A., Lawton M.T., Jadhav A.P., Ducruet A.F., Albuquerque F.C. Total 1-year hospital cost of middle meningeal artery embolization compared to surgery for chronic subdural hematomas: a propensity-adjusted analysis. J. Neurointerventional Surg. 2022;14(8):804–806. doi: 10.1136/neurintsurg-2021-018327. [DOI] [PubMed] [Google Scholar]
- Dian J., Linton J., Shankar J.J. Risk of recurrence of subdural hematoma after EMMA vs surgical drainage - systematic review and meta-analysis. Intervent Neuroradiol. 2021;27(4):577–583. doi: 10.1177/1591019921990962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dicpinigaitis A.J., Al-Mufti F., Cooper J.B., Faraz Kazim S., Couldwell W.T., Schmidt M.H., Gandhi C.D., Cole C.D., Bowers C.A. Nationwide trends in middle meningeal artery embolization for treatment of chronic subdural hematoma: a population-based analysis of utilization and short-term outcomes. J. Clin. Neurosci. 2021;94:70–75. doi: 10.1016/j.jocn.2021.10.001. [DOI] [PubMed] [Google Scholar]
- Fantoni M., Eliezer M., Serrano F., Civelli V., Labeyrie M.A., Saint-Maurice J.P., Houdart E. High frequency of ophthalmic origin of the middle meningeal artery in chronic subdural hematoma. Neuroradiology. 2020;62(5):639–644. doi: 10.1007/s00234-020-02363-6. [DOI] [PubMed] [Google Scholar]
- Foreman P., Goren O., Griessenauer C.J., Dalal S.S., Weiner G., Schirmer C.M. Middle meningeal artery embolization for chronic subdural hematomas: cautious optimism for a challenging pathology. World Neurosurg. 2019;126:528–529. doi: 10.1016/j.wneu.2019.03.160. [DOI] [PubMed] [Google Scholar]
- Gilligan J., Gologorsky Y. Middle meningeal artery embolization for chronic subdural hematoma: current state and future directions. World Neurosurg. 2020;139:622–623. doi: 10.1016/j.wneu.2020.05.010. [DOI] [PubMed] [Google Scholar]
- Haldrup M., Munyemana P., Ma'aya A., Jensen T.S.R., Fugleholm K. Surgical occlusion of middle meningeal artery in treatment of chronic subdural haematoma: anatomical and technical considerations. Acta Neurochir. 2021;163(4):1075–1081. doi: 10.1007/s00701-021-04754-x. [DOI] [PubMed] [Google Scholar]
- Holl D.C., Volovici V., Dirven C.M.F., Peul W.C., van Kooten F., Jellema K., van der Gaag N.A., Miah I.P., Kho K.H., den Hertog H.M., Lingsma H.F., Dammers R., (DSHR), D. C. S. H. R. G. Pathophysiology and nonsurgical treatment of chronic subdural hematoma: from past to present to future. World Neurosurg. 2018;116:402–411.e2. doi: 10.1016/j.wneu.2018.05.037. [DOI] [PubMed] [Google Scholar]
- Hutchinson P.J., Edlmann E., Bulters D., Zolnourian A., Holton P., Suttner N., Agyemang K., Thomson S., Anderson I.A., Al-Tamimi Y.Z., Henderson D., Whitfield P.C., Gherle M., Brennan P.M., Allison A., Thelin E.P., Tarantino S., Pantaleo B., Caldwell K., Davis-Wilkie C., Mee H., Warburton E.A., Barton G., Chari A., Marcus H.J., King A.T., Belli A., Myint P.K., Wilkinson I., Santarius T., Turner C., Bond S., Kolias A.G., Collaborative B.N.T.R., Collaborators D.-C.T. Trial of dexamethasone for chronic subdural hematoma. N. Engl. J. Med. 2020;383(27):2616–2627. doi: 10.1056/NEJMoa2020473. [DOI] [PubMed] [Google Scholar]
- Jiang R., Zhao S., Wang R., Feng H., Zhang J., Li X., Mao Y., Yuan X., Fei Z., Zhao Y., Yu X., Poon W.S., Zhu X., Liu N., Kang D., Sun T., Jiao B., Liu X., Yu R., Gao G., Hao J., Su N., Yin G., Lu Y., Wei J., Hu J., Hu R., Li J., Wang D., Wei H., Tian Y., Lei P., Dong J.F. Safety and efficacy of atorvastatin for chronic subdural hematoma in Chinese patients: a randomized ClinicalTrial. JAMA Neurol. 2018;75(11):1338–1346. doi: 10.1001/jamaneurol.2018.2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyce E., Bounajem M.T., Scoville J., Thomas A.J., Ogilvy C.S., Riina H.A., Tanweer O., Levy E.I., Spiotta A.M., Gross B.A., Jankowitz B.T., Cawley C.M., Khalessi A.A., Pandey A.S., Ringer A.J., Hanel R., Ortiz R.A., Langer D., Levitt M.R., Binning M., Taussky P., Kan P., Grandhi R. Middle meningeal artery embolization treatment of nonacute subdural hematomas in the elderly: a multiinstitutional experience of 151 cases. Neurosurg. Focus. 2020;49(4):E5. doi: 10.3171/2020.7.FOCUS20518. [DOI] [PubMed] [Google Scholar]
- Kan P., Maragkos G.A., Srivatsan A., Srinivasan V., Johnson J., Burkhardt J.K., Robinson T.M., Salem M.M., Chen S., Riina H.A., Tanweer O., Levy E.I., Spiotta A.M., Kasab S.A., Lena J., Gross B.A., Cherian J., Cawley C.M., Howard B.M., Khalessi A.A., Pandey A.S., Ringer A.J., Hanel R., Ortiz R.A., Langer D., Kelly C.M., Jankowitz B.T., Ogilvy C.S., Moore J.M., Levitt M.R., Binning M., Grandhi R., Siddiq F., Thomas A.J. Middle meningeal artery embolization for chronic subdural hematoma: a multi-center experience of 154 consecutive embolizations. Neurosurgery. 2021;88(2):268–277. doi: 10.1093/neuros/nyaa379. [DOI] [PubMed] [Google Scholar]
- Link T.W., Boddu S., Paine S.M., Kamel H., Knopman J. Middle meningeal artery embolization for chronic subdural hematoma: a series of 60 cases. Neurosurgery. 2019;85(6):801–807. doi: 10.1093/neuros/nyy521. [DOI] [PubMed] [Google Scholar]
- Liu Z., Wang Y., Tang T., Zhang Y., Sun Y., Kuang X., Wei T., Zhou L., Peng A., Cao D., Hongsheng W., Qi W., Chenyi W., Shan Q. Time and influencing factors to chronic subdural hematoma resolution following middle meningeal artery embolization. World Neurosurg. 2023 doi: 10.1016/j.wneu.2023.03.050. [DOI] [PubMed] [Google Scholar]
- Martinez-Perez R., Rayo N., Tsimpas A. Endovascular Embolisation of the Middle Meningeal Artery to Treat Chronic Subdural Haematomas: Effectiveness, Safety, and the Current Controversy. A Systematic Review. 2020. Neurologia (Engl Ed) [DOI] [PubMed] [Google Scholar]
- Matsumoto H., Hanayama H., Okada T., Sakurai Y., Minami H., Masuda A., Tominaga S., Miyaji K., Yamaura I., Yoshida Y. Which surgical procedure is effective for refractory chronic subdural hematoma? Analysis of our surgical procedures and literature review. J. Clin. Neurosci. 2018;49:40–47. doi: 10.1016/j.jocn.2017.11.009. [DOI] [PubMed] [Google Scholar]
- McCann C.P., Brandel M.G., Wali A.R., Steinberg J.A., Pannell J.S., Santiago-Dieppa D.R., Khalessi A.A. Safety of middle meningeal artery embolization for treatment of subdural hematoma: a nationwide propensity score matched analysis. J Cerebrovasc Endovasc Neurosurg. 2023 doi: 10.7461/jcen.2023.E2023.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta V., Harward S.C., Sankey E.W., Nayar G., Codd P.J. Evidence based diagnosis and management of chronic subdural hematoma: a review of the literature. J. Clin. Neurosci. 2018;50:7–15. doi: 10.1016/j.jocn.2018.01.050. [DOI] [PubMed] [Google Scholar]
- Miah I.P., Holl D.C., Blaauw J., Lingsma H.F., den Hertog H.M., Jacobs B., Kruyt N.D., van der Naalt J., Polinder S., Groen R.J.M., Kho K.H., van Kooten F., Dirven C.M.F., Peul W.C., Jellema K., Dammers R., van der Gaag N.A., Collaborators D. Dexamethasone versus surgery for chronic subdural hematoma. N. Engl. J. Med. 2023;388(24):2230–2240. doi: 10.1056/NEJMoa2216767. [DOI] [PubMed] [Google Scholar]
- Mohamed S., Villabona A., Kennion O., Padmananbhan R., Siddiqui A., Khan S., Prasad M., Mukerji N. Middle meningeal artery embolisation for chronic subdural haematomas: the first prospective UK study. Br. J. Neurosurg. 2022:1–6. doi: 10.1080/02688697.2022.2097200. [DOI] [PubMed] [Google Scholar]
- Mori K., Maeda M. Surgical treatment of chronic subdural hematoma in 500 consecutive cases: clinical characteristics, surgical outcome, complications, and recurrence rate. Neurol. Med.-Chir. 2001;41(8):371–381. doi: 10.2176/nmc.41.371. [DOI] [PubMed] [Google Scholar]
- Nia A.M., Srinivasan V.M., Lall R.R., Kan P. Middle meningeal artery embolization for chronic subdural hematoma: a national database study of 191 patients in the United States. World Neurosurg. 2021;153:e300–e307. doi: 10.1016/j.wneu.2021.06.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onyinzo C., Berlis A., Abel M., Kudernatsch M., Maurer C.J. Efficacy and mid-term outcome of middle meningeal artery embolization with or without burr hole evacuation for chronic subdural hematoma compared with burr hole evacuation alone. J. Neurointerventional Surg. 2022;14(3):297–300. doi: 10.1136/neurintsurg-2021-017450. [DOI] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., McGuinness L.A., Stewart L.A., Thomas J., Tricco A.C., Welch V.A., Whiting P., Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips B., Ball C., Sackett D., Badenoch D., Straus S., Haynes B., Dawes M., Howick J. 2009. Oxford Centre for Evidence-Based Medicine-Levels of Evidence. March 2009) [Google Scholar]
- Pichert G., Henn V. [Conservative therapy of chronic subdural hematomas] Schweiz. Med. Wochenschr. 1987;117(47):1856–1862. [PubMed] [Google Scholar]
- Piergallini L., Dargazanli C., Derraz I., Costalat V. Immediate development of dural arteriovenous fistula after middle meningeal artery embolization: first angiographic demonstration. World Neurosurg. 2019;128:606–610.e1. doi: 10.1016/j.wneu.2019.04.246. [DOI] [PubMed] [Google Scholar]
- Raviskanthan S., Mortensen P.W., Zhang Y.J., Lee A.G. Bilateral abducens nerve palsies after middle meningeal artery embolization for chronic subdural hematoma. J. Neuro Ophthalmol. 2021;42(2):e505–e507. doi: 10.1097/WNO.0000000000001305. [DOI] [PubMed] [Google Scholar]
- Salem M.M., Kuybu O., Nguyen Hoang A., Baig A.A., Khorasanizadeh M., Baker C., Hunsaker J.C., Mendez A.A., Cortez G., Davies J.M., Narayanan S., Cawley C.M., Riina H.A., Moore J.M., Spiotta A.M., Khalessi A.A., Howard B.M., Hanel R., Tanweer O., Levy E.I., Grandhi R., Lang M.J., Siddiqui A.H., Kan P., Ogilvy C.S., Gross B.A., Thomas A.J., Jankowitz B.T., Burkhardt J.K. Middle meningeal artery embolization for chronic subdural hematoma: predictors of clinical and radiographic failure from 636 embolizations. Radiology. 2023;307(4) doi: 10.1148/radiol.222045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schucht P., Fischer U., Fung C., Bernasconi C., Fichtner J., Vulcu S., Schöni D., Nowacki A., Wanderer S., Eisenring C., Krähenbühl A.K., Mattle H.P., Arnold M., Söll N., Tochtermann L., Z'Graggen W., Jünger S.T., Gralla J., Mordasini P., Dahlweid F.M., Raabe A., Beck J. Follow-up computed tomography after evacuation of chronic subdural hematoma. N. Engl. J. Med. 2019;380(12):1186–1187. doi: 10.1056/NEJMc1812507. [DOI] [PubMed] [Google Scholar]
- Shotar E., Premat K., Barberis E., Talbi A., Lenck S., Cohen C., Degos V., Sourour N.A., Mathon B., Clarençon F. Dural arteriovenous fistula formation following bilateral middle meningeal artery embolization for the treatment of a chronic subdural hematoma: a case report. Acta Neurochir. 2021;163(4):1069–1073. doi: 10.1007/s00701-020-04696-w. [DOI] [PubMed] [Google Scholar]
- Shotar E., Premat K., Lenck S., Degos V., Marijon P., Pouvelle A., Pouliquen G., Mouyal S., Abi Jaoude S., Sourour N.A., Mathon B., Clarençon F. Angiographic Anatomy of the Middle Meningeal Artery in Relation to Chronic Subdural Hematoma Embolization. Clin. Neuroradiol. 2021;32(1):57–67. doi: 10.1007/s00062-021-00996-5. [DOI] [PubMed] [Google Scholar]
- Sioutas G.S., Mouchtouris N., Saiegh F.A., Naamani K.E., Amllay A., Becerril-Gaitan A., Velagapudi L., Gooch M.R., Herial N.A., Jabbour P., Rosenwasser R.H., Tjoumakaris S.I. Middle meningeal artery embolization for subdural hematoma: an institutional cohort and propensity score-matched comparison with conventional management. Clin. Neurol. Neurosurg. 2023;233 doi: 10.1016/j.clineuro.2023.107895. [DOI] [PubMed] [Google Scholar]
- Srivatsan A., Mohanty A., Nascimento F.A., Hafeez M.U., Srinivasan V.M., Thomas A., Chen S.R., Johnson J.N., Kan P. Middle meningeal artery embolization for chronic subdural hematoma: meta-analysis and systematic review. World Neurosurg. 2019;122:613–619. doi: 10.1016/j.wneu.2018.11.167. [DOI] [PubMed] [Google Scholar]
- Starnoni D., Giammattei L., Messerer M., Daniel R.T. Letter to the editor regarding: "middle meningeal artery embolization for chronic subdural hematoma: meta-analysis and systematic review. World Neurosurg. 2019;124:480–481. doi: 10.1016/j.wneu.2018.12.138. [DOI] [PubMed] [Google Scholar]
- Tempaku A., Yamauchi S., Ikeda H., Tsubota N., Furukawa H., Maeda D., Kondo K., Nishio A. Usefulness of interventional embolization of the middle meningeal artery for recurrent chronic subdural hematoma: five cases and a review of the literature. Intervent Neuroradiol. 2015;21(3):366–371. doi: 10.1177/1591019915583224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang W., Huang J. Chronic subdural hematoma: epidemiology and natural history. Neurosurg. Clin. 2017;28(2):205–210. doi: 10.1016/j.nec.2016.11.002. [DOI] [PubMed] [Google Scholar]
- Yu J., Guo Y., Xu B., Xu K. Clinical importance of the middle meningeal artery: a review of the literature. Int. J. Med. Sci. 2016;13(10):790–799. doi: 10.7150/ijms.16489. [DOI] [PMC free article] [PubMed] [Google Scholar]