Abstract
Objective
The objective of this study was to determine the feasibility and effectiveness of using SUpported Motivational InTerviewing (SUMIT) to increase physical activity in people with knee osteoarthritis (KOA).
Design
Randomised controlled trial.
Setting
We recruited people who had completed Good Life with osteoArthritis Denmark (GLA:D) from private, public and community settings in Victoria, Australia.
Interventions
Participants were randomised to receive SUMIT or usual care. SUMIT comprised five motivational interviewing sessions targeting physical activity over 10 weeks, and access to a multimedia web-based platform.
Participants
Thirty-two participants were recruited (17 SUMIT, 15 control) including 22 females (69%).
Outcome measures
Feasibility outcomes included recruitment rate, adherence to motivational interviewing, ActivPAL wear and drop-out rate. Effect sizes (ESs) were calculated for daily steps, stepping time, time with cadence >100 steps per minute, time in bouts >1 min; 6 min walk distance, Knee Osteoarthritis Outcome Score (KOOS) subscales (pain, symptoms, function, sport and recreation, and quality of life (QoL)), Euroqual, systolic blood pressure, body mass index, waist circumference, 30 s chair stand test and walking speed during 40 m walk test.
Results
All feasibility criteria were achieved, with 32/63 eligible participants recruited over seven months; with all participants adhering to all motivational interviewing calls and achieving sufficient ActivPAL wear time, and only two drop-outs (6%).
12/15 outcome measures showed at least a small effect (ES>0.2) favouring the SUMIT group, including daily time with cadence >100 steps per minute (ES=0.43). Two outcomes, walking speed (ES= 0.97) and KOOS QoL (ES=0.81), showed a large effect (ES>0.8).
Conclusion
SUMIT is feasible in people with knee osteoarthritis. Potential benefits included more time spent walking at moderate intensity, faster walking speeds and better QoL.
Trial registration number
ACTRN12621000267853.
Keywords: knee, physical therapy modalities, rehabilitation medicine
STRENGTHS AND LIMITATIONS OF THIS STUDY.
We modified our trial by increasing recruitment sites, advertising and reducing the recruitment target number due to the impact of COVID-19 restrictions, and have reported our trial according to the Consolidated Standards or Reporting Trials and SPIRIT Extension for RCTs Revised in Extenuating Circumstances checklist to aide transparency.
We used rigorous randomisation and assessment blinding procedures and accredited motivational interviewing training and treatment fidelity so that our methods could be repeated.
Our ActivPAL analyses were completed by the same researcher who delivered the SUpported Motivational InTerviewing intervention which may present risk of unconscious bias. Future studies should provide a provision for a blinded researcher to undertake data analysis.
Our participant groups were different at baseline, possibly due to the small sample size, which may have impacted the findings for the secondary aims.
Introduction
Physical activity participation has considerable health benefits.1–3 Meeting physical activity guidelines of at least 150 min per week of moderate-vigorous physical activity is considered vital to reducing the risk of development or worsening of at least 35 chronic diseases.1–3 For people with knee osteoarthritis, less than half (41%) reach 150 min per week,4 compared with 73% of adults in the general population.5 Knee osteoarthritis and insufficient physical activity are independently associated with greater comorbidity risk, including cardiovascular disease and earlier mortality.6–8
Patient education and exercise therapy are recommended as first-line treatments for knee osteoarthritis in major guidelines,9 based on their effectiveness to reduce pain and improve knee function.10 Good Living with osteoArthritis from Denmark (GLA:D) is a guideline-based education and exercise-therapy program implemented in nine countries, including Australia.11 Participation is associated with clinically meaningful improvements in knee pain and joint-related quality of life (QoL) at 3 months, with these benefits sustained for at least 12 months.10 12 People with knee osteoarthritis completing GLA:D also report improved confidence to increase physical activity participation.13 However, completing GLA:D is not associated with increased physical activity participation at 12 months.10 13 This is consistent with a recent systematic review indicating exercise-therapy alone does not result in medium-term (6–12 months) or long-term (>12 months) changes in physical activity compared with non-exercise interventions.14
Increasing physical activity participation in people with knee osteoarthritis may require interventions to address both physical and personal barriers, such as motivation and confidence.15 Motivational interviewing is a person-centred behaviour change approach involving counselling style sessions with a trained health professional, aiming to address personal barriers to behaviour change.16 It is associated with moderate benefits for increasing physical activity in people with chronic health conditions when they present to primary care.17 However, in knee osteoarthritis, research on the effects of motivational interviewing is limited. One study reported no increase in moderate-vigorous physical activity compared with usual care in the short or long term.18 However, sessions were infrequent (every 3 months), which is atypical for motivational interviewing interventions.17 Phone counselling targeting physical activity provided more frequently (biweekly) has been reported to increase moderate-vigorous physical activity in the short term (<3 months).19
Digital support tools for osteoarthritis are emerging as a cost-effective approach to provide information and education, and assist people with osteoarthritis to engage with prescribed exercise to improve patient outcomes.20 21 In addition to behaviour change interventions, such as motivational interviewing, they can be used to monitor and/or promote physical activity, and may help to increase physical activity.22 However, the influence of digital support tools on physical activity behaviour change is unknown.22
Our primary objective was to determine the feasibility of conducting a fully powered trial evaluating the effectiveness of increasing physical activity using SUpported Motivational InTerviewing (SUMIT), following completion of an education and exercise-therapy program in people with knee osteoarthritis. Our secondary objective was to determine if a worthwhile treatment effect occurred for physical activity, physical endurance, knee-related QoL, health-related QoL and pain.
Methods
Trial design
This pilot feasibility randomised controlled trial (RCT) compared an intervention comprising motivational interviewing and website) with a usual care control group. The trial was registered with the Australian New Zealand Clinical Trials Registry (ANZCTR) (ACTRN12621000267853). Study reporting adheres to the Consolidated Standards or Reporting Trials (CONSORT) for pilot and feasibility trials.23 Due to the interruption from the COVID-19, we reported limitations according to the CONSORT and Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) Extension for RCTs Revised in Extenuating Circumstances (CONSERVE) guidelines.24
Setting
All assessments were conducted at a private hospital in metropolitan Melbourne, Australia, or a private physiotherapy clinic in regional Victoria, Australia. All intervention sessions were completed online via Zoom or phone call (according to participant preference).
Participants
Women and men with a clinical diagnosis of knee osteoarthritis25 who had completed GLA:D within the previous 2 years12 were recruited from March 2021 to April 2022 and provided written informed consent. Knee osteoarthritis was guided by the National Institute for Health and Care Excellence (NICE) guidelines including (1) being aged >45 years, (2) activity-related knee pain and (3) morning stiffness of the knee which lasts less than 30 min or no knee stiffness.25 GLA:D involves two education and 12 supervised exercise therapy sessions.12 Education covers information about osteoarthritis, treatment options, exercise and physical activity, and self-management.12 Exercise therapy includes neuromuscular, resistance training and functional exercises.12 Participants were deemed ineligible if they (1) had a comorbidity preventing them from increasing physical activity levels as assessed by the Exercise and Sports Science Australia adult prescreening tool26; (2) were not proficient in English and/or (3) had back/lower limb surgery or knee corticosteroid injection on the affected limb within 12 months prior to enrolling.
Patients and public involvement
Design of the motivational interviewing sessions took place with consultation between physiotherapists and a psychologist. Design of the multimedia website took place prior to consumer consultation. People with knee osteoarthritis were provided the website link and asked what improvements could be made to suit their needs. They also provided patient stories about their experience of the benefits of physical activity for their knee and overall health. Findings of the study will be emailed to participants. A subsequent qualitative analysis will take place to determine the acceptability of the intervention and participant ideas for improvement.
Deviations from protocol
During piloting, participants did not have a good understanding of motivational interviewing prior to the intervention. For this reason, the Borcovek and Nau acceptability questionnaire27 (online supplemental appendix 1) was removed from the protocol prior to randomisation commencement, as this tool was deemed to be unclear when answering questions about motivational interviewing. Our protocol indicated the inclusion of pain and QoL subscales from the Knee Osteoarthritis Outcome Score (KOOS); however, all five domains were included to give us a more detailed understanding of intervention outcomes. Our registration did not mention exclusion of people who had a corticosteroid injection within 12 months of recruitment; however, this criterion was included and adhered to from inception.
bmjopen-2023-075014supp001.pdf (4.4MB, pdf)
Recruitment was impacted by the COVID-19-related government restrictions, including limitations on in-person healthcare, gymnasium closures and limitations in allowable time away from personal residence for 25 weeks in 2021. As a result, we expanded the recruitment time frame from within 1 year of completing GLA:D to within 2 years. Lockdowns posed a risk of bias to either reduce (less incidental activity) or amplify (more time for exercise) our intervention. Participants who were impacted by lockdown at baseline during ActivPAL collection had their ActivPAL reapplied prior to group allocation.
Randomisation and blinding
Participants were randomised using a computer-generated program with a 1:1 ratio in permuted blocks of 4–6 and stratified by sex. Randomisation was prepared by a member of the research team not involved in assessment (MFP). Group allocations were concealed in sequentially numbered opaque envelopes, sealed until the point of group allocation. Participants were informed of their group allocation by the coordinating physiotherapist (ECB). Due to the nature of the study, the outcome assessor was the only person able to be blinded to participant allocation.
Intervention
Motivational interviewing
All participants randomised to the SUMIT group received five, 30 min sessions of motivational interviewing over a 10-week period. Sessions were conducted in weeks 1, 2, 4, 7 and 10 by an investigator trained in motivational interviewing (ECB). ECB had 5 years of experience as a physiotherapy clinician, completed a 2-day motivational interviewing course online and five 1:1 coaching sessions with a Motivational Interviewing Network Trainer and accredited psychologist (PO’H). ECB was graded proficient according to the Motivational Interviewing Treatment Integrity (MITI) assessment tool.28
Motivational interviewing sessions involved collaboration between clinician and participant aiming to evoke behaviour change to increase physical activity (online supplemental appendix 2). Consistent with the principles of motivational interviewing,13 sessions followed recommended motivational interviewing processes: engagement, focusing, evoking and planning; and were tailored to individual needs and level of preparedness for behaviour change (online supplemental appendix 2). Participant importance and confidence of engaging in physical activity was discussed over the course of the intervention, providing valuable information about shifts in potential barriers and facilitators to activity.13
Digital support tool
All participants were encouraged to access the same customised website (https://sumit.trekeducation.org/) prior to their first motivational interviewing session. The website included information about physical activity, knee osteoarthritis, goal setting, research and activities, and patient stories. Participants were encouraged to access the website prior to their first motivational interviewing session. Subsequent use was based on individual participant preference.
Control
The control group (usual care) received no additional interventions or access to the digital support tool. They were permitted to engage in routine services for their knee osteoarthritis management including visits to their general practitioner, physiotherapist or other health professionals. Participants were asked to refrain from knee steroid injections or surgery during the trial. At the conclusion of the follow-up assessments, control participants were emailed the digital support tool to access if they chose.
Outcomes
Primary: feasibility
The trial was considered feasible if all criteria were met or if reasonable amendments could be made to achieve these criteria in future trials (table 1). Recruitment, adherence and retention were calculated excluding the 6 months of COVID-19-related government restrictions during 2021.
Table 1.
Measures of feasibility
| Item | Measure of feasibility |
| Number of eligible volunteers | Minimum 2–3 participants per site, per month. Totalling 6–9 participants being eligible per month. |
| Recruitment rate | Minimum two participant per site, per month. Totalling six participants recruited per month. |
| Adherence with motivational interviewing sessions | Minimum attendance of 4/5 sessions (80%). |
| ActivPAL use | Measured by time worn per participant being >16 hours per day for 7 days (to account for waking hours). |
| Drop-out rate | <20% of participants drop out of the study. |
Adverse events
Participants were asked if they had experienced any adverse events (any injury or illness requiring medical attention as a result of participating in the trial) at the 3-month assessment.
Sample size
To test feasibility, we aimed to recruit 42 participants over 5–7 months, which accounting for drop-outs would allow analysis of at least 33 participants.
Secondary
Secondary outcomes were collected at baseline and 3 months after baseline data collection.
Device-measured physical activity
ActivPAL accelerometers (PAL Technologies, Glasgow, Scotland) were fitted to each participant’s right thigh with gauze and clear Flexifix tape for 7 days. They are reliable and valid measures of step count and cadence,29 accurate in older adults30 and do not to provide feedback to participants. We extracted average steps, minutes with cadence >100 steps per minute,31 and minutes where bouts were >1 min in duration per day. Walking cadence >100 steps per minute was chosen as an outcome since it predicts lower premature mortality in older adults, and was considered to be similar to moderate to vigorous physical activity.32
Self-reported physical activity
To triangulate accelerometer results, we also recorded physical activity using the University of California Los Angeles (UCLA) Physical Activity Scale, and the International Physical Activity Questionnaire long form (IPAQ-long). UCLA is a reliable and valid tool33 commonly used as a measure of physical activity participation in people with knee osteoarthritis.10 12 13 34 and the IPAQ long provides valuable information about the domain in which PA is undertaken.
Physical endurance
Physical endurance was measured using the 6 minute walk test (6MWT), measured in metres and reported as the six minute walk distance (6MWD), which is reliable and valid.35
Knee-related burden
The KOOS was used to measure knee pain, symptoms, function, sport and recreation and QoL.36 The questionnaire produces a score from 0 to 100 for each subscale, higher scores indicate lower burden. All subscales have high reliability and validity.36
Health-related quality of life
The EuroQoL 5-Dimension-5 Long (EQ-5D-5L) was used to measure participants health-related QoL through five domains. It is reliable, valid and responsive in osteoarthritis populations, with the index score ranging from 1 or less, with 1 being optimal health, and negative values indicating a health state worse than death.37 38
General health
Body mass index (BMI) (kg/m2), waist circumference (cm) and systolic blood pressure (BP) (mm Hg) were all recorded by a blinded research assessor.
Functional performance
The 30-second chair stand and walking speed (40 m walk) tests are both recommended by guidelines as feasible and reliable performance measures for knee osteoarthritis,39 and were completed by a blinded assessor.
Confidence and importance of physical activity
SUMIT participants were asked in weeks 2 and 10 to rate their confidence and perceived importance of changing physical activity participation on a scale from 0 to 10: where 0 is not at all important/confident and 10 is maximum importance/confidence.
Demographic data collected at baseline via Research Electronic Data Capture included age, sex, BMI, knee most affected, medication use, employment and highest level of education. An excel spreadsheet was set up to record adverse events.
Statistical analysis
Statistical analysis was performed by using SPSS V.28 (SPSS). Demographics were reported as frequencies or mean (SD). Feasibility outcomes were reported descriptively. Between group changes for continuous variables were calculated using analysis of covariance with Bonferroni adjustment and baseline measures as covariates.
The UCLA physical activity scale was dichotomised as ‘more’ and ‘less’ active, consistent with other similar studies.13 34 We defined ‘less active’ as a score of ≤6 (‘regularly participates in moderate activities, such as swimming and unlimited housework or shopping’); and defined ‘more active’ as≥7 (‘regularly participates in active events such as bicycling’) (online supplemental appendix 3). χ2 tests for independence were used to compare groups for the UCLA physical activity scale (dichotomous).
Desired treatment effects were defined using minimum detectable changes (MDC), which were set as 8–10 for all KOOS subscales,40 75 m for 6MWD,41 0.07 for health-related QoL,37 2 stands for 30 s chair stand test42 and 0.19 m per second for 40 m walk test.42 There is no documented MDC for device-measured physical activity, the IPAQ-long, UCLA physical activity scale, BMI, BP or waist circumference. Standardised mean differences (effect sizes) based on within group changes between SUMIT and control groups were calculated using Review Manager V.5.3 (The Nordic Cochrane Centre, Copenhagen, Denmark).
Confidence and importance of physical activity were reported descriptively at 2 and 10 weeks as mean (SD) using a paired t-test to determine statistical significance.
Results
Primary outcome
All feasibility criteria were met or could be achieved by using reasonable amendments in future trials (table 2).
Table 2.
Feasibility outcomes
| Criterion | Achieved | Proceed | Proceed with amendments | |
| Eligibility | ||||
| Number of eligible participants | 2–3 per site, per month, totalling 6–9 per month | 63 participants screened in 7 months accounting for lockdowns and community restrictions in Melbourne (13 months elapsed) | Yes* | Strategies to identify more eligible participants. |
| Recruitment | ||||
| Number of participants recruited | 2 participants per month, per site, totalling 6 participants per month | 32 participants recruited over 7 months (13 months elapsed) | No | Strategies to increase recruitment rate. |
| Adherence | ||||
| Adherence to motivational interviewing sessions | Minimum 4/5 sessions (80%) | 100% of motivational interviewing sessions were attended within 1 week of scheduled session time | Yes | – |
| ActivPAL | ||||
| ActivPAL wear time | >16 hours for 7 days | Malfunctioning ActivPAL uploads resulted in 3 missing ActivPAL files. | Yes | – |
| Drop-outs | ||||
| Drop-out rate | <20% | 2 drop-outs (6%), both from the control group | Yes | – |
*Proceed with protocol deviation to expand the number of recruitment sites.
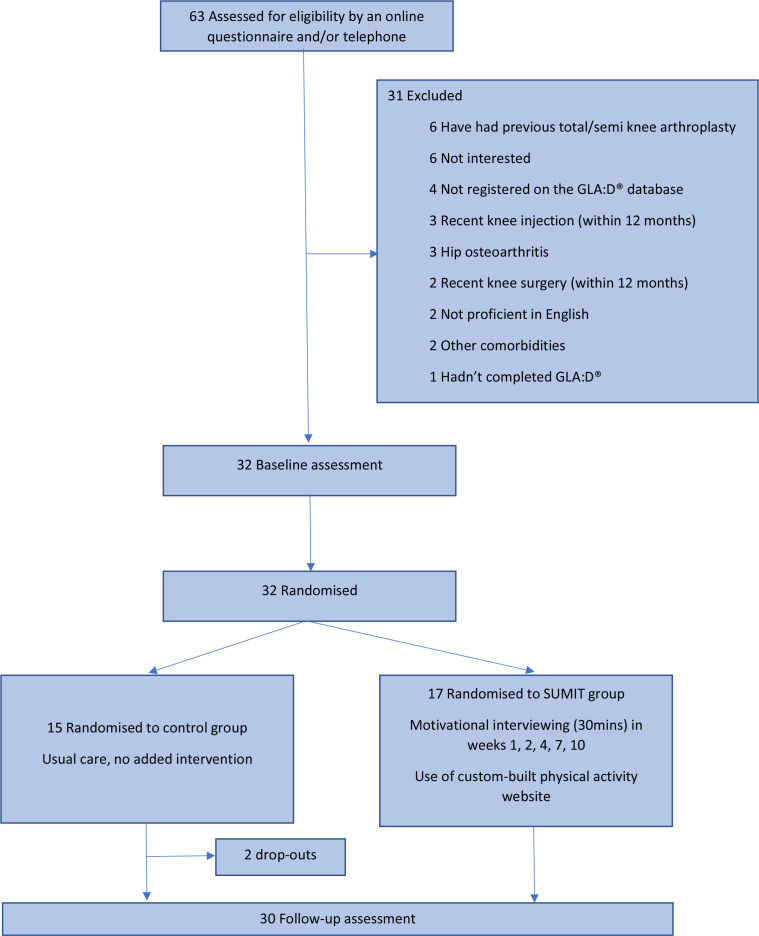
Eligibility and recruitment rates were impacted by oscillating COVID-19 lockdowns in Melbourne, Australia. We expanded recruitment time frames (from completing GLA:D within 12 months, adjusted to 24 months), and recruitment sites (from three sites to anywhere in Melbourne, Torquay or Ballarat, in Victoria, Australia) to increase our yield. Despite this, very few GLA:D programs were running effectively until April 2022. We subsequently concluded recruitment at 32 participants (instead of 42) (figure 1).
Figure 1.
Study timeline. GLA:D, Good Life with osteoArthritis Denmark, SUMIT, SUpported Motivational InTerviewing.
Sixty-nine per cent (n=22) of participants were female. Mean (SD) for BMI and waist circumference were 30.8 (6.5) kg/m2 and 101.6 (14.3) cm, respectively. A full summary of the characteristics of included participants is provided in table 3.
Table 3.
Characteristics of included participants
| Combined Mean (SD) n=32 |
SUMIT Mean (SD) n=17 |
Control Mean (SD) n=15 |
|
| Age, years | 71 (7) | 68 (5) | 73 (9) |
| Sex, female, n (%) | 22 (69%) | 11 (65%) | 11 (73%) |
| Height, m | 1.69 (0.09) | 1.69 (0.09) | 1.69 (0.10) |
| Weight, kg | 87 (17) | 92.9 (17.6) | 79.4 (13.4) |
| Recruitment | |||
| Private practice | 22 | 14 | 8 |
| Hospital | 7 | 3 | 4 |
| Community | 3 | 0 | 3 |
| Education | |||
| Completed primary school | 1 | 0 | 1 |
| Completed high school | 2 | 1 | 1 |
| Completed an apprenticeship | 0 | 0 | 0 |
| Completed certificate | 4 | 1 | 3 |
| Completed diploma | 2 | 1 | 1 |
| Completed undergraduate degree | 10 | 4 | 6 |
| Completed postgraduate degree | 9 | 4 | 5 |
| Not reported | 4 | 4 | 0 |
| Time elapsed since completing GLA:D, months | 11 (8) | 11 (9) | 10 (7) |
| Not reported, n | 5 | 4 | 1 |
Two (6%) participants dropped out of the trial prior to receiving their group allocation. One participant cited concern to be in public places due to the high ongoing risk of contracting COVID-19 and the other cited lack of time. One participant from the SUMIT group was not able to complete their follow-up ActivPAL collection due to COVID-19 lockdown timing and subsequent need for surgery, missing the follow-up period. Two participants at baseline and four participants at follow-up were undergoing ActivPAL monitoring at a time when new movement restrictions were announced (ie, COVID-19 lockdowns). In these instances, monitoring was ceased, then restarted following the removal of movement restrictions.
No participants in either group experienced any adverse events as a result of data collection or the intervention during the trial. Two participants in the SUMIT group reported back pain prior to the trial and continued to experience back pain during the intervention period. One participant in the SUMIT group had a fall 1 week prior to follow-up, reducing their ability to participate in physical activities during the ActivPAL recording week.
Secondary outcomes
The desired treatment effect was contained within the 95% CI for all KOOS subscales, health-related QoL and walking speed (table 4, online supplemental appendices 7–10). An MDC was achieved for KOOS pain and QoL subscales, and health-related QoL (table 4, online supplemental appendices 7a,e and 8). The desired treatment effect was not met for 6MWD or 30 s chair stand test (table 4, online supplemental appendices 6,10b). Detailed findings are provided in online supplemental appendices 4–10.
Table 4.
Within and between group differences for all secondary outcomes
| Outcome |
Within group differences |
Within group differences | Between group differences | |||||
| Week 0 | Week 12 | week 12 minus Week 0 | Week 0 | Week 12 | week 12 minus Week 0 | Week 12 SUMIT minus control | ||
| SUMIT Mean (SD) n=17 |
SUMIT Mean (SD) n=17 |
SUMIT MD (SD) n=17 |
Control Mean (SD) n=13 |
Control Mean (SD) n=13 |
Control MD (SD) n=13 |
MD (95% CI), P value | Previously published MDC values | |
| Steps per day | 7209 (3159) | 7213 (2681) | 4 (1308) | 7484 (2903)* | 7676 (2773)* | 192 (1627)* | 247 (−1264 to 769), 0.62 | N/A |
| Daily stepping time | 92 (37) | 92 (32) | 0.6 (16) | 98 (37)* | 103 (40)* | 5 (18)* | 7 (−19 to 6), 0.30 | N/A |
| Daily time with cadence >100 spm | 7 (9) | 15 (12) | 8 (9) | 7 (9)* | 10 (10)* | 3 (14)* | 5 (−0.4 to 11), 0.67 | N/A |
| Daily time with bouts >1 min | 23 (19) | 52 (20) | 29 (13) | 23 (19)* | 44 (29)* | 21 (24)* | 8 (−6 to 21), 0.27 | N/A |
| IPAQ bike | 21 (42)* | 8 (30)* | 13 (55)* | 9 (33) | 0 (0) | 9 (33) | 8 (−9 to 26), 0.35 | N/A |
| IPAQ walk | 299 (507)* | 187 (224)* | 112 (556)* | 205 (387) | 171 (370) | 34 (72) | 11 (−220 to 197), 0.91 | N/A |
| IPAQ gardening (vig) | 84 (178)* | 41 (95)* | 43 (196)* | 92 (198) | 83 (96) | 9 (198) | 41 (−115 to 32), 0.26 | N/A |
| IPAQ gardening (mod) | 252 (429)* | 61 (83)* | 191 (398)* | 156 (253) | 157 (186) | 1 (328) | 101 (−209 to 7), 0.07 | N/A |
| IPAQ housework | 215 (359)* | 217 (318)* | 2 (144)* | 353 (301) | 167 (225) | 187 (368) | 123 (−50 to 297), 0.16 | N/A |
| IPAQ leisure walking | 94 (140)* | 157 (236)* | 63(245)* | 142 (210) | 183 (91) | 41 (183) | 12 (−154 to 130), 0.89 | N/A |
| IPAQ leisure (vig) | 37 (52)* | 27 (72)* | 10 (47)* | 39 (81) | 5 (17) | 35 (73) | 23 (−14 to 59), 0.21 | N/A |
| IPAQ leisure (mod) | 15 (30)* | 52 (76)* | 37 (75)* | 51 (98) | 59 (78) | 8 (110) | 2 (−59 to 62), 0.96 | N/A |
| 6MWD, m | 484 (114)* | 503 (102)* | 19 (53)* | 525 (97) | 527 (106) | 2 (40) | 11 (−25 to 48), 0.52 | 75 m (44) |
| KOOS pain | 67 (16)* | 79 (15)* | 12 (13)*† | 74 (14) | 76 (14) | 2 (13) | 8 (−3 to 18), 0.14† | 8–10 points (43) |
| KOOS symptoms | 65 (12)* | 74 (13)* | 9 (11)* | 74 (11) | 77 (14) | 2 (16) | 2 (−9 to 13), 0.73 | 8–10 points (43) |
| KOOS function | 70 (19)* | 83 (12)* | 14 (15)* | 78 (12) | 81 (15) | 3 (12) | 7 (−3 to 16), 0.16 | 8–10 points (43) |
| KOOS sport and recreation | 37 (19)* | 52 (21)* | 14 (21)* | 45 (29) | 58 (29) | 14 (28) | 2 (−20 to 16), 0.81 | 8–10 points (43) |
| KOOS QoL | 47 (20)* | 60 (20)* | 13 (11)*† | 54 (18) | 55 (20) | 1 (17) | 10 (−2 to 22), 0.09† | 8–10 points (43) |
| EQ5D | 0.69 (0.22)* | 0.79 (0.12)* | 0.10 (0.23)*† | 0.77 (0.10 | 0.74 (0.11) | 0.03 (0.13) | 0.07 (−0.03 to 0.16), 0.15 | 0.07 (40) |
| Body mass index, kg/m2 | 33 (7)* | 33 (6)* | 0.0 (0.8)* | 28 (6) | 28 (6) | 0.1 (0.4) | 0.3 (−0.2 to 0.8), 0.23 | N/A |
| Systolic blood pressure, mm Hg | 138 (15)* | 131 (11)* | 7 (12) | 135 (10) | 132 (15) | 3 (14) | 3 (−11 to 6), 0.56 | N/A |
| Waist circumference, cm | 106 (14)* | 106 (14)* | 0.3 (5.2)* | 95 (13) | 98 (13) | 2.5 (4.8) | 1.4 (−5.6 to 2.7), 0.47 | N/A |
| 30 s chair stand test | 12 (2)* | 12 (3)* | 1 (1)* | 12 (2) | 12 (2) | 0 (2) | 0.5 (−0.8 to 1.7), 0.44 | 2 stands (45) |
| Walking speed, m/s | 1.5 (0.3)* | 1.7 (0.4)* | 0.1 (0.2) | 1.7 (0.5) | 1.7 (0.4) | 0.1 (0.2) | 0.15 (−0.01 to 0.31), 0.06 | 0.19 m/s (45) |
Bold denotes CIs which include the defined minimal detectable change.
†Mean difference achieved a minimal detectable change.
*Mean difference achieved a minimal detectable change
EQ5D, Euro QoL 5-Dimension; IPAQ, International Physical Activity Questionnaire; KOOS, Knee Osteoarthritis Outcome Score; MD, mean difference; MDC, minimal detectable change; 6MWD, 6-minute min walk distance; N/A, not applicable; QOL, quality of life; SUMIT, SUpported Motivational InTerviewing; vig, vigorous.
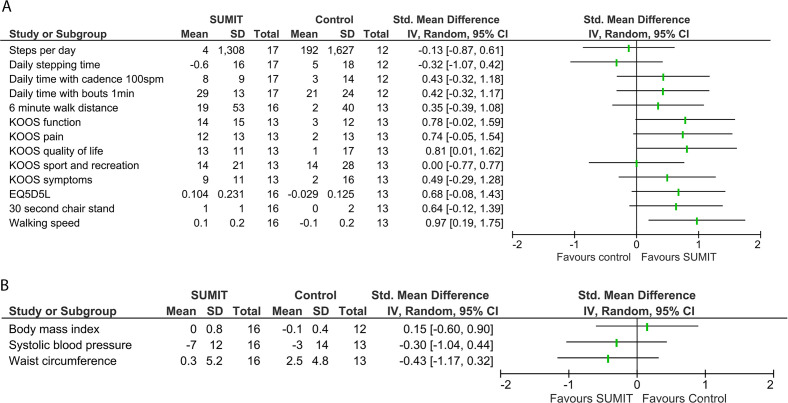
Overall, 10 of the 13 outcome measures (figure 2A) and 2 of the 3 health outcomes (figure 2B) showed at least a small effect favouring the SUMIT group, including 2 outcomes (walking speed and KOOS QoL) showing a large effect.
Figure 2.
(A) Forest plot comparing within group change scores between SUMIT and control groups. (B) Forest plot comparing within group change scores between SUMIT and control groups for health outcomes. EQ5D5L, Euroqual 5-Dimension 5-Level; IV, inverse variance; KOOS, Knee Osteoarthritis Outcome Score; SUMIT, SUpported Motivational InTerviewing.
The proportion of ‘more’ active participants was 18% and 31% at baseline for SUMIT and control groups, respectively (χ2=0.71, p=0.40), and 31% and 8% at 3 months (χ2=0.99, p=0.31) (online supplemental appendix 5a–c).
For the SUMIT group, both perceived confidence and importance of participating in regular physical activity improved between week 2 and week 10, mean (SD): 7.1 (2.2) to 8.8 (0.8) (p=0.002) and 8.6 (0.8) to 9.4 (0.9) (p=0.006), respectively.
Discussion
Our findings suggest that it is feasible to proceed to a large-scale RCT to evaluate the effectiveness of motivational interviewing, supported by a digital support tool, on physical activity in people with knee osteoarthritis. All feasibility criteria were either met or could be reasonably altered to be met in future trials. Of those who were screened, more than half were eligible (59%), with a modest recruitment rate achieved (four per month). The drop-out rate was 6% which is considered acceptable.43 However, community restrictions including lockdowns imposed in Melbourne during the trial44 led to the need to broaden recruitment sources, and delays to assessments. Notably, the number of GLA:D completers dramatically reduced during our recruitment period due to restrictions on in-person care, an unlikely problem in future trials. Our adherence was high (100%), which may be attributed to the flexibility of the booking schedule and options (phone or Zoom) provided, a feature that should be adopted in future trials.
The desired treatment effects potentially favouring the intervention in this pilot study were contained within the 95% CI for most clinical outcomes. However, steps per day and daily stepping time outcomes favoured the control group. This should be considered in the context of greater improvement in walking speed (40 m walk test) and fitness (6MWD) at follow-up and increased time spent walking at a cadence of >100 steps per minute or completing daily bouts of physical activity >1 min during the intervention period for the SUMIT group. Combined, these findings may indicate the intervention led to capacity to cover ground in less time, and possible improvement in moderate intensity physical activity following the intervention.31 The SUMIT group reached an average of 15 min per day walking with a cadence >100 steps per minute at 3 months, achieving the threshold to reduce all-cause mortality.45
Additional outcomes favouring the intervention group with moderate to large effects included KOOS symptoms, pain, function and QoL, EQ-5D-5L, 30 s chair stand test, and systolic BP. Health-related QoL and BP are particularly notable as they indicate that the intervention may be associated with improved general health, which would need to be tested in a larger trial. The large effect observed in favour of the SUMIT group for KOOS QoL may be related to benefits experienced due to motivational interviewing or could be related to regular contact with a health professional during COVID-19.
While our study showed promising effect sizes favouring the intervention, it was not powered to find between group differences. The lack of between group differences may also be accounted for by differences in baseline characteristics which favoured our control group. There is no recommended dose for motivational interviewing,17 however, it is possible that our intervention did not include enough sessions to see a substantial difference between groups. Our intervention included five sessions compared with other studies which have reported that 8-weekly motivational interviewing calls resulted in meaningful differences in people with hip fractures.46 It is possible that our participants’ physical activity was influenced by COVID-19 restrictions/lockdowns.47 The impact may have had mixed effects, including physical activity being negatively influenced by lower incidental activities, and safety concerns of being outside the home.48 Conversely, physical activity may have increased for others during COVID-19 restrictions due to increased time and opportunity to access outside activities.48 Our results contrast another motivational interviewing RCT which reported no difference in physical activity between groups, which may be explained by our motivational interviewing sessions being delivered closely together, allowing participants to reinforce behaviour change more effectively.18 However, improvements in pain and function in this RCT were consistent with our findings, which may be attributed to therapeutic contact with a health professional.
Findings of our study should be interpreted within the context of its strengths and limitations. We modified our trial by increasing recruitment sites, advertising and reducing the recruitment target number due to the impact of COVID-19 restrictions, and have reported our trial according to the CONSERVE checklist to aide transparency. At baseline, our participants in both groups were completing 7000–7500 steps, which may be already adequate to maintain good health,49 and potentially challenging to increase. Further increases in physical activity in those already more active are still likely to improve health,50 51 and increasing cadence50 51 during walking as occurred in our intervention group also provides additional health benefits. However, future RCTs may consider targeting ‘less’ active participants where there is a greater potential for improvement in physical activity participation and health benefits. People who have completed GLA:D report being more confident to participate in physical activities,13 therefore, we chose to include this subset of the knee osteoarthritis population. It is important to note that this group has been willing to participate in an exercise-based intervention previously, and in many cases paid out of pocket and/or claimed private health insurance to support their participation. This selection bias may limit the external applicability of our findings to the broader knee osteoarthritis population. Recruiting for SUMIT following GLA:D participation may be more successful due to their change in perception towards physical activity.13 Nonetheless, our findings indicate SUMIT may be effective and feasible following a widely implemented education and exercise therapy program (ie, GLA:D), which as at December 2022 had been provided to 12 884 people with osteoarthritis in Australia.52 Our participant groups were different at baseline, possibly due to the small sample size, which may have impacted the findings for the secondary aims. We used rigorous randomisation and assessment blinding procedures, and accredited motivational interviewing training and treatment fidelity so that our methods could be repeated. Our ActivPAL analyses were completed by the same researcher who delivered the SUMIT intervention which may present risk of unconscious bias. Future studies should provide a provision for a blinded researcher to undertake data analysis.
Our pilot feasibility trial allowed us to identify areas for improvement in a large-scale RCT. Partnering with high volume GLA:D clinics would enable early identification of eligible participants, and direct recruitment for completers. Trial advertising may increase the number of potential participants self-identifying and being screened. Our intervention may be improved by introducing adjunct accountability methods such as a downloadable self-monitoring tool (eg, spreadsheet via our SUMIT digital support tool) or formal goal setting tools.53 We recommend that future trials use a longer follow-up period to track effectiveness of the intervention on physical activity. Adding booster motivational interviewing sessions have effectively increased physical activity in other musculoskeletal conditions,54 and are encouraged in future knee osteoarthritis trials.55
Conclusion
Our study found that motivational interviewing and a web-based multimedia platform are feasible to target physical activity in people with knee osteoarthritis. Secondary findings indicate this intervention may be associated with improved moderate physical activity, but this requires testing in a larger high-quality RCT. We have provided recommendations to improve future trials including refining recruitment strategies, reducing participant burden and optimising motivational interviewing dose.
Supplementary Material
Acknowledgments
We would like to thank Complete Sports Care, Lake Health Group, Offshore Physiotherapy Access Health & Community, and Cabrini Health for their contribution and assistance with recruitment. We would like to thank our participants for their time.
Footnotes
Twitter: @millybelly4
Correction notice: This article has been corrected since it was first published. Affiliation has been updated for 'Emily Catherine Bell' and 'Christian J Barton'.
Contributors: ECB and CJB took responsibility for the integrity of the data and correctness of the data analysis, including being joint responsible for the overall content as the guarantors. ECB is a PhD candidate and this trial is contributing to her doctoral dissertation. Concept and Design: ECB, CJB, PO'H and JAW; Acquisition of the data: ECB, research assistants; analysis or interpretation of the data: all; Drafting of the manuscript: ECB, PO'H, JAW, CJB and KMC; Critical revision of the manuscript: all; Obtained funding: All.
Funding: This study is supported by a La Trobe University Postgraduate Stipend (ECB). This trial was supported by a Cabrini Foundation Research Grant to the value of AUD$29 999.65 and Arthritis Australia to the value of AUD$10 000. The remaining funds required were supported by in-kind funds from La Trobe University.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by La Trobe University Human Research Ethics Committee #20506. Participants gave informed consent to participate in the study before taking part.
References
- 1.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distictions for health-related research. Public Health Rep 1985;100:126–31. [PMC free article] [PubMed] [Google Scholar]
- 2.Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol 2012;2:1143–211. 10.1002/cphy.c110025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: WHO Press, 2009. [Google Scholar]
- 4.Wallis JA, Webster KE, Levinger P, et al. What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta-Anaylsis. Osteoarthritis and Cartilage 2013;21:1648–59. 10.1016/j.joca.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 5.Australian Bureau of Statistics . Physical activity. 2022. Available: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/physical-activity/latest-release
- 6.Wallis JA, Webster KE, Levinger P, et al. Perceptions about participation in a 12-week walking program for people with severe knee osteoarthritis: a qualitative analysis. Disabil Rehabil 2019;41:779–85. 10.1080/09638288.2017.1408710 [DOI] [PubMed] [Google Scholar]
- 7.Veronese N, Cereda E, Maggi S, et al. Osteoarthritis and mortality: a prospective cohort study and systematic review with meta-analysis. Semin Arthritis Rheum 2016;46:160–7. 10.1016/j.semarthrit.2016.04.002 [DOI] [PubMed] [Google Scholar]
- 8.Nüesch E, Dieppe P, Reichenbach S, et al. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ 2011;342:d1165. 10.1136/bmj.d1165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Royal Australian College of General Practitioners . Guideline for the management of knee and hip osteoarthritis. 2018. Available: https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/knee-and-hip-osteoarthritis
- 10.Skou ST, Roos EM. Good life with osteoArthrisi in Denmark (GLA:DTM): evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Musculoskelet Disord 2017;18:72. 10.1186/s12891-017-1439-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.GLA:D® Australia . Annual report 2019. 2019. Available: https://gladaustralia.com.au/wp-content/uploads/2020/10/GLAD-ANNUAL-REPORT-2019.pdf
- 12.Barton CJ, Kemp JL, Roos EM, et al. Program evaluation of GLA:D® Australia: physiotherapist training outcomes and effectiveness of implementation for people with knee osteoarthritis. Osteoarthr Cartil Open 2021;3:100175. 10.1016/j.ocarto.2021.100175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bell EC, O’Halloran P, Pazzinatto MF, et al. “I feel more confident”: a mixed-methods evaluation of the influence of good life with osteoarthritis Denmark (Gla:D®) on physical activity participation, capability, barriers and facilitators in people with knee osteoarthritis. Osteoarthritis and Cartilage 2023;31:S388–9. 10.1016/j.joca.2023.01.445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bell EC, Wallis JA, Goff AJ, et al. Does land-based exercise-therapy improve physical activity in people with knee osteoarthritis? A systematic review with meta-analyses. Osteoarthritis and Cartilage 2022;30:1420–33. 10.1016/j.joca.2022.07.008 [DOI] [PubMed] [Google Scholar]
- 15.Kanavaki AM, Rushton A, Efstathiou N, et al. Barriers and facilitators of physical activity in knee and hip osteoarthritis: a systematic review of qualitative evidence. BMJ Open 2017;7:e017042. 10.1136/bmjopen-2017-017042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller W, Rollnick S. Motivational interviewing: helping people change. 3rd ed. New York: The Guilford Press, 2013. [Google Scholar]
- 17.O’Halloran PD, Blackstock F, Shields N, et al. Motivational interviewing to increase physical activity in people with chronic health conditions: a systematic review and meta-analysis. Clin Rehabil 2014;28:1159–71. 10.1177/0269215514536210 [DOI] [PubMed] [Google Scholar]
- 18.Gilbert AL, Lee J, Ehrlich-Jones L, et al. A randomized trial of a motivational interviewing intervention to increase lifestyle physical activity and improve self-reported function in adults with arthritis. Semin Arthritis Rheum 2018;47:732–40. 10.1016/j.semarthrit.2017.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li LC, Feehan LM, Xie H, et al. Effects of a 12-week multifaceted wearable-based program for people with knee osteoarthritis: randomized controlled trial. JMIR Mhealth Uhealth 2020;8:e19116. 10.2196/19116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ekman B, Nero H, Lohmander LS, et al. Costing analysis of a digitial first-line treatment platform for patients with knee and hip osteoarthritis in Sweden. PLoS ONE 2020;15:e0236342. 10.1371/journal.pone.0236342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gao Z, Lee J. Emerging technology in promoting physical activity and health: challenge and opportunities. JCM 2019;8:1830. 10.3390/jcm8111830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hinman RS, Lawford BJ, Nelligan RK, et al. Virtual tools to enable management of knee osteoarthritis. Curr Treatm Opt Rheumatol 2023;2023:1–21. 10.1007/s40674-023-00202-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355:i5239. 10.1136/bmj.i5239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Orkin AM, Gill PJ, Ghersi D, et al. Guidelines for reporting trial protocols and completed trials modified due to the COVID-19 pandemic and other extenuating circumstances. JAMA 2021;326:257. 10.1001/jama.2021.9941 [DOI] [PubMed] [Google Scholar]
- 25.National Institute for Health and Clinical Excellence . NICE guideline on osteoarthritis: the care and management of osteoarthritis in adults. 2014. [Google Scholar]
- 26.Exercise & Sports Science Australia . Adult pre-exercise screening system (APSS) V2. 2019. Available: https://www.essa.org.au/Public/ABOUT_ESSA/Pre-Exercise_Screening_Systems.aspx
- 27.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry 2000;31:73–86. 10.1016/s0005-7916(00)00012-4 [DOI] [PubMed] [Google Scholar]
- 28.Moyers TB, Rowell LN, Manuel JK, et al. The motivational interviewing treatment integrity code (MITI 4): rationale, preliminary reliability and validity. J Subst Abuse Treat 2016;65:36–42. 10.1016/j.jsat.2016.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ryan CG, Grant PM, Tigbe WW, et al. The validity and reliability of a novel activity monitor as a measure of walking. Br J Sports Med 2006;40:779–84. 10.1136/bjsm.2006.027276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grant PM, Dall PM, Mitchell SL, et al. Activity-monitor accuracy in measuring step number and cadence in community-dwelling older adults. J Aging Phys Act 2008;16:201–14. 10.1123/japa.16.2.201 [DOI] [PubMed] [Google Scholar]
- 31.Tudor-Locke C, Han H, Aguiar EJ, et al. How fast is fast enough? Walking cadence (steps/min) as a practical estimate of intensity in adults: a narrative review. Br J Sports Med 2018;52:776–88. 10.1136/bjsports-2017-097628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brown JC, Harhay MO, Harhay MN. Walking cadence and mortality among community-dwelling older adults. J Gen Intern Med 2014;29:1263–9. 10.1007/s11606-014-2926-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Terwee CB, Bouwmeester W, van Elsland SL, et al. Instruments to assess physical activity in patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Osteoarthritis and Cartilage 2011;19:620–33. 10.1016/j.joca.2011.01.002 [DOI] [PubMed] [Google Scholar]
- 34.Bell EC, Pazzinatto MF, Wallis JA, et al. Association of baseline physical activity participation with participant characteristics and outcomes following education and exercise-therapy in people with knee osteoarthritis: a GLA:D® Australia prospective cohort study. Musculoskeletal Care 2023. 10.1002/msc.1828 [Epub ahead of print 5 Oct 2023]. [DOI] [PubMed] [Google Scholar]
- 35.Ateef M, Kulandaivelan S, Tahseen S. Test–retest reliability and correlates of 6-minute walk test in patients with primary osteoarthritis of knees. Indian J Rheumatol 2016;11:192. 10.4103/0973-3698.192668 [DOI] [Google Scholar]
- 36.Collins NJ, Prinsen CAC, Christensen R, et al. Knee injury and osteoarthritis outcome score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthritis and Cartilage 2016;24:1317–29. 10.1016/j.joca.2016.03.010 [DOI] [PubMed] [Google Scholar]
- 37.Bilbao A, García-Pérez L, Arenaza JC, et al. Psychometric properties of the EQ-5D-5L in patients with hip or knee osteoarthritis: reliability, validity and responsiveness. Qual Life Res 2018;27:2897–908. 10.1007/s11136-018-1929-x [DOI] [PubMed] [Google Scholar]
- 38.Busija L, Ackerman IN, Haas R, et al. Adult measures of general health and health-related quality of life (invited). Arthritis Care Res (Hoboken) 2020;72 Suppl 10:522–64. 10.1002/acr.24216 [DOI] [PubMed] [Google Scholar]
- 39.Dobson F, Hinman RS, Hall M, et al. Measurement properties of performance-based measures to assess physical function in hip and knee osteoarthritis: a systematic review. Osteoarthritis and Cartilage 2012;20:1548–62. 10.1016/j.joca.2012.08.015 [DOI] [PubMed] [Google Scholar]
- 40.Roos EM, Lohmander LS. The knee injury and osteoarthritis outcome score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 2003;1:64. 10.1186/1477-7525-1-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Benaim C, Blaser S, Léger B, et al. "Minimal clinically important difference" estimates of 6 commonly-used performance tests in patients with chronic musculoskeletal pain completing a work-related multidisciplinary rehabilitation program. BMC Musculoskelet Disord 2019;20:16. 10.1186/s12891-018-2382-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dobson F, Hinman RS, Hall M, et al. Reliability and measurement error of the osteoarthritis research society International (OARSI) recommended performance-based tests of physical function in people with hip and knee osteoarthritis. Osteoarthritis and Cartilage 2017;25:1792–6. 10.1016/j.joca.2017.06.006 [DOI] [PubMed] [Google Scholar]
- 43.Furlan AD, Pennick V, Bombardier C, et al. 2009 updated method guidelines for systematic reviews in the Cochrane back review group. Spine (Phila Pa 1976) 2009;34:1929–41. 10.1097/BRS.0b013e3181b1c99f [DOI] [PubMed] [Google Scholar]
- 44.Victorian Department of Health . Pandemic order register 2022. n.d. Available: https://www.health.vic.gov.au/covid-19/pandemic-order-register
- 45.Wen CP, Wai JPM, Tsai MK, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet 2011;378:1244–53. 10.1016/S0140-6736(11)60749-6 [DOI] [PubMed] [Google Scholar]
- 46.O’Halloran PD, Shields N, Blackstock F, et al. Motivational interviewing increases physical activity and self-efficacy in people living in the community after hip fracture: a randomized controlled trial. Clin Rehabil 2016;30:1108–19. 10.1177/0269215515617814 [DOI] [PubMed] [Google Scholar]
- 47.Stockwell S, Trott M, Tully M, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med 2021;7:e000960. 10.1136/bmjsem-2020-000960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Park AH, Zhong S, Yang H, et al. Impact of COVID-19 on physical activity: a rapid review. J Glob Health 2022;12:05003. 10.7189/jogh.12.05003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee I-M, Shiroma EJ, Kamada M, et al. Association of step volume and intensity with all-cause mortality in older women. JAMA Intern Med 2019;179:1105–12. 10.1001/jamainternmed.2019.0899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Del Pozo Cruz B, Ahmadi MN, Lee I-M, et al. Prospective associations of daily step counts and intensity with cancer and cardiovascular disease incidence and mortality and all-cause mortality. JAMA Intern Med 2022;182:1139–48. 10.1001/jamainternmed.2022.4000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Saint-Maurice PF, Troiano RP, Bassett DR, et al. Association of daily step count and step intensity with mortality among US adults. JAMA 2020;323:1151. 10.1001/jama.2020.1382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Crossley K, Barton C, Kemp J, et al. GLA:D® Australia 2022 annual report. 2022. [Google Scholar]
- 53.Whittaker JL, Truong LK, Losciale JM, et al. Efficacy of the SOAR knee health program: protocol for a two-arm stepped-wedge randomized delayed-controlled trial. BMC Musculoskelet Disord 2022;23:85. 10.1186/s12891-022-05019-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fjeldsoe B, Neuhaus M, Winkler E, et al. Systematic review of maintenance of behavior change following physical activity and dietary interventions. Health Psychol 2011;30:99–109. 10.1037/a0021974 [DOI] [PubMed] [Google Scholar]
- 55.Lilienthal KR, Pignol AE, Holm JE, et al. Telephone-based motivational interviewing to promote physical activity and stage of change progression in older adults. J Aging Phys Act 2014;22:527–35. 10.1123/japa.2013-0056 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-075014supp001.pdf (4.4MB, pdf)
Data Availability Statement
Data are available on reasonable request.