Abstract
Background
A rare disease is a health condition that rarely occurs in the population. It is estimated that up to 400 million people around the world suffer from a rare disease. This retrospective study aimed to investigate factors associated with length of hospitalization in 78 626 patients with sarcoidosis, 3294 patients with adults-onset Still’s disease, and 35 549 patients with systemic sclerosis between 2009 and 2018 using data from the National Institute of Public Health in Poland.
Material/Methods
In this population-based study, we analyzed hospital discharge records of first-time and subsequent hospitalizations. To perform the statistical analyses, R software was used.
Results
The average length of hospitalization over the selected period in the diseases was 5.39 days for sarcoidosis, 6.22 days for scleroderma, and 7.44 days for Still’s disease, and was shorter for each of the diseases analyzed compared with the length of hospitalization for second and subsequent stays. There were no substantial differences in length of hospitalization between males and females. The average length of hospitalization increased with each additional comorbidity.
Conclusions
The study showed that hospitalizations for selected rare diseases do not cause a significant burden on the healthcare system. The results also showed that advanced age and comorbidities are important factors determining the length of hospitalization. The average length of hospital stay for selected rare diseases in Poland is not longer than the European Union (EU) average, so it can be assumed that the process of inpatient treatment in Poland is optimal.
Keywords: Length of Stay; Rare Diseases; Registries; Sarcoidosis; Scleroderma, Systemic; Still’s Disease, Adult-Onset
Background
A rare disease (RD) is a health condition that rarely occurs in the population; it is most often genetically determined and characterized by a chronic course, which is often severe [1]. Rare diseases have high rates of mortality, hospital admission, and readmission, and high cost of illness [2]. According to a report by the Professional Society for Health Economics and Outcomes Research (ISPOR), there are 112 definitions of the term rare disease worldwide. The main difference between the definitions is the threshold of morbidity and reference to a medical condition, disability, or genetic condition of the disease [3]. Most often, low prevalence is taken as prevalence of less than 5 per 10 000 in the community [4].
It is estimated that up to 400 million people around the world (6–8% of the population) have a rare disease [5]. Considering the incidence of rare diseases exclusively in the European Union, 27–36 million Europeans, and 2.3–3 million Poles have rare diseases [5]. Information collected by the National Health Fund show that rare diseases have been diagnosed in 1.6 million persons in Poland (2019) [5]. A noticeable difference in the statistics may indicate either a lower level of the diagnosis of rare diseases than in other countries, or it may result from an inaccuracy of the data collection in this group of patients. There are no specific epidemiological data on rare diseases in Poland. However, indirect data are available, and they are analyzed in scientific publications, such as by the Department of Social Medicine and Public Health at the Medical University of Warsaw [6–8].
In the European Union legislation, rare diseases gained special status on 29 April 1999, when the European Commission began a program of community action on rare diseases within the framework for action in the field of public health [9]. Regulation No. 141/2000 of the European Parliament and of the Council of 16 December 1999 states that patients suffering from rare conditions should be entitled to the same quality of treatment as other patients. Pursuant to the Decision of the European Parliament and the EU Council (No. 1350/2007/EC), the EU Council Recommendation of 8 June 2009 on an action in the field of rare diseases (2009/C 151/02) was issued, which recommends that Member States establish and implement plans for rare diseases [9]. As a result, the National Plan for Rare Diseases was instituted in Poland on 24 August 2021 [10]. That document is a tool to ensure a sustainable health policy focused on the needs of patients with rare diseases. It introduces systemic solutions to health and social problems of patients with rare diseases [9].
Ever-increasing healthcare costs and demands for high-quality care call for appropriate and effective solutions for calculating and lowering costs of treatment, including treatment of rare diseases. Direct costs related to treatment expenses are variable, and depend on the number of services provided. Due to unavailability of data on cost and labor intensity in cost estimation, less accurate methods are used to assess the expenditure on the treatment of patients, such as per-day cost of a patient’s hospital stay [11].
Hospitals account for a significant amount of global healthcare spending due to the complex and specialized care that they provide. Hospital length of stay (LOS) has been studied since the 1970s for use as metric to increase performance and improve quality [12].
Patient’s length of stay in a hospital is one of the main performance measures frequently used to evaluate hospital effectiveness. It is frequently used to determine resource utilization, cost, and sickness severity. If all else is equal, a shorter stay will result in lower per-discharge costs and a movement of treatment from expensive inpatient facilities to less expensive post-acute ones. The use of LOS as an effectiveness measure is therefore based on the assumption that the lower the LOS, the greater the hospital’s efficiency [13].
The use LOS as an effectiveness metric is supported by findings that many patient days in hospitals are inappropriate [14]. Prolonged length of stay is linked to higher incidence of medical issues, which add to costs and further delay hospital discharge [15].
LOS is calculated as the total number of days spent in hospital following a single admission event [16]. Although straightforward in calculation, patient’s length of stay in hospital is influenced by a variety of factors, including health care systems’ characteristics, patients’ characteristics, social and family characteristics, health care professionals’ (HCP) characteristics, LOS and related complications, and patient satisfaction [13]. Several factors of hospital organization affect patient’s length of stay. LOS can be influenced by admission services (emergency or elective admissions), time of admission (weekend or afterhours admission result in greater LOS), bed availability, or development of clinical pathways. Older age and comorbidities are also associated with prolonged bed use [13].
A similar metric, average length of stay in hospitals (ALOS), is often calculated by dividing the sum of all inpatient days in a year by the total number of admissions or discharges. ALOS for acute care in Poland is 6.8 days, placing it somewhere in the middle of both OECD (Organization for Economic Cooperation and Development) countries (the shortest length of stay has been observed for Turkey with 4.5 days and the longest one for Japan with 16.4 days) and EU countries (the shortest ALOS has been registered in the Netherlands: 5.2 days and the longest in Portugal: 9.8 days) [17].
Rare diseases constitute a significant public health problem due to the frequency of hospitalization as compared to other diseases or health problems. Therefore, it is worth performing analyses and scientific investigations regarding the burden of hospitalization of patients with rare diseases on the health care system.
Therefore, this retrospective study aimed to investigate factors associated with length of hospitalization in 78 626 patients with sarcoidosis, 3294 patients with adults-onset Still’s disease, and 35 549 patients with systemic sclerosis between 2009 and 2018 using data from the National Institute of Public Health in Poland.
Objectives
Rare diseases, due to their specificity, require a separate approach in terms of predictive factors affecting the duration of hospitalization.
The main aim of this study was to identify selected predictive factors and the length of stay in selected rare autoimmune diseases in Poland. Considering the previous cycle of epidemiology research, this study included the analysis of sarcoidosis [6], systematic sclerosis [7] and adult-onset Still’s disease [8]. The secondary aim was to verify the average length of hospitalization for selected rare diseases in Poland as compared with the EU average.
This was a descriptive study. The obtained preliminary results may lay the groundwork for future analysis, such as using length of stay as an indirect hospital cost factor, assessing costs of rare diseases in Poland, evaluating factors influencing increased spending, and proposing cost optimization strategies. An analysis of predictive factors in these selected rare diseases is based on data on hospital morbidity collected in multiannual studies on public statistics.
Material and Methods
Ethics Statement
The study protocol was submitted and reviewed by the Ethics Committee at the Medical University of Warsaw – document number: AKBE/166/2023. Written informed consent was obtained from all participants.
Research Methodology
Data Acquisition
In this retrospective, population-based study, we analyzed hospital discharge records of patients diagnosed with sarcoidosis, Still’s disease, and systemic sclerosis. Data were obtained from the National Institute of Public Health (NIH), National Research Institute in Poland, and they covered 78 626, 3294, and 35 549 hospitalizations, respectively, which were reported in the years 2009–2018. The analyzed time period is strongly related to the previous cycle of epidemiology research.
All hospitals in Poland, except psychiatric and military facilities, are legally required to send discharge data to the Institute. The data are anonymous and include information on hospitalizations with ICD10-code diagnoses, dates of admission and discharge, birth date, sex, and place of residence. We also obtained demographic data for the general Polish population from the Central Statistical Office of Poland. We assumed that diagnoses in hospitals were based on the most current, widely used criteria.
The high degree of completeness of data on hospital morbidity results from the legal obligation imposed on inpatient healthcare units to periodically report data on hospitalizations to the National Institute of Public Health, National Institute of Hygiene. The accuracy and credibility of data result from the efficiency and accuracy of reporting by individual entities. The large group of respondents covering almost 100% of hospitalizations in Poland guaranteed the accuracy and reliability of the data analyzed in this study. Data from the national register are anonymous, but properly adjusted tools for statistical analysis made it possible to obtain data on hospitalizations and predictive factors.
Statistical Analysis
To perform the statistical analyses, R software was used. We computed means and medians for continuous variables, and counts and percentages for categorical variables. The analysis broken down by hospital departments was based on the Pareto principle, and it presents entities where about 80% of all hospitalizations took place. The analysis of the length of hospitalization included first-time and subsequent hospitalizations.
Literature Analysis
A literature search was performed using the PubMed electronic database. The search term used to identify the articles was the length of stay. The search was limited to full-text English-language studies published in the years 2018–2022. The reference lists of relevant studies were searched to identify additional articles.
Results
LOS vs Timelines
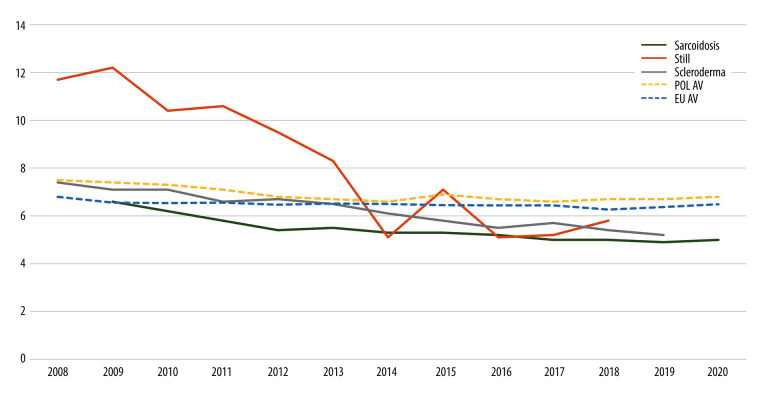
In the analyzed period, the average length of hospitalization for selected diseases was steadily decreasing, and in 2009–2018 it was 5.39 days (standard deviation, SD=5.31) for sarcoidosis (78 626 cases), 6.22 days (SD=6.29) for scleroderma (35 549 cases), and 7.44 days (SD=9.15) for Still’s disease (3294 cases). The largest difference in the average value between 2009 and 2018 was recorded for Still’s disease, where 11.7 days and 5.81 days were reported, respectively. The difference was not as significant for other diseases, but at the end of 2018 it was less than 6 days. After 2016, the average length of hospitalization for the analyzed diseases was shorter than the average for all-cause hospitalizations in Poland and in the European Union (Figure 1).
Figure 1.
Average length of hospitalizations for sarcoidosis, Still’s disease, and scleroderma, and the average length of hospitalizations in Poland (POL AV) and the European Union (EU AV) in the years 2008–2020 for all reported hospitalization cases. AV – average; POL – Poland; EU – European Union. Software: R Core Team (2021). R (Version 4.1.1): A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria.
LOS vs Number of Hospitalizations
The average length of stay in the group of patients with first-time hospitalization was shorter for each of the analyzed diseases as compared to the length of the second and subsequent hospitalizations. The most significant differences were observed in Still’s disease and the least significant ones in sarcoidosis. Details are presented in Table 1.
Table 1.
The mean, standard deviation (SD), and median of length of first-time, second, and subsequent hospitalization.
| First-time hospitalization | Second-time and consecutive | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Median | Mean | SD | Median | |
| Sarcoidosis | 4.85 | 4.98 | 3 | 5.65 | 5.44 | 4 |
| Scleroderma | 5.70 | 5.67 | 4 | 7.05 | 7.08 | 5 |
| Still | 7.07 | 8.96 | 4 | 10.6 | 10.2 | 9 |
Source: own elaboration. SD – standard seviation.
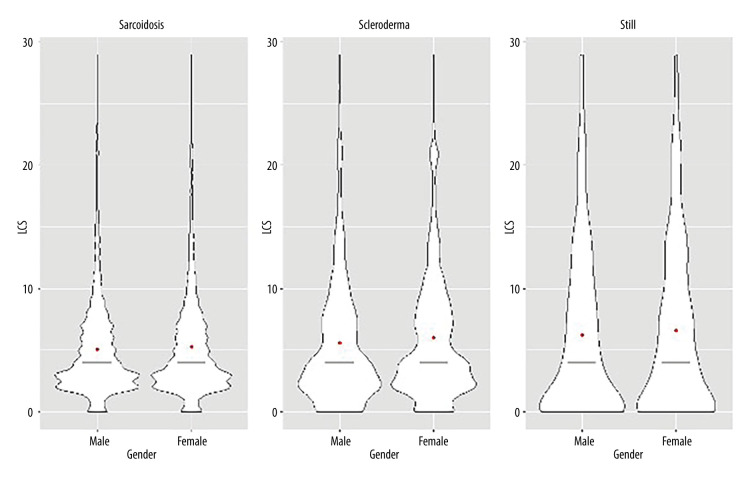
LOS vs Sex
No significant differences were observed for the length of hospitalization between males and females. The mean length of hospitalization for sarcoidosis was 5.48 days (SD=5.30) in women and 5.31 (SD=5.31) days in men. The mean length of hospitalization for scleroderma was 6.28 days (SD=6.24) in women and 5.97 days (SD=6.50) in men. The mean length of hospitalization for Still’s disease was 7.39 days (SD=8.47) in women and 7.52 days (SD=10.0) in men. However, an increased proportion of hospitalizations of over 10 days was observed for scleroderma and Still’s disease as compared to sarcoidosis (Figure 2).
Figure 2.
Distribution of the length of hospitalization for sarcoidosis, Still’s disease, and scleroderma by sex. The figure presents hospital stays in the time range (0–30 days) and includes all reported hospitalizations. Software: R Core Team (2021). R (Version 4.1.1): A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria.
LOS vs Age Groups
Analysis by sex showed significant differences in lengths of hospitalization for Still’s disease. The longest hospitalizations were recorded in both the youngest and the oldest age groups. Similar differences were not observed in sarcoidosis and scleroderma, which showed an increase in mean and median length of hospitalization with age (Table 2).
Table 2.
Mean, standard deviation, and median hospitalization for sarcoidosis and Still’s disease by age group, including all recorded hospitalizations.
| Age | Sarcoidosis | Scleroderma | Still | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Median | Mean | SD | Median | Mean | SD | Median | |
| 0–18 | 4.3 | 7.4 | 2.0 | 4.4 | 6.5 | 2.0 | 11.2 | 9.8 | 9.0 |
| 18–24 | 5.2 | 4.4 | 4.0 | 4.7 | 4.6 | 4.0 | 6.4 | 9.2 | 3.0 |
| 25–34 | 4.8 | 4.2 | 4.0 | 5.2 | 5.6 | 4.0 | 5.3 | 7.9 | 2.0 |
| 35–44 | 4.8 | 4.6 | 4.0 | 5.0 | 5.4 | 4.0 | 7.3 | 8.7 | 5.0 |
| 45–54 | 5.4 | 5.2 | 4.0 | 6.1 | 5.9 | 4.0 | 8.1 | 8.3 | 6.0 |
| 55–64 | 6.1 | 6.1 | 4.0 | 6.2 | 6.0 | 4.0 | 8.8 | 9.2 | 7.0 |
| 65–74 | 6.7 | 6.9 | 5.0 | 6.6 | 7.1 | 5.0 | 12.7 | 11.0 | 10.0 |
| 75+ | 8.2 | 8.8 | 7.0 | 7.6 | 6.5 | 7.0 | 12.1 | 8.4 | 11.0 |
Source: own elaboration. SD – standard deviation.
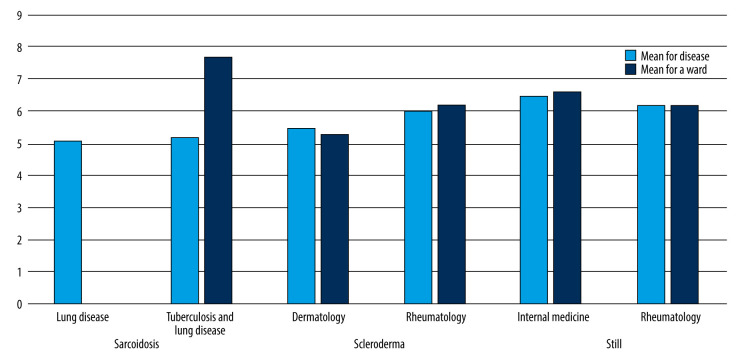
LOS vs Hospital Wards
A comparison of the mean length of hospitalization for the analyzed diseases in 2 wards where the percentage of hospitalization was the highest in a given disease, with the average length of hospitalization in these wards, regardless of the disease, shows that it is similar for all diseases and wards (Figure 3), except for sarcoidosis. The mean length of hospitalization in tuberculosis and lung disease wards was 7.7 days (sarcoidosis 5.2 days), internal medicine ward 6.6 days (Still’s disease 6.5 days), rheumatology ward 6.2 days (Still’s disease 6.2 days, scleroderma 6 days), and dermatology ward 5.3 days (scleroderma 5.5 days) (Figure 3). There are no data on the length of hospitalization for sarcoidosis in lung disease wards in Poland.
Figure 3.
Mean length of hospitalization for sarcoidosis and Still’s disease in 2 wards with the highest percentage of hospitalizations for a given disease and the mean length of hospitalization (irrespective of the disease) in these wards, including all recorded hospitalizations. Software: R Core Team (2021). R (Version 4.1.1): A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria.
LOS vs Multimorbidity (Volume)
The mean length of hospitalization increased with each additional comorbidity, whereby 3 additional comorbidities prolonged the average hospital stay by more than 4 times. The greatest differences were observed for Still’s disease; however, the dispersion of results for 2 and 3 comorbidities was comparable to or smaller than other diseases. Details are presented in Table 3.
Table 3.
Mean length of hospitalization for the analyzed diseases in the group of patients with 1, 2, or 3 comorbidities, including all recorded hospitalizations.
| One | Two | Three | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Median | Mean | SD | Median | Mean | SD | Median | |
| Sarcoidosis | 5.39 | 5.31 | 4 | 12.8 | 13.8 | 9 | 24.2 | 25.3 | 18 |
| Scleroderma | 6.22 | 6.29 | 4 | 13.3 | 14.5 | 9 | 24.4 | 24.6 | 20 |
| Still | 7.44 | 9.15 | 4 | 17.9 | 13.4 | 14 | 39.2 | 19.8 | 41.5 |
Source: own elaboration. SD – standard deviation.
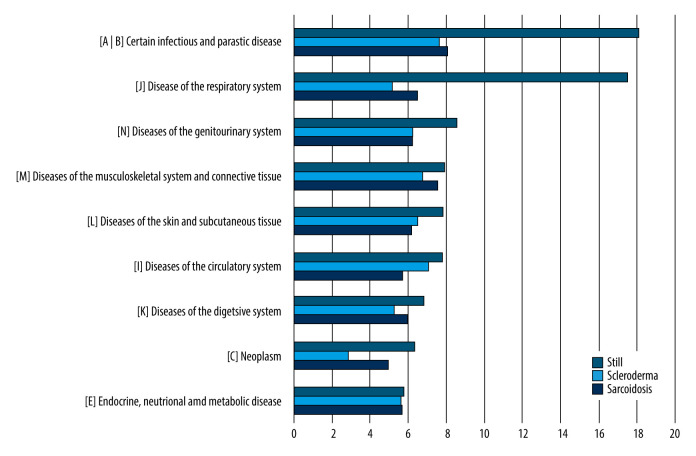
LOS vs Multimorbidity (Types)
A large variation was observed in the mean length of hospitalization for Still’s disease in the group of patients with parasitic and respiratory diseases as compared to other comorbidities. The average length of hospitalization among persons with parasitic diseases was the longest in scleroderma and sarcoidosis patients. The second most common group of comorbidities in patients with sarcoidosis was skeletal diseases. Among patients with scleroderma, these were cardiovascular diseases; however, in this group of patients, hospitalizations were clearly shorter in patients with cancer. Details are shown in Figure 4.
Figure 4.
The mean length of hospitalization in patients with the analyzed diseases and comorbidities, including all recorded hospitalizations. Software: R Core Team (2021). R (Version 4.1.1): A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria.
Discussion
The current study is the first study based on a large national database to investigate patient characteristics related to the length of hospital stay for selected rare diseases (sarcoidosis, Still’s disease, and scleroderma) in Poland. The average length of hospitalization over the selected period in the diseases was: sarcoidosis 5.39 days, scleroderma 6.22 days, and Still’s disease 7.44 days, and was shorter for each of the diseases analyzed compared with the length of hospitalization for second and subsequent stays. There were no substantial differences in length of hospitalization between males and females, but the average length of hospitalization increased with each additional comorbidity.
Across studies and countries, patients with rare diseases had longer hospital LOS. In Switzerland, patients with 1 rare disease had longer LOS by 28% and 49% if they were diagnosed with more than 1 rare disease. They were also associated with higher Intensive Care Unit (ICU) admissions, longer ICU LOS (increase by 14% and 40% for 1 and >1 rare disease), and higher 30-day readmissions [18]. A study of Italian patients showed that patients with rare diseases had more hospital admissions and longer average hospital stays as compared to the general population [19]. In a Unites States (US) population study, patients with rare diseases had a longer LOS (6.3 days) compared to those with common conditions (3.8 days) [20]. Similar results were reported for Australian patients [21].
In Poland, the average length of stay fell by 0.8 days between 2008 and 2019 (from 7.5 in 2008 to 6.7 in 2018) [17]. The analyzed data show that the average length of stay for the selected rare diseases in Poland was similar to that of the general population (especially for the last years subject to analysis). We found that LOS for Polish sarcoidosis patients is similar to that of US or Swiss patients. Sarcoidosis patients are reported to have similar average lengths of stay as non-sarcoidosis hospitalizations [10]. However, a Swiss population study found that sarcoidosis was related to an increased hospital stay (6 days vs 4 days for controls) [24]. The mean LOS for the US scleroderma patients was 6.6 days, which is almost 1 day longer than we observed for the Polish patients [25]. The mean LOS in a US study of a systemic scleroderma (SS) cohort was 5.5 days for SSc-related admissions and 5.7 days for non-SSc-related admissions [26]. Longitudinal data show the average length of stay for Still’s disease patients in Australia was 9 days, the same as we observed for the Polish population [27]. A single-center study of 30 patients with adult-onset Still’s disease in Pakistan noted an average hospital length of stay of 12.5 days, much longer than for the Polish population in our analysis [28].
In our analysis, sex did not significantly influence the length of stay. Similar findings were reported in other studies. For scleroderma patients in the US, there were no statically significant differences between LOS in men and women. LOS increased with age, however, and it was the highest in patients >65 years old [25].
Across studies, advanced age was associated with inappropriate hospital stay and prolonged bed use [13]. In our study, patients with advanced age had longer LOS than the general Polish population (6.8 days). This was true for sarcoidosis in persons aged 75+ (with the average LOS of 8.2 days) and scleroderma in patients aged 75+ (average LOS of 7.6 days). LOS in Still’s disease patients was longer than the Polish average for all age groups apart from 18- to 34-year-olds. The longest LOS was observed in the youngest age group (0–18 years old) with 11.2 days of hospitalization and in the group of patients aged 65–74 with 12.7 days of hospitalization. Patients who were older or had other health conditions were more likely to require longer hospital stays, reflecting the multifaceted nature of these diseases and the impact they can have on overall health.
We observed that multimorbidity greatly prolonged hospitalization in patients with rare diseases, increasing it 2-fold for 2 comorbidities and 4-fold for 3 comorbidities. Similar observations were made with regard to patients with common conditions, where a greater number of chronic diseases was associated with longer hospital stays. A Swiss study on elderly people (>65 years of age) found that the length of stay doubled in the presence of multimorbidity (7.9 days for patients with single condition and 14.3 for patients with multimorbidity) [29]. An increased LOS was also observed for the number of affected body systems, with an odds ratio (OR) of >20 for individuals with more than 7 affected body systems [30].
Comparing the mean for Polish hospital wards, the average LOS for all analyzed diseases was similar to that of the general population [31], suggesting that the studied conditions did not have a significant impact on how long patients had to stay in the hospital. However, when a specific diagnosis was considered, patients with Still’s disease had greatly prolonged length of stay in the group of patients with parasitic and respiratory diseases.
These findings highlight the need for more targeted and personalized treatment. By identifying and addressing the underlying factors that drive the length of hospitalization, healthcare providers may be able to reduce the burden of hospitalization and improve the overall outcomes in these populations.
In summary, this study is the only report to date that characterizes the length of stay for sarcoidosis, Still’s disease, and scleroderma in Poland. Although in general, the length of stay for the analyzed rare diseases did not differ from the Polish average, we identified factors that extended patient’s stay in hospital. These were advanced age, second-time and subsequent hospitalization, and multimorbidity. Overall, this study adds to the growing body of evidence highlighting the complex nature of rare chronic diseases such as sarcoidosis, Still’s disease, and scleroderma. By better understanding the factors associated with hospitalization length, healthcare providers can work towards more effective prevention and management strategies, ultimately improving the lives of patients with these challenging conditions.
Study Advantages and Limitations
This epidemiological study’s main strength is that it used population-based registry data related to hospital data, which enabled analysis of the inpatients’ characteristics and trends in length of stay of patients with sarcoidosis, scleroderma, and Still’s disease. Therefore, we were able to estimate the healthcare burden of those RDs in a large cohort of patients.
The limitation of the study is its descriptive and exploratory nature aimed at investigation of length of hospital stay as an organizational factor in the management of rare diseases. Further research and statistical analyses are needed to show the strength of the impact of individual factors on length of stay. In the long-term research perspective, it is also worth analyzing length of stay as an indirect cost-generating factor in health care. These results can be used for more efficient organization and financing of treatment of rare diseases in Poland and across the globe.
Conclusions
The issue of rare diseases in Poland is receiving increasing attention. It can be concluded that rare diseases are a special and specific group of diseases that require individual analyses, which can only be performed on the basis of large national data registers.
The main aim of this study was to analyze selected predictive factors and the length of hospital stay in chosen rare autoimmune diseases in Poland. Considering the previous cycle of epidemiology research, this study includes the analysis of sarcoidosis, systematic sclerosis, and adult-onset Still’s disease.
The study showed that hospitalizations of selected rare diseases do not cause a significant burden for the healthcare system. Therefore, the strategy that has been implemented so far in inpatient treatment of rare diseases should be continued. However, it is important to draw public and social attention to the very issue of rare diseases in order to improve the quality and availability of care for patients with rare diseases. Due to the specificity of their disease, these patients tend to have difficulties in obtaining a proper diagnosis, and it often takes a long time before they get to the right specialist and start treatment [32].
The results of the conducted research also showed that advanced age and comorbidities are important factors determining the length of hospitalization. The average length of hospital stay for selected rare diseases in Poland is not longer than the EU average, so it can be assumed that the process of inpatient treatment in Poland is optimal.
The findings for hospitalization rate and average LOS could serve as a starting point for further improvement in organization of treatment of rare diseases. Studies on the burden of RDs and their costs are crucial to the planning of resource distribution because funds for RD prevention, diagnosis, and treatment are typically distributed using a prevalence-based criterion.
Further studies are needed on holistic, systemic solutions for patients and their families. This topic requires a holistic approach, integrated activities of many groups of specialists, and decisive action. Optimization of the treatment will also be possible thanks to the use of the results of this study and further in-depth analyses.
Footnotes
Conflict of interest: None declared
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: None declared
References
- 1.Polish Ministry of Health. [cited 2023 Jul 29] Available from: https://www.gov.pl/web/zdrowie/choroby-rzadkie [in Polish]
- 2.Ferreira CR. The burden of rare diseases. Am J Med Genet. 2019;179(6):885–92. doi: 10.1002/ajmg.a.61124. [DOI] [PubMed] [Google Scholar]
- 3.Richter T, Nestler-Parr S, Babela R, et al. Rare disease terminology and definitions – a systematic global review: Report of the ISPOR Rare Disease Special Interest Group. Value Health. 2015;18(6):906–14. doi: 10.1016/j.jval.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 4.European Commission. Useful information on rare diseases from an EU perspective. [cited 2023 Jul 29[; Available from: https://ec.europa.eu/health/ph_information/documents/ev20040705_rd05_en.pdf.
- 5.Pieklak M, Pałka K, Frelas K, et al. 2020. [cited 2023 Jul 29] Available from: www.dzp.pl/files/shares/Publikacje/Raport%20Choroby%20rzadkie%20dostepnosc%20terpii%20przeglad%20polskich%20rozwiazan%20i%20rekomendacje%20dla%20Polski.pdf [in Polish]
- 6.Bogdan M, Nitsch-Osuch A, Kanecki K, et al. Sarcoidosis among hospitalized patients in Poland: A national hospital register-based study. Pol Arch Intern Med. 2019;129(9):580–85. doi: 10.20452/pamw.14927. [DOI] [PubMed] [Google Scholar]
- 7.Bogdan M, Nitsch-Osuch A, Tyszko P, et al. Systemic sclerosis among hospitalized patients in Poland: A study based on a national hospital registry. Arch Med Sci. 2022;129(9):580–85. doi: 10.20452/pamw.14927. [DOI] [PubMed] [Google Scholar]
- 8.Bogdan M, Nitsch-Osuch A, Samel-Kowalik P, et al. Adult-onset Still’s disease in Poland – a nationwide population-based study. Ann Agric Environ Med. 2021;28(2):250–54. doi: 10.26444/aaem/132451. [DOI] [PubMed] [Google Scholar]
- 9.Polish Ministry of Health. Narodowy plan dla chorób rzadkich. [cited 2023 Jul 29]; Available from: https://www.gov.pl/web/zdrowie/narodowy-plan-dla-chorob-rzadkich [in Polish]
- 10. [Resolution No. 110 of the Council of Ministers of August 24, 2021 on the adoption of the document Plan for Rare Diseases]. [in Polish] [Google Scholar]
- 11.Czech M. Ed 1. [Pharmacoeconomics: The economic evaluation of health programs]. Warsaw: Oficyna Wydawnicza Politechniki Warszawskiej; 2004. [in Polish] [Google Scholar]
- 12.Cannoodt LJ, Knickman JR. The effect of hospital characteristics and organizational factors on pre- and postoperative lengths of hospital stay. Health Serv Res. 1984;19(5):561–85. [PMC free article] [PubMed] [Google Scholar]
- 13.Buttigieg SC, Abela L, Pace A. Variables affecting hospital length of stay: A scoping review. J Health Organ Manag. 2018;32(3):463–93. doi: 10.1108/JHOM-10-2017-0275. [DOI] [PubMed] [Google Scholar]
- 14.Barisonzo R, Wiedermann W, Unterhuber M, Wiedermann CJ. Length of stay as risk factor for inappropriate hospital days: Interaction with patient age and co-morbidity: Age and co-morbidity in inappropriate hospital use. J Eval Clin Pract. 2013;19(1):80–85. doi: 10.1111/j.1365-2753.2011.01775.x. [DOI] [PubMed] [Google Scholar]
- 15.Lim SC, Doshi V, Castasus B, et al. Factors causing delay in discharge of elderly patients in an acute care hospital. Ann Acad Med Singap. 2006;35(1):27–32. [PubMed] [Google Scholar]
- 16.Stone K, Zwiggelaar R, Jones P, Mac Parthaláin N. A systematic review of the prediction of hospital length of stay: Towards a unified framework. In: Yoon D, editor. PLoS Digit Health. 4. Vol. 1. 2022. p. e0000017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.OECD. Length of hospital stay. [cited 2023 Jul 29]; Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/length-of-hospital-stay/indicator/english_8dda6b7a-en.
- 18.Blazsik RM, Beeler PE, Tarcak K, et al. Impact of single and combined rare diseases on adult inpatient outcomes: A retrospective, cross-sectional study of a large inpatient population. Orphanet J Rare Dis. 2021;16(1):105. doi: 10.1186/s13023-021-01737-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baldacci S, Santoro M, Pierini A, et al. Healthcare burden of rare diseases: A population-based study in Tuscany (Italy) Int J Environ Res Public Health. 2022;19(13):7553. doi: 10.3390/ijerph19137553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Navarrete-Opazo AA, Singh M, Tisdale A, et al. Can you hear us now? The impact of health-care utilization by rare disease patients in the United States. Genet Med. 2021;23(11):2194–201. doi: 10.1038/s41436-021-01241-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walker CE, Mahede T, Davis G, et al. The collective impact of rare diseases in Western Australia: An estimate using a population-based cohort. Genet Med. 2017;19(5):546–52. doi: 10.1038/gim.2016.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ungprasert P, Crowson CS, Achenbach SJ, et al. Hospitalization among patients with sarcoidosis: A population-based cohort study 1987–2015. Lung. 2017;195(4):411–18. doi: 10.1007/s00408-017-0012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ungprasert P, Wijarnpreecha K, Cheungpasitporn W, et al. Inpatient prevalence, expenditures, and comorbidities of sarcoidosis: Nationwide inpatient sample 2013–2014. Lung. 2019;197(2):165–71. doi: 10.1007/s00408-019-00210-x. [DOI] [PubMed] [Google Scholar]
- 24.Pohle S, Baty F, Brutsche M. In-hospital disease burden of sarcoidosis in Switzerland from 2002 to 2012. PLoS One. 2016;11(3):e0151940. doi: 10.1371/journal.pone.0151940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chung L, Krishnan E, Chakravarty EF. Hospitalizations and mortality in systemic sclerosis: Results from the Nationwide Inpatient Sample. Rheumatology. 2007;46(12):1808–13. doi: 10.1093/rheumatology/kem273. [DOI] [PubMed] [Google Scholar]
- 26.Sankar S, Habib M, Jaafar S, et al. Hospitalizations related to systemic sclerosis and the impact of interstitial lung disease – analysis of patients hospitalized at the University of Michigan. Clin Exp Rheumatol. 2021;39(Suppl 131):43–51. doi: 10.55563/clinexprheumatol/9ivp9g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nossent J, Raymond W, Keen H, et al. Adult-onset Still’s disease in Western Australia: Epidemiology, comorbidity and long-term outcome. Int J of Rheum Dis. 2022;25(11):1306–14. doi: 10.1111/1756-185X.14424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hassan SA, Choudhry AS, Jamal S, et al. Adult onset Still’s disease: A retrospective, single-center study. Cureus. 2020;12(8):e10008. doi: 10.7759/cureus.10008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bähler C, Huber CA, Brüngger B, Reich O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: A claims data based observational study. BMC Health Serv Res. 2015;15(1):23. doi: 10.1186/s12913-015-0698-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aubert CE, Schnipper JL, Fankhauser N, et al. Association of patterns of multimorbidity with length of stay: A multinational observational study. Medicine. 2020;99(34):e21650. doi: 10.1097/MD.0000000000021650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Statistics Poland, Social Surveys Department, Statistical Office in Cracow. Health and health care in 2019. Warsaw, Cracow: 2020. [Google Scholar]
- 32.University Hospital in Cracow. Center for Rare Diseases; [cited 2023 Jul 29]; Available from: https://www.su.krakow.pl/jednostki/choroby-rzadkie [in Polish] [Google Scholar]