Abstract
Objectives:
We sought to assess whether there were any parameter(s) on baseline computed-tomography-perfusion (CTP) strongly correlating with final-infarct-volume, and infarct volume progression after endovascular recanalization of acute ischemic stroke (AIS) with primary distal, medium vessel occlusion (DMVO).
Materials and Methods:
We performed a retrospective analysis of consecutive AIS patients who were successfully recanalized by thrombectomy for DMVO. By comparing baseline CTP and follow-up MRI, we evaluated the correlation between baseline infarct and hypoperfusion volumes, and final infarct volume and infarct volume progression. We also examined their effect on good clinical outcome at 3 months (defined as an mRS score of 0 to 2).
Results:
Between January 2018 and January 2021, 38 patients met the inclusion criteria (76% [29/38] female, median age 75 [66–86] years). Median final infarct volume and infarct volume progression were 8.4 mL [IQR: 5.2–44.4] and 7.2 mL [IQR: 4.3–29.1] respectively. TMax > 10 sec volume was strongly correlated with both (r = 0.831 and r = 0.771 respectively, p < 0.0001), as well as with good clinical outcome (–0.5, p = 0.001). A higher baseline TMax > 10 sec volume increased the probability of a higher final-infarct-volume (r2 = 0.690, coefficient = 0.83 [0.64–1.00], p < 0.0001), whereas it decreased the probability of good clinical outcome at 3 months (odds ratio = –0.67 [–1.17 to –0.18], p = 0.008).
Conclusion:
TMax > 10 sec volume on baseline CTP correlates strongly with final infarct volume as well as with clinical outcome after mechanical thrombectomy for an AIS with DMVO.
Keywords: acute ischemic stroke, endovascular recanalization, distal thrombectomy, perfusion imaging
Introduction
Endovascular thrombectomy (EVT) is now the standard of care for acute ischemic stroke (AIS) patients with an anterior large vessel occlusion (LVO) [1,2]; however, not all patients who undergo recanalization will clinically benefit from it.
Furthermore, there is still no definitive recommendation in the literature to perform EVT in patients with distal, medium vessel occlusions (DMVO) (defined by consensus as the A2–A4 segments of the anterior cerebral artery, the M3–M4 segments of the medial cerebral artery, the P2–P4 segments of the posterior cerebral artery, as well as the posterior inferior, anterior inferior, and superior cerebellar arteries [3]), despite representing up to 40% of AIS, either as primary occlusions or as secondary emboli to new territories after LVO recanalization [3,4,5,6].
Final infarct volume is a key determinant of clinical outcome [7,8,9,10], the risk of cerebral edema [11,12,13,14], and the risk of craniectomy [15,16,17], as well as that of hemorrhagic transformation [18,19,20,21] in stroke despite recanalization by EVT. Unfortunately, prediction of final infarct volume and infarct volume progression between the baseline and post-EVT imaging remains challenging in clinical practice, both in the anterior [22,23,24] and posterior [25] circulation.
Baseline imaging often includes perfusion CT as a tool to improve diagnostic accuracy [26,27], but we pondered whether the information provided by such protocols could be used as early imaging predictors of infarct volume progression. We hypothesized that the final infarct volume may be correlated with severely hypoperfused brain tissue on baseline computed tomography perfusion (CTP), regardless of successful endovascular recanalization of AIS with primary DMVO.
We sought to assess which parameter on baseline computed tomography perfusion (CTP) could be correlated with final infarct volume, infarct volume progression, as well as clinical outcome after successful endovascular recanalization of an AIS with a primary DMVO.
Materials and Methods
This study was approved by our local institutional review board and ethics committee. Informed consent was waived based on minimal patient risk and practical inability to perform the study without the waiver.
The data that support the findings of this study are available from the corresponding author upon reasonable request. Adherence to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) criteria was enforced [28].
Study Population
We retrospectively identified consecutive patients diagnosed with AIS due to primary DMVO in our comprehensive stroke center between January 2018 and January 2021, who met the following criteria:
CTP imaging was performed in-house and provided a technically adequate assessment of the baseline infarct and hypoperfusion volumes (regional cerebral blood flow – rCBF and time-to-maximum – TMax volumes).
National Institutes of Health Stroke Scale (NIHSS) ≥1 at presentation.
Time from symptom onset to groin puncture < 6h.
Underwent endovascular treatment with successful recanalization, modified Treatment In Cerebral Infarction (mTICI) scale ≥2c.
Received follow-up magnetic resonance imaging (MRI) on day 3 post-EVT to assess the final infarct volume on fluid attenuation inversion recovery (FLAIR).
Clinical evaluation with modified Rankin Scale (mRS) at 3 months by a certified stroke neurologist.
The decision to perform the endovascular procedure was made by a multidisciplinary team on an individual-patient basis; the technical aspects were left at the discretion of the treating neurointerventionalist, following standard of care. Patients’ baseline clinical and radiological characteristics, procedure details, as well as outcomes, were collected using standardized definitions [29]. All cases were reviewed by two board-certified neuroradiologists with 5+ years of experience as senior staff members, they determined the angiographic treatment success using the mTICI scale. In cases of inter-observer inconsistency, a decision was made by consensus.
Radiological Evaluation
Baseline imaging automatically assessed the infarct volume (mL; rCBF < 30% on CTP) and hypoperfusion volumes (mL; TMax > 4 sec, TMax > 6 sec, TMax > 8 sec, and TMax > 10 sec volumes) [30] before EVT using automated software (RAPID, iSchemaView, Menlo Park). CTPs with major artifacts were not included, and manual correction of the initial core lesion volumes was not required.
Final infarct volume (mL) was assessed on day 3 on axial FLAIR imaging [31] using the Horos Dicom Viewer (Horos Project, Geneva, Switzerland) by the same board-certified neuroradiologists, blinded to the initial CTP, EVT result, and clinical outcome. FLAIR axial sequences were performed on a 3T Siemens scan with the following parameters: TR 9000 msec, TE 91 msec, slice was 4mm, slice gap of 0.0, and FOV of 230 × 230mm. The readers were allowed to look at the DWI sequences to avoid misinterpretation of the FLAIR images [32].
Infarct volume progression (in mL) between baseline CTP and day 3 MRI was calculated as the difference between both infarct volumes.
Statistical analyses
First, Pearson’s correlations were calculated to find the baseline imaging parameter (among rCBF and TMax volumes as determined on baseline CTP) with the highest correlation with final infarct volume, infarct volume progression, and 3 months good clinical outcome (mRS 0–2).
Then, we evaluated the association of this parameter with final infarct volume and infarct volume progression using linear regression, and its association with 3 months good clinical outcome using binary logistic regression.
Using receiver operating characteristic (ROC) curves analyses, we determined the optimal baseline volume threshold to predict a low final infarct volume (final infarct volume < median), a low infarct volume progression (infarct volume progression < median), and good clinical outcome (mRS 0–2 at 3 months) with optimal sensitivity and specificity.
Categorical variables are reported as proportions. Continuous variables are reported as median (inter-quartile range). Statistical significance was set at the p = 0.05 level. All statistical analyses were performed with XLSTAT (Addinsoft, New York City, NY).
Results
From January 2018 to January 2021, we identified 76 consecutive patients who came into our stroke center with AIS due to DMVO. Fifty-eight patients underwent a computed tomography (CT) angiogram and CT perfusion as the first imaging method with available and adequate perfusion and infarct volumes, 40 of these patients were successfully recanalized by EVT, and 38 had magnetic resonance imaging (MRI) performed on day 3 with FLAIR sequence to assess the final infarct volume as well as a clinical evaluation at 3-months. These 38 patients were included (Figure 1).
Figure 1.
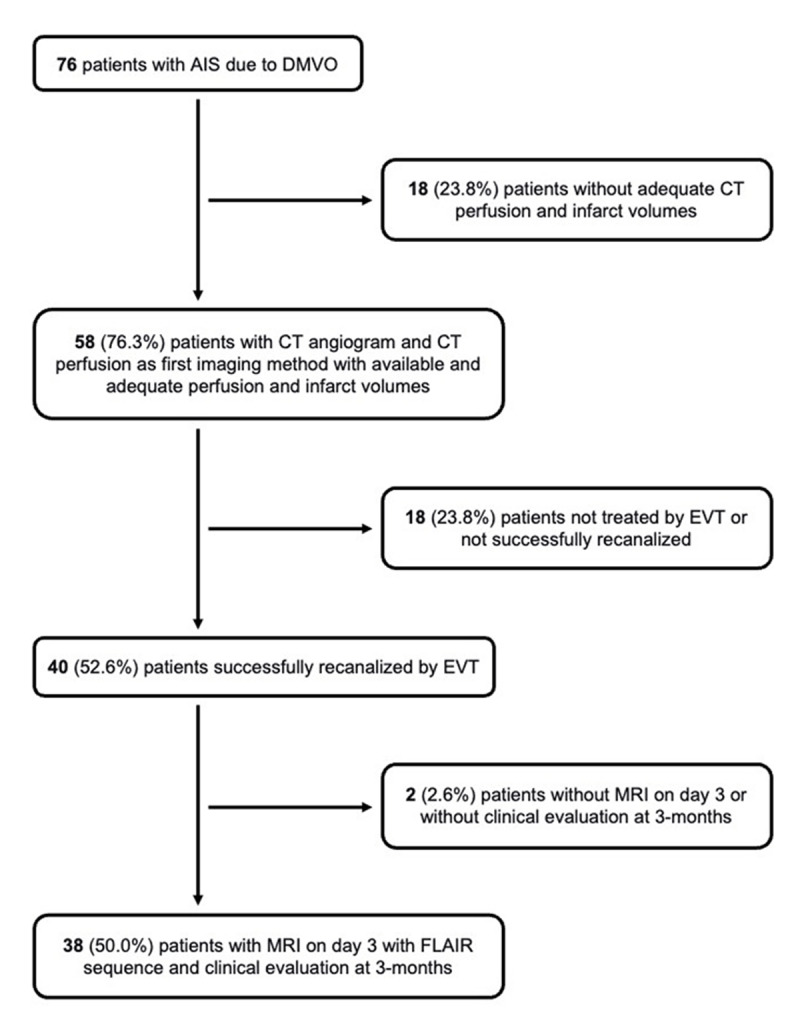
Flowchart of the patient selection.
Among them, 76% [29/38] were female, and median age was 75 [66–86] years). Baseline median infarct volume was 0.3 mL (0.3–6.8) (Table 1). Median final infarct volume and infarct volume progression were respectively, 8.4 mL [IQR: 5.2–44.4] and 7.2 mL [IQR: 4.3–29.1] (Table 2).
Table 1.
Baseline characteristics of all patients.
|
| |
|---|---|
| ALL | |
|
| |
| Number of patients | 38 (100%) |
|
| |
| Age, years (median, IQR) | 75 (66–86) |
|
| |
| Female (%) | 29 (76%) |
|
| |
| Medical History | |
|
| |
| High Blood Pressure (%) | 33 (87%) |
|
| |
| Diabetes (%) | 9 (24%) |
|
| |
| Hyperlipidemia (%) | 18 (47%) |
|
| |
| Weight (kg) (median, IQR) | 75 (65–94) |
|
| |
| Antiplatelets (%) | 12 (32%) |
|
| |
| Anticoagulants (%) | 7 (18%) |
|
| |
| Current Smoking (%) | 6 (16%) |
|
| |
| Pre-stroke mRS of 0–1 (%) | 36 (95%) |
|
| |
| Clinical Presentation | |
|
| |
| Heart rate (bpm) (median, IQR) | 76 (68–88) |
|
| |
| Systolic Blood Pressure (mmHg) (median, IQR) | 146 (125–170) |
|
| |
| Diastolic Blood Pressure (mmHg) (median, IQR) | 80 (75–85) |
|
| |
| Temperature (°C) (median, IQR) | 36.9 (36.4–37.2) |
|
| |
| Baseline NIHSS (median, IQR) | 10 (8–15) |
|
| |
| IVT (%) | 26 (68%) |
|
| |
| Times | |
|
| |
| Time Onset to Puncture in min (median, IQR) | 210 (166–296) |
|
| |
| Unknown Onset (%) | 10 (26%) |
|
| |
| Occlusion | |
|
| |
| M2 (%) | 27 (71%) |
|
| |
| M3 (%) | 11 (29%) |
|
| |
| Left Side (%) | 20 (53%) |
|
| |
| Imaging | |
|
| |
| Baseline infarct volume, mL (median, IQR) | 0.3 (0.3–6.8) |
|
| |
| TMax > 4 sec volume, mL (median, IQR) | 102 (73–126) |
|
| |
| TMax > 6 sec volume, mL (median, IQR) | 50 (34–76) |
|
| |
| TMax > 8 sec volume, mL (median, IQR) | 25 (10–48) |
|
| |
| TMax > 10 sec volume, mL (median, IQR) | 12.5 (0.3–37) |
|
| |
| Mismatch volume, mL (median, IQR) | 43.9 (30.2–58.9) |
|
| |
| Mismatch ratio (median, IQR) | 295 (7–488) |
|
| |
| Etiology | |
|
| |
| Atherosclerosis (%) | 9 (24%) |
|
| |
| Cardio-embolic (%) | 28 (74%) |
|
| |
| Unknown (%) | 1 (2%) |
|
| |
* Continuous variables are reported as median (inter-quartile range), categorical variables as percentages.
Table 2.
Procedural characteristics and clinical outcomes.
|
| |
|---|---|
| ALL | |
|
| |
| Number of patients | 38 (100%) |
|
| |
| Mechanical Thrombectomy | |
|
| |
| Admission Mothership (%) | 20 (53%) |
|
| |
| Type of anesthesia | |
|
| |
| General Anesthesia (GA) (%) | 37 (97%) |
|
| |
| Conscious Sedation then GA (%) | 1 (3%) |
|
| |
| Technique | |
|
| |
| Contact Aspiration (%) | 13 (34%) |
|
| |
| Stent-retriever (%) | 6 (16%) |
|
| |
| Combined technique (%) | 19 (50%) |
|
| |
| Number of Passes (median, IQR) | 2 (1–3) |
|
| |
| Procedural Complication (%) | 0 (0%) |
|
| |
| Times | |
|
| |
| Time Puncture to Recanalization in min (median, IQR) | 30 (20–55) |
|
| |
| Time Onset to Recanalization in min (median, IQR) | 242 (191–326) |
|
| |
| Early Outcomes | |
|
| |
| Day 1 NIHSS (median, IQR) | 4 (1–7) |
|
| |
| NIHSS Shift (median, IQR) | –3 (–9 to –1) |
|
| |
| Day 1 Hemorrhagic Transformation (%) | 6 (25%) |
|
| |
| ECASS PH-Type (%) | 2 (7%) |
|
| |
| Final infarct volume, mL (median, IQR) | 8.4 (5.2–44.4) |
|
| |
| Infarct volume progression, mL (median, IQR) | 7.2 (4.3–29.1) |
|
| |
| Long-Term (3 months) Outcomes | |
|
| |
| mRS 0–1 (%) | 18 (47%) |
|
| |
| mRS 0–2 (%) | 23 (61%) |
|
| |
| Mortality (%) | 2 (5%) |
|
| |
* Continuous variables are reported as median (inter-quartile range), categorical variables as percentages.
TMax > 10 sec volume had the strongest correlation with final infarct volume and infarct volume progression (respectively, r = 0.831, p < 0.0001 and r = 0.771, p < 0.0001), as well as with good clinical outcome at 3 months (–0.5, p = 0.001).
A higher baseline TMax > 10 sec volume raised the probability of a higher final infarct volume (r2 = 0.690, coefficient = 0.83 [0.64–1.00], p < 0.0001) (Figure 2) and increased infarct volume progression (r2 = 0.595, coefficient = 0.77 [0.56–0.98], p < 0.0001) (Figure 3), whereas a higher baseline TMax > 10 sec volume decreased the probability of good clinical outcome at 3 months (odds ratio = –0.67 [–1.17 to –0.18], p = 0.008) (Figure 4).
Figure 2.
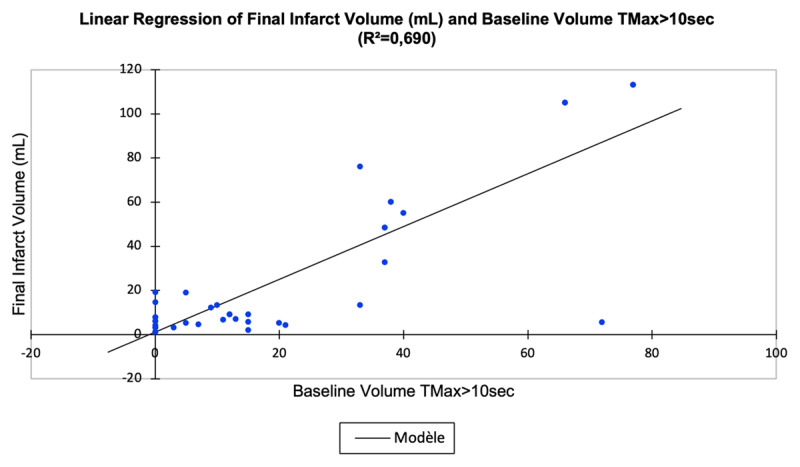
Association of baseline volume of severely hypoperfused brain tissue (TMax > 10 sec; mL) and final infarct volume (mL).
Figure 3.
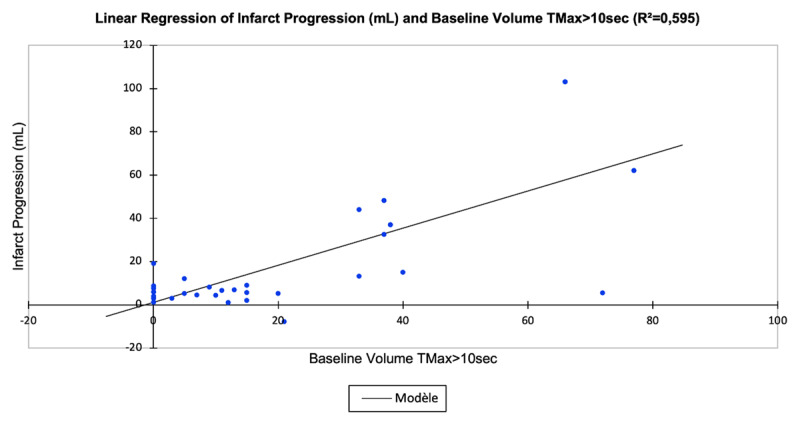
Association of baseline volume of severely hypoperfused brain tissue (TMax > 10 sec; mL) and infarct volume progression (mL).
Figure 4.
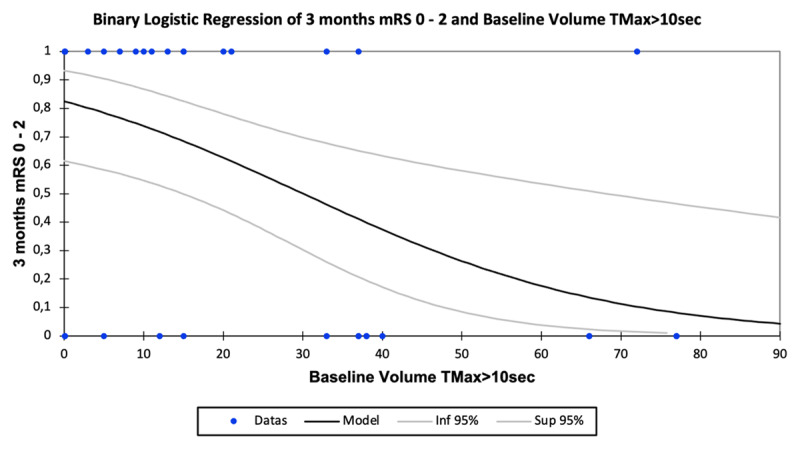
Association of baseline volume of severely hypoperfused brain tissue (TMax > 10 sec; mL) and the probability of good clinical outcome at 3 months (mRS 0-2).
ROC curves identified a TMax > 10 sec volume of less than 33 mL as the optimal threshold to predict a low final infarct volume (AUC = 0.802, sensitivity = 0.947, specificity = 0.632), a low infarct volume progression (AUC = 0.735, sensitivity = 0.947, specificity = 0.632), and good clinical outcome (AUC = 0.786, sensitivity = 0.870, specificity = 0.667).
Discussion
Our data indicate that severely hypoperfused brain tissue defined as the TMax > 10 sec volume assessed on baseline CTP may reasonably predict final irreversibly-injured brain tissue. Patients with a low volume of severely hypoperfused brain tissue (TMax > 10 sec) had minimal infarct volume progression after successful EVT and had a higher probability of good clinical outcome.
Recently, CTP has been increasingly added to CTA in AIS evaluation for a more accurate diagnosis. Severely hypoperfused brain tissue assessed by CT perfusion has been widely used to provide a surrogate for collaterals in large vessel occlusions using the hypoperfusion intensity ratio [30,33] but has not yet extensively been evaluated in distal occlusions.
Becks at al. highlighted that CTP may improve intracranial vascular blockage detection especially in distal occlusions and posterior circulation [34]. Likewise, Amukotuwa et al. showed that TMax maps help identify infarct volume related to DMVOs [26]. Furthermore, CTP may have a prognostic role in AIS, as an association between TMax target mismatch and clinical outcomes for LVO patients has already been demonstrated [35], and CTP-derived lesion thresholds have been used to predict poor clinical outcomes or death [36].
TMax thresholds have already been evaluated for large vessel occlusions, and while Wan et al. showed an association between the hypoperfusion intensity ratios with functional outcomes [37], Seker et al. demonstrated that higher TMax volumes correlated with worse outcomes [38].
In AIS, the differentiation between core, penumbra and benign oligemia and its impact on clinical outcome still is a challenge; and severity-weighted definitions based in perfusion anomalies (as opposed to the single threshold-based concept) have already been put forward [39,40]. In patients with mild symptoms, the perfusion severity-weighted model was evaluated and showed the risk of progression of oligemic volumes to actual infarction [41,42]. Indeed, among patients with similar hypoperfusion volumes, those with proportionally larger volumes of severe TMax delays were more disposed to early neurological decline. In the Defuse 3 trial, Rao et al. demonstrated that the addition of irreversibly injured ischemic core and persistently hypoperfused tissue volumes (defined as TMax > 6sec) predicted infarct volume at day 1; other TMax thresholds however were not tested [43]. On the other hand, Fainardi et al. analyzed higher TMax thresholds in LVO patients selected for mechanical thrombectomy and demonstrated that all TMax parameters were predictors of final infarct volume and outcome but that the higher thresholds ( > 6 seconds) had the strongest association with final infarct volume and good outcome [36]. A recently published study evaluated multiple TMax delays in DMVO patients with failed recanalization, and found that longer TMax delays, with the preeminence of TMax > 10 sec, were best correlated to final infarct volume [44].
Our preliminary data have the potential to guide further research in identifying non-salvageable tissue before EVT, and in determining imaging protocols for future trials involving DMVO stroke patients. Identifying salvageable vs. irreversibly damaged brain tissue, and thus determining which patients would benefit most from EVT remains an important consideration in the treatment of acute stroke especially in difficult situations such as DMVOs. This could have implications in the management of those patients, such as the need of repeating brain imaging in case of delayed transfer, as well as prognosis evaluation and clinical and imaging follow-up.
Our findings are the results of a retrospective, observational study with inherent biases such as single-center design and small sample size. Therefore, these findings are preliminary, hypothesis-generating, and do not allow for firm conclusions. Consequently, these data need to be replicated in larger cohorts as well as for patients with unsuccessful recanalization.
Concerning the evaluation of recanalization results, one would prefer to solely use the mTICI 3 score instead of mTICI 2c, however it would not be technically feasible in DMVO to go for a mTICI 3 after reaching a mTICI 2c considering the distality of the remaining occlusions.
The final infarct volume was estimated from MRI scans obtained three days after symptom onset. Ideally, infarct growth should be determined by the same imaging modality detecting irreversibly injured brain tissue at baseline and during follow-up, unfortunately no imaging modality would display the exact ischemic brain infarction within the first 6 hours of stroke onset. Non-contrast CT hypoattenuation represents ionic edema, diffusion impairment on DWI depicts extracellular space shrinkage and consecutive cellular edema, showing brain areas with neuronal function failure, but does not exactly differentiate reversible and irreversible injury [45].
We did not calculate an infarct-growth rate (volume difference between follow-up infarct volume and baseline infarct volume divided by the time period between both images) because of our small sample size and relatively large proportion of patients without clear onset.
Lastly, final infarct volume assessment on FLAIR at day 3 post-stroke onset may be restricting [32] as ischemia is a dynamic process of cytotoxic, ionic, and vasogenic edema, and the influence of other factors on brain hypoperfusion has yet to be addressed in larger prospective studies. Yet, all patients underwent the same process and readers were allowed to evaluate the DWI sequence at the same time.
Conclusions
This preliminary study suggests that severely hypoperfused brain tissue defined as TMax > 10 sec volume on baseline CTP is strongly associated with final infarct volume and progression as well as clinical outcome after EVT recanalization of AIS due to DMVO.
Competing Interests
The authors have no competing interests to declare.
References
- 1.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet. 2016. Apr 23; 387(10029): 1723–31. DOI: 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 2.Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019. Dec; 50(12): e344–418. DOI: 10.1161/STR.0000000000000211 [DOI] [PubMed] [Google Scholar]
- 3.Saver JL, Chapot R, Agid R, et al. Thrombectomy for distal, medium vessel occlusions: A consensus statement on present knowledge and promising directions. Stroke. 2020. Sep; 51(9): 2872–84. DOI: 10.1161/STROKEAHA.120.028956 [DOI] [PubMed] [Google Scholar]
- 4.Rikhtegar R, Mosimann PJ, Weber R, et al. Effectiveness of very low profile thrombectomy device in primary distal medium vessel occlusion, as rescue therapy after incomplete proximal recanalization or following iatrogenic thromboembolic events. J Neurointerv Surg. 2021. Dec; 13(12): 1067–72. DOI: 10.1136/neurintsurg-2020-017035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ospel JM, Menon BK, Demchuk AM, et al. Clinical course of acute ischemic stroke due to medium vessel occlusion with and without intravenous alteplase treatment. Stroke. 2020. Nov; 51(11): 3232–40. DOI: 10.1161/STROKEAHA.120.030227 [DOI] [PubMed] [Google Scholar]
- 6.Mistry EA, Dumont AS. Medium vessel occlusion and acute ischemic stroke. Stroke. 2020. Nov; 51(11): 3200–2. DOI: 10.1161/STROKEAHA.120.032357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vagal AS, Sucharew H, Prabhakaran S, et al. Final infarct volume discriminates outcome in mild strokes. Neuroradiol J. 2015. Aug 1; 28(4): 404–8. DOI: 10.1177/1971400915609347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Padroni M, Bernardoni A, Tamborino C, et al. Cerebral blood volume ASPECTS is the best predictor of clinical outcome in acute ischemic stroke: A retrospective, combined semi-quantitative and quantitative assessment. PLoS One. 2016. Jan 29; 11(1): e0147910. DOI: 10.1371/journal.pone.0147910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ospel JM, Hill MD, Menon BK, et al. Strength of association between infarct volume and clinical outcome depends on the magnitude of infarct size: Results from the ESCAPE-NA1 trial. American Journal of Neuroradiology. 2021. Aug; 42(8): 1375–9. DOI: 10.3174/ajnr.A7183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meng X, Ji J. Infarct volume and outcome of cerebral ischaemia, a systematic review and meta-analysis. Int J Clin Pract. 2021. Nov 12; 75(11). DOI: 10.1111/ijcp.14773 [DOI] [PubMed] [Google Scholar]
- 11.Dávalos A, Toni D, Iweins F, Lesaffre E, Bastianello S, Castillo J. Neurological deterioration in acute ischemic stroke. Stroke. 1999. Dec; 30(12): 2631–6. DOI: 10.1161/01.str.30.12.2631 [DOI] [PubMed] [Google Scholar]
- 12.Barber PA, Darby DG, Desmond PM, et al. Identification of major ischemic change. Stroke. 1999. Oct; 30(10): 2059–65. DOI: 10.1161/01.str.30.10.2059 [DOI] [PubMed] [Google Scholar]
- 13.Dostovic Z, Dostovic E, Smajlovic D, Avdic O. Brain edema after ischaemic stroke. Medical Archives. 2016; 70(5): 339. DOI: 10.5455/medarh.2016.70.339-341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foroushani HM, Hamzehloo A, Kumar A, et al. Accelerating prediction of malignant cerebral edema after ischemic stroke with automated image analysis and explainable neural networks. Neurocrit Care. 2022. Apr 20; 36(2): 471–82. DOI: 10.1007/s12028-021-01325-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santana-Cabrera L, Ocampo-Pérez J, Rodríguez-Escot C, Granados-Rodríguez M, Rodríguez-Pérez H. Safety and outcomes of decompressive craniectomy after intravenous tissue plasminogen activator administration for malignant cerebral infarction. Br J Neurosurg. 2016. Mar 3; 30(2): 274–6. DOI: 10.3109/02688697.2016.1161177 [DOI] [PubMed] [Google Scholar]
- 16.Brondani R, Garcia de Almeida A, Abrahim Cherubini P, et al. high risk of seizures and epilepsy after decompressive hemicraniectomy for malignant middle cerebral artery stroke. Cerebrovasc Dis Extra. 2017. Mar 30; 7(1): 51–61. DOI: 10.1159/000458730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Casolla B, Kuchcinski G, Kyheng M, et al. Infarct volume before hemicraniectomy in large middle cerebral artery infarcts poorly predicts catastrophic outcome. Stroke. 2020. Aug; 51(8): 2404–10. DOI: 10.1161/STROKEAHA.120.029920 [DOI] [PubMed] [Google Scholar]
- 18.Nogueira RG, Gupta R, Jovin TG, et al. Predictors and clinical relevance of hemorrhagic transformation after endovascular therapy for anterior circulation large vessel occlusion strokes: A multicenter retrospective analysis of 1122 patients. J Neurointerv Surg. 2015. Jan; 7(1): 16–21. DOI: 10.1136/neurintsurg-2013-010743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marsh EB, Llinas RH, Schneider ALC, et al. Predicting hemorrhagic transformation of acute ischemic stroke. Medicine. 2016. Jan; 95(2): e2430. DOI: 10.1097/md.0000000000002430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elsaid N, Mustafa W, Saied A. Radiological predictors of hemorrhagic transformation after acute ischemic stroke: An evidence-based analysis. Neuroradiol J. 2020. Apr 23; 33(2): 118–33. DOI: 10.1177/1971400919900275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Austein F, Fischer AC, Fiehler J, Jansen O, Lindner T, Gellißen S. Value of perfusion CT in the prediction of intracerebral hemorrhage after endovascular treatment. Stroke Res Treat. 2021. Jul 22; 2021: 1–9. DOI: 10.1155/2021/9933015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wouters A, Robben D, Christensen S, et al. Prediction of stroke infarct growth rates by baseline perfusion imaging. Stroke. 2022. Feb; 53(2): 569–77. DOI: 10.1161/STROKEAHA.121.034444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abdelkhaleq R, Kim Y, Khose S, et al. Automated prediction of final infarct volume in patients with large-vessel occlusion acute ischemic stroke. Neurosurg Focus. 2021. Jul; 51(1): E13. DOI: 10.3171/2021.4.FOCUS21134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hakim A, Christensen S, Winzeck S, et al. Predicting infarct core from computed tomography perfusion in acute ischemia with machine learning: Lessons from the ISLES challenge. Stroke. 2021. Jul; 52(7): 2328–37. DOI: 10.1161/STROKEAHA.120.030696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jadhav AP, Desai SM, Panczykowski DM, et al. Predicting outcomes after acute reperfusion therapy for basilar artery occlusion. Eur J Neurol. 2020. Nov 28; 27(11): 2176–84. DOI: 10.1111/ene.14406 [DOI] [PubMed] [Google Scholar]
- 26.Amukotuwa SA, Wu A, Zhou K, Page I, Brotchie P, Bammer R. Distal medium vessel occlusions can be accurately and rapidly detected using Tmax maps. Stroke. 2021. Oct; 52(10): 3308–17. DOI: 10.1161/STROKEAHA.120.03294 [DOI] [PubMed] [Google Scholar]
- 27.Amukotuwa SA, Wu A, Zhou K, Page I, Brotchie P, Bammer R. Time-to-maximum of the tissue residue function improves diagnostic performance for detecting distal vessel occlusions on CT angiography. American Journal of Neuroradiology. 2021. Jan 11; 42(1): 65–72. DOI: 10.3174/ajnr.A689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. The Lancet. 2007. Oct; 370(9596): 1453–7. DOI: 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 29.Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018. Mar; 49(3). DOI: 10.1161/STR.0000000000000158 [DOI] [PubMed] [Google Scholar]
- 30.Olivot JM, Mlynash M, Inoue M, et al. Hypoperfusion intensity ratio predicts infarct progression and functional outcome in the DEFUSE 2 cohort. Stroke. 2014. Apr; 45(4): 1018–23. DOI: 10.1161/STROKEAHA.113.003857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brant-Zawadzki M, Atkinson D, Detrick M, Bradley WG, Scidmore G. Fluid-Attenuated Inversion Recovery (FLAIR) for assessment of cerebral infarction. Stroke. 1996. Jul; 27(7): 1187–91. DOI: 10.1161/01.str.27.7.1187 [DOI] [PubMed] [Google Scholar]
- 32.Sibon I, Ménégon P, Orgogozo J, et al. Inter- and intraobserver reliability of five MRI sequences in the evaluation of the final volume of cerebral infarct. Journal of Magnetic Resonance Imaging. 2009. Jun 26; 29(6): 1280–4. DOI: 10.1002/jmri.21779 [DOI] [PubMed] [Google Scholar]
- 33.Guenego A, Fahed R, Albers GW, et al. Hypoperfusion intensity ratio correlates with angiographic collaterals in acute ischaemic stroke with M1 occlusion. Eur J Neurol. 2020. May 13; 27(5): 864–70. DOI: 10.1111/ene.14181 [DOI] [PubMed] [Google Scholar]
- 34.Becks MJ, Manniesing R, Vister J, Pegge SAH, Steens SCA, van Dijk EJ, et al. Brain CT perfusion improves intracranial vessel occlusion detection on CT angiography. Journal of Neuroradiology. 2019. Mar; 46(2): 124–9. DOI: 10.1016/j.neurad.2018.03.003 [DOI] [PubMed] [Google Scholar]
- 35.Fainardi E, Busto G, Rosi A, et al. T max volumes predict final infarct size and functional outcome in ischemic stroke patients receiving endovascular treatment. Ann Neurol. 2022. Jun 2; 91(6): 878–88. DOI: 10.1002/ana.26354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Keenan KJ, Christensen S, Inoue M, Mlynash M, Albers GW, Smith WS. Validation and iteration of CT perfusion defined malignant profile thresholds for acute ischemic stroke. International Journal of Stroke. 2020. Jan 22; 15(1): 55–60. DOI: 10.1177/1747493019832987 [DOI] [PubMed] [Google Scholar]
- 37.Wan Z, Meng Z, Xie S, et al. Correlation between hypoperfusion intensity ratio and functional outcome in large-vessel occlusion acute ischemic stroke: Comparison with multi-phase CT angiography. J Clin Med. 2022. Sep 7; 11(18): 5274. DOI: 10.3390/jcm11185274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seker F, Pfaff J, Potreck A, et al. Correlation of T max volumes with clinical outcome in anterior circulation stroke. Brain Behav. 2017. Sep 26; 7(9). DOI: 10.1002/brb3.772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tisserand M, Seners P, Turc G, et al. Mechanisms of unexplained neurological deterioration after intravenous thrombolysis. Stroke. 2014. Dec; 45(12): 3527–34. DOI: 10.1161/STROKEAHA.114.006745 [DOI] [PubMed] [Google Scholar]
- 40.Nagakane Y, Christensen S, Ogata T, et al. Moving beyond a single perfusion threshold to define penumbra: A novel probabilistic mismatch definition. Stroke. 2012. Jun; 43(6): 1548–55. DOI: 10.1161/STROKEAHA.111.643932 [DOI] [PubMed] [Google Scholar]
- 41.Alawneh JA, Moustafa RR, Baron JC. Hemodynamic factors and perfusion abnormalities in early neurological deterioration. Stroke. 2009. Jun; 40(6): e443–50. DOI: 10.1161/STROKEAHA.108.532465 [DOI] [PubMed] [Google Scholar]
- 42.Seners P, Hurford R, Tisserand M, et al. Is Unexplained early neurological deterioration after intravenous thrombolysis associated with thrombus extension? Stroke. 2017. Feb; 48(2): 348–52. DOI: 10.1161/STROKEAHA.116.015414 [DOI] [PubMed] [Google Scholar]
- 43.Rao V, Christensen S, Yennu A, et al. Ischemic core and hypoperfusion volumes correlate with infarct size 24 hours after randomization in DEFUSE 3. Stroke. 2019. Mar; 50(3): 626–31. DOI: 10.1161/STROKEAHA.118.023177 [DOI] [PubMed] [Google Scholar]
- 44.Yedavalli V, Hamam O, Mohseni A, et al. Pretreatment brain CT perfusion thresholds for predicting final infarct volume in distal medium vessel occlusions. Journal of Neuroimaging. 2023. Jun 25; DOI: 10.1111/jon.13142 [DOI] [PubMed] [Google Scholar]
- 45.Fiehler J, Foth M, Kucinski T, et al. Severe ADC decreases do not predict irreversible tissue damage in humans. Stroke. 2002. Jan; 33(1): 79–86. DOI: 10.1161/hs0102.100884 [DOI] [PubMed] [Google Scholar]


