Abstract
This paper reviews ultrasound of the hip, which is a commonly requested examination for symptomatic hip issues. This includes both intra-articular and extra-articular causes of hip pain. Ultrasound is easily accessible, lacks radiation exposure, and allows for evaluation of the contralateral hip as well as assessment of dynamic maneuvers. Ultrasound can be used to guide interventional procedures. Ultrasound of the hip can be challenging due to the deep location of structures and complex anatomy. Typically, high-frequency transducers are used to examine the hip, however the choice of ultrasound transducer depends on the patient’s body habitus, with lower frequency transducers required to penetrate deep structures in obese patients. It is important to have an approach to ultrasound of the hip which includes assessment of the anterior, lateral, posterior, and medial aspects of the hip. The technique and relevant anatomy of each of these compartments are discussed as well as the use of Doppler examination of the hip. Several dynamic maneuvers can be performed to help determine the cause of hip pathology in various locations, and these are described and illustrated. Ultrasound is useful for guided procedures about the hip, and these indications will be reviewed.
Keywords: ultrasound, hip joint, hip anatomy, dynamic ultrasound, hip pathology
Introduction
Hip ultrasound (US) is a commonly requested examination for a variety of clinical indications, both intra-articular and extra-articular. It is easily accessible, lacks radiation exposure, allows for evaluation of the contralateral hip as well as dynamic maneuvers, and can be used to guide interventional procedures. However, US of the hip can be challenging due to the deep location of structures and complex anatomy(1). Typically, high-frequency 5 to 18 MHz transducers are used. The choice depends on the patient’s body habitus, with lower frequency transducers required to penetrate deep structures in obese patients.
It is important to have a systematic approach to hip US, as hip pain can often be non-specific. While a targeted evaluation can be performed, it is usually appropriate to assess both the anterior hip for an effusion and the lateral hip for bursitis in every examination, as these are common causes of hip pain.
Various guidelines discuss US imaging of the hip(2). This paper reviews an approach to evaluation of the adult hip, including the anterior, lateral, posterior, and medial hip, and demonstrates the importance of dynamic maneuvers for certain indications. The use of US guidance for interventional procedures is also briefly discussed.
Anterior hip
Technique and normal anatomy
US of the anterior hip is performed to assess for joint effusion, synovitis, proximal quadriceps injury, and causes of snapping hip syndrome. This is usually the first area of the hip to be examined, and it is readily accessible in most patients. The structures to be assessed in the anterior hip are the anterior joint recess for joint effusion and paralabral cyst, iliopsoas and rectus femoris myotendinous complexes/tendons, lateral femoral cutaneous nerve and anterior femoral neurovascular structures including the femoral vein, femoral artery and femoral nerve.
The patient is positioned supine, with the hip and knee extended. In the first instance, the transducer should be placed in an oblique longitudinal plane over the region of the femoral head/neck junction in order to assess the anterior joint recess (Fig. 1). Just cranial to the femoral head lies the fibrocartilaginous acetabular labrum, which should be homogenously hyperechoic. The iliofemoral ligament can be seen superficial to the anterior acetabular labrum. This ligament extends from the anterior inferior iliac spine and runs obliquely over the anterior aspect of the hip joint to attach to the intertrochanteric line of the femur. Its role is to prevent overextension of the hip joint and limit external rotation when the hip is flexed.
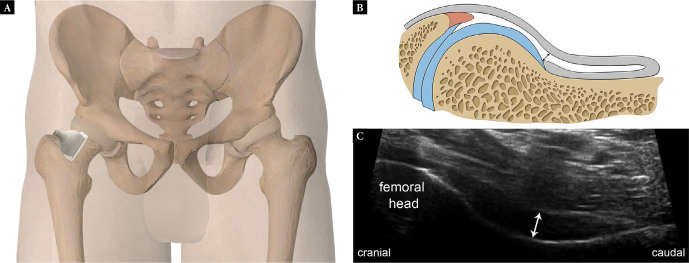
Fig. 1.
Normal anterior joint recess. Graphic illustrations (A, B) showing the transducer position (A) and equivalent anatomy (B) for long-axis scanning of the anterior hip joint recess. Long-axis US image (C) is depicted. Double-headed arrows in B and C demonstrate measurement of the recess (US image shows a recess measuring 5 mm)
The iliopsoas tendon is readily imaged just proximal to the level of the hip joint. The tendons of the psoas and iliacus muscles come together to form the iliopsoas tendon distally. Sometimes, these can be seen as separate structures, particularly proximally, where the psoas tendon forms before the iliacus tendon. Transverse and transverse oblique scans are optimal for evaluating both muscular and tendinous components (Fig. 2). The tendon is located eccentrically within the deep portion of the muscle, appearing as a hyperechoic, fibrillar structure which lies superficial to the pectineal eminence.
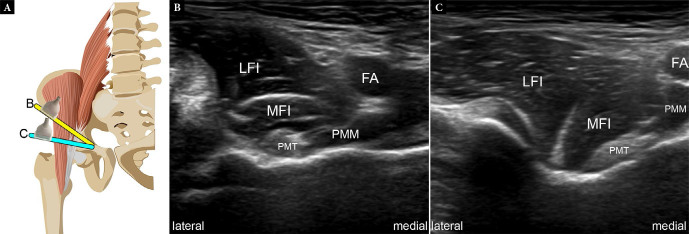
Fig. 2.
Normal iliopsoas myotendinous junction (MTJ) complex on US. Graphic illustration (A) showing normal transducer positions and equivalent short-axis oblique (B) and short-axis (C) US images (LFI – lateral iliacus muscle; MFI – medial iliacus muscle; PMT – psoas tendon; PMM – psoas major muscle; FA – femoral artery). Fig. 2 A is modified with permission from Flores et al.(3)
As it courses towards its insertion at the lesser trochanter, it is best assessed on longitudinal oblique scanning, appearing superficial to the acetabular margin and the anterior femoral head (Fig. 3). The iliopsoas bursa is assessed along with the iliopsoas tendon and best delineated when expanded by fluid. Hip joint effusion can distend the bursa when there is excessive intra-articular pressure. Large collections may compress the adjacent femoral nerve. The bursa can be differentiated from a paralabral cyst by its compressibility upon transducer pressure(4).
Fig. 3.
Normal iliopsoas tendon on US. Graphic illustration (A) and long-axis US image (B) show normal iliopsoas tendon (arrowheads) (LT – lesser trochanter with contour outlined in light blue). Fig. 3 A is modified with permission from Flores et al.(3)
The proximal rectus femoris tendon and the myotendinous junction (MTJ) are commonly injured and can be assessed with US. The rectus femoris has three separate tendinous origins: the straight or direct head which originates from the anterior inferior iliac spine, and the reflected or indirect head which arises from the superior lateral acetabular ridge. A third smaller capsular head has also been described in the literature but is not well seen on imaging(5). These tendons merge a few centimeters distal to the origin to form the conjoint tendon(6). In order to assess the proximal rectus femoris tendons on US, the patient should be in the supine position, with the hip extended. The examination should be performed with a moderate- to high-frequency transducer. The direct head tendon is easily seen in either a transverse or longitudinal plane with the transducer placed anteriorly over the anterior superior iliac spine (Fig. 4). In this position, the indirect head will appear hypoechoic in nature with posterior acoustic shadowing. To see the reflected head, the transducer will need to be positioned obliquely in a more lateral position due to the angle of origin of this tendon. The direct head ultimately forms the anterior and more superficial tendon within the rectus femoris, and the indirect head forms the central tendon or central aponeurosis. Deep to the rectus femoris muscle, the vastus muscles will be seen in the proximal thigh. Superficial to the proximal rectus femoris muscle in its proximal aspect, the sartorius muscle is present on the medial side, and the tensor fascia lata on the lateral side.
Fig. 4.
Normal rectus femoris anatomy. Graphic illustration (A) showing normal transducer positions and equivalent long-axis US images of the direct head (arrowheads) (B) and indirect head (arrows) (C) origins (blue outline – direct head origin at the ASIS; yellow outline – indirect head origin at the acetabular ridge)
The lateral femoral cutaneous nerve of the thigh is a branch of the lumbar plexus which arises from the posterior rami of the 2nd and 3rd lumbar nerves(7). It passes directly through the psoas muscle, and after emerging from its lateral border (Fig. 5), it runs over the anterior surface of the iliacus towards the anterior superior iliac spine. The anatomy at this level is slightly variable, with the nerve lying medial to the ASIS in 62% of cases, superficial in 27% of cases, and lateral to the ASIS in 11% of cases(8). It is in this location that the nerve is readily assessed on US, while also allowing for symptomatic steroid injection in the setting of meralgia paraesthetica. Scanning distally from the level of the ASIS with the transducer in a transverse plane, the nerve can then be followed as it courses over the anterior surface of the sartorius muscle.
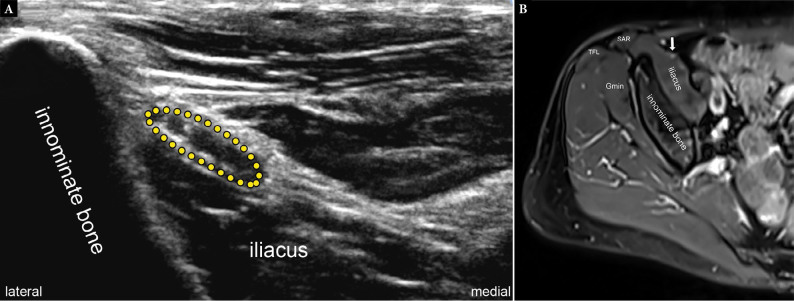
Fig. 5.
Normal US and MRI of the LFCN. Short-axis US image (A) and axial PD-weighted fat-suppressed MR image (B) at the level of the iliacus muscle show a normal LFCN (yellow dotted outline in A and arrow in B) medial to the innominate bone and superficial to the iliacus muscle (Gmin – gluteus minimus; SAR – sartorius, TFL – tensor fascia lata)
Pathology
Joint effusion
Signs of joint effusion are not readily detected on clinical examination and, therefore, they are best evaluated under US. A joint effusion can be seen as a region of anechoic or hypoechoic fluid which distends the anterior capsule (Fig. 6). It can be assessed by measuring the distance between the anterior femoral neck and the joint capsule. A joint effusion has been described to be present if the distance measured is over 7 mm or if the distance is over 1 mm greater than on the contralateral side(9). Anterior recess distention and echogenicity have been shown to be unreliable indicators of adult hip joint effusion, either in native or postoperative hips, and arthrocentesis may be needed in some instances, such as infection. Distention may have no fluid but may be due to synovitis. Positioning is also important, as internal rotation can distort the capsule, resulting in an artifactually thickened recess greater than 7 mm. In some instances (i.e. prior surgery), fluid may be loculated(10,11).
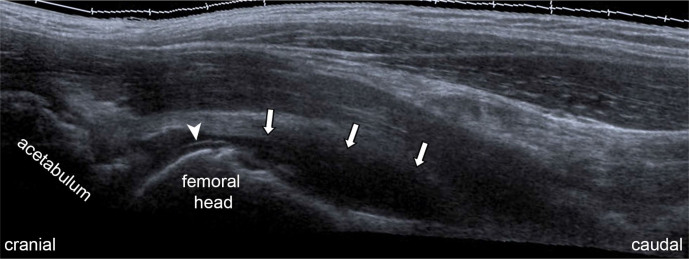
Fig. 6.
Joint effusion on US. Long-axis US image in an adult patient, with clinical concern for joint effusion, demonstrates joint fluid pooling in the anterior joint recess (arrows). The presence o fluid outlines the cartilage (arrowhead), making it more conspicuous (cartilage conspicuity sign)
A joint effusion in a healthy asymptomatic adult is uncommon(9). However, in conditions such as inflammatory arthropathy or septic arthritis, a joint effusion is often present; studies have shown that there is a relationship between the presence of a joint effusion and clinical signs(12). An effusion in cases of osteoarthritis (OA) is thought to be uncommon, so the presence of a large effusion should raise the possibility of rapidly progressive OA(13). There may also be synovitis, which will be seen as hypoechoic or anechoic intra-articular soft tissue which is non-compressible(14). In addition, synovitis will usually display a degree of Doppler signal.
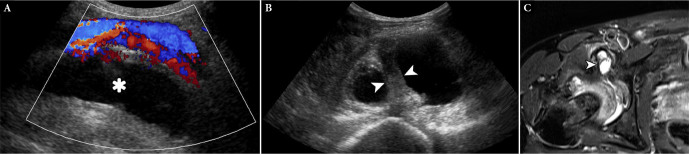
The ability of US to assess fluid collections is especially useful in screening for pseudotumors in the setting of total hip arthroplasty (THA) or other hardware which may produce artifacts on CT or MRI (Fig. 7).
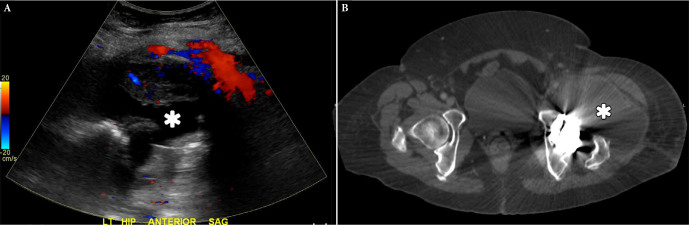
Fig. 7.
THA pseudotumor in a 60-year-old female with left hip swelling. Screening US was requested and long-axis US image of the left hip (A) shows large fluid collection (*) with hyperemia on color Doppler interrogation at the anterior aspect of the left hip. Transverse CT image of the pelvis (B) was requested the next day, confirming the pseudotumor (*). Note the streak artifacts emanating from the hardware on the CT image, though the large size of the pseudotumor enabled easy visualization
Paralabral cyst
Acetabular labral tears are common and found at arthroscopy in up to 55% of cases of intractable hip pain(15). Tears of the labrum may be seen in the anterior position, and the majority of symptomatic tears are seen within the anterior superior quadrant(16). The findings manifest as a cleft within the anterior labrum, with hypoechoic fluid tracking into the region of tearing. In addition, an associated paralabral cyst may be identified on US imaging as a well-defined hypoechoic region which lies adjacent to the acetabular wall, often connecting to the labrum (Fig. 8).
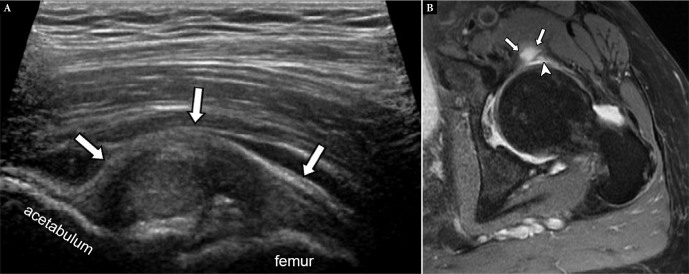
Fig. 8.
Anterosuperior paralabral cyst in a 70-year-old female with left hip pain of 4 months’ duration. Long-axis US image at the level of the hip (A) shows a complex lesion (arrows) arising from the joint space. This was noncompressible on transducer pressure, raising the possibility of a paralabral cyst. Axial PD-weighted fat-suppressed MR image (B) confirms a paralabral cyst (arrows) associated with an underlying labral tear (arrowhead)
Tendon/musculotendinous pathology
The tendons/musculotendinous complexes of interest in the anterior hip are the iliopsoas and rectus femoris. In tendinopathy, the iliopsoas tendon appears thickened and enlarged, with loss of the usual fibrillar structure. This is a common cause of groin pain following total hip arthroplasty(17).
Partial tears of the iliopsoas tendon tend to occur in athletic injury. Spontaneous full-thickness injury of the iliopsoas tendon is uncommon but has been described in the elderly with associated risk factors including advanced age, steroid use, and chronic disease(18) (Fig. 9). Tears usually occur near the tendinous attachment, at or close to the lesser trochanter(19).
Fig. 9.
Iliopsoas avulsion in a 90-year-old female with suspected joint effusion. Long-axis US at the level of the femoral head (A) shows a curvilinear echogenic lesion with marked shadowing (arrowheads) at the level of the femoral head, raising the possibility of an avulsed fracture fragment likely related to the iliopsoas. Radiographs were requested. AP radiograph (B) confirmed an avulsed bony fragment (arrowhead) along with a frank pathologic fracture of the proximal femoral diaphysis
The iliopsoas bursa is a large synovial bursa which lies between the iliopsoas tendon and the anterior capsule of the hip. This is the largest bursa in the human body, extending proximally under the iliacus muscle to the pelvic brim. The bursa is usually collapsed and not perceptible on US; its function is to reduce friction associated with the movement of the tendon over the anterior hip(20). On US, a distended bursa is deep to the femoral vessels and superficial over the iliopsoas tendon; it may appear compartmentalized when the tendon is bifid or contains multiple slips (Fig. 10). The iliopsoas bursa frequently communicates with the hip joint, so joint disease and joint effusion may led to distension of the bursa(21).
Fig. 10.
Iliopsoas bursal fluid in a 68-year-old female with right hip and groin pain, query labral tear. Long-axis (A) and short-axis (B) US images show a large fluid collection (*) deep to the femoral vessels. It appears to be compartmentalized on short-axis image related to a prominent band of tissue suspected to be either a septation, a bifid or slip of the psoas tendon (arrowheads in B). Axial PD-weighted fat-suppressed MR image (C) confirms the bursal fluid and the band of tissue (arrowhead in C), which was confirmed to be a bifid tendon on the rest of the axial MR images. A hip joint effusion is also noted
Dynamic US may identify mechanical snapping of the iliopsoas tendon, but this is not seen in all cases of clinical snapping hip. A study looking at static and dynamic US in patients with clinical features of ’snapping hip’ showed that in only 9 out of 40 patients was snapping actually demonstrated on the US study(22). The transducer should be placed in a transverse oblique plane over the anterior hip, at the level of the iliopsoas tendon: the patient should then be asked to place their leg into the frog leg position: flexion, abduction, external rotation position, and then subsequently to extend the leg. During the first phase of the movement, the tendon itself rotates laterally and comes to lie anteriorly within the muscle. As the leg is extended, the tendon should then rotate smoothly back to its posteromedial position. In cases of the snapping hip, the tendon will abruptly flip back to its original posterior position rather than moving in a smooth fashion (Video 1).
The rectus femoris is the most commonly injured of the quadriceps muscles, with injury to the proximal tendon and myotendinous junction often seen in kicking sports such as soccer. The facts that the muscle spans over two joints, and has predominantly type II fibers and a long fusiform shape, all contribute to its susceptibility to injury(23). In young people, avulsion of the rectus femoris origin may be seen at the apophysis at the anterior inferior iliac spine. In this instance, a bony fragment may be identified on US, surrounded by anechoic fluid. Intrasubstance tearing of the proximal tendon and proximal myotendinous junction injury are more common in skeletally mature individuals. Either one head or both may be involved in proximal injury. Features of an acute muscle injury include ill-defined hyper- or hypoechoic lesions within the muscle associated with disruption of the muscle fibers(24). Subsequent scar formation with the healed or healing muscle will be seen as a hyperechoic focus within the muscle at the site of previous injury, with a varying degree of retraction of the muscle fibers(24).
Interventions about the anterior hip
Interventions around the hip for either diagnostic or therapeutic purposes may be undertaken in a variety of pathologies. A steroid or anesthetic injection into the hip joint is usually performed using an anterior approach. It may be undertaken for the symptomatic relief of either inflammatory arthritis or osteoarthritis, to assess the source of pain or to introduce contrast into the joint prior to CT or MRI arthrogram. The same technique is used for US-guided aspiration of a joint effusion. This can be performed with the transducer in the longitudinal oblique plane, with the needle angled along the line of transducer down onto the femoral neck.
Injection may also be considered in cases or snapping hip, particularly that of a snapping iliopsoas tendon. There may be associated bursitis or tendinopathic change to the iliopsoas tendon, however, imaging of the tendon itself will often be normal. Injection of a corticosteroid around the deep surface of the iliopsoas tendon at the level of the anterior hip joint may be considered for symptomatic relief in patients who have pain associated with the snapping sensation. A study of patients who presented with groin pain and clinical snapping of the iliopsoas tendon showed that these patients could benefit from US-guided injection of the iliopsoas bursa, even when snapping is not demonstrated sonographically(22).
Finally, an injection around the lateral femoral cutaneous nerve can be performed for symptoms of meralgia paresthetica(25).
Lateral hip
Technique and normal anatomy
The most common indication for imaging of the lateral hip is greater trochanteric pain syndrome (GTPS). The structures to be assessed in the lateral hip include the hip “rotator cuff” or the abductors, intervening bursae, iliotibial band, and surrounding soft tissues.
The patient is asked to lie on the non-symptomatic side, with the hips and knees flexed (Fig. 11). Transverse scans are obtained with the transducer at the level of the greater trochanter perpendicular to the long axis of the femur. This plane is useful for determining pathology at the greater trochanter and the relationship of gluteus tendons with the iliotibial band (ITB) and with each other. Longitudinal scans confirm transverse scan findings and depict intrasubstance pathology.
Fig. 11.
Graphic illustration showing normal transducer position for assessing the lateral hip. For evaluation of the gluteus tendons at the facets, the transducer can be swept anterior to posterior and vice-versa (doubleheaded curved arrow)
The hip abductors, gluteus medius and minimus, are first localized by delineating the trochanteric facets onto which they attach, analogous to the tendons and facets about the shoulder(26,27). The key landmarks are the apex between the anterior and lateral facets, and the more rounded superoposterior facet situated posterior to the lateral facet(28). Overlying the echogenic contours of the facets are the round or ovoid tendons with multiple echogenic dots or lines. The gluteus minimus tendon is identified over the anterior facet; the gluteus medius over the lateral facet; and the gluteus maximus over the superoposterior facet (Fig. 12)(28). The main tendon of the gluteus minimus attaches to the anterior facet, while a thinner short muscular component inserts along the ventral superior capsule of the hip joint(29,30). It is the main tendon that is readily assessed on transverse US; its oblique course as it inserts onto the anterior facet may be subject to anisotropy on longitudinal scanning(29). Superficial to the gluteus minimus tendon over the anterior facet is the hypoechoic muscle of the gluteus medius and the iliotibial tract or band (ITB)(28). The gluteus medius tendon attaches to the anterosuperior portion of the greater trochanter over a broad U-shaped area(29). It can be further localized by shifting the transducer over its posterior fibers, which are covered by the hypoechoic anterior gluteus maximus muscle. The posterior fibers of the tendon form a thick band which becomes thinner further anteriorly(29).
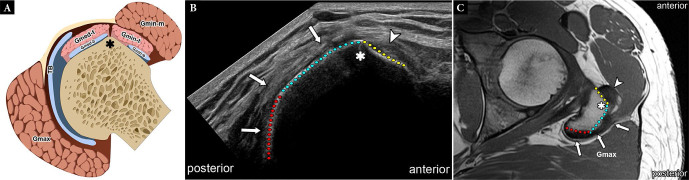
Fig. 12.
Normal facets. Graphic illustration (A), short-axis US image (B) and axial T1-weighted MR image (C) show normal facets. The anterior (yellow dotted outline) and lateral (light blue dotted outline) facets are demarcated by a sharp bony angulation (*) while the contour between the lateral and posterior (red dotted outline in B and C) curves more gently. The gluteus minimus tendon (arrowheads in B and C) attaches to the anterior facet, while the gluteus medius tendon (arrows in B and C) to the lateral and superoposterior facets. Intervening bursae are also shown (Gmed-t – gluteus medius tendon; Gmed- m – gluteus medius muscle; Gmin-t – gluteus minimus tendon; Gmin-m – gluteus minimus muscle; Gmax – gluteus maximus muscle; TB – trochanteric bursa; Gmed-b – subgluteus medius bursa; Gmin-b – subgluteus minimus bursa; Gmax – gluteus maximus muscle)
The gluteus tendons are interspersed with bursae at the level of the greater trochanter. The greater trochanteric bursa is located at the echogenic interface of the gluteus medius tendon and gluteus maximus muscle (Fig. 13)(31), whereas the subgluteus medius bursa is deep to the gluteus medius tendon, and the subgluteus minimus bursa deep to the gluteus minimus tendon. All three bursae are imperceptibly thin under normal, nondistended conditions. Moving the transducer cranial to the greater trochanter shows the hypoechoic gluteus medius (superficial) and gluteus minimus (deep) muscles; the two are separated by an echogenic layer of fascia and fat(29). The ITB covers the tensor fascia lata anteriorly, and the gluteus maximus muscle and gluteal aponeurotic fascia posteriorly(32). It consists of three layers that fuse in the region of the greater trochanter, although the ITB itself does not insert onto the greater trochanter(32). It extends, abducts, and laterally rotates the hip. On US, it appears as a single thin hyperechoic linear stripe with a fibrillar pattern(31).
Fig. 13.
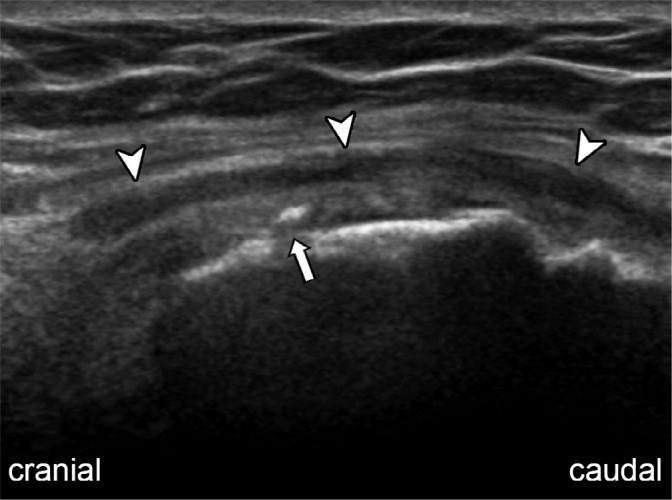
Small amount of trochanteric bursal fluid in a 84-year-old female with THA and concern for a pseudotumor. Long-axis US image of the greater trochanter shows trace fluid in the overlying trochanteric bursa (arrowheads). There is a small enthesophyte (arrow) adjacent to the greater trochanter
Pathology
Gluteus tendinosis and tears
Greater trochanteric pain syndrome (GTPS) consists of pain and tenderness over the greater trochanter, and it is diagnosed based on a combination of medical history, physical examination, and imaging findings. Risk factors include female gender in the sixth decade, femoral neck-shaft angle less than 134°, and leg length discrepancies(33). While GTPS was traditionally ascribed to trochanteric bursitis, it is increasingly recognized that gluteus tendinopathy and ITB pathology may be more significant contributors(29,34,35). The pathophysiology may be analogous to shoulder impingement, with attrition of the iliotibial band (ITB) and fascia lata against the abductor tendons being similar to the friction of the acromion against the rotator cuff(27). Recent studies also suggest an association with acetabular morphology and hip snapping(33).
Hip abductor or gluteal tendinopathy most commonly occurs near the tendon insertions at the trochanteric facets. It includes peritendinitis, tendinosis, partial tear, and complete rupture, which probably represents a pathologic continuum rather than isolated entities(35). Soft tissue edema surrounding the gluteus minimus or gluteus medius tendons represents peritendinitis and is the earliest sign of gluteal tendinopathy(35); tendon architecture remains intact. Tendinosis refers to a degenerated tendon and is often seen in middle-aged individuals, both in athletes and sedentary subjects; females are more commonly affected compared to males(36). On US, this appears as a thickened and heterogeneous tendon with some loss of the normal fibrillar pattern, either with or without superimposed calcification(29,34)(Fig. 14). Increased vascularity on color or power Doppler and tendon tenderness on sonopalpation are ancillary signs of tendinosis but are uncommon in clinical practice(35).
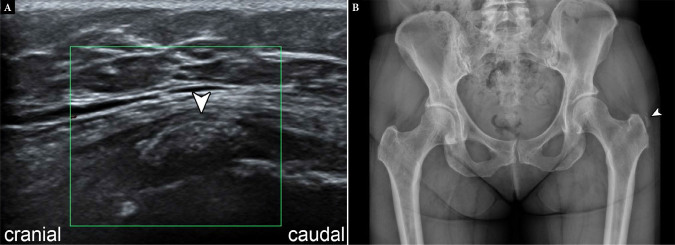
Fig. 14.
Calcific tendinosis in a 57-year-old female with severe left hip pain when lying on side. Long-axis US image (A) shows faint echogenic lesion adjacent to the greater trochanter (arrowhead). There is no significant hyperemia on color Doppler interrogation. AP radiograph of the pelvis (B) confirms calcification consistent with calcific tendinosis by the left greater trochanter
In Bunker and colleagues’ original description of hip rotator cuff tears and subsequent studies thereafter, gluteus tendon tears can occur during the following scenarios: (1) at the time of THA or hemiarthroplasty for fractures of the neck of the femur; (2) avulsion following THA performed via an anterolateral or trans-gluteal approach (3) chronic, non-traumatic tear in pre-existing tendinosis; and (4) trauma or spontaneously. Gluteus tendon tears often occur as the by-product of long-standing tendon degeneration or tendinosis rather than an acute traumatic event(26,37,38). A partial tear is seen as focal discontinuity in the fibrillar pattern of the tendon(34). It can also present with discrete anechoic foci or intrasubstance clefts(29). A complete tear is a full-thickness interruption of the tendon fibers that may either be fluid-filled or depicted by loss of tendon mass(34). A “bald” facet and avulsed bone fragment are compatible with a complete tear(26,35). Lengthening of the gluteus medius tendon between the musculotendinous junction and the insertion onto the greater trochanter which exceeds 2 cm is also an indirect sign of a tear(35). The anterior fibers of the gluteus medius tendon are the most common site of both partial and complete tears(29). The gluteus minimus tendon is rarely torn in isolation and is more commonly injured along with the gluteus medius tendon (Fig. 15)(29). Atrophy of the corresponding muscle may be seen in chronic partial or complete tears but it is nonspecific(26,38). Previous investigations have shown age-related progression from tendinosis to tears with associated advancement in muscle atrophy in the absence of injury(26,38). Cortical irregularity and enthesopathy of the greater trochanter are present in a vast majority of gluteus tendinopathy cases(29). Gluteus tendon tear is also an important cause of persistent hip pain after THA (Fig. 16). US is especially valuable as a post-operative imaging tool, allowing evaluation of the tendon without susceptibility artifact from the prosthesis or other hardware (Fig. 17).
Fig. 15.
Complete gluteus minimus tendon tear and partial width gluteus medius tendon tear in an 82-year-old female with symptoms of abductor insufficiency. Short-axis US image shows bare appearance of the anterior facet (yellow dotted outline) and part of the lateral facet (light blue dotted outline), consistent with complete gluteus minimus and partial width gluteus medius tendon tears. The rest of the gluteus medius tendon fibers (arrows) are thickened but intact (border between anterior and lateral facets demarcated by *)
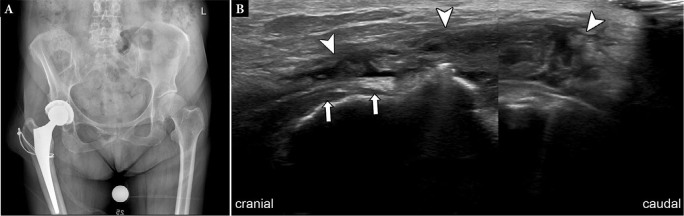
Fig. 16.
Partial intrasubstance tears and tendinosis of the gluteus medius in a 57-year-old female with lateral hip pain after THA, US ordered to evaluate for pseudotumor. AP radiograph of the pelvis (A) shows the right THA with a cerclage cable along the proximal femoral metaphysis. Long-axis US images (B) demonstrate thickening, irregularity, and small anechoic clefts within the gluteus medius tendon (arrowheads), consistent with partial intrasubstance tears and tendinosis. A few of the proximal fibers (arrows) appear intact
Fig. 17.
Gluteus medius tendon repair dehiscence in a 70-year-old woman with lateral hip pain after THA and abductor tendon repair. Short-axis US images of the left hip (A, B) and axial PD-weighted fat-suppressed MR image of the pelvis (C) show a bare lateral facet (light blue dotted outline), consistent with a high-grade dehiscence of the anterior gluteus medius tendon fibers. The more posterior fibers attaching to the superoposterior facet are tendinotic but intact arrowheads in A and C). Note the associated trochanteric bursal fluid (* in B and C)
Trochanteric bursitis
Abductor tendinopathy may present with bursal distension or inflammation (i.e. bursitis)(29). The association of gluteus tendinopathy with trochanteric bursitis has been likened by a few authors to rotator cuff abnormalities with subacromial bursitis(39). Caution must therefore be practiced in diagnosing isolated bursitis without careful scanning and scrutiny of the abductor tendons. On US, a normal bursa is collapsed and just represents a potential space(40). In such cases, its position may only be inferred from adjacent structures, with the greater trochanteric bursa being superficial to the gluteus medius tendon and deep to the ITB. Murray and colleagues recommend dynamic US to localize this bursa by alternatively internally and externally rotating the hip. This maneuver demonstrates the gluteus medius and minimus tendons sliding back and forth under the relatively static iliotibial band, and may be especially useful during US-guided injections(40). Gentle transducer pressure must be applied to avoid displacement or compression of the small amount of bursal fluid. The primary advantage of MRI over US is demonstrating bony changes in the trochanter and marrow edema. Bursal location is variable; it may be located adjacent to the superoposterior facet of the greater trochanter or between the lateral facet and the iliotibial band(35). Compared to MRI, which shows gluteus tendinosis or trochanteric bursitis even in asymptomatic patients(41), US enables concomitant clinical assessment by eliciting tenderness upon transducer pressure over the area of concern(34). Image-guided procedures performed to address lateral hip symptoms are directed towards managing GTPS either by steroid injection to the trochanteric bursa (Video 2) or dry needling the tendons(42).
External snapping
External snapping hip syndrome refers to abnormal “jerky” movement or transient subluxation of the junction between the iliotibial band and the anterior margin of the gluteus maximus muscle over the greater trochanter(43). Most cases are idiopathic, though femoral osteochondroma and other space-occupying masses can be implicated(43–45). Young individuals, especially those who engage in high-level athletic activities. are at increased risk(43). On US, findings include a thickened and hypoechoic iliotibial band, and a fluid-filled, inflamed trochanteric bursa(43). Dynamic evaluation of snapping is best performed on transverse scans (Video 3). Normal dynamic hip flexion and extension show a smooth gliding movement of the iliotibial band and anterior margin of the gluteus maximus muscle anteriorly during flexion and posteriorly during extension over the greater trochanter(43). Painful snapping is characterized by transient entrapment of the ITB and gluteus maximus against the posterolateral aspect of the greater trochanter during early flexion. With further flexion, the ITB and gluteus maximus escape and then suddenly move forward over the anterior edge of the lateral facet of the greater trochanter, producing the audible “snapping”43). The snapping may also be elicited while standing and leaning on the symptomatic side or during hip extension(43).
Morel-Lavallée lesion
The lateral aspect of the hip is a common site of the Morel-Lavallée lesion, or posttraumatic hematoma/seroma that extends along the trochanteric region and the proximal thigh. Motor vehicle collisions are the most common mechanism; low-velocity crush injury and contact sports such as football and wrestling are other causes(46). In the lateral hip, the superficial tissues (subcutaneous fat and dermis) are characteristically mobile compared to the relatively firm and immobile ITB, placing these tissues at risk of shearing injury, with accumulation of hemolymphatic fluid between these planes(46).
This lesion can occur in isolation but is more commonly associated with underlying fractures(46). Clinical symptoms are pain, swelling, and a soft fluctuant area of contour deformity, which may have skin mobility(46) (Fig. 18). Injury to the cutaneous nerves may result in decreased cutaneous sensation over the area of internal degloving. On US, they appear as nonspecific, compressible and avascular fluid collections with heterogeneous echogenicity, dependent on the stage of evolution of the blood products(46)(Fig. 19). Acute and subacute (<1 month) lesions have a heterogeneous appearance with irregular margins, whereas chronic lesions (>18 months) are frequently more homogeneous, with smooth margins and flat or fusiform shape(46). Light pressure with the transducer should be utilized when examining the collection to prevent compressing the bloody effusion away from the field-of-view(4). Collections with atypical features – such as marked heterogeneity – may appear similar to soft-tissue tumors, and may be further evaluated on MRI(4). On MRI, Morel-Lavallée lesions are classified into six types according to T1 and T2 appearances and enhancement features. Type I is a serohematic effusion or a seroma. Type II is a subacute hematoma, while type III is more chronic and organized hematoma. Types IV and V are both perifascial lesions. Type IV presents with perifascial dissection with closed fatty laceration, while type V manifests as a perifascial pseudonodular lesion. Type VI is an infected lesion with variable sinus tract formation, internal septations, and thick enhancing capsule. Although MRI is more optimal for classification, US contributes to treatment through image-guided intervention. US-aspiration, either with or without injection of sclerosing agents (doxycycline, erythromycin, alcohol, bleomycin, tetracycline, talc), has been shown to be helpful when compression banding fails(46).
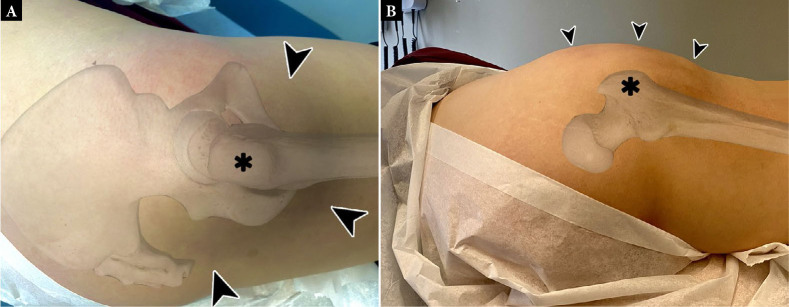
Fig. 18.
Clinical photograph of a Morel-Lavallée lesion in a ski cross athlete after a crash. Note the marked swelling over the lateral hip (arrowheads) centered on the greater trochanter (*)
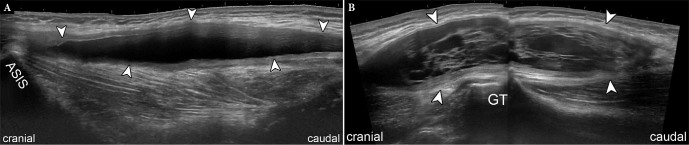
Fig. 19.
Morel-Lavallée lesion in a 32-year-old male who fell to his side during cycling. Long-axis US images (A, B) demonstrate a large, spindle-shaped complex fluid collection (arrowheads) adjacent to the greater trochanter (GT) extending to the anterior superior iliac spine (ASIS)
Posterior hip
Technique and normal anatomy
US of the posterior hip is performed primarily to assess for hamstring tendon pathology. Other structures to be evaluated are the ischiofemoral space in the setting of impingement, the sciatic nerve and surrounding bursae. The patient is placed prone on the examination bed; the knee may need to be flexed to facilitate internal and external rotation during assessment of ischiofemoral impingement.
The gluteus maximus muscle is the most superficial structure at the posterior aspect of the hip. The deep gluteal space lies deep to this, bound by the posterior cortex of the femoral neck, the joint capsule and posterior acetabular column anteriorly, the ischial tuberosity and common hamstring origin inferiorly, the sacrotuberous and falciform fascia medially, the linea aspera and greater trochanter laterally, and the inferior margin of the greater sciatic notch(47). The ischial tuberosity and greater trochanter are easily appreciated on US. The space contains the short external rotator muscles (piriformis, superior gemellus, obturator internus, inferior gemellus, and quadratus femoris), fat, and multiple neurovascular structures, most importantly the sciatic nerve.
The common hamstring tendons originate from the ischial tuberosity. The biceps femoris and semitendinosus tendons attach to the posteromedial facet as a conjoint tendon, and the semimembranosus tendon attaches anterolaterally(48). Distal to the attachment, at the proximal third of the femur, the conjoint tendons migrate superficial to the semimembranosus tendon to end up laterally(49,50) (Fig 20). The adductor magnus tendon is considered a ‘mini-hamstring muscle’ with an ischiochondylar origin that is indistinguishable from the hamstring tendons both functionally and on US(51).
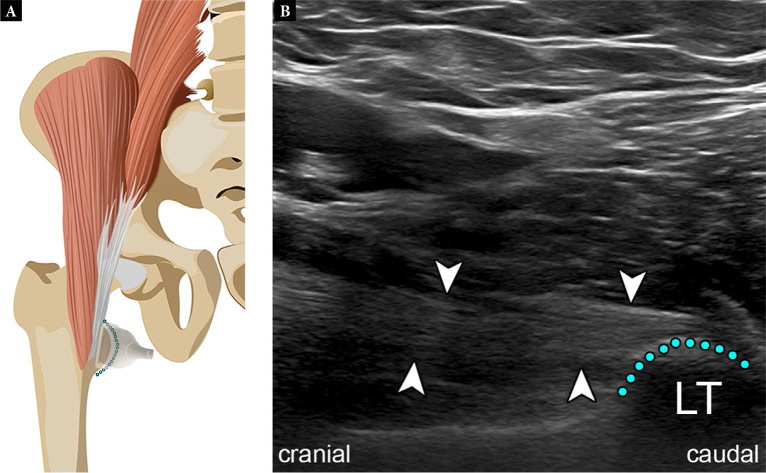
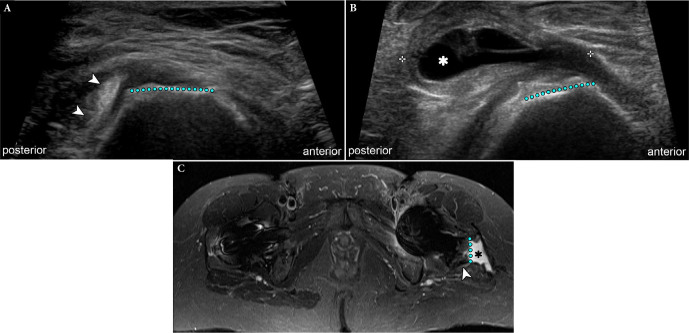
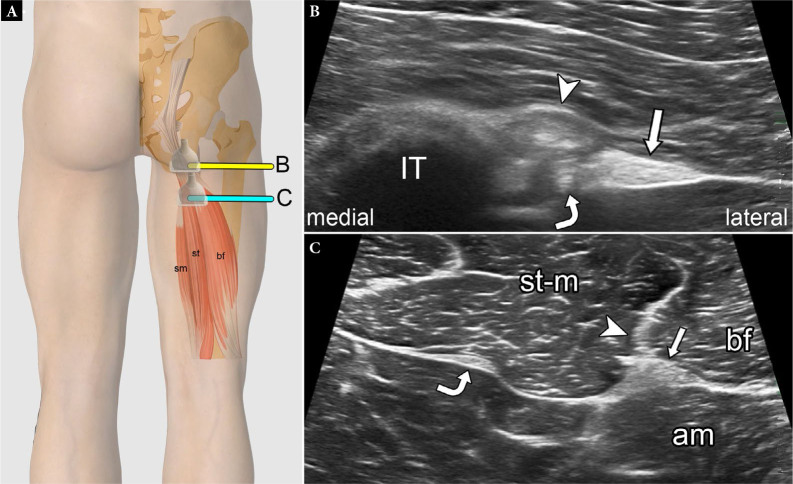
Fig. 20.
Normal proximal hamstring tendons on US. Graphic illustration (A) showing normal transducer positions and equivalent short-axis US images at the level of the ischial tuberosity (IT) (B) and proximal thigh (C) (arrowheads – conjoint tendon; arrows – sciatic nerve; curved arrows – semimembranosus tendon; st-m – semitendinosus muscle; am – adductor magnus muscle; bf – biceps femoris tendon). Fig. 20 A is modified with permission from Flores et al.(3)
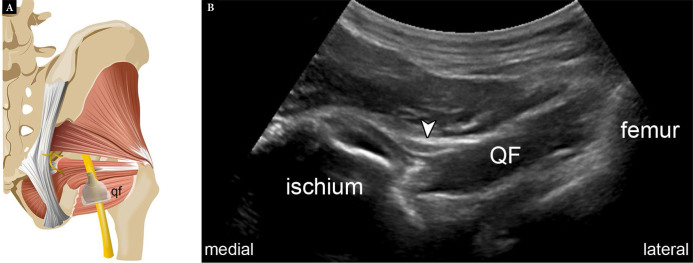
Depending on the patient’s body habitus and depth of the soft tissues, the structures of the posterior hip are visible to various degrees on US. The gluteal crease serves a useful landmark. A transducer with sufficient penetration placed transversely should allow identification of the subcutaneous fat and the gluteus maximus muscle, and deep to this, the ischial tuberosity as a horizontal hyperechoic line. The hamstring tendons are identified in cross-section as ovoid hypoechoic structures superficial to the hyperechoic cortex of ischial tuberosity, and in long axis as a short hyperechoic striated structure merging into the muscle belly. In cross section, the sciatic nerve appears as hyperechoic structure with a honeycomb appearance, lateral to the hamstring tendons. On US, the ischiofemoral space is typically interrogated at the level of the quadratus femoris muscle (Fig. 21). This is performed by moving the transducer slightly cranial and laterally from the ischial tuberosity until the ischiofemoral space with the intervening quadratus femoris muscle and sciatic nerve are visualized.
Fig. 21.
Normal ischiofemoral space. Graphic illustration (A) demonstrates normal transducer position for assessing the ischiofemoral space. Short-axis US image (B) shows the normal sonographic appearance of the space (qf – quadratus femoris; arrowhead – sciatic nerve) Fig. 21 A is modified with permission from Flores et al.(3)
Pathology
Proximal hamstrings pathology
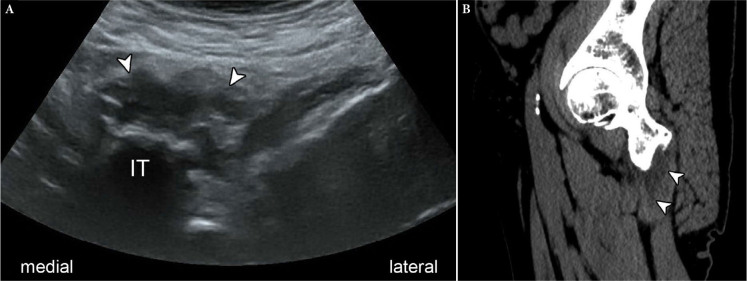
Disorders of the hamstrings at the hip include tendinosis, and partial or complete tears. Tendinosis manifests with decreased echogenicity and thickening of the tendons. Speckled hyperechogenicity in the substance of the tendons can reflect calcific tendinopathy; this may be indistinguishable from enthesopathy when located directly at the ischial tuberosity origin. A partial tear presents with irregularity and partial discontinuity of tendon fibers, with focal or anechoic clefts. A small tear may be difficult to detect in the presence of severe tendinosis. A complete tear presents with a full-thickness cleft and with an intervening hematoma or fluid gap. In contrast to partial tears, it can manifest with frank separation or retraction of torn tendon fibers (Fig. 22). The ischiogluteal bursa lying between the ischial tuberosity and the gluteus maximus muscle may be expanded and inflamed in the setting of hamstring patho logy, and has also been reported following exercise activities or prolonged sitting (Fig. 23).
Fig. 22.
Complete hamstring tendon tear in a 55-year-old soccer player who felt a pop after a kick. Long-axis US image shows a complex tear of the proximal hamstrings with distal retraction of torn tendon fibers to the level of the proximal thigh (arrowheads) IT – ischial tuberosity). Sagittal PD-weighted fat-suppressed MR image confirms the tear (arrowheads)
Fig. 23.
Ischiogluteal bursitis in a 52-year-old female with persistent pain during sitting. Short-axis US image (A) and sagittal CT (B) show a fluid collection (arrowheads) superficial to the ischial tuberosity (IT), consistent with ischiogluteal bursal fluid
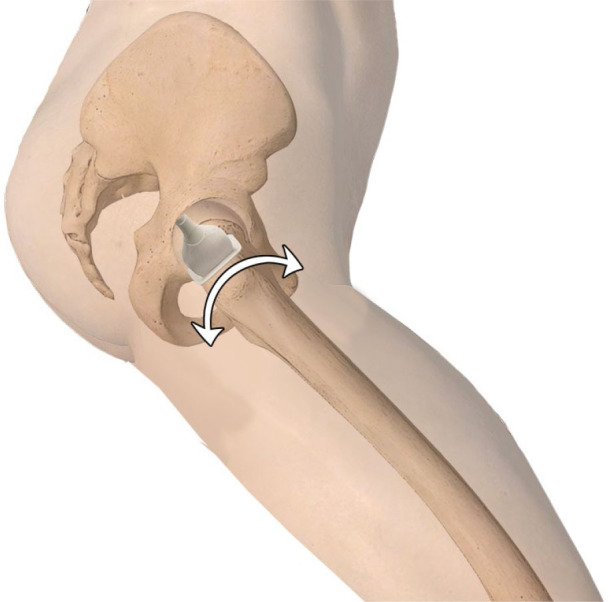
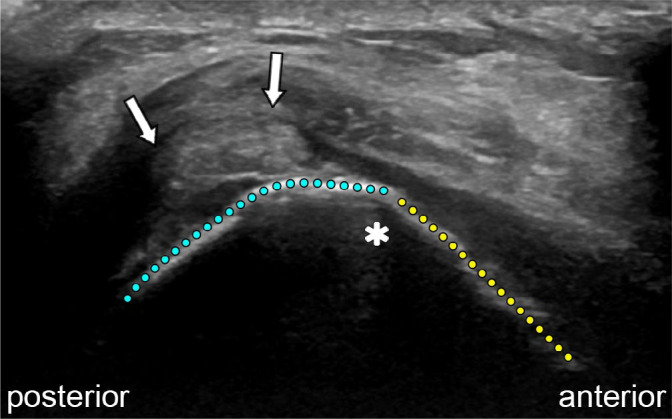
Ischiofemoral impingement
Narrowing of the interval between the ischial tuberosity and lesser trochanter is implicated in the symptoms of ischiofemoral impingement. In the normal setting, with the hip in adduction, external rotation and extension, the interval is approximately 2 cm(52). The space can be assessed dynamically on US by adducting, abducting, and internally and externally rotating the hip while scanning posteriorly. US signs positive for impingement are an “erupted” appearance to the quadratus femoris or reproduction of the patient’s symptoms from internal to external rotation(53) (Video 4). The primary advantage of MRI over US is demonstration of edematous changes within the quadratus femoris muscle.
Interventions about the posterior hip
Hamstring tendinosis
Conservative treatments are generally employed in mild hamstring complex injury or low-grade tendinopathy, however, in up to 20% of patients, symptoms can persist for more than 6 months and become recalcitrant to conservative treatment(54). In these cases, more invasive treatment options may be considered. Injection of the hamstring origin is performed with the patient lying in the prone position. A long 21-gauge needle can be passed down to the level of tendon origin and ischial tuberosity.
There are many treatment options, and at present, only limited evidence is available to support many of these, though it has been demonstrated that percutaneous dry needling is effective in reducing pain in patients with chronic tendinopathy in the proximal hamstring complex, with improved pain scores with dry needling at 1 and 3 months compared with standard conservative management(55). Corticosteroids, plateletrich plasma injections, and prolotherapy may also be considered.
Medial hip
Technique and normal anatomy
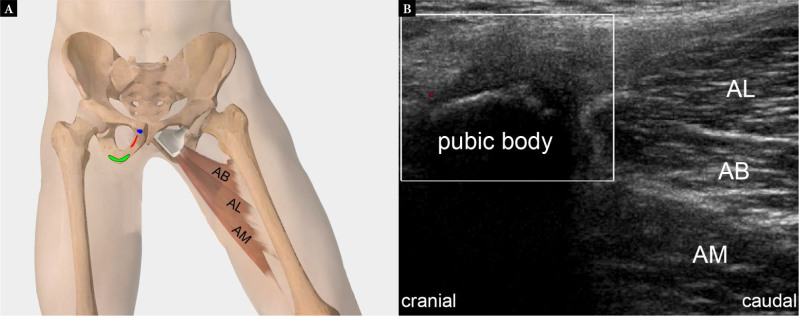
The main muscles at the medial hip include the adductor longus, adductor brevis, and adductor magnus. The adductor longus muscle originates from the body of pubis, inferior to the pubic crest and lateral to the pubic symphysis, being the most superficial. It extends to attach at the adductor canal, inserting into the middle third of the medial lip of the linea aspera. The adductor brevis lies deep to the pectineus and adductor longus, and originates from the outer surface of the body of the pubis and inferior pubic ramus between the gracilis and obturator externus. It inserts into the upper part of the linea aspera lateral to the insertion of the pectineus and proximal to the adductor longus. The adductor magnus is a large muscle arising from the inferior pubic ramus and inserting into the linea aspera medial to the gluteus maximus. It is the deepest of the adductor muscles, with the broadest and most distal attachment. From superficial to deep, the adductor muscles are layered; adductor longus, adductor brevis, and adductor magnus.
The medial hip is examined with the patient lying in the supine position, while the hip is positioned in abduction and external rotation, with the knee flexed(1,2) (Fig. 24). The adductors can be evaluated in the transverse plane, and the three muscle layers can be seen; the superficial layer being the adductor longus muscle (laterally) and gracilis muscle (medially), the middle layer being the adductor brevis muscle, and the deep layer being the adductor magnus muscle(1,2). Neurovascular structures can typically be seen between the different muscle layers.
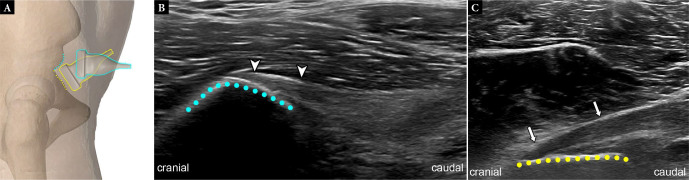
Fig. 24.
Graphic illustration (A) demonstrates the osseous footprints and normal transducer position for assessing the adductor tendons (AB – adductor brevis, footprint highlighted in red; AL – adductor longus, footprint highlighted in blue; AM – adductor magnus, footprint highlighted in green). Long-axis US image (B) shows the normal sonographic appearance of the same muscles
The transducer should be moved proximally to the insertion of the tendons at the pubis. The adductor insertion is examined with the transducer placed longitudinally along the long axis of the tendon insertion(1).
Pathology
Hip adductor injuries usually occur with hip in hyperabduction and abdominal wall hyperextension, occasionally with forced external rotation of the leg(56). The adductor longus and the gracilis muscles are most often affected(57).
Adductor tendinopathy can be seen as hypoechoic thickening of the tendon; however, US has a low sensitivity in low-grade injuries or chronic adductor tendinopathy compared with MRI(56).
In contrast to the other regions of the hip, the medial hip is not optimally depicted on US. In our practice, the primary use of US in the medial hip is for guidance during intervention procedures such as tenotomy or dry needling of the common adductor tendon or intraarticular injection into the symphysis pubis to relieve symptoms of athletic pubalgia or sports hernia.
Conclusions
US of the hip is a very commonly requested examination, particularly for the assessment of the anterior, lateral, and posterior hip. Knowledge of the anatomy is crucial, as is an understanding of the range of pathology in each region. Proper patient positioning and use of correct transducer frequency is extremely important, as this will assist in performing an appropriate diagnostic study. US is useful for dynamic maneuvers and can help to guide interventional procedures.
Footnotes
Conflict of interest
The authors do not report any financial or personal connections with other persons or organizations which might negatively affect the contents of this publication and/or claim authorship rights to this publication.
Author contributions
Writing of manuscript: LP, DF, ER, MC, AA. Final approval of manuscript: LP, DF, ER, MC, AA. Critical review of manuscript: LP, DF, ER, MC, AA.
References
- 1.Lin YT, Wang TG Ultrasonographic examination of the adult hip J Med Ultrasound. 2012;20:201. doi: 10.1016/j.jmu.2012.10.009. : . ; : –. . doi: . [DOI] [Google Scholar]
- 2.Beggs I, Bianchi S, Bueno A, Cohen M, Court-Payen M, Grainger A, et al. Musculoskeletal ultrasound technical guidelines IV. Hip. European Society of Musculo-Skeletal Radiology. : . .
- 3.Flores DV, Umpire DF, Sampaio ML, Cresswell ME, Pathria MN US and MRI of pelvic tendon anatomy and pathologic conditions Radiographics. 2022;42:1433. doi: 10.1148/rg.220055. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 4.Martinoli C, Garello I, Marchetti A, Palmieri F, Altafini L, Valle M, et al. Hip ultrasound Eur J Radiol. 2012;81:3824. doi: 10.1016/j.ejrad.2011.03.102. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 5.Armstrong T, Pass B, O’Connor P The capsular head of the proximal rectus femoris muscle: a review of the imaging anatomy of proximal muscle injury in professional athletes – early experience Br J Radiol. 2022;95:20220278. doi: 10.1259/bjr.20220278. : . ; : . doi: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gyftopoulos S, Rosenberg ZS, Schweitzer ME, Bordalo-Rodrigues M Normal anatomy and strains of the deep musculotendinous junction of the proximal rectus femoris: MRI features AJR Am J Roentgenol. 2008;190:W182. doi: 10.2214/AJR.07.2947. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 7.Becciolini M, Pivec C, Riegler G Ultrasound of the lateral femoral cutaneous nerve: a review of the literature and pictorial essay J Ultrasound Med Off J Am Inst Ultrasound Med. 2022;41:1273. doi: 10.1002/jum.15809. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 8.Rudin D, Manestar M, Ullrich O, Erhardt J, Grob K The anatomical course of the lateral femoral cutaneous nerve with special attention to the anterior approach to the hip joint J Bone Joint Surg Am. 2016;98:561. doi: 10.2106/JBJS.15.01022. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 9.Koski JM, Anttila PJ, Isomäki HA Ultrasonography of the adult hip joint Scand J Rheumatol. 1989;18:113. doi: 10.3109/03009748909099926. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 10.Weybright PN, Jacobson JA, Murry KH, Lin J, Fessell DP, Jamadar DA, et al. Limited effectiveness of sonography in revealing hip joint effusion: preliminary results in 21 adult patients with native and postoperative hips AJR Am J Roentgenol. 2003;181:215. doi: 10.2214/ajr.181.1.1810215. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 11.Jacobson JA, Khoury V, Brandon CJ Ultrasound of the groin: techniques, pathology, and pitfalls AJR Am J Roentgenol. 2015;205:513. doi: 10.2214/AJR.15.14523. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 12.Bierma-Zeinstra SM, Bohnen AM, Verhaar JA, Prins A, Ginai-Karamat AZ, Laméris JS Sonography for hip joint effusion in adults with hip pain Ann Rheum Dis. 2000;59:178. doi: 10.1136/ard.59.3.178. : . ; : –. . doi: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Birn J, Pruente R, Avram R, Eyler W, Mahan M, van Holsbeeck M Sonographic evaluation of hip joint effusion in osteoarthritis with correlation to radiographic findings J Clin Ultrasound. 2014;42:205. doi: 10.1002/jcu.22112. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 14.Wakefield RJ, Balint PV, Szkudlarek M, Filippucci E, Backhaus M, D’Agostino MA, et al. Musculoskeletal ultrasound including definitions for ultrasonographic pathology J Rheumatol. 2005;32:2485. : . ; : –. . [PubMed] [Google Scholar]
- 15.Petersilge CA Chronic adult hip pain: MR arthrography of the hip RadioGraphics. 2000;20:S43. doi: 10.1148/radiographics.20.suppl_1.g00oc12s43. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 16.Palmer W, Bancroft L, Bonar F, Choi JA, Cotten A, Griffith JF, et al. Glossary of terms for musculoskeletal radiology Skeletal Radiol. 2020;49:1. doi: 10.1007/s00256-020-03465-1. : . ; : –. . doi: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Verhaegen JCF, Vandeputte FJ, Van den Broecke R, Roose S, Driesen R, Timmermans A, et al. Risk factors for iliopsoas tendinopathy after anterior approach total hip arthroplasty J Arthroplasty. 2023;38:511. doi: 10.1016/j.arth.2022.10.015. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 18.Rubio M, Rodriguez M, Patnaik S, Wang P Spontaneous iliopsoas tendon tear Geriatr Orthop Surg Rehabil. 2016;7:30. doi: 10.1177/2151458515627309. : . ; : –. . doi: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bui KL, Sundaram M Radiologic case study: iliopsoas tendon rupture Orthopedics. 2008 : . ; 31. [PubMed] [Google Scholar]
- 20.Bianchi S, Martinoli C, Keller A, Bianchi-Zamorani MP Giant iliopsoas bursitis: Sonographic findings with magnetic resonance correlations J Clin Ultrasound. 2002;30:437. doi: 10.1002/jcu.10093. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 21.Lungu E, Michaud J, Bureau NJ US Assessment of sports-related hip injuries Radiogr Rev Publ Radiol Soc N Am Inc. 2018;38(3):867. doi: 10.1148/rg.2018170104. : . ; ( ): –. . doi: . [DOI] [PubMed] [Google Scholar]
- 22.Blankenbaker DG, De Smet AA, Keene JS Sonography of the iliopsoas tendon and injection of the iliopsoas bursa for diagnosis and management of the painful snapping hip Skeletal Radiol. 2006;35:565. doi: 10.1007/s00256-006-0084-6. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 23.Jacobson JA Ultrasound in sports medicine Radiol Clin North Am. 2002;40:363. doi: 10.1016/s0033-8389(02)00005-2. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 24.Pasta G, Nanni G, Molini L, Bianchi S Sonography of the quadriceps muscle: Examination technique, normal anatomy, and traumatic lesions J Ultrasound. 2010;13:76. doi: 10.1016/j.jus.2010.07.004. : . ; : –. . doi: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klauser AS, Abd Ellah MMH, Halpern EJ, Sporer I, Martinoli C, Tagliafico A, et al. Meralgia paraesthetica: Ultrasound-guided injection at multiple levels with 12-month follow-up Eur Radiol. 2016;26:764. doi: 10.1007/s00330-015-3874-1. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 26.Chung CB, Robertson JE, Cho GJ, Vaughan LM, Copp SN, Resnick D Gluteus medius tendon tears and avulsive injuries in elderly women: imaging findings in six patients Am J Roentgenol. 1999;173:351. doi: 10.2214/ajr.173.2.10430134. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 27.Bunker TD, Esler CN, Leach WJ Rotator-cuff tear of the hip J Bone Joint Surg Br. 1997;79:618. doi: 10.1302/0301-620x.79b4.7033. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 28.Jacobson JA . In: Fundamentals of Musculoskeletal Ultrasound. Second. Jacobson JA, editor. Philadelphia: W.B. Saunders; 2013. [2023.06.04]. Hip and Thigh Ultrasound; pp. e4.https://www.sciencedirect.com/science/article/pii/B9781455738182000069 : (ed.): ( Edition) [Internet]. : ; –. . . Available from: [accessed: ]. [Google Scholar]
- 29.Connell DA, Bass C, Sykes CAJ, Young D, Edwards E Sonographic evaluation of gluteus medius and minimus tendinopathy Eur Radiol. 2003;13:1339. doi: 10.1007/s00330-002-1740-4. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 30.Walters J, Solomons M, Davies J Gluteus minimus: observations on its insertion J Anat. 2001;198:239. doi: 10.1046/j.1469-7580.2001.19820239.x. : . ; : –. . doi: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McEvoy JR, Lee KS, Blankenbaker DG, del Rio AM, Keene JS Ultrasound-guided corticosteroid injections for treatment of greater trochanteric pain syndrome: greater trochanter bursa versus subgluteus medius bursa AJR Am J Roentgenol. 2013;201:W313. doi: 10.2214/AJR.12.9443. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 32.Huang BK, Campos JC, Michael Peschka PG, Pretterklieber ML, Skaf AY, Chung CB, et al. Injury of the gluteal aponeurotic fascia and proximal iliotibial band: anatomy, pathologic conditions, and MR imaging Radiogrphics. 2013;33:1437. doi: 10.1148/rg.335125171. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 33.Klontzas ME, Karantanas AH Greater trochanter pain syndrome: a descriptive MR imaging study Eur J Radiol. 2014;83:1850. doi: 10.1016/j.ejrad.2014.06.009. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 34.Long SS, Surrey DE, Nazarian LN Sonography of greater trochanteric pain syndrome and the rarity of primary bursitis AJR Am J Roentgenol. 2013;201:1083. doi: 10.2214/AJR.12.10038. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 35.Kong A, Van der Vliet A, Zadow S MRI and US of gluteal tendinopathy in greater trochanteric pain syndrome Eur Radiol. 2007;17:1772. doi: 10.1007/s00330-006-0485-x. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 36.Docking SI, Cook J, Chen S, Scarvell J, Cormick W, Smith P, et al. Identification and differentiation of gluteus medius tendon pathology using ultrasound and magnetic resonance imaging Musculoskelet Sci Pract. 2019;41:1. doi: 10.1016/j.msksp.2019.01.011. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 37.Cvitanic O, Henzie G, Skezas N, Lyons J, Minter J MRI diagnosis of tears of the hip abductor tendons (gluteus medius and gluteus minimus) Am J Roentgenol. 2004;182:137. doi: 10.2214/ajr.182.1.1820137. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 38.Chi AS, Long SS, Zoga AC, Read PJ, Deely DM, Parker L, et al. Prevalence and pattern of gluteus medius and minimus tendon pathology and muscle atrophy in older individuals using MRI Skeletal Radiol. 2015;44:1727. doi: 10.1007/s00256-015-2220-7. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 39.Kingzett-Taylor A, Tirman PF, Feller J, McGann W, Prieto V, Wischer T, et al. Tendinosis and tears of gluteus medius and minimus muscles as a cause of hip pain: MR imaging findings Am J Roentgenol. 1999;173:1123. doi: 10.2214/ajr.173.4.10511191. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 40.Murray TÉ, Roberts D, Rattan B, Murphy DT, Cresswell M Dynamic ultrasound-guided trochanteric bursal injection Skeletal Radiol. 2020;49:1155. doi: 10.1007/s00256-020-03411-1. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 41.Blankenbaker DG, Ullrick SR, Davis KW, De Smet AA, Haaland B, Fine JP Correlation of MRI findings with clinical findings of trochanteric pain syndrome Skeletal Radiol. 2008;37:903. doi: 10.1007/s00256-008-0514-8. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 42.Chiavaras MM, Jacobson JA Ultrasound-guided tendon fenestration Semin Musculoskelet Radiol. 2013;17:85. doi: 10.1055/s-0033-1333942. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 43.Bureau NJ Sonographic evaluation of snapping hip syndrome J Ultrasound Med. 2013;32:895. doi: 10.7863/ultra.32.6.895. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 44.Chun YS, Rhyu KH, Cho KY, Cho YJ, Lee CS, Han CS Osteochondroma arising from anterior inferior iliac spine as a cause of snapping hip Clin Orthop Surg. 2016;8:123. doi: 10.4055/cios.2016.8.1.123. : . ; : –. . doi: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Inoue S, Noguchi Y, Mae T, Rikimaru S, Hotokezaka S An external snapping hip caused by osteochondroma of the proximal femur Mod Rheumatol. 2005;15:432. doi: 10.1007/s10165-005-0433-7. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 46.Bonilla-Yoon I, Masih S, Patel DB, White EA, Levine BD, Chow K, et al. The Morel-Lavallée lesion: pathophysiology, clinical presentation, imaging features, and treatment options Emerg Radiol. 2014;21:35. doi: 10.1007/s10140-013-1151-7. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 47.Park JW, Lee YK, Lee YJ, Shin S, Kang Y, Koo KH Deep gluteal syndrome as a cause of posterior hip pain and sciatica-like pain Bone Jt J. 2020:556. doi: 10.1302/0301-620X.102B5.BJJ-2019-1212.R1. : . ; 102-B: –. . doi: . [DOI] [PubMed] [Google Scholar]
- 48.Koulouris G, Connell D Hamstring muscle complex: an imaging review Radiographics. 2005;25:571. doi: 10.1148/rg.253045711. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 49.Bianchi S, Martinoli C . In: Ultrasound of the Musculoskeletal System. Bianchi S, Martinoli C, editors. Springer; Berlin, Heidelberg: 2007. Thigh; pp. 611–636. : (eds.): [Internet]. , : –. . doi: . [DOI] [Google Scholar]
- 50.Balius R, Pedret C, Iriarte I, Sáiz R, Cerezal L Sonographic landmarks in hamstring muscles Skeletal Radiol. 2019;48:1675. doi: 10.1007/s00256-019-03208-x. : . ; : –. . doi: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Broski SM, Murthy NS, Krych AJ, Obey MR, Collins MS The adductor magnus “mini-hamstring”: MRI appearance and potential pitfalls Skeletal Radiol. 2016;45:213. doi: 10.1007/s00256-015-2291-5. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 52.Torriani M, Souto SCL, Thomas BJ, Ouellette H, Bredella MA Ischiofemoral impingement syndrome: an entity with hip pain and abnormalities of the quadratus femoris muscle Am J Roentgenol. 2009;193:186. doi: 10.2214/AJR.08.2090. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 53.Chen YT, Jenkins KM Ultrasound finding of ischiofemoral impingement syndrome and novel treatment with botulinum toxin chemodenervation: A Case Report PM R. 2018;10:665. doi: 10.1016/j.pmrj.2017.11.010. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 54.Wilson JJ, Best TM Common overuse tendon problems: a review and recommendations for treatment Am Fam Physician. 2005;72:811. : . ; : –. . [PubMed] [Google Scholar]
- 55.Housner JA, Jacobson JA, Misko R Sonographically guided percutaneous needle tenotomy for the treatment of chronic tendinosis J Ultrasound Med. 2009;28:1187. doi: 10.7863/jum.2009.28.9.1187. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 56.Rizio L, Salvo JP, Schürhoff MR, Uribe JW Adductor longus rupture in professional football players: acute repair with suture anchors: a report of two cases Am J Sports Med. 2004;32:243. doi: 10.1177/0363546503258836. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 57.Robinson P, Barron DA, Parsons W, Grainger AJ, Schilders EMG, O’Connor PJ Adductor-related groin pain in athletes: correlation of MR imaging with clinical findings Skeletal Radiol. 2004;33:451. doi: 10.1007/s00256-004-0753-2. : . ; : –. . doi: . [DOI] [PubMed] [Google Scholar]
- 58.Flores DV, Bohyn C, Murray TÉ, Murphy DT, Cresswell M Dynamic US of Mus culoskeletal Disorders: A Pictorial Review with Emphasis on Techniques Radiographics. 2023;43:e220130. doi: 10.1148/rg.220130.PMID:37471248. : . ; : . doi: . [DOI] [PubMed] [Google Scholar]