Abstract
This study investigated how the Coronavirus Disease 2019 (COVID-19) pandemic has affected the rate of healthcare-associated infections (HAIs). PubMed, Scopus and Google Scholar were searched to identify potentially eligible studies published from December 2019 to September 2022. A random effect model was used to determine the changes in the rate of HAIs during the pandemic. Thirty-seven studies, mostly from the United States (n = 13), were included. Fifteen studies described how the pandemic affected the rate of CLABSIs and CAUTIs, and eight of them showed a significant increase in CLABSIs. The risk of CLABSIs and CDIs was 27% (pooled odds ratio [OR]: 0.73; confidence interval [CI]: 0.61–0.89; p < 0.001) and 20% (pooled OR: 1.20; CI: 1.10–1.31; p < 0.001) higher during the pandemic compared to before the COVID-19 pandemic period, respectively. However, the overall risk of HAIs was unaffected by the pandemic (pooled OR: 1.00; 95 CI: 0.80–1.24; p = 0.990). Furthermore, there were no significant changes in the risk of CAUTIs (pooled OR: 1.01; 95 CI: 0.88–1.16; p = 0.890), and SSIs (pooled OR: 1.27; CI: 0.91–1.76; p = 0.16) between the two periods. The COVID-19 pandemic had no effect on the overall risk of HAIs among hospitalized patients, but an increased risk of CLABSIs and CDI were observed during the pandemic. Therefore, more stringent infection control and prevention measures and prudent interventions to promote the rational use of antibiotics are warranted across all healthcare facilities to reduce the burden of HAIs.
Keywords: healthcare-associated infections, COVID-19 pandemic, central line-associated bloodstream infections, catheter-associated urinary tract infection, surgical site infection, Clostridium difficile infection, hospital-acquired pneumonia, ventilator-associated pneumonia
1. Introduction
One of the major patient safety concerns during hospitalization is the occurrence of healthcare-associated infections (HAIs). This is because HAIs cause an increase in morbidity, mortality, and healthcare-associated cost [1]. There are variations in the rate of HAIs between countries, with 4% in the United States (US) [2], 6.5% in Europe [3], 9.0% in Asia [4], and approximately 16% in developing countries [5]. Africa has a two-fold higher rate of HAIs as compared to the developed countries [6,7]. HAIs are potentially preventable through compliance with infection control and prevention recommendations [1]. Hand hygiene is the mainstay for the prevention of HAIs and this is beneficial in reducing the transmission of multidrug-resistant organisms [8]. Infection control and prevention programs were disrupted during the COVID-19 pandemic, and this has a potential impact on the incidence of HAIs and transmission of multidrug-resistant organisms. The rate of multidrug-resistant Gram-negative and Gram-positive pathogens has increased during the COVID-19 pandemic [9]. Prior to the COVID-19 pandemic, compliance with recommendations from guidelines on hand hygiene was poor among healthcare workers [10]. However, improved hand hygiene and environmental hygiene was reported during the COVID-19 pandemic [11], and this could potentially reduce the rate of HAIs and transmission of multidrug-resistant organisms.
Conversely, hospital resources, including infection prevention and control resources, were diverted to the management of the COVID-19 pandemic, and this could potentially affect the compliance with infection control and prevention recommendations leading to an increase in the rate of HAIs [12]. The diversion of hospital resources may potentially nullify the benefits of improved hand hygiene on the rate of HAIs during the COVID-19 pandemic [13]. In addition, there was a decline in hospital visits and overcrowding due to the enforcement of movement restrictions during the pandemic, and this could potentially benefit infection prevention and control programs [14,15]. Furthermore, the transmission of hospital-acquired respiratory pathogens was reduced due to the increase in the use of face masks by healthcare workers and patients [15]. Currently, the effect of the COVID-19 pandemic on the rate of HAIs is a subject of debate. While some believe that COVID-19 mitigation strategies could potentially reduce the rate of HAIs [13,16], others have argued that the diversion of hospital resources during the pandemic could potentially increase the rate of HAIs [13]. This study aimed to synthesize the effect of the COVID-19 pandemic on the overall risk of HAIs, and determine the effect of the pandemic on the risk of individual types of HAIs, including central line-associated bloodstream infections (CLABSI), catheter-associated urinary tract infections (CAUTI), Clostridium difficile infection (CDI), surgical site infections (SSI), and ventilator-associated pneumonia/hospital-acquired pneumonia (VAP/HAP).
2. Materials and Methods
2.1. Study Design
The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statements 2020 was used to conduct and report this systematic review [17]. The study protocol was registered with PROPSPERO (reference ID: CRD42023463262).
2.2. Eligibility Criteria
2.2.1. Inclusion Criteria
A study was included if it fulfilled the following predefined criteria:
Compared the rate of HAIs between the periods before the pandemic and during the pandemic using interrupted time series or before and after study design;
Published between December 2019 and September 2022;
Published in English language;
Available as free full-text article.
2.2.2. Exclusion Criteria
A study was excluded if it fulfilled any of the following criteria:
Described nosocomial transmission of COVID-19 infections;
Preprints, correspondence, commentary, and letters to the editor;
Qualitative studies.
2.3. Information Sources
PubMed and Scopus databases were searched by two reviewers to find potentially eligible studies. Supplementary search of Google Scholar was conducted to identify eligible studies. The reference list of the selected studies was manually examined to find additional studies.
2.4. Search Strategy
The relevant keywords for HAIs and the COVID-19 pandemic were combined using Boolean indicators (AND/OR). The following keywords were used for the search: impact OR effect OR change AND “hospital-acquired infection*” OR “healthcare-associated infection*” OR “nosocomial infection*” AND “SARS-CoV-2” OR “COVID-19” OR “coronavirus disease 2019” OR “severe acute respiratory syndrome coronavirus 2” OR “coronavirus infection” OR “coronavirus pandemic” OR “COVID-19 pandemic”.
2.5. Selection Process
The results of the searches from all the databases were combined in one folder and duplicate studies were removed. The titles and abstracts of the studies were initially assessed and irrelevant studies were excluded. The full-text articles of the remaining studies were assessed based on the inclusion and exclusion criteria for selection and data extraction.
2.6. Data Extraction Process
The included studies were reviewed for data extraction using a predefined data collection form. Data extraction was performed by an independent reviewer (UA) and the extracted data were checked by a second reviewer for accuracy. All disagreements were resolved by the reviewers through dialogue.
2.7. Data Items
Data items extracted from the included studies include: name of author and year of publication, study location, study setting, the study design, study period, sample size, hospital units involved, rate of HAIs before and during the COVID-19 pandemic, type of HAIs, and the p-value. In addition, the frequency of HAI, the number of patients, the total patient days and total device days (for urinary catheter and central catheter) for both periods were extracted.
2.8. Study Risk of Bias Assessment
Methodological quality of the included studies was assessed by two independent reviewers (AHY and KA) using the Newcastle–Ottawa scale (NOS) [18]. NOS consists of three sections including: selection, comparability, and outcomes. The reviewers resolved any discrepancies through dialogue.
2.9. Outcome Assessment and Effect Measures
The primary outcome was the effect of the COVID-19 pandemic on the overall risk of HAIs, and this was determined by comparing the overall rate of HAIs before versus during the COVID-19 pandemic. The Centers for Disease Control and Prevention (CDC) [19] and the European Centres for Disease Prevention and Control (ECDC) guidelines were used to define HAIs [20]. The secondary outcomes assessed include the risk of CLABSI, CAUTI, CDI, SSI, and VAP/HAP presented as odds ratio with 95% confidence interval. These infections are referred by CDC as types of HAIs.
2.10. Data Synthesis
Both qualitative and quantitative synthesis was used. Review Manager (RevMan) [Computer program], version 5.4. The Cochrane Collaboration, 2020 was used for the quantitative synthesis. The pooled estimate was determined using random-effects meta-analysis, and the findings were presented using forest plots. Higgins I2 statistic was employed to assess the level of heterogeneity using the following criteria; <40% = low heterogeneity, 30–60% = moderate heterogeneity, 50–90% = substantial heterogeneity, and 75–100% considerable heterogeneity [21]. The overall rate of HAIs was evaluated as the number of patients with HAI as a proportion of all hospitalized patients. The overall risk of HAIs was estimated by comparing the overall rate of HAIs before versus the rate during the COVID-19 pandemic. Furthermore, the risk for the different types of HAIs (CLABSI, CAUTI, SSI, CDI, and HAP/VAP) was estimated by comparing the rate of HAIs (number of events divided by the total patient days or total-device days) between the period before and the period during the COVID-19 pandemic. For each type of HAI, data were meta-analyzed when at least two studies reported that particular HAI.
3. Results
3.1. Study Selection
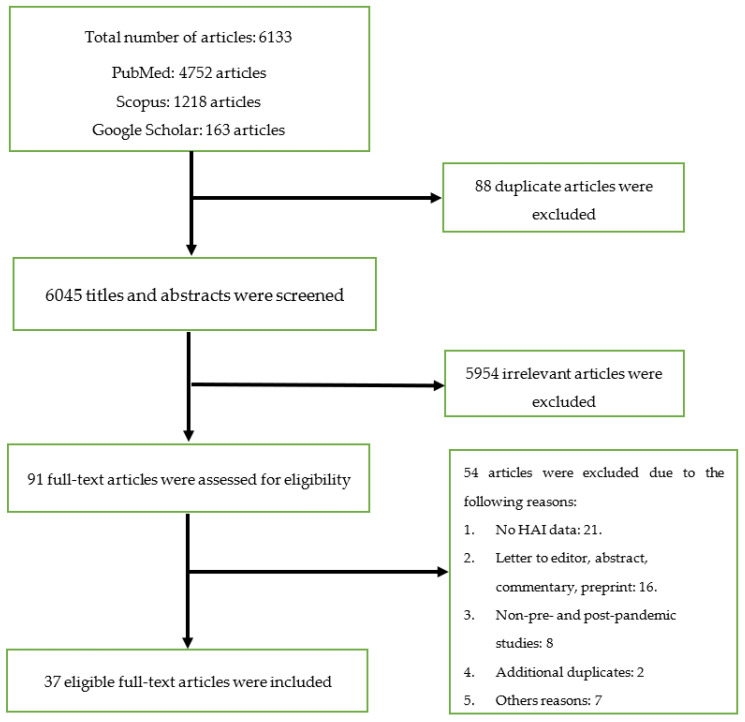
The database searches produced 6133 articles, out of which 88 duplicates were removed. The title and abstract of the de-duplicated articles was screened and 5954 irrelevant articles were excluded. The remaining 91 full-text articles were evaluated for inclusion, and 37 articles that fulfilled the criteria were eventually selected. Figure 1 illustrates the PRISMA flow diagram for the screening and selection process.
Figure 1.
Flow chart for the screening and selection processes.
3.2. Study Characteristics
North America (n = 14; 37.8%), Europe (n = 11; 29.7%), and Asia (n = 5; 13.5%) had the highest number of studies. The US had the highest number of studies (n = 13; 35.1%) followed by Italy (n = 4; 10.8%), and Spain (n = 3; 8.1%). Most of the studies (n = 27; 72.9%) included hospital-wide data, while four studies (10.8%) involved data from intensive care units (ICUs) only. Furthermore, the majority of the studies (n = 26; 70.3%) included multiple study centers. Six studies compared the overall prevalence of HAIs between the period before the COVID-19 pandemic and during the pandemic [22,23,24,25,26,27]. CLABSIs (n = 15; 40.5%) [28,29,30,31,32,33,34,35,36,37,38,39,40,41,42], CAUTIs (n = 15; 40.5%) [22,28,30,31,32,33,34,35,36,39,40,41,42,43,44], and CDI (n = 14; 37.8%) [28,30,31,32,34,36,40,43,45,46,47,48,49,50] were the most reported HAIs in the selected studies. Table 1 presents the characteristics of the studies included in this review.
Table 1.
Characteristics of the studies included in the review.
| S/No. | Author and Year | Country and Continent | Study Setting/No of Centers | Study Design | Period of the Study | Number of Participants | Types of HAIs Included | Prevalence/Incidence of HAIs before Pandemic | Prevalence/Incidence of HAIs during Pandemic | p Value |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Irelli et al., 2020 [26] | Italy/Europe | Neurology and stroke unit/single center | Retrospective case–control study | 8 March 2020 to 31 May 2020 versus same period in 2019 | 216 (2019) 103 (2020) |
Overall HAI | 31.5% | 23.3% | 0.120 |
| 2 | Alsuhaibani et al., 2022 [28] | USA/North America | Hospital-wide/single center | NA | 2018–2019 versus January–December 2020 | NA | CLABSI | 0.7–1.4 per 1000 central line days | 1.8 per 1000 central line days | 0.04 |
| CAUTI | 0.8–1.7 per 1000 catheter days | 0.6–1.6 per 1000 catheter days | 0.54 | |||||||
| CDI | 0.6–1.0 per 10,000 patient days | 0.4–0.6 per 10,000 patient days | 0.11 | |||||||
| 3 | Sturm et al., 2022 [51] | USA/North America | Hospital-wide/multicenter (69 hospitals) | Before and after | Pre-COVID-19 (1 January 2019 to 28 February 2020), and COVID-19 pandemic period (1 March 2020 to 30 April 2021). |
NA | Bloodstream infection | 2.78 per 10,000 patient days | 3.56 per 10,000 patient days | <0.001 |
| 4 | Perez-Granda et al., 2022 [29] | Spain/Europe | Hospital-wide/single center | Retrospective before and during the COVID-19 pandemic | March to May 2019 March to May 2020 |
12,111 versus 10,479 patients. | Catheter-related BSI | 1.89 per 1000 admission | 5.53 per 1000 admission | <0.001 |
| 5 | Wee et al., 2021 [30] | Singapore/Asia | Hospital-wide/multicenter | Retrospective before and after | January 2018–January 2020 versus February–August 2020 | NA | RVI | 9.69 per 10,000 patient days | 0.83 per 10,000 patient days | <0.05 |
| CLABSI | 0.83 per 1000 device days | 0.20 per 1000 device days | <0.05 | |||||||
| CAUTI | 1.8 per 1000 device days | 1.8 per 1000 device days | NA | |||||||
| CDI | 3.65 per 10,000 patient days | 3.47 per 10,000 patient days | 0.66 | |||||||
| 6 | Ochoa-Hein et al., 2021 [47] | Mexico/South America | Hospital-wide/single center | Before–after observational study | January 2019–February 2020 versus April–July 2020 | NA | CDI | 9.3 per 10,000 patient days | 1.4 per 10,000 patient days | NA |
| 7 | Polly et al., 2022 [52] | Brazil/South America | Hospital-wide/single center | Retrospective before–after observational study | 2017–2019 versus 2020 | NA | HCAIs due to MDR bacteria | 3.14 per 1000 patient days | 3.89 per 1000 patient days | <0.005 |
| 8 | Halverson et al., 2022 [31] | USA/North America | Hospital-wide/multicenter | Retrospective cohort study | September 2017 to December 2020 | NA | CLABSI | 0.13 per 1000 patient days | 0.24 | 0.0082 |
| CAUTI | 0.13 per 1000 patient days | 0.17 | 0.052 | |||||||
| CDI | 0.52 per 1000 patient days | 0.55 | 0.670 | |||||||
| Overall HAIs | 0.80 per 1000 patient days | 1.06 | 0.017 | |||||||
| 9 | Kitt et al., 2022 [53] | USA/North America | Hospital-wide/single center | Retrospective cohort study | July 2017–June 2021 | NA | HAVI | 0.19 per 1000 patient days | 0.06 per 1000 patient days | <0.01 |
| 10 | Advan et al., 2022 [32] | USA/North America | Hospital-wide/multicenter | Retrospective longitudinal | January 2018–February 2020 versus March 2020–March 2021 | NA | CLABSI | 0.6 per 1000 catheter days | 0.9 | 0.0023 |
| CAUTI | 0.7 per 1000 catheter days | 0.7 | 0.810 | |||||||
| CDI | 3.6 per 10,000 patient days | 2.6 | <0.001 | |||||||
| 11 | Fakih et al., 2022 [33] | USA/North America | Hospital-wide/multicenter | Retrospective | March 2019–February 2020 versus March–August 2020 | NA | CLABSI | 0.56 per 1000 line days | 0.85 | <0.001 |
| CAUTI | 0.86 per 1000 catheter days | 0.77 | 0.190 | |||||||
| 12 | Teixeira et al., 2022 [54] | Portugal/Europe | Urology ward/multicenter | Retrospective observational | April–June 2018 versus April–June 2020 | 425 patients versus 273 patients | SSI | 14.1% | 12.1% | 0.494 |
| 13 | Ponce-Alonso et al., 2021 [49] | Spain/Europe | Hospital-wide/single center | Retrospective | Mar–May 2019 versus March–May 2020 | 39,795 hospital stay (pre) versus 44,831 (pandemic era) hospital stays | CDI | 8.54 per 10,000 patient days | 2.68 per 10,000 patient days | 0.0002 |
| 14 | Bobbitt et al., 2022 [34] | USA/North America | Hematology and stem cell transplant patients/single center | Retrospective observational | March–July 2019 versus March–July 2020 | 295 patients versus 259 patients | CDI | 2.61 per 1000 patient days | 1.58 | 0.512 |
| CLABSI | 0.44 per 1000 patient days | 1.064 | 0.516 | |||||||
| CAUTI | 0.44 per 1000 patient days | 0.53 | 0.899 | |||||||
| 15 | Kong et al., 2021 [36] | USA/North America | Hospital-wide/single center | Retrospective observational | January 2019–February 2020 versus March 2020–June 2020 | NA | CDI | 0.48 ± 0.12 | 0.26 ± 0.25 | 0.200 |
| CLABSI | 1.47 ± 1.63 | 0.37 ± 0.73 | 0.210 | |||||||
| CAUTI | 1.10 ± 1.18 | 0.87 ± 0.58 | 0.720 | |||||||
| 16 | Tham et al., 2022 [27] | Australia | Hospital-wide/single center | Retrospective cohort study | April–June 2019 versus April–June 2020 | 3415 admission (pre-COVID-19) versus 2530 (COVID-19 era) | Overall HAIs | 6.6% | 7.1% | NA |
| UTI | 1.3% | 1.6% | NA | |||||||
| SSI | 1.5% | 1.7% | NA | |||||||
| HAP | 2.5% | 2.3% | NA | |||||||
| BSI | 0.4% | 0.4% | NA | |||||||
| GI | 0.4% | 0.2% | NA | |||||||
| 17 | Mohammadi et al., 2022 [55] | Iran/Asia | Hospital-wide/single center | Retrospective study | April–November 2019 versus April–December 2020 | 16,687 admission (pre pandemic) versus 10,553 admission (pandemic era) | Overall HAIs | 4.73% | 4.78% | NA |
| 18 | Chen et al., 2021 [25] | China/Asia | Hospital-wide/single center | Retrospective before and after | 2018–2019 versus 2020 | 62,625 patients (2018) 70,091 (2019) 59,167 (2020) |
Overall HAIs | 1.64% (2018) 1.56% (2019) |
1.82% | 0.001 |
| LRI | 39.5% | 39.7% | 0.971 | |||||||
| UTI | 14.8% | 10.5% | 0.002 | |||||||
| BSI | 11.28% | 12.91% | 0.079 | |||||||
| SSI | 11.83% | 14.84% | 0.084 | |||||||
| GTI | 7.49% | 9.62% | 0.068 | |||||||
| 19 | Losurdo et al., 2020 [56] | Italy/Europe | Surgery department/single center | Retrospective | 2018–2019 versus 2020 | 418 patients (pre-COVID era) versus 123 (COVID-19 era) | SSI | 8.4% | 3.3% | 0.035 |
| Superficial SSI | 5.3% | 0.8% | 0.018 | |||||||
| Deep SSI | 3.4% | 0.0% | 0.025 | |||||||
| Organ-space SSI | 3.6% | 1.6% | 0.209 | |||||||
| 20 | Geffer et al., 2022 [35] | Germany/Europe | ICU/multicenter | NA | 2019 versus 2020 | 863,999 patients (2019) and 696,085 patients (2020) | CLABSI | 0.7 per 1000 central line days | 0.64 | 0.263 |
| VALRTI | 2.95 per ventilator days | 2.02 | <0.001 | |||||||
| CAUTI | 0.61 per 1000 catheter days | 0.49 | 0.008 | |||||||
| 21 | Porto et al., 2022 [37] | Brazil /South America | ICU/multicenter | NA | April–June 2019 versus April–June 2020 | 531 (2019) versus 357 (2020) | CLABSI | 1.60 per 1000 central line days | 2.81 | 0.002 |
| VAP | 2.99 per 1000 ventilator days | 3.65 | 0.167 | |||||||
| 22 | Samaroo-Campbell et al., 2022 [41] | USA/North America | Hospital-wide/multicenter | Retrospective | 15 months before and 15 months after the onset of the pandemic | NA | CLABSI | 1.09 ± 0.43 per 1000 catheter days | 1.76 | NA |
| CAUTI | 1.03 ± 0.18 per 1000-catheter days | 1.80 ± 0.21 | 0.0003 | |||||||
| 23 | Ochoa-Hein et al., 2021 [43] | Mexico/South America | Hospital-wide/single center | Before–after observational study | January 2019–February 2020 versus Apr–Jul 2020 | NA | Overall HAIs | 6.2 per 1000 patient days | 11.8 | 0.023 |
| VAP | 10% | 54.7% | <0.001 | |||||||
| HAP | 26.9% | 18.2% | 0.025 | |||||||
| BSI | 1.3% | 20.6% | <0.001 | |||||||
| CAUTI | 8.3% | 3.5% | 0.039 | |||||||
| SSI | 25.2% | 0.0% | NA | |||||||
| CDI | 15.2% | 1.8% | <0.001 | |||||||
| Candidemia | 0.0% | 8.2% | <0.001 | |||||||
| 24 | Ghali et al., 2021 [24] | Tunisia/Africa | Hospital-wide/single center | Repeated point-prevalence | 2019 versus 2020 | 306 patients versus 296 patients | Overall HAIs | 9.5% | 15.5% | 0.01 |
| 25 | AlAhdal et al., 2022 [42] | Saudi Arabia/Asia | Hospital-wide/single center | Retrospective observational | January–December 2019 versus January–December 2020 | NA | CLABSI | 1.2 per 1000 device days | 0.5 | NA |
| CAUTI | 0.94 per 1000 device days | 0.5 | NA | |||||||
| VAP | 1.3 per 1000 device days | 0.9 | NA | |||||||
| 26 | Ereth et al., 2021 [57] | USA/North America | Hospital-wide/single center | NA | March–December 2019 versus March–December 2020 | NA | NA | 6.71 per 1000 patient days | 1.03 per 1000 patient days | NA |
| 27 | Bentivegna et al., 2021 [45] | Italy/Europe | Medical ward/single center | Retrospective study | 2017–2019 versus March–June 2020 | NA | CDI | 0.066 | 0.037 | NA |
| 28 | Choi et al., 2022 [46] | Canada/North America | Hospital-wide/multicenter | Interrupted time series analysis | January 2015–Febr 2020 versus March 2020–June 2021 | 8,475,872 patient days versus 8,694,620 patient days | CDI | 3.4 | 3.5 | 0.0896 |
| 29 | Rosenthal et al., 2022 [39] | Multinational study/Asia and Europe | ICU/multicenter | Pre and post | January–December 2019 versus January–May 2020 | 7775 patients (pre) versus 1778 patients (pandemic) | CLABSI | 2.54 per 1000 line days | 4.73 per 1000 line days | 0.0006 |
| CAUTI | 1.64 per 1000 catheter days | 1.43 per 1000 catheter days | 0.690 | |||||||
| 30 | Manea et al., 2021 [48] | Romania/Europe | Hospital-wide/single center | Retrospective cohort | March 2017–February 2018 versus 2020–2021 | NA | CDI | 6.1 per 1000 adult discharge | 5.6 per 1000 discharge | 0.600 |
| 31 | Jabarpour et al., 2021 [23] | Iran/Asia | Hospital-wide/single center | Cross-sectional design | March–July 2019 versus March–July 2020 | 7454 patients (pre) versus 6135 patients (pandemic era) | Overall HAIs | 4.6% | 3.7% | 0.020 |
| UTI | 0.8% | 0.5% | 0.040 | |||||||
| BSI | 0.8% | 0.9% | 0.460 | |||||||
| SSI | 1.4% | 0.9% | 0.020 | |||||||
| 32 | Baccolini et al., 2021 [22] | Italy/Europe | ICU/single center | NA | March–April 2019 versus March–April 2020 | 42 patients (pre) and 62 patients (pandemic era) | Overall HAIs | 26.2% | 43.6% | NA |
| 33 | Whitaker et al., 2022 [44] | USA/North America | Hospital-wide/single center | NA | 2019 versus 2020 | NA | CAUTI | 0.37 per 1000 catheter days | 0.23 | NA |
| 34 | Ramos-Matinez et al., 2020 [58] | Spain/Europe | Hospital-wide/single center | NA | 2015–2019 versus March–April 2020 | NA | HAI endocarditis | 0.119 per 1000 days | 0.0194 per 1000 days | <0.001 |
| 35 | Sipos et al., 2021 [50] | Romania/Europe | Hospital-wide/single center | Retrospective | March–November 2018 & 2019 versus March–November 2020 | 43,126 patients (pre) versus 25,124 (pandemic era) | CDI | 151/43126 (0.36%) | 65/25124 (0.26%) | 0.0484 |
| 80.8 per 100,000 bed days | 70.5 per 100,000 bed days | |||||||||
| 36 | Lastinger et al., 2022 [40] | USA/North America | Hospital-wide/single center | NA | First, second and third quarters 2019 versus 1st–3rd quarter 2021 | 1st quarter | CLABSI | 0.687 | 0.998 | <0.05 |
| CAUTI | 0.748 | 0.834 | <0.05 | |||||||
| VAE | 0.948 | 1.431 | <0.05 | |||||||
| SSI colon surgery | 0.866 | 0.820 | >0.05 | |||||||
| SSI abdominal hysterectomy | 0.926 | 0.976 | >0.05 | |||||||
| Lab ID CDI | 0.628 | 0.530 | <0.05 | |||||||
| 2nd quarter | CLABSI | 0.697 | 0.778 | <0.05 | ||||||
| CAUTI | 0.709 | 0.706 | >0.05 | |||||||
| VAE | 0.957 | 1.209 | <0.05 | |||||||
| SSI colon surgery | 0.870 | 0.848 | >0.05 | |||||||
| SSI abdominal hysterectomy | 0.980 | 0.988 | >0.05 | |||||||
| Lab ID CDI | 0.582 | 0.500 | <0.05 | |||||||
| 3rd quarter | CLABSI | 0.699 | 1.037 | <0.05 | ||||||
| CAUTI | 0.705 | 0.801 | <0.05 | |||||||
| VAE | 0.999 | 1.600 | <0.05 | |||||||
| SSI colon surgery | 0.877 | 0.796 | <0.05 | |||||||
| SSI abdominal hysterectomy | 1.087 | 1.042 | >0.05 | |||||||
| Lab ID CDI | 0.564 | 0.482 | <0.05 | |||||||
| 37 | Patel et al., 2022 [38] | USA/North America | Hospital-wide/single center | NA | 2nd quarter 2019 versus 2nd quarter 2020 | NA | CLABSI | 0.68 | 0.87 | <0.05 |
ICU: intensive care unit; CLABSI: central line-associated bloodstream infections; CAUTI: catheter-associated urinary tract infections; CDI: Clostridium difficile infection; SSI: surgical site infections; RVI: respiratory viral infections; HAVI: hospital-acquired viral infections; MDR: multidrug-resistant; HAP: hospital-acquired pneumonia; VAP: ventilator-associated pneumonia; BSI: bloodstream infection; VALRTI: ventilator-associated lower respiratory tract infection; NA: Not available.
3.3. Quality Assessment of the Studies
Most of the included studies had a truly or somewhat representative target population. In addition, the sample size for most of the studies was satisfactory and justified. The quality score for the included studies ranged from 6 to 7, with 33 studies (89.2%) scoring 7 points. Overall, the methodological quality was good in the majority of the studies (89.2%), although, four studies were found to have a fair methodological quality. Table 2 illustrates the quality assessment results of the included studies.
Table 2.
Methodological quality assessment of the studies included in the review.
| S/No | Author Name and Year | Selection | Comparability | Outcomes | Quality Score |
Quality Scale | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Representatives of Sample |
Sample Size |
Non-Respondents | Ascertainment of Exposure |
Based on Design and Analysis |
Assessment of Outcomes |
Statistical Test |
||||
| 1. | Irelli et al., 2020 [26] | * | * | NA | * | * | ** | * | 7 | Good |
| 2. | Alsuhaibani et al., 2022 [28] | * | * | NA | * | * | ** | * | 7 | Good |
| 3. | Sturm et al., 2022 [51] | * | * | NA | * | * | ** | * | 7 | Good |
| 4. | Perez-Granda et al., 2022 [29] | * | * | NA | * | * | ** | * | 7 | Good |
| 5. | Wee et al., 2021 [30] | * | * | NA | * | * | ** | * | 7 | Good |
| 6. | Ochoa-Hein et al., 2021 [47] | * | * | NA | * | * | * | * | 6 | Fair |
| 7. | Polly et al., 2022 [52] | * | * | NA | * | * | ** | * | 7 | Good |
| 8. | Halverson et al., 2022 [31] | * | * | NA | * | * | ** | * | 7 | Good |
| 9. | Kitt et al., 2022 [53] | * | * | NA | * | * | ** | * | 7 | Good |
| 10. | Advani et al., 2022 [32] | * | * | NA | * | * | ** | * | 7 | Good |
| 11. | Fakih et al., 2022 [33] | * | * | NA | * | * | ** | * | 7 | Good |
| 12. | Teixeira et al., 2022 [54] | * | * | NA | * | * | ** | * | 7 | Good |
| 13. | Ponce-Alonso et al., 2021 [49] | * | * | NA | * | * | ** | * | 7 | Good |
| 14. | Bobbitt et al., 2022 [34] | * | * | NA | * | * | ** | * | 7 | Good |
| 15. | Kong et al., 2021 [36] | * | * | NA | * | * | ** | * | 7 | Good |
| 16. | Tham et al., 2022 [27] | * | * | NA | * | * | ** | * | 7 | Good |
| 17. | Mohammadi et al., 2022 [55] | * | * | NA | * | * | ** | * | 7 | Good |
| 18. | Chen et al., 2021 [25] | * | * | NA | * | * | ** | * | 7 | Good |
| 19. | Losurdo et al., 2020 [56] | * | * | NA | * | * | ** | * | 7 | Good |
| 20. | Geffer et al., 2022 [35] | * | * | NA | * | * | ** | * | 7 | Good |
| 21. | Porto et al., 2022 [37] | * | * | NA | * | * | ** | * | 7 | Good |
| 22. | Samaroo-Campbell et al., 2022 [41] | * | * | NA | * | * | ** | * | 7 | Good |
| 23. | Ochoa-Hein et al., 2021 [43] | * | * | NA | * | * | ** | * | 7 | Good |
| 24. | Ghali et al., 2021 [24] | * | * | NA | * | * | ** | * | 7 | Good |
| 25. | AlAhdal et al., 2022 [42] | * | * | NA | * | * | ** | * | 7 | Good |
| 26. | Ereth et al., 2021 [57] | * | * | NA | * | * | ** | * | 7 | Good |
| 27. | Bentivegna et al., 2021 [45] | * | * | NA | * | * | ** | * | 7 | Good |
| 28. | Choi et al., 2022 [46] | * | * | NA | * | * | * | * | 6 | Fair |
| 29. | Rosenthal et al., 2022 [39] | * | * | NA | * | * | ** | * | 7 | Good |
| 30. | Manea et al., 2021 [48] | * | * | NA | * | * | * | * | 6 | Fair |
| 31. | Jabarpour et al., 2021 [23] | * | * | NA | * | * | ** | * | 7 | Good |
| 32. | Baccolini et al., 2021 [22] | * | * | NA | * | * | ** | * | 7 | Good |
| 33. | Whitaker et al., 2022 [44] | * | * | NA | * | * | ** | * | 7 | Good |
| 34. | Ramos-Matinez et al., 2020 [58] | * | * | NA | * | * | * | * | 6 | Fair |
| 35. | Sipos et al., 2021 [50] | * | * | NA | * | * | ** | * | 7 | Good |
| 36. | Lastinger et al., 2022 [40] | * | * | NA | * | * | ** | * | 7 | Good |
| 37. | Patel et al., 2022 [38] | * | * | NA | * | * | ** | * | 7 | Good |
NA: Not applicable; Number of * represents the number of points.
3.4. Qualitative Summary of Results
3.4.1. The Effect of COVID-19 Pandemic on Overall Rate of Healthcare-Associated Infections (HAIs)
Six studies reported the overall effect of the pandemic on the HAIs [22,23,24,25,26,27]. Four of them showed a 7.6% to 66.4% increase in the overall rate of HAIs during the pandemic [22,24,25,27]. However, two studies reported an overall reduction in HAIs during the pandemic [23,26].
3.4.2. The Effect of COVID-19 Pandemic on Central Line-Associated Bloodstream Infections (CLABSIs)
The effect of the pandemic on CLABSIs was described in 15 studies [28,29,30,31,32,33,34,35,36,37,38,39,40,41,42]. The majority of the studies (n = 11, 73.3%) showed an increase in the rate of during the COVID-19 pandemic, and the increase ranged from 27.9% to 192.6% [28,29,31,32,33,34,37,38,39,40,41]. Of these studies, eight reported a statistically significant increase in CLABSIs during the pandemic [28,29,31,32,33,37,38,39]. Four studies reported a decrease in CLABSIs during the pandemic [30,35,36,42], but only one was statistically significant [30].
3.4.3. The Effect of COVID-19 Pandemic on Catheter-Associated Urinary Tract Infections (CAUTIs)
Similarly, 15 studies reported the impact of the COVID-19 pandemic on CAUTIs [22,28,30,31,32,33,34,35,36,39,40,41,42,43,44]. Seven studies demonstrated a 10.5% to 46.8% decrease in CAUTIs during the pandemic [28,33,35,36,42,43,44], while three studies reported a 20.5% to 74.7% increase in CAUTIs during the pandemic [31,34,41]. Two studies showed that there was no change in the rate of CAUTIs during the pandemic [30,32].
3.4.4. The Effect of COVID-19 Pandemic on Healthcare-Associated Clostridium Difficile Infection (CDI)
Of the 14 studies that reported this outcome, 12 studies (85.7%) showed a 4.9% to 88.2% decrease in the rate of healthcare-associated CDI during the pandemic [28,30,32,34,36,43,45,46,47,48,49,50]. However, only four of them demonstrated a significant reduction in CDI during the pandemic [32,46,49,50]. One study reported a non-statistically significant increase in the rate of CDI during the pandemic [31].
3.4.5. The Effect of COVID-19 Pandemic on Surgical Site Infections (SSIs)
Overall, the impact of the COVID-19 pandemic on SSIs was reported in seven studies [23,25,27,40,43,54,56]. Four of them showed a 14.2% to 60.7% decrease in SSIs during the pandemic [23,43,54,56], and only two studies showed a significant reduction in SSIs [23,56]. Conversely, Chen et al. reported an increase in SSIs from 11.8% to 14.8% during the pandemic (p = 0.084) [25].
3.4.6. The Effect of COVID-19 Pandemic on Ventilator-Associated Pneumonia
Four studies reported the effect of the pandemic on the rate of VAP [35,37,42,43], with two of them showing a significant reduction in VAP during the COVID-19 pandemic [35,42]. Geffer et al. found that the incidence of ventilator-associated lower respiratory tract infections declined from 2.95 before COVID-19 outbreak to 2.02 after COVID-19 outbreak (p < 0.001) [35].
3.5. Quantitative Summary of Results
3.5.1. Meta-Analysis for the Effect of COVID-19 Pandemic on Overall HAIs
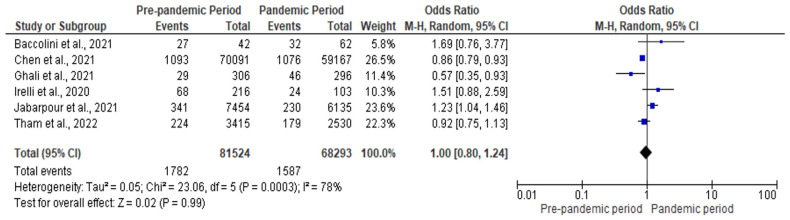
All the studies that reported the overall effect of the COVID-19 pandemic on HAIs was included in the meta-analysis. Figure 2 illustrates the forest plot for the effect of the pandemic on the overall risk of HAIs. The pooled estimate showed that the overall risk of HAIs in the pandemic period was similar to the pre-pandemic period (pooled odds ratio [OR]: 1.00; 95 CI: 0.80–1.24; p = 0.990). Nevertheless, the level of heterogeneity was high (I2 = 78%).
Figure 2.
Forest plot for the overall effect of COVID-19 pandemic on HAIs [22,23,24,25,26,27].
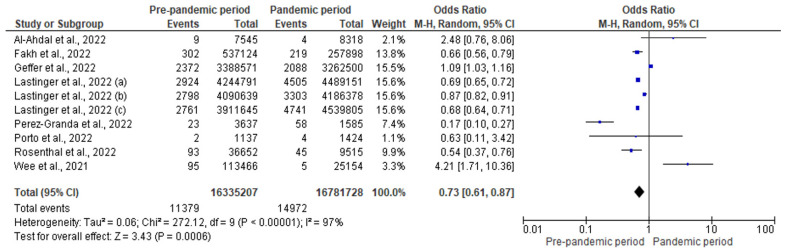
3.5.2. Meta-Analysis for the Effect of COVID-19 Pandemic on CLABSI
A forest plot (Figure 3) revealed that the risk of CLABSI was lower in the pre-pandemic period compared to the pandemic period (pooled OR: 0.73; 95% CI: 0.61–0.89). In other words, the risk of CLABSI was 27% lower in the pre-pandemic period (p < 0.001). However, there was a considerable degree of heterogeneity in this analysis (I2 = 97%).
Figure 3.
Forest plot for the effect of COVID-19 pandemic on CLABSI [29,30,33,35,37,39,40,42].
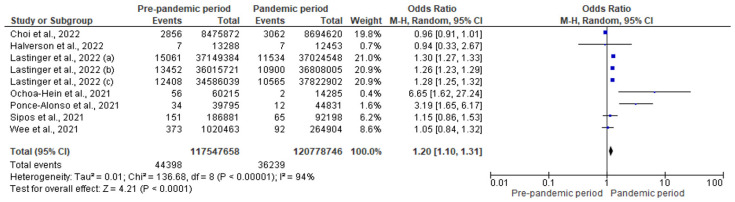
3.5.3. Meta-Analysis for the Effect of COVID-19 Pandemic on CDI
Figure 4 presents the forest plot for the effect of the COVID-19 pandemic on CDI. In the pre-pandemic period, 44,398 CDIs were reported in 117,547,658 patient days compared to 36,239 CDIs in 120,778,746 patient days observed during the pandemic. This corresponds to a significant 20% increase in the risk of CDI during the pandemic (pooled OR: 1.20; 95% CI: 1.10–1.31; p < 0.001).
Figure 4.
Forest plot for the impact of COVID-19 pandemic on CDI [30,31,40,46,47,49,50].
3.5.4. Meta-Analysis for the Effect of COVID-19 Pandemic on CAUTI
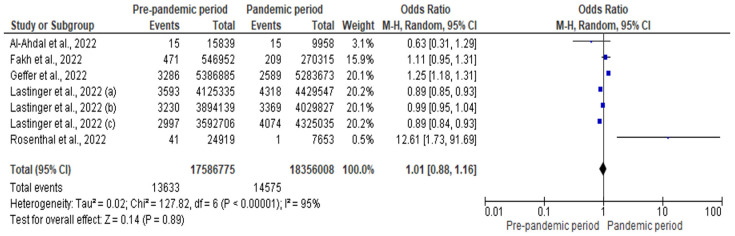
The number of CAUTIs was 13,633 and 14,575 during the pre-pandemic and pandemic period, respectively. There were 17,586,775 urinary catheter days in the pre-pandemic period and 18,356,008 urinary catheter days in the pandemic period. Figure 5 shows that there was a non-significant increase in the risk of CAUTI during the pandemic (pooled OR: 1.01; 95% CI: 0.88–1.16; p = 0.890; with a high degree of heterogeneity [I2 = 95%]).
Figure 5.
Forest plot for the impact of COVID-19 pandemic on CAUTI [33,35,39,40,42].
3.5.5. Meta-Analysis of the Impact of COVID-19 Pandemic on SSI
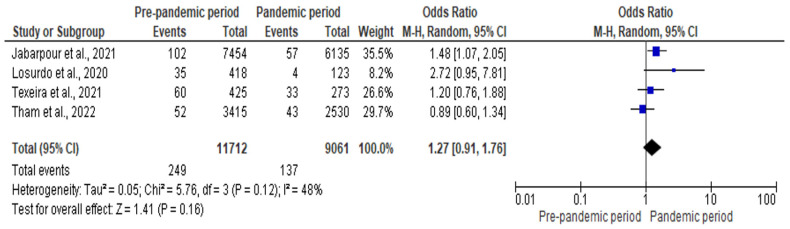
Four studies involving 11,712 and 9061 patients in the pre-pandemic and pandemic period, respectively, were included in the meta-analysis. The risk of SSI was 27% higher during the pandemic period compared to the pre-pandemic period (OR: 1.27; CI: 0.91–1.76; p = 0.16). There was a moderate degree of heterogeneity in this analysis (I2 = 48%). Figure 6 represents the forest plot for the meta-analysis of the impact of the COVID-19 pandemic on SSI.
Figure 6.
Forest plot for the impact of COVID-19 pandemic on SSI [23,27,54,56].
4. Discussion
This review examined the effect of the COVID-19 pandemic on the rate of HAIs, and included studies from different continents across the world. The majority of the studies were from North America and Europe with a few studies coming from Africa, Asia, South America, and Oceania. There was no difference in the overall risk of HAIs between the two periods. Conversely, patients hospitalized before the COVID-19 pandemic had a lower risk of CLABSI compared to those in the COVID-19 pandemic period. Similarly, there was a significant 20% increase in the risk of CDI during the COVID-19 pandemic. There was no significant increase in the risk of CAUTI and SSI during the pandemic. Therefore, infection prevention and control programs should be strengthened to reduce the burden of HAIs during and after the pandemic. The available evidence has shown that HAIs, particularly those involving multidrug-resistant organisms, have a high mortality rate [59,60]. There were no variations in the overall risk of HAIs between the two periods, and this implies that COVID-19 mitigation strategies did not affect the overall risk of HAIs. The improvements in hand and environmental hygiene during the COVID-19 pandemic was expected to reduce the incidence of HAIs [16]. However, this potential benefit could be counteracted by the disruption of other infection prevention and control programs such as the surveillance of HAIs, contact precaution and isolation of those colonized with multidrug-resistant pathogens in a separate room [12,13,61]. Therefore, the COVID-19 mitigation strategies that improved hand and environmental hygiene should be sustained, while the infection control measures that were disrupted during the pandemic should be resumed to reduce the incidence of HAIs.
The result also revealed that there was an increase in the risk of CLABSI during the pandemic compared to the period before the pandemic. Generally, hospitalized COVID-19 patients, especially those who are critically ill, have a higher risk of bloodstream infections compared to hospitalized non-COVID-19 patients [62]. This was attributed to the frequent use of a central line, use of immunosuppressive therapy, and reduced compliance with hand hygiene due to increased workload [62,63]. Therefore, improved hand hygiene is recommended to reduce the incidence of CLABSIs [64]. Furthermore, COVID-19 was significantly associated with a higher risk of CDI. CDI has been significantly associated with antibiotic use, the number of prescribed antibiotics, and the duration of antibiotic therapy [65,66,67]. There was a high rate of antibiotic prescription among COVID-19 patients [68,69,70]. The excessive use of antibiotics in COVID-19 patients despite a low rate of secondary infections explains the increase in the risk of CDI during the pandemic [71,72]. Therefore, antimicrobial stewardship is recommended to promote the rational use of antibiotics to reduce the risk of CDI. The effectiveness of antimicrobial stewardship programs in reducing the risk of CDI has been established [73]. In addition, infection control and prevention recommendations should be improved to minimize the horizontal transmission of CDI [74].
The results indicate that there was no significant increase in the risk of CAUTI and SSI during the pandemic. This implies that the infection control recommendations implemented to curb the transmission of COVID-19 did not significantly impact the risk of CAUTI and SSI. In the case of SSI, there are other measures besides infection control recommendations that are used to prevent SSI before, during, and after surgery. Typically, SSIs are preventable through preoperative antimicrobial prophylaxis. Previous studies have shown a low rate of compliance with recommendations for surgical antibiotic prophylaxis before the pandemic [75,76,77]. However, there was an increase in the use of preoperative antimicrobial prophylaxis for genitourinary procedures in the pandemic era compared to the period before the pandemic [78]. In addition to surgical antimicrobial prophylaxis, the duration of surgery, comorbidities such as diabetes and hypertension, tobacco smoking, and the American Society of Anesthesia (ASA) score, are significantly associated with SSIs [79,80,81,82]. These factors could explain the lack of significant improvement in the SSI rate in the pandemic era. Therefore, managing the modifiable risk factors associated with SSI coupled with infection control measures, and surgical antimicrobial prophylaxis is required to reduce the burden of SSI.
The results of this systematic review and meta-analysis should be interpreted with caution in light of some limitations. First, the distribution of the included studies was skewed towards North America and Europe, which accounted for most of the studies and this may affect the generalizability of the findings. However, all the continents were represented in the qualitative and quantitative analyses. Second, there were variations in the definition of HAIs and the classification of HAIs among the included studies, and this is a potential source of assessment and measurement bias. Third, the heterogeneous risk estimates were used by the included studies, where some studies reported the prevalence, while others reported the incidence per 1000 device days or per 1000 patient days. These variations reduced the number of studies included in the meta-analyses, which could potentially affect the findings. However, it is noteworthy that only studies with similar units of measurement were meta-analyzed. In addition, the study period for the included studies was highly variable. While some studies compared the prevalence or incidence in 2019 with 2020, others compared 2019 with 2021. Fourth, the infection prevention and control practices vary from one institution to another and between countries; therefore, the impact of the pandemic on HAIs could be inconsistent. Fifth, most of the studies used a before and after study design, which is associated with a high rate of bias. Sixth, the results for HAP/VAP were not meta-analyzed because the included studies used different units of measurement. Finally, substantial statistical heterogeneity was found in most of the meta-analyses. In spite of the limitations, this study shows evidence of the effect of the COVID-19 pandemic on the risk of HAIs among hospitalized patients.
5. Conclusions
The overall risk of HAI was observed to be unaffected by the COVID-19 pandemic. However, the COVID-19 pandemic was significantly associated with a higher risk of CLABSI and CDI. Therefore, more stringent infection prevention and control measures as well as prudent antimicrobial stewardship programs are warranted across all healthcare facilities to reduce the burden of HAIs during such pandemics. Further studies are required from developing countries, especially those in Africa and Asia.
Author Contributions
Conceptualization, U.A.; methodology, U.A., A.A., A.H.K. and K.A.; software, U.A.; formal analysis, U.A. and A.H.K.; writing—original draft preparation, U.A.; writing—review and editing, A.A., A.H.K. and K.A.; funding acquisition, U.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Open Access funding provided by Qatar University.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Storr J., Twyman A., Zingg W., Damani N., Kilpatrick C., Reilly J., Price L., Egger M., Grayson M.L., Kelley E., et al. Core components for effective infection prevention and control programmes: New WHO evidence-based recommendations. Antimicrob. Resist. Infect. Control. 2017;6:6. doi: 10.1186/s13756-016-0149-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Magill S.S., Edwards J.R., Bamberg W., Beldavs Z.G., Dumyati G., Kainer M.A., Lynfield R., Maloney M., McAllister-Hollod L., Nadle J., et al. Multistate point-prevalence survey of health care–associated infections. N. Engl. J. Med. 2014;370:1198–1208. doi: 10.1056/NEJMoa1306801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suetens C., Latour K., Kärki T., Ricchizzi E., Kinross P., Moro M.L., Jans B., Hopkins S., Hansen S., Lyytikäinen O., et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: Results from two European point prevalence surveys, 2016 to 2017. Eurosurveillance. 2018;23:1800516. doi: 10.2807/1560-7917.ES.2018.23.46.1800516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ling M.L., Apisarnthanarak A., Madriaga G. The burden of healthcare-associated infections in Southeast Asia: A systematic literature review and meta-analysis. Clin. Infect. Dis. 2015;60:1690–1699. doi: 10.1093/cid/civ095. [DOI] [PubMed] [Google Scholar]
- 5.Allegranzi B., Nejad S.B., Combescure C., Graafmans W., Attar H., Donaldson L., Pittet D. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. Lancet. 2011;377:228–241. doi: 10.1016/S0140-6736(10)61458-4. [DOI] [PubMed] [Google Scholar]
- 6.Abubakar U., Amir O., Rodríguez-Baño J. Healthcare-associated infections in Africa: A systematic review and meta-analysis of point prevalence studies. J. Pharm. Policy Pract. 2022;15:99. doi: 10.1186/s40545-022-00500-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abubakar U. Point-prevalence survey of hospital acquired infections in three acute care hospitals in Northern Nigeria. Antimicrob. Resist. Infect. Control. 2020;9:1–7. doi: 10.1186/s13756-020-00722-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loftus M.J., Guitart C., Tartari E., Stewardson A.J., Amer F., Bellissimo-Rodrigues F., Lee Y.F., Mehtar S., Sithole B.L., Pittet D. Hand hygiene in low-and middle-income countries. Int. J. Infect. Dis. 2019;86:25–30. doi: 10.1016/j.ijid.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Abubakar U., Al-Anazi M., Alanazi Z., Rodríguez-Baño J. Impact of COVID-19 pandemic on multidrug resistant gram positive and gram negative pathogens: A systematic review. J. Infect. Public Health. 2023;16:320–331. doi: 10.1016/j.jiph.2022.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ataiyero Y., Dyson J., Graham M. Barriers to hand hygiene practices among health care workers in sub-Saharan African countries: A narrative review. Am. J. Infect. Control. 2019;47:565–573. doi: 10.1016/j.ajic.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y., Yang J., Qiao F., Feng B., Hu F., Xi Z.A., Wu W., Ni Z.L., Liu L., Yuan Y. Compared hand hygiene compliance among healthcare providers before and after the COVID-19 pandemic: A rapid review and meta-analysis. Am. J. Infect. Control. 2022;50:563–571. doi: 10.1016/j.ajic.2021.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stevens M.P., Doll M., Pryor R., Godbout E., Cooper K., Bearman G. Impact of COVID-19 on traditional healthcare-associated infection prevention efforts. Infect. Control Hosp. Epidemiol. 2020;41:946–947. doi: 10.1017/ice.2020.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodríguez-Baño J., Rossolini G.M., Schultsz C., Tacconelli E., Murthy S., Ohmagari N., Holmes A., Bachmann T., Goossens H., Canton R., et al. Antimicrobial resistance research in a post-pandemic world: Insights on antimicrobial resistance research in the COVID-19 pandemic. J. Glob. Antimicrob. Resist. 2021;25:5–7. doi: 10.1016/j.jgar.2021.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Subramanya S.H., Czyż D.M., Acharya K.P., Humphreys H. The potential impact of the COVID-19 pandemic on antimicrobial resistance and antibiotic stewardship. Virus Dis. 2021;32:330–337. doi: 10.1007/s13337-021-00695-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McBride D.L. The impact of visiting restrictions during the COVID-19 pandemic on pediatric patients. J. Pediatr. Nurs. 2021;61:436–438. doi: 10.1016/j.pedn.2021.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abubakar U., Usman M.N., Baba M., Sulaiman A., Kolo M., Adamu F., Jaber A.A. Practices and perception of healthcare workers towards infection control measures during the COVID-19 pandemic: A cross-sectional online survey from Nigeria. J. Infect. Dev. Ctries. 2022;16:1398–1405. doi: 10.3855/jidc.14066. [DOI] [PubMed] [Google Scholar]
- 17.Page M.J., Moher D., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi: 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wells G.A., Shea B., O’Connell D., Peterson J., Welch V., Losos M., Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. [(accessed on 3 September 2023)]. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 19.Garner J.S., Jarvis W.R., Emori T.G., Horan T.C., Hughes J.M. CDC definitions for nosocomial infections, 1988. Am. J. Infect. Control. 1988;16:128–140. doi: 10.1016/0196-6553(88)90053-3. [DOI] [PubMed] [Google Scholar]
- 20.European Center for Disease Prevention and Control . Point Prevalence Survey of Healthcare Associated Infections and Antimicrobial Use in European Acute Care Hospitals—Protocol Version 5.3. ECDC; Stockholm, Sweden: 2016. [Google Scholar]
- 21.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baccolini V., Migliara G., Isonne C., Dorelli B., Barone L.C., Giannini D., Marotta D., Marte M., Mazzalai E., Alessandri F., et al. The impact of the COVID-19 pandemic on healthcare-associated infections in intensive care unit patients: A retrospective cohort study. Antimicrob. Resist. Infect. Control. 2021;10:87. doi: 10.1186/s13756-021-00959-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jabarpour M., Dehghan M., Afsharipour G., Hajipour Abaee E., Mangolian Shahrbabaki P., Ahmadinejad M., Maazallahi M. The impact of COVID-19 outbreak on nosocomial infection rate: A case of Iran. Can. J. Infect. Dis. Med. Microbiol. 2021;2021:6650920. doi: 10.1155/2021/6650920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghali H., Ben Cheikh A., Bhiri S., Khefacha S., Latiri H.S., Ben Rejeb M. Trends of Healthcare-associated Infections in a Tuinisian University Hospital and Impact of COVID-19 Pandemic. INQUIRY J. Health Care Organ. Provis. Financ. 2021;58:00469580211067930. doi: 10.1177/00469580211067930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen C., Zhu P., Zhang Y., Liu B. Effect of the “Normalized Epidemic Prevention and Control Requirements” on hospital-acquired and community-acquired infections in China. BMC Infect. Dis. 2021;21:1178. doi: 10.1186/s12879-021-06886-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Irelli E.C., Orlando B., Cocchi E., Morano A., Fattapposta F., Di Piero V., Toni D., Ciardi M.R., Giallonardo A.T., Fabbrini G., et al. The potential impact of enhanced hygienic measures during the COVID-19 outbreak on hospital-acquired infections: A pragmatic study in neurological units. J. Neurol. Sci. 2020;418:117111. doi: 10.1016/j.jns.2020.117111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tham N., Fazio T., Johnson D., Skandarajah A., Hayes I.P. Hospital Acquired Infections in Surgical Patients: Impact of COVID-19-Related Infection Prevention Measures. World J. Surg. 2022;46:1249–1258. doi: 10.1007/s00268-022-06539-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alsuhaibani M., Kobayashi T., McPherson C., Holley S., Marra A.R., Trannel A., Dains A., Abosi O.J., Jenn K.E., Meacham H., et al. Impact of COVID-19 on an infection prevention and control program, Iowa 2020–2021. Am. J. Infect. Control. 2022;50:277–282. doi: 10.1016/j.ajic.2021.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pérez-Granda M.J., Carrillo C.S., Rabadán P.M., Valerio M., Olmedo M., Muñoz P., Bouza E. Increase in the frequency of catheter-related bloodstream infections during the COVID-19 pandemic: A plea for Control. J. Hosp. Infect. 2022;119:149–154. doi: 10.1016/j.jhin.2021.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wee L.E., Conceicao E.P., Tan J.Y., Magesparan K.D., Amin I.B., Ismail B.B., Toh H.X., Jin P., Zhang J., Wee E.G., et al. Unintended consequences of infection prevention and control measures during COVID-19 pandemic. Am. J. Infect. Control. 2021;49:469–477. doi: 10.1016/j.ajic.2020.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Halverson T., Mikolajczak A., Mora N., Silkaitis C., Stout S. Impact of COVID-19 on hospital acquired infections. Am. J. Infect. Control. 2022;50:831–833. doi: 10.1016/j.ajic.2022.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Advani S.D., Sickbert-Bennett E., Moehring R., Cromer A., Lokhnygina Y., Dodds-Ashley E., Kalu I.C., DiBiase L., Weber D.J., Anderson D.J., et al. The Disproportionate Impact of COVID-19 Pandemic on Healthcare-Associated Infections in Community Hospitals: Need for Expanding the Infectious Disease Workforce. Clin. Infect. Dis. 2022;76:e34–e41. doi: 10.1093/cid/ciac684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fakih M.G., Bufalino A., Sturm L., Huang R.H., Ottenbacher A., Saake K., Winegar A., Fogel R., Cacchione J. Coronavirus disease 2019 (COVID-19) pandemic, central-line–associated bloodstream infection (CLABSI), and catheter-associated urinary tract infection (CAUTI): The urgent need to refocus on hardwiring prevention efforts. Infect. Control Hosp. Epidemiol. 2022;43:26–31. doi: 10.1017/ice.2021.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bobbitt L.J., Satyanarayana G., Baum L.V., Nebhan C.A., Kassim A.A., Gatwood K.S. Evaluation of healthcare-associated infection rates in patients with hematologic malignancies and stem cell transplantation during the coronavirus disease 2019 (COVID-19) pandemic. Antimicrob. Steward. Healthc. Epidemiol. 2022;2:e11. doi: 10.1017/ash.2021.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Geffers C., Schwab F., Behnke M., Gastmeier P. No increase of device associated infections in German intensive care units during the start of the COVID-19 pandemic in 2020. Antimicrob. Resist. Infect. Control. 2022;11:67. doi: 10.1186/s13756-022-01108-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kong A., Botero Suarez C.S., Rahamatalli B., Shankweiler J., Karasik O. Hand Hygiene and Hospital-Acquired Infections During COVID-19 Increased Vigilance: One Hospital’s Experience. HCA Healthc. J. Med. 2021;2:11. doi: 10.36518/2689-0216.1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Porto A.P., Borges I.C., Buss L., Machado A., Bassetti B.R., Cocentino B., Bicalho C.S., Carrilho C.M., Rodrigues C., Neto E.A., et al. Healthcare-associated infections on the intensive care unit in 21 Brazilian hospitals during the early months of the coronavirus disease 2019 (COVID-19) pandemic: An ecological study. Infect. Control Hosp. Epidemiol. 2022;44:284–290. doi: 10.1017/ice.2022.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Patel P.R., Weiner-Lastinger L.M., Dudeck M.A., Fike L.V., Kuhar D.T., Edwards J.R., Pollock D., Benin A. Impact of COVID-19 pandemic on central-line–associated bloodstream infections during the early months of 2020, National Healthcare Safety Network. Infect. Control Hosp. Epidemiol. 2022;43:790–793. doi: 10.1017/ice.2021.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosenthal V.D., Myatra S.N., Divatia J.V., Biswas S., Shrivastava A., Al-Ruzzieh M.A., Ayaad O., Bat-Erdene A., Bat-Erdene I., Narankhuu B., et al. The impact of COVID-19 on health care–associated infections in intensive care units in low-and middle-income countries: International Nosocomial Infection Control Consortium (INICC) findings. Int. J. Infect. Dis. 2022;118:83–88. doi: 10.1016/j.ijid.2022.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lastinger L.M., Alvarez C.R., Kofman A., Konnor R.Y., Kuhar D.T., Nkwata A., Patel P.R., Pattabiraman V., Xu S.Y., Dudeck M.A. Continued Increases in HAI Incidence During the Second Year of the COVID-19 Pandemic. Infect. Control Hosp. Epidemiol. 2023;44:997–1001. doi: 10.1017/ice.2022.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Samaroo-Campbell J., Qiu W., Asrat H., Abdallah M., Fornek M., Episcopia B., Quale J. The initial and lingering impact of coronavirus disease 2019 (COVID-19) on catheter-associated infections in a large healthcare system in New York City. Antimicrob. Steward. Healthc. Epidemiol. 2022;2:e77. doi: 10.1017/ash.2022.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.AlAhdal A.M., Alsada S.A., Alrashed H.A., Al Bazroun L.I., Alshoaibi A. Impact of the COVID-19 Pandemic on Levels of Device-Associated Infections and Hand Hygiene Compliance. Cureus. 2022;14:e24254. doi: 10.7759/cureus.24254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ochoa-Hein E., González-Lara M.F., Huertas-Jiménez M.A., Chávez-Ríos A.R., de-Paz-García R., Haro-Osnaya A., González-González R., Cruz-Juárez B.S., Hernández-Gilsoul T., Rivero-Sigarroa E., et al. Surge in Ventilator-Associated Pneumonias and Bloodstream Infections in An Academic Referral Center Converted to Treat COVID-19 Patients. Rev. Investig. Clínica. 2021;73:210–215. doi: 10.24875/RIC.21000130. [DOI] [PubMed] [Google Scholar]
- 44.Whitaker A., Colgrove G., Scheutzow M., Ramic M., Monaco K., Hill J.L., Jr. Decreasing Catheter-Associated Urinary Tract Infection (CAUTI) at a community academic medical center using a multidisciplinary team employing a multi-pronged approach during the COVID-19 pandemic. Am. J. Infect. Control. 2023;51:319–323. doi: 10.1016/j.ajic.2022.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bentivegna E., Alessio G., Spuntarelli V., Luciani M., Santino I., Simmaco M., Martelletti P. Impact of COVID-19 prevention measures on risk of health care-associated Clostridium difficile infection. Am. J. Infect. Control. 2021;49:640–642. doi: 10.1016/j.ajic.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Choi K.B., Du T., Silva A., Golding G.R., Pelude L., Mitchell R., Rudnick W., Hizon R., Al-Rawahi G.N., Chow B., et al. Trends in Clostridioides difficile infection rates in Canadian hospitals during the coronavirus disease 2019 (COVID-19) pandemic. Infect. Control Hosp. Epidemiol. 2022;44:1180–1183. doi: 10.1017/ice.2022.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ochoa-Hein E., Rajme-López S., Rodríguez-Aldama J.C., Huertas-Jiménez M.A., Chávez-Ríos A.R., de Paz-García R., Haro-Osnaya A., González-Colín K.K., González-González R., González-Lara M.F., et al. Substantial reduction of healthcare facility-onset Clostridioides difficile infection (HO-CDI) rates after conversion of a hospital for exclusive treatment of COVID-19 patients. Am. J. Infect. Control. 2021;49:966–968. doi: 10.1016/j.ajic.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Manea E., Jipa R., Milea A., Roman A., Neagu G., Hristea A. Healthcare-associated infection during the COVID-19 pandemic in a tertiary care hospital in Romania. Rom. J. Intern. Med. 2021;59:409–415. doi: 10.2478/rjim-2021-0020. [DOI] [PubMed] [Google Scholar]
- 49.Ponce-Alonso M., De La Fuente J.S., Rincón-Carlavilla A., Moreno-Nunez P., Martínez-García L., Escudero-Sánchez R., Pintor R., García-Fernández S., Cobo J. Impact of the coronavirus disease 2019 (COVID-19) pandemic on nosocomial Clostridioides difficile infection. Infect. Control Hosp. Epidemiol. 2021;42:406–410. doi: 10.1017/ice.2020.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sipos S., Vlad C., Prejbeanu R., Haragus H., Vlad D., Cristian H., Dumitrascu C., Popescu R., Dumitrascu V., Predescu V. Impact of COVID-19 prevention measures on Clostridioides difficile infections in a regional acute care hospital. Exp. Ther. Med. 2021;22:1215. doi: 10.3892/etm.2021.10649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sturm L.K., Saake K., Roberts P.B., Masoudi F.A., Fakih M.G. Impact of COVID-19 pandemic on hospital onset bloodstream infections (HOBSI) at a large health system. Am. J. Infect. Control. 2022;50:245–249. doi: 10.1016/j.ajic.2021.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Polly M., de Almeida B.L., Lennon R.P., Cortês M.F., Costa S.F., Guimarães T. Impact of the COVID-19 pandemic on the incidence of multidrug-resistant bacterial infections in an acute care hospital in Brazil. Am. J. Infect. Control. 2022;50:32–38. doi: 10.1016/j.ajic.2021.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kitt E., Brennan L., Harrison C., Hei H., Paul E., Satchell L., Wilson K.B., Smathers S., Handy L., Coffin S.E. Dodging the bundle—Persistent healthcare-associated rhinovirus infection throughout the pandemic. Am. J. Infect. Control. 2022;50:1140–1144. doi: 10.1016/j.ajic.2022.04.016. [DOI] [PubMed] [Google Scholar]
- 54.Teixeira B.L., Cabral J., Marques-Pinto A., Vila F., Lindoro J., Fraga A. How the COVID-19 pandemic changed postoperative infections in urology wards: A retrospective cohort study from two urology departments. Can. Urol. Assoc. J. 2022;16:E267. doi: 10.5489/cuaj.7521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mohammadi A., Khatami F., Azimbeik Z., Khajavi A., Aloosh M., Aghamir S.M. Hospital-acquired infections in a tertiary hospital in Iran before and during the COVID-19 pandemic. Wien. Med. Wochenschr. 2022;172:220–226. doi: 10.1007/s10354-022-00918-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Losurdo P., Paiano L., Samardzic N., Germani P., Bernardi L., Borelli M., Pozzetto B., de Manzini N., Bortul M. Impact of lockdown for SARS-CoV-2 (COVID-19) on surgical site infection rates: A monocentric observational cohort study. Updates Surg. 2020;72:1263–1271. doi: 10.1007/s13304-020-00884-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ereth M.H., Fine J., Stamatatos F., Mathew B., Hess D., Simpser E. Healthcare-associated infection impact with bioaerosol treatment and COVID-19 mitigation measures. J. Hosp. Infect. 2021;116:69–77. doi: 10.1016/j.jhin.2021.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ramos-Martínez A., Fernández-Cruz A., Domínguez F., Forteza A., Cobo M., Sánchez-Romero I., Asensio A. Hospital-acquired infective endocarditis during Covid-19 pandemic. Infect. Prev. Pract. 2020;2:100080. doi: 10.1016/j.infpip.2020.100080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Abubakar U., Tangiisuran B., Elnaem M.H., Sulaiman S.A., Khan F.U. Mortality and its predictors among hospitalized patients with infections due to extended spectrum beta-lactamase (ESBL) Enterobacteriaceae in Malaysia: A retrospective observational study. Future J. Pharm. Sci. 2022;8:17. doi: 10.1186/s43094-022-00406-8. [DOI] [Google Scholar]
- 60.Abubakar U., Zulkarnain A.I., Rodríguez-Baño J., Kamarudin N., Elrggal M.E., Elnaem M.H., Harun S.N. Treatments and Predictors of Mortality for Carbapenem-Resistant Gram-Negative Bacilli Infections in Malaysia: A Retrospective Cohort Study. Trop. Med. Infect. Dis. 2022;7:415. doi: 10.3390/tropicalmed7120415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Elliott T.M., Hurst C., Doidge M., Hurst T., Harris P.N., Gordon L.G. Unexpected benefit of COVID-19 hospital restrictions: Reduction in patients isolating with multidrug resistant organisms after restrictions were lifted. Infect. Dis. Health. 2022;27:10–14. doi: 10.1016/j.idh.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ippolito M., Simone B., Filisina C., Catalanotto F.R., Catalisano G., Marino C., Misseri G., Giarratano A., Cortegiani A. Bloodstream infections in hospitalized patients with COVID-19: A systematic review and meta-analysis. Microorganisms. 2021;9:2016. doi: 10.3390/microorganisms9102016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Giacobbe D.R., Battaglini D., Ball L., Brunetti I., Bruzzone B., Codda G., Crea F., De Maria A., Dentone C., Di Biagio A., et al. Bloodstream infections in critically ill patients with COVID-19. Eur. J. Clin. Investig. 2020;50:e13319. doi: 10.1111/eci.13319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Balla K.C., Rao S.P., Arul C., Shashidhar A., Prashantha Y.N., Nagaraj S., Suresh G. Decreasing central line-associated bloodstream infections through quality improvement initiative. Indian Pediatr. 2018;55:753–756. doi: 10.1007/s13312-018-1374-5. [DOI] [PubMed] [Google Scholar]
- 65.Eze P., Balsells E., Kyaw M.H., Nair H. Risk factors for Clostridium difficile infections–an overview of the evidence base and challenges in data synthesis. J. Glob. Health. 2017;7:010417. doi: 10.7189/jogh.07.010417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chalmers J.D., Akram A.R., Singanayagam A., Wilcox M.H., Hill A.T. Risk factors for Clostridium difficile infection in hospitalized patients with community-acquired pneumonia. J. Infect. 2016;73:45–53. doi: 10.1016/j.jinf.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 67.Loo V.G., Bourgault A.M., Poirier L., Lamothe F., Michaud S., Turgeon N., Toye B., Beaudoin A., Frost E.H., Gilca R., et al. Host and pathogen factors for Clostridium difficile infection and colonization. N. Engl. J. Med. 2011;365:1693–1703. doi: 10.1056/NEJMoa1012413. [DOI] [PubMed] [Google Scholar]
- 68.Dieringer T.D., Furukawa D., Graber C.J., Stevens V.W., Jones M.M., Rubin M.A., Goetz M.B. Inpatient antibiotic utilization in the Veterans’ Health Administration during the coronavirus disease 2019 (COVID-19) pandemic. Infect. Control Hosp. Epidemiol. 2021;42:751–753. doi: 10.1017/ice.2020.1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Elligsen M., Wan M., Lam P.W., Lo J., Taggart L.R., Chan A.J., Downing M., Gough K., Seah J., Leung E. Trends in hospital antibiotic utilization during the coronavirus disease 2019 (COVID-19) pandemic: A multicenter interrupted time-series analysis. Antimicrob. Steward. Healthc. Epidemiol. 2022;2:e128. doi: 10.1017/ash.2022.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Castro-Lopes A., Correia S., Leal C., Resende I., Soares P., Azevedo A., Paiva J.A. Increase of antimicrobial consumption in a tertiary care hospital during the first phase of the COVID-19 pandemic. Antibiotics. 2021;10:778. doi: 10.3390/antibiotics10070778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Langford B.J., So M., Raybardhan S., Leung V., Westwood D., MacFadden D.R., Soucy J.P., Daneman N. Bacterial co-infection and secondary infection in patients with COVID-19: A living rapid review and meta-analysis. Clin. Microbiol. Infect. 2020;26:1622–1629. doi: 10.1016/j.cmi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Langford B.J., So M., Raybardhan S., Leung V., Soucy J.P., Westwood D., Daneman N., MacFadden D.R. Antibiotic prescribing in patients with COVID-19: Rapid review and meta-analysis. Clin. Microbiol. Infect. 2021;27:520–531. doi: 10.1016/j.cmi.2020.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Patton A., Davey P., Harbarth S., Nathwani D., Sneddon J., Marwick C.A. Impact of antimicrobial stewardship interventions on Clostridium difficile infection and clinical outcomes: Segmented regression analyses. J. Antimicrob. Chemother. 2018;73:517–526. doi: 10.1093/jac/dkx413. [DOI] [PubMed] [Google Scholar]
- 74.Ananthakrishnan A.N. Clostridium difficile infection: Epidemiology, risk factors and management. Nat. Rev. Gastroenterol. Hepatol. 2011;8:17–26. doi: 10.1038/nrgastro.2010.190. [DOI] [PubMed] [Google Scholar]
- 75.Abubakar U. Antibiotic use among hospitalized patients in northern Nigeria: A multicenter point-prevalence survey. BMC Infect. Dis. 2020;20:86. doi: 10.1186/s12879-020-4815-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Abubakar U., Syed Sulaiman S.A., Adesiyun A.G. Utilization of surgical antibiotic prophylaxis for obstetrics and gynaecology surgeries in Northern Nigeria. Int. J. Clin. Pharm. 2018;40:1037–1043. doi: 10.1007/s11096-018-0702-0. [DOI] [PubMed] [Google Scholar]
- 77.Abubakar U., Syed Sulaiman S.A., Adesiyun A.G. Impact of pharmacist-led antibiotic stewardship interventions on compliance with surgical antibiotic prophylaxis in obstetric and gynecologic surgeries in Nigeria. PLoS ONE. 2019;14:e0213395. doi: 10.1371/journal.pone.0213395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mukai S., Nomi M., Kozawa S., Yanagiuchi A., Shigemura K., Sengoku A. The impact of the coronavirus disease 2019 pandemic on changes in antimicrobial prophylaxis and development of genito-urinary tract infections after urodynamic study: A retrospective comparative study of a single rehabilitation hospital in Japan. Neurourol. Urodyn. 2022;41:1440–1450. doi: 10.1002/nau.24979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.AlGamdi S.S., Alawi M., Bokhari R., Bajunaid K., Mukhtar A., Baeesa S.S. Risk factors for surgical site infection following spinal surgery in Saudi Arabia: A retrospective case–control study. Medicine. 2021;100:e25567. doi: 10.1097/MD.0000000000025567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Patel S., Thompson D., Innocent S., Narbad V., Selway R., Barkas K. Risk factors for surgical site infections in neurosurgery. Ann. R. Coll. Surg. Engl. 2019;101:220–225. doi: 10.1308/rcsann.2019.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Xue D.Q., Qian C., Yang L., Wang X.F. Risk factors for surgical site infections after breast surgery: A systematic review and meta-analysis. Eur. J. Surg. Oncol. (EJSO) 2012;38:375–381. doi: 10.1016/j.ejso.2012.02.179. [DOI] [PubMed] [Google Scholar]
- 82.Jain R.K., Shukla R., Singh P., Kumar R. Epidemiology and risk factors for surgical site infections in patients requiring orthopedic surgery. Eur. J. Orthop. Surg. Traumatol. 2015;25:251–254. doi: 10.1007/s00590-014-1475-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.