Abstract
Circulating tumor cells (CTCs) have emerged as pivotal biomarkers with significant predictive and prognostic implications in solid tumors. Their presence in peripheral blood offers a non-invasive window into the dynamic landscape of cancer progression and treatment response. This narrative literature review synthesizes the current state of knowledge surrounding the multifaceted role of CTCs in predicting clinical outcomes and informing prognosis across a spectrum of solid tumor malignancies. This review delves into the evolving landscape of CTC-based research, emphasizing their potential as early indicators of disease recurrence, metastatic potential, and therapeutic resistance. Moreover, we have underscored the dynamic nature of CTCs and their implications for personalized medicine. A descriptive and critical analysis of CTC detection methodologies, their clinical relevance, and their associated challenges is also presented, with a focus on recent advancements and emerging technologies. Furthermore, we examine the integration of CTC-based liquid biopsies into clinical practice, highlighting their role in guiding treatment decisions, monitoring treatment efficacy, and facilitating precision oncology. This review highlights the transformative impact of CTCs as predictive and prognostic biomarkers in the management of solid tumors by promoting a deeper understanding of the clinical relevance of CTCs and their role in advancing the field of oncology.
Keywords: circulating tumor cells, cancer genetics, prognosis, biomarkers, tumor heterogeneity
1. Introduction
Cancer has emerged as a prominent cause of death in both the United States and globally. In contrast to other severe ailments, the mortality rate associated with cancer has been steadily decreasing. In the past decade, there has been an overall reduction in cancer-related deaths, with a notable decline of approximately 33% [1]. This decrease is attributed to a myriad of factors, encompassing more effective cancer screening, enhanced diagnostic tools, advancements in surgical and radiological techniques, and the emergence of systemic treatments such as chemotherapy, immunotherapy, and targeted therapies. The key to further diminishing cancer-related mortality in the future lies in early cancer detection, personalized treatment approaches, and the implementation of effective strategies to prevent or mitigate metastasis. The majority of solid tumor diagnoses are typically established through radiographic and physical examinations, and subsequently confirmed through pathological findings obtained via tissue biopsy.
An innovative alternative for cancer detection is liquid biopsy, which entails the examination of circulating tumor cells (CTCs) and circulating tumor DNA (ctDNA). Remarkably, although CTCs were identified as far back as 1869 and ctDNA in 1948 [2], their practical application has only recently come to fruition. CTCs have high vitality and possess significant metastatic potential. They originate from primary or metastatic tumors of epithelial origin and enter the bloodstream. CTCs represent a crucial component of liquid biopsy, offering a dynamic window into real-time tumor progression monitoring [3,4]. Unlike traditional high-throughput sequencing analysis of tumor tissue, which involves analyzing a mixed sample of millions of cells and reflects the overall genomic characteristics of the cells, CTCs and cancer stem cells (CSCs), along with other low-abundance yet functionally significant cells, often have their genetic material diluted in such analyses. Thanks to the advent of single-cell sequencing technology, the possibility of isolating and characterizing CTCs is poised to become increasingly integral in cancer management [5,6].
In this narrative review, we explore various CTC detection methods and present the current body of evidence supporting the integration of CTC detection into clinical practice. This article delves into the potential applications of CTCs in solid tumors, encompassing cancer screening, diagnostics, treatment guidance, and surveillance. We have conducted a review and synthesis of pertinent studies available on PubMed and Google Scholar (last accessed on 2 September 2023) regarding the role of CTCs in solid tumors, which are anticipated to influence the future landscape of CTC utilization.
2. Role of CTCs in Metastatic Pathway
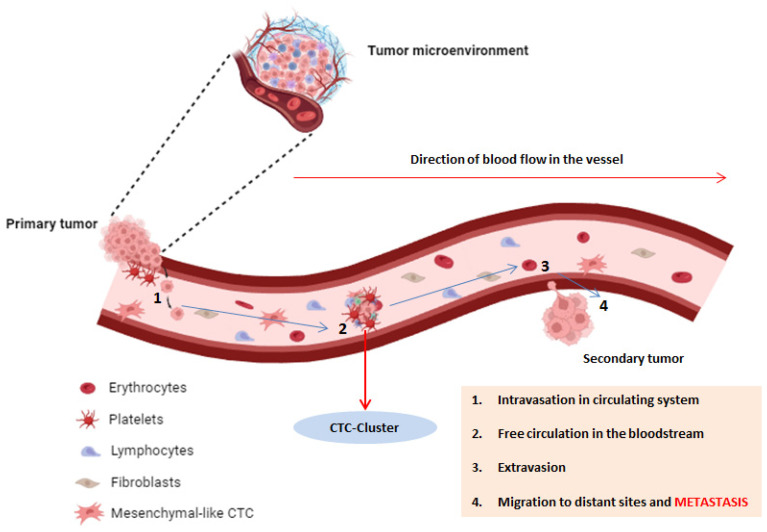
Metastasis, the dissemination of cancer from the primary tumor to distant bodily locations, represents a highly intricate and dynamic process. This multifaceted event unfolds through a sequence of distinct stages, including local invasion, intravasation, circulation survival, extravasation, and the eventual establishment of colonies in remote organs [7]. Central to this process are CTCs, which have detached from the primary tumor and entered the bloodstream, facilitating their journey to distant sites throughout the body. Their presence in peripheral blood has the potential to predict the development of metastasis, associated with poor prognosis, making them a crucial focus in the study of metastatic pathways [8]. Several interesting studies in the literature suggest that probably only a specific subset of tumor cells possess the ability to metastasize, such as those with clonogenic potential and stem cell properties. Conversely, a significant majority of cells with a tumor cell phenotype may not survive in the circulation [9]. CTCs encompass a diverse array of cells displaying a range of characteristics, encompassing epithelial, mesenchymal, and hybrid phenotypes. The heterogeneous nature of CTCs presents considerable complexities in deciphering their exact functions in the metastatic process. Recent investigations have shed light on the dynamic phenotypic transitions that CTCs experience as they traverse the circulatory system, and these transformations can significantly impact their capacity for extravasation and the establishment of colonies in distant organs [10]. To initiate the metastatic process, tumor cells must initially breach the basement membrane, allowing their eventual entry into the bloodstream through a phenomenon known as intravasation (Figure 1).
Figure 1.
The depiction of CTCs involves their detachment from the primary tumor, intravasation into the bloodstream, and subsequent circulation for the purpose of colonizing distant organs. Following extravasation, they establish secondary metastases. Fundamentally, the process involves circulating tumor cells undergoing epithelial-to-mesenchymal transition (EMT). During EMT, cancerous epithelial cells lose their cell-to-cell contact, adopting a more motile and less differentiated mesenchymal phenotype. CTCs can manifest either as single cells or as cell clusters, the latter exhibiting an enhanced metastatic potential. This diversity in CTC presentation captures a broader spectrum of clonal populations within a tumor, providing a comprehensive portrayal of tumor composition and its dynamic changes over time. Distinguishing themselves from other circulating cells in the blood, CTCs express specific EMT biomarkers, such as epithelial cell adhesion molecules (EpCAM) and cytokeratins (CKs).
This transition involves the downregulation of epithelial cadherin and the upregulation of neural cadherin, leading to the disruption of cell-to-cell adhesion and the acquisition of a mesenchymal phenotype. The degradation of the extracellular matrix is primarily driven by the action of matrix metalloproteinases and the urokinase plasminogen activator system, with their involvement often linked to the process of epithelial–mesenchymal transition (EMT) [11]. In the context of CTCs, there is noteworthy upregulation of EMT-related markers. This upregulation suggests a spectrum in the development of CTC phenotypes, ranging from an epithelial to a mesenchymal differentiation state. Intriguingly, various cancer types exhibit distinctive CTC phenotypes [12]. For instance, in lobular tumors, CTCs predominantly display epithelial characteristics, whereas in triple-negative and human epidermal growth factor receptor 2 (HER2)-positive tumors, CTCs tend to adopt a more mesenchymal profile [13]. Furthermore, in patients responding to therapy, mesenchymal CTCs were found in reduced numbers. In an intriguing study, the role of transforming growth factor-beta (TGF-beta) in EMT has been proposed, with EMT-related markers demonstrating more accurate prognostic value compared to epithelial markers. Therefore, the inclusion of EMT markers is believed to aid in identifying the more aggressive CTC phenotype, as these cells possess the potential for extravasation and adaptation to the microenvironment [14].
One of the critical challenges CTCs face is surviving in the hostile environment of the bloodstream. Platelets play a pivotal role in protecting CTCs from immune surveillance, thereby enhancing their survival. Understanding the interactions between CTCs and platelets is essential for unraveling the mechanisms that enable CTCs to evade immune defenses. Indeed, it has been discovered that when entering the systemic circulation, CTCs encounter a hostile environment. Platelets aggregate with these tumor cells, shielding them from natural killer cell-mediated lysis [15]. Consequently, a higher platelet count is associated with reduced survival. Conversely, treatment with anticoagulants has shown the ability to decrease metastasis [16,17,18]. The microenvironment at the metastatic site plays a pivotal role in determining whether CTCs can successfully colonize and establish secondary tumors. This microenvironment comprises various cell types, including endothelial cells, stromal fibroblasts, and immune cells. Crosstalk between CTCs and the microenvironment can modulate the fate of disseminated tumor cells and influence their dormancy or proliferation. For example, it has been discovered that tumor-associated macrophages enhance invasiveness through the release of epidermal growth factors [19]. A fascinating aspect of CTC biology is their ability to enter a state of dormancy, where they remain quiescent for extended periods. This dormancy period can be influenced by various factors, including immune surveillance, angiogenic signals, and interactions with the microenvironment. Understanding the mechanisms underlying CTC dormancy and reactivation is essential for developing targeted therapeutic strategies [20].
Certain malignancies exhibit a predilection for particular organs during the metastatic process, a phenomenon that is orchestrated by chemokines such as stromal cell-derived factor-1 (SDF-1) and CCL21. These chemokines are typically expressed at the sites of metastasis, and tumor cells frequently exhibit an overexpression of the corresponding receptor, CXCR4 [21]. To facilitate the reception of incoming tumor cells, the microenvironment at the metastatic site needs to be prepped accordingly. Some research indicates that hematopoietic progenitor cells play a role in creating this conducive niche. When tumor cells interact with the local microenvironment, they undergo a transition to an epithelial phenotype, enabling adhesion and proliferation. Consequently, secondary metastatic lesions often closely resemble the primary tumor in terms of phenotype. This phenomenon, known as mesenchymal–epithelial transition (MET), is marked by characteristics such as unlimited replicative potential, tissue invasion, and metastatic spread [22]. CTCs play a crucial role in the metastatic process, and their investigation will yield valuable insights into the mechanisms governing cancer spread, thereby creating new opportunities for the development of targeted therapies aimed at disrupting the metastatic cascade and enhancing the outlook for cancer patients.
3. Circulating Tumor Cells: Detection and Isolation
CTCs are highly dynamic cancer cells found in the peripheral blood of individuals afflicted with solid tumors. They serve as a crucial component in liquid tumor biopsies, holding significant diagnostic value. Both the quantity and the phenotypic characteristics of CTCs demonstrate a notable correlation with the progression of the primary tumor. The scrutiny and examination of CTC quantities and phenotypes offer an indirect means to glean insights into the characteristics of the tumor lesions [23]. The application of CTCs for monitoring the advancement of solid tumors through peripheral blood analysis has gained widespread recognition. Given the relatively low prevalence of CTCs in peripheral blood in comparison to other blood cell types, distinguishing them poses a considerable challenge. In the context of liquid biopsy, approximately one CTC can be identified among ten million white blood cells per milliliter of blood [24]. Adding a layer of complexity, akin to primary tumors, these circulating cells demonstrate heterogeneity, featuring multiple subpopulations expressing diverse molecular markers [25]. The absence of a universally shared marker or molecular signature across all cancer cells poses a formidable challenge in devising highly accurate CTC isolation techniques. To address this challenge, innovative isolation devices have been developed, focusing on leveraging epithelial marker proteins that are expressed on tumor cells while being absent in surrounding blood cells. As biological technologies continue to advance, especially with the development of novel nanomaterials and microfluidic systems, several techniques have emerged for the detection of peripheral CTCs in blood [26]. These methodologies can be broadly classified into two primary categories: label-dependent (Table 1) [27,28,29,30] and label-independent detection (Table 2) [31,32,33,34,35,36,37].
Table 1.
Schematic representation of the main CTC label-dependent isolation techniques.
| CTC Isolation Technique |
Method | Tumor Type | Clinical Objective | Major Advantages |
Major Disadvantages |
Ref. | |
|---|---|---|---|---|---|---|---|
| Label-Dependent Isolation |
Magnetic nanoparticles |
Antibody conjugation to magnetic nanoparticles selectively linked to specific markers expressed by CTCs | Breast Colorectal Prostate Ovarian |
Prognosis Treatment |
High capture Very Fast |
Expensive Low cell viability Low sensitivity |
[27] |
| Microfluidic chip | Microfluidic chip with functionalized Surfaces in controlled flow to enhance CTC binding to antibody |
Breast Prostate Pancreatic Lung |
Diagnosis Prognosis Treatment |
Cheap High sensitivity High efficiency High cell variability |
Small sample vol. Slow flow rate |
[28,29] | |
| Dual modality | Microfluidic platform (columns) with micromagnetic particles functionalized (EpCAM) | Breast Prostate NSCLC Colorectal |
Prognosis Diagnosis |
Very high efficiency Very high purity |
Expensive Medium sensitivity |
[30] |
Abbreviations: NSCLC: non-small-cell lung cancer; EpCAM: epithelial cell adhesion molecule.
Table 2.
Schematic representation of the main CTC label-independent isolation techniques.
| CTC Isolation Technique |
Method | Tumor Type | Clinical Objective | Major Advantages |
Major Disadvantages |
Ref. | |
|---|---|---|---|---|---|---|---|
| Label-Independent Isolation |
Filtration | Filter-based isolation and enrichment | Breast Melanoma Liver Lung Pancreatic |
Diagnosis Prognosis Treatment |
Very Fast High efficiency |
Low purity Filter clogging |
[31] |
| Microfluidics (no antibodies) |
Microscale separation of CTCs according to their dimensions and deformability | Ovarian | Diagnosis | High sensitivity High cell viability |
Small sample vol. | [32] | |
| Density gradient separation | Centrifugal separation of CTCs from blood cells based on their varying densities | Breast Gastric Pancreatic NSCLC |
Prognosis | Inexpensive Efficient process |
Low purity Loss of cells |
[33] | |
| Imaging | Utilization of a fiber optic array laser scanning system for visual identification of CTCs | Breast Prostate Liver |
Diagnosis Prognosis Treatment |
High resolution Enumeration of CTCs |
Not very precise Difficult sample processing Loss of cells |
[34] | |
| Label-Independent Isolation |
Dielectrophoresis | Detection of CTCs with application of non-uniform electric field | Breast | Prognosis | High recovery rate High efficiency High cell viability Detection accuracy |
Limited volume Low purity Very elaborate procedure |
[35] |
| Inertial focusing | CTC separation using fluid inertia at high flow rates and inertial focusing | Breast Lung |
Diagnosis Prognosis Treatment |
High cell viability High precision Speed of processes |
Deformation of cells | [36,37] |
Abbreviations: NSCLC: non-small-cell lung cancer; CTC: circulating tumor cell.
Label-dependent isolation methods rely on the use of antibodies that selectively target cell surface antigens found in circulating tumor cells (CTCs). Unlike regular blood cells, CTCs are characterized by the presence of epithelial markers, such as epithelial cell adhesion molecules (EpCAM) and cytokeratin (CK) [38,39]. Specific techniques that leverage this principle include the conjugation of antibodies to magnetic nanoparticles and the use of microfluidics [40,41]. While there is some variability in the phenotypic and functional definitions of CTCs across different studies, it is widely agreed upon that CTCs typically lack the CD45 marker and exhibit the presence of EpCAM and CK [42]. It is worth noting that the expression pattern of cytokeratin may vary among different types of cancer and often mirrors the pattern observed in tissue biopsy specimens. Furthermore, this pattern can change over time as patients undergo treatment or experience disease progression. Label-independent detection methods allow for the isolation of CTCs without relying on cell surface markers. Instead, these techniques focus on distinguishing CTCs from blood cells based on differences in their size, deformability, and various biophysical characteristics [43]. This approach is centered on discerning the unique properties of CTCs to effectively separate them from regular blood cells. CTCs have been detected in the peripheral blood of patients with different types of solid tumors [44]; indeed, there exists a substantial volume of research validating the diagnostic and prognostic significance of CTC examination in advanced breast [45], prostate [46], liver [47], gastric [48], lung [49], and colorectal [50] cancers.
As previously elucidated, the majority of cancers originate from epithelial cells, making EpCAM the most commonly used marker for CTCs. EpCAM is considered a “universal” epithelial marker for various cancer types [44,45,46,47,48,49,50]. However, the utility of EpCAM as a CTC marker is constrained. It cannot be applied to tumors that lack EpCAM expression or have low levels of expression, such as neurogenic cancers [51]. Additionally, CTCs can undergo epithelial-to-mesenchymal transition (EMT), during which epithelial markers like EpCAM are downregulated [52]. This phenomenon hampers the detection of EpCAM-positive CTCs. Hence, it is noteworthy that relying solely on the detection of EpCAM-positive CTCs likely underestimates the total CTC population and overlooks crucial biological information pertaining to EpCAM-negative CTCs, i.e., those undergoing EMT. From a methodological perspective, the challenge is compounded by the fact that many EMT-related molecules are cytoplasmic or nuclear proteins, rendering them unsuitable for use with currently available membrane-based molecular technologies for CTC detection. Therefore, single-cell CTC sequencing technologies (see beyond) may prove more beneficial for enhancing our understanding of the phenotype of EpCAM-negative CTCs and improving their isolation, enabling a more comprehensive assessment of the EMT status of CTCs at the RNA level.
In our opinion, despite the limitations posed by the heterogeneity of marker expression patterns, label-dependent techniques employing antibodies to target CTCs are the most efficient and specific means of CTC isolation. It is also important to note that label-dependent methods are widely used and firmly established in the field. In other words, the biological isolation of CTCs is a highly compelling area of study, and its potential will grow as our knowledge of tumor phenotypes continues to expand. Therefore, the current limitations of label-dependent methods for isolation are more closely related to the constraints of our oncological knowledge than to any inherent “flaw” in the method.
4. Clinical Utility of CTCs: Emergence as Multifunctional Biomarkers
As the body of evidence on the prognostic significance of CTCs continues to expand, researchers have initiated studies to explore interventions that could enhance the survival outcomes for patients facing a grim prognosis marked by elevated CTC counts or an adverse change in CTC levels. Additionally, investigations have been carried out to ascertain whether the biological insights derived from CTCs hold the potential to advance patient care. Indeed, it is crucial to give significant attention to circulating tumor cells (CTCs), viewing them not merely as progression disease (PD) endpoints, but also recognizing their role as prognostic indicators and as biomarkers for predicting and assessing responses at intermediate endpoints [53]. Various investigations have substantiated the prognostic relevance of CTC counts across diverse tumor types. These studies offer additional confirmation of the tumoral origins of CTCs [54,55,56]. In particular, CTC enumeration serves as a current prognostic marker for progression-free survival (PFS) and overall survival (OS) in breast, colorectal, and prostate cancer [57]. The utilization of CTCs as a surrogate biomarker involves establishing a minimum cutoff value to assess prognostic outcomes. However, this cutoff value varies depending on the isolation device, the protein marker employed, and the origin of the primary tumor. For instance, a retrospective analysis determined that ≥5 CTCs in 7.5 mL of blood signifies a cutoff value indicating poor prognosis for OS and PFS in metastatic breast cancer patients when an EpCAM-dependent device is used (CellSearch System® isolating CTCs by using EpCAM-based capture, fluorescent labeling, and computer-assisted identification, distinguishing them from CD45+ leukocytes) [58]. This determination led to the establishment of “BCTC-positivity” as a widely adopted cutoff value for prognostication in breast cancer [59]. A similar retrospective determination of CTC cutoff values was observed in clinical trials for metastatic prostate cancer, where the use of ≥5 CTCs as a cutoff correlated with OS [60]. In colorectal cancer (CRC), retrospective findings associated >3 CTCs with OS and PFS [61]. Although correlations between enumeration and survival rates have been established [62], determining optimal cutoff values remains a challenge, particularly for cancers positive for epithelial markers, with variations across trials [63,64,65]. Studies focusing on other cancer types encounter difficulties in defining prognostic cutoff values [66], underscoring the need for more effective CTC isolation techniques and retrospective analyses.
Beyond serving as a prognostic biomarker, CTC enumeration is employed as an exploratory indicator of efficacy and a measure of treatment response [67]. Notably, a decline in CTC counts demonstrated promise as an early efficacy endpoint in a study examining cabazitaxel response in metastatic castration-resistant prostate cancer patients with docetaxel resistance [68]. Enumeration was also evaluated as a patient stratification biomarker in the SWOG S0500 trial, where changes in CTC counts in response to therapy were used as an early indicator of therapy resistance, although this prospective use proved ineffective at extending overall survival in metastatic breast cancer patients [69]. To enhance the utility of CTCs as a biomarker, enumeration is employed as a secondary outcome measure to improve the accuracy of other prognostic markers utilized in clinical practice, such as tumor-associated protein markers (e.g., PSA, CEA, CA125) and imaging tests. A specific study revealed that combining CTC enumeration with positron emission computerized tomography (PET-CT) had greater prognostic significance than either measure alone [70]. Ensuring uniformity in isolation and characterization methods is crucial to explore the predictive value of CTCs in the clinical setting. Without uniformity, there is inconsistency in the analyzed CTC population, encompassing phenotypic variability and inconsistent capture efficiency in various cancer types, thus limiting the scope of significant findings [71]. Moreover, the identification of new markers poses technical challenges [72]. Technological advancements and extensive clinical validation are essential to understand CTCs’ role in guiding personalized medicine and drug development.
Detecting CTCs holds a critical role in cancer prognosis, influencing clinical decision-making. Prognostic assessment is pivotal for weighing the risks and benefits of proposed treatments. Extensive efforts have been directed towards unravelling the clinical significance of CTCs in prognostic estimation and their role in guiding therapeutic decisions. To illustrate and validate the prognostic, and at times diagnostic, implications of CTCs across diverse cancer types, we have identified some studies utilizing various CTC detection technologies. In most cases, as evidenced by the selected studies, patients with a heightened count of CTCs (deemed unfavorable) faced a poorer prognosis, primarily assessed through PFS and OS estimates (Table 3) [73,74,75,76,77,78,79,80,81]. The outcomes of these investigations not only clarify the tangible potential of CTC enumeration but also offer profound insights into the feasibility of using CTCs as liquid biopsies.
Table 3.
Selected CTC clinical trials on outcome measures (OS and/or PFS) after the year 2015.
| CTC Isolation Technique |
Tumor Type | Number of Patients |
Outcome Measures |
Synthetic Results |
Final Remarks |
Ref. |
|---|---|---|---|---|---|---|
| Magnetic Nanoparticles (CellSearch) |
Metastatic NENs | 138 | OS |
|
|
[73] |
| Magnetic Nanoparticles (CellSearch) |
CRC | 287 | OS and PFS |
|
|
[74] |
| Magnetic Nanoparticles (CellSearch) |
EC | 100 | OS |
|
|
[75] |
| Magnetic Nanoparticles (CellSearch) |
Breast Cancer |
3173 | OS |
|
|
[76] |
| Imaging (Epic Sciences) |
mCRPC | 161 | OS |
|
|
[77] |
| Magnetic Nanoparticles (CellSearch) |
Lung Cancer | 13 | OS and PFS |
|
|
[78] |
| Microfluidics (STEMCELL) |
CRC | 55 | OS and PFS |
|
|
[79] |
| EPISPOT STEMCELL FCM |
rHNSCC | 65 | PFS |
|
|
[80] |
| EPISPOT CellSearch |
CRC | 155 | OS and PFS |
|
|
[81] |
Abbreviations: NENs: neuroendocrine neoplasms; CRC: colorectal cancer; HR: hazard ratio; EC: esophageal cancer; CI: confidence interval; mCRPC: metastatic castration-resistant prostate cancer; AR-V7: androgen receptor splice variant 7; ARS: androgen receptor signaling; rHNSCC: metastatic head and neck squamous cell carcinoma; EGFR: epidermal growth factor; FCM: flow cytometry.
5. Characterization of CTCs: Beyond Diagnosis and Prognosis
In the realm of cancer research, the characterization of CTCs transcends conventional diagnostic and prognostic paradigms. Expanding beyond their role as biomarkers for disease presence and outcome prediction, a nuanced understanding of CTCs necessitates an exploration of their molecular and functional attributes. Unraveling the heterogeneity within the CTC population and deciphering the underlying mechanisms governing their dynamics becomes imperative. Advances in single-cell analysis techniques and high-throughput technologies have propelled investigations into the diverse phenotypic and genotypic profiles of CTCs, shedding light on their potential as indicators of therapeutic response and avenues for targeted interventions. Certainly, extending past the realms of diagnostic applications and prognostic guidance, CTCs play a pivotal role as pharmacodynamic biomarkers, gauging both inherent and acquired resistance in response to distinct treatment modalities. The molecular profiling of CTCs has exerted a discernible impact on tailoring therapeutic strategies in specific instances. Moreover, it has advanced our comprehension of the intricate mechanisms governing cancer metastasis, concurrently uncovering novel therapeutic targets amenable to intervention. Several studies in the literature suggest the potential use of CTCs as predictive markers for the selection of administered chemotherapy [82,83,84]. Moreover, studies demonstrate the potential role of CTCs combined with ctDNA as a complementary biomarker for the early indication of treatment response [85,86]. Among these, we would like to emphasize an intriguing study—a phase II clinical trial conducted by Punnoose et al. investigating erlotinib and pertuzumab in patients with advanced non-small-cell lung cancer (NSCLC). In this study, the decrease in CTC count after treatment was correlated with a longer PFS. Interestingly, patients with EGFR mutations exhibited a substantial reduction in CTC count during treatment. Mutational analysis of EGFR revealed that ctDNA had a higher sensitivity in detecting mutations compared to CTCs, and, after treatment, a decrease in mutational burden suggested a partial response to the treatment [87].
Similar to CTCs, ctDNA does possess certain limitations. Firstly, ctDNA solely facilitates the genotypic characterization of malignancy, in contrast to CTCs, which permit phenotypic analysis. Furthermore, the sensitivity of ctDNA might exhibit variations based on organ involvement. Notably, investigations into recurrent metastatic CRCs have indicated higher sensitivity in cases of hepatic metastasis compared to pulmonary metastasis [88].
The study of circulating tumor cells (CTCs), including novel single-cell techniques, can offer valuable insights into the realm of personalized therapy. In this context, we can reconcile the early characterization of tumor heterogeneity with the resolving power and informative capacity of emerging single-cell technologies. Briefly, single-cell sequencing stands as a groundbreaking approach that allows for the examination of the genetic material of individual tumor cells. This methodology provides insights into the genome, transcriptome, and other multi-omics data at the single-cell level. It is important to note that this section will not delve into the specifics of single-cell whole-genome amplification techniques (scWGA). For detailed information on certain methods such as MALBAC, eMDA, LIANTI, SISSOR, and META-CS, additional references are needed [89,90,91,92,93]. It is crucial to understand that these techniques share a commonality in that the cellular samples can originate from primary, metastatic sites or peripheral blood. Subsequently, microfluidic devices or plates are employed to individually capture isolated single cells. The DNA of these captured cells undergoes scWGA, and the resulting genomic DNA libraries are then subjected to high-throughput sequencing. The sequencing data obtained for each individual cell contain valuable information regarding gene expression, mutations, copy number variations, and other genomic features. Single-cell sequencing empowers the identification of distinct cell populations within a tumor, providing a comprehensive view of its heterogeneity. By monitoring genetic changes in individual cancer cells from CTCs, single-cell sequencing can unveil their phenotype and enable the acquisition of crucial characteristics. Through these techniques, the isolation and sequencing of CTCs have revealed the actionability of several molecular alterations, including copy number variations (CNV) and key-driver gene mutations, during the development of resistance in various cancer types, including prostate [94], gastric [95], breast [96], small-cell lung [78], and colorectal cancers [97]. The exceedingly early detection of CTCs with such characteristics could potentially enable the application of highly personalized therapy, targeting a limited number of cells, which would be theoretically more effective than treating a clinically evident disease. These are the frontiers of science where diagnostics and therapy intertwine innovatively, necessitating large-scale clinical studies for validation.
6. Conclusions and Perspectives
The presence of CTCs in peripheral blood offers a non-invasive window into the dynamic landscape of cancer progression and treatment response. This review has highlighted their multifaceted role in predicting clinical outcomes and informing prognosis across various solid tumor malignancies. As the field of oncology continues to advance, the transformative impact of CTCs as predictive and prognostic biomarkers in the management of solid tumors will become increasingly evident, offering special promises for targeted and personalized medicine. In the near future, the perspectives surrounding CTCs hold immense promise. One particularly exciting prospect is their potential to serve as indicators of residual disease, especially in the context of oligo-metastatic disease [98]. In fact, the detection and monitoring of CTCs could become a valuable tool in identifying patients at risk of disease recurrence or progression after curative aggressive treatments. This could lead to more targeted and aggressive interventions at an earlier stage, potentially improving the outcomes of oligo-metastatic patients. Furthermore, CTCs have the potential to guide treatment decisions, monitor treatment efficacy, and facilitate precision oncology. As the technologies for CTC detection and isolation continue to improve, their clinical relevance is set to grow.
In the future, research should focus on standardizing CTC detection methods, defining optimal cutoff values for different cancer types, and exploring their role in combination with other biomarkers like circulating tumor DNA (ctDNA) for a more comprehensive assessment of cancer status. Overall, CTCs are poised to play an increasingly crucial role in the diagnosis, prognosis, and treatment of solid tumors, bringing us closer to the era of personalized and precision medicine in oncology.
Acknowledgments
A.O. and M.C. thank their parents for the continuous support, love, and encouragement that have allowed them to embrace science and become free-thinking and visionary individuals.
Author Contributions
Conceptualization, A.O. and M.C.; methodology, M.C. and F.F.; software, M.C.; validation, M.S. and M.C.; formal analysis, M.C. and A.Z.; investigation, A.O. and M.S.; resources, F.F. and A.Z.; data curation, M.C.; writing—original draft preparation, M.C. and A.Z.; writing—review and editing, A.O., F.F. and M.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Non-applicable due to the nature of the study, which is not centered on presenting original data or performing new data analyses.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Siegel R.L., Miller K.D., Wagle N.S., Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17–48. doi: 10.3322/caac.21763. [DOI] [PubMed] [Google Scholar]
- 2.Tan C.R., Zhou L., El-Deiry W.S. Circulating Tumor Cells Versus Circulating Tumor DNA in Colorectal Cancer: Pros and Cons. Curr. Color. Cancer Rep. 2016;12:151–161. doi: 10.1007/s11888-016-0320-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee J., Kwak B. Simultaneous on-chip isolation and characterization of circulating tumor cell sub-populations. Biosens. Bioelectron. 2020;168:112564. doi: 10.1016/j.bios.2020.112564. [DOI] [PubMed] [Google Scholar]
- 4.Wang D., Ge C., Liang W., Yang Q., Liu Q., Ma W., Shi L., Wu H., Zhang Y., Wu Z., et al. In Vivo Enrichment and Elimination of Circulating Tumor Cells by Using a Black Phosphorus and Antibody Functionalized Intravenous Catheter. Adv. Sci. 2020;7:2000940. doi: 10.1002/advs.202000940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lim S.B., Lim C.T., Lim W.T. Single-Cell Analysis of Circulating Tumor Cells: Why Heterogeneity Matters. Cancers. 2019;11:1595. doi: 10.3390/cancers11101595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Orrapin S., Thongkumkoon P., Udomruk S., Moonmuang S., Sutthitthasakul S., Yongpitakwattana P., Pruksakorn D., Chaiyawat P. Deciphering the Biology of Circulating Tumor Cells through Single-Cell RNA Sequencing: Implications for Precision Medicine in Cancer. Int. J. Mol. Sci. 2023;24:12337. doi: 10.3390/ijms241512337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hamidi H., Ivaska J. Every step of the way: Integrins in cancer progression and metastasis. Nat. Rev. Cancer. 2018;18:533–548. doi: 10.1038/s41568-018-0038-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin D., Shen L., Luo M., Zhang K., Li J., Yang Q., Zhu F., Zhou D., Zheng S., Chen Y., et al. Circulating tumor cells: Biology and clinical significance. Signal Transduct. Target. Ther. 2021;6:404. doi: 10.1038/s41392-021-00817-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Y., Wu S., Bai F. Molecular characterization of circulating tumor cells-from bench to bedside. Semin. Cell Dev. Biol. 2018;75:88–97. doi: 10.1016/j.semcdb.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 10.Zhang X., Wei L., Li J., Zheng J., Zhang S., Zhou J. Epithelial-mesenchymal transition phenotype of circulating tumor cells is associated with distant metastasis in patients with NSCLC. Mol. Med. Rep. 2019;19:601–608. doi: 10.3892/mmr.2018.9684. [DOI] [PubMed] [Google Scholar]
- 11.Canel M., Serrels A., Frame M.C., Brunton V.G. E-cadherin-integrin crosstalk in cancer invasion and metastasis. J. Cell Sci. 2013;126:393–401. doi: 10.1242/jcs.100115. [DOI] [PubMed] [Google Scholar]
- 12.Orrapin S., Udomruk S., Lapisatepun W., Moonmuang S., Phanphaisarn A., Phinyo P., Pruksakorn D., Chaiyawat P. Clinical Implication of Circulating Tumor Cells Expressing Epithelial Mesenchymal Transition (EMT) and Cancer Stem Cell (CSC) Markers and Their Perspective in HCC: A Systematic Review. Cancers. 2022;14:3373. doi: 10.3390/cancers14143373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu M., Bardia A., Wittner B.S., Stott S.L., Smas M.E., Ting D.T., Isakoff S.J., Ciciliano J.C., Wells M.N., Shah A.M., et al. Circulating breast tumor cells exhibit dynamic changes in epithelial and mesenchymal composition. Science. 2013;339:580–584. doi: 10.1126/science.1228522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Langley R.R., Fidler I.J. The seed and soil hypothesis revisited--the role of tumor-stroma interactions in metastasis to different organs. Int. J. Cancer. 2011;128:2527–2535. doi: 10.1002/ijc.26031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schlesinger M. Role of platelets and platelet receptors in cancer metastasis. J. Hematol. Oncol. 2018;11:125. doi: 10.1186/s13045-018-0669-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang R.W., Liu Z.G., Xie Y., Wang L.X., Li M.C., Sun X. In vitro inhibition of invasion and metastasis in colon cancer cells by TanIIA. Genet. Mol. Res. 2016;15:1–7. doi: 10.4238/gmr.15039008. [DOI] [PubMed] [Google Scholar]
- 17.Wang L., Jiang G., Li X. Diterpenoid Tanshinone Attenuates the Metastasis of Non-small-cell Lung Cancer (NSCLC) Cells by Inhibiting the Cavin-1-mediated ERK/Smad2 Signaling Pathway. Anticancer Agents Med. Chem. 2023;23:1618–1625. doi: 10.2174/1871520623666230417090504. [DOI] [PubMed] [Google Scholar]
- 18.Shen Y., Ye H., Zhang D., Yang M., Ji Y., Tang L., Zhu X., Yuan L. The role of exosomal CDC6 in the hirudin-mediated suppression of the malignant phenotype of bladder cancer cells. Gene. 2022;821:146269. doi: 10.1016/j.gene.2022.146269. [DOI] [PubMed] [Google Scholar]
- 19.Fu L.Q., Du W.L., Cai M.H., Yao J.Y., Zhao Y.Y., Mou X.Z. The roles of tumor-associated macrophages in tumor angiogenesis and metastasis. Cell Immunol. 2020;353:104119. doi: 10.1016/j.cellimm.2020.104119. [DOI] [PubMed] [Google Scholar]
- 20.Dianat-Moghadam H., Azizi M., Eslami S.Z., Cortés-Hernández L.E., Heidarifard M., Nouri M., Alix-Panabières C. The Role of Circulating Tumor Cells in the Metastatic Cascade: Biology, Technical Challenges, and Clinical Relevance. Cancers. 2020;12:867. doi: 10.3390/cancers12040867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith H.A., Kang Y. The metastasis-promoting roles of tumor-associated immune cells. J. Mol. Med. 2013;91:411–429. doi: 10.1007/s00109-013-1021-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fedele M., Sgarra R., Battista S., Cerchia L., Manfioletti G. The Epithelial-Mesenchymal Transition at the Crossroads between Metabolism and Tumor Progression. Int. J. Mol. Sci. 2022;23:800. doi: 10.3390/ijms23020800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pailler E., Faugeroux V., Oulhen M., Catelain C., Farace F. Routine clinical use of circulating tumor cells for diagnosis of mutations and chromosomal rearrangements in non-small cell lung cancer-ready for prime-time? Transl. Lung Cancer Res. 2017;6:444–453. doi: 10.21037/tlcr.2017.07.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moon D.H., Lindsay D.P., Hong S., Wang A.Z. Clinical indications for, and the future of, circulating tumor cells. Adv. Drug Deliv. Rev. 2018;125:143–150. doi: 10.1016/j.addr.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 25.Zhou H., Neelakantan D., Ford H.L. Clonal cooperativity in heterogenous cancers. Semin. Cell Dev. Biol. 2017;64:79–89. doi: 10.1016/j.semcdb.2016.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen J.Y., Chang Y.C. Strategies for Isolation and Molecular Profiling of Circulating Tumor Cells. Adv. Exp. Med. Biol. 2017;994:43–66. doi: 10.1007/978-3-319-55947-6_2. [DOI] [PubMed] [Google Scholar]
- 27.Huang Q., Wang Y., Chen X., Wang Y., Li Z., Du S., Wang L., Chen S. Nanotechnology-Based Strategies for Early Cancer Diagnosis Using Circulating Tumor Cells as a Liquid Biopsy. Nanotheranostics. 2018;2:21–41. doi: 10.7150/ntno.22091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Law K.S., Huang C.E., Chen S.W. Detection of Circulating Tumor Cell-Related Markers in Gynecologic Cancer Using Microfluidic Devices: A Pilot Study. Int. J. Mol. Sci. 2023;24:2300. doi: 10.3390/ijms24032300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cho H.Y., Choi J.H., Lim J., Lee S.N., Choi J.W. Microfluidic Chip-Based Cancer Diagnosis and Prediction of Relapse by Detecting Circulating Tumor Cells and Circulating Cancer Stem Cells. Cancers. 2021;13:1385. doi: 10.3390/cancers13061385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edd J.F., Mishra A., Smith K.C., Kapur R., Maheswaran S., Haber D.A., Toner M. Isolation of circulating tumor cells. iScience. 2022;25:104696. doi: 10.1016/j.isci.2022.104696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Adams D.L., Stefansson S., Haudenschild C., Martin S.S., Charpentier M., Chumsri S., Cristofanilli M., Tang C.M., Alpaugh R.K. Cytometric characterization of circulating tumor cells captured by microfiltration and their correlation to the CellSearch(®) CTC test. Cytom. A. 2015;87:137–144. doi: 10.1002/cyto.a.22613. [DOI] [PubMed] [Google Scholar]
- 32.Parvin D., Hashemi Z.S., Shokati F., Mohammadpour Z., Bazargan V. Immunomagnetic Isolation of HER2-Positive Breast Cancer Cells Using a Microfluidic Device. ACS Omega. 2023;8:21745–21754. doi: 10.1021/acsomega.3c01287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lapin M., Tjensvoll K., Oltedal S., Buhl T., Gilje B., Smaaland R., Nordgård O. MINDEC-An Enhanced Negative Depletion Strategy for Circulating Tumour Cell Enrichment. Sci. Rep. 2016;6:28929. doi: 10.1038/srep28929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vidlarova M., Rehulkova A., Stejskal P., Prokopova A., Slavik H., Hajduch M., Srovnal J. Recent Advances in Methods for Circulating Tumor Cell Detection. Int. J. Mol. Sci. 2023;24:3902. doi: 10.3390/ijms24043902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Balasubramanian P., Kinders R.J., Kummar S., Gupta V., Hasegawa D., Menachery A., Lawrence S.M., Wang L., Ferry-Galow K., Davis D., et al. Antibody-independent capture of circulating tumor cells of non-epithelial origin with the ApoStream® system. PLoS ONE. 2017;12:e0175414. doi: 10.1371/journal.pone.0175414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mohamadsharifi A., Hajghassem H., Kalantar M., Karimi A., Tabatabaei Asl M., Hosseini S., Badieirostami M. High-Efficiency Inertial Separation of Microparticles Using Elevated Columned Reservoirs and Vortex Technique for Lab-on-a-Chip Applications. ACS Omega. 2023;8:28628–28639. doi: 10.1021/acsomega.3c03136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee Y., Guan G., Bhagat A.A. ClearCell® FX, a label-free microfluidics technology for enrichment of viable circulating tumor cells. Cytom. A. 2018;93:1251–1254. doi: 10.1002/cyto.a.23507. [DOI] [PubMed] [Google Scholar]
- 38.Houvast R.D., Badr N., March T., de Muynck L.D.A.N., Sier V.Q., Schomann T., Bhairosingh S., Baart V.M., Peeters J.A.H.M., van Westen G.J.P., et al. Preclinical evaluation of EpCAM-binding designed ankyrin repeat proteins (DARPins) as targeting moieties for bimodal near-infrared fluorescence and photoacoustic imaging of cancer. Eur. J. Nucl. Med. Mol. Imaging. 2023. epub ahead of print . [DOI] [PMC free article] [PubMed]
- 39.Bulfoni M., Turetta M., Del Ben F., Di Loreto C., Beltrami A.P., Cesselli D. Dissecting the Heterogeneity of Circulating Tumor Cells in Metastatic Breast Cancer: Going Far Beyond the Needle in the Haystack. Int. J. Mol. Sci. 2016;17:1775. doi: 10.3390/ijms17101775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Martel A., Mograbi B., Romeo B., Gastaud L., Lalvee S., Zahaf K., Fayada J., Nahon-Esteve S., Bonnetaud C., Salah M., et al. Assessment of Different Circulating Tumor Cell Platforms for Uveal Melanoma: Potential Impact for Future Routine Clinical Practice. Int. J. Mol. Sci. 2023;24:11075. doi: 10.3390/ijms241311075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yeo D., Kao S., Gupta R., Wahlroos S., Bastian A., Strauss H., Klemm V., Shrestha P., Ramirez A.B., Costandy L., et al. Accurate isolation and detection of circulating tumor cells using enrichment-free multiparametric high resolution imaging. Front. Oncol. 2023;13:1141228. doi: 10.3389/fonc.2023.1141228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ning Y., Hanna D.L., Zhang W., Mendez A., Yang D., El-Khoueiry R., Matsusaka S., Sunakawa Y., Stremitzer S., Parekh A., et al. Cytokeratin-20 and Survivin-Expressing Circulating Tumor Cells Predict Survival in Metastatic Colorectal Cancer Patients by a Combined Immunomagnetic qRT-PCR Approach. Mol. Cancer Ther. 2015;14:2401–2408. doi: 10.1158/1535-7163.MCT-15-0359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gabriel M.T., Calleja L.R., Chalopin A., Ory B., Heymann D. Circulating Tumor Cells: A Review of Non-EpCAM-Based Approaches for Cell Enrichment and Isolation. Clin. Chem. 2016;62:571–581. doi: 10.1373/clinchem.2015.249706. [DOI] [PubMed] [Google Scholar]
- 44.Habli Z., AlChamaa W., Saab R., Kadara H., Khraiche M.L. Circulating Tumor Cell Detection Technologies and Clinical Utility: Challenges and Opportunities. Cancers. 2020;12:1930. doi: 10.3390/cancers12071930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Harigopal M., Kowalski D., Vosoughi A. Enumeration and molecular characterization of circulating tumor cells as an innovative tool for companion diagnostics in breast cancer. Expert. Rev. Mol. Diagn. 2020;20:815–828. doi: 10.1080/14737159.2020.1784009. [DOI] [PubMed] [Google Scholar]
- 46.Cieślikowski W.A., Antczak A., Nowicki M., Zabel M., Budna-Tukan J. Clinical Relevance of Circulating Tumor Cells in Prostate Cancer Management. Biomedicines. 2021;9:1179. doi: 10.3390/biomedicines9091179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ahn J.C., Teng P.C., Chen P.J., Posadas E., Tseng H.R., Lu S.C., Yang J.D. Detection of Circulating Tumor Cells and Their Implications as a Biomarker for Diagnosis, Prognostication, and Therapeutic Monitoring in Hepatocellular Carcinoma. Hepatology. 2021;73:422–436. doi: 10.1002/hep.31165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thanh Huong P., Gurshaney S., Thanh Binh N., Gia Pham A., Hoang Nguyen H., Thanh Nguyen X., Pham-The H., Tran P.T., Truong Vu K., Xuan Duong N., et al. Emerging Role of Circulating Tumor Cells in Gastric Cancer. Cancers. 2020;12:695. doi: 10.3390/cancers12030695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Maly V., Maly O., Kolostova K., Bobek V. Circulating Tumor Cells in Diagnosis and Treatment of Lung Cancer. In Vivo. 2019;33:1027–1037. doi: 10.21873/invivo.11571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yu H., Ma L., Zhu Y., Li W., Ding L., Gao H. Significant diagnostic value of circulating tumour cells in colorectal cancer. Oncol. Lett. 2020;20:317–325. doi: 10.3892/ol.2020.11537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rodriguez E.F., Jones R., Miller D., Rodriguez F.J. Neurogenic Tumors of the Mediastinum. Semin. Diagn. Pathol. 2020;37:179–186. doi: 10.1053/j.semdp.2020.04.004. [DOI] [PubMed] [Google Scholar]
- 52.Brown M.S., Muller K.E., Pattabiraman D.R. Quantifying the Epithelial-to-Mesenchymal Transition (EMT) from Bench to Bedside. Cancers. 2022;14:1138. doi: 10.3390/cancers14051138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu S., Zhao S., Cui D., Xie J. Advances in the Biology, Detection Techniques, and Clinical Applications of Circulating Tumor Cells. J. Oncol. 2022;2022:7149686. doi: 10.1155/2022/7149686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Muchlińska A., Wenta R., Ścińska W., Markiewicz A., Suchodolska G., Senkus E., Żaczek A.J., Bednarz-Knoll N. Improved Characterization of Circulating Tumor Cells and Cancer-Associated Fibroblasts in One-Tube Assay in Breast Cancer Patients Using Imaging Flow Cytometry. Cancers. 2023;15:4169. doi: 10.3390/cancers15164169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yu J., Bai Y., Jin L., Zhang Z., Yang Y. A Prospective Long-Term Follow-Up Study: The Application of Circulating Tumor Cells Analysis to Guide Adjuvant Therapy in Stage II Colorectal Cancer. Ann. Surg. Oncol. 2023;30:8495–8500. doi: 10.1245/s10434-023-14168-x. [DOI] [PubMed] [Google Scholar]
- 56.Trujillo B., Wu A., Wetterskog D., Attard G. Blood-based liquid biopsies for prostate cancer: Clinical opportunities and challenges. Br. J. Cancer. 2022;127:1394–1402. doi: 10.1038/s41416-022-01881-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fischer C., Turchinovich A., Feisst M., Riedel F., Haßdenteufel K., Scharli P., Hartkopf A.D., Brucker S.Y., Michel L., Burwinkel B., et al. Circulating miR-200 Family and CTCs in Metastatic Breast Cancer before, during, and after a New Line of Systemic Treatment. Int. J. Mol. Sci. 2022;23:9535. doi: 10.3390/ijms23179535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cristofanilli M., Budd G.T., Ellis M.J., Stopeck A., Matera J., Miller M.C., Reuben J.M., Doyle G.V., Allard W.J., Terstappen L.W., et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N. Engl. J. Med. 2004;351:781–791. doi: 10.1056/NEJMoa040766. [DOI] [PubMed] [Google Scholar]
- 59.Helissey C., Berger F., Cottu P., Diéras V., Mignot L., Servois V., Bouleuc C., Asselain B., Pelissier S., Vaucher I., et al. Circulating tumor cell thresholds and survival scores in advanced metastatic breast cancer: The observational step of the CirCe01 phase III trial. Cancer Lett. 2015;360:213–218. doi: 10.1016/j.canlet.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 60.Isebia K.T., Dathathri E., Verschoor N., Nanou A., De Jong A.C., Coumans F.A.W., Terstappen L.W.M.M., Kraan J., Martens J.W.M., Bansal R., et al. Characterizing Circulating Tumor Cells and Tumor-Derived Extracellular Vesicles in Metastatic Castration-Naive and Castration-Resistant Prostate Cancer Patients. Cancers. 2022;14:4404. doi: 10.3390/cancers14184404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kahounová Z., Pícková M., Drápela S., Bouchal J., Szczyrbová E., Navrátil J., Souček K. Circulating tumor cell-derived preclinical models: Current status and future perspectives. Cell Death Dis. 2023;14:530. doi: 10.1038/s41419-023-06059-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Paoletti C., Hayes D.F. Circulating Tumor Cells. Adv. Exp. Med. Biol. 2016;882:235–258. doi: 10.1007/978-3-319-22909-6_10. [DOI] [PubMed] [Google Scholar]
- 63.Agerbæk M.Ø., Bang-Christensen S.R., Yang M.H., Clausen T.M., Pereira M.A., Sharma S., Ditlev S.B., Nielsen M.A., Choudhary S., Gustavsson T., et al. The VAR2CSA malaria protein efficiently retrieves circulating tumor cells in an EpCAM-independent manner. Nat. Commun. 2018;9:3279. doi: 10.1038/s41467-018-05793-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bang-Christensen S.R., Pedersen R.S., Pereira M.A., Clausen T.M., Løppke C., Sand N.T., Ahrens T.D., Jørgensen A.M., Lim Y.C., Goksøyr L., et al. Capture and Detection of Circulating Glioma Cells Using the Recombinant VAR2CSA Malaria Protein. Cells. 2019;8:998. doi: 10.3390/cells8090998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Eslami S.Z., Cortés-Hernández L.E., Alix-Panabières C. Epithelial Cell Adhesion Molecule: An Anchor to Isolate Clinically Relevant Circulating Tumor Cells. Cells. 2020;9:1836. doi: 10.3390/cells9081836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Flaig T.W., Wilson S., van Bokhoven A., Varella-Garcia M., Wolfe P., Maroni P., Genova E.E., Morales D., Lucia M.S. Detection of circulating tumor cells in metastatic and clinically localized urothelial carcinoma. Urology. 2011;78:863–867. doi: 10.1016/j.urology.2011.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eigl B.J., Chi K., Tu D., Hotte S.J., Winquist E., Booth C.M., Canil C., Potvin K., Gregg R., North S., et al. A randomized phase II study of pelareorep and docetaxel or docetaxel alone in men with metastatic castration resistant prostate cancer: CCTG study IND 209. Oncotarget. 2018;9:8155–8164. doi: 10.18632/oncotarget.24263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Anido U., Fita M.J.J., Munielo-Romay L., Pérez-Valderrama B., Mellado B., de Olza M.O., Calvo O.F., Castellano D., Parra E.M.F., Domenec M., et al. Phase II study of weekly cabazitaxel for ‘unfit’ metastatic castration resistant prostate cancer patients (mCRPC) progressing after docetaxel (D) treatment. Circulating tumour cell (CTC) analysis (SOGUGCABASEM Trial) Ann. Oncol. 2016;27((Suppl. S6)):753. doi: 10.1093/annonc/mdw372.37. [DOI] [Google Scholar]
- 69.Smerage J.B., Barlow W.E., Hortobagyi G.N., Winer E.P., Leyland-Jones B., Srkalovic G., Tejwani S., Schott A.F., O’Rourke M.A., Lew D.L., et al. Circulating tumor cells and response to chemotherapy in metastatic breast cancer: SWOG S0500. J. Clin. Oncol. 2014;32:3483–3489. doi: 10.1200/JCO.2014.56.2561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kim J.E., Chae S.Y., Kim J.H., Kim H.J., Kim T.W., Kim K.P., Kim S.Y., Lee J.L., Oh S.J., Kim J.S., et al. 3′-Deoxy-3′-18F-Fluorothymidine and 18F-Fluorodeoxyglucose positron emission tomography for the early prediction of response to Regorafenib in patients with metastatic colorectal cancer refractory to all standard therapies. Eur. J. Nucl. Med. Mol. Imaging. 2019;46:1713–1722. doi: 10.1007/s00259-019-04330-7. [DOI] [PubMed] [Google Scholar]
- 71.Visal T.H., den Hollander P., Cristofanilli M., Mani S.A. Circulating tumour cells in the -omics era: How far are we from achieving the ‘singularity’? Br. J. Cancer. 2022;127:173–184. doi: 10.1038/s41416-022-01768-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wang D., Wu L., Liu X. Glycan Markers as Potential Immunological Targets in Circulating Tumor Cells. Adv. Exp. Med. Biol. 2017;994:275–284. doi: 10.1007/978-3-319-55947-6_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Khan M.S., Kirkwood A.A., Tsigani T., Lowe H., Goldstein R., Hartley J.A., Caplin M.E., Meyer T. Early Changes in Circulating Tumor Cells Are Associated with Response and Survival Following Treatment of Metastatic Neuroendocrine Neoplasms. Clin. Cancer Res. 2016;22:79–85. doi: 10.1158/1078-0432.CCR-15-1008. [DOI] [PubMed] [Google Scholar]
- 74.Bork U., Rahbari N.N., Schölch S., Reissfelder C., Kahlert C., Büchler M.W., Weitz J., Koch M. Circulating tumour cells and outcome in non-metastatic colorectal cancer: A prospective study. Br. J. Cancer. 2015;112:1306–1313. doi: 10.1038/bjc.2015.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Reeh M., Effenberger K.E., Koenig A.M., Riethdorf S., Eichstädt D., Vettorazzi E., Uzunoglu F.G., Vashist Y.K., Izbicki J.R., Pantel K., et al. Circulating Tumor Cells as a Biomarker for Preoperative Prognostic Staging in Patients with Esophageal Cancer. Ann. Surg. 2015;261:1124–1130. doi: 10.1097/SLA.0000000000001130. [DOI] [PubMed] [Google Scholar]
- 76.Janni W.J., Rack B., Terstappen L.W., Pierga J.Y., Taran F.A., Fehm T., Hall C., de Groot M.R., Bidard F.C., Friedl T.W., et al. Pooled Analysis of the Prognostic Relevance of Circulating Tumor Cells in Primary Breast Cancer. Clin. Cancer Res. 2016;22:2583–2593. doi: 10.1158/1078-0432.CCR-15-1603. [DOI] [PubMed] [Google Scholar]
- 77.Scher H.I., Lu D., Schreiber N.A., Louw J., Graf R.P., Vargas H.A., Johnson A., Jendrisak A., Bambury R., Danila D., et al. Association of AR-V7 on Circulating Tumor Cells as a Treatment-Specific Biomarker With Outcomes and Survival in Castration-Resistant Prostate Cancer. JAMA Oncol. 2016;2:1441–1449. doi: 10.1001/jamaoncol.2016.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Carter L., Rothwell D.G., Mesquita B., Smowton C., Leong H.S., Fernandez-Gutierrez F., Li Y., Burt D.J., Antonello J., Morrow C.J., et al. Molecular analysis of circulating tumor cells identifies distinct copy-number profiles in patients with chemosensitive and chemorefractory small-cell lung cancer. Nat. Med. 2017;23:114–119. doi: 10.1038/nm.4239. [DOI] [PubMed] [Google Scholar]
- 79.Chou W.C., Wu M.H., Chang P.H., Hsu H.C., Chang G.J., Huang W.K., Wu C.E., Hsieh J.C. A Prognostic Model Based on Circulating Tumour Cells is Useful for Identifying the Poorest Survival Outcome in Patients with Metastatic Colorectal Cancer. Int. J. Biol. Sci. 2018;14:137–146. doi: 10.7150/ijbs.23182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Garrel R., Mazel M., Perriard F., Vinches M., Cayrefourcq L., Guigay J., Digue L., Aubry K., Alfonsi M., Delord J.P., et al. Circulating Tumor Cells as a Prognostic Factor in Recurrent or Metastatic Head and Neck Squamous Cell Carcinoma: The CIRCUTEC Prospective Study. Clin. Chem. 2019;65:1267–1275. doi: 10.1373/clinchem.2019.305904. [DOI] [PubMed] [Google Scholar]
- 81.Mazard T., Cayrefourcq L., Perriard F., Senellart H., Linot B., de la Fouchardière C., Terrebonne E., François E., Obled S., Guimbaud R., et al. Clinical Relevance of Viable Circulating Tumor Cells in Patients with Metastatic Colorectal Cancer: The COLOSPOT Prospective Study. Cancers. 2021;13:2966. doi: 10.3390/cancers13122966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lin X., Bo Z.H., Lv W., Zhou Z., Huang Q., Du W., Shan X., Fu R., Jin X., Yang H., et al. Miniaturized microfluidic-based nucleic acid analyzer to identify new biomarkers of biopsy lung cancer samples for subtyping. Front. Chem. 2022;10:946157. doi: 10.3389/fchem.2022.946157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mitchell M.I., Ma J., Carter C.L., Loudig O. Circulating Exosome Cargoes Contain Functionally Diverse Cancer Biomarkers: From Biogenesis and Function to Purification and Potential Translational Utility. Cancers. 2022;14:3350. doi: 10.3390/cancers14143350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sarioglu A.F., Aceto N., Kojic N., Donaldson M.C., Zeinali M., Hamza B., Engstrom A., Zhu H., Sundaresan T.K., Miyamoto D.T., et al. A microfluidic device for label-free, physical capture of circulating tumor cell clusters. Nat. Methods. 2015;12:685–691. doi: 10.1038/nmeth.3404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Radovich M., Jiang G., Hancock B.A., Chitambar C., Nanda R., Falkson C., Lynce F.C., Gallagher C., Isaacs C., Blaya M., et al. Association of Circulating Tumor DNA and Circulating Tumor Cells After Neoadjuvant Chemotherapy With Disease Recurrence in Patients with Triple-Negative Breast Cancer: Preplanned Secondary Analysis of the BRE12-158 Randomized Clinical Trial. JAMA Oncol. 2020;6:1410–1415. doi: 10.1001/jamaoncol.2020.2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Batth I.S., Mitra A., Manier S., Ghobrial I.M., Menter D., Kopetz S., Li S. Circulating tumor markers: Harmonizing the yin and yang of CTCs and ctDNA for precision medicine. Ann. Oncol. 2017;28:468–477. doi: 10.1093/annonc/mdw619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Punnoose E.A., Atwal S., Liu W., Raja R., Fine B.M., Hughes B.G., Hicks R.J., Hampton G.M., Amler L.C., Pirzkall A., et al. Evaluation of circulating tumor cells and circulating tumor DNA in non-small cell lung cancer: Association with clinical endpoints in a phase II clinical trial of pertuzumab and erlotinib. Clin. Cancer Res. 2012;18:2391–2401. doi: 10.1158/1078-0432.CCR-11-3148. [DOI] [PubMed] [Google Scholar]
- 88.Fabisiewicz A., Szostakowska-Rodzos M., Zaczek A.J., Grzybowska E.A. Circulating Tumor Cells in Early and Advanced Breast Cancer; Biology and Prognostic Value. Int. J. Mol. Sci. 2020;21:1671. doi: 10.3390/ijms21051671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chen C., Xing D., Tan L., Li H., Zhou G., Huang L., Xie X.S. Single-cell whole-genome analyses by Linear Amplification via Transposon Insertion (LIANTI) Science. 2017;356:189–194. doi: 10.1126/science.aak9787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chu W.K., Edge P., Lee H.S., Bansal V., Bafna V., Huang X., Zhang K. Ultraaccurate genome sequencing and haplotyping of single human cells. Proc. Natl. Acad. Sci. USA. 2017;114:12512–12517. doi: 10.1073/pnas.1707609114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fu Y., Li C., Lu S., Zhou W., Tang F., Xie X.S., Huang Y. Uniform and accurate single-cell sequencing based on emulsion whole-genome amplification. Proc. Natl. Acad. Sci. USA. 2015;112:11923–11928. doi: 10.1073/pnas.1513988112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Xing D., Tan L., Chang C.H., Li H., Xie X.S. Accurate SNV detection in single cells by transposon-based whole-genome amplification of complementary strands. Proc. Natl. Acad. Sci. USA. 2021;118:e2013106118. doi: 10.1073/pnas.2013106118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zong C., Lu S., Chapman A.R., Xie X.S. Genome-wide detection of single-nucleotide and copy-number variations of a single human cell. Science. 2012;338:1622–1626. doi: 10.1126/science.1229164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gao Y., Ni X., Guo H., Su Z., Ba Y., Tong Z., Guo Z., Yao X., Chen X., Yin J., et al. Single-cell sequencing deciphers a convergent evolution of copy number alterations from primary to circulating tumor cells. Genome Res. 2017;27:1312–1322. doi: 10.1101/gr.216788.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mishima Y., Matsusaka S., Chin K., Mikuniya M., Minowa S., Takayama T., Shibata H., Kuniyoshi R., Ogura M., Terui Y., et al. Detection of HER2 Amplification in Circulating Tumor Cells of HER2-Negative Gastric Cancer Patients. Target. Oncol. 2017;12:341–351. doi: 10.1007/s11523-017-0493-6. [DOI] [PubMed] [Google Scholar]
- 96.Jacot W., Cottu P., Berger F., Dubot C., Venat-Bouvet L., Lortholary A., Bourgeois H., Bollet M., Servent V., Luporsi E., et al. Actionability of HER2-amplified circulating tumor cells in HER2-negative metastatic breast cancer: The CirCe T-DM1 trial. Breast Cancer Res. 2019;21:121. doi: 10.1186/s13058-019-1215-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pan X., Zhang X. Utility of circulating tumor cells and DNA in the management of advanced colorectal cancer. Future Oncol. 2020;16:1289–1299. doi: 10.2217/fon-2020-0073. [DOI] [PubMed] [Google Scholar]
- 98.Ottaiano A., Santorsola M., Circelli L., Trotta A.M., Izzo F., Perri F., Cascella M., Sabbatino F., Granata V., Correra M., et al. Oligo-Metastatic Cancers: Putative Biomarkers, Emerging Challenges and New Perspectives. Cancers. 2023;15:1827. doi: 10.3390/cancers15061827. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Non-applicable due to the nature of the study, which is not centered on presenting original data or performing new data analyses.