Abstract
The birth and delivery plan is the center of clinical communication between the pregnant woman and the midwife, which is in the scope of health care services and is designed and provided to specialists with the participation of the woman and her husband during pregnancy. This document reflects the preferences, expectations, and fears of pregnant women regarding the birth process. This study was conducted with the aim of determining the maternal and neonatal outcomes of the birth plan: a review study. In this review study, Persian databases Magiran, SID, and English databases Pubmed, Scopus, SID Elsevier, Web of Sciences, and Google Scholar search engine using English keywords including Maternal outcome, neonatal outcome, birth schedule, delivery plan, birth plan, and their Persian equivalents were searched from 2000 to 2022. Numerous studies were selected and analyzed in a quantitative and qualitative manner that was related to the purpose of the present study in terms of content. Among 948 articles, 13 of the most relevant ones were selected and analyzed for this study. The results of the review of the studies showed that the birth plan has an effect on women's empowerment, satisfaction with childbirth, positive experience of childbirth, cesarean section rate, epidural use rate, episiotomy rate, Apgar, and umbilical cord pH of the newborn. The maternal and neonatal consequences of the birth plan prevail over its negative consequences, and the use of the birth plan can increase women's empowerment, satisfaction with childbirth, positive experience of childbirth, and reduce the rate of cesarean section and negative maternal-neonatal consequences.
Keywords: Birth plan, delivery plan, maternal outcome, neonatal outcome
Introduction
The concept of birth and delivery plan was invented by Kitzinger (1980) in the United States.[1] This program was used in European and American countries in response to the increasing medicalization of childbirth and the need for childbirth with the least medical intervention.[2] In 1993, in England, a birth plan was used in 78% of delivery rooms. The start of this program in Spain was in 2007.[3] Natural childbirth care strategy is mentioned in the national health system and natural birth plan, and since February 2013, the Ministry of Health published policies related to childbirth and birth plan.[4] A birth and delivery plan is a written legal document in which a pregnant woman, after receiving information about pregnancy, delivery method, and postpartum care, requests participation in handling all her personal needs.[5] In fact, the birth and delivery plan is the center of the clinical communication between the pregnant woman and the midwife, which is in the scope of health care services and is designed and provided to specialists with the participation of the woman and her husband during pregnancy.[2] This document reflects the preferences, expectations, and fears of pregnant women regarding the birth process. The birth plan facilitates women's communication with service providers, improves the satisfaction of pregnant women, and strengthens their participation and decision-making in the delivery process.[5,6,7]
This plan gives the opportunity to express women's expectations, preferences, and needs regarding the birthing process, and ultimately increases women's participation, sense of control over the birthing process increases women's satisfaction and the pleasant experience of the birthing process, desires and deepens of trusting and respectful relationships between women and health service providers and empowers pregnant women.[5,6,7] Also, according to the studies conducted by researchers, the birth plan can have positive effects on fetal, and maternal outcomes and women's empowerment. In this regard, studies have shown that with increasing compliance with the birth plan, the rate of cesarean section decreases, and the results of Apgar and umbilical cord pH improve. They also stated that the birth plan can be an effective tool to support the natural and physiological birth process, better communication with specialists, more control of pregnant women over the birth process, better results for women and childbirth, and more satisfaction.[8,9,10] According to the mentioned cases, the researchers decided to conduct a study with the aim of determining the maternal-infant outcomes of the birth plan: a narrative review study.
Materials and Methods
Study design and setting
The present study was a narrative review study that was conducted with the aim of determining the maternal and neonatal outcomes of the birth plan.
Study participants and sampling
Examples of this study are all articles published in Persian and English journals, abstracts of congresses and conferences, books, theses, and reference sites. The articles were extracted from the Persian databases Magiran, SID, and English databases PubMed, Scopus, SID, Web Of Sciences, and Google Scholar search engine.
Data collection tool and technique
In order to access all the desired Persian and English articles from the Persian keywords and their English equivalents Birth and plan, delivery and plan, birth plan or delivery plan, Maternal and outcomes, Neonatal and outcomes, Maternal outcomes or Neonatal outcomes Women and empowerment, women and Participation and a combination of these keywords in the databases mentioned in the range were searched in the period of 2000-2022. The search period started on June 1, 2022, and lasted until July 31, 2022.
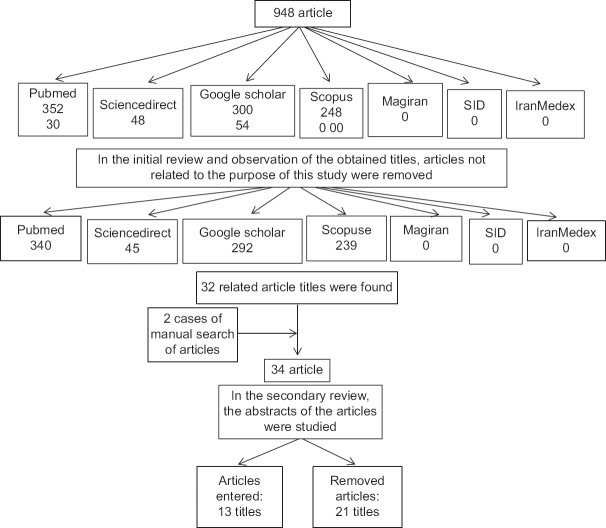
Searching databases with high sensitivity (High Sensitive Searching) was done by a researcher and a senior expert in the field of searching databases. In the beginning, the titles of the articles that were searched by the research team with the mentioned keywords were 948 titles. To avoid bias, the search was conducted by two researchers independently, then similar and repeated searches were excluded from the study. A checklist was designed based on the objectives and by studying other available sources. Then the abstracts of the collected articles were studied and the articles that did not have the required information according to the checklist were excluded from the study. Based on the search strategy and keywords, a list of all the articles reviewed in the mentioned databases was prepared. The titles of the searched articles were reviewed and articles with duplicate titles were removed. Then, the title and abstract of the remaining articles were examined and the articles not related to the present study were discarded. In the next step, the full text of the remaining articles was examined using the STROBE checklist. Finally, the articles that received the maximum quality evaluation score were included in the present study. All the mentioned steps were done by two independent researchers in order to avoid bias. If there was a difference of opinion between the two researchers, the article was reviewed by a third person. The purpose of the STROBE checklist was to provide recommendations to clarify the design, implementation method, and findings of observational studies. This checklist has 6 general sections, title and abstract, introduction, methods, results, discussion, and other information. The number of cases are divided into other sub-categories and in total this statement has 22 clauses. Out of 22 items, 18 items are generally used in all types of observational studies, including cohort, case-control, and cross-sectional studies. 4 cases are also considered specialized according to the type of study. In this checklist, it evaluates different aspects of methodology, including sampling methods, measuring variables, statistical analysis, and adjustment of confounders, mentioning the validity and reliability of the instrument used, and the objectives of the study. Each part of the checklist was given two points, and at the end, the total points obtained by the articles were compared by two researchers. The minimum obtainable score was 15.5. The articles that received the quorum of the quality evaluation score were included in the study.
In the beginning, 948 articles were found, and finally, 34 articles were fully reviewed, and after checking the entry and exit criteria and quality assessment, 17 related articles were included in the study and were reviewed [Figure 1]. The inclusion criteria of the articles were: articles published in Farsi or English, articles whose content was the investigation of maternal and newborn consequences of the birth plan, articles that have been refereed. Therefore, the texts that were in the form of letters to the editor, summaries of articles, and articles presented at conferences were excluded from the study.
Figure 1.
Number of reviewed articles after checking in different databases
Ethical consideration
In this review study, the reviewed studies were used to write a reproductive health doctorate proposal with approved code IR.MUI.NUREMA.REC.1400.064. The utmost care was taken in mentioning the results of the studied studies.
Results
Finally, 13 studies were eligible for meta-analysis [Figure 1]. The results of the reviewed studies are summarized in Table 1. In general, the results of various studies showed that the birth plan can be effective in giving birth satisfaction and empowering women. It can also cause positive consequences on childbirth and the baby, but in a few studies, the results showed the adverse effect of the birth plan on the baby.
Table 1.
Characteristics of the reviewed studies
| No | Author | Type of research | The purpose of the research | Number of samples | Research tool | Result |
|---|---|---|---|---|---|---|
| 1 | Hidalgo-Lopezosa (2021)[11] | Multicenter and retrospective case-control | Determining the association between birth plan use and maternal and neonatal outcomes in southern Spain: a case-control study | 457 pregnant women | Birth plan, questionnaire to check demographic characteristics and maternal and newborn outcomes | Birth programs were associated with less intervention, a more natural birth process, and better outcomes for mothers and babies. Birth plans can improve the well-being of mother and baby and lead to a more natural birth. |
| 2 | Hidalgo-Lopezosa (2017)[8] | Retrospective, descriptive and analytical | Adherence to the birth schedule and its relationship with maternal and newborn outcomes | 178 pregnant women | Birth plan, questionnaire to check demographic characteristics and maternal and newborn outcomes | A birth plan can be an effective tool to achieve better outcomes for the mother and her child. |
| 3 | Farahat (2015)[9] | semi experimental | The effect of implementing a birth plan on women’s childbirth experiences and maternal and neonatal outcomes | 260 pregnant women | Demographic questionnaire, birth expectation fulfillment questionnaire and birth satisfaction data, semi-structured interview with nurse and doctor, observation checklist to evaluate mother and baby outcomes. | Women who receive birth planning care during childbirth are more satisfied than women who do not receive the necessary care. |
| 4 | López-Gimeno (2021)[12] | Descriptive multicenter retrospective | Presentation of birth plan to hospitals and its relationship with midwifery results and selected methods of pain relief during childbirth | 432 pregnant women | Birth plan, demographic profile questionnaire and observation checklist | Mothers with a birth plan were more likely to initiate breastfeeding in the delivery room. Epidural analgesia was the most commonly used method for pain relief, and women who presented with a birth plan tended to use more concurrent non-pharmacological methods. |
| 5 | Ahmadpour (2020)[13] | Qualitative | Evaluation of birth program implementation: a parallel convergent mixed study | 106 pregnant women | Obstetric history review questionnaire, birth plan checklist, childbirth experience questionnaire, Edinburgh postpartum depression scale, partogram, childbirth fear scale, PTSD symptoms scale, maternal-fetal outcome evaluation checklist | The importance of birth planning stems from the principle of respect for biology and independence, and as a result, increases women’s control over the birth process and their satisfaction. Also, due to providing information and creating awareness and communication with women, it can reduce their fear and create positive feedback for women. The birth plan facilitates communication with obstetricians and gynecologists and increases women’s satisfaction with the birth process and increases participation in the decision-making process for childbirth. |
| 6 | Soliman Abdelalim (2020)[10] | Intervention | The effect of implementation of the birth plan on childbirth outcomes and women’s empowerment | 194 pregnant women | Birth plan implementation questionnaire, childbirth results questionnaire, empowerment scale related to childbirth | The birth program leads to a higher implementation of maternity care, it has a positive effect on maternal and fetal outcomes, and in total, women’s empowerment scores increased significantly after the implementation of the birth and delivery program compared to the control group. |
| 7 | Davis (2019)[14] | A prospective, non-randomized controlled trial | The effect of the birth plan on the outcomes of mother and baby delivery | Birth plan, maternal and newborn outcome assessment checklist | A delivery schedule was associated with a significant increase in metabolic acidemia indices in infants. A longer delivery schedule was also associated with a significantly higher rate of cesarean delivery. | |
| 8 | Hidalgo-Lopezosa (2013)[15] | Retrospective case-control | Are birth plans associated with improved maternal or neonatal outcomes? | 182 pregnant women | Birth plan, maternal and newborn outcome assessment checklist | Birth plans may be beneficial and not associated with any adverse obstetric or neonatal outcomes. Mothers who have birth plans and their babies have at least as good outcomes as those who do not. Infants of primiparous women with planned delivery had better umbilical cord blood pH values than those of primiparous women without planned delivery. |
| 9 | Hadar (2013)[16] | Retrospect | Obstetric outcomes in women with self-planned birth plans | All women with birth plans | Birth plan, maternal outcome assessment checklist | Compared to the control group matched for age, fertility and gestational week, women who present with a birth plan are less likely to undergo cesarean section, have a higher probability of first and second degree perineal tears, and are more likely to use an epidural. |
| 10 | Deering (2007)[17] | Evidence case | Patients presenting with delivery plans: a case-control study of delivery outcomes | 128 pregnant women | Birth plan, maternal outcome assessment checklist | Compared with age- and parity-matched controls, patients with birth plans did not have an increased incidence of episiotomy or caesarean section, but were less likely to receive an epidural during labor. |
| 11 | Medeiros (2019)[18] | Review | Determining the consequences of using the birth plan in the birth process | 13 articles | Integrated literature review in LILACS, PUBMED, CINAHL and SciELO, in the period from 2008 to 2018 | The birth plan increases the mother’s satisfaction with childbirth. There are still challenges related to using this program. |
| 12 | Alba-Rodríguez (2022)[19] | Qualitative | The birth program experience - a pilot qualitative study in southern Spain | 7 contributors | interview | Women find it helpful to be offered a birth plan because it informs them about the birth process and gives them the opportunity to have a better birth experience. |
| 13 | Mirghafourvand (2019)[20] | Review | The impact of birth plans on the birth experience: a systematic review | 3 clinical trial articles | Cochrane Library, Web of Science, MEDLINE, Embase, CINAHL, Scopus, PsycINFO, ACP Journal Club, Google Scholar and Persian databases (SID, Magiran and Barakat) until February 10, 2018 | There is insufficient evidence to support or refute that birth planning can improve the birth experience or birth satisfaction. |
| 14 | Jolles (2019)[21] | Retrospect | Prevalence, characteristics and women’s satisfaction with birth planning in the Netherlands | 1159 | Birth plan, demographic profile survey questionnaire | Although birth plans are recommended for every pregnant woman, it is still not a routine practice. Therefore, the purpose of birth plans, to facilitate shared decision-making, is not fully realized. Implementation strategies are needed to increase the acceptance of birth plans for every woman. |
| 15 | Afshar (2017)[22] | Retrospective section | Childbirth training classes and childbirth programs are associated with natural childbirth | 14630 people | Birth plan, demographic profile survey questionnaire | Attending a childbirth preparation class and/or having a birth plan was associated with natural birth. These findings suggest that patient education and birth preparation may influence delivery. Childbirth preparation classes and childbirth programs can be used as quality improvement tools to potentially reduce cesarean rates. |
| 16 | Afshar (2018)[23] | Prospective cohort | Birth plans - influence on mode of delivery, midwifery interventions, and satisfaction with the birth experience: a prospective cohort study. | 297 people | Birth plan, maternal characteristics questionnaire, factors during pregnancy, newborn characteristics and patient satisfaction criteria | Women with and without a birth plan had similar odds of cesarean delivery. Although women with a birth plan had fewer midwifery interventions, they were less satisfied with their birth experience. More research is needed to understand how to improve patient satisfaction with childbirth. |
| 17 | Hadar (2012)[16] | Retrospec | Obstetric outcomes in women with self-prepared birth plan | 616 people | Compared to the control group matched for age, fertility, and gestational week, women who come with a birth plan are less likely to have a cesarean section, and have a lower probability of first- and second-degree perineal tears. Also, women with a birth plan are more likely to use an epidural. Lack of data and misconceptions of medical staff suggest that larger prospective studies are needed. |
Discussion
Although pregnancy and childbirth is a natural and physiological processes, the experience of a mother during her pregnancy and the birth of her child is very important. A positive childbirth experience can be accompanied by a feeling of control, strength, satisfaction, and confidence in mothers and can affect the health of the mother, the baby, and their emotional connection, the mother's sexual activity, and the desire to have children again in the future.[24,25,26] This is while about 7-35% of women have mentioned a negative experience of childbirth.[27,28,29,30,31] According to the studies, the birth plan can be an effective tool to achieve better results for the mother and her child. Studies that emphasized the positive outcomes of birth plans reported that birth plans were associated with less intervention, a more natural birth process, and better outcomes for mothers and babies. Birth plans can improve the well-being of the mother and baby and lead to birth in a more natural way.[11] They also stated that the birth plan can be an effective tool to achieve better results for the mother and her child.[8] In addition, women who receive birth planning care (birth plan) during childbirth are more satisfied than women who do not receive the necessary care.[9] Also, mothers with a birth plan were more likely to start breastfeeding in the delivery room. Epidural analgesia was the most common method used for pain relief, and women who presented with a birth plan tried to use more non-pharmacological methods at the same time.[12] The birth plan leads to a higher implementation of maternity care, it has a positive effect on maternal and fetal outcomes, and in general, women's empowerment scores increased after the implementation of the birth and delivery plan.[10] Birth plans may be beneficial and not associated with any adverse obstetric or neonatal outcomes. Mothers who have birth plans and their babies have at least as good outcomes as those who do not. Infants of primiparous women with a delivery schedules had better umbilical cord blood pH values than those of primiparous women without a delivery schedule.[11] Women who come with a birth plan are less likely to undergo a cesarean section, the probability of first- and second-degree perineal tears is higher, and they are more likely to use an epidural.[16] Patients with birth plans did not have an increased incidence of episiotomy or cesarean section, but they were less likely to receive epidural anesthesia during labor.[17] But one study showed different results and reported that a delivery program was associated with a significant increase in metabolic acidemia indices in infants. A longer delivery schedule was also associated with a significantly higher rate of cesarean delivery.[14] A number of studies also stated that more studies should be done in this field. In this case, Afshar et al. reported in their study that women with and without a birth plan had similar odds of cesarean delivery. Although women with a birth plan had fewer midwifery interventions, they were less satisfied with their birth experience. More research is needed to understand how to improve patient satisfaction with childbirth.[23] They also stated that compared to the control group matched for age, fertility, and gestational week, women who come with a birth plan are less likely to have a cesarean section, and have a lower probability of first- and second-degree perineal tears. Also, women with a birth plan are more likely to use an epidural. The lack of data and misconceptions about medical staff suggest that larger prospective studies are needed.[16]
Limitation and recommendation
According to the results of the studies, the positive effects of the birth plan on maternal and newborn outcomes are more than their negative effects, but more studies are needed in this field to express a definite opinion. Also, it is recommended that Iranian pregnant women use the birth plan and its results are examined to increase the ability to generalize the results to the Iranian society.
Conclusion
According to the results of the conducted studies, the maternal and neonatal consequences of the birth plan prevail over its negative consequences, and the use of the birth plan can increase the empowerment of women, satisfaction with childbirth, the positive experience of childbirth, and reduce the rate of cesarean section, negative maternal and newborn consequences.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
This study is the result of the studies reviewed for the thesis proposal approved by Isfahan University of Medical Sciences with code IR.MUI.NUREMA.REC.1400.064. Hereby, thanks and appreciation is given to the respected vice-chancellor of technological research of Isfahan University of Medical Sciences and all the authors of the articles whose results are the result of their efforts.
References
- 1.Hasenmiller R. Do Birth Plans influence Childbirth Satisfaction? Philadelphia: Philadelphia University; 2001. [Google Scholar]
- 2.Suárez-Cortés M, Armero-Barranco D, Canteras-Jordana M, Martínez-Roche ME. Use and influence of delivery and birth plans in the humanizing delivery process. Rev Lat Am Enfermagem. 2015;23:520–6. doi: 10.1590/0104-1169.0067.2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ministerio de Sanidad y Consumo (ES) Estrategia de Atención al Parto Normal. Madrid: Ministerio de Sanidad y Consumo; 2007. [Google Scholar]
- 4.Federación de Asociación de Matronas de España Iniciativa Parto Normal. 2007 [Google Scholar]
- 5.Aragon M, Chhoa E, Dayan R, Kluftinger A, Lohn Z, Buhler K. Perspectives of expectant women and health care providers on birth plans. J Obstet Gynaecol Can. 2013;35:979–85. doi: 10.1016/S1701-2163(15)30785-4. [DOI] [PubMed] [Google Scholar]
- 6.Rulon V. Obtaining quality healthcare through patient and caregiver engagement. J American Health Inf Manag Assoc. 2015;86:48–51. [Google Scholar]
- 7.Anderson CJ, Kilpatrick C. Supporting patients’ birth plans: Theories, strategies and implications for nurses. Nursing for Womens Health. 2012;16:210–8. doi: 10.1111/j.1751-486X.2012.01732.x. [DOI] [PubMed] [Google Scholar]
- 8.Hidalgo-Lopezosa P, Hidalgo-Maestre M, Rodríguez-Borrego MA. Birth plan compliance and its relation to maternal and neonatal outcomes. Rev Latino-Am Enfermagem. 2017;25:e2953. doi: 10.1590/1518-8345.2007.2953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farahat AH, Mohamed HES, Elkader ShA. Effect of implementing A birth plan on womens’ childbirth experiences and maternal and neonatal outcomes. J Educ Pract. 2015;6:24–31. [Google Scholar]
- 10.Soliman Abdelalim R, Emam A, Sarhan A. Effect of implementing birth plan on women childbirth outcomes and empowerment. Am J Nurs Sci. 2020;9:160. [Google Scholar]
- 11.Hidalgo-Lopezosa P, Rodríguez-Borrego MA, Muñoz-Villanueva MC. Are birth plans associated with improved maternal or neonatal outcomes? MCN Am J Matern Child Nurs. 2013;38:150–6. doi: 10.1097/NMC.0b013e31827ea97f. [DOI] [PubMed] [Google Scholar]
- 12.López-Gimeno E, Falguera-Puig G, Vicente-Hernández MM. Birth plan presentation to hospitals and its relation to obstetric outcomes and selected pain relief methods during childbirth. BMC Pregnancy Childbirth. 2021;21:274. doi: 10.1186/s12884-021-03739-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmadpour P, Mosavi S, Mohammad-Alizadeh-Charandabi S. Evaluation of the birth plan implementation: A parallel convergent mixed study. Reprod Health. 2020;17:138. doi: 10.1186/s12978-020-00989-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis B, Clark S, McDonald K, Young T, Swaim L. The impact of a birth plan on maternal and neonatal delivery outcomes. Am J Obstet Gynecology. 2019 [Google Scholar]
- 15.Hidalgo-Lopezosa P, Cubero-Luna AM, Jiménez-Ruz A, Hidalgo-Maestre M, Rodríguez-Borrego MA, López-Soto PJ. Association between birth plan use and maternal and neonatal outcomes in southern Spain: A case-control study. Int J Environ Res Public Health. 2021;18:456. doi: 10.3390/ijerph18020456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hadar E, Raban O, Gal B, Yogev Y, Melamed N. Obstetrical outcome in women with self-prepared birth plan. J Matern Fetal Neonatal Med. 2012;25:2055–7. doi: 10.3109/14767058.2012.678438. [DOI] [PubMed] [Google Scholar]
- 17.Deering SH, Zaret J, McGaha K, Satin AJ. Patients presenting with birth plans: A case-control study of delivery outcomes. J Reprod Med. 2007;52:884–7. [PubMed] [Google Scholar]
- 18.Medeiros RMK, Figueiredo G, Correa Á CP, Barbieri M. Repercussions of using the birth plan in the parturition process. Rev Gaucha Enferm. 2019;40:e20180233. doi: 10.1590/1983-1447.2019.20180233. [DOI] [PubMed] [Google Scholar]
- 19.Alba-Rodríguez R, Coronado-Carvajal MP, Hidalgo-Lopezosa P. The birth plan experience-A pilot qualitative study in Southern Spain. Healthcare (Basel) 2022;10:95. doi: 10.3390/healthcare10010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mirghafourvand M, Mohammad Alizadeh Charandabi S, Ghanbari-Homayi S, Jahangiry L, Nahaee J, Hadian T. Effect of birth plans on childbirth experience: A systematic review. Int J Nurs Pract. 2019;25:e12722. doi: 10.1111/ijn.12722. [DOI] [PubMed] [Google Scholar]
- 21.Jolles MW, de Vries M, Hollander MH, van Dillen J. Prevalence, characteristics, and satisfaction of women with a birth plan in The Netherlands. Birth. 2019;46:686–92. doi: 10.1111/birt.12451. [DOI] [PubMed] [Google Scholar]
- 22.Afshar Y, Wang ET, Mei J, Esakoff TF, Pisarska MD, Gregory KD. Childbirth education class and birth plans are associated with a vaginal delivery. Birth. 2017;44:29–34. doi: 10.1111/birt.12263. [DOI] [PubMed] [Google Scholar]
- 23.Afshar Y, Mei JY, Gregory KD, Kilpatrick SJ, Esakoff TF. Birth plans-Impact on mode of delivery, obstetrical interventions, and birth experience satisfaction: A prospective cohort study. Birth. 2018;45:43–9. doi: 10.1111/birt.12320. [DOI] [PubMed] [Google Scholar]
- 24.Mukamurigo JU, Berg M, Ntaganira J, Nyirazinyoye L, Dencker A. Associations between perceptions of care and women's childbirth experience: A population-based cross-sectional study in Rwanda. BMC Pregnancy Childbirth. 2017;17:181. doi: 10.1186/s12884-017-1363-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nilsson L, Thorsell T, Hertfelt Wahn E, Ekström A. Factors influencing positive birth experiences of First-time mothers. Nurs Res Pract. 2013;2013:1–6. doi: 10.1155/2013/349124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ulfsdottir H, Nissen E, Ryding E, Lund-Egloff D, Wiberg-Itzel E. The association bwtween labour variables and primiparous women's experience of childbirth; A prospective cohort study. BMC Pregnancy Childbirth. 2014;14:208. doi: 10.1186/1471-2393-14-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sigurdardottir VL, Gamble J, Gudmundsdottir B, Kristjansdottir H, Sveinsdottir H, Gottfredsdottir H. The predictive role of support in the birth experience: A longitudinal cohort study. Women Birth. 2017;30:450–9. doi: 10.1016/j.wombi.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 28.Saeidi R, Tafazoli M, Gholami Robatsangi M. Kangaroo mother care for infantile colic: a randomized clinical trial. Tehran Univ Med J. 2010;67(12):870–875. [Google Scholar]
- 29.Partovi S, Kianifar H R, Gholami Robatsangi M, Ghorbani Z, Saeidi R. Evaluation of massage with oil containing medium chain triglyceride on weight gaining in preterm. Koomesh. 2009;11:1–6. [Google Scholar]
- 30.Charoghchian Khorasani E, Peyman N, Esmaily H. Effect of education based on the theory of self-efficacy and health literacy strategies on exclusive breastfeeding: A randomized clinical trial. Koomesh. 2019;21:633–8. [Google Scholar]
- 31.Jafari A, Alami A, Charoghchian E, Delshad Noghabi A, Nejatian M. The impact of effective communication skills training on the status of marital burnout among married women. BMC Womens Health. 2021;21:231. doi: 10.1186/s12905-021-01372-8. [DOI] [PMC free article] [PubMed] [Google Scholar]