Abstract
Telemedicine is the use of technology to provide healthcare services and information remotely, without requiring physical proximity between patients and healthcare providers. The coronavirus disease 2019 (COVID-19) pandemic has accelerated the rapid growth of telemedicine worldwide. Integrating artificial intelligence (AI) into telemedicine has the potential to enhance and expand its capabilities in addressing various healthcare needs, such as patient monitoring, healthcare information technology (IT), intelligent diagnosis, and assistance. Despite the potential benefits, implementing AI in telemedicine presents challenges that can be overcome with physician-guided implementation. AI can assist physicians in decision-making, improve healthcare delivery, and automate administrative tasks. To ensure optimal effectiveness, AI-powered telemedicine should comply with existing clinical practices and adhere to a framework adaptable to various technologies. It should also consider technical and scientific factors, including trustworthiness, reproducibility, usability, availability, and cost. Education and training are crucial for the appropriate use of new healthcare technologies such as AI-enabled telemedicine. This article examines the benefits and limitations of AI-based telemedicine in various medical domains and underscores the importance of physician-guided implementation, compliance with existing clinical practices, and appropriate education and training for healthcare providers.
Keywords: Artificial intelligence (AI), COVID-19, intensive care unit (ICU), telemedicine, telehealth, tele-ICU
Introduction
The integration of artificial intelligence (AI) and telemedicine represents a state-of-the-art solution in the healthcare industry that boosts medical care accessibility, efficiency, and quality.[1] This integration offers limitless opportunities for tailoring healthcare solutions using AI to cater to specific needs. Telemedicine assisted by AI can improve the patient experience, healthcare outcomes, and the quality of services offered by physicians. By speeding up disease screening and diagnosis, making diagnoses more precise and personalized, and decreasing the necessity for in-person consultations, AI can exhibit a very important role in promoting and facilitating access to integrated health care throughout a person's lifespan. In managing chronic diseases, AI-enabled remote care can enhance communication and connections across various healthcare delivery elements, enabling healthcare professionals for interaction and providing a knowledge repository for managing patients.[2]
Telemedicine and its importance
Telemedicine is defined by the World Health Organization as using information and communication technologies to provide healthcare services when distance is a critical factor.[3] The definition encompasses several aspects, such as diagnosing, treating, preventing diseases and injuries, conducting research, and providing continuing education to healthcare providers, with the final aim to promote the health of individuals and communities. Telemedicine is a healthcare method and not a tool; it can be carried out through different modalities, such as live video consultations or store-and-forward messaging systems. Although terms such as telemedicine and telehealth are frequently used interchangeably,[4] they carry separate technical and regulatory definitions, and other terms such as digital health and mobile health are used to provide a broader and more comprehensive view of people's health care in the digital age.
Telemedicine refers specifically to the provision of healthcare services and consultations through remote technologies such as videoconferencing, while telehealth is a broader term that includes all healthcare services delivered through technology, including remote monitoring, patient education, and medical record management.
In other words, telemedicine is a subset of telehealth, which encompasses a wider range of healthcare services delivered through technology. While telemedicine focuses on virtual consultations and diagnosis, telehealth includes all aspects of health care that can be delivered through technology, such as patient monitoring, disease management, and medication adherence.
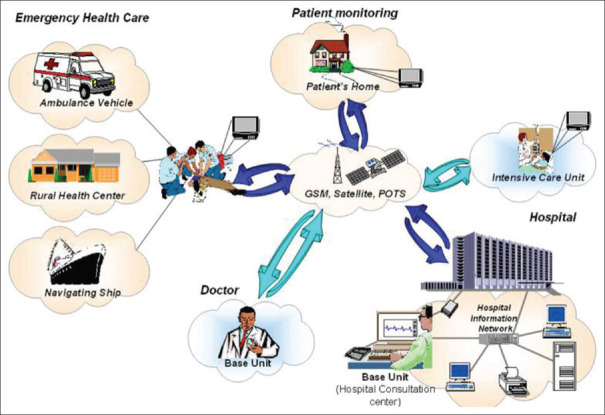
Figure 1 displays the telemedicine system's overall architecture.[5]
Figure 1.
Telemedicine architecture[5]
In each instance, the telemedicine unit is situated at the patient's location, while the base unit/doctor's unit is positioned at the site where the patient's signals and images are monitored and transmitted. The telemedicine device collects various kinds of data including images and biosignals from the patient and transmits it automatically to the base unit. The doctor's unit consists of several user-friendly software modules capable of receiving data from the telemedicine device, transmitting information to it, and storing critical data in a local database. The system offers several applications that may differ slightly depending on the nature and requirements of the current healthcare provision.
Telemedicine has demonstrated its benefits in various medical specialties, including managing type 2 diabetes,[6] remote monitoring in cardiovascular patients,[7] and effective interventions in teleoncology.[8] The utilization of telemedicine has significantly surged due to the coronavirus disease 2019 (COVID-19) pandemic. Telemedicine allows patients to access medical services from the convenience of their own homes, diminishing the requirement for unwarranted visits to healthcare facilities and minimizing the risk of infection. Additionally, healthcare professionals experienced in treating severe COVID-19 cases can offer support to their colleagues in various hospitals, regardless of their location, even in different countries.[9]
AI in telemedicine: Integration and challenges
AI has the potential to enhance the capabilities of healthcare professionals and improve the efficiency and safety of telemedicine. AI is anticipated to tackle the issue of avoidable medical errors and enhance workflow efficiencies, which are currently at a high rate in healthcare provision.[10] However, its integration into everyday practice has been limited due to various factors including safety, regulatory, and financial challenges.[11]
Integrating AI into telemedicine has the potential to revolutionize health care, but it also poses several challenges and limitations. One of the primary concerns is safety, as AI algorithms may not always be accurate and can make errors that could harm patients. Another major challenge is regulatory compliance, as AI-powered telemedicine platforms must adhere to strict regulations to ensure patient privacy and data security.
Moreover, the financial factor is also a major concern as integrating AI in telemedicine requires significant investment in infrastructure and technology, which may not be feasible for small or resource-constrained healthcare providers. Additionally, there is a need to address the ethical concerns surrounding the use of AI in health care, such as issues of bias and transparency.
To overcome these challenges, it is essential to establish clear guidelines and regulations around the use of AI in telemedicine. Healthcare providers must also invest in training and upskilling their workforce to ensure they are proficient in utilizing AI technologies. Finally, collaboration between healthcare providers, policymakers, and technology companies can help create an ecosystem that fosters innovation while ensuring patient safety and compliance with regulatory requirements.
Four emerging trends in which AI is impacting telemedicine[12] are as follows: 1) monitoring of patients, 2) using information technology in health care, 3) use of intelligent assistance and diagnosis, and 4) collaborative information analysis. Despite these effects, the adoption of AI in healthcare requires convincing evidence of its benefits for both the medical community and patients.[1]
Physicians have a critical role to play in the adoption of AI in health care by serving as knowledgeable guides and leaders in the process. While AI may be more accurate than a physician in some specific situations, it cannot replace the comprehensive role of physicians. Physicians are trained to react dynamically to new patient information, make new diagnoses and therapeutic decisions, and understand the potential consequences and unintended side effects of a diagnosis. In conclusion, AI integration into telemedicine has significant potential benefits, but challenges and limitations must be addressed to ensure safe, effective, and ethical implementation. Physicians must play a key role in guiding the integration process, and convincing evidence of AI benefits is necessary for its adoption by both the medical community and patients.
AI has the potential to aid physicians in decision-making and various tasks to enhance healthcare delivery. This release of time enables healthcare professionals to allocate more valuable time directly to care of patients.[13] As almost half of a doctor's time is consumed on electronic health records (EHRs),[14] innovative tools such as speech recognition could replace the usage of keyboards for entering and retrieving info, further improving efficiency.
In the early diagnosis of a patient's health problem, the role of history taking is more significant than physical inspection, with a few studies indicating an influence of 76% by history and 11% by physical inspection.[15] The integration of AI into a telehealth application has the potential to assist in the diagnostic process by providing prompts and hints, suggesting appropriate follow-up questions based on the responses given, and ultimately saving the physician's time.[16]
For AI-enabled telemedicine to be scalable, it must align with existing clinical practice. To validate technological innovations for real-world applications, a transparent and rigorous framework is essential. This framework must be flexible enough to apply to a wide range of technologies and should take into account various technical and scientific factors, as well as considerations such as trustworthiness, reproducibility, usableness, availability, and cost.[17] Ethical considerations and independent governance should also be included in the framework.
While AI can be highly advantageous for critical reasoning and problem-solving, particularly with huge volumes of data, it should not undermine the critical skills of physicians in health care.[16] Contextual information and distinguishing relevant versus nonrelevant input are areas where AI may fall short, requiring physicians to handle healthcare contingencies. Any AI-powered system should prioritize evidence-based management principles for the collective good and performance.[16]
To ensure the protection of healthcare data, which is of a sensitive nature, measures such as data encryption and blockchain technology are necessary. Medical associations from different countries have recommended that AI developers take responsibility and obtain medical liability insurance to cover system failures or misdiagnosis resulting from autonomous AI systems.[18] To ensure the real-world validation of AI-enabled telemedicine, a robust and transparent framework is necessary, which should incorporate independent governance and ethical aspects.[17]
Potential challenges of implementing AI-enabled telemedicine in resource-limited settings
Implementing AI-enabled telemedicine in resource-limited settings can bring a number of potential challenges. Some of the key challenges are as follows:
Lack of access to technology: One of the main challenges in resource-limited settings is the lack of access to technology. AI-enabled telemedicine requires advanced technology and infrastructure, including high-speed Internet, computers, and mobile devices. In areas where these resources are scarce, it can be difficult to implement and sustain telemedicine services.
Limited human resources: Another challenge is the limited number of healthcare professionals available in resource-limited settings. AI-enabled telemedicine requires skilled professionals to develop, operate, and maintain the systems. In areas where there is already a shortage of healthcare professionals, it can be difficult to find and train individuals with the necessary skills.
Language and cultural barriers: Communication barriers can be a significant challenge when implementing telemedicine in resource-limited settings. Many communities in these areas have diverse languages and cultures, and finding healthcare professionals who can speak and understand local languages can be a challenge. The use of AI-enabled natural language processing can help overcome some of these barriers, but it may not be fully effective in all situations.
Data privacy and security concerns: Another challenge is ensuring the privacy and security of patient data. AI-enabled telemedicine relies heavily on the use and exchange of patient data. In areas where there are limited resources and infrastructure to support data security and privacy, there is a risk of data breaches and loss of sensitive information.
Limited financial resources: Implementing AI-enabled telemedicine can be expensive, particularly in resource-limited settings where financial resources are scarce. The costs of developing and maintaining the technology and infrastructure, as well as training and paying staff, can be a significant challenge.
The Synergy of Telemedicine and AI in Healthcare
Tele-intensive care unit (ICU) and the role of AI
Tele-ICU or telemedicine in intensive care units refers to the exchange of health information from one hospital's critical care unit to another via electronic communications.[19] The use of tele-ICU allows intensivists to remotely monitor and manage critically ill patients in multiple locations simultaneously. Research has demonstrated that this approach can enhance clinical outcomes, lessen mortality rates, and shorten the length of stay in the ICU.
During the COVID-19 pandemic, ICU patient capacities have varied significantly, ranging from 52% to 289% during surge conditions.[20] These patients are the most critically ill in acute care and have a mortality rate as high as 41% in the COVID-19 era.[21] Health care spending in the United States represents approximately 17% of the gross domestic product, with ICU care accounting for up to 4.1% of this spending.[22] It is crucial to develop approaches that enhance patient outcomes and optimize the efficiency of care delivery. Tele-ICU has been utilized to lower mortality rates and improve patient safety outcomes.[23,24,25]
The potential of AI to enhance the capabilities of tele-ICU is considerable, as it can provide real-time analysis of patient data and aid in scientific decision-making. AI programs can be trained to identify patterns in the data of the patient and provide alerts when a patient's condition deviates from expected norms. This can help clinicians intervene earlier and prevent adverse events. In addition to real-time monitoring, AI can also be used to predict patient outcomes and assist with resource allocation. For example, AI algorithms can predict which patients are at the highest risk of developing sepsis or other complications, allowing clinicians to prioritize their care. AI can also assist in predicting the need for mechanical ventilation or other interventions, allowing for more efficient use of resources.
On March 27, 2020, the CLEW AI-based tele-ICU solution was implemented in two Israeli hospitals, Sheba and Sourasky Medical Center. The solution employs an AI-based analytics platform to expand ICU capacity, manage resources, and care for COVID-19-infected patients while also safeguarding frontline healthcare workers.[26] CLEW uses machine learning algorithms to forecast respiratory failure and enable timely interventions that can enhance clinical outcomes, particularly in COVID-19 patients. It also enables medical personnel to monitor the severity of illness from a remote control center. In anticipation of a surge in ICU admissions, both hospitals have set up field ICU that will serve as significant care units in Israel. These units employ telemedicine facilities to enable remote patient monitoring from a centralized control center.[27] Figure 2 depicts the CLEW model.[27]
Figure 2.
Model of CLEW AI-based tele-ICU[27]
One of the main challenges with implementing AI in tele-ICU is ensuring that the algorithms are accurate and reliable. This requires robust training datasets and ongoing validation to ensure that the algorithms are performing as intended. Moreover, it is crucial to guarantee transparency and explainability in the utilization of AI, enabling clinicians to comprehend the reasoning behind the algorithms’ predictions and make informed judgments. Overall, the combination of AI with tele-ICU has the potential to improve patient outcomes and increase access to critical care expertise, while also improving efficiency and resource allocation. Nonetheless, it is crucial to exercise prudence when utilizing this technology in a responsible and right manner.
Ethical concerns with implementing AI in tele-ICU
One potential ethical concern with implementing AI in tele-ICU is the risk of relying too heavily on technology and neglecting the importance of human expertise and judgment. It is essential to ensure that AI is used as a tool to support and augment clinical decision-making, rather than replacing it entirely. Additionally, there is a risk of bias in the AI algorithms, which could lead to disparities in care for certain patient populations. To address these concerns, it is crucial to involve a diverse group of experts in the development and implementation of AI algorithms and to regularly evaluate the algorithms for accuracy, bias, and transparency. It is also important to provide training and education to clinicians on the proper use and interpretation of AI outputs to ensure they are making informed decisions. Finally, transparency in the development, implementation, and use of AI in tele-ICU is critical to ensuring that patients and clinicians understand how the technology is being used and can trust its capabilities.
Telecardiology and the role of AI
Telecardiology is the use of telemedicine to remotely diagnose and manage heart-related conditions.[28] It encompasses the utilization of technology to transmit medical data, images, and other information related to cardiac care from one location to another. This enables remote consultation and diagnosis, which can be especially advantageous for patients residing in rural or isolated regions, or those with restricted mobility. Telecardiology has been shown to improve patient results and cut costs, making it an attractive option for many healthcare providers.
The use of AI in telecardiology is rapidly expanding, as it has the ability to rapidly and accurately analyze substantial amounts of data. This can assist in the diagnosis and treatment of heart-related ailments. For instance, AI algorithms can be employed to examine electrocardiograms (ECGs) and other cardiac imaging tests, identifying patterns and anomalies that may prove challenging for human clinicians to discern. This can help with the early diagnosis and treatment of heart disease, leading to improved results for patients.
AI can also be used in telecardiology to help with remote patient monitoring. Wearable devices such as smartwatches and fitness trackers can collect data on heart rate, rhythm, and activity levels, which can be transmitted to healthcare providers for analysis. AI algorithms can be used to study and examine these data in real time, alerting healthcare providers to any abnormalities or changes that may require further attention. This can be especially beneficial for patients who suffer from chronic heart conditions and necessitate continuous monitoring to manage their condition. In addition to remote patient monitoring, AI can also be used to assist with decision-making in telecardiology. For instance, AI algorithms can be used to examine patient information and medical records to predict the likelihood of heart-related events such as heart attacks or strokes. The data obtained through AI analysis can be utilized to create tailored treatment plans for individual patients, improving outcomes and reducing the risk of complications.
A study published in the journal Nature in 2020[29] found that an AI-based telemedicine system was able to outperform radiologists in identifying breast cancer in mammograms. The system was also able to reduce the number of false positives and false negatives.
Overall, the use of AI in telecardiology has the potential to transform the way that heart-related conditions are diagnosed and managed. By leveraging the power of technology, healthcare providers can enhance patient outcomes and lower expenses, while also ensuring that patients receive the utmost quality of care regardless of their location or mobility.
Teleoncology and the role of AI
Teleoncology is the use of telemedicine technologies to provide cancer care and management to patients who are located remotely or do not have access to specialized oncology services.[30] With the increasing prevalence of cancer worldwide, teleoncology is emerging as a crucial tool for enhancing access to care, lessening patient burden, and improving the efficiency of healthcare delivery.
One of the key advantages of teleoncology is its ability to facilitate multidisciplinary consultations and care coordination among oncology specialists, primary care providers, and patients, regardless of their location. This is particularly useful in areas where cancer care resources are limited or inaccessible, such as rural or remote regions. Teleoncology can also help to decrease the costs and time associated with travel for patients and their families, allowing for more frequent check-ins and follow-up visits.
The significance of AI in teleoncology is growing progressively due to its capacity to improve the precision, accuracy, and efficiency of cancer diagnosis, treatment planning, and monitoring. Medical data of substantial size, including imaging studies and pathology reports, can be analyzed by AI algorithms to detect patterns and trends that human clinicians may not readily perceive. This can help improve the accuracy of cancer diagnosis, which is crucial for determining the appropriate treatment options. In addition, AI can assist in treatment planning by providing personalized recommendations based on the patient's medical history, genetic profile, and treatment response. This can help to optimize treatment outcomes and minimize the risk of adverse effects. AI can also help to monitor patient progress during and after treatment, allowing for early detection of any potential complications or recurrence of cancer.
However, it is noteworthy to mention that the utilization of AI in teleoncology should be accompanied by rigorous ethical and regulatory standards to ensure patient safety, privacy, and informed consent.[31] It is equally essential to acknowledge that AI is not designed to supplant human clinicians but rather to aid them in making more accurate and efficient decisions. In conclusion, teleoncology and the role of AI are important tools in the fight against cancer. They can help improve access to care, reduce patient burden, and enhance the accuracy and efficiency of cancer diagnosis, treatment planning, and monitoring. Ensuring responsible and ethical usage of these technologies is crucial in the advancement of teleoncology, to optimize patient outcomes.
Telepsychiatry and the role of AI
Telepsychiatry is the practice of providing mental healthcare services through remote communication technologies such as video conferencing, phone calls, or messaging platforms.[32] In recent years, it has gained popularity as a form of telemedicine, particularly in underserved areas where the availability of mental health care is restricted.
The use of telepsychiatry has numerous advantages, including increasing access to mental health care, reducing travel time and costs, and providing flexibility for both patients and providers. Nevertheless, certain obstacles require attention, including privacy and security concerns, regulatory barriers, and the necessity for adequate training and education for providers.[33]
One potential solution to some of these challenges is the integration of AI into telepsychiatry. AI has the potential to improve the efficiency and accuracy of mental health assessments and treatment, as well as to address some of the limitations of traditional telepsychiatry. For instance, AI can be used to analyze speech patterns and facial expressions in real time to help detect signs of depression, anxiety, or other mental health conditions. It can also assist in identifying potential medication interactions or side effects and provide personalized treatment recommendations based on a patient's symptoms and history.
AI can also help address the shortage of mental healthcare providers in certain areas by providing virtual therapy sessions and counseling. It can also provide self-help resources and tools for patients to use outside of therapy sessions, such as cognitive-behavioral therapy exercises or mindfulness meditation.
However, there are also concerns about the potential misuse of AI in mental health care, particularly in areas such as diagnosis and treatment recommendations. Validating the reliability of any AI tools utilized in telepsychiatry based on sound clinical evidence is essential.[34] On the whole, integrating AI into telepsychiatry has the potential to greatly enhance the quality and accessibility of mental healthcare services. However, it is important to approach this technology with caution and to always prioritize patient safety and privacy.
Telestroke and the role of AI
Stroke is a primary cause of disability and mortality globally, with significant financial costs for healthcare services, patients, and their families. Low- and middle-income countries account for 85% of strokes, and delays in diagnosis and treatment can lead to poor outcomes.[35]
Telestroke is a medical service that uses telemedicine technology to connect neurologists with patients who are experiencing a stroke in remote or underserved areas.[36] Telemedicine, particularly teleneurology, has emerged as a cost-effective method for providing neurological care, especially in areas with a shortage of neurologists. Telestroke systems have even incorporated AI algorithms, including machine learning and deep learning that can be utilized to automate the interpretation and categorization of radiologic imaging. These algorithms have shown the ability to accurately identify stroke location, severity, and subtypes, including midline shifts.[37] In some cases, these automated systems have also helped in the decision-making process for endovascular reperfusion therapy.[38]
Various aspects of acute stroke management now integrate AI algorithms. In prehospital notifications, AI can alert emergency departments to incoming strokes, allowing for appropriate preparation and management according to stroke type and other characteristics.[37] Platforms such as ASPECTS[39] and Rapid Processing of Perfusion and Diffusion A (RapidAI)[40] use machine learning and neuroimaging to assess the extent of early ischemic stroke and provide real-time views of brain perfusion, respectively. Medtronic and Zydus Hospitals have recently entered into an agreement in the state of Gujarat, India, to collaborate on the implementation of AI technology to provide remote stroke care.[41]
While AI has shown significant improvements in treatment decisions and clinical outcomes in telestroke, future studies are needed to validate its techniques for widespread use.
Teleurology and the role of AI
Teleurology involves the use of telecommunication technology to remotely provide urological care to patients.[42] The utilization of teleurology and digital health applications proved to be highly advantageous, particularly amid the COVID-19 pandemic.[43] In urology, AI can help with the analysis of medical images and the identification of abnormalities or patterns that may be indicative of certain conditions or diseases.
Some of the hospitals using AI-based teleurology to provide remote urological care to patients are mentioned below:
The University of California, Los Angeles (UCLA) Health System has implemented an AI-powered teleurology program that provides remote consultations for patients with urological conditions. The program uses AI algorithms to analyze medical images and provide diagnostic recommendations to healthcare providers.[44]
The University of Southern California (USC) Institute of Urology has developed an AI-powered tool called UroScore that can predict the likelihood of prostate cancer based on various factors such as age, family history, and prostate-specific antigen (PSA) levels. UroScore is used in conjunction with teleurology consultations to provide remote prostate cancer screening and follow-up care.[45]
The Cleveland Clinic has developed an AI tool called Predictive Analytics for Kidney Injury (PAKI) that can predict the likelihood of acute kidney injury in patients undergoing urological surgeries. PAKI is used in conjunction with teleurology consultations to remotely monitor patients and provide early intervention if necessary.[46]
Overall, AI-based teleurology has the potential to significantly improve patient outcomes and access to care, especially in areas with limited access to specialist services.
Role of education and training in adopting AI-Enabled telemedicine technology
Education and training are very vital for the appropriate use of new healthcare technologies such as telemedicine and AI. Although some progress has been made in incorporating telemedicine training into medical education, there remains a lack of education in this area. Incorporating telemedicine training into their curriculum is advisable for medical schools, with a focus on educating students about the advantages and limitations of telemedicine, emphasizing the importance of maintaining a strong patient–doctor relationship, and ensuring patient privacy protection. The education on telemedicine and AI should cover a range of topics such as the following:
Access to care: How telemedicine and AI can improve access to healthcare services, particularly for individuals living in remote or underserved areas.
Cost: The potential cost savings associated with telemedicine and AI, as well as the costs of implementing these technologies.
Cost-effectiveness: The efficacy and cost-effectiveness of telemedicine and AI in comparison with traditional healthcare delivery models.
Patient experience: The impact of telemedicine and AI on patient satisfaction, engagement, and overall experience.
Clinician experience: The impact of telemedicine and AI on clinician workload, job satisfaction, and the overall practice of medicine.
It is recommended that medical specialty boards and societies consider creating specialty-specific educational modules that focus on AI.
There are many other areas that could be covered in education on telemedicine and AI. Some additional areas that could be included are as follows:
Legal and regulatory issues related to telemedicine and AI
Ethical considerations for telemedicine and AI, such as informed consent and privacy concerns
Technical aspects of telemedicine and AI, including how to use the technologies and troubleshoot technical issues
Cultural considerations for telemedicine and AI, such as language barriers and cultural competence.
Conclusion and Future Scope
Collaboratively, telemedicine and AI have the potential to transform healthcare delivery by enhancing access to care, enhancing diagnostic accuracy, and optimizing treatment outcomes. However, it is important to ensure that these technologies are implemented ethically, and their effectiveness and safety are validated through rigorous research and evaluation. Without becoming experts in AI, physicians should have a good understanding of the capabilities and limitations of AI algorithms to make the best use of them. Overall, AI has the potential to significantly improve the quality of care delivered through telemedicine, particularly during times of crisis such as the COVID-19 pandemic.
Ethics
To carry out the study, permission was obtained from Dr. Raj Raval, Gujarat Pulmonary and Critical Care Medicine, Ahmedabad, India, and he was ready to participate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6:94–8. doi: 10.7861/futurehosp.6-2-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haleem A, Javaid M, Singh RP, Suman R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens Int. 2021;2:100117. doi: 10.1016/j.sintl.2021.100117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Group Consultation on Health Telematics. A health telematics policy in support of WHO's Health for-All strategy for global health development: Report of the WHO group consultation on health telematics, 11-16 December, Geneva. World Health Organization; 1997. [[Last accessed on 2023 Feb 24]]. Available from: https://apps.who.int/iris/handle/10665/63857 . [Google Scholar]
- 4.Bitar H, Alismail S. The role of eHealth, telehealth, and telemedicine for chronic disease patients during COVID-19 pandemic: A rapid systematic review. Digit Health. 2021;7:20552076211009396. doi: 10.1177/20552076211009396. doi: 10.1177/20552076211009396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ajami S, Lamoochi P. Use of telemedicine in disaster and remote places. J Edu Health Promot. 2014;3:26. doi: 10.4103/2277-9531.131886. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 6.Tchero H, Kangambega P, Briatte C, Brunet-Houdart S, Retali GR, Rusch E. Clinical effectiveness of telemedicine in diabetes mellitus: A meta-analysis of 42 randomized controlled trials. Telemed J E Health. 2019;25:569–83. doi: 10.1089/tmj.2018.0128. [DOI] [PubMed] [Google Scholar]
- 7.Zhu Y, Gu X, Xu C. Effectiveness of telemedicine systems for adults with heart failure: A meta-analysis of randomized controlled trials. Heart Fail Rev. 2020;25:231–43. doi: 10.1007/s10741-019-09801-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hazin R, Qaddoumi I. Teleoncology: Current and future applications for improving cancer care globally. Lancet Oncol. 2010;11:204–10. doi: 10.1016/S1470-2045(09)70288-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Razu SR, Yasmin T, Arif TB, Islam MS, Islam SMS, Gesesew HA, et al. Challenges faced by healthcare professionals during the covid-19 pandemic: A qualitative inquiry from Bangladesh. Front Public Health. 2021;9:647315. doi: 10.3389/fpubh.2021.647315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Topol EJ. High-performance medicine: The convergence of human and artificial intelligence. Nat Med. 2019;25:44–56. doi: 10.1038/s41591-018-0300-7. [DOI] [PubMed] [Google Scholar]
- 11.Faes L, Liu X, Wagner SK, Fu DJ, Balaskas K, Sim DA, et al. A clinician's guide to artificial intelligence: How to critically appraise machine learning studies. Transl Vis Sci Technol. 2020;9:7. doi: 10.1167/tvst.9.2.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pacis DM, Subido ED, Jr, Bugtai NT. Trends in telemedicine utilizing artificial intelligence. AIP Conf Proc. 2018;13:1933. [Google Scholar]
- 13.Bohr A, Memarzadeh K. The rise of artificial intelligence in healthcare applications. Artif Intell Healthcare. 2020;10:25–60. doi: 10.1016/B978-0-12-818438-7.00002-2. [Google Scholar]
- 14.Xia X, Ma Y, Luo Y, Lu J. An online intelligent electronic medical record system via speech recognition? Int J Distrib Sens Netw. 2022;18:15–25. doi: 10.1177/15501329221134479. [Google Scholar]
- 15.Davis JL, Murray JF. Murray and Nadel's Textbook of Respiratory Medicine. Elsevier; 2016. History and physical examination; pp. 263–77.e2. doi: 10.1016/B978-1-4557-3383-5.00016-6. [Google Scholar]
- 16.Bhaskar S, Bradley S, Sakhamuri S, Moguilner S, Chattu VK, Pandya S, et al. Designing futuristic telemedicine using artificial intelligence and robotics in the COVID-19 era. Front Public Health. 2020;8:556789. doi: 10.3389/fpubh.2020.556789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mathews SC, McShea MJ, Hanley CL, Ravitz A, Labrique AB, Cohen AB. Digital health: A path to validation. NPJ Digit Med. 2019;2:38. doi: 10.1038/s41746-019-0111-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gerke S, Minssen T, Cohen G. Ethical and legal challenges of artificial intelligence-driven healthcare. Artif Intell Healthcare. 2020;10:295–336. [Google Scholar]
- 19.Grundy BL, Jones PK, Lovitt A. Telemedicine in critical care: Problems in design, implementation, assessment. Crit Care Med. 1982;10:471–5. doi: 10.1097/00003246-198207000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Douin DJ, Ward MJ, Lindsell CJ, Howell MP, Hough CL, Exline MC, et al. ICU bed utilization during the coronavirus disease 2019 pandemic in a multistate analysis-March to June 2020. Crit Care Explor. 2021;3:e0361. doi: 10.1097/CCE.0000000000000361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Armstrong RA, Kane AD, Cook TM. Outcomes from intensive care in patients with COVID-19: A systematic review and meta-analysis of observational studies. Anaesthesia. 2020;75:1340–9. doi: 10.1111/anae.15201. [DOI] [PubMed] [Google Scholar]
- 22.Society for Critical Care Medicine. Critical care statistics. [[Last accessed on 2023 Feb 10]]. Available from: https://www.sccm.org/communications/critical-carestatistics .
- 23.Becker CD, Fusaro MV, Al Aseri Z, Millerman K, Scurlock C. Effects of telemedicine ICU intervention on care standardization and patient outcomes: An observational study. Crit Care Explor. 2020;2:e0165. doi: 10.1097/CCE.0000000000000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fusaro MV, Becker C, Miller D, Hassan IF, Scurlock C. ICU telemedicine implementation and risk-adjusted mortality differences between daytime and nighttime coverage. Chest. 2021;159:1445–51. doi: 10.1016/j.chest.2020.10.055. [DOI] [PubMed] [Google Scholar]
- 25.Fusaro MV, Becker C, Scurlock C. Evaluating tele-ICU implementation based on observed and predicted ICU mortality: A systematic review and meta-analysis. Crit Care Med. 2019;47:501–7. doi: 10.1097/CCM.0000000000003627. [DOI] [PubMed] [Google Scholar]
- 26.Gupta S, Bag P, Dewan S, Huh SJ, Shirato H, Hashimoto S, et al. Extending Tele-ICU/E-ICU to rationalize antibiotic usage in coronary care unit in Indian scenario. 26th Annual Congress of the European Society of Intensive Care Medicine, 2013. Abstract [Google Scholar]
- 27.Fortis S, Sarrazin MV, Beck BF, Panos RJ, Reisinger HS. ICU telemedicine reduces interhospital ICU transfers in the veterans health administration. Chest. 2018;154:69–76. doi: 10.1016/j.chest.2018.04.021. [DOI] [PubMed] [Google Scholar]
- 28.Scalvini S, Glisenti F. Centenary of tele-electrocardiography and telephonocardiography – where are we today? J Telemed Telecare. 2005;11:325–30. doi: 10.1258/135763305774472051. [DOI] [PubMed] [Google Scholar]
- 29.McKinney SM, Sieniek M, Godbole V, Godwin J, Antropova A, Ashrafian H, et al. International evaluation of an AI system for breast cancer screening. Nature. 2020;577:89–94. doi: 10.1038/s41586-019-1799-6. [DOI] [PubMed] [Google Scholar]
- 30.Huh SJ, Shirato H, Hashimoto S, Shimizu S, Kim DY, Ahn YC, et al. An integrated service digital network (ISDN)-based international telecommunication between Samsung Medical Center and Hokkaido University using telecommunication helped radiotherapy planning and information system (THERAPIS) Radiother Oncol. 2000;56:121–3. doi: 10.1016/s0167-8140(00)00179-1. [DOI] [PubMed] [Google Scholar]
- 31.Bi WL, Hosny A, Schabath MB, Giger ML, Birkbak NJ, Mehrtash A, et al. Artificial intelligence in cancer imaging: Clinical challenges and applications. CA Cancer J Clin. 2019;69:127–57. doi: 10.3322/caac.21552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hubley S, Lynch SB, Schneck C, Thomas M, Shore J. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6:269–82. doi: 10.5498/wjp.v6.i2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Malhotra S, Chakrabarti S, Shah R. Telepsychiatry: Promise, potential, and challenges. Indian J Psychiatry. 2013;55:3–11. doi: 10.4103/0019-5545.105499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thenral M, Annamalai A. Challenges of building, deploying, and using AI-enabled telepsychiatry platforms for clinical practice among urban Indians: A qualitative study. Indian J Psychol Med. 2021;43:336–42. doi: 10.1177/0253717620973414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuriakose D, Xiao Z. Pathophysiology and treatment of stroke: Present status and future perspectives. Int J Mol Sci. 2020;21:7609. doi: 10.3390/ijms21207609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Demaerschalk BM, Berg J, Chong BW, Gross H, Nystrom K, Adeoye O, et al. American Telemedicine Association: Telestroke guidelines. Telemed J E Health. 2017;23:376–89. doi: 10.1089/tmj.2017.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ali F, Hamid U, Zaidat O, Bhatti D, Kalia JS. Role of artificial intelligence in TeleStroke: An overview. Front Neurol. 2020;11:559322. doi: 10.3389/fneur.2020.559322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vagal A, Wintermark M, Nael K, Bivard A, Parsons M, Grossman AW, et al. Automated CT perfusion imaging for acute ischemic stroke. Neurology. 2019;93:888. doi: 10.1212/WNL.0000000000008481. [DOI] [PubMed] [Google Scholar]
- 39.Nagel S, Sinha D, Day D, Reith W, Chapot R, Papanagiotou P, et al. e-ASPECTS software is non-inferior to neuroradiologists in applying the ASPECT score to computed tomography scans of acute ischemic stroke patients. Int J Stroke. 2017;12:615–22. doi: 10.1177/1747493016681020. [DOI] [PubMed] [Google Scholar]
- 40.Kauw F, Heit JJ, Martin BW, van Ommen F, Kappelle LJ, Velthuis BK, et al. Computed tomography perfusion data for acute ischemic stroke evaluation using rapid software: Pitfalls of automated postprocessing. J Comput Assist Tomogr. 2020;44:75–7. doi: 10.1097/RCT.0000000000000946. [DOI] [PubMed] [Google Scholar]
- 41.Implementation of AI technology to provide remote stroke care in the state of Gujarat, India. [[Last accessed on 2023 Feb 13]]. Available from: https://www.healthcareitnews.com/news/asia/medtronic-zydushospitals-facilitate-remote-stroke-care-using-ai .
- 42.Novara G, Checcucci E, Crestani A, Abrate A, Esperto F, Pavan N, et al. Telehealth in urology: A systematic review of the literature.How much can telemedicine be useful during and after the COVID-19 pandemic? Eur Urol. 2020;78:786–811. doi: 10.1016/j.eururo.2020.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim J, Gewertz B. Teleurology and digital health app in COVID-19 pandemic. Investig Clin Urol. 2020;61:333–4. doi: 10.4111/icu.2020.61.4.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shah M, Naik N, Somani BK, Hameed BMZ. Artificial intelligence (AI) in urology-Current use and future directions: An iTRUE study. Turk J Urol. 2020;46(Suppl 1):S27–39. doi: 10.5152/tud.2020.20117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Prostate Cancer Prediction Tool That Has Unmatched Accuracy. [[Last accessed on 2023 Feb 13]]. Available from: https://www.mountsinai.org/about/newsroom/2019/mount-sinai-and-usc-researchersdevelop-prostate-cancer-prediction-tool-that-has-unmatchedaccuracy .
- 46.Gameiro J, Branco T, Lopes JA. Artificial intelligence in acute kidney injury risk prediction. J Clin Med. 2020;9:678. doi: 10.3390/jcm9030678. [DOI] [PMC free article] [PubMed] [Google Scholar]