Abstract
Purpose:
Adolescent sexual minority males (ASMM) comprise a high-risk group that may benefit from expanded human immunodeficiency virus (HIV) and sexually transmitted disease (STD) prevention services. The purpose of this study was to estimate the prevalence of HIV and STD testing among ASMM from pooled high school Youth Risk Behavior Surveys (YRBSs).
Methods:
Data came from 26 YRBSs from 2005 to 2013, which included questions on sexual identity and/or sex of sexual contacts and questions on ever being tested for HIV and/or STDs. Multivariable logistic regression was used to identify factors independently associated with lifetime HIV testing among sexually experienced ASMM.
Results:
Overall, 3027 of 43,037 (6.3%, 95% confidence interval [CI]: 5.8%–6.8%) males were categorized as ASMM. Among 1229 sexually experienced ASMM, 413 (26.6%, 95% CI: 21.8%–31.4%) reported ever being tested for HIV, and among 571 ASMM who reported not using a condom during last intercourse, 192 (29.4%, 95% CI: 21.3%–37.6%) reported testing. A longer duration since first intercourse (≥3 vs. ≤1 year: adjusted prevalence ratio [aPR]: 1.6, 95% CI: 1.0–2.6) and recent intercourse (within the past 3 months vs. earlier: aPR: 2.2, 95% CI: 1.4–3.4) was associated with a higher adjusted prevalence of HIV testing. Sixty-four of 252 (30.2%, 95% CI: 20.0%–40.4%) sexually experienced ASMM reported ever being tested for STDs.
Conclusion:
Low levels of testing among sexually experienced ASMM, particularly those who reported sex without a condom at last intercourse, highlight the exigency of improving age-appropriate HIV and STD prevention services. Educating healthcare providers to better assess adolescent sexual histories is essential to increasing testing.
Keywords: adolescent sexual minority males, HIV testing, prevention services for adolescents, STD testing, young men who have sex with men
Introduction
ADOLESCENT AND YOUNG MEN WHO HAVE SEX WITH MEN (MSM) in the United States (US) are at high risk for acquiring sexually transmitted diseases (STDs), including human immunodeficiency virus (HIV).1 According to the Centers for Disease Control and Prevention (CDC), 72% of the estimated 12,200 incident HIV infections in 2010 among 13–24-year-olds were attributable to male–male sexual contact.2 Surveillance data reported by state and local STD control programs indicate that the rates of gonorrhea and chlamydia infections in 2013 were highest among 15–24-year-olds.3 Despite these epidemiological trends, limited information exists regarding HIV-related risk behaviors4–7 or the prevalence and correlates of testing8–11 among adolescent sexual minority males (ASMM) aged 13 to 19 years. In a recent study with 14–18-year-old gay and bisexual men, less than a third of 152 sexually experienced participants had ever been tested, and nearly half of them did not know where they could go to get tested.11 Although sexual experimentation during adolescence is normal, engaging in risky behaviors such as condomless intercourse12 may have undesired consequences such as HIV and/or STD acquisition.
ASMM may benefit from a variety of HIV and STD prevention resources. HIV testing is the cornerstone of almost all comprehensive risk reduction efforts. Besides being the portal to accessing treatment and support, knowledge of one’s positive serostatus could help decrease risk behaviors that facilitate onward transmission.13 Seronegative ASMM could be offered age-appropriate behavioral and/or biomedical interventions to help maintain their status. The US Preventive Services Task Force (USPSTF) recommends repeated screening of adolescents known to be at risk for HIV infection and those who actively engage in risky behaviors.14 CDC 2015 STD treatment guidelines recommend annual screening for gonorrhea, chlamydia, and syphilis for sexually active MSM of all ages.15 The American Academy of Pediatrics recommends repeat annual office-based HIV testing for high-risk adolescents16 and testing for gonorrhea and chlamydia in adolescent and young MSM who had insertive or receptive anal intercourse during the preceding year.17
Since 1990, the Youth Risk Behavior Surveillance System has monitored health-related behaviors that contribute to leading causes of mortality, disability, and social problems among US adolescents.18 One component of this system is the high school Youth Risk Behavior Survey (YRBS) conducted among students in grades 9 through 12. Although a question on lifetime HIV testing history was added to the national YRBS in 2005, respondents are not currently asked about testing for other STDs.19 Questions on sexual identity or the sex of sexual contacts were not added to the national YRBS questionnaire until 2015, precluding the calculation of national estimates for HIV testing prevalence among ASMM. However, in recent years, some state and district YRBSs have included these questions, in addition to asking respondents about previous testing for HIV and/or STDs, and represent the sources of data for this article.
Our primary objective was to estimate the prevalence of self-reported lifetime HIV testing among ASMM in a pooled dataset of high school students from selected jurisdictions in the US. In addition, we sought to identify demographic and behavioral characteristics independently associated with ever HIV testing among ASMM who reported previously having sexual intercourse. A secondary objective was to estimate the prevalence of self-reported lifetime STD testing among ASMM in a pooled dataset of selected YRBSs. Given the unavailability of such estimates from large samples across diverse geographic settings, our results could serve as useful baseline data against which future testing trends may be evaluated and provide parameter estimates for in-depth studies of HIV and STD prevention strategies among ASMM.
Methods
Data sources and pooling
Data for this study came from 26 state and district high school YRBSs conducted between 2005 and 2013, which included questions on sexual identity and/or sex of sexual contacts, as well as questions on respondents’ lifetime history of testing for HIV and/or STDs. Some datasets were provided to us directly by the CDC and others were provided to us by YRBS site coordinators after reviewing and approving our formal data requests. Data requests began in February 2015 and were concluded in July 2015. The Emory University IRB determined that this project did not require IRB review.
SUDAAN version 11.0 (RTI International, Research Triangle Park, NC) and survey procedures in SAS version 9.3 (SAS Institute Inc., Cary, NC) were used for these analyses to account for the complex sampling design of YRBS.20 Datasets from multiple jurisdictions and years were pooled to formulate different subset combinations based on variable availability, in accordance with CDC best practices.21
ASMM and testing outcome definitions
ASMM were defined as males (self-reported sex on YRBS) in grades 9 through 12 who identified as gay or bisexual and/or reported lifetime sexual contact with males or both males and females. Under this inclusive definition, heterosexual (straight)-identifying male students, those who reported being unsure of their sexual identity, and those with missing data for this variable were also categorized as ASMM if they reported previous sexual contact with males or both sexes. For our main analyses, we used an outcome definition of lifetime testing for HIV derived from the question, “Have you ever been tested for HIV, the virus that causes AIDS? (Do not count tests done if you donated blood.).” For secondary analyses, we used an outcome definition of lifetime testing for STDs derived from the question, “Have you ever been tested for other STDs such as genital herpes, chlamydia, syphilis, or genital warts?” Data availability by jurisdiction year is presented in Table 1.
Table 1.
Data Availability for ASMM and Outcome Categorizations in Selected State and District High School YRBSs from 2005 to 2013
| Jurisdiction | Year | Variables for ASMMa categorizations | Variables for outcomeb categorizations | ||
|---|---|---|---|---|---|
| Sexual identityc | Sex of sexual contactsd | Ever tested for HIVe | Ever tested for STDsf | ||
| Chicago, IL | 2013 | ✓ | ✓ | ✓ | |
| Connecticut | 2007 | ✓ | ✓ | ||
| 2009 | ✓ | ✓ | |||
| 2011 | ✓ | ✓ | ✓ | ||
| 2013 | ✓ | ✓ | ✓ | ||
| Duval County, FL | 2013 | ✓ | ✓ | ||
| Hawaii | 2013 | ✓ | ✓ | ✓ | |
| Houston, TX | 2013 | ✓ | ✓ | ✓ | |
| Los Angeles, CA | 2011 | ✓ | ✓ | ✓ | |
| 2013 | ✓ | ✓ | ✓ | ||
| Massachusettsg | 2005 | ✓ | ✓ | ✓ | ✓ |
| 2007 | ✓ | ✓ | ✓ | ✓ | |
| 2009 | ✓ | ✓ | ✓ | ✓ | |
| 2011 | ✓ | ✓ | ✓ | ✓ | |
| 2013 | ✓ | ✓ | ✓ | ✓ | |
| Memphis, TN | 2013 | ✓ | ✓ | ✓ | |
| Michigan | 2013 | ✓ | ✓ | ✓ | |
| New Jersey | 2013 | ✓ | ✓ | ✓ | |
| New York City, NY | 2009 | ✓ | ✓ | ✓ | |
| 2011 | ✓ | ✓ | ✓ | ||
| 2013 | ✓ | ✓ | ✓ | ||
| North Carolina | 2013 | ✓ | ✓ | ✓ | |
| Orange County, FL | 2013 | ✓ | ✓ | ✓ | |
| Palm Beach, FL | 2013 | ✓ | ✓ | ✓ | |
| San Diego, CA | 2013 | ✓ | ✓ | ✓ | |
| Vermont | 2011 | ✓ | ✓ | ✓ | |
Despite containing relevant survey questions, Baltimore, MD, Detroit, MI, Philadelphia, PA, and Washington, D.C., were not included in our analyses because we did not have access to their data at the time of drafting this article. Although the 2009 high school YRBS in Vermont, the 2009–2011 surveys in Seattle, WA, and the 2013 survey in San Francisco, CA, collected information for ASMM categorization and regarding ever testing for HIV, we did not consider these datasets as they lacked information on relevant sexual behavior characteristics. The 2007–2013 high school YRBSs in Boston, MA, collected relevant information, but we excluded these data in favor of larger samples from Massachusetts as combining potentially overlapping samples was deemed inappropriate with respect to weighting. Although the 2009–2013 surveys in North Dakota collected information for ASMM categorization, we did not include these datasets because we were unable to separate information about lifetime HIV and STD testing from their composite question: “Have you ever been tested for a STD, including HIV, the virus that causes AIDS?” Response options: “Yes”; “No”; and “Not sure.”
ASMM for the main analyses were defined as males in grades 9 through 12 who identified as gay or bisexual and/or reported lifetime sexual contact with males or both males and females.
Outcome for the main analyses was defined as lifetime testing for HIV. Outcome for the secondary analyses was defined as lifetime testing for STDs.
High school YRBS question: “Which of the following best describes you?” Response options: “Heterosexual (straight)”; “Gay or lesbian”; “Bisexual”; “and Not sure.”
High school YRBS question: “During your life, with whom have you had sexual contact?” Response options: “I have never had sexual contact”; “Females”; “Males”; and “Females and males.”
High school YRBS question: “Have you ever been tested for HIV, the virus that causes AIDS? (Do not count tests done if you donated blood.).” Response options: “Yes”; “No”; and “Not sure.”
High school YRBS question: “Have you ever been tested for other STDs such as genital herpes, chlamydia, syphilis, or genital warts?” Response options: “Yes”; “No”; and “Not sure.”
High school YRBS question in 2005: “Have you ever been tested for HIV infection or other STDs such as genital herpes, chlamydia, syphilis, or genital warts?” Response options: “No, I have never been tested for HIV or other STDs”; “Yes, I have been tested for HIV”; “Yes, I have been tested for other STDs”; and “Yes, I have been tested for both HIV and for other STDs.”
ASMM, adolescent sexual minority males; HIV, human immunodeficiency virus; STD, sexually transmitted disease; YRBS, Youth Risk Behavior Survey.
Statistical analyses
The pooled dataset for our main analyses, which focused on lifetime HIV testing, included 26 jurisdiction years. First, we estimated the proportion of males who were categorized as ASMM, followed by the prevalence of testing in this group. We then compared the prevalence of lifetime HIV testing between ASMM and non-ASMM using the Rao–Scott design-adjusted chi-square test in the overall sample, in the subgroup that reported previously having sexual intercourse (sexually experienced), and in the subgroup that reported never having intercourse (sexually inexperienced). Because not all jurisdictions specifically asked the question, “Have you ever had sexual intercourse?” we used responses from “How old were you when you had sexual intercourse for the first time?” which included an option for never having engaged in intercourse to categorize ASMM self-reported sexual history.
Next, the prevalence of lifetime HIV testing was estimated within strata of age, grade, and race/ethnicity for all ASMM and among those who were sexually experienced. For the latter subgroup, we also estimated testing prevalence within categories of time since first intercourse, number of lifetime sexual contacts, condom use by respondent or his partner during last intercourse, alcohol or drug use before last intercourse, and recent sexual activity. Time since first sexual intercourse was derived by subtracting respondents’ self-reported age at first intercourse from their current age.
Finally, bivariate analyses were conducted to examine the unadjusted associations of selected characteristics with lifetime HIV testing among sexually experienced ASMM, followed by multivariable logistic regression. We estimated crude and adjusted prevalence ratios (PRs), with corresponding 95% confidence intervals (CIs), using predicted marginal probabilities because odds ratio estimates for nonrare outcomes in cross-sectional studies are comparatively inflated. Age was not considered for inclusion in the multivariable model because of its correlation with grade, but grade and race/ethnicity were forced into the model a priori. Potential explanatory sexual behavior variables were added in a stepwise manner and retained if their association with lifetime HIV testing was statistically significant at an alpha level of 0.05. Variables in the final model were assessed for collinearity issues.
Secondary analyses were performed on a pooled dataset of 6 jurisdiction years to estimate the prevalence of lifetime STD testing, overall and among sexually experienced ASMM. These data were not stratified by demographic or behavioral characteristics because of the small number of participants. In addition, we conducted sensitivity analyses to examine heterogeneity of our findings based on alternative definitions for ASMM. Lifetime HIV and STD testing prevalence was separately estimated for ASMM categorized either solely on the basis of their sexual identity or depending upon the sex of their sexual contacts.
Results
Statistics presented in the following sections and in the descriptive tables represent unweighted frequencies and weighted percentages. Using our inclusive definition, 3027 of 43,037 (6.3%, 95% CI: 5.8%–6.8%) males in the pooled dataset of 26 jurisdiction years for our main analyses were categorized as ASMM. Overall, 700 of 2596 (23.5%, 95% CI: 20.3%–26.6%) ASMM who provided data on lifetime HIV testing reported ever being tested for HIV, which was approximately twice as high as 5075 of 36,381 (11.9%, 95% CI: 11.2%–12.6%) males not categorized as ASMM; Rao–Scott chi-square P < 0.01. Among 1229 sexually experienced ASMM, 413 (26.6%, 95% CI: 21.8%–31.4%) reported lifetime testing for HIV, which was significantly greater than 2859 of 13,564 (17.7%, 95% CI: 16.4%–19.0%) sexually experienced non-ASMM; Rao–Scott chi-square P < 0.01. However, the prevalence of lifetime HIV testing among those who were sexually inexperienced was almost identical for both groups: 51 of 612 (5.6%, 95% CI: 2.5%–8.8%) among ASMM and 1227 of 18,866 (5.3%, 95% CI: 4.7%–5.9%) among non-ASMM. Additional details, including missing frequencies for lifetime HIV testing and history of sexual intercourse, are presented in Figure 1.
FIG. 1.
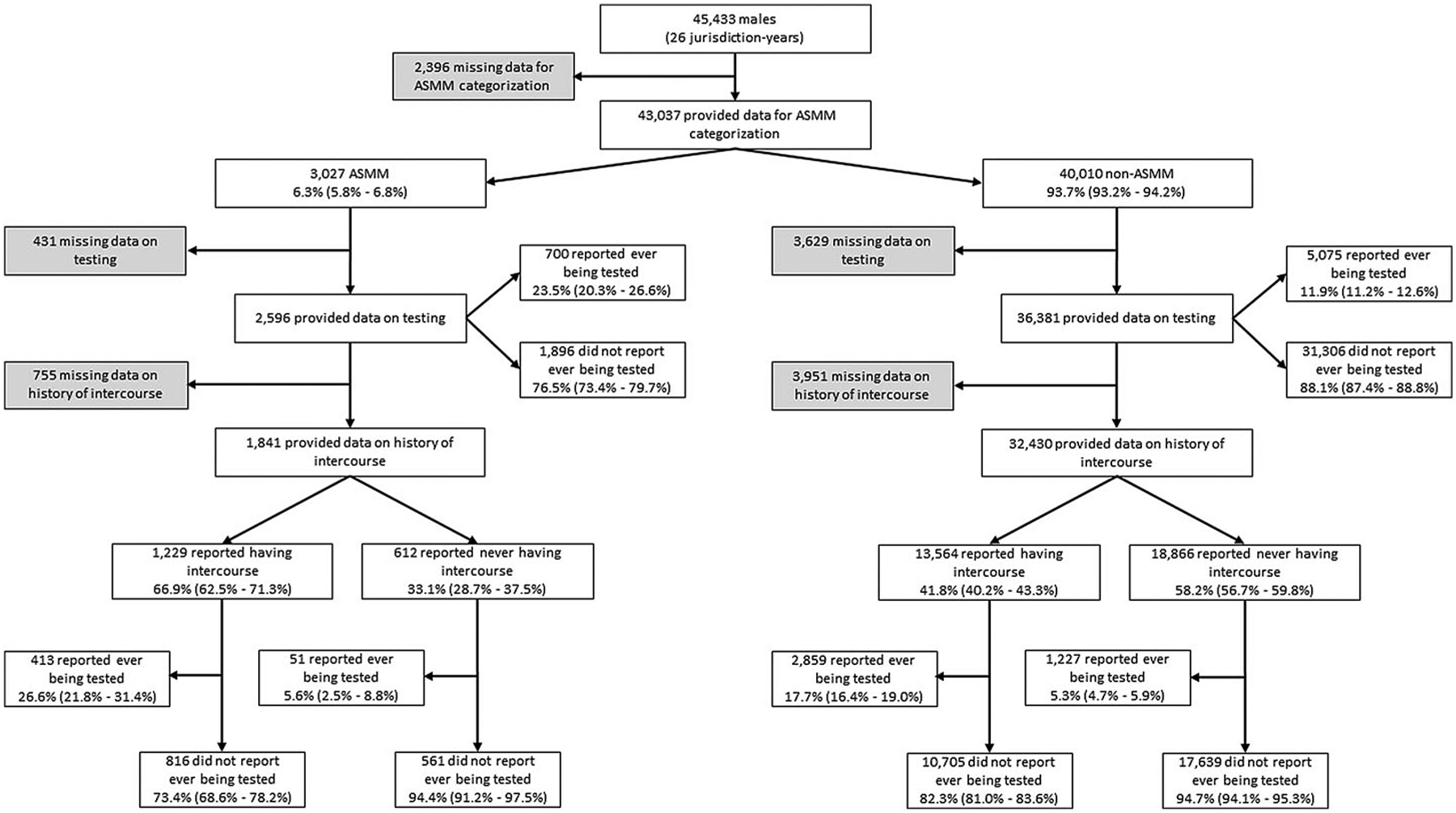
Lifetime HIV testing prevalence among ASMM and non-ASMM, overall and stratified by history of sexual intercourse, pooled high school YRBS state and district data from selected surveys from 2005 to 2013. ASMM, adolescent sexual minority males; YRBS, Youth Risk Behavior Survey.
Table 2 summarizes lifetime HIV testing behavior within strata of selected demographic characteristics among 2596 ASMM overall and in the subgroup of 1229 sexually experienced ASMM. Non-Hispanic black students had a higher prevalence of self-reported HIV testing compared with other racial/ethnic groups in the overall sample, but this result was not observed in the sexually experienced subgroup. HIV testing history stratified by selected sexual behavior characteristics among 1229 sexually experienced ASMM is presented in Table 3. Despite being low, testing prevalence increased with longer durations since first intercourse and greater numbers of lifetime sexual contacts. Less than a third of 571 (29.4%, 95% CI: 21.3%–37.6%) ASMM who reported that either they or their partner did not use a condom during last sexual intercourse reported ever being tested for HIV. Finally, the testing prevalence among ASMM who reported having sexual intercourse within the past 3 months was more than twice as high compared with those who did not report recent intercourse (32.0% compared with 15.0%, respectively, Rao–Scott chi-square P < 0.01).
Table 2.
Lifetime HIV Testing Behavior Among ASMM Within Strata of Selected Demographic Characteristics, Pooled High School YRBS State and District Data from Selected Surveys from 2005 to 2013
| ASMMa characteristic | Overall sample | Subgroup that reported previously having sexual intercourse | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Nb | n testedb | Weighted % testedc | (95% Cl)c | Pd | Nb | n testedb | Weighted % testedc | (95% Cl)c | Pd | |
| Age (years) | ||||||||||
| 14 or younger | 361 | 86 | 18.8 | (12.0–25.6) | 0.05 | 129 | 38 | 27.4 | (13.5–41.3) | 0.66 |
| 15 | 554 | 129 | 17.9 | (13.0–22.9) | 224 | 65 | 23.2 | (14.7–31.7) | ||
| 16 | 652 | 165 | 20.6 | (14.1–27.1) | 312 | 106 | 21.8 | (12.7–30.9) | ||
| 17 | 644 | 196 | 28.6 | (21.4–35.7) | 337 | 122 | 30.7 | (20.6–40.9) | ||
| 18 or older | 381 | 124 | 29.5 | (20.3–38.6) | 225 | 82 | 29.2 | (17.5–41.0) | ||
| Grade | ||||||||||
| 9 | 584 | 146 | 21.4 | (15.5–27.3) | 0.60 | 227 | 75 | 26.2 | (17.1–35.3) | 0.88 |
| 10 | 617 | 139 | 20.2 | (12.9–27.6) | 269 | 76 | 23.3 | (10.9–35.7) | ||
| 11 | 651 | 185 | 26.1 | (17.9–34.3) | 319 | 119 | 29.4 | (19.2–39.7) | ||
| 12 | 676 | 205 | 25.6 | (18.9–32.3) | 382 | 133 | 27.6 | (18.7–36.5) | ||
| Race/Ethnicity | ||||||||||
| White, non-Hispanic | 784 | 147 | 15.8 | (11.8–19.9) | <0.01 | 387 | 98 | 21.0 | (13.6–28.4) | 0.28 |
| Black, non-Hispanic | 437 | 151 | 34.9 | (24.9–44.9) | 212 | 89 | 32.1 | (20.9–43.3) | ||
| Hispanic/Latino | 840 | 255 | 24.0 | (18.2–29.9) | 413 | 163 | 29.8 | (20.5–39.2) | ||
| Othere | 413 | 100 | 30.9 | (18.9–42.8) | 177 | 52 | 33.0 | (12.8–53.1) | ||
| Total | 2596 | 700 | 23.5 | (20.3–26.6) | 1229 | 413 | 26.6 | (21.8–31.4) | ||
Pooled high school YRBS state and district data from the following jurisdictions and years: Chicago, IL (2013); Connecticut (2007, 2009, 2011, 2013); Duval County, FL (2013); Hawaii (2013); Houston, TX (2013); Los Angeles, CA (2011, 2013); Massachusetts (2005, 2007, 2009, 2011, 2013); Memphis, TN (2013); Michigan (2013); New Jersey (2013); New York City, NY (2009, 2011, 2013); North Carolina (2013); Orange County, FL (2013); Palm Beach, FL (2013); San Diego, CA (2013); and Vermont (2011).
ASMM defined as males in grades 9 through 12 who identified as gay or bisexual and/or reported lifetime sexual contact with males or both males and females.
Unweighted frequencies. Numbers may not add to total because of missing data.
Weighted percentages (%) and 95% CIs.
P-values from Rao–Scott design-adjusted chi-square test.
Other includes 171 Asian (34 reported testing, 36.2%, 95% CI: 17.6%–54.8%), 72 Native Hawaiian/other Pacific Islander (18 reported testing, 24.5%, 95% CI: 10.1%–38.9%), 41 American Indian/Alaska Native (9 reported testing, 17.3%, 95% CI, 0.0%–34.9%), and 129 multiple races, non-Hispanic (39 reported testing, 27.6%, 95% CI: 12.0%–43.2%) in the overall sample, and 68 Asian (18 reported testing, 42.0%, 95% CI: 8.7%–75.3%), 32 Native Hawaiian/other Pacific Islander (10 reported testing, 21.6%, 95% CI: 2.9%–40.3%), 18 American Indian/Alaska Native (3 reported testing, 8.3%, 95% CI: 0.0%–20.3%), and 59 multiple races, non-Hispanic (21 reported testing, 26.5%, 95% CI: 10.6%–42.3%) in the subgroup that reported previously having sexual intercourse.
CIs, confidence intervals.
Table 3.
Lifetime HIV Testing Behavior Among 1229 ASMM Who Reported Previously Having Sexual Intercourse Within Strata of Selected Behavioral Characteristics, Pooled High School YRBS State and District Data from Selected Surveys from 2005 to 2013
| ASMMa characteristic | Nb | n testedb | Weighted % testedc | (95% CI)c | Pd |
|---|---|---|---|---|---|
| Time since first sexual intercourse | |||||
| Less than or equal to 1 year | 436 | 113 | 19.9 | (13.5–26.3) | 0.07 |
| 2 years | 238 | 94 | 25.4 | (16.5–34.3) | |
| 3 or more years | 553 | 206 | 32.2 | (23.2–41.2) | |
| Number of lifetime sexual contacts | |||||
| 1 person | 338 | 73 | 16.5 | (10.8–22.2) | 0.01 |
| 2 people | 211 | 66 | 27.2 | (16.4–37.9) | |
| 3 or more people | 648 | 261 | 31.4 | (23.9–38.9) | |
| Condom use by respondent or partner during last sexual intercourse | |||||
| Yes | 594 | 198 | 24.5 | (17.9–31.0) | 0.38 |
| No | 571 | 192 | 29.4 | (21.3–37.6) | |
| Alcohol or drug use before last sexual intercourse | |||||
| Yes | 355 | 126 | 33.6 | (23.0–44.1) | 0.10 |
| No | 849 | 282 | 24.4 | (19.3–29.4) | |
| Sexual intercourse with at least one person | |||||
| More than 3 months ago | 378 | 88 | 15.0 | (9.5–20.6) | <0.01 |
| Within the past 3 months | 824 | 315 | 32.0 | (25.2–38.8) | |
Pooled high school YRBS state and district data from the following jurisdictions and years: Chicago, IL (2013); Connecticut (2007, 2009, 2011, 2013); Duval County, FL (2013); Hawaii (2013); Houston, TX (2013); Los Angeles, CA (2011, 2013); Massachusetts (2005, 2007, 2009, 2011, 2013); Memphis, TN (2013); Michigan (2013); New Jersey (2013); New York City, NY (2009, 2011, 2013); North Carolina (2013); Orange County, FL (2013); Palm Beach, FL (2013); San Diego, CA (2013); and Vermont (2011).
ASMM defined as males in grades 9 through 12 who identified as gay or bisexual and/or reported lifetime sexual contact with males or both males and females.
Unweighted frequencies. Numbers may not add to total because of missing data.
Weighted percentages (%) and 95% CIs.
P-values from Rao–Scott design-adjusted chi-square test.
Table 4 presents results from the bivariate and multivariable analyses of factors potentially associated with lifetime HIV testing among sexually experienced ASMM. The final multivariable model used 1133 of 1229 observations that were not missing data on any of the explanatory variables of interest and we did not detect any issues with collinearity. A longer duration since first intercourse (3 or more years vs. less than or equal to 1 year) was independently associated with a higher prevalence of testing. ASMM who reported having intercourse within the past 3 months were significantly more likely to report ever being tested compared with those who did not have recent intercourse. Number of lifetime sexual contacts, condom use by respondent or his partner during last sexual intercourse, and alcohol or drug use before last intercourse were not retained in the model as they met the 0.05 significance level for removal. Grade and race/ethnicity were not associated with HIV testing history among sexually experienced ASMM in the adjusted analyses.
Table 4.
Demographic and Behavioral Characteristics Associated with Lifetime HIV Testing Among ASMM Who Reported Previously Having Sexual Intercourse, Pooled High School YRBS State and District Data from Selected Surveys from 2005 to 2013
| Crude associations | Adjusted associations | |||
|---|---|---|---|---|
| ASMMa characteristic | cPRb | (95% CI)c | aPRd | (95% CI)c |
| Grade | ||||
| 9 | Ref. | Ref. | ||
| 10 | 0.9 | (0.5–1.7) | 0.9 | (0.5–1.6) |
| 11 | 1.1 | (0.7–1.8) | 1.1 | (0.7–1.8) |
| 12 | 1.1 | (0.7–1.7) | 1.0 | (0.6–1.6) |
| Race/Ethnicity | ||||
| White, non-Hispanic | Ref. | Ref. | ||
| Black, non-Hispanic | 1.5 | (0.9–2.5) | 1.5 | (0.9–2.6) |
| Hispanic/Latino | 1.4 | (0.9–2.3) | 1.5 | (1.0–2.4) |
| Othere | 1.6 | (0.7–3.3) | 1.5 | (0.7–2.8) |
| Time since first sexual intercourse | ||||
| Less than or equal to 1 year | Ref. | Ref. | ||
| 2 years | 1.3 | (0.8–2.0) | 1.2 | (0.7–1.9) |
| 3 or more years | 1.6 | (1.1–2.5) | 1.6 | (1.0f–2.6) |
| Number of lifetime sexual contacts | — | |||
| 1 person | Ref. | |||
| 2 people | 1.7 | (1.0–2.8) | ||
| 3 or more people | 1.9 | (1.3–2.9) | ||
| Condom use by respondent or partner during last sexual intercourse | — | |||
| Yes | Ref. | |||
| No | 1.2 | (0.8–1.8) | ||
| Alcohol or drug use before last sexual intercourse | — | |||
| Yes | Ref. | |||
| No | 0.7 | (0.5–1.1) | ||
| Sexual intercourse with at least one person | ||||
| More than 3 months ago | Ref. | Ref. | ||
| Within the past 3 months | 2.1 | (1.4–3.3) | 2.2 | (1.4–3.4) |
Pooled high school YRBS state and district data from the following jurisdictions and years: Chicago, IL (2013); Connecticut (2007, 2009, 2011, 2013); Duval County, FL (2013); Hawaii (2013); Houston, TX (2013); Los Angeles, CA (2011, 2013); Massachusetts (2005, 2007, 2009, 2011, 2013); Memphis, TN (2013); Michigan (2013); New Jersey (2013); New York City, NY (2009, 2011, 2013); North Carolina (2013); Orange County, FL (2013); Palm Beach, FL (2013); San Diego, CA (2013); and Vermont (2011). Results in bold indicate a statistically significant association (P < 0.05).
ASMM defined as males in grades 9 through 12 who identified as gay or bisexual and/or reported lifetime sexual contact with males or both males and females.
Crude prevalence ratio (cPR).
95% CIs accounting for YRBS complex survey design.
Adjusted prevalence ratio (aPR).
Other includes Asian, Native Hawaiian/other Pacific Islander, American Indian/Alaska Native, and multiple races, non-Hispanic.
Result was statistically significant. Lower limit of the 95% CI rounded down from 1.04 to 1.0.
Secondary analyses on a subset of 6 jurisdiction years (5 from Massachusetts and 1 from New Jersey) revealed that 92 of 465 (23.9%, 95% CI: 17.8%–29.9%) ASMM overall and 64 of 252 (30.2%, 95% CI: 20.0%–40.4%) sexually experienced ASMM reported ever being tested for STDs. Sixty-five of 92 (73.3%, 95% CI: 54.6%–92.0%) ASMM who reported lifetime HIV testing had also been tested for STDs, and 50 of 69 (72.4%, 95% CI: 52.0%–92.7%) sexually experienced ASMM who reported lifetime HIV testing had also been tested for STDs. Results from sensitivity analyses performed on different jurisdiction–year combinations, formulated based on data availability for either sexual identity or for the sex of sexual contacts, are presented in Tables 5 (overall samples) and 6 (sexually experienced subgroups). In the pooled datasets for estimating lifetime HIV testing prevalence, we found that 4.2% (95% CI: 3.9%–4.6%) of males identified as gay or bisexual and 4.6% (95% CI: 4.2%–5.1%) reported lifetime sexual contact with males or both sexes. Using a definition based solely on sexual identity, 24.2% (95% CI:18.8%–29.5%) of sexually experienced ASMM reported ever being tested for HIV. Defining ASMM based solely on the sex of their sexual contacts, 27.3% (95% CI: 22.0%–32.6%) reported lifetime HIV testing.
Table 5.
Lifetime HIV and STD Testing Behavior Among ASMM, Pooled High School YRBS State and District Data from Selected Surveys from 2005 to 2013
| Definitions | (1) Reported ever being tested for HIV | (2) Reported ever being tested for STDs |
|---|---|---|
| (1) Identified as gay or bisexual and/or reported lifetime sexual contact with males or both males and females | 26 jurisdiction years a | 6 jurisdiction years b |
| 3027 ASMM/43,037 males 6.3% (5.8%–6.8%) | 489 ASMM/8053 males 5.5% (4.6%–6.4%) | |
| 700/2596 ASMM reported testing 23.5% (20.3%–26.6%) | 92/465 ASMM reported testing 23.9% (17.8%–29.9%) | |
| (2) Identified as gay or bisexual | 23 jurisdiction years c | 5 jurisdiction years d |
| 1886 ASMM/39,669 males 4.2% (3.9%–4.6%) | 263 ASMM/7259 males 3.5% (3.1%–4.0%) | |
| 431/1618 ASMM reported testing 20.3% (16.7%–23.9%) | 51/248 ASMM reported testing 20.0% (14.6%–25.4%) | |
| (3) Reported lifetime sexual contact with males or both males and females | 25 jurisdiction years e | 6 jurisdiction years f |
| 1963 ASMM/40,181 males 4.6% (4.2%–5.1%) | 374 ASMM/7845 males 4.9% (4.0%–5.8%) | |
| 506/1706 ASMM reported testing 26.1% (21.9%–30.2%) | 80/360 ASMM reported testing 25.5% (18.7%–32.4%) |
Pooled high school YRBS state and district data from the following jurisdictions and years: Chicago, IL (2013); Connecticut (2007, 2009, 2011, 2013); Duval County, FL (2013); Hawaii (2013); Houston, TX (2013); Los Angeles, CA (2011, 2013); Massachusetts (2005, 2007, 2009, 2011, 2013); Memphis, TN (2013); Michigan (2013); New Jersey (2013); New York City, NY (2009, 2011, 2013); North Carolina (2013); Orange County, FL (2013); Palm Beach, FL (2013); San Diego, CA (2013); and Vermont (2011).
Pooled high school YRBS state and district data from the following jurisdictions and years: Massachusetts (2005, 2007, 2009, 2011, 2013); New Jersey (2013).
Pooled high school YRBS state and district data from a EXCEPT: Connecticut (2007, 2009); New Jersey (2013).
Pooled high school YRBS state and district data from the following jurisdictions and years: Massachusetts (2005, 2007, 2009, 2011, 2013).
Pooled high school YRBS state and district data from a EXCEPT: Duval County, FL (2013).
Pooled high school YRBS state and district data from the following jurisdictions and years: Massachusetts (2005, 2007, 2009, 2011, 2013); New Jersey (2013).
Discussion
ASMM in the US face substantial risks of HIV and STD infections. Less than a quarter of all ASMM in our study and less than a third of sexually experienced ASMM reported ever being tested for either HIV or STDs. The prevalence of lifetime HIV testing among ASMM who did not use a condom during last sexual intercourse was low despite the CDC recommendation of at least annual testing for this risk group.22 National estimates indicate that 62%, 66%, and 71% of adult MSM in 2008, 2011, and 2014, respectively, had been tested for HIV in the previous 12 months.23 Our results highlight the exigency for improving HIV/STD prevention services for adolescent males at highest risk.
Sexual minority youth have unique needs and may experience developmental challenges that could influence HIV/STD testing uptake.24 Research suggests that a lack of frank communication between providers and younger patients concerning sexual risk behaviors could be a reason for low levels of testing.25,26 Other potential barriers include fear of being outed as gay or bisexual for inquiring about or seeking prevention services, denial of risk factors, and lack of knowledge about testing locations.5,11,27 Furthermore, adolescents might not be aware that they can consent to HIV/STD testing without parental permission.28 Our finding of greater lifetime HIV testing prevalence among sexually experienced ASMM compared with non-ASMM is encouraging. This may indicate a higher awareness about HIV-related exposures and risk behaviors among ASMM or their healthcare providers in the represented jurisdictions.
However, it is disconcerting that more than two-thirds of ASMM who engaged in condomless sex at last intercourse did not report ever being tested for HIV; only 26.6% of 1229 sexually experienced ASMM reported ever being tested. Our finding is similar to that from a recent smaller study in which 30.3% of 152 sexually experienced gay and bisexual men aged 14–18 years had ever been tested.11 Although HIV testing prevalence in our pooled dataset is lower than historically documented estimates for young MSM,7,10 those studies recruited from public venues, such as bars, dance clubs, and bathhouses, and their results are not directly comparable with our findings from a more general high school-based setting. We are not aware of published estimates for STD testing prevalence among ASMM. Given that only 30.2% of sexually experienced ASMM in our study reported ever being tested for STDs, we believe that current practices are falling short of targeting those who are the most vulnerable.
Although sexually inexperienced ASMM and non-ASMM reported low levels of lifetime HIV testing, the prevalence in these groups was similar (between 5% and 6%). This might suggest that providers may not be adequately assessing adolescent sexual histories or entirely trusting the information provided to them by adolescents. It may also suggest that providers could be using age as the sole indicator for HIV testing in healthcare settings, highlighting the need to refine population-based testing guidelines for adolescents to better focus limited testing funds on those with potential exposure to HIV.
Race/ethnicity was not associated with HIV testing history among sexually experienced ASMM in our multivariable analysis. This parallels findings from studies among adolescent and adult MSM in the US over the past two decades.29–31 Our result might reflect a gradual increase in HIV testing specifically among black, non-Hispanic sexual minority youth (but not those of other race/ethnicities) during a similar time period.29 Indeed, the prevalence of lifetime HIV testing among black non-Hispanic ASMM in our overall sample was higher than any other racial/ethnic group. This is reassuring in light of racial health disparities experienced by black MSM of all ages.32 Given the disproportionate burden of HIV and the lack of serostatus awareness among young black MSM,33 it is important to continue supporting testing services in this population. Our result that a duration of 3 or more years since first sexual intercourse was positively associated with lifetime HIV testing is not unexpected and can likely be attributed to a greater opportunity to access prevention resources during the longer period following sexual debut.
Strengths of our study include utilizing data from population-based YRBS samples rather than convenience samples and generating estimates of HIV and STD testing behaviors in a large diverse group of ASMM, which could serve as baseline measures against which to evaluate future trends. Although we recognize that the sexual identity and behavioral dimensions we used to categorize ASMM are not conceptually equivalent, we elected to define a composite measure to allow for the inclusion of as many sexually experienced ASMM as possible, a subgroup at potentially high risk. Unfortunately, not all jurisdictions included questions on both sexual identity and sex of sexual contacts of high school students. However, sensitivity analyses using separate ASMM categorizations revealed a similar prevalence of testing among sexually experienced males identifying as gay or bisexual and among males who reported lifetime sexual contact with males or both sexes.
Our study is not without limitations. Caution should be exercised in generalizing results beyond the included jurisdictions and to ASMM who are not enrolled in school. Given that we only used YRBSs that collected information on sexual identity and/or sex of sexual contacts, our data likely came from more progressive jurisdictions. Secondary analyses to estimate the prevalence of lifetime STD testing only included data from Massachusetts (5 jurisdiction years) and New Jersey (1 jurisdiction year). Although jurisdictions can choose to modify the standard YRBS questionnaire by including optional questions provided by the CDC, many jurisdictions did not prioritize asking about lifetime STD testing. Because these data are self-reported, there exists a possibility for misclassification of testing histories and sexual behavior characteristics, but the quality of information provided by YRBSs is widely believed to be reliable.12 Due to the lack of information about timing or frequency of HIV testing, we are unable to comment on testing patterns. Finally, although physically forced sexual intercourse has been associated with higher HIV testing among adolescents in the US,34 we did not include this variable as many YRBSs did not ask this question. Upon investigating in a combined dataset of 20 jurisdiction years with available data, we did not find a higher prevalence of lifetime HIV testing among ASMM who reported ever being physically forced to have sexual intercourse.
Conclusion
Our work informs an important research gap in the current knowledge of HIV and STD testing prevalence among ASMM. Low levels of HIV testing among ASMM in the represented jurisdictions, especially among those who did not use a condom during last intercourse, reflect a systematic failure to target those at increased risk as part of comprehensive prevention efforts. Given the recent inclusion of questions on sexual identity and sex of sexual contacts in the national high school YRBS (since 2015),19 lifetime HIV testing estimates from a nationally representative sample of ASMM in grades 9 through 12 who attend public and private schools are hopefully forthcoming. Educating high school students about HIV and STD prevention, including providing information that they can consent to testing without parental permission, could set the stage for lifelong protection among all youth, including those at highest risk for infection. Educating healthcare providers to better assess adolescent sexual histories is essential to increasing the efficiency of HIV and STD testing. Multiple, innovative, and age-appropriate strategies are needed to ensure that ASMM who engage in condomless intercourse get tested for HIV at least annually.
Table 6.
Lifetime HIV and STD Testing Behavior Among ASMM Who Reported Previously Having Sexual Intercourse, Pooled High School YRBS State and District Data from Selected Surveys from 2005 to 2013
| Definitions | (1) Reported ever being tested for HIV | (2) Reported ever being tested for STDs |
|---|---|---|
| (1) Identified as gay or bisexual and/or reported lifetime sexual contact with males or both males and females | 26 jurisdiction years a | 6 jurisdiction years b |
| 1401/2067 ASMM reported having sexual intercourse 67.8% (63.6%–72.0%) | 264/382 ASMM reported having sexual intercourse 75.1% (68.1%–82.1%) | |
| 413/1229 reported testing 26.6% (21.8%–31.4%) | 64/252 reported testing 30.2% (20.0%–40.4%) | |
| (2) Identified as gay or bisexual | 23 jurisdiction years c | 5 jurisdiction years d |
| 800/1307 ASMM reported having sexual intercourse 57.6% (51.6%–63.5%) | 131/213 ASMM reported having sexual intercourse 60.6% (53.1%–68.0%) | |
| 246/702 reported testing 24.2% (18.8%–29.5%) | 34/124 reported testing 27.8% (19.3%–36.3%) | |
| (3) Reported lifetime sexual contact with males or both males and females | 25 jurisdiction years e | 6 jurisdiction years f |
| 1118/1384 ASMM reported having sexual intercourse 81.4% (77.4%–85.4%) | 237/295 ASMM reported having sexual intercourse 82.0% (74.0%–89.9%) | |
| 344/999 reported testing 27.3% (22.0%–32.6%) | 60/229 reported testing 31.0% (20.3%–41.7%) |
Pooled high school YRBS state and district data from the following jurisdictions and years: Chicago, IL (2013); Connecticut (2007, 2009, 2011, 2013); Duval County, FL (2013); Hawaii (2013); Houston, TX (2013); Los Angeles, CA (2011, 2013); Massachusetts (2005, 2007, 2009, 2011, 2013); Memphis, TN (2013); Michigan (2013); New Jersey (2013); New York City, NY (2009, 2011, 2013); North Carolina (2013); Orange County, FL (2013); Palm Beach, FL (2013); San Diego, CA (2013); and Vermont (2011).
Pooled high school YRBS state and district data from the following jurisdictions and years: Massachusetts (2005, 2007, 2009, 2011, 2013); New Jersey (2013).
Pooled high school YRBS state and district data from a EXCEPT: Connecticut (2007, 2009); New Jersey (2013).
Pooled high school YRBS state and district data from the following jurisdictions and years: Massachusetts (2005, 2007, 2009, 2011, 2013).
Pooled high school YRBS state and district data from a EXCEPT: Duval County, FL (2013).
Pooled high school YRBS state and district data from the following jurisdictions and years: Massachusetts (2005, 2007, 2009, 2011, 2013); New Jersey (2013).
Acknowledgments
This work was supported by the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP) Epidemiologic and Economic Modeling Agreement number 5U38PS004646-02, funded by the Centers for Disease Control and Prevention.
Footnotes
Disclaimer
The conclusions, findings, and opinions expressed in this article are solely the responsibility of the authors and do not necessarily reflect the official views of the Centers for Disease Control and Prevention, the U.S. Department of Health and Human Services, or the authors’ affiliated institutions.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Mustanski BS, Newcomb ME, Du Bois SN, et al. : HIV in young men who have sex with men: A review of epidemiology, risk and protective factors, and interventions. J Sex Res 2011;48:218–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC): Vital signs: HIV infection, testing, and risk behaviors among youths—United States. MMWR Morb Mortal Wkly Rep 2012;61:971–976. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of STD Prevention: Sexually Transmitted Disease Surveillance 2013. 2014. Available at www.cdc.gov/std/stats13/surv2013-print.pdf Accessed November 25, 2016.
- 4.Outlaw AY, Phillips G 2nd, Hightow-Weidman LB, et al. : Age of MSM sexual debut and risk factors: Results from a multisite study of racial/ethnic minority YMSM living with HIV. AIDS Patient Care STDS 2011;25 Suppl 1: S23–S29. [DOI] [PubMed] [Google Scholar]
- 5.MacKellar DA, Valleroy LA, Secura GM, et al. : Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men: Opportunities for advancing HIV prevention in the third decade of HIV/AIDS. J Acquir Immune Defic Syndr 2005;38:603–614. [DOI] [PubMed] [Google Scholar]
- 6.Celentano DD, Sifakis F, Hylton J, et al. : Race/ethnic differences in HIV prevalence and risks among adolescent and young adult men who have sex with men. J Urban Health 2005;82:610–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valleroy LA, MacKellar DA, Karon JM, et al. : HIV prevalence and associated risks in young men who have sex with men. JAMA 2000;284:198–204. [DOI] [PubMed] [Google Scholar]
- 8.Hall HI, Walker F, Shah D, Belle E: Trends in HIV diagnoses and testing among U.S. adolescents and young adults. AIDS Behav 2012;16:36–43. [DOI] [PubMed] [Google Scholar]
- 9.Sifakis F, Hylton JB, Flynn C, et al. : Prevalence of HIV infection and prior HIV testing among young men who have sex with men. The Baltimore young men’s survey. AIDS Behav 2010;14:904–912. [DOI] [PubMed] [Google Scholar]
- 10.Sumartojo E, Lyles C, Choi K, et al. : Prevalence and correlates of HIV testing in a multi-site sample of young men who have sex with men. AIDS Care 2008;20:1–14. [DOI] [PubMed] [Google Scholar]
- 11.Phillips G 2nd, Ybarra ML, Prescott TL, et al. : Low rates of Human Immunodeficiency Virus testing among adolescent gay, bisexual, and queer men. J Adolesc Health 2015;57: 407–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kann L, Kinchen S, Shanklin SL, et al. : Youth risk behavior surveillance—United States, 2013. MMWR Suppl 2014;63: 1–168. [PubMed] [Google Scholar]
- 13.Marks G, Crepaz N, Senterfitt JW, Janssen RS: Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: Implications for HIV prevention programs. J Acquir Immune Defic Syndr 2005;39:446–453. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Preventive Services Task Force: Final Recommendation Statement: Human Immunodeficiency Virus (HIV) Infection: Screening. 2013. Available at www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/human-immunodeficiency-virus-hiv-infection-screening Accessed November 25, 2016.
- 15.Workowski KA, Bolan GA; Centers for Disease Control and Prevention: Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015;64:1–137. [PMC free article] [PubMed] [Google Scholar]
- 16.Emmanuel PJ, Martinez J: Adolescents and HIV infection: The pediatrician’s role in promoting routine testing. Pediatrics 2011;128:1023–1029. [DOI] [PubMed] [Google Scholar]
- 17.Levine DA: Office-based care for lesbian, gay, bisexual, transgender, and questioning youth. Pediatrics 2013;132: e297–e313. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention (CDC), Brener ND, Kann L, et al. : Methodology of the Youth Risk Behavior Surveillance System—2013. MMWR Recomm Rep 2013;62:1–20. [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention: Youth Risk Behavior Survey (YRBS) 2017 Standard Questionnaire Item Rationale. Available at www.cdc.gov/healthyyouth/data/yrbs/pdf/2017/2017_standard_yrbs_item_rationale.pdf Accessed November 25, 2016.
- 20.Centers for Disease Control and Prevention: Software for analysis of YRBS data. 2014. Available at www.cdc.gov/healthyyouth/data/yrbs/pdf/yrbs_analysis_software.pdf Accessed November 25, 2016.
- 21.Centers for Disease Control and Prevention: Combining YRBS data across years and sites. 2014. Available at www.cdc.gov/healthyyouth/data/yrbs/pdf/yrbs_combining_data.pdf Accessed November 25, 2016.
- 22.Branson BM, Handsfield HH, Lampe MA, et al. : Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep 2006;55:1–17. [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention: HIV infection risk, prevention, and testing behaviors among men who have sex with men: National HIV Behavioral Surveillance,20 U.S. cities, 2014. HIV Surveillance Special Report 15, 2016. Available at www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-hssr-nhbs-msm-2014.pdf Accessed November 25, 2016. [Google Scholar]
- 24.Kurth AE, Lally MA, Choko AT, et al. : HIV testing and linkage to services for youth. J Int AIDS Soc 2015;18(2 Suppl 1):19433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ashton MR, Cook RL, Wiesenfeld HC, et al. : Primary care physician attitudes regarding sexually transmitted diseases. Sex Transm Dis 2002;29:246–251. [DOI] [PubMed] [Google Scholar]
- 26.Peralta L, Deeds BG, Hipszer S, Ghalib K: Barriers and facilitators to adolescent HIV testing. AIDS Patient Care STDS 2007;21:400–408. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention (CDC): Unrecognized HIV infection, risk behaviors, and perceptions of risk among young black men who have sex with men—Six U.S. cities, 1994–1998. MMWR Morb Mortal Wkly Rep 2002;51:733–736. [PubMed] [Google Scholar]
- 28.Guttmacher Institute: Minors’ access to STI services. 2016. Available at www.guttmacher.org/state-policy/explore/minors-access-sti-services. Accessed November 25, 2016.
- 29.Cooley LA, Oster AM, Rose CE, et al. : Increases in HIV testing among men who have sex with men—National HIV Behavioral Surveillance System, 20 U.S. metropolitan statistical areas, 2008 and 2011. PLoS One 2014;9: e104162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Millett GA, Flores SA, Peterson JL, Bakeman R: Explaining disparities in HIV infection among black and white men who have sex with men: A meta-analysis of HIV risk behaviors. AIDS 2007;21:2083–2091. [DOI] [PubMed] [Google Scholar]
- 31.Sanchez T, Finlayson T, Drake A, et al. : Human Immunodeficiency Virus (HIV) risk, prevention, and testing behaviors—United States, National HIV Behavioral Surveillance System: Men who have sex with men, November 2003–April 2005. MMWR Surveill Summ 2006;55:1–16. [PubMed] [Google Scholar]
- 32.Millett GA, Peterson JL, Flores SA, et al. : Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: A meta-analysis. Lancet 2012;380:341–348. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention (CDC): Prevalence and awareness of HIV infection among men who have sex with men—21 cities, United States, 2008. MMWR Morb Mortal Wkly Rep 2010;59:1201–1207. [PubMed] [Google Scholar]
- 34.Balaji AB, Eaton DK, Voetsch AC, et al. : Association between HIV-related risk behaviors and HIV testing among high school students in the United States, 2009. Arch Pediatr Adolesc Med 2012;166:331–336. [DOI] [PubMed] [Google Scholar]


