Abstract
Background and Objectives: Protective equipment, including seatbelts and airbags, have dramatically reduced the morbidity and mortality rates associated with motor vehicle collisions (MVCs). While generally associated with a reduced rate of injury, the effect of motor vehicle protective equipment on patterns of chest wall trauma is unknown. We hypothesized that protective equipment would affect the rate of flail chest after an MVC. Materials and Methods: This study was a retrospective analysis of the 2019 iteration of the American College of Surgeons Trauma Quality Program (ACS-TQIP) database. Rib fracture types were categorized as non-flail chest rib fractures and flail chest using ICD-10 diagnosis coding. The primary outcome was the occurrence of flail chests after motor vehicle collisions. The protective equipment evaluated were seatbelts and airbags. We performed bivariate and multivariate logistic regression to determine the association of flail chest with the utilization of vehicle protective equipment. Results: We identified 25,101 patients with rib fractures after motor vehicle collisions. In bivariate analysis, the severity of the rib fractures was associated with seatbelt type, airbag status, smoking history, and history of cerebrovascular accident (CVA). In multivariate analysis, seatbelt use and airbag deployment (OR 0.76 CI 0.65–0.89) were independently associated with a decreased rate of flail chest. In an interaction analysis, flail chest was only reduced when a lap belt was used in combination with the deployed airbag (OR 0.59 CI 0.43–0.80) when a shoulder belt was used without airbag deployment (0.69 CI 0.49–0.97), or when a shoulder belt was used with airbag deployment (0.57 CI 0.46–0.70). Conclusions: Although motor vehicle protective equipment is associated with a decreased rate of flail chest after a motor vehicle collision, the benefit is only observed when lap belts and airbags are used simultaneously or when a shoulder belt is used. These data highlight the importance of occupant seatbelt compliance and suggest the effect of motor vehicle restraint systems in reducing severe chest wall injuries.
Keywords: flail chest, rib fracture, seatbelt, airbag, vehicle protective equipment, motor vehicle collision
1. Introduction
Motor vehicle collisions (MVCs) remain a prevalent and critical public health concern, contributing significantly to the global burden of trauma-related injuries and fatalities. MVCs account for nearly 1.35 million deaths every year worldwide, making it the eighth leading cause of death in all age groups globally [1]. Studies of injury patterns demonstrate that MVCs are more likely to lead to severe chest injuries compared to other mechanisms [2]. Thoracic trauma accounts for nearly 25% of trauma-related mortality, with approximately 40% presenting with rib fractures after blunt chest trauma [3,4,5]. Of this subset, approximately 6% of patients present with flail chest [4,5]. Among the myriad of injuries resulting from MVCs, rib fractures and flail chests represent common and often severe consequences, contributing substantially to morbidity and mortality rates. While most isolated rib fractures are often treated non-operatively, flail chest is often associated with higher morbidity and mortality rates [5,6]. In turn, patients with increasing severity of rib fracture patterns, such as flail chest, are at a higher risk of pulmonary complications, prolonged ventilator use, and longer ICU and hospital stays [5,6,7]. As previous studies have drawn attention to the significance of the patient population affected by these injuries, there is a pressing need to better understand and mitigate the associated risks.
Seatbelt utilization and the incorporation of airbags in contemporary vehicles mark significant milestones in occupant safety. Protective vehicle equipment, such as seatbelts and airbags, have dramatically reduced the morbidity and mortality rates associated with motor vehicle collisions. The National Highway Traffic Safety Administration estimates that in 2017, 14,955 lives of occupants aged 5 and older were saved by seatbelts, and 2790 lives of those aged 13 and older were saved by frontal airbags [8]. Seatbelt use is associated with less severe injuries and lower in-hospital mortality [9,10,11]. Although generally associated with reduced rates of injury, mortality, and morbidity, protective equipment has been shown to alter the injury patterns in abdominal trauma and orthopedic injuries [12]. Restrained occupants demonstrated a significant reduction in the severity of injury in all body areas, lower mortality rates, shorter hospital stays, and a lower number of operations. However, these occupants also had significantly higher rates of hollow viscos injury compared to unrestrained occupants [12,13]. The use of airbags alone is associated with a decrease in injuries to the brain, face, cervical spine, thorax, and abdomen [14]. The greatest reduction in injuries has been noted when seatbelts are used in conjunction with airbags, with the exception of an increase in extremity fractures with airbag deployment [14]. Understanding the intricate relationship between seatbelt use, airbag deployment, and traumatic injuries is paramount for refining injury prevention strategies and enhancing vehicle safety systems.
To our knowledge, there have been no studies evaluating the impact of vehicle protective equipment, such as seatbelts and airbags, on the pattern and severity of rib fractures. As such, the effect of motor vehicle protective equipment on the patterns and severity of rib fractures is unknown. The aim of this study is to evaluate the impact of vehicle protective equipment on chest wall injury patterns, specifically flail chest. We hypothesized that the utilization of vehicle protective equipment would decrease the rate of flail chest among patients presenting with rib fractures after MVCs.
2. Materials and Methods
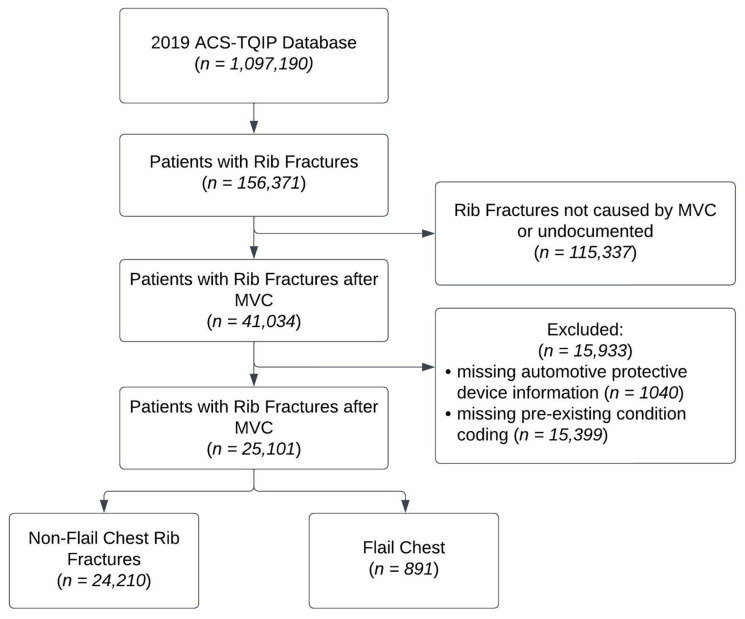
We performed a retrospective database analysis of the 2019 American College of Surgeons Trauma Quality Program (ACS-TQIP) database [15]. This is a large, deidentified database of trauma registry information from participating trauma centers. We identified all adult patients ≥ 16 years of age, without missing data, who sustained rib fractures secondary to a blunt injury mechanism, as defined using ICD-10 external cause coding (Figure 1). Study design was created using a Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (Supplementary Materials—Table S1) [16]. Further grouping was performed based on external cause coding to identify patients who were involved in MVCs. Patients were further categorized by rib fracture type (single rib, multiple ribs, and flail chest) using ICD-10 diagnosis coding. A flail chest is defined as three or more consecutive rib fractures in two or more locations, creating a flail segment. Pre-existing conditions were grouped into diagnoses using Clinical Classifications Software Refined v2023.1 for ICD-10 [17]. Abbreviated Injury Scale (AIS) scoring was calculated using the ICD-PIC R package to determine maximum AIS scores per body region [18,19].
Figure 1.
Retrospective database analysis of the 2019 American College of Surgeons Trauma Quality Program (ACS-TQIP) database of patients presenting with rib fractures after motor vehicle collision (MVC).
Safety device information, such as seatbelt usage, was defined in the TQIP database as the device used by the patient at time of injury. Lap belt was used to define lap belt usage as well as unspecified seatbelt restraints found on patients at the time of injury via TQIP [20]. Shoulder belt group was defined as having the presence of both a lap and shoulder belt at the time of injury. Airbag deployment was defined according to the location of airbag (front, side, or other) or non-deployment. Our primary goal was to determine the occurrence of flail chest injury with other variables of interest, including age, gender, pre-existing conditions, seatbelt type used, airbag type deployed, and AIS scoring by body region.
Descriptive analyses were performed using Chi-square testing for categorical variables and Wilcoxon rank-sum testing for continuous variables. All continuous variables were assumed to be non-normally distributed, and all analyses of continuous variables were conducted accordingly. Multivariate logistic regression was performed using clinically salient variables to determine the odds of flail chest injury. A further multivariate regression analysis of the interaction between seatbelt and airbag types was performed to determine the synergistic effects of protective devices on the severity of rib fractures. Results are presented as odds ratio (OR) with 95% confidence intervals (95% CI). Findings were considered significant for p ≤ 0.05. All analyses were performed using STATA SE/17 (StataCorp, College Station, TX, USA). This study was determined to be exempt from receiving an Institutional Review Board review and did not require informed consent for the use of deidentified data.
3. Results
3.1. Patient Characteristics
The analysis includes 25,101 patients with rib fractures after motor vehicle collisions who met the inclusion criteria. This includes 4704 single rib fractures (18.7%), 19,506 multiple rib fractures (77.7%), and 891 flail chest injuries (3.6%). The demographic characteristics of the patients are shown in Table 1. In bivariate analysis, the type of seatbelt used and the airbag status were associated with flail chest. Patients with flail chest were more likely to be older (p = 0.0368) and to have higher maximum AIS scores in the head/neck, face, extremities, and abdominal regions (p < 0.001). Furthermore, patients with flail chest had higher rates of a history of smoking (5.6% vs. 4.2%, p = 0.040) and a history of cerebrovascular accidents (CVA) (1.46% vs. 0.61%, p = 0.002) compared to patients with non-flail rib fractures.
Table 1.
Relationship of clinical and demographic factors to the occurrence of flail chest among patients with rib fractures after motor vehicle collision as identified in the 2019 ACS-TQIP database. Data shown as n (%) for categorical variables or Median (IQR) for continuous variables. AIS—Abbreviated Injury Scale. CVA—cerebrovascular accident. IQR—Interquartile range.
| Variable | Non-Flail Chest Rib Fractures (n = 24,210) |
Flail Chest (n = 891) |
p Value |
|---|---|---|---|
| Age (Median) | 58 (40–71) | 59 (44–71) | 0.0368 |
| Sex | 0.481 | ||
| Female | 10,994 (45.4%) | 394 (44.22%) | |
| Male | 12,213 (54.6%) | 497 (55.8%) | |
| Race | |||
| White | 18,653 (77.0%) | 703 (78.9%) | 0.196 |
| Black | 3174 (13.1%) | 111 (12.5%) | 0.571 |
| Asian | 423 (1.7%) | 15 (1.7%) | 0.887 |
| Ethnicity | 0.221 | ||
| Hispanic or Latino | 2167 (9.3%) | 69 (8.1%) | |
| Not Hispanic or Latino | 21,121 (90.7%) | 786 (91.9%) | |
| Seatbelt Type | <0.001 | ||
| No seatbelt | 7304 (30.2%) | 350 (39.3%) | |
| Lap belt only | 3366 (13.9%) | 106 (11.9%) | |
| Shoulder belt | 13,540 (55.9%) | 435 (48.8%) | |
| Airbag Status | <0.001 | ||
| No airbag present | 6254 (25.8%) | 296 (33.2%) | |
| Airbag present not deployed | 2683 (11.1%) | 94 (10.6%) | |
| Airbag deployed | 15,273 (63.1%) | 501 (56.2%) | |
| Body region maximum AIS (median IQR) | |||
| Head/Neck | 1 (0–1) | 1 (0–3) | <0.001 |
| General | 0 (0–0) | 0 (0–0) | 0.0753 |
| Face | 0 (0–0) | 0 (0–1) | 0.003 |
| Extremities | 1 (0–1) | 1 (1–2) | <0.001 |
| Abdomen | 1 (0–1) | 1 (0–2) | <0.001 |
| History of Smoking | 1017 (4.2%) | 50 (5.61%) | 0.040 |
| History of CVA | 147 (0.61%) | 13 (1.46%) | 0.002 |
3.2. Seatbelt Use and Airbag Deployment
A multivariate logistic regression was performed to investigate the risk of flail chest after an MVC (Table 2). Increasing age was independently associated with flail chest (OR 1.01, 1.01–1.02, p < 0.001). Compared to patients with no seatbelt, patients with a lap belt (OR 0.72, CI 0.57–0.90) or shoulder belt (OR 0.73, CI 0.63–0.86) were at lower risks of flail chest. Similarly, airbag deployment was associated with a lower risk of flail chest (OR 0.76, CI 0.65–0.89). In contrast, an increased risk of flail chest was associated with patients with non-chest maximum AIS scores in their head/neck (OR 1.13, CI 1.07–1.18), extremity (OR 1.22, CI 1.15–1.30), and abdomen (OR 1.38, CI 1.31–1.45) regions. It is worth noting that a history of CVA was associated with an increased risk of flail chest (OR 2.17, CI 1.21–3.88).
Table 2.
Multivariate logistic regression of factors associated with flail chest injuries among patients with rib fractures after motor vehicle collisions in the 2019 ACS-TQIP database. AIS—Abbreviated Injury Scale. CVA—cerebrovascular accident. IQR—Interquartile range.
| Variable | Odds Ratio | 95% Confidence Interval | p Value |
|---|---|---|---|
| Age | 1.01 | 1.01–1.02 | <0.001 |
| Male sex | 1.03 | 0.89–1.18 | 0.701 |
| Seatbelt Type | |||
| No seatbelt | reference | ||
| Lap belt only | 0.72 | 0.57–0.90 | 0.004 |
| Shoulder belt | 0.73 | 0.63–0.86 | <0.001 |
| Airbag | |||
| No airbag present | reference | ||
| Airbag present not deployed | 0.86 | 0.67–1.09 | 0.208 |
| Airbag deployed | 0.76 | 0.65–0.89 | 0.001 |
| Body region maximum AIS | |||
| Head/Neck | 1.13 | 1.07–1.18 | <0.001 |
| General | 1.04 | 0.93–1.16 | 0.500 |
| Face | 1.07 | 0.95–1.20 | 0.255 |
| Extremities | 1.22 | 1.15–1.30 | <0.001 |
| Abdomen | 1.38 | 1.31–1.45 | <0.001 |
| History of Smoking | 1.29 | 0.96–1.73 | 0.096 |
| History of CVA | 2.17 | 1.21–3.88 | 0.009 |
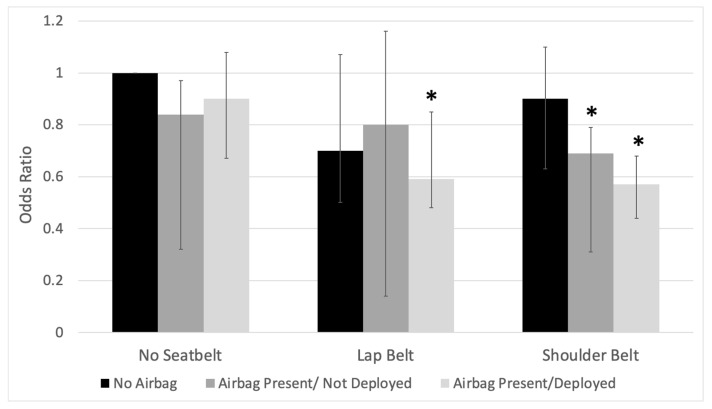
3.3. Synergistic Effects of Seatbelts and Airbags
A further multivariable logistic regression analysis of the interaction between seatbelt and airbag type was performed to determine the synergistic effects between protective devices (Table 3). In this analysis, increasing age was associated with an increased risk of flail chest (OR 1.01, CI 1.01–1.02). Interestingly, the risk of flail chest was only reduced when a lap belt was used in combination with the deployed airbag (OR 0.59, CI 0.43–0.80) when a shoulder belt was used when airbags were present but not deployed (OR 0.69, CI 0.49–0.97), or when a shoulder belt was used with an airbag deployed (OR 0.57, CI 0.46–0.70) (Figure 2). Like our previous multivariate analysis, a history of CVA (OR 2.16, CI 1.21–3.87) and maximum AIS in the head/neck (OR 1.13, CI 1.07–1.18), extremities (OR 1.22, CI 1.15–1.30), and abdomen (OR 1.38, CI 1.31–1.45) were associated with an increased risk of flail chest.
Table 3.
Multivariate interaction analysis of factors associated with flail chest injuries among patients with rib fractures after motor vehicle collisions in the 2019 ACS-TQIP database. AIS—Abbreviated Injury Scale. CVA—cerebrovascular accident. IQR—Interquartile range.
| Variable | Odds Ratio | 95% Confidence Interval | p Value |
|---|---|---|---|
| Age | 1.01 | 1.01–1.02 | <0.001 |
| Male sex | 1.03 | 0.89–1.18 | 0.720 |
| Seatbelt Type and airbag status (Interaction variable) | |||
| No seatbelt/no airbag | reference | ||
| No seatbelt/airbag present, not deployed | 0.84 | 0.57–1.22 | 0.358 |
| No seatbelt/airbag deployed | 0.90 | 0.72–1.13 | 0.377 |
| Lap belt/no airbag | 0.70 | 0.47–1.04 | 0.079 |
| Lap belt/airbag present, not deployed | 0.80 | 0.44–1.46 | 0.468 |
| Lap belt/airbag deployed | 0.59 | 0.43–0.80 | 0.001 |
| Shoulder belt/no airbag | 0.90 | 0.70–1.17 | 0.448 |
| Shoulder belt/airbag present, not deployed | 0.69 | 0.49–0.97 | 0.030 |
| Shoulder belt/airbag deployed | 0.57 | 0.46–0.70 | <0.001 |
| Body region maximum AIS | |||
| Head/Neck | 1.13 | 1.07–1.18 | <0.001 |
| General | 1.04 | 0.93–1.16 | 0.519 |
| Face | 1.07 | 0.95–1.20 | 0.257 |
| Extremities | 1.22 | 1.15–1.30 | <0.001 |
| Abdomen | 1.38 | 1.30–1.45 | <0.001 |
| History of Smoking | 1.28 | 0.95–1.73 | 0.103 |
| History of CVA | 2.16 | 1.21–3.87 | 0.009 |
Figure 2.
Association of risk of flail chest and vehicle protective equipment amongst patients with rib fractures after motor vehicle collisions in the 2019 ACS = TQIP database. Odds ratio from multivariate model was adjusted for age, sex, vehicle protective equipment, maximum abbreviated injury scale, history of smoking, and history of cerebrovascular accident. Reference group—no seatbelt/no airbags. Asterisk (*) denotes significance p ≤ 0.05.
4. Discussion
This is a retrospective national database analysis demonstrating the impact of vehicle protective equipment on patterns of chest wall injuries in patients presenting with rib fractures after MVCs. More specifically, this study further elucidates the complex relationship between the use of protective devices, such as seatbelts and airbags, and the risk of flail chest after MVCs. Although motor vehicle protective equipment utilization is associated with a decreased rate of flail chest after motor vehicle collision, there is only a benefit when lap belts and airbags are used simultaneously, or a shoulder belt is used (with or without airbag deployment). There was no difference in the severity of rib fractures among unbelted passengers when airbags were deployed. Furthermore, an increase in age, a history of smoking, and a history of CVA were associated with an increased risk of flail chest. Of note, patients with maximum AIS scores in the head/neck, extremities, or abdomen were associated with a higher likelihood of flail chest among patients presenting with rib fractures after MVCs. The findings of this study reveal essential insights into the reduction in flail chest rates when specific protective devices are employed and underscore the importance of identifying high-risk individuals who may benefit from improved preventative measures and management.
Flail chest can lead to chest wall instability, asynchronous movement of the flail segment, and paradoxical chest wall motion [4,5,6,21]. As such, this leads to deformity of the chest wall and a loss of thoracic volume. This will ultimately cause atelectasis, decreased lung volume, dyspnea, and chronic pain [5,6,21]. Given the severity of these injuries, flail chest is associated with higher morbidity (intensive care unit (ICU) admission, mechanical ventilation, need for chest tubes, tracheostomy, acute respiratory distress syndrome (ARDS), and sepsis) as well as higher mortality [6]. Current treatment guidelines for flail chest injuries include a multimodal pain regimen, chest physiotherapy, pulmonary toilet, positive pressure ventilation, and, in certain circumstances, rib stabilization [6,22,23]. Given the significant morbidity and mortality risks associated with flail chest in patients after blunt thoracic trauma, a focus on preventative measures is imperative.
Vehicle protective equipment, including seatbelts and airbags, has been associated with differences in injury patterns compared to patients who do not use protective equipment [11]. In a prospective study performed on injury patterns and the impact of seat belt use, unrestrained patients were more likely to have a higher AIS score in the thorax, back, and lower extremities compared to restrained passengers and were more likely to have lower GCS scores or undergo surgical operations [13]. A similar study evaluating mechanisms of injury and restraint use demonstrated decreases in brain injuries in restrained passengers involved in frontal MVCs while having found no difference in lateral MVCs [24]. Furthermore, they suggested seatbelt use did not protect against lung, liver, spleen, pelvis, and lower extremity injury, suggesting that the direction of a crash appeared to play a more significant role. Lower extremity injuries were higher in frontal crashes, while pelvic injuries were associated with lateral crashes [24]. Here, we demonstrated that among patients presenting with rib fractures after MVCs, seatbelt use and airbag deployment were independently associated with decreased rates of flail chest. In our interaction multivariate analysis, we demonstrated the synergistic relationship between seatbelt use and airbag deployment. However, it should be noted that this relationship differed based on the seatbelt type used. Patients with lap belts had lower rates of flail chests only when airbags were deployed. Furthermore, when a shoulder belt was utilized alone with an airbag present (deployed or not deployed), the risk of flail chest decreased. This further demonstrates the significance of the type of restraint used and the synergistic benefit of vehicle protective equipment on impacting chest wall injury pattern and severity. We propose that the biomechanical differences in forces experienced by the patient, with and without protective devices, play a significant role in the injury the patients may sustain. Thus, this synergistic effect underscores the necessity of public education on the proper and comprehensive use of safety features in vehicles.
As previously highlighted, flail chest is associated with significant morbidity and mortality. As such, identifying patients at risk may offer valuable insights into guiding the management of these patients for more favorable outcomes. In the study of patients with rib fractures after MVCs, it is important to consider underlying risk factors associated with these injuries. Diminished bone density is associated with an increased risk of bone fractures [25]. Particularly after blunt thoracic trauma, previous literature has demonstrated that patients with lower bone mineral density have higher rates of rib fractures compared to patients with normal bone mineral density [26]. There may be many factors associated with diminished bone density. An increase in age is strongly associated with diminished bone density and thus more susceptible to fractures [25,26,27]. Furthermore, other factors, such as a history of smoking, have been linked to reduced bone density and a higher risk of bone fracture [28]. In our cohort, an increase in age and a history of smoking were independently associated with an increased risk of flail chest amongst patients presenting with rib fractures after MVCs. While we were unable to analyze bone density among our cohort, as it is not included in the ACS-TQIP database, we speculate that both an increase in age and a history of smoking are associated with decreased bone density. In turn, these patients are more likely to sustain more severe rib fracture patterns, such as flail chest, after MVCs. Interestingly, we found that patients with a history of CVA are also independently associated with an increased risk of flail chest. Patients with a history of CVA may exhibit lower bone density due to underuse or secondary motor deficits [29]. In contrast, there is also an increased risk of stroke among patients with diminished bone density [30]. In our cohort, we are unable to assess bone density as it relates to a history of CVA. However, a history of CVA may provide insights into a patient’s bone density. More specifically, we hypothesize that a history of CVA may be indicative of diminished bone density in these patients, subsequently leading to an increased risk of flail chest after MVCs. Lastly, our analysis demonstrated that patients with flail chest had maximum AIS scores in the head/neck, extremities, and abdomen. Collectively, this information can be used by providers for more expeditious identification of these patients at risk to help guide management plans for improved outcomes. Future studies should focus on identifying other underlying factors that may be associated with an increased risk of more severe fracture patterns, such as flail chest, after MVCs.
The findings of our study have significant implications for clinical practice, particularly in a trauma care setting. Healthcare professionals should consider the observed synergistic effects of seatbelts and airbags in reducing incidences of flail chest injuries among patients with rib fractures after MVCs. Trauma care teams may need to emphasize the importance of proper seatbelt usage and advocate for comprehensive occupant protection. Furthermore, this information can guide emergency medical personnel in providing more targeted and effective interventions for patients at risk of severe chest injuries. Additionally, these findings further highlight the importance of public health initiatives and education campaigns focused on vehicular safety. Raising awareness about the specific protective devices, such as seatbelts and airbags, that contribute to a decreased severity of chest wall trauma can have a profound impact on reducing the overall morbidity and mortality associated with MVCs. Public health organizations should consider incorporating these findings into educational materials and campaigns aimed at encouraging proper seatbelt use and advocating for the widespread adoption of safety features in vehicles. Recognizing the multidisciplinary nature of addressing chest trauma after MVCs, collaboration across the medical, engineering, and public health disciplines is indispensable. A holistic approach, encompassing healthcare professionals, engineers specializing in vehicle safety, and public health experts, can combine efforts to formulate comprehensive strategies. Integrating engineering insights into vehicle design with medical expertise in trauma care ensures a more cohesive and effective approach to injury prevention and patient management.
Limitations
While the benefit of seatbelts in the alteration of injury patterns has been heavily advocated, to our knowledge, no study has evaluated the impact of other vehicle protective equipment, like airbags, in conjunction with seatbelt use. Moreover, no study has evaluated the impact of these devices on patterns of chest wall trauma. We recognize that this study has several limitations. The ACS-TQIP database is a deidentified administrative database and, as such, individual entries cannot be verified for accuracy. As a result, errors in billing and coding information cannot be addressed. Patients were identified using ICD-10 coding, and the study population could potentially be impacted by errors in coding. Furthermore, we were unable to evaluate other factors that may increase the risk of more severe rib fractures, such as bone density. While the ACS-TQIP database provides a select history of underlying comorbidities, more granular information regarding pertinent patients’ medical history would allow for a more comprehensive analysis of risk factors associated with the severity of injuries after MVCs. Protective device information was provided by the TQIP database and defined as protective device usage noted at the time of injury by emergency personnel. As a result, potential damage or patient factors could misidentify the device use. In addition, unspecified restraints were all categorized as lap belts, though they may not have been lap belts. Furthermore, information regarding crash severity, the direction of the collision, the speed of the collision, and vehicle information were not available for analysis in the ACS-TQIP database. Such factors have previously been demonstrated to be associated with altered injury severity and patterns in patients sustaining injuries through MVCs. Future studies should focus on developing and utilizing a database that contains both comprehensive clinical information on patients as well as more granular details pertaining to the MVCs. Despite these limitations, we believe that our study captures the impact of multiple vehicle protective devices on the severity of chest wall trauma patterns in patients presenting with rib fractures after MVCs.
5. Conclusions
In conclusion, the use of vehicle protective equipment reduces the rate of flail chest amongst patients presenting with rib fractures after MVCs. The benefits have only been observed with lap belts and simultaneous airbag deployment or shoulder belts (with or without airbag deployment). These data highlight the importance of occupant seatbelt compliance and suggest the connection between the use of motor vehicle protective equipment and the reduction in severe chest wall injuries. By identifying patient risk factors, clinicians can better recognize those at higher risk of flail chest following MVCs, ultimately leading to improved patient care and outcomes. Future studies should aim to explore additional factors that may contribute to more severe rib fracture patterns and expand our understanding of the biomechanical aspects of these injuries during MVCs.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/medicina59112046/s1. Table S1: Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement checklist of items that should be included in reports of observational studies for study titled “Motor Vehicle Protective Device Usage Associated with Decreased Rate of Flail Chest: A Retrospective Database Analysis”.
Author Contributions
Conceptualization, A.B. (Aria Bassiri), A.B. (Avanti Badrinathan) and C.W.T.; methodology A.B. (Aria Bassiri), A.B. (Avanti Badrinathan) and C.W.T.; software, A.B. (Aria Bassiri), A.B. (Avanti Badrinathan) and C.W.T.; validation, A.B. (Aria Bassiri), A.B. (Avanti Badrinathan) and C.W.T.; formal analysis, A.B. (Aria Bassiri), A.B. (Avanti Badrinathan) and C.W.T.; investigation, A.B. (Aria Bassiri), A.B. (Avanti Badrinathan) and C.W.T.; resources, A.B. (Aria Bassiri), A.B. (Avanti Badrinathan) and C.W.T.; data curation, A.B. (Aria Bassiri), A.B. (Avanti Badrinathan) and C.W.T.; writing—original draft preparation, A.B. (Aria Bassiri), A.B. (Avanti Badrinathan), S.K., J.S., P.A.L., V.P.H. and C.W.T.; writing—review and editing, A.B. (Aria Bassiri), A.B. (Avanti Badrinathan), S.K., J.S., P.A.L., V.P.H. and C.W.T.; visualization, A.B. (Aria Bassiri); supervision, C.W.T.; project administration, C.W.T.; funding acquisition, C.W.T. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was determined to be exempt from an Institutional Review Board review because all the data was deidentified.
Informed Consent Statement
Not applicable.
Data Availability Statement
Upon request, the corresponding author can provide the data utilized in this study.
Conflicts of Interest
C.W.T. is a consultant for Zimmer Biomet, Astra Zeneca, Atricure, and Medtronic and is a grant recipient from Zimmer Biomet and Intuitive Foundation. V.P.H. is supported by the CTSC of Cleveland (KL2TR002547). None of these relationships have affected this manuscript or the accuracy of the data analysis. The other authors have no disclosures, sources of funding, or financial relationships to declare.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.World Health Organization (WHO) Global Status Report on Road Safety 2018. The World Health Organization (WHO); Geneva, Switzerland: 2018. [Google Scholar]
- 2.Parreira J.G., Rondini G.Z., Below C., Tanaka G.O., Pelluchi J.N., Arantes-Perlingeiro J., Soldá S.C., Assef J.C. Trauma mechanism predicts the frequency and the severity of injuries in blunt trauma patients. Rev. Col. Bras. Cir. 2017;44:340–347. doi: 10.1590/0100-69912017004007. [DOI] [PubMed] [Google Scholar]
- 3.Demetriades D., Murray J., Charalambides K., Alo K., Velmahos G., Rhee P., Chan L. Trauma fatalities: Time and location of hospital deaths. J. Am. Coll. Surg. 2004;198:20–26. doi: 10.1016/j.jamcollsurg.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 4.Sirmali M., Turut H., Topcu S., Gulhan E., Yazici U., Kaya S., Taştepe I. A comprehensive analysis of traumatic rib fractures: Morbidity, mortality and management. Eur. J. Cardio-Thorac. Surg. 2003;24:133–138. doi: 10.1016/S1010-7940(03)00256-2. [DOI] [PubMed] [Google Scholar]
- 5.Lafferty P.M., Anavian J., Will R.E., Cole P.A. Operative Treatment of Chest Wall Injuries: Indications, Technique, and Outcomes. JBJS. 2011;93:97. doi: 10.2106/JBJS.I.00696. [DOI] [PubMed] [Google Scholar]
- 6.Dehghan N., de Mestral C., McKee M.D., Schemitsch E.H., Nathens A. Flail chest injuries: A review of outcomes and treatment practices from the National Trauma Data Bank. J. Trauma Acute Care Surg. 2014;76:462. doi: 10.1097/TA.0000000000000086. [DOI] [PubMed] [Google Scholar]
- 7.Flagel B.T., Luchette F.A., Reed R.L., Esposito T.J., Davis K.A., Santaniello J.M., Gamelli R.L. Half-a-dozen ribs: The breakpoint for mortality. Surgery. 2005;138:717–723; discussion 723–725. doi: 10.1016/j.surg.2005.07.022. [DOI] [PubMed] [Google Scholar]
- 8.National Highway Traffic Safety Administration . Lives Saved in 2017 by Restraint Use and Minimum-Drinking-Age Laws. National Highway Traffic Safety Administration; Washington, DC, USA: 2016. [(accessed on 20 March 2023)]. DOT HS 812. Available online: https://crashstats.nhtsa.dot.gov/Api/Public/Publication/812683. [Google Scholar]
- 9.Layrisse V., García-Rodríguez O., Ramos-Meléndez E., Rodríguez-Ortiz P. A Comparative Analysis of the Injury Patterns and In-Hospital Mortality Rates of Belted and Unbelted Motor-Vehicle Occupants—Puerto Rico, January 2000 to December 2014. Puerto Rico Health Sci. J. 2018;37:213–219. [PubMed] [Google Scholar]
- 10.Elkbuli A., Dowd B., Spano P.J., Hai S., Boneva D., McKenney M. The association between seatbelt use and trauma outcomes: Does body mass index matter? Am. J. Emerg. Med. 2019;37:1716–1719. doi: 10.1016/j.ajem.2018.12.023. [DOI] [PubMed] [Google Scholar]
- 11.Boserup B., Sutherland M., Paloka R., McKenney M., Elkbuli A. The Impact of Seatbelt Use on Trauma Outcomes in Adult Motor Vehicle Collision Patients With Rib Fractures: A National ACS-TQPs-PUF Database Analysis. J. Surg. Res. 2022;270:376–385. doi: 10.1016/j.jss.2021.06.067. [DOI] [PubMed] [Google Scholar]
- 12.Nash N.A., Okoye O., Albuz O., Vogt K.N., Karamanos E., Inaba K., Demetriades D. Seat Belt Use and its Effect on Abdominal Trauma: A National Trauma Databank Study. Am. Surg. 2016;82:134–139. doi: 10.1177/000313481608200216. [DOI] [PubMed] [Google Scholar]
- 13.Abu-Zidan F.M., Abbas A.K., Hefny A.F., Eid H.O., Grivna M. Effects of Seat Belt Usage on Injury Pattern and Outcome of Vehicle Occupants After Road Traffic Collisions: Prospective Study. World J. Surg. 2012;36:255–259. doi: 10.1007/s00268-011-1386-y. [DOI] [PubMed] [Google Scholar]
- 14.Williams R.F., Fabian T.C., Fischer P.E., Zarzaur B.L., Magnotti L.J., Croce M.A. Impact of Airbags on a Level I Trauma Center: Injury Patterns, Infectious Morbidity, and Hospital Costs. J. Am. Coll. Surg. 2008;206:962. doi: 10.1016/j.jamcollsurg.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 15.American College of Surgeons Trauma Quality Programs (TQP) Participant Use File (PUF) User Manual, Admission Year 2020. [(accessed on 1 December 2022)]. Available online: https://www.facs.org/media/3zjdbmxz/tqp-puf-user-manual-2020.pdf.
- 16.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014;12:1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 17.Clinical Classifications Software Refined (CCSR) Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality, Rockville, MD. [(accessed on 1 December 2022)];2021 October; Available online: www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp.
- 18.Clark D.E., Osler T.M., Hahn D.R. ICDPIC: Stata Module to Provide Methods for Translating International Classification of Diseases (Ninth Revision) Diagnosis Codes into Standard Injury Categories and/or Scores. Boston College Department of Economics; Boston, MA, USA: 2009. Statistical Software Components S457028. revised 29 October 2010. [Google Scholar]
- 19.Clark D.E., Black A.W., Skavdahl D.H., Hallagan L.D. Open-access programs for injury categorization using ICD-9 or ICD-10. Inj. Epidemiol. 2018;5:11. doi: 10.1186/s40621-018-0149-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.ACS NTDS National Trauma Data Standard: Data Dictionary 2019. [(accessed on 1 March 2022)]. Available online: https://www.facs.org/quality-programs/trauma/quality/national-trauma-data-bank/national-trauma-data-standard/data-dictionary/
- 21.Engel C., Krieg J.C., Madey S.M., Long W.B., Bottlang M. Operative Chest Wall Fixation with Osteosynthesis Plates. J. Trauma Acute Care Surg. 2005;58:181. doi: 10.1097/01.TA.0000063612.25756.60. [DOI] [PubMed] [Google Scholar]
- 22.Simon B., Ebert J., Bokhari F., Capella J., Emhoff T., Hayward T., Rodriguez A., Smith L. Management of pulmonary contusion and flail chest: An Eastern Association for the Surgery of Trauma practice management guideline. J. Trauma Acute Care Surg. 2012;73:S351. doi: 10.1097/TA.0b013e31827019fd. [DOI] [PubMed] [Google Scholar]
- 23.Nirula R., Diaz J.J., Trunkey D.D., Mayberry J.C. Rib Fracture Repair: Indications, Technical Issues, and Future Directions. World J. Surg. 2009;33:14–22. doi: 10.1007/s00268-008-9770-y. [DOI] [PubMed] [Google Scholar]
- 24.Siegel J.H., Mason-Gonzalez S., Dischinger P., Cushing B., Read K., Robinson R., Smialek J., Heatfield B., Hill W., Bents W., et al. Safety Belt Restraints And Compartment Intrusions In Frontal And Lateral Motor Vehicle Crashes: Mechanisms Of Injuries, Complications, And Acute Care Costs. J. Trauma Acute Care Surg. 1993;34:736. doi: 10.1097/00005373-199305000-00017. [DOI] [PubMed] [Google Scholar]
- 25.NIH Consensus Development Panel on Osteoporosis Prevention D and Therapy Osteoporosis Prevention, Diagnosis, and Therapy. JAMA. 2001;285:785–795. doi: 10.1001/jama.285.6.785. [DOI] [PubMed] [Google Scholar]
- 26.Prins J.T.H., Van Lieshout E.M.M., Reijnders M.R.L., Verhofstad M.H.J., Wijffels M.M.E. Rib fractures after blunt thoracic trauma in patients with normal versus diminished bone mineral density: A retrospective cohort study. Osteoporos. Int. 2020;31:225–231. doi: 10.1007/s00198-019-05219-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim W., Gong H.S., Lee S.H., Park J.W., Kim K., Baek G.H. Low evaluation rate for osteoporosis among patients presenting with a rib fracture. Arch. Osteoporos. 2017;12:61. doi: 10.1007/s11657-017-0357-9. [DOI] [PubMed] [Google Scholar]
- 28.Yuan S., Michaëlsson K., Wan Z., Larsson S.C. Associations of Smoking and Alcohol and Coffee Intake with Fracture and Bone Mineral Density: A Mendelian Randomization Study. Calcif. Tissue Int. 2019;105:582–588. doi: 10.1007/s00223-019-00606-0. [DOI] [PubMed] [Google Scholar]
- 29.Beaupre G.S., Lew H.L. Bone-Density Changes After Stroke. Am. J. Phys. Med. Rehabil. 2006;85:464. doi: 10.1097/01.phm.0000214275.69286.7a. [DOI] [PubMed] [Google Scholar]
- 30.Myint P.K., Clark A.B., Kwok C.S., Loke Y.K., Yeong J.K.-Y., Luben R.N., Wareham N.J., Khaw K.-T. Bone Mineral Density and Incidence of Stroke. Stroke. 2014;45:373–382. doi: 10.1161/STROKEAHA.113.002999. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Upon request, the corresponding author can provide the data utilized in this study.