Abstract
There is substantial experimental and clinical interest in providing effective ways to both prevent and slow the onset of hearing loss. Auditory hair cells, which occur along the basilar membrane of the cochlea, often lose functionality due to age-related biological alterations, as well as from exposure to high decibel sounds affecting a diminished/damaged auditory sensitivity. Hearing loss is also seen to take place due to neuronal degeneration before or following hair cell destruction/loss. A strategy is necessary to protect hair cells and XIII cranial/auditory nerve cells prior to injury and throughout aging. Within this context, it was proposed that cochlea neural stem cells may be protected from such aging and environmental/noise insults via the ingestion of protective dietary supplements. Of particular importance is that these studies typically display a hormetic-like biphasic dose–response pattern that prevents the occurrence of auditory cell damage induced by various model chemical toxins, such as cisplatin. Likewise, the hormetic dose–response also enhances the occurrence of cochlear neural cell viability, proliferation, and differentiation. These findings are particularly important since they confirmed a strong dose dependency of the significant beneficial effects (which is biphasic), whilst having a low-dose beneficial response, whereas extensive exposures may become ineffective and/or potentially harmful. According to hormesis, phytochemicals including polyphenols exhibit biphasic dose–response effects activating low-dose antioxidant signaling pathways, resulting in the upregulation of vitagenes, a group of genes involved in preserving cellular homeostasis during stressful conditions. Modulation of the vitagene network through polyphenols increases cellular resilience mechanisms, thus impacting neurological disorder pathophysiology. Here, we aimed to explore polyphenols targeting the NF-E2-related factor 2 (Nrf2) pathway to neuroprotective and therapeutic strategies that can potentially reduce oxidative stress and inflammation, thus preventing auditory hair cell and XIII cranial/auditory nerve cell degeneration. Furthermore, we explored techniques to enhance their bioavailability and efficacy.
Keywords: polyphenols, hormesis, vitagenes, HSPs neuroprotection, Nrf2
1. Introduction
There is substantial experimental and clinical interest in providing effective ways to both prevent and slow the onset of hearing loss. Auditory hair cells, which occur along the basilar membrane of the cochlea, often lose functionality due to age-related biological alterations, exposure to high-decibel sounds, or genetic disorders affecting the inner and middle ear. These conditions can manifest as various types of hearing loss, including sensorineural, conductive, or mixed hearing loss, for instance, Pendred or Usher Syndrome [1,2]. Hearing loss is also seen as consequence of neuronal degeneration occurring before or following hair cell destruction/loss. A strategy is therefore necessary to protect hair cells and XIII cranial/auditory nerve cells prior to injury and throughout the aging process.
Within this context, it has been proposed that cochlea neural stem cells may be protected from such age-related and/or environmental/noise insults via the ingestion of protective dietary supplements. In fact, protection of auditory cells was reported with phytochemicals, including ginkgo biloba [3,4,5,6], ginseng [7], and alpha lipoic acid [8]. Of particular importance is that these studies typically display a hormetic-like biphasic dose–response pattern that prevents the occurrence of auditory cell damage induced by various model chemical toxins, such as cisplatin. In these experimental settings the hormetic dose–response also enhances cochlear neural cell viability, proliferation, and differentiation [5]. The cochlear nerve transmits signals from the inner ear to the cochlear nuclei within the brainstem and ultimately to the primary auditory cortex within the temporal lobe. These beneficial activities of the xenobiotics in plants are particularly important since they confirm a strong dose dependency for significant beneficial effects (which is biphasic), whilst having a low-dose beneficial response, whereas extensive exposures may become ineffective and/or potentially harmful. On the other hand, it is known that polyphenols, which were suggested to prevent hearing loss, have very low bioavailability when ingested orally [9] and are extremely unlikely to reach effective high concentrations in hair cells or auditory nerves. Consistently, they are beneficial in preventing hearing loss.
This review explores natural inducers, such as polyphenols, targeting the Nrf2 pathway and its dependent vitagenes, which include also heat shock protein (HSP) system, to develop neuroprotective and therapeutic strategies that can potentially reduce oxidative stress and inflammation, and thus, prevent auditory hair cell and XIII cranial/auditory nerve cell degeneration. Furthermore, we explored techniques to enhance their bioavailability and efficacy.
2. Nrf2 and Neuroprotection
In the central nervous system (CNS), hair cells and XIII cranial/auditory nerve cells, functional redox signaling and low levels of reactive oxygen species (ROS) are thought to play an essential role in neurogenesis and synaptic plasticity [10,11]. These cells possess a low buffering capacity against ROS accumulation, rendering them highly vulnerable to oxidative stress-induced damage, as one major cause of neurodegeneration [12]. NF-E2-related factor 2 (Nrf2) is a master regulator of stress maintenance pathways in several pathological conditions. These include major neurodegenerative diseases such as Alzheimer’s disease (AD) and Parkinson’s disease (PD) [13] along with hearing loss. Under normal circumstances, Nrf2 is located in the cytosol, where its inhibition is modulated by Keap-like ECH-associated protein 1 (KEAP1). Nrf2 is ubiquitously expressed [14] and has a critical role in the defense against toxic insults in the neuron, glial, and astrocytic cells in the brain [15,16]. Specific natural activators of Nrf2 are neuroprotective, making them effective preventive and therapeutic agents for neurodegenerative diseases [17]. In particular, several studies showed that polyphenols have the potential to act as antioxidants, anti-inflammatories, anti-amyloidogenic agents, anti-α-synuclein aggregators, and antidepressants by modulating the Nrf2 pathways and molecular antioxidant biomarkers to prevent the onset and progression of various chronic inflammatory diseases, especially neurodegenerative diseases, both in vitro and in vivo (see Figure 1) [18,19,20,21,22,23,24,25,26].
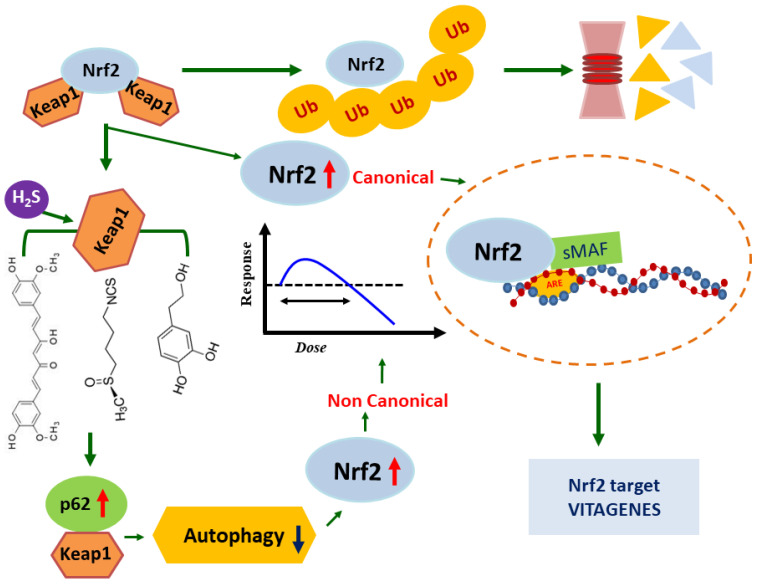
Figure 1.
Canonical and non-canonical activation of Nrf2. Nrf2 is localized in the cytosol and interacts with KEAP1 for ubiquitination and proteasomal degradation, under basal conditions. Oxidative stress causes conformational changes of KEAP1-C151, leading to Nrf2 dissociation. Free Nrf2 enters into the nucleus where it forms dimers with MAF proteins and binds to the antioxidant response element (ARE) regulatory sequences of target genes, inducing their expression. In the non-canonical Nrf2 activation, polyphenol-dependent inhibition of autophagy results in increased p62, which competitively binds with KEAP1 and thus contributes to Nrf2 activation in a KEAP1-C151-independent manner. The relationship with hormesis is inferred.
The activation of Nrf2 is the molecular mechanism by which polyphenols induce neuroprotective effects against oxidative stress and inflammation. Nrf2 accumulates, translocates into the nucleus, and binds to the antioxidant response element (ARE), causing the transcription of multiple target genes, including phase II detoxification enzymes such as NAD(P)H-Quinone oxidoreductase 1 (NQO1), heme oxygenase 1 (HO-1), thioredoxin (Trx), γ-glutamylcysteine synthetase, and glutathione S-transferase (GST). These have been identified as contributors to the antioxidant pathway regulated by Nrf2, protecting against various forms of stress, such as mitochondrial dysfunction, oxidative damage and environmental stress [27,28]. Vitagenes, such as Hsp 70, HO-1, γ-GCs, Trx, and SIRTs were identified by various studies [29,30,31,32,33,34] as biomarkers for stress adaptation, cross-tolerance, and cellular resilience, which are relevant for hormesis or preconditioning [35,36]. Increasing evidence suggests that dysfunction to the Nrf2 pathway significantly contributes to neurodegeneration [37,38,39,40].
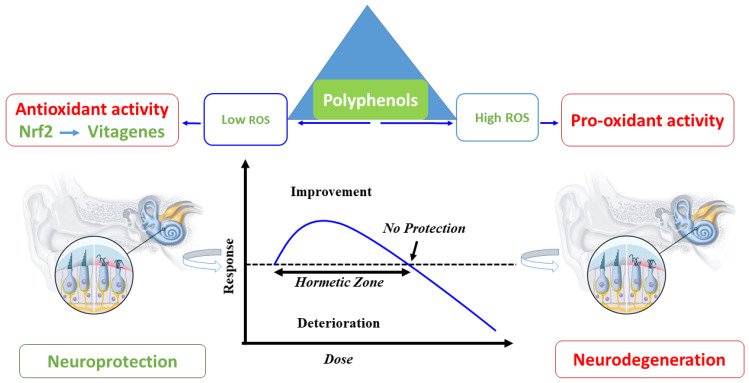
Specifically, cellular senescence may contribute to the dysfunction of the Nrf2 pathway and the progression of neuroinflammation and cognitive decline [41]. Furthermore, it is well-documented that Nrf2 is downregulated during times of oxidative stress, inflammation, and neurodegeneration [42,43]. Conversely, the activation of the Nrf2 pathway and related antioxidant vitagenes by polyphenols reduces cognitive decline and neuronal death in animal models of Alzheimer’s disease (AD) and Parkinson’s disease (PD), as well as in humans (Figure 2) [43,44]. Importantly, Nrf2 is crucial for mitochondrial function as it helps to maintain mitochondrial homeostasis, which affects the mitochondrial membrane potential, respiration, oxidative phosphorylation, ATP synthesis, mitochondrial biogenesis and integrity [45,46]. Thus, deregulation of Nrf2 and damage to mitochondria are essential factors causing the development of neurodegenerative diseases since neurons are highly susceptible to oxidative stress [47,48]. Activation of Nrf2 occurs endogenously in response to elevated levels of oxidative stress and inflammation, and can be bursted by nutritional agents administered exogenously. In recent years, researchers have shown interest in the effects of nutritional polyphenols on the prevention and treatment of AD and PD. This was demonstrated by many preclinical and clinical studies focusing on the neuropharmacological activity of these compounds [49,50,51,52,53].
Figure 2.
Schematic representation of hormetic neuroprotection. Polyphenols modulate Nrf2-related vitagenes in the low range of hormetic dose–response. On the other hand, at higher stimulation, detrimental effects are observed and neurodegeneration occurs.
3. Heat Shock Response and Neuroprotection
Cellular and organismal functions rely on properly synthesized and folded proteins. The quality of the proteome becomes especially important during disease and the exposure to endogenous and environmental stresses when cells experience physical and chemical fluctuations that they have to adapt to. The homeostasis of protein synthesis, folding, and degradation is called protein homeostasis or proteostasis [54]. Due to its central role in aging and decline of nervous function, proteostasis in neural tissues has become an intense field of research [55].
Many components of the cellular network that ensure protein homeostasis are under the control of the transcription factor Heat shock factor (HSF) 1 and its relatives HSF2, HSF3 and HSF4. This ancient family of gene regulators is involved in the induction of a number of molecular chaperones under stress conditions [56]. Together with Nrf2, HSFs represent a strong defense line against a very broad spectrum of stress inducers and are indispensable components of stress response in human cells. However, the complementarity and interchangeability of the two systems remain less well understood. Specifically, it is not clear which HSF-induced components could replace the Nrf2-induced proteins in protecting the cell from different stressors. HSF1 is the best understood member of the HSF family. In mammalian cells, HSF1 rests in a monomeric inactive state in the cytosol. Upon different stress stimuli, including heat shock, HSF1 trimerizes and acquires DNA-binding capacity [56]. The widely accepted model of HSF1 activation suggests that the transcription factor is kept inactive by association with molecular chaperones. According to the model, the titration of chaperones during stress to other, more affine and abundant targets releases HSF1 for oligomerization [57]. However, oligomerization of HSF1 might not be sufficient for its full activity, and a number of post-translational modifications are known to influence HSF1 function [58]. The known modifications include phosphorylation, acetylation, and sumoylation. Yet another factor to be considered is the role of HSF stability, which in turn affects the cellular levels of the transcription factor. Neurodegeneration is often accompanied by decreased levels of HSF1, which then impairs the capacity of cells to react to stress and induces a protective stress response [58,59,60].
The defects in HSF1 function during aging and neurodegeneration are numerous and are extensively documented [61]. The insufficient activity of HSF1 affects the upregulation of molecular chaperones that otherwise would help protect cellular proteins from misfolding or dissolving already aggregated species. As a consequence, the progression of neurodegeneration is increased, and its clinical manifestations are exaggerated. In a murine model of Huntington’s disease, a lack of HSF1 enhanced mutant huntingtin aggregation [62]. Conversely, overexpression of active HSF1 significantly suppressed huntingtin aggregate formation [63]. Interestingly, HSF2 knock-outs also displayed an increased huntingtin aggregation in the striatum, which caused a reduced lifespan for the experimental animals [64]. Similarly, several Parkinson’s disease models support the protective role of the heat shock response in neurodegeneration. For example, overexpression of a dominant-positive version of HSF1 in human cells decreased a-synuclein levels and ameliorated a-synuclein-induced toxicity [65]. α-Synuclein was found to induce aberrant HSF1 degradation in cell lines and in vivo, which was linked to the activity of the E3 ligase neural precursor cell expressed developmentally downregulated protein (NEDD) 4 that is increased in Parkinson’s [59]. Overexpression of HSF1 in the cerebellum reversed the deficiency of Purkinje cells in Alzheimer’s disease [66], and activation of HSF1 using the HSP90 inhibitor tanespimycin (17-AAG) attenuated Aβ-induced synaptic toxicity and memory impairment [67]. The motor neuron disease amyotrophic lateral sclerosis (ALS) is characterized by aggregates of the superoxide dismutase superoxide dismutase (SOD) 1. Low activity of HSF1 in ALS neurons was linked with their susceptibility to SOD1 aggregation [68]. The neuroprotective effects of HSF1 as exemplified above can be attributed to the induction and action of a number of molecular chaperones. In this regard, HSP70 and HSP90 are the members of the chaperone family that are analyzed most and whose neuroprotective activity is understood best [69]. Chaperones counteract the toxicity of aggregates using at least three mechanisms: (1) preventing amyloid formation, (2) disaggregating misfolded proteins, and (3) sequestering aggregates to specialized subcellular structures [54].
Prevention of amyloid formation is the first strategy of molecular chaperone action. One of the first mechanistic explanations of the protective function of chaperones came with the analyses of huntingtin aggregation in vitro and in vivo. It was shown that HSP70, with the help of its cofactor HSP40, can interfere with the conformational change in mutant huntingtin and thus prevent its aberrant interaction and inactivation of the transcription factor TBP [70]. In these models, induction of HSPs, especially HSP70, is observed in hair cells, accompanied by elevated blood glucocorticoids [71]. It was also reported that in rats, HSP70 (induced by sound conditioning) decreased susceptibility to noise-induced trauma, suggesting the result of enhancement of vitagene through the HSP70/Bmi1–FoxO1–SOD signaling pathway [72].
The neuroprotective effects of HSF1 as exemplified above can be attributed to the induction and action of a number of molecular chaperones. In this regard, HSP70 and HSP90 are the members of the chaperone family, which are analyzed most and whose neuroprotective activity is understood best [69]. Chaperones counteract the toxicity of aggregates by preventing amyloid formation, disaggregating misfolded proteins, and sequestering aggregates to specialized subcellular structures [54]. One of the first mechanistic explanations of the protective function of chaperones came with the analyses of huntingtin aggregation in vitro and in vivo. It was shown that HSP70 with the help of it cofactor HSP40 can interfere with the conformational change in mutant huntingtin and thus prevent its aberrant interaction and inactivation of the transcription factor TBP [73]. The role of the HSP70–HSP40 system in preventing primary nucleation of fibrils and their elongation was demonstrated for different aggregation-prone disease proteins and thus can be considered as the general feature of these molecular chaperones [74,75].
Disaggregation is another mechanism of how chaperones contribute to the neuroprotective effect of the HSF1-mediated stress response. It has been known for a long time that fungi contain the HSP100 family of chaperones that are specialized in dissolving already formed aggregates in an ATP-dependent manner [76,77]. Mammals lack HSP100 chaperones, and their disaggregating function is performed by HSP70 supported by the HSP70 homologue nucleotide exchange factor HSP110 [78,79,80]. Here, proteasomal degradation becomes critical to prevent toxic effects of dissolved species that may exist in potentially dangerous intermediate states [81]. An imbalance of the disaggregating activity of chaperones and the cellular protein degradation capacity would contribute to the paradoxical toxicity of the chaperone overexpression, an example of a complex dose–response relationship in cellular biochemistry.
The third neuroprotective strategy used by cells is to sequester aggregates in dedicated subcellular structures. Molecular chaperones also actively participate in the aggregate sequestration. Specifically, the small Heat shock protein (sHSP) family was shown to be critically involved in this process [82]. Mechanistically, sHSP oligomerization underlies the sHSP-aggregate interactions, which, in contrast to the classical mechanisms of other chaperones, is ATP-independent. In cells exposed to increased temperature, the small heat shock protein sHSP42 concentrates misfolded proteins into small foci, its function mediated by a prion-like domain [83,84,85]. The sequestration activity of sHSPs reduces the substrate burden for other components of the proteostasis machinery and thus contributes to the cellular survival during stress [86]. The concentration of aggregates in mammalian cells lead to the formation of large inclusion bodies, called aggresomes, at the microtubule-organizing center [87]. The sequestration of misfolded species in inclusion bodies has a protective role in a cell. It was shown that inclusion body formation improves survival and leads to decreased levels of mutant huntingtin elsewhere in neurons [88].
In addition to mutant protein-driven aggregation that underlies the pathogenesis of a number of neurodegenerative disorders, there is overwhelming evidence of a general decrease in proteome solubility and an increase in protein aggregation during the aging process, especially in the nervous system. It is believed that the amount of oxidatively damaged proteins increases with age, especially in non-dividing and long-lived cells, such as neurons, which increases the substrate load for the proteostasis machinery probably above manageable levels [54,89,90]. To make things worse, the expression of ATP-dependent molecular chaperones in the aging human brain is repressed significantly [91]. These findings emphasize the need for nutritional and pharmaceutical approaches to boost the heat shock response via HSF1 or support the function of individual chaperones, not only in the clinical setting, but also in the general population to support healthy aging; however, the relationships of molecular chaperones with antioxidative nutrients are complex and not yet well understood. Specifically, polyphenols are known to induce the expression of a number of heat shock proteins and, at the same time, can act as potent inhibitors of their action [92,93]. Furthermore, several polyphenols were reported to increase HSP expression in various organs, reduce oxidative stress, and suppress the exacerbation of symptoms in rodent models of inflammation [94,95]. However, it is still not well understood whether these changes occur in neurons and exhibit a hormetic dose–response, and future research is expected.
4. Polyphenols
It is well known that polyphenols are the most diverse of all secondary plant metabolites, with more than 8000 of them identified to date [96], They are divided into subclasses based on their chemical structures, flavonoids (flavonol, flavanol, flavone, anthocyanidin, isoflavonoid, and so on), stilbenes, hydrolyzed tannins, phlorotannins, and phenolic acids. Polyphenols are known to chemically interact strongly with ROS and reactive nitrogen species (RNS) and exert anti-inflammatory effects in vitro and in vivo [97]. Recent studies have reported that some polyphenols reduce damage to cochlear auditory hair cells induced by noise, antibiotics, and anticancer drugs [98,99].
On the other hand, polyphenols are generally less bioavailable [100] and have a limited increase in concentration in the brain. Polyphenol and their associated compound levels can differ significantly in terms of quantity and quality. Clinical studies show that after consuming 10 to 100 mg of a single phenolic compound, plasma concentrations normally do not surpass 1 µM [101]. Aglycones are removed from polyphenol glycosides ingested through food and taken in by the small intestine. It is recognized that the activation of proteins in the excretory system contributes to the low absorption rate from the small intestine. Only a small percentage of these aglycones are taken up by epithelial cells, rapidly conjugated with glucuronide or sulfate, and subsequently secreted into the portal vein. Polyphenols that enter the liver through the portal vein undergo reactions such as glucuronic acid conjugation, sulfate conjugation, methylation, etc. After conversion, they are secreted as metabolites into the peripheral blood [102,103]. These metabolites are then transported into the bloodstream and eliminated in the urine. Part of the polyphenols that reach the lower part of the gastrointestinal tract are degraded by intestinal bacteria and many types of degradation products are produced in the colon [104,105]. The microbiota metabolism of polyphenols involves cleaving glycosidic linkages and breaking down the heterocyclic backbone [106]. It was reported that the primary genera responsible for the metabolism of various phenolics, such as isoflavones, flavonols, flavones, and flavan-3-ols, are Clostridium and Eubacterium. The microbiome breaks down procyanidins and tannins that remain unabsorbed in the upper gastrointestinal tract and produces characteristic, low-molecular-weight degradation products in the colon [107]. For instance, procyanidins and flavan-3-ol oligomers are examples of compounds that can undergo intestinal bacterial catabolism to produce 3,4-dihydroxyphenylvaleric acid, which is further degraded into phenolic acids like 3,4-dihydroxyphenylpropionic acid and 3,4-dihydroxybenzoic acid [108]. Since these degradation products are more readily absorbed than the original polyphenol compounds, it was suggested that they might impact biological activity.
In addition, recent reports suggest that polyphenol consumption causes temporary changes to the composition of microbiota [107]. These alterations in microbiota in the gut modulate the intestinal barrier function, innate and adaptive immune response, and signaling pathways and then impact host homeostasis [109]. However, only a limited number of papers in relation to this are reported to date, and the relationship between the alterations in the intestinal environment of polyphenols and their positive effects on the central nervous system, cardiovascular system, and inner ear is uncertain. Nevertheless, the mechanism by which polyphenols show preventive or therapeutic effects against inner ear disorders has attracted much attention. Therefore, we selected papers related to polyphenols and hearing loss from Google Scholar, Scopus, PubMed, and the Web of Science using the following keywords in June 2023: “polyphenol, flavonoid, flavanol, flavanon, flavone, flavonol, flavanonol, isoflavon, procyanidin, anthocyanin, chalcone, tannin, phenolc acid, and/or curcumin” and “hearing loss, hair cell, and/or neurodegeneration”. In addition, papers containing mixtures of polyphenols such as plant extracts or whose contents were unknown were excluded from the selection. We additionally examined the literature on the bioavailability of compounds whose effectiveness was expressed in the survey findings.
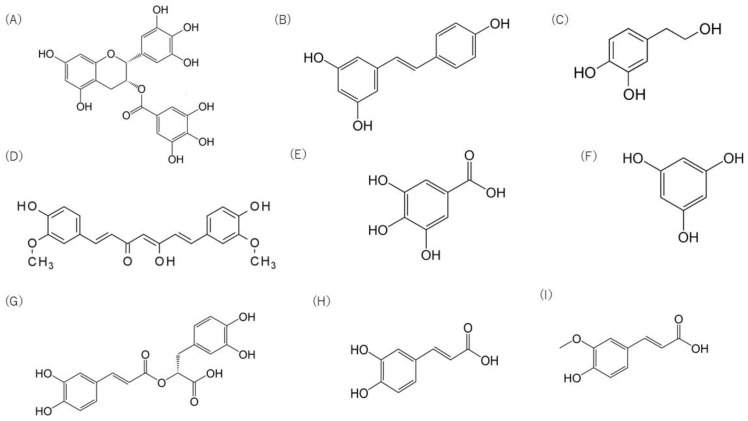
4.1. Flavonoids
Flavonoids are a group of compounds characterized by a backbone of 15 carbon atoms and two phenyl rings A and B linked by a heterocyclic (pyran) ring [110]. Epigallocatechin gallate (EGCG, Figure 3A), a flavanol as a subgroup of flavonoids, is the most representative polyphenolic compound found in green tea [111]. The anti-inflammatory activities of EGCG are well demonstrated in in vitro and in vivo models, accompanied by increased Nrf2 signaling and inhibited NFkB pathway through its antioxidant activity [112,113,114]. These effects are not observed in Nrf2 knockout mice or their cells, suggesting that EC indirectly induces Nrf2 and its underlying signals to exert its effect [113]. EGCG was reported to inhibit NO-mediated ototoxicity. Kim et al. examined the preventive effect of EGCG on a HEI-OC1 auditory cells ototoxicity model using RNS generated by S-nitroso-N-acetylpenicillamine (SNAP), an NO donor. SNAP released cytochrome c and activated caspase-3 from the cells, but EGCG inhibited this change and the subsequent reduction in cell viability [115,116,117]. EGCG also reduced SNAP-induced destruction of hair cell arrays in the organ of Corti by suppressing the activation of caspase-3/NF-κB. It was also suggested that EGCG may protect cochlear hair cells from the ototoxic drug gentamicin. Gentamicin is known to increase γ-secrectase activity and to suppress Notch signaling, which inhibits hair cell proliferation. EGCG inhibited γ-secretase activity and promoted hair cell proliferation and regeneration in the damaged cochlea [118]. ROS and RNS in the cochlea, which increase with age, are known to cause age-related hearing loss. It was reported that the redox balance in the cochlea of rats fed for up to 24 months was gradually altered, with decreased SOD and GPx and increased total ROS/RNS and nitrotyrosine. However, supplementation with a mixture of flavonoids and other phenolics consisting of quercetin, rutin and morin, tannic acid, resveratrol, and gallic acid in their drinking water significantly inhibited these changes, thus protecting against ototoxicity [119]. In addition, flavanol derived from cocoa, consisted of (-)-epicatechin and its oligomers, inhibits the activation of senescence-related apoptotic signaling by decreasing oxidative stress in auditory senescent cells such as the HEI-OC1 cell, the stria vascularis-derived cell line SV-k1, and the organ of Corti (OC-k3) cells derived from the auditory organ of a transgenic mouse [120].
Figure 3.
Chemical structure of major polyphenolic compounds: (A) epigallocatechin gallate, (B) resveratrol, (C) hydroxytyrosol, (D) curcumin, (E) gallic acid, (F) phloroglucinol, (G) rosmarinic acid, (H) caffeic acid, (I) ferulic acid.
EGCG is shown to have poor bioavailability in human volunteers. The peak plasma concentration of EGCG 1.5–2.6 h after intake of green tea is in the submicromolar range and half-lives of it last for a few hours [121]. Moreover, the bioavailability of EGCG is only about 2%. This low bioavailability of EGCG is related to its instability in the intestine, poor pharmacokinetic properties, and tissue accumulation. It is also well known that cocoa flavanols have poor bioavailability [122]. In particular, the oligomers that make up 80% of them are not absorbed at all and can only be detected in small amounts in the blood [123,124]. Despite this low biophysical availability, it is very interesting that they prevent hair cell damage and understanding the mechanisms involved is important.
4.2. Stilbene
Stilbene is characterized by a carbon skeleton of 1,2-diphenylethylene (C6–C2–C6), consisting of an ethylene moiety in the middle of two benzene rings [125]. Several plants produce natural stilbenes to protect themselves against stress conditions such as excessive ultraviolet (UV) radiation, heat, insect attack, and fungal or the bacterial infection Pecyna. The neuroactive compounds of blueberry pterostilbene possess the ability to activate cellular resilience pathways Nrf2-dependent scavenging free radicals and inhibiting the NF-κB inflammatory pathway and consequently protecting against oxidative, inflammatory cell damage, and cytotoxicity [126]. Resveratrol (Figure 3B) is a compound with three hydroxyl groups with a stilbene skeleton and is found in fruits such as grapes and grape products, especially red wine. It exhibits health-promoting effects including prevention and/or treatment of neurodegenerative disorders modulating the Nrf2 pathway and stress resilience vitagenes [127]. It was also revealed that resveratrol protects cochlear cells from cisplatin-induced ototoxicity [128] and neuronal cells from hydrogen peroxide-induced oxidative damage dose-dependently [129]. Consistent with hormesis, in vitro studies have shown that a low dose (50 μM) of resveratrol significantly attenuates CoCl2-induced cochlear hair cell damage via activation of Sirt1, which deacetylates NF-κB [130]. Similarly, in vivo studies have demonstrated that a low dose (0.5 mg/kg) of resveratrol exerts otoprotective effects on cisplatin-induced ototoxicity by reducing hearing loss and inflammatory responses (NF-κB, IL6, and IL1β), as well as increasing the expression of antioxidant molecules (CYP1A1 and RAGE). On the other hand, a high-dose (50 mg) of resveratrol activated pro-inflammatory cytokines and did not ameliorate cisplatin-induced ototoxicity [131]. Moreover, a low-dose of resveratrol inhibited serine/threonine protein kinase (RIPK3)-mediated necroptosis in aging cochlea and delayed the onset of age-related hearing loss in old mice [132]. In addition, resveratrol at a low dose of 10 mg/kg also exerted potent antioxidant effects against amikacin ototoxicity in rats [133]. Notably, intratympanic dexamethasone in synergy with resveratrol provided significant protection against cisplatin-induced ototoxicity in rats [134]. Importantly, resveratrol is the first natural agonist of Sirt1 and induces protection of cochlear hair cells, delaying age-related hearing loss via autophagy. Specifically, the activation of Sirt1 modulates the deacetylation status of ATG9A, which acts as a sensor of endoplasmic reticulum stress and restores cochlear autophagy impairment in C57BL/6 AHL mice [135]. Furthermore, resveratrol upregulated miR-455-5p, reducing apoptosis and oxidative stress in HEI-OC1 cells and inhibiting hair cell damage in cochlear tissues from cisplatin-treated mice via the PTEN-PI3K-Akt signaling pathway [136]. The imbalance of mitophagy and mitochondrial biogenesis is present in the cochlear hair cells during aging or under oxidative stress, contributing to mitochondrial dysfunction and cell damage. In this regard, it was shown that long-term supplementation with resveratrol targeting Sirt1 enhanced mitochondrial function and attenuated spiral ganglion neuron loss in the aging cochlea [137], as well as improving resistance to intense noise exposure damage [138]. Likewise, the pharmacological inhibition of an miR-34a deficiency protected cochlear hair cells and improved age-related hearing loss induced by oxidative stress in C57BL/6 mice [137]. Resveratrol also exhibits promising neuroprotective effects by modulating antioxidant and anti-inflammatory pathways. Other recent evidence showed that resveratrol reduced the phosphorylated and acetylated levels of NF-κB and STAT3, as well as attenuated manganese-induced oxidative stress and inflammatory cytokines by activating Sirt1 signaling. Conversely, EX527, a potent Sirt1 inhibitor, inactivated Sirt1 by inhibiting resveratrol in adult mice [121]. Notably, resveratrol (100 mg/kg) exerted cognitive enhancement and neuroprotection against amyloid and tau pathologies by increasing AMPK protein levels and upregulating the SIRT1 pathway in AD transgenic mice. The improvement of proteostasis by resveratrol, in both healthy and AD mice, suggests that it is a mechanism of brain resilience and defense against neurodegeneration caused by the accumulation of aberrant proteins [122]. Importantly, resveratrol induced significant changes in BBB permeability, edema formation, and the distribution of aquaporin 1 and 4, in addition to the astrocyte profile in the animal model of autism [123]. Taken together, stilbenes, especially resveratrol, induce protection in moderate doses by activating vitagenes, primarily targeting the Sirt1 pathway, and this could provide a promising antioxidant therapeutic strategy to delay the neurodegeneration of vulnerable neurons leading to hearing loss and brain dysfunction in humans.
Resveratrol shows high intestinal absorption and rapid and intense metabolism in the gastrointestinal tract and/or liver [139]. Recent stable isotope-labeled studies have reported a high resveratrol absorption rate of 43.9 ± 25.9% [140]. Only resveratrol conjugated derivatives are detected in plasma, such as glucuronide, sulfate, and methoxy forms, with little unchanged form. These resveratrol metabolites might interfere with its therapeutic use because of their difficulty in crossing cell membranes, particularly the BBB, due to their water solubility.
4.3. Hydroxytyrosol
Hydroxytyrosol (HT, Figure 3C) is a metabolite of the secoiridoid compound oleuropein found in green olive skins, seeds, and leaves. The degradation of oleuropein to hydroxytyrosol, elenolic acid, and glucose is promoted by acid or heat treatment [141], similar to that in the gastrointestinal tract. In an isotopic study, 90% of ingested HT was absorbed and excreted in the urine within 5 h, suggesting that HT is readily absorbed [142]. The peak of HT in plasma was reported to occur 0.5–1 h after administration. Absorbed HT is oxidized by phase I enzymes to 3,4-dihydroxyphenylacetic acid (DOPAC) and 3,4-dihydroxyphenylacetaldehyde, metabolites produced in the dopamine pathway, which are subsequently metabolized by phase II reactions to O-methylated forms, specifically homovanillic acid [143]. Recent research has focused on the brain health benefits of the major olive oil polyphenols, especially HT and HT-rich aqueous olive pulp extract (Hidrox®), which exert multiple preventive and pharmacological activities at low doses, such as antioxidant [144], anti-aging [24], and anti-proliferative effects in vitro and in vivo [145]. Among the phenolic compounds, hydroxytyrosol (50–70%) is the major constituent of the pulp extract, while other polyphenols present include oleuropein (5–10%), tyrosol (0.3%), oleuropein aglycone, and gallic acid [144]. In vitro studies on endothelial cells [146] and the human monocytic cell line [147] have highlighted the ability of HT to downregulate NF-κB activation and its translocation into the nucleus. Recent double-blind randomized preclinical studies have shown that the neuroprotective effect of a HT-enriched diet, in particular a dose of 45 mg HT/kg BW/day, favors recovery after ischemic stroke by improving stroke-associated learning and motor impairments. This effect is probably related to an increase in cerebral blood flow (CBF). In addition, a growing body of evidence reports the brain health benefits of HT supplementation, which at a dose of (50 mg/kg diet) improved cognitive function and reduced Aβ42 and pE3-Aβ plaque in the cortex of TgCRND8 mice [148]. Furthermore, aged mice were shown to have a downregulation of Sirt1, CREB, Gap43 and GPx-1 gene expression in brain tissue [149]. Also in the inner ear, the right dose range is essential to explain the protective effects of antioxidants. Indeed, a high dose of hydroxytyrosol (100 uM) was reported to induce cisplatin-induced ototoxicity in vitro via apoptosis-related JNK and AIF pathways [150].
4.4. Curcumin
Curcumin (Figure 3D), diferuloylmethane, is a bright yellow lipophilic pigment found in turmeric [151]. Curcumin is present in the root of the Curcuma longa herb, originally from Asia, in particular from India and Pakistan, a nutritional compound commonly used in food as a spice, mainly in the traditional cuisine of these geographical areas (Middle Eastern and Indian) [152]. The root is the component of greatest nutritional interest, it consists of an aromatic rhizome, yellow or orange in color. Curcuma longa possesses powerful biological activities and has various properties, including antioxidant, anti-inflammatory, antiviral, antibacterial, immunomodulatory, and anticancer activities. It was widely proven since ancient times that this polyphenolic compound has anti-inflammatory characteristics. Due to its anti-inflammatory action, both in the acute and chronic phase, it acts on the arachidonic acid cascade, at the level of cyclooxygenase and lipoxygenase enzymes [153] blocking the synthesis of inflammatory mediators, prostaglandins, and leukotrienes. Curcumin is a strong antioxidant and is one of the compounds expected to be effective against neurodegenerative diseases [154]. In AD model cells, it was reported that curcumin suppresses oxidative stress and increases cell viability by activating the Nrf2 pathway with increased DNA repair enzyme expressions [155]. Curcumin was also shown to improve rotational behavior in rotenone-induced PD rats by reducing oxidative stress via Nrf2 signaling activation. In rats, curcumin alone and/or in synergy with vitamin E prevented cisplatin ototoxicity [156]. In addition, curcumin treatment at a dose of 200 mg attenuated cisplatin-induced ototoxicity and hearing loss by decreasing 4-HNE expression and increasing HO-1 expression in rats [157].
Moreover, dietary curcumin is extensively bio-transformed in phases I and II. A reductase reduces the double bonds of curcumin in enterocytes and hepatocytes to curcumin derivatives [103]. These curcumin derivatives are rapidly absorbed and then found in small amounts in the blood. The plasma concentration ranged from 1 to 3200 ng/mL depending on the dose, which ranged from 2 to 10 g [158]. Studies have shown that curcumin’s bioavailability remains a barrier to understanding the mechanisms behind its neuroprotective effects.
4.5. Tannins
Tannins, a class of polyphenolic biomolecules, are large polyphenolic compounds containing sufficient hydroxyl moiety to form strong complexes with various macromolecules. The chemical structures of plant tannins are diverse and can be broadly divided into hydrolyzed tannins and condensed tannins. Hydrolyzed tannins consist of polyphenol nuclei and condensed tannins are oligomeric or polymeric flavan 3-ols with molecular weights ranging from 500 to 20,000 Da [159]. Pomegranate fruit is known to be rich in hydrolyzable tannins, a type of tannin that yields gallic acid on heating with hydrochloric or sulfuric acids (Figure 3E). Administration of pomegranate extract rich in hydrolyzable tannins inhibited cisplatin-induced reduction in distortion product otoacoustic emissions and reduction in mid-turn external ciliated cells in the cochlea [160]. Phlorotannins, the oligomer of phloroglucinol (Figure 3F), are tannins found in brown and red algae. It was reported that dieckol, a phlorotannin, prevents gentamicin-induced hair cell loss in rat cochlear explants [161]. It was also reported that dieckol or phlorofucofuroeckol A, a phlorotannin, suppressed the shift of auditory brainstem response threshold by noise exposure in mice. These phlorotannins showed higher hair cell survival after exposure in the apical turn. In general, highly polymerized, high-molecular-weight tannins are poorly absorbed in the small intestine [162]. The biological activity of tannins was thought to be limited to localized areas such as the gastrointestinal tract so far. Because tannins are a large molecule among polyphenols, ranging from 500 Da to 20 kDa, their bioavailability is known to be extremely low [163]. It is, therefore, unclear whether the efficacy of tannins on the inner ear is due to the breakdown of high-molecular-weight tannins into more bioavailable low-molecular-weight compounds or whether they have an entirely different mechanism.
4.6. Phenolic Acid
Rosmarinic acid (RA, Figure 3G is an ester of caffeic acid and 3,4-dihydroxyphenyl lactic acid. It is widely distributed in the Lamiaceae family: basil, lemon balm, rosemary, marjoram, sage, thyme, and peppermint [164]. It was shown to have potent anti-inflammatory properties through antioxidant activities in animal models such as the house dust mite allergy model [165], diesel exhaust particle-induced lung injury model [166], LPS-induced liver damage model [167], or phorbol ester-induced skin irritation model [168], as well as seasonal allergic rhinoconjunctivitis in clinical trials [169,170]. The preventive effect of RA on Cd2+-induced ototoxicity in vitro and ex vivo was reported. The results showed that RA inhibited ROS generation, IL-6 and IL-1β production, and caspase-3 translocation in the auditory cells HEI-OC1. RA also prevented the destruction of hair cell arrays in the rat organ of Corti primary explants induced by Cd2+ [171]. It was reported that RA inhibits apoptosis in the primary organ of Corti explants. Administration of RA reduced the thresholds of the auditory brainstem response in cisplatin-injected mice, along with inhibiting the caspase-1 downstream signaling pathway, such as activation of caspase-3 and -9, release of cytochrome c, translocation of apoptosis-inducing factor, upregulation of Bax, downregulation of Bcl-2, generation of ROS, and activation of NFκB [172]. Trans-tympanic and systemic administration of RA were previously compared to prevent damage to hair cells caused by noise exposure. Systemic administration of RA to rats, similar to the trans-tympanic treatment, significantly reduced noise-induced hearing loss, and improvement in auditory function paralleled the significant reduction in cochlear oxidative stress, such as O2− production and lipid peroxidation, [173]. In addition, RA potentiates the Nrf2/HO-1 signaling pathway, resulting in endogenous antioxidant defenses, as decreased O2− production and the expression of 4-HNE, and upregulation of SODs. Finally, RA attenuates noise-induced hearing loss, reducing the threshold shift, and promotes hair cell survival [174]. In rodents and humans, approximately 75% of orally administered RA was reported to be excreted in the urine and detected as metabolites. In addition to methylated RA, the degradation products of RA, caffeic acid (Figure 3H), ferulic acid (Figure 3I), and their conjugates (glucuronide and/or sulfate) were detected in plasma [170,175]. Therefore, it is unclear whether the beneficial effects on hair cells are mediated by RA or its breakdown products, such as caffeic acid or ferulic acid, produced during absorption from the gut and passage through the liver. In fact, caffeic acid, a breakdown product of RA, and its esters were reported to prevent inner ear damage. In streptozotocin-induced ototoxicity, intramuscular administration of caffeic acid ester prevented otoacoustic emissions and the loss of hair cells [176]. Caffeic acid also inhibited hair cell damage induced by cisplatin in vitro [177], or neomycin-induced cell damage in zebrafish [178]. It also prevented HEI-OC1 cell damage by the cisplatin treatment in vitro [179]. Furthermore, noise-induced hearing loss in guinea pigs was significantly reduced by the administration of ferulic acid [180,181]. Based on these findings, it will be necessary to verify the in vivo degradation process of RA to determine the mechanism by which the beneficial effects of RA on inner ear dysfunction occur.
5. Attempt to Increase the Bioavailability of Polyphenols
As mentioned above, polyphenols were shown to suppress hair cell damage and potentially reduce the risk of hearing loss. However, one of the limitations to the effectiveness of polyphenols is their poor bioavailability. Therefore, numerous attempts are currently being made to improve the bioavailability of polyphenols. The development of formulations and delivery systems, such as prodrugs or conjugates using nanotechnologies to target the appropriate molecules, has been attempted [182]. For instance, resveratrol-loaded PLGA nanoparticles were observed to enhance resveratrol penetration into the BBB and induce neuroprotection within the brain in experimental models of PD [183]. Of equal importance, the oral administration of novel resveratrol-selenium peptide nanoparticles was reported to effectively improve cognitive dysfunction by interacting with Aβ and decreasing Aβ aggregation and deposition in the hippocampus, reducing Aβ-induced ROS and increasing the activity of antioxidant enzymes in PC12 cells and in vivo. Furthermore, in the same study, resveratrol downregulated Aβ-induced neuroinflammation via the NF-κB/mitogen-activated protein kinase/Akt signaling pathway in BV-2 cells and in vivo and alleviated gut microbiota disturbance, particularly as regards oxidative stress and inflammation-related bacteria such as Alistipes, Helicobacter, Rikenella, Desulfovibrio, and Faecalibaculum [184]. Similar results were also shown in the inner ear disorders via resveratrol-loaded polymer nanoparticles, which did not show any cytotoxicity in vitro and thus could be a suitable model for antioxidant delivery in the cochlea for otoprotection [185]. Nano-encapsulated curcumin administered with dexamethasone protected against cisplatin-induced hearing loss by reducing toxic damage to auditory cells in animal models [186]. Curcumin nanoparticles at a much lower dose than dexamethasone provided otoprotection via the inhibition of Caspase-3 and Bax activation, thereby reducing the concentration of ROS and protecting mitochondrial integrity in hair cells in vitro and in vivo [187]. Interestingly, Yamaguchi and coworkers demonstrated that curcumin abolished intranuclear translocation of nuclear factor-κB-p65 and the generation of 4-hydroxynonenal-adducted proteins found in the cochlea after noise exposure. In particular, Theracurmin®, a highly absorbable and bioavailable preparation of curcumin, has shown preventive solid effects on hearing loss induced by repeated noise exposure and suggests it is a promising therapeutic candidate for preventing sensorineural hearing loss [188].
6. Development of Model Systems to Elucidate the Hearing Loss Prevention Mechanism of Polyphenols
Clarifying the process by which polyphenols reduce the risk of hearing loss by protecting hair cells is a key priority, as is improving their bioavailability. For this purpose, two model systems are currently considered promising.
6.1. C. elegans Models
C. elegans is an approximately 1 mm long free-living nematode, which exists predominantly as a self-fertilizing hermaphrodite with a minor percentage of males. It has a rapid life cycle, high reproductive capacity, and limited adult life span of about three weeks under standard culture conditions. The C. elegans genome displays about 80% homology to human sequences and more than 42% to human disease-related genes [189]. Functional studies of corresponding or related human genes can be performed either with various mutants available or by RNA interference (RNAi), the latter being easily and exclusively achieved in the nematodes by feeding Escherichia coli expressing target-gene dsRNA [190]. Moreover, in the absence of endogenous homologues, C. elegans can be transgenically manipulated to express human disease-associated genes in specific cell types, including neurons [191]. Even the co-expression of pathogenic proteins is possible, as was exemplified for the co-expression of β-amyloid and tau, both involved in the pathogenesis of Alzheimer’s disease [192], or for β-amyloid and α-synuclein reflecting the pathogenesis of Lewy-body dementia [193]. Finally, the transparency of C. elegans allows the in vivo visualization of neuronal function expression of fluorescent protein reporters in free form or attached to transgenic proteins [194,195]. The primary functional constituents of synaptic transmission found in mammals, including transmitters, receptors, transporters, and ion channels, are preserved in C. elegans. Consequently, it could be valuable in assessing hearing impairment.
There are, moreover, C. elegans models for further neurodegenerative diseases such as amyotrophic lateral sclerosis, frontotemporal dementia, or Huntington’s disease [196]. Especially for the first, disturbed redox balance appears to represent a pathomechanism. Pan-neuronal expression of the G85R mutant of superoxide dismutase in C. elegans is associated with locomotor defects, development of aggregates, and axonal abnormalities [196]. C. elegans can be a viable model for neurodevelopmental disorders, depicting challenges in social interaction and communication like autism, and displays great versatility for application.
Like humans, C. elegans exhibits a decline in physical ability with age and loss of ability to recover from stress. Those alterations are expressed in the nematodes by reduced body movement and increased sensitivity to heat and oxidative stress [197], These findings suggest that C. elegans could be utilized as an advantageous model for evaluating hearing impairment and defects in auditory neurodegeneration. Additionally, it is promising that C. elegans is highly responsive to antioxidant nutrients.
Various secondary plant compounds were shown to improve the phenotype in C. elegans models of neurodegeneration. In a recent study, the flavonoid chrysin reduced the α-synuclein-induced toxicity in so far as the degeneration of dopaminergic neurons and food-sensing behavioral disabilities, both of which occur after the administration of 6-hydroxydopamine [198]. Chrysin triggered the ubiquitin-like proteasome and superoxide dismutase activities, in agreement with the general concept that oxidative stress and accumulation of non-functional cellular proteins underlie the degeneration of neurons in various neurodegenerative diseases [198]. Hydroxytyrosol from olive oil in its “natural” environment in C. elegans Parkinson´s disease models, characterized either by α-synuclein expression in muscles or in dopaminergic neurons, was shown by the authors to significantly improve swimming performance [24]. 10-O-trans-p-Coumaroylcatalpol, a monoterpene extracted from arni, was demonstrated to decrease the aggregation of α-synuclein in transgenic nematodes in association with an increased tolerance against chemical-induced stress, improved chemotaxis index, and reduced content of reactive oxygen species [199]. Moreover, catalpol improved the locomotory ability of aged nematodes, while lipofuscin levels were attenuated, suggesting that catalpol may affect age-associated changes of nematode [200]. At the molecular level, these effects appear to be mediated through DAF-16 and SKN-1, orthologues of mammalian FOXO-transcription factors, and Nrf2, respectively [200].
In a C. elegans strain expressing β-amyloid, we demonstrated that the polyphenol quercetin, occurring in substantial amounts in apples and onions, dose-dependently decreased the amount of aggregated proteins in solution and also paralysis [201]. Those effects were mediated through the activation of proteasomal protein degradation or macroautophagy, as discovered when using RNA-interference for members of those pathways [201]. Quercetin, together with kaempferol, were identified as two major effective compounds of Ginkgo biloba extract with regard to the attenuation of basal H2O2-related reactive oxygen species, which increase in wild-type C. elegans with age, but also in a strain with constitutive β-amyloid expression, where initial rates of reactive oxygen species are greatly increased versus the wild-type nematodes [202]. Also, with regard to Alzheimer´s disease, ingredients of olive oil show promising results. Here, it is oleuropein aglycone (OLE), the most abundant polyphenol in extra virgin olive oil, which caused reduced β-amyloid plaque deposition, less abundant toxic β-amyloid oligomers, and decreased paralysis of nematodes expressing β-amyloid in muscle cells [203]. So far, however, investigations of promising compounds from plant food in C. elegans models for neurodegeneration are rather scarce.
6.2. Organoid Models
The complexity of brain and sensory nerve architecture and physiology, and the scarcity of approaches available, have limited the investigation of their functions over the years. The advent of human-induced pluripotent stem cell (hiPSC) technology and the development of three-dimensional organoid models boosted the opportunities for studying brain function and disorders in in vitro models. hiPSCs are generated by reprogramming adult human cells, obtained from tissues such as skin, blood, or urine, into a pluripotent state [204,205]. The 3D culture system provides the right environment for the stem cells so they can follow their own genetic instructions to self-organize, forming an organ-like tissue composed of multiple cell types. Neural differentiation protocols allow the formation of key features of brain-specific cytoarchitecture and brain processes, including synaptogenesis, differentiation, cell migration, and cell–cell and cell–matrix interactions. This provides researchers with a limitless supply of human organotypic models that recapitulate sophisticated aspects of human in vivo organs, enabling experimental studies that are difficult or impossible to conduct in human subjects [206]. Using brain organoids with these properties has provided a detailed understanding of age-related auditory neuropathy and is valuable for developing therapeutic and preventive strategies for physiologically active substances, such as the polyphenols found in food.
Furthermore, several pathological characteristics of neuropsychiatric disorders were recapitulated using human brain organoids [207]. For example, genetically modified iPSC brain organoids carrying mutations in CHD8 (chromodomain helicase DNA-binding protein 8), one of the most commonly mutated genes in patients with autism spectrum disorder (ASD), bipolar disorder (BPI), schizophrenia and intellectual disabilities, were generated [208,209]. Accordingly, current technology makes it nearly possible to establish a model for hearing organ damage by employing organoids and building an experimental setup capable of assessing active compounds, like polyphenols.
7. Polyphenol and the Hormesis Paradigm: Conclusions and Future Perspectives
This review proposes that polyphenols are an effective and clinically applicable way to prevent or delay the onset of hearing loss by activating vitagenes such as Nrf2 and HSP. In addition, these effects, as typified by resveratrol, have potential effectiveness within a hormetic response framework. This conclusion is supported by a limited but consistent series of studies, as summarized below. These studies consist of various experimental protocols, including both direct stimulation and chemoprotective studies within preconditioning protocols. When appropriate dosages were used, the dose–response pattern follows a biphasic dose–response that mirrors the quantitative characteristics of the hormetic dose–response [210]. Additionally, the unified mechanism for hormetic-induced chemoprevention is shown to involve the activation of Nrf2 (Figure 2), as extensively demonstrated in this study. Despite the generally observed hormetic dose–response pattern, it is probable that each studied clinical endpoint has its specific hormetic pattern regarding dose optimality and the quantitative pattern for the stimulatory amplitude and width of the protective treatment zone [211]. However, although there may be variations in the dose–response optimality for specific endpoints, several clinical studies have demonstrated effective dosing for various endpoints at comparable doses. This indicates a potential overlap in the optimal range for multiple therapeutic endpoints, all operating within a comparable hormetic dose–response and mechanistic strategy. These findings may prevent a wide range of neurodegenerative disorders through hormetic mechanisms among diverse groups of people who have varying risk factors for these disorders. This could prove to be an effective public health strategy with widespread implications [212,213,214]. Such a preventive strategy at the population level has the potential to revolutionize public health practices with the realistic objective of considerably reducing the onset and severity of neurodegenerative diseases within society.
Although data from experimental studies look convincing, further well-designed clinical trials are needed to confirm the use of polyphenols for the prevention and treatment of hearing loss, including auditory hair cell and XIII cranial/auditory nerve cell degeneration. Future research could be directed to assessing potential synergy at low doses of the several key active constituents. However, such interactions would likely display a maximum therapeutic response that would to be limited to a 30–60% improvement range of the hormetic dose–response. These suggestive general findings have the potential to guide future studies with respect to the doses employed in the experimental and clinical evaluations. In addition, the employment of polyphenols in the prevention strategies encounters various challenges. Researchers are presently working to increase the preventive effects of polyphenols by improving their bioavailability but further testing is needed to determine whether their efforts will be successful. As previously indicated, there are reports verifying that the ingestion of polyphenols results in significant changes to the intestinal environment. It cannot be excluded that this may have some influence on sensory function. Further research is necessary to comprehend the exact mechanisms that underlie the advantageous impacts of polyphenols.
Overall, the data highlight the neuropharmacological relevance of hormetic nutrition from dietary polyphenols and the upregulation of the stress resilience Nrf2/vitagenes axis as a potential therapeutic target to counteract oxidative stress and inflammation, as well as to prevent neuronal loss associated with neurodegeneration ensuring brain health in humans [215].
Acknowledgments
The authors extend their appreciation to the Deanship of Scientific Research and the Research Center, College of Pharmacy, King Saud University for their financial support.
Author Contributions
Conceptualization, N.O., E.G., L.M., G.L., C.D.A., U.W., E.J.C., R.M.V. and V.C.; Methodology, F.R., V.Z., M.R.M., D.M. and M.L.O.; Validation, S.M., G.L., C.D.A. and M.L.O.; Draft Preparation, N.O., E.G., T.F. and V.C.; Writing—review and editing, N.O., S.M., A.S.A., E.G., R.M.V., E.J.C. and V.C.; Resources, V.C. and A.S.A. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Funding Statement
This study was supported by grants from “Piano di incentivi per la Ricerca, Linea Intervento 2 PIACERI, 2020–2022”, University of Catania, Italy.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Ferlito S., Fadda G., Lechien J.R., Cammaroto G., Bartel R., Borello A., Cavallo G., Piccinini F., La Mantia I., Cocuzza S., et al. Type 1 tympanoplasty outcomes between cartilage and temporal fascia grafts: A long-term retrospective study. J. Clin. Med. 2022;11:7000. doi: 10.3390/jcm11237000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aldè M., Cantarella G., Zanetti D., Pignataro L., La Mantia I., Maiolino L., Ferlito S., Di Mauro P., Cocuzza S., Lechien J.R., et al. Autosomal dominant non-syndromic hearing loss (dfna): A comprehensive narrative review. Biomedicines. 2023;11:1616. doi: 10.3390/biomedicines11061616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choi S., Kim S., Lee J., Lim H., Kim Y., Tian C., So H., Park R., Choung Y. Gingko biloba extracts protect auditory hair cells from cisplatin-induced ototoxicity by inhibiting perturbation of gap junctional intercellular communication. Neuroscience. 2013;244:49–61. doi: 10.1016/j.neuroscience.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Wang C., Wang B. Ginkgo biloba extract attenuates oxidative stress and apoptosis in mouse cochlear neural stem cells. Phytother. Res. 2016;30:774–780. doi: 10.1002/ptr.5572. [DOI] [PubMed] [Google Scholar]
- 5.Wang C., Han Z. Ginkgo Biloba Extract Enhances Differentiation and Performance of Neural Stem Cells in Mouse Cochlea. Cell. Mol. Neurobiol. 2015;35:861–869. doi: 10.1007/s10571-015-0180-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Han J., Wang M., Jing X., Shi H., Ren M., Lou H. (−)-Epigallocatechin Gallate Protects against Cerebral Ischemia-Induced Oxidative Stress via Nrf2/ARE Signaling. Neurochem. Res. 2014;39:1292–1299. doi: 10.1007/s11064-014-1311-5. [DOI] [PubMed] [Google Scholar]
- 7.Choung Y.-H., Kim S.W., Tian C., Min J.Y., Lee H.K., Park S.-N., Bin Lee J., Park K. Korean red ginseng prevents gentamicin-induced hearing loss in rats. Laryngoscope. 2011;121:1294–1302. doi: 10.1002/lary.21756. [DOI] [PubMed] [Google Scholar]
- 8.Koo D.Y., Lee S.H., Lee S., Chang J., Jung H.H., Im G.J. Comparison of the effects of lipoic acid and glutathione against cisplatin-induced ototoxicity in auditory cells. Int. J. Pediatr. Otorhinolaryngol. 2016;91:30–36. doi: 10.1016/j.ijporl.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Gonzales G.B., Smagghe G., Grootaert C., Zotti M., Raes K., Van Camp J. Flavonoid interactions during digestion, absorption, distribution and metabolism: A sequential structure–activity/property relationship-based approach in the study of bioavailability and bioactivity. Drug Metab. Rev. 2015;47:175–190. doi: 10.3109/03602532.2014.1003649. [DOI] [PubMed] [Google Scholar]
- 10.Boas S.M., Joyce K.L., Cowell R.M. The NRF2-Dependent Transcriptional Regulation of Antioxidant Defense Pathways: Relevance for Cell Type-Specific Vulnerability to Neurodegeneration and Therapeutic Intervention. Antioxidants. 2021;11:8. doi: 10.3390/antiox11010008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bórquez D.A., Urrutia P.J., Wilson C., van Zundert B., Núñez M.T., González-Billault C. Dissecting the role of redox signaling in neuronal development. J. Neurochem. 2016;137:506–517. doi: 10.1111/jnc.13581. [DOI] [PubMed] [Google Scholar]
- 12.Salim S. Oxidative Stress and the Central Nervous System. J. Pharmacol. Exp. Ther. 2017;360:201–205. doi: 10.1124/jpet.116.237503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sandberg M., Patil J., D’Angelo B., Weber S.G., Mallard C. NRF2-regulation in brain health and disease: Implication of cerebral inflammation. Neuropharmacology. 2014;79:298–306. doi: 10.1016/j.neuropharm.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moi P., Chan K., Asunis I., Cao A., Kan Y.W. Isolation of NF-E2-related factor 2 (Nrf2), a NF-E2-like basic leucine zipper transcriptional activator that binds to the tandem NF-E2/AP1 repeat of the beta-globin locus control region. Proc. Natl. Acad. Sci. USA. 1994;91:9926–9930. doi: 10.1073/pnas.91.21.9926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen W., Sun Z., Wang X.-J., Jiang T., Huang Z., Fang D., Zhang D.D. Direct Interaction between Nrf2 and p21Cip1/WAF1 Upregulates the Nrf2-Mediated Antioxidant Response. Mol. Cell. 2009;34:663–673. doi: 10.1016/j.molcel.2009.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vargas M.R., Johnson J.A. The Nrf2–ARE cytoprotective pathway in astrocytes. Expert Rev. Mol. Med. 2009;11:e17. doi: 10.1017/s1462399409001094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brandes M.S., Gray N.E. NRF2 as a Therapeutic Target in Neurodegenerative Diseases. ASN Neuro. 2020;12:1759091419899782. doi: 10.1177/1759091419899782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cordaro M., Salinaro A.T., Siracusa R., D’amico R., Impellizzeri D., Scuto M., Ontario M.L., Cuzzocrea S., Di Paola R., Fusco R., et al. Key Mechanisms and Potential Implications of Hericium erinaceus in NLRP3 Inflammasome Activation by Reactive Oxygen Species during Alzheimer’s Disease. Antioxidants. 2021;10:1664. doi: 10.3390/antiox10111664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cordaro M., Scuto M., Siracusa R., D’Amico R., Filippo Peritore A., Gugliandolo E., Fusco R., Crupi R., Impellizzeri D., Pozzebon M., et al. Effect of N-palmitoylethanolamine-oxazoline on comorbid neuropsychiatric disturbance associated with inflammatory bowel disease. FASEB J. 2020;34:4085–4106. doi: 10.1096/fj.201901584RR. [DOI] [PubMed] [Google Scholar]
- 20.Cordaro M., Salinaro A.T., Siracusa R., D’amico R., Impellizzeri D., Scuto M., Ontario M.L., Crea R., Cuzzocrea S., Di Paola R., et al. Hidrox® Roles in Neuroprotection: Biochemical Links between Traumatic Brain Injury and Alzheimer’s Disease. Antioxidants. 2021;10:818. doi: 10.3390/antiox10050818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cordaro M., Salinaro A.T., Siracusa R., D’Amico R., Impellizzeri D., Scuto M., Ontario M.L., Interdonato L., Crea R., Fusco R., et al. Hidrox® and Endometriosis: Biochemical Evaluation of Oxidative Stress and Pain. Antioxidants. 2021;10:720. doi: 10.3390/antiox10050720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fusco R., Salinaro A.T., Siracusa R., D’amico R., Impellizzeri D., Scuto M., Ontario M.L., Crea R., Cordaro M., Cuzzocrea S., et al. Hidrox® Counteracts Cyclophosphamide-Induced Male Infertility through NRF2 Pathways in a Mouse Model. Antioxidants. 2021;10:778. doi: 10.3390/antiox10050778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brunetti G., Di Rosa G., Scuto M., Leri M., Stefani M., Schmitz-Linneweber C., Calabrese V., Saul N. Healthspan Maintenance and Prevention of Parkinson’s-like Phenotypes with Hydroxytyrosol and Oleuropein Aglycone in C. elegans. Int. J. Mol. Sci. 2020;21:2588. doi: 10.3390/ijms21072588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Di Rosa G., Brunetti G., Scuto M., Salinaro A.T., Calabrese E.J., Crea R., Schmitz-Linneweber C., Calabrese V., Saul N. Healthspan Enhancement by Olive Polyphenols in C. elegans Wild Type and Parkinson’s Models. Int. J. Mol. Sci. 2020;21:3893. doi: 10.3390/ijms21113893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jembrek M.J., Oršolić N., Mandić L., Sadžak A., Šegota S. Anti-Oxidative, Anti-Inflammatory and Anti-Apoptotic Effects of Flavonols: Targeting Nrf2, NF-κB and p53 Pathways in Neurodegeneration. Antioxidants. 2021;10:1628. doi: 10.3390/antiox10101628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou Z.D., Xie S.P., Saw W.T., Ho P.G.H., Wang H.Y., Zhou L., Zhao Y., Tan E.K. The Therapeutic Implications of Tea Polyphenols Against Dopamine (DA) Neuron Degeneration in Parkinson’s Disease (PD) Cells. 2019;8:911. doi: 10.3390/cells8080911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amara I., Timoumi R., Annabi E., Di Rosa G., Scuto M., Najjar M.F., Calabrese V., Abid-Essefi S. Di (2-ethylhexyl) phthalate targets the thioredoxin system and the oxidative branch of the pentose phosphate pathway in liver of Balb/c mice. Environ. Toxicol. 2020;35:78–86. doi: 10.1002/tox.22844. [DOI] [PubMed] [Google Scholar]
- 28.Amara I., Scuto M., Zappalà A., Ontario M.L., Petralia A., Abid-Essefi S., Maiolino L., Signorile A., Salinaro A.T., Calabrese V. Hericium erinaceus Prevents DEHP-Induced Mitochondrial Dysfunction and Apoptosis in PC12 Cells. Int. J. Mol. Sci. 2020;21:2138. doi: 10.3390/ijms21062138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.D’amico R., Salinaro A.T., Fusco R., Cordaro M., Impellizzeri D., Scuto M., Ontario M.L., Dico G.L., Cuzzocrea S., Di Paola R., et al. Hericium erinaceus and Coriolus versicolor Modulate Molecular and Biochemical Changes after Traumatic Brain Injury. Antioxidants. 2021;10:898. doi: 10.3390/antiox10060898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scuto M., Salinaro A.T., Modafferi S., Polimeni A., Pfeffer T., Weigand T., Calabrese V., Schmitt C.P., Peters V. Carnosine Activates Cellular Stress Response in Podocytes and Reduces Glycative and Lipoperoxidative Stress. Biomedicines. 2020;8:177. doi: 10.3390/biomedicines8060177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cornelius C., Koverech G., Crupi R., Di Paola R., Koverech A., Lodato F., Scuto M., Salinaro A.T., Cuzzocrea S., Calabrese E.J., et al. Osteoporosis and alzheimer pathology: Role of cellular stress response and hormetic redox signaling in aging and bone remodeling. Front. Pharmacol. 2014;5:120. doi: 10.3389/fphar.2014.00120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cornelius C., Perrotta R., Graziano A., Calabrese E.J., Calabrese V. Stress responses, vitagenes and hormesis as critical determinants in aging and longevity: Mitochondria as a “chi”. Immun. Ageing. 2013;10:15. doi: 10.1186/1742-4933-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Amara I., Ontario M.L., Scuto M., Dico G.M.L., Sciuto S., Greco V., Abid-Essefi S., Signorile A., Salinaro A.T., Calabrese V. Moringa oleifera Protects SH-SY5YCells from DEHP-Induced Endoplasmic Reticulum Stress and Apoptosis. Antioxidants. 2021;10:532. doi: 10.3390/antiox10040532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salinaro A.T., Cornelius C., Koverech G., Koverech A., Scuto M., Lodato F., Fronte V., Muccilli V., Reibaldi M., Longo A., et al. Cellular stress response, redox status, and vitagenes in glaucoma: A systemic oxidant disorder linked to Alzheimer’s disease. Front. Pharmacol. 2014;5:129. doi: 10.3389/fphar.2014.00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Calabrese V., Santoro A., Salinaro A.T., Modafferi S., Scuto M., Albouchi F., Monti D., Giordano J., Zappia M., Franceschi C., et al. Hormetic approaches to the treatment of Parkinson’s disease: Perspectives and possibilities. J. Neurosci. Res. 2018;96:1641–1662. doi: 10.1002/jnr.24244. [DOI] [PubMed] [Google Scholar]
- 36.Calabrese E.J., Mattson M.P., Dhawan G., Kapoor R., Calabrese V., Giordano J. Hormesis: A potential strategic approach to the treatment of neurodegenerative disease. Int. Rev. Neurobiol. 2020;155:271–301. doi: 10.1016/bs.irn.2020.03.024. [DOI] [PubMed] [Google Scholar]
- 37.Abdalkader M., Lampinen R., Kanninen K.M., Malm T.M., Liddell J.R. Targeting Nrf2 to Suppress Ferroptosis and Mitochondrial Dysfunction in Neurodegeneration. Front. Neurosci. 2018;12:466. doi: 10.3389/fnins.2018.00466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johnson D.A., Johnson J.A. Nrf2—A therapeutic target for the treatment of neurodegenerative diseases. Free Radic. Biol. Med. 2015;88:253–267. doi: 10.1016/j.freeradbiomed.2015.07.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cuadrado A., Rojo A.I., Wells G., Hayes J.D., Cousin S.P., Rumsey W.L., Attucks O.C., Franklin S., Levonen A.-L., Kensler T.W., et al. Therapeutic targeting of the NRF2 and KEAP1 partnership in chronic diseases. Nat. Rev. Drug Discov. 2019;18:295–317. doi: 10.1038/s41573-018-0008-x. [DOI] [PubMed] [Google Scholar]
- 40.Ren P., Chen J., Li B., Zhang M., Yang B., Guo X., Chen Z., Cheng H., Wang P., Wang S., et al. Nrf2 Ablation Promotes Alzheimer’s Disease-Like Pathology in APP/PS1 Transgenic Mice: The Role of Neuroinflammation and Oxidative Stress. Oxidative Med. Cell. Longev. 2020;2020:3050971. doi: 10.1155/2020/3050971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ungvari Z., Tarantini S., Nyúl-Tóth Á., Kiss T., Yabluchanskiy A., Csipo T., Balasubramanian P., Lipecz A., Benyo Z., Csiszar A. Nrf2 dysfunction and impaired cellular resilience to oxidative stressors in the aged vasculature: From increased cellular senescence to the pathogenesis of age-related vascular diseases. GeroScience. 2019;41:727–738. doi: 10.1007/s11357-019-00107-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anandhan A., Nguyen N., Syal A., A Dreher L., Dodson M., Zhang D.D., Madhavan L. NRF2 Loss Accentuates Parkinsonian Pathology and Behavioral Dysfunction in Human α-Synuclein Overexpressing Mice. Aging Dis. 2021;12:964–982. doi: 10.14336/AD.2021.0511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Buendia I., Michalska P., Navarro E., Gameiro I., Egea J., León R. Nrf2–ARE pathway: An emerging target against oxidative stress and neuroinflammation in neurodegenerative diseases. Pharmacol. Ther. 2016;157:84–104. doi: 10.1016/j.pharmthera.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 44.Ontario M.L., Siracusa R., Modafferi S., Scuto M., Sciuto S., Greco V., Bertuccio M.P., Salinaro A.T., Crea R., Calabrese E.J., et al. Potential prevention and treatment of neurodegenerative disorders by olive polyphenols and hidrox. Mech. Ageing Dev. 2022;203:111637. doi: 10.1016/j.mad.2022.111637. [DOI] [PubMed] [Google Scholar]
- 45.Dinkova-Kostova A.T., Abramov A.Y. The emerging role of Nrf2 in mitochondrial function. Free. Radic. Biol. Med. 2015;88:179–188. doi: 10.1016/j.freeradbiomed.2015.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ryoo I.-G., Kwak M.-K. Regulatory crosstalk between the oxidative stress-related transcription factor Nfe2l2/Nrf2 and mitochondria. Toxicol. Appl. Pharmacol. 2018;359:24–33. doi: 10.1016/j.taap.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 47.Ammal Kaidery N., Ahuja M., Thomas B. Crosstalk between Nrf2 signaling and mitochondrial function in Parkinson’s disease. Mol. Cell. Neurosci. 2019;101:103413. doi: 10.1016/j.mcn.2019.103413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Surmeier D.J. Determinants of Dopaminergic Neuron Loss in Parkinson’s Disease. FEBS J. 2018;285:3657–3668. doi: 10.1111/febs.14607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Manochkumar J., Doss C.G.P., El-Seedi H.R., Efferth T., Ramamoorthy S. The neuroprotective potential of carotenoids in vitro and in vivo. Phytomedicine. 2021;91:153676. doi: 10.1016/j.phymed.2021.153676. [DOI] [PubMed] [Google Scholar]
- 50.Mattioli R., Francioso A., D’erme M., Trovato M., Mancini P., Piacentini L., Casale A.M., Wessjohann L., Gazzino R., Costantino P., et al. Anti-Inflammatory Activity of A Polyphenolic Extract from Arabidopsis thaliana in In Vitro and In Vivo Models of Alzheimer’s Disease. Int. J. Mol. Sci. 2019;20:708. doi: 10.3390/ijms20030708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yamakawa M.Y., Uchino K., Watanabe Y., Adachi T., Nakanishi M., Ichino H., Hongo K., Mizobata T., Kobayashi S., Nakashima K., et al. Anthocyanin suppresses the toxicity of Aβ deposits through diversion of molecular forms in in vitro and in vivo models of Alzheimer’s disease. Nutr. Neurosci. 2016;19:32–42. doi: 10.1179/1476830515Y.0000000042. [DOI] [PubMed] [Google Scholar]
- 52.Blandini F., Giuliano C., Cerri S. Potential therapeutic effects of polyphenols in Parkinson’s disease: In vivo and in vitro pre-clinical studies. Neural Regen. Res. 2021;16:234–241. doi: 10.4103/1673-5374.290879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Petramfar P., Hajari F., Yousefi G., Azadi S., Hamedi A. Efficacy of oral administration of licorice as an adjunct therapy on improving the symptoms of patients with Parkinson’s disease, A randomized double blinded clinical trial. J. Ethnopharmacol. 2020;247:112226. doi: 10.1016/j.jep.2019.112226. [DOI] [PubMed] [Google Scholar]
- 54.Hipp M.S., Kasturi P., Hartl F.U. The proteostasis network and its decline in ageing. Nat. Rev. Mol. Cell Biol. 2019;20:421–435. doi: 10.1038/s41580-019-0101-y. [DOI] [PubMed] [Google Scholar]
- 55.Tseng C.-S., Chao Y.-W., Liu Y.-H., Huang Y.-S., Chao H.-W. Dysregulated proteostasis network in neuronal diseases. Front. Cell Dev. Biol. 2023;11:1075215. doi: 10.3389/fcell.2023.1075215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Anckar J., Sistonen L. Regulation of HSF1 Function in the Heat Stress Response: Implications in Aging and Disease. Annu. Rev. Biochem. 2011;80:1089–1115. doi: 10.1146/annurev-biochem-060809-095203. [DOI] [PubMed] [Google Scholar]
- 57.Sivéry A., Courtade E., Thommen Q. A minimal titration model of the mammalian dynamical heat shock response. Phys. Biol. 2016;13:066008. doi: 10.1088/1478-3975/13/6/066008. [DOI] [PubMed] [Google Scholar]
- 58.Xu Y.-M., Huang D.-Y., Chiu J.-F., Lau A.T.Y. Post-Translational Modification of Human Heat Shock Factors and Their Functions: A Recent Update by Proteomic Approach. J. Proteome Res. 2012;11:2625–2634. doi: 10.1021/pr201151a. [DOI] [PubMed] [Google Scholar]
- 59.Kim E., Wang B., Sastry N., Masliah E., Nelson P.T., Cai H., Liao F.-F. NEDD4-mediated HSF1 degradation underlies α-synucleinopathy. Hum. Mol. Genet. 2016;25:211–222. doi: 10.1093/hmg/ddv445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gomez-Pastor R., Burchfiel E.T., Neef D.W., Jaeger A.M., Cabiscol E., McKinstry S.U., Doss A., Aballay A., Lo D.C., Akimov S.S., et al. Abnormal degradation of the neuronal stress-protective transcription factor HSF1 in Huntington’s disease. Nat. Commun. 2017;8:14405. doi: 10.1038/ncomms14405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gomez-Pastor R., Burchfiel E.T., Thiele D.J. Regulation of heat shock transcription factors and their roles in physiology and disease. Nat. Rev. Mol. Cell Biol. 2018;19:4–19. doi: 10.1038/nrm.2017.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hayashida N., Fujimoto M., Tan K., Prakasam R., Shinkawa T., Li L., Ichikawa H., Takii R., Nakai A. Heat shock factor 1 ameliorates proteotoxicity in cooperation with the transcription factor NFAT. EMBO J. 2010;29:3459–3469. doi: 10.1038/emboj.2010.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fujimoto M., Takaki E., Hayashi T., Kitaura Y., Tanaka Y., Inouye S., Nakai A. Active HSF1 Significantly Suppresses Polyglutamine Aggregate Formation in Cellular and Mouse Models. J. Biol. Chem. 2005;280:34908–34916. doi: 10.1074/jbc.M506288200. [DOI] [PubMed] [Google Scholar]
- 64.Shinkawa T., Tan K., Fujimoto M., Hayashida N., Yamamoto K., Takaki E., Takii R., Prakasam R., Inouye S., Mezger V., et al. Heat shock factor 2 is required for maintaining proteostasis against febrile-range thermal stress and polyglutamine aggregation. Mol. Biol. Cell. 2011;22:3571–3583. doi: 10.1091/mbc.e11-04-0330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liangliang X., Yonghui H., Shunmei E., Shoufang G., Wei Z., Jiangying Z. Dominant-positive HSF1 decreases alpha-synuclein level and alpha-synuclein-induced toxicity. Mol. Biol. Rep. 2010;37:1875–1881. doi: 10.1007/s11033-009-9623-2. [DOI] [PubMed] [Google Scholar]
- 66.Jiang Y.-Q., Wang X.-L., Cao X.-H., Ye Z.-Y., Li L., Cai W.-Q. Increased heat shock transcription factor 1 in the cerebellum reverses the deficiency of Purkinje cells in Alzheimer’s disease. Brain Res. 2013;1519:105–111. doi: 10.1016/j.brainres.2013.04.059. [DOI] [PubMed] [Google Scholar]
- 67.Chen Y., Wang B., Liu D., Li J.J., Xue Y., Sakata K., Zhu L.Q., Heldt S.A., Xu H., Liao F.-F. Hsp90 Chaperone Inhibitor 17-AAG Attenuates Aβ-Induced Synaptic Toxicity and Memory Impairment. J. Neurosci. 2014;34:2464–2470. doi: 10.1523/JNEUROSCI.0151-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Batulan Z., Shinder G.A., Minotti S., He B.P., Doroudchi M.M., Nalbantoglu J., Strong M.J., Durham H.D. High Threshold for Induction of the Stress Response in Motor Neurons Is Associated with Failure to Activate HSF1. J. Neurosci. 2003;23:5789–5798. doi: 10.1523/JNEUROSCI.23-13-05789.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Prodromou C., Aran-Guiu X., Oberoi J., Perna L., Chapple J.P., van der Spuy J. Hsp70-hsp90 chaperone networking in protein-misfolding disease. Subcell Biochem. 2023;101:389–425. doi: 10.1007/978-3-031-14740-1_13. [DOI] [PubMed] [Google Scholar]
- 70.Harrison R.T., DeBacker J.R., Trevino M., Bielefeld E.C., Lobarinas E. Cochlear Preconditioning as a Modulator of Susceptibility to Hearing Loss. Antioxid. Redox Signal. 2022;36:1215–1228. doi: 10.1089/ars.2021.0055. [DOI] [PubMed] [Google Scholar]
- 71.Zuo H., Cui B., She X., Wu M. Changes in Guinea Pig Cochlear Hair Cells after Sound Conditioning and Noise Exposure. J. Occup. Health. 2008;50:373–379. doi: 10.1539/joh.L8032. [DOI] [PubMed] [Google Scholar]
- 72.Zhu G., Wu Y., Qiu Y., Tian K., Mi W., Liu X., Chen Y., Jia J., Luo J., Lu L., et al. Hsp70/Bmi1-FoxO1-SOD Signaling Pathway Contributes to the Protective Effect of Sound Conditioning against Acute Acoustic Trauma in a Rat Model. Neural Plast. 2020;2020:8823785. doi: 10.1155/2020/8823785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schaffar G., Breuer P., Boteva R., Behrends C., Tzvetkov N., Strippel N., Sakahira H., Siegers K., Hayer-Hartl M., Hartl F. Cellular Toxicity of Polyglutamine Expansion Proteins: Mechanism of Transcription Factor Deactivation. Mol. Cell. 2004;15:95–105. doi: 10.1016/j.molcel.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 74.Muchowski P.J., Schaffar G., Sittler A., Wanker E.E., Hayer-Hartl M.K., Hartl F.U. Hsp70 and Hsp40 chaperones can inhibit self-assembly of polyglutamine proteins into amyloid-like fibrils. Proc. Natl. Acad. Sci. USA. 2000;97:7841–7846. doi: 10.1073/pnas.140202897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dedmon M.M., Christodoulou J., Wilson M.R., Dobson C.M. Heat Shock Protein 70 Inhibits α-Synuclein Fibril Formation via Preferential Binding to Prefibrillar Species. J. Biol. Chem. 2005;280:14733–14740. doi: 10.1074/jbc.M413024200. [DOI] [PubMed] [Google Scholar]
- 76.Parsell D.A., Kowal A.S., Singer M.A., Lindquist S. Protein disaggregation mediated by heat-shock protein Hspl04. Nature. 1994;372:475–478. doi: 10.1038/372475a0. [DOI] [PubMed] [Google Scholar]
- 77.Glover J.R., Lindquist S. Hsp104, Hsp70, and Hsp40: A Novel Chaperone System that Rescues Previously Aggregated Proteins. Cell. 1998;94:73–82. doi: 10.1016/S0092-8674(00)81223-4. [DOI] [PubMed] [Google Scholar]
- 78.Nillegoda N.B., Kirstein J., Szlachcic A., Berynskyy M., Stank A., Stengel F., Arnsburg K., Gao X., Scior A., Aebersold R., et al. Crucial HSP70 co-chaperone complex unlocks metazoan protein disaggregation. Nature. 2015;524:247–251. doi: 10.1038/nature14884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Faust O., Abayev-Avraham M., Wentink A.S., Maurer M., Nillegoda N.B., London N., Bukau B., Rosenzweig R. HSP40 proteins use class-specific regulation to drive HSP70 functional diversity. Nat. Cell Biol. 2020;587:489–494. doi: 10.1038/s41586-020-2906-4. [DOI] [PubMed] [Google Scholar]
- 80.Wentink A.S., Nillegoda N.B., Feufel J., Ubartaitė G., Schneider C.P., Rios P.D.L., Hennig J., Barducci A., Bukau B. Molecular dissection of amyloid disaggregation by human HSP70. Nature. 2020;587:483–488. doi: 10.1038/s41586-020-2904-6. [DOI] [PubMed] [Google Scholar]
- 81.Jawed A., Ho C.-T., Grousl T., Shrivastava A., Ruppert T., Bukau B., Mogk A. Balanced activities of Hsp70 and the ubiquitin proteasome system underlie cellular protein homeostasis. Front. Mol. Biosci. 2022;9:1106477. doi: 10.3389/fmolb.2022.1106477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Webster J.M., Darling A.L., Uversky V.N., Blair L.J. Small Heat Shock Proteins, Big Impact on Protein Aggregation in Neurodegenerative Disease. Front. Pharmacol. 2019;10:1047. doi: 10.3389/fphar.2019.01047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Malinovska L., Kroschwald S., Munder M.C., Richter D., Alberti S. Molecular chaperones and stress-inducible protein-sorting factors coordinate the spatiotemporal distribution of protein aggregates. Mol. Biol. Cell. 2012;23:3041–3056. doi: 10.1091/mbc.e12-03-0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Miller S.B.M., Ho C.T., Winkler J., Khokhrina M., Neuner A., Mohamed M.Y.H., Guilbride D.L., Richter K., Lisby M., Schiebel E., et al. Compartment-specific aggregases direct distinct nuclear and cytoplasmic aggregate deposition. EMBO J. 2015;34:778–797. doi: 10.15252/embj.201489524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Grousl T., Ungelenk S., Miller S., Ho C.-T., Khokhrina M., Mayer M.P., Bukau B., Mogk A. A prion-like domain in Hsp42 drives chaperone-facilitated aggregation of misfolded proteins. J. Cell Biol. 2018;217:1269–1285. doi: 10.1083/jcb.201708116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Reinle K., Mogk A., Bukau B. The Diverse Functions of Small Heat Shock Proteins in the Proteostasis Network. J. Mol. Biol. 2022;434:167157. doi: 10.1016/j.jmb.2021.167157. [DOI] [PubMed] [Google Scholar]
- 87.Kopito R.R. Aggresomes, inclusion bodies and protein aggregation. Trends Cell Biol. 2000;10:524–530. doi: 10.1016/S0962-8924(00)01852-3. [DOI] [PubMed] [Google Scholar]
- 88.Arrasate M., Mitra S., Schweitzer E.S., Segal M.R., Finkbeiner S. Inclusion body formation reduces levels of mutant huntingtin and the risk of neuronal death. Nature. 2004;431:805–810. doi: 10.1038/nature02998. [DOI] [PubMed] [Google Scholar]
- 89.Kundra R., Ciryam P., Morimoto R.I., Dobson C.M., Vendruscolo M. Protein homeostasis of a metastable subproteome associated with Alzheimer’s disease. Proc. Natl. Acad. Sci. USA. 2017;114:E5703–E5711. doi: 10.1073/pnas.1618417114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sala A.J., Bott L.C., Morimoto R.I. Shaping proteostasis at the cellular, tissue, and organismal level. J. Cell Biol. 2017;216:1231–1241. doi: 10.1083/jcb.201612111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Brehme M., Voisine C., Rolland T., Wachi S., Soper J.H., Zhu Y., Orton K., Villella A., Garza D., Vidal M., et al. A Chaperome Subnetwork Safeguards Proteostasis in Aging and Neurodegenerative Disease. Cell Rep. 2014;9:1135–1150. doi: 10.1016/j.celrep.2014.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Moura C.S., Lollo P.C.B., Neder Morato P., Amaya-Farfan J. Dietary Nutrients and Bioactive Substances Modulate Heat Shock Protein (HSP) Expression: A Review. Nutrients. 2018;10:683. doi: 10.3390/nu10060683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hussain T., Wang J., Murtaza G., Metwally E., Yang H., Kalhoro M.S., Kalhoro D.H., Rahu B.A., Tan B., Sahito R.G.A., et al. The Role of Polyphenols in Regulation of Heat Shock Proteins and Gut Microbiota in Weaning Stress. Oxidative Med. Cell. Longev. 2021;2021:6676444. doi: 10.1155/2021/6676444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Inoue H., Akiyama S., Maeda-Yamamoto M., Nesumi A., Tanaka T., Murakami A. High-dose green tea polyphenols induce nephrotoxicity in dextran sulfate sodium-induced colitis mice by down-regulation of antioxidant enzymes and heat-shock protein expressions. Cell Stress Chaperon. 2011;16:653–662. doi: 10.1007/s12192-011-0280-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chander K., Vaibhav K., Ahmed E., Javed H., Tabassum R., Khan A., Kumar M., Katyal A., Islam F., Siddiqui M.S. Quercetin mitigates lead acetate-induced behavioral and histological alterations via suppression of oxidative stress, Hsp-70, Bak and upregulation of Bcl-2. Food Chem. Toxicol. 2014;68:297–306. doi: 10.1016/j.fct.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 96.Arts I.C., Hollman P.C. Polyphenols and disease risk in epidemiologic studies. Am. J. Clin. Nutr. 2005;81:317S–325S. doi: 10.1093/ajcn/81.1.317S. [DOI] [PubMed] [Google Scholar]
- 97.Rudrapal M., Khairnar S.J., Khan J., Bin Dukhyil A., Ansari M.A., Alomary M.N., Alshabrmi F.M., Palai S., Deb P.K., Devi R. Dietary Polyphenols and Their Role in Oxidative Stress-Induced Human Diseases: Insights Into Protective Effects, Antioxidant Potentials and Mechanism(s) of Action. Front. Pharmacol. 2022;13:806470. doi: 10.3389/fphar.2022.806470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Fetoni A.R., Paciello F., Troiani D. Cisplatin Chemotherapy and Cochlear Damage: Otoprotective and Chemosensitization Properties of Polyphenols. Antioxid. Redox Signal. 2022;36:1229–1245. doi: 10.1089/ars.2021.0183. [DOI] [PubMed] [Google Scholar]
- 99.Pisani A., Paciello F., Montuoro R., Rolesi R., Galli J., Fetoni A.R. Antioxidant Therapy as an Effective Strategy against Noise-Induced Hearing Loss: From Experimental Models to Clinic. Life. 2023;13:1035. doi: 10.3390/life13041035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Di Lorenzo C., Colombo F., Biella S., Stockley C., Restani P. Polyphenols and Human Health: The Role of Bioavailability. Nutrients. 2021;13:273. doi: 10.3390/nu13010273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Stromsnes K., Lagzdina R., Olaso-Gonzalez G., Gimeno-Mallench L., Gambini J. Pharmacological Properties of Polyphenols: Bioavailability, Mechanisms of Action, and Biological Effects in In Vitro Studies, Animal Models, and Humans. Biomedicines. 2021;9:1074. doi: 10.3390/biomedicines9081074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Murota K., Nakamura Y., Uehara M. Flavonoid metabolism: The interaction of metabolites and gut microbiota. Biosci. Biotechnol. Biochem. 2018;82:600–610. doi: 10.1080/09168451.2018.1444467. [DOI] [PubMed] [Google Scholar]
- 103.Luca S.V., Macovei I., Bujor A., Miron A., Skalicka-Woźniak K., Aprotosoaie A.C., Trifan A. Bioactivity of dietary polyphenols: The role of metabolites. Crit. Rev. Food Sci. Nutr. 2020;60:626–659. doi: 10.1080/10408398.2018.1546669. [DOI] [PubMed] [Google Scholar]
- 104.Ozdal T., Sela D.A., Xiao J., Boyacioglu D., Chen F., Capanoglu E. The Reciprocal Interactions between Polyphenols and Gut Microbiota and Effects on Bioaccessibility. Nutrients. 2016;8:78. doi: 10.3390/nu8020078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Moco S., Martin F.-P.J., Rezzi S. Metabolomics View on Gut Microbiome Modulation by Polyphenol-rich Foods. J. Proteome Res. 2012;11:4781–4790. doi: 10.1021/pr300581s. [DOI] [PubMed] [Google Scholar]
- 106.Cardona F., Andrés-Lacueva C., Tulipani S., Tinahones F.J., Queipo-Ortuño M.I. Benefits of polyphenols on gut microbiota and implications in human health. J. Nutr. Biochem. 2013;24:1415–1422. doi: 10.1016/j.jnutbio.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 107.Cheng H., Zhang D., Wu J., Liu J., Zhou Y., Tan Y., Feng W., Peng C. Interactions between gut microbiota and polyphenols: A mechanistic and metabolomic review. Phytomedicine. 2023;119:154979. doi: 10.1016/j.phymed.2023.154979. [DOI] [PubMed] [Google Scholar]
- 108.Appeldoorn M.M., Vincken J.-P., Aura A.-M., Hollman P.C.H., Gruppen H. Procyanidin Dimers Are Metabolized by Human Microbiota with 2-(3,4-Dihydroxyphenyl)acetic Acid and 5-(3,4-Dihydroxyphenyl)-γ-valerolactone as the Major Metabolites. J. Agric. Food Chem. 2009;57:1084–1092. doi: 10.1021/jf803059z. [DOI] [PubMed] [Google Scholar]
- 109.Wan M.L.Y., Co V.A., El-Nezami H. Dietary polyphenol impact on gut health and microbiota. Crit. Rev. Food Sci. Nutr. 2021;61:690–711. doi: 10.1080/10408398.2020.1744512. [DOI] [PubMed] [Google Scholar]
- 110.Farias S.A.d.S., da Costa K.S., Martins J.B.L. Analysis of Conformational, Structural, Magnetic, and Electronic Properties Related to Antioxidant Activity: Revisiting Flavan, Anthocyanidin, Flavanone, Flavonol, Isoflavone, Flavone, and Flavan-3-ol. ACS Omega. 2021;6:8908–8918. doi: 10.1021/acsomega.0c06156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ullah C., Unsicker S.B., Fellenberg C., Constabel C.P., Schmidt A., Gershenzon J., Hammerbacher A. Flavan-3-ols Are an Effective Chemical Defense against Rust Infection. Plant Physiol. 2017;175:1560–1578. doi: 10.1104/pp.17.00842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cheng C.-Y., Barro L., Tsai S.-T., Feng T.-W., Wu X.-Y., Chao C.-W., Yu R.-S., Chin T.-Y., Hsieh M.F. Epigallocatechin-3-Gallate-Loaded Liposomes Favor Anti-Inflammation of Microglia Cells and Promote Neuroprotection. Int. J. Mol. Sci. 2021;22:3037. doi: 10.3390/ijms22063037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Leonardo C.C., Agrawal M., Singh N., Moore J.R., Biswal S., Doré S. Oral administration of the flavanol (−)-epicatechin bolsters endogenous protection against focal ischemia through the Nrf2 cytoprotective pathway. Eur. J. Neurosci. 2013;38:3659–3668. doi: 10.1111/ejn.12362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Shah Z.A., Li R., Ahmad A.S., Kensler T.W., Yamamoto M., Biswal S., Doré S. The flavanol (-)-epicatechin prevents stroke damage through the Nrf2/HO1 pathway. J. Cereb. Blood Flow Metab. 2010;30:1951–1961. doi: 10.1038/jcbfm.2010.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wei J.C.-C., Huang H.-C., Chen W.-J., Huang C.-N., Peng C.-H., Lin C.-L. Epigallocatechin gallate attenuates amyloid β-induced inflammation and neurotoxicity in EOC 13.31 microglia. Eur. J. Pharmacol. 2016;770:16–24. doi: 10.1016/j.ejphar.2015.11.048. [DOI] [PubMed] [Google Scholar]
- 116.Xu Y., Xie M., Xue J., Xiang L., Li Y., Xiao J., Xiao G., Wang H. EGCG ameliorates neuronal and behavioral defects by remodeling gut microbiota and TotM expression in Drosophila models of Parkinson’s disease. FASEB J. 2020;34:5931–5950. doi: 10.1096/fj.201903125RR. [DOI] [PubMed] [Google Scholar]
- 117.Kim S.-J., Lee J.-H., Kim B.-S., So H.-S., Park R., Myung N.-Y., Um J.-Y., Hong S.-H. (-)-Epigallocatechin-3-Gallate Protects against NO-Induced Ototoxicity through the Regulation of Caspase- 1, Caspase-3, and NF-κB Activation. PLoS ONE. 2012;7:e43967. doi: 10.1371/journal.pone.0043967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gu L.-T., Yang J., Su S.-Z., Liu W.-W., Shi Z.-G., Wang Q.-R. Green Tea Polyphenols Protects Cochlear Hair Cells from Ototoxicity by Inhibiting Notch Signalling. Neurochem. Res. 2015;40:1211–1219. doi: 10.1007/s11064-015-1584-3. [DOI] [PubMed] [Google Scholar]
- 119.Sánchez-Rodríguez C., Martín-Sanz E., Cuadrado E., Granizo J.J., Sanz-Fernández R. Protective effect of polyphenols on presbycusis via oxidative/nitrosative stress suppression in rats. Exp. Gerontol. 2016;83:31–36. doi: 10.1016/j.exger.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 120.Rivas-Chacón L.d.M., Yanes-Díaz J., de Lucas B., Riestra-Ayora J.I., Madrid-García R., Sanz-Fernández R., Sánchez-Rodríguez C. Preventive Effect of Cocoa Flavonoids via Suppression of Oxidative Stress-Induced Apoptosis in Auditory Senescent Cells. Antioxidants. 2022;11:1450. doi: 10.3390/antiox11081450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Łuczaj W., Skrzydlewska E. Antioxidative properties of black tea. Prev. Med. 2005;40:910–918. doi: 10.1016/j.ypmed.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 122.Osakabe N., Terao J. Possible mechanisms of postprandial physiological alterations following flavan 3-ol ingestion. Nutr. Rev. 2018;76:174–186. doi: 10.1093/nutrit/nux070. [DOI] [PubMed] [Google Scholar]
- 123.Baba S., Osakabe N., Natsume M., Terao J. Absorption and urinary excretion of procyanidin b2 [epicatechin-(4beta-8)-epicatechin] in rats. Free Radic. Biol. Med. 2002;33:142–148. doi: 10.1016/S0891-5849(02)00871-7. [DOI] [PubMed] [Google Scholar]
- 124.Serra A., Macià A., Romero M.-P., Valls J., Bladé C., Arola L., Motilva M.-J. Bioavailability of procyanidin dimers and trimers and matrix food effects in in vitro and in vivo models. Br. J. Nutr. 2010;103:944–952. doi: 10.1017/S0007114509992741. [DOI] [PubMed] [Google Scholar]
- 125.Al-Khayri J.M., Mascarenhas R., Harish H.M., Gowda Y., Lakshmaiah V.V., Nagella P., Al-Mssallem M.Q., Alessa F.M., Almaghasla M.I., Rezk A.A.-S. Stilbenes, a Versatile Class of Natural Metabolites for Inflammation—An Overview. Molecules. 2023;28:3786. doi: 10.3390/molecules28093786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Zhang Y., Han Z., Jiang A., Wu D., Li S., Liu Z., Wei Z., Yang Z., Guo C. Protective Effects of Pterostilbene on Lipopolysaccharide-Induced Acute Lung Injury in Mice by Inhibiting NF-κB and Activating Nrf2/HO-1 Signaling Pathways. Front. Pharmacol. 2020;11:591836. doi: 10.3389/fphar.2020.591836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zhu L., Lu F., Zhang X., Liu S., Mu P. SIRT1 Is Involved in the Neuroprotection of Pterostilbene Against Amyloid β 25–35-Induced Cognitive Deficits in Mice. Front. Pharmacol. 2022;13:877098. doi: 10.3389/fphar.2022.877098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lee S.H., Kim H.S., An Y.S., Chang J., Choi J., Im G.J. Protective effect of resveratrol against cisplatin-induced ototoxicity in HEI-OC1 auditory cells. Int. J. Pediatr. Otorhinolaryngol. 2015;79:58–62. doi: 10.1016/j.ijporl.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 129.Cosar M.Y., Erdogan M.A., Yilmaz O. Epigallocatechin-3-gallate and resveratrol attenuate hydrogen peroxide induced damage in neuronal cells. Bratisl. Med. J. 2023;124:205–211. doi: 10.4149/BLL_2023_033. [DOI] [PubMed] [Google Scholar]
- 130.Wang P., Du B., Yin W., Wang X., Zhu W. Resveratrol Attenuates CoCl2-Induced Cochlear Hair Cell Damage through Upregulation of Sirtuin1 and NF-κB Deacetylation. PLoS ONE. 2013;8:e80854. doi: 10.1371/journal.pone.0080854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lee C.H., Kim K.W., Lee S.M., Kim S.Y. Dose-Dependent Effects of Resveratrol on Cisplatin-Induced Hearing Loss. Int. J. Mol. Sci. 2020;22:113. doi: 10.3390/ijms22010113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Yang Z., Zhang Y., Yang S., Ding Y., Qu Y. Low-Dose Resveratrol Inhibits RIPK3-Mediated Necroptosis and Delays the Onset of Age-Related Hearing Loss. Front. Pharmacol. 2022;13:910308. doi: 10.3389/fphar.2022.910308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Avci D., Erkan M., Sonmez M.F., Kokoglu K., Gunes M.S., Gundogdu R., Gulec S., Karabulut D. A Prospective Experimental Study on the Protective Effect of Resveratrol against Amikacin-Induced Ototoxicity in Rats. J. Int. Adv. Otol. 2016;12:290–297. doi: 10.5152/iao.2016.2617. [DOI] [PubMed] [Google Scholar]
- 134.Simsek G., Taş B.M., Muluk N.B., Azman M., Kılıç R. Comparison of the protective efficacy between intratympanic dexamethasone and resveratrol treatments against cisplatin-induced ototoxicity: An experimental study. Eur. Arch. Oto-Rhino-Laryngol. 2019;276:3287–3293. doi: 10.1007/s00405-019-05635-x. [DOI] [PubMed] [Google Scholar]
- 135.Pang J., Xiong H., Ou Y., Yang H., Xu Y., Chen S., Lai L., Ye Y., Su Z., Lin H., et al. SIRT1 protects cochlear hair cell and delays age-related hearing loss via autophagy. Neurobiol. Aging. 2019;80:127–137. doi: 10.1016/j.neurobiolaging.2019.04.003. [DOI] [PubMed] [Google Scholar]
- 136.Liu Y., Wu H., Zhang F., Yang J., He J. Resveratrol upregulates miR-455-5p to antagonize cisplatin ototoxicity via modulating the PTEN–PI3K–AKT axis. Biochem. Cell Biol. 2021;99:385–395. doi: 10.1139/bcb-2020-0459. [DOI] [PubMed] [Google Scholar]
- 137.Xiong H., Chen S., Lai L., Yang H., Xu Y., Pang J., Su Z., Lin H., Zheng Y. Modulation of miR-34a/SIRT1 signaling protects cochlear hair cells against oxidative stress and delays age-related hearing loss through coordinated regulation of mitophagy and mitochondrial biogenesis. Neurobiol. Aging. 2019;79:30–42. doi: 10.1016/j.neurobiolaging.2019.03.013. [DOI] [PubMed] [Google Scholar]
- 138.Xiong H., Ou Y., Xu Y., Huang Q., Pang J., Lai L., Zheng Y. Resveratrol Promotes Recovery of Hearing following Intense Noise Exposure by Enhancing Cochlear SIRT1 Activity. Audiol. Neurotol. 2017;22:303–310. doi: 10.1159/000485312. [DOI] [PubMed] [Google Scholar]
- 139.Springer M., Moco S. Resveratrol and Its Human Metabolites—Effects on Metabolic Health and Obesity. Nutrients. 2019;11:143. doi: 10.3390/nu11010143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Walle T., Hsieh F., DeLegge M.H., Oatis J.E., Jr., Walle U.K. High absorption but very low bioavailability of oral resveratrol in humans. Drug Metab. Dispos. 2004;32:1377–1382. doi: 10.1124/dmd.104.000885. [DOI] [PubMed] [Google Scholar]
- 141.Britton J., Davis R., O’connor K.E. Chemical, physical and biotechnological approaches to the production of the potent antioxidant hydroxytyrosol. Appl. Microbiol. Biotechnol. 2019;103:5957–5974. doi: 10.1007/s00253-019-09914-9. [DOI] [PubMed] [Google Scholar]
- 142.D’Angelo S., Manna C., Migliardi V., Mazzoni O., Morrica P., Capasso G., Pontoni G., Galletti P., Zappia V. Pharmacokinetics and metabolism of hydroxytyrosol, a natural antioxidant from olive oil. Drug Metab. Dispos. 2001;29:1492–1498. [PubMed] [Google Scholar]
- 143.Nikou T., Sakavitsi M.E., Kalampokis E., Halabalaki M. Metabolism and Bioavailability of Olive Bioactive Constituents Based on In Vitro, In Vivo and Human Studies. Nutrients. 2022;14:3773. doi: 10.3390/nu14183773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Soni M.G., Burdock G.A., Christian M.S., Bitler C.M., Crea R. Safety assessment of aqueous olive pulp extract as an antioxidant or antimicrobial agent in foods. Food Chem. Toxicol. 2006;44:903–915. doi: 10.1016/j.fct.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 145.Luo S., Jiang X., Jia L., Tan C., Li M., Yang Q., Du Y., Ding C. In Vivo and In Vitro Antioxidant Activities of Methanol Extracts from Olive Leaves on Caenorhabditis elegans. Molecules. 2019;24:704. doi: 10.3390/molecules24040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Calabriso N., Massaro M., Scoditti E., D’amore S., Gnoni A., Pellegrino M., Storelli C., De Caterina R., Palasciano G., Carluccio M.A. Extra virgin olive oil rich in polyphenols modulates VEGF-induced angiogenic responses by preventing NADPH oxidase activity and expression. J. Nutr. Biochem. 2016;28:19–29. doi: 10.1016/j.jnutbio.2015.09.026. [DOI] [PubMed] [Google Scholar]
- 147.Zhang X., Cao J., Zhong L. Hydroxytyrosol inhibits pro-inflammatory cytokines, iNOS, and COX-2 expression in human monocytic cells. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2009;379:581–586. doi: 10.1007/s00210-009-0399-7. [DOI] [PubMed] [Google Scholar]
- 148.Pantano D., Luccarini I., Nardiello P., Servili M., Stefani M., Casamenti F. Oleuropein aglycone and polyphenols from olive mill waste water ameliorate cognitive deficits and neuropathology. Br. J. Clin. Pharmacol. 2017;83:54–62. doi: 10.1111/bcp.12993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Reutzel M., Grewal R., Silaidos C., Zotzel J., Marx S., Tretzel J., Eckert G.P. Effects of Long-Term Treatment with a Blend of Highly Purified Olive Secoiridoids on Cognition and Brain ATP Levels in Aged NMRI Mice. Oxidative Med. Cell. Longev. 2018;2018:4070935. doi: 10.1155/2018/4070935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Zhang W., Man R., Yu X., Yang H., Yang Q., Li J. Hydroxytyrosol enhances cisplatin-induced ototoxicity: Possible relation to the alteration in the activity of JNK and AIF pathways. Eur. J. Pharmacol. 2020;887:173338. doi: 10.1016/j.ejphar.2020.173338. [DOI] [PubMed] [Google Scholar]
- 151.Nelson K.M., Dahlin J.L., Bisson J., Graham J., Pauli G.F., Walters M.A. The essential medicinal chemistry of curcumin. J. Med. Chem. 2017;60:1620–1637. doi: 10.1021/acs.jmedchem.6b00975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Abd El-Hack M.E., El-Saadony M.T., Swelum A.A., Arif M., Abo Ghanima M.M., Shukry M., Noreldin A., Taha A.E., El-Tarabily K.A. Curcumin, the active substance of turmeric: Its effects on health and ways to improve its bioavailability. J. Sci. Food Agric. 2021;101:5747–5762. doi: 10.1002/jsfa.11372. [DOI] [PubMed] [Google Scholar]
- 153.Aggarwal B.B., Deb L., Prasad S. Curcumin Differs from Tetrahydrocurcumin for Molecular Targets, Signaling Pathways and Cellular Responses. Molecules. 2014;20:185–205. doi: 10.3390/molecules20010185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Abrahams S., Haylett W.L., Johnson G., Carr J.A., Bardien S. Antioxidant effects of curcumin in models of neurodegeneration, aging, oxidative and nitrosative stress: A review. Neuroscience. 2019;406:1–21. doi: 10.1016/j.neuroscience.2019.02.020. [DOI] [PubMed] [Google Scholar]
- 155.Sarkar B., Dhiman M., Mittal S., Mantha A.K. Curcumin revitalizes Amyloid beta (25–35)-induced and organophosphate pesticides pestered neurotoxicity in SH-SY5Y and IMR-32 cells via activation of APE1 and Nrf2. Metab. Brain Dis. 2017;32:2045–2061. doi: 10.1007/s11011-017-0093-2. [DOI] [PubMed] [Google Scholar]
- 156.Soyalıç H., Gevrek F., Koç S., Avcu M., Metin M., Aladağ İ. Intraperitoneal curcumin and vitamin E combination for the treatment of cisplatin-induced ototoxicity in rats. Int. J. Pediatr. Otorhinolaryngol. 2016;89:173–178. doi: 10.1016/j.ijporl.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 157.Fetoni A.R., Eramo S.L.M., Paciello F., Rolesi R., Podda M.V., Troiani D., Paludetti G. Curcuma Longa (Curcumin) Decreases In Vivo Cisplatin-Induced Ototoxicity through Heme Oxygenase-1 Induction. Otol. Neurotol. 2014;35:e169–e177. doi: 10.1097/MAO.0000000000000302. [DOI] [PubMed] [Google Scholar]
- 158.Dei Cas M., Ghidoni R. Dietary Curcumin: Correlation between Bioavailability and Health Potential. Nutrients. 2019;11:2147. doi: 10.3390/nu11092147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Tong Z., He W., Fan X., Guo A. Biological Function of Plant Tannin and Its Application in Animal Health. Front. Veter-Sci. 2021;8:803657. doi: 10.3389/fvets.2021.803657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Saad H., Bouhtoury F.C.-E., Pizzi A., Rode K., Charrier B., Ayed N. Characterization of pomegranate peels tannin extractives. Ind. Crop. Prod. 2012;40:239–246. doi: 10.1016/j.indcrop.2012.02.038. [DOI] [Google Scholar]
- 161.Chang M.Y., Byon S.-H., Shin H.-C., Han S.E., Kim J.Y., Byun J.Y., Lee J.D., Park M.K. Protective effects of the seaweed phlorotannin polyphenolic compound dieckol on gentamicin-induced damage in auditory hair cells. Int. J. Pediatr. Otorhinolaryngol. 2016;83:31–36. doi: 10.1016/j.ijporl.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 162.Fraga-Corral M., Otero P., Cassani L., Echave J., Garcia-Oliveira P., Carpena M., Chamorro F., Lourenço-Lopes C., Prieto M.A., Simal-Gandara J. Traditional Applications of Tannin Rich Extracts Supported by Scientific Data: Chemical Composition, Bioavailability and Bioaccessibility. Foods. 2021;10:251. doi: 10.3390/foods10020251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Fabbrini M., D’amico F., Barone M., Conti G., Mengoli M., Brigidi P., Turroni S. Polyphenol and Tannin Nutraceuticals and Their Metabolites: How the Human Gut Microbiota Influences Their Properties. Biomolecules. 2022;12:875. doi: 10.3390/biom12070875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Petersen M., Simmonds M.S.J. Rosmarinic acid. Phytochemistry. 2003;62:121–125. doi: 10.1016/S0031-9422(02)00513-7. [DOI] [PubMed] [Google Scholar]
- 165.Sanbongi C., Takano H., Osakabe N., Sasa N., Natsume M., Yanagisawa R., Inoue K., Sadakane K., Ichinose T., Yoshikawa T. Rosmarinic acid in perilla extract inhibits allergic inflammation induced by mite allergen, in a mouse model. Clin. Exp. Allergy. 2004;34:971–977. doi: 10.1111/j.1365-2222.2004.01979.x. [DOI] [PubMed] [Google Scholar]
- 166.Sanbongi C., Takano H., Osakabe N., Sasa N., Natsume M., Yanagisawa R., Inoue K.-I., Kato Y., Osawa T., Yoshikawa T. Rosmarinic acid inhibits lung injury induced by diesel exhaust particles. Free Radic. Biol. Med. 2003;34:1060–1069. doi: 10.1016/S0891-5849(03)00040-6. [DOI] [PubMed] [Google Scholar]
- 167.Osakabe N., Yasuda A., Natsume M., Sanbongi C., Kato Y., Osawa T., Yoshikawa T. Rosmarinic acid, a major polyphenolic component of perilla frutescens, reduces lipopolysaccharide (lps)-induced liver injury in d-galactosamine (d-galn)-sensitized mice. Free Radic. Biol. Med. 2002;33:798–806. doi: 10.1016/S0891-5849(02)00970-X. [DOI] [PubMed] [Google Scholar]
- 168.Osakabe N., Yasuda A., Natsume M., Yoshikawa T. Rosmarinic acid inhibits epidermal inflammatory responses: Anticarcinogenic effect of Perilla frutescens extract in the murine two-stage skin model. Carcinogenesis. 2004;25:549–557. doi: 10.1093/carcin/bgh034. [DOI] [PubMed] [Google Scholar]
- 169.Osakabe N., Takano H., Sanbongi C., Yasuda A., Yanagisawa R., Inoue K., Yoshikawa T. Anti-inflammatory and anti-allergic effect of rosmarinic acid (RA); inhibition of seasonal allergic rhinoconjunctivitis (SAR) and its mechanism. BioFactors. 2004;21:127–131. doi: 10.1002/biof.552210125. [DOI] [PubMed] [Google Scholar]
- 170.Takano H., Osakabe N., Sanbongi C., Yanagisawa R., Inoue K., Yasuda A., Natsume M., Baba S., Ichiishi E., Yoshikawa T. Extract of perilla frutescens enriched for rosmarinic acid, a polyphenolic phytochemical, inhibits seasonal allergic rhinoconjunctivitis in humans. Exp. Biol. Med. 2004;229:247–254. doi: 10.1177/153537020422900305. [DOI] [PubMed] [Google Scholar]
- 171.Kim S.J., Um J.Y., Kim S.H., Hong S.H. Protective effect of rosmarinic acid is through regulation of inflammatory cytokine in cadmium-induced ototoxicity. Am. J. Chin. Med. 2013;41:391–404. doi: 10.1142/S0192415X13500298. [DOI] [PubMed] [Google Scholar]
- 172.Jeong H.-J., Choi Y., Kim M.-H., Kang I.-C., Lee J.-H., Park C., Park R., Kim H.-M. Rosmarinic Acid, Active Component of Dansam-Eum Attenuates Ototoxicity of Cochlear Hair Cells through Blockage of Caspase-1 Activity. PLoS ONE. 2011;6:e18815. doi: 10.1371/journal.pone.0018815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Fetoni A.R., Eramo S.L.M., Di Pino A., Rolesi R., Paciello F., Grassi C., Troiani D., Paludetti G. The Antioxidant Effect of Rosmarinic Acid by Different Delivery Routes in the Animal Model of Noise-Induced Hearing Loss. Otol. Neurotol. 2018;39:378–386. doi: 10.1097/MAO.0000000000001700. [DOI] [PubMed] [Google Scholar]
- 174.Fetoni A., Paciello F., Rolesi R., Eramo S., Mancuso C., Troiani D., Paludetti G. Rosmarinic acid up-regulates the noise-activated Nrf2/HO-1 pathway and protects against noise-induced injury in rat cochlea. Free Radic. Biol. Med. 2015;85:269–281. doi: 10.1016/j.freeradbiomed.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 175.Baba S., Osakabe N., Natsume M., Yasuda A., Muto Y., Hiyoshi T., Takano H., Yoshikawa T., Terao J. Absorption, metabolism, degradation and urinary excretion of rosmarinic acid after intake of Perilla frutescens extract in humans. Eur. J. Nutr. 2005;44:1–9. doi: 10.1007/s00394-004-0482-2. [DOI] [PubMed] [Google Scholar]
- 176.Bakır S., Özbay M., Gün R., Yorgancılar E., Kınış V., Keleş A., Abakay A., Gökalp O., Topçu I. The protective role of caffeic acid phenethyl ester against streptomycin ototoxicity. Am. J. Otolaryngol. 2013;34:16–21. doi: 10.1016/j.amjoto.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 177.Choi J., Kim S.H., Rah Y.C., Chae S.W., Lee J.D., Lee B.D., Park M.K. Effects of caffeic acid on cisplatin-induced hair cell damage in HEI-OC1 auditory cells. Int. J. Pediatr. Otorhinolaryngol. 2014;78:2198–2204. doi: 10.1016/j.ijporl.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 178.Park M.K., Im G.J., Chang J., Chae S.W., Yoo J., Han W.-G., Hwang G.H., Jung J.Y., Choi J., Jung H.H., et al. Protective effects of caffeic acid phenethyl ester (CAPE) against neomycin-induced hair cell damage in zebrafish. Int. J. Pediatr. Otorhinolaryngol. 2014;78:1311–1315. doi: 10.1016/j.ijporl.2014.05.018. [DOI] [PubMed] [Google Scholar]
- 179.Jo E.-R., Youn C.K., Jun Y., Cho S.I. The protective role of ferulic acid against cisplatin-induced ototoxicity. Int. J. Pediatr. Otorhinolaryngol. 2019;120:30–35. doi: 10.1016/j.ijporl.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 180.Fetoni A., Mancuso C., Eramo S., Ralli M., Piacentini R., Barone E., Paludetti G., Troiani D. In vivo protective effect of ferulic acid against noise-induced hearing loss in the guinea-pig. Neuroscience. 2010;169:1575–1588. doi: 10.1016/j.neuroscience.2010.06.022. [DOI] [PubMed] [Google Scholar]
- 181.Fetoni A.R., Eramo S., Troiani D., Paludetti G. Therapeutic window for ferulic acid protection against noise-induced hearing loss in the guinea pig. Acta Oto-Laryngol. 2011;131:419–427. doi: 10.3109/00016489.2010.539263. [DOI] [PubMed] [Google Scholar]
- 182.Rassu G., Sorrenti M., Catenacci L., Pavan B., Ferraro L., Gavini E., Bonferoni M.C., Giunchedi P., Dalpiaz A. Conjugation, Prodrug, and Co-Administration Strategies in Support of Nanotechnologies to Improve the Therapeutic Efficacy of Phytochemicals in the Central Nervous System. Pharmaceutics. 2023;15:1578. doi: 10.3390/pharmaceutics15061578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Katila N., Duwa R., Bhurtel S., Khanal S., Maharjan S., Jeong J.-H., Lee S., Choi D.-Y., Yook S. Enhancement of blood–brain barrier penetration and the neuroprotective effect of resveratrol. J. Control. Release. 2022;346:1–19. doi: 10.1016/j.jconrel.2022.04.003. [DOI] [PubMed] [Google Scholar]
- 184.Li C., Wang N., Zheng G., Yang L. Oral Administration of Resveratrol-Selenium-Peptide Nanocomposites Alleviates Alzheimer’s Disease-like Pathogenesis by Inhibiting Aβ Aggregation and Regulating Gut Microbiota. ACS Appl. Mater. Interfaces. 2021;13:46406–46420. doi: 10.1021/acsami.1c14818. [DOI] [PubMed] [Google Scholar]
- 185.Musazzi U.M., Youm I., Murowchick J.B., Ezoulin M.J., Youan B.-B.C. Resveratrol-loaded nanocarriers: Formulation, optimization, characterization and in vitro toxicity on cochlear cells. Colloids Surf. B Biointerfaces. 2014;118:234–242. doi: 10.1016/j.colsurfb.2014.03.054. [DOI] [PubMed] [Google Scholar]
- 186.Salehi P., Akinpelu O.V., Waissbluth S., Peleva E., Meehan B., Rak J., Daniel S.J. Attenuation of Cisplatin Ototoxicity by Otoprotective Effects of Nanoencapsulated Curcumin and Dexamethasone in a Guinea Pig Model. Otol. Neurotol. 2014;35:1131–1139. doi: 10.1097/MAO.0000000000000403. [DOI] [PubMed] [Google Scholar]
- 187.Chen X., Zhang H., Wang C., Su Y., Xiong M., Feng X., Chen D., Ke Z., Wen L., Chen G. Curcumin-Encapsulated Chitosan-Coated Nanoformulation as an Improved Otoprotective Strategy for Ototoxic Hearing Loss. Mol. Pharm. 2022;19:2217–2230. doi: 10.1021/acs.molpharmaceut.2c00067. [DOI] [PubMed] [Google Scholar]
- 188.Yamaguchi T., Yoneyama M., Onaka Y., Imaizumi A., Ogita K. Preventive effect of curcumin and its highly bioavailable preparation on hearing loss induced by single or repeated exposure to noise: A comparative and mechanistic study. J. Pharmacol. Sci. 2017;134:225–233. doi: 10.1016/j.jphs.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 189.Culetto E., Sattelle D.B. A role for Caenorhabditis elegans in understanding the function and interactions of human disease genes. Hum. Mol. Genet. 2000;9:869–877. doi: 10.1093/hmg/9.6.869. [DOI] [PubMed] [Google Scholar]
- 190.Fire A., Xu S., Montgomery M.K., Kostas S.A., Driver S.E., Mello C.C. Potent and specific genetic interference by double-stranded RNA in Caenorhabditis elegans. Nature. 1998;391:806–811. doi: 10.1038/35888. [DOI] [PubMed] [Google Scholar]
- 191.Dosanjh L.E., Brown M.K., Rao G., Link C.D., Luo Y. Behavioral Phenotyping of a Transgenic Caenorhabditis Elegans Expressing Neuronal Amyloid-β. J. Alzheimer’s Dis. 2010;19:681–690. doi: 10.3233/JAD-2010-1267. [DOI] [PubMed] [Google Scholar]
- 192.Wang C., Saar V., Leung K.L., Chen L., Wong G. Human amyloid β peptide and tau co-expression impairs behavior and causes specific gene expression changes in Caenorhabditis elegans. Neurobiol. Dis. 2018;109:88–101. doi: 10.1016/j.nbd.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 193.Huang X., Wang C., Chen L., Zhang T., Leung K.L., Wong G. Human amyloid beta and α-synuclein co-expression in neurons impair behavior and recapitulate features for Lewy body dementia in Caenorhabditis elegans. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 2021;1867:166203. doi: 10.1016/j.bbadis.2021.166203. [DOI] [PubMed] [Google Scholar]
- 194.Nass R., Hall D.H., Miller D.M., Blakely R.D. Neurotoxin-induced degeneration of dopamine neurons in Caenorhabditis elegans. Proc. Natl. Acad. Sci. USA. 2002;99:3264–3269. doi: 10.1073/pnas.042497999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Link C.D., Fonte V., Hiester B., Yerg J., Ferguson J., Csontos S., Silverman M.A., Stein G.H. Conversion of Green Fluorescent Protein into a Toxic, Aggregation-prone Protein by C-terminal Addition of a Short Peptide. J. Biol. Chem. 2006;281:1808–1816. doi: 10.1074/jbc.M505581200. [DOI] [PubMed] [Google Scholar]
- 196.Wang J., Farr G.W., Hall D.H., Li F., Furtak K., Dreier L., Horwich A.L. An ALS-Linked Mutant SOD1 Produces a Locomotor Defect Associated with Aggregation and Synaptic Dysfunction When Expressed in Neurons of Caenorhabditis elegans. PLoS Genet. 2009;5:e1000350. doi: 10.1371/journal.pgen.1000350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Bansal A., Zhu L.J., Yen K., Tissenbaum H.A. Uncoupling lifespan and healthspan in Caenorhabditis elegans longevity mutants. Proc. Natl. Acad. Sci. USA. 2015;112:E277–E286. doi: 10.1073/pnas.1412192112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Muhammad F., Liu Y., Wang N., Zhao L., Zhou Y., Yang H., Li H. Anti-α-synuclein Toxicity and Anti-neurodegenerative Role of Chrysin in Transgenic Caenorhabditis elegans Models of Parkinson’s Disease. ACS Chem. Neurosci. 2022;13:442–453. doi: 10.1021/acschemneuro.1c00548. [DOI] [PubMed] [Google Scholar]
- 199.Shukla V., Phulara S.C., Yadav D., Tiwari S., Kaur S., Gupta M.M., Nazir A., Pandey R. Iridoid Compound 10-O-trans-p-Coumaroylcatalpol Extends Longevity and Reduces Alpha Synuclein Aggregation in Caenorhabditis elegans. CNS Neurol. Disord.-Drug Targets. 2012;11:984–992. doi: 10.2174/1871527311211080007. [DOI] [PubMed] [Google Scholar]
- 200.Seo H.W., Cheon S.M., Lee M.-H., Kim H.J., Jeon H., Cha D.S. Catalpol Modulates Lifespan via DAF-16/FOXO and SKN-1/Nrf2 Activation inCaenorhabditis elegans. Evidence-Based Complement. Altern. Med. 2015;2015:524878. doi: 10.1155/2015/524878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Regitz C., Dußling L.M., Wenzel U. Amyloid-beta (Aβ1–42)-induced paralysis inCaenorhabditis elegansis inhibited by the polyphenol quercetin through activation of protein degradation pathways. Mol. Nutr. Food Res. 2014;58:1931–1940. doi: 10.1002/mnfr.201400014. [DOI] [PubMed] [Google Scholar]
- 202.Smith J.V., Luo Y. Elevation of oxidative free radicals in Alzheimer’s disease models can be attenuated by Ginkgo biloba extract EGb 761. J. Alzheimer’s Dis. 2003;5:287–300. doi: 10.3233/JAD-2003-5404. [DOI] [PubMed] [Google Scholar]
- 203.Diomede L., Rigacci S., Romeo M., Stefani M., Salmona M. Oleuropein Aglycone Protects Transgenic C. elegans Strains Expressing Aβ42 by Reducing Plaque Load and Motor Deficit. PLoS ONE. 2013;8:e58893. doi: 10.1371/journal.pone.0058893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Zhou T., Benda C., Dunzinger S., Huang Y., Ho J.C., Yang J., Wang Y., Zhang Y., Zhuang Q., Li Y., et al. Generation of human induced pluripotent stem cells from urine samples. Nat. Protoc. 2012;7:2080–2089. doi: 10.1038/nprot.2012.115. [DOI] [PubMed] [Google Scholar]
- 205.Raab S., Klingenstein M., Liebau S., Linta L. A Comparative View on Human Somatic Cell Sources for iPSC Generation. Stem Cells Int. 2014;2014:768391. doi: 10.1155/2014/768391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Torrens-Mas M., Perelló-Reus C., Navas-Enamorado C., Ibargüen-González L., Sanchez-Polo A., Segura-Sampedro J.J., Masmiquel L., Barcelo C., Gonzalez-Freire M. Organoids: An Emerging Tool to Study Aging Signature across Human Tissues. Modeling Aging with Patient-Derived Organoids. Int. J. Mol. Sci. 2021;22:10547. doi: 10.3390/ijms221910547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Gulimiheranmu M., Li S., Zhou J. In Vitro Recapitulation of Neuropsychiatric Disorders with Pluripotent Stem Cells-Derived Brain Organoids. Int. J. Environ. Res. Public Health. 2021;18:12431. doi: 10.3390/ijerph182312431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Modafferi S., Zhong X., Kleensang A., Murata Y., Fagiani F., Pamies D., Hogberg H.T., Calabrese V., Lachman H., Hartung T., et al. Gene–Environment Interactions in Developmental Neurotoxicity: A Case Study of Synergy between Chlorpyrifos and CHD8 Knockout in Human BrainSpheres. Environ. Health Perspect. 2021;129:77001. doi: 10.1289/EHP8580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Wang J., Chen L., Liang Z., Li Y., Yuan F., Liu J., Tian Y., Hao Z., Zhou F., Liu X., et al. Genipin Inhibits LPS-Induced Inflammatory Response in BV2 Microglial Cells. Neurochem. Res. 2017;42:2769–2776. doi: 10.1007/s11064-017-2289-6. [DOI] [PubMed] [Google Scholar]
- 210.Bani S., Pandey A., Agnihotri V., Pathania V., Singh B. Selective Th2 Upregulation byCrocus sativus: A Neutraceutical Spice. Evidence-Based Complement. Altern. Med. 2010;2011:639862. doi: 10.1155/2011/639862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Cornelius C., Salinaro A.T., Scuto M., Fronte V., Cambria M.T., Pennisi M., Bella R., Milone P., Graziano A., Crupi R., et al. Cellular stress response, sirtuins and UCP proteins in Alzheimer disease: Role of vitagenes. Immun. Ageing. 2013;10:41. doi: 10.1186/1742-4933-10-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Salinaro A.T., Pennisi M., Di Paola R., Scuto M., Crupi R., Cambria M.T., Ontario M.L., Tomasello M., Uva M., Maiolino L., et al. Neuroinflammation and neurohormesis in the pathogenesis of Alzheimer’s disease and Alzheimer-linked pathologies: Modulation by nutritional mushrooms. Immun. Ageing. 2018;15:8. doi: 10.1186/s12979-017-0108-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Pennisi M., Crupi R., Di Paola R., Ontario M.L., Bella R., Calabrese E.J., Crea R., Cuzzocrea S., Calabrese V. Inflammasomes, hormesis, and antioxidants in neuroinflammation: Role of NRLP3 in Alzheimer disease. J. Neurosci. Res. 2017;95:1360–1372. doi: 10.1002/jnr.23986. [DOI] [PubMed] [Google Scholar]
- 214.Renis M., Calabrese V., Russo A., Calderone A., Barcellona M., Rizza V. Nuclear DNA strand breaks during ethanol-induced oxidative stress in rat brain. FEBS Lett. 1996;390:153–156. doi: 10.1016/0014-5793(96)00647-3. [DOI] [PubMed] [Google Scholar]
- 215.Calabrese E.J., Osakabe N., Di Paola R., Siracusa R., Fusco R., D’Amico R., Impellizzeri D., Cuzzocrea S., Fritsch T., Abdelhameed A.S., et al. Hormesis defines the limits of lifespan. Ageing Res. Rev. 2023;91:102074. doi: 10.1016/j.arr.2023.102074. [DOI] [PubMed] [Google Scholar]