CLINICAL CONTEXT
Osteosarcoma is the most common primary bone tumor in children and young adults accounting for approximately 400 new cases per year. Up to 20% of children will have metastatic disease on presentation, most commonly to the lung (74%) or bone (9%).1 The presence of metastases is assosciated with a significantly abbreviated 5-year overall survival of 20–30%.2 Pulmonary metastasectomy infers a survival benefit, although long-term survival associated with complete surgical extirpation and systemic therapy is approximately 40%.2 An open approach to metastasectomy via sternotomy or thoracotomy is the current standard of care as manual lung palpation allows for improved localization, identification, and detection of lesions. In fact, approximatley one-fourth of patients undergoing pulmonary metatasectomy via an open approach will have additional lesions discovered intraoperatively that were not previously seen on preoperative computed tomography (CT).3 However, clinical benefit from resection of these radiographically occult lesions remains unclear.4 As such, metastasectomy technique remains a topic of debate as open techniques are associated with increased postoperative pain, longer inpatient stay, and potential long-term morbidity and chest deformity.2
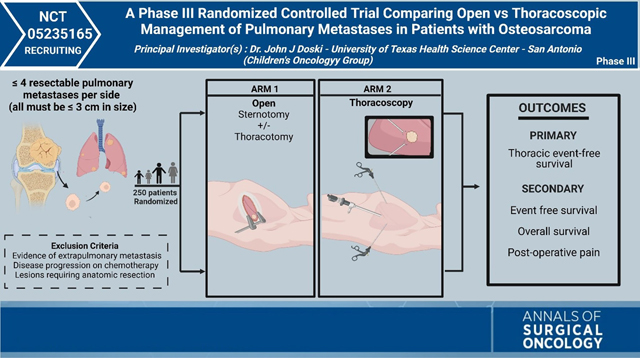
A multi-institutional retrospective study of 202 pediatric patients with metastatic osteosarcoma comparing thoracotomy versus minimally invasive thoracoscopy demonstrated equitable 5-year overall and pulmonary disease-free survival for patients with limited pulmonary disease burden.2 Although promising, the generalizabilty of these findings were limited by selection bias thus underscoring the need for a randomized, clinical trial. The Phase III trial led by Dr. John Doski of the Children’s Oncology Group (COG), is a multi-institutional, prospective, randomized, controlled trial comparing open versus minimally invasive pulmonary metastasectomy in patients with metastatic osteosarcoma. A total of 250 patients will be randomized to an open (sternotomy and/or thoracotomy) or thoracoscopic approach. Eligible patients must be younger than aged 50 years, have ≤4 resectable, peripheral lesions per lung—all measuring ≤ 3 cm, with at least one being ≥3 mm. Newly diagnosed patients must have had surgical resection of their primary tumor or planned simultaneous resection of the primary tumor with metastastic disease. Additonally, patients must currently be receiving or had previously received standard of care chemotherapy (methotrexate, doxorubicin, and cisplatin (MAP)). Patients are excluded if there is disease progression on chemotherapy or evidence of extrapulmonary metastatic disease. Patients with bilateral disease who are randomized to an open approach must undergo surgical clearance of bilateral pulmonary lesions on the same day or within 14 days of each other if perfomed in a staged manner. The primary objective of the study is to determine the thoracic event-free survival (tEFS) for each surgical approach. The study will additionally evaluate overall event-free survival (EFS), overall survival (OS), collection and analysis of patient reported outcome data, and the use of short- and long-term postoperative pain medication.
INVESTIGATOR INSIGHTS
Osteosarcoma is an exceedingly rare tumor, with metastatic disease (synhronous or metachronous) protending poor outcomes.1 Surgical clearance of pulmonary metastases has been associated with improved long-term survival. However, consensus on surgical approach is lacking, because standard of care thoracotomy can be associated with significant long-term sequelae, and thoracoscopy often is limited by its inability to provide haptic feedback. While advances in imaging modalities may reduce the rate of radiologically occult disease, current literature does not support clinical benefit from resection of these lesions. Retrospective and prospective studies in adults and children highlight the advantages of thoracoscopy, including the aformentioned study on oligometastatic osteosarcoma in the pediatric population. Following that study, the membership of the American Pediatric Surgical Association (APSA) was queried on their likelihood to endorse a randomized control trial comparing outcomes between techniques, and more than 80% of respondents were in favor of participating in this initiative.5 While this study originated in the Children’s Oncology Group, the disease process also is seen in adults. As such, adult enrollment in this study is sought and encouraged. Eligibility criteria extends to age 50 years. The protocol has been presented extensively at other National Clinical Trials Network (NCTN) group meetings (SWOG, ECOG-ACRIN, and Alliance), and NCTN study champions have been identified in these groups to promote enrollment of adult patients meeting the other eligibility criteria.
Overall, this trial will be the first of its kind to investigate whether a thoracoscopic approach provides noninferior surgical management in this setting. Findings of the study may inform decision making and provide additional options to families and patients. Further studies may be warranted to facillitate its implementation into practice, although demonstration of noninferiority will impact the management of oligometasatic disease in patients with osteosarcoma.
METHODS
Supplementary Material
Footnotes
DISCLOSURE The authors declare they have no conflict of interest and nothing to disclose.
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1245/s10434-022-12488-y.
REFERENCES
- 1.Gill J, Gorlick R. Advancing therapy for osteosarcoma. Nat Rev Clin Oncol. 2021;18(10):609–24. 10.1038/s41571-021-00519-8. [DOI] [PubMed] [Google Scholar]
- 2.Lautz TB, Farooqui Z, Jenkins T, et al. Thoracoscopy vs thoracotomy for the management of metastatic osteosarcoma: A Pediatric Surgical Oncology Research Collaborative Study. Int J Cancer. 2021;148(5):1164–71. 10.1002/ijc.33264. [DOI] [PubMed] [Google Scholar]
- 3.Kempf-Bielack B, Bielack SS, Jürgens H, et al. Osteosarcoma relapse after combined modality therapy: an analysis of unselected patients in the Cooperative Osteosarcoma Study Group (COSS). J Clin Oncol. 2005;23(3):559–68. 10.1200/JCO.2005.04.063. [DOI] [PubMed] [Google Scholar]
- 4.Heaton TE, Hammond WJ, Farber BA, et al. A 20-year retrospective analysis of CT-based pre-operative identification of pulmonary metastases in patients with osteosarcoma: A single-center review. J Pediatr Surg. 2017;52(1):115–9. 10.1016/j.jpedsurg.2016.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lautz TB, Krailo MD, Han R, Heaton TE, Dasgupta R, Doski J. Current surgical management of children with osteosarcoma and pulmonary metastatic disease: A survey of the American Pediatric Surgical Association. J Pediatr Surg. 2021;56(2):282–5. 10.1016/j.jpedsurg.2020.09.060. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


