Abstract
Background
The aim of this study is to evaluate comparative biomechanical fixation provided with the BDSF method with the conventional CC screw fixation for treatment of femoral neck fractures with three parallel cannulated screws.
Methods
This is a prospective cohort study. There were two teams of surgeons out of which one team operated the patients with BDSF technique and second with conventional CC screw fixation technique; thus, the patients were randomly distributed into two groups. Patients were included in the study as per the following inclusion and exclusion criteria.
Results
Union was achieved in 15 (83.33%) patients managed by conventional CC screw technique, while union was achieved in 11 (91.67%) patients managed by BDSF technique in the present study. The average Harris hip score in present study was 90 score in patients managed by BDSF technique, while the average Harris hip score in present study was 80 score in patients managed by BDSF technique.
Conclusion
Both BDSF and conventional CC screw fixation are good fixation methods for fracture neck of femur. But functional outcome and fracture union rates are better with BDSF Technique. Although, there are some minor problems noted in BDSF technique such as outer cortical fracture at the entry point of beam screw and opening up of anterior cortex of oblique fracture patterns. Thus, BDSF method provides reliable fixation in which early mobilization and partial weight bearing of the patient may be allowed.
Keywords: HHS, BDSF, CC
Introduction
Hip fractures are increasingly being common and these comprises of high operative workload of orthopedic trauma unit. Understanding of this fracture is important as the incidence of the fracture in elderly population in our society is rising exponentially and management still remains challenging to orthopedic surgeons. Fracture neck femur still remains the “unsolved fracture” today. We can say that this fracture is endemic disease in elderly population having tremendous impact on our health care system.
There have been marked improvements in implant design, surgical techniques, patient care, and rehabilitation since last decades. We have done this study to understand the biomechanics of various implants and surgical techniques to manage the fracture and prevent complications (Figs. 1 , 2).
Figs. 1, 2.
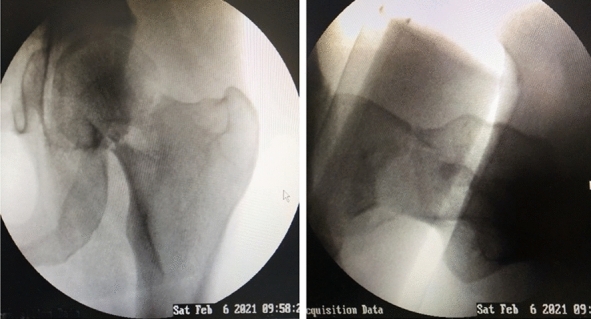
Pre-operative image intensifier picture
Previous decades have seen multiple implants available for the management of fracture neck femur are: (i) Multiple Moore pins or C.C. screws, (ii) fixed angle nail, (iii) sliding hip screw with or without derotation screw.
There are many controversies in deciding the treatment algorithm for management like, timing of surgery, open versus closed reduction, the choice of implant for internal fixation, the capsular tamponade, internal fixation versus arthroplasty, THR versus bipolar, and bipolar versus unipolar. In our study, we focused on comparing the biomechanics and results of biplane double-supported screw fixation (BDSF) versus conventional C.C. screw fixation. In both systems, the cannulation allows use of guide wires which enables use of guide system which helps to achieve parallel placement of screws (Fig. 3).
Fig. 3.
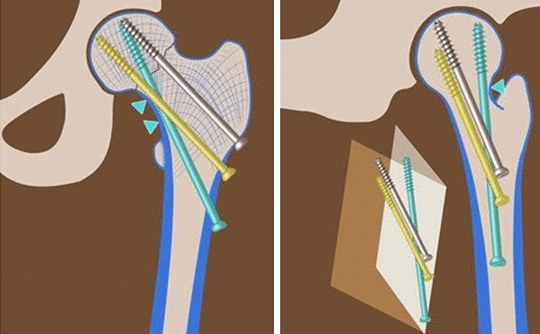
The original described method BDSF
From the study by different surgeons in the world, it has been found that biplane double-supported screw fixation (BDSF) can increase fixation stability and it has demonstrated a high reproducibility when the standard surgical procedure as described is followed. This new concept of positioning the screws in two planes makes it possible to place three cannulated screws at steeper angles to the anatomical axis of femur which in turn improve their beam function and cortical support [1]. The critical element in fracture stability is the density of the bone. Multiple screw fixation technique in itself is not free from disadvantages. Various study shows neck length is best achieved with sliding hip screw. Biomechanically, fixation is less rigid with cannulated screws when compared with sliding hip screw. Sliding hip screw buttresses better in cases with posterior comminution. The sliding hip screw also has multiple disadvantages. We have focused our study and discussion on multiple cannulated screw fixation techniques.
Hence, we have conducted this study to evaluate comparative biomechanical fixation provided with the BDSF method with the conventional CC screw fixation for treatment of femoral neck fractures with three parallel cannulated screws.
Materials and Methods
The study was conducted in the Department of Orthopaedics at L.L.R.M. Medical College, Meerut during 2018-20. The patients attending OPD, Emergency and IPD of SVBP Hospital and operated for fracture neck femur were taken up for the study. Clearance from the institutional ethical committee was taken. Procedure includes positioning of patient supine on the fracture table. Lateral incision is performed at the level of the lower border of the greater trochanter. Closed reduction maneuver Whitman's method was used (Figs. 1 and 2). Guidewires were positioned as distal at 150'-165' angle, middle at 130'-140' angle proximal parallel to 2nd middle wire as per the original described method (Fig. 3). The middle and proximal screws were placed first and then foot traction is released. Finally, the distal screw is placed (Figs. 4 and 5). Post-op care and follow-up include pain relief, wound dressing at 3rd post op day, and stitches removal at 2 weeks. We followed our patients at 1 month, 3 months, 6 months, 9 months, and 1 year with X-rays (Figs. 6 and 7) we focused on comparing the biomechanics and results of biplane double-supported screw fixation (BDSF)functional assessment (Figs. 8 and 9) using Harris hip scoring. Clinical and radiological outcome was assessed. Full weight-bearing mobilization was started at 8-12 weeks.
Figs. 4, 5.
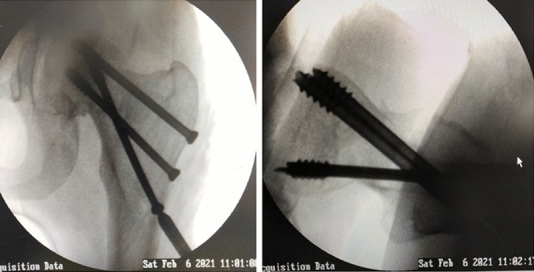
Post-operative image intensifier picture
Figs. 6, 7.

Post-operative X-ray picture on follow-up
Figs. 8, 9.

Functional outcome in patient at follow-up
Study Design
It is a prospective cohort study. There were two teams of surgeons out of which one team operated the patients with BDSF technique and second with conventional CC screw fixation technique; thus, the patients were randomly distributed into two groups. Patients were included in the study as per the following inclusion and exclusion criteria.
Inclusion Criteria
Patients agreed with and signed the informed consent form.
Garden stages I–IV fracture of neck femur
Age
< 60 years with any type of fracture of neck femur and age > 60 years with undisplaced type of fracture of neck femur
Exclusion Criteria
Patients with legal incompetence
Pediatric fractures
Patients with delayed presentations
Patients with fracture neck of femur with hip dislocation
Age > 65 years, displaced.
Patients with active sepsis of the hip joint and systemic sepsis.
Intravenous drug abusers.
Patients anesthetically unfit for surgery.
Bone diseases or neuromuscular disorders.
All the patients based on the inclusion and exclusion criteria were taken for the study. History was taken from the patients regarding mode of injury, time since injury, and any chronic illness like hypertension, diabetes mellitus, coronary artery disease, COPD, tuberculosis, stroke, osteoporosis, etc. Diagnosis was made on the clinical and radiological ground. All patients were examined clinically and investigated for preanesthetic checkup (Figs. 8, 9).
Study Group
We divided our patients in two groups:
Group A includes treatment by BDSF technique.
Group B includes treatment by conventional CC screw fixation technique.
Observation and Results
This study was conducted during 2018–20 on 35 patients who presented with fracture neck of femur and were treated with internal fixation (osteosynthesis). Amongst them, 5 patients were lost to follow-up and did not complete one year mandatory follow-up period. Hence for the study, remaining 30 patients were analyzed, 12 with BDSF and 18 with conventional CC screw.
The study comprised 12 males (40%) and 18 females (60%), of age group 15–62 years, the mean age being 40.93 years. They were grouped age and gender wise. Out of 30 patients, 2 patients were in garden type 1, 6 patients in garden stage 2, 12 patients in garden type 3, and 10 patients in garden type 4.
Most of the patients (26.67%) were in their fourth and fifth decades, 3 (10%) patients (male 1, female 2) in 10–20 years group, 6 (20%) in 21–30 group (male 1, female 5), 4 (13.33%) in 31–40 group (male 3, female 1), 8 (26.67%) in 41–50 group (males , female 5), 8 (26.67%) in 51–60 group (male 4, female 4), 1 (3.3%) in 61–70 group (male 0, female 1). Incidentally, 12 (40%) fractures were on the left side and 18 (60%) were on the right side. 16 (53.33%) fractures were sustained in road accidents, and 14 (46.67%) were sustained due to trivial injury.
In the present study, pre-reduction and post-reduction Garden index was calculated on AP skiagram under the supervision of guide and co-guide.
In all patients treated by either BDSF or conventional CC screw fixation, the GAR index improved in post-reduction X-ray as shown in Table 1.
Table 1.
Relation between Garden alignment (GAR) index and number of patients
| Garden index | No of patients |
|---|---|
| Pre-reduction | |
| 141–150 | 9 |
| 151–160 | 17 |
| 161–170 | 4 |
| Post-reduction | |
| 151–160 | 5 |
| 161–170 | 25 |
In pre-reduction Garden index, it was observed that 9 patients (30%) had Garden index between 141 and 150; 17 patients (56.67%) had Garden index between 151 and 160; while the remaining 4 patients (13.33%) had Garden index between 161 and 170.
Similarly in post-reduction, 5 patients (16.67%) had Garden index between 151 and 160; while the remaining 25 patients (83.33%) had Garden index between 161 and 170.
In this study, in conventional CC screw fixation patients, Harris Hip Score evaluated at 6th month for 14 patients was 80–89 points. 4 patients achieved fair HHS. As per garden staging, the HHS score is mentioned in Table 2.
Table 2.
Harris hip score and trends at six-month follow-up
| Garden Stage | BDSF | CCS |
|---|---|---|
| 1 | 90–100 | 90–100 |
| 2 | 80–89 | 80–89 |
| 3 | 80–89 | 70–79 |
| 4 | 70–79 | < 70 |
Residual pain score as per garden staging system in the follow-up patients is mentioned Table 3.
Table 3.
Degree of residual pain score (RPS) at 6 months
| Garden staging | BDSF | CCS |
|---|---|---|
| 1 | Grade 1–2 | Grade 1–2 |
| 2 | Grade 1–2 | Grade 1–2 |
| 3 | Grade 1–2 | Grade 2–3 |
| 4 | Grade 1–2 | Grade 2–3 |
The above Table 4 shows residual pain score grades in both methods employed.
Table 4.
Residual pain score grades in both methods employed
| Procedure | Grade 6 | Grade 5 | Grade 4 | Grade 3 | Grade 2 | Grade 1 |
|---|---|---|---|---|---|---|
| B.D.S.F | 0 | 0 | 0 | 0 | 4 | 8 |
| Conventional CC screw fixation | 0 | 0 | 0 | 9 | 9 | 0 |
| Total | 0 | 0 | 0 | 9 | 13 | 8 |
Mobility score in follow-up visit as per garden staging is mentioned in Table 5.
Table 5.
Mobility score in follow-up visit as per garden staging
| Garden staging | BDSF | CCS |
|---|---|---|
| 1 | Grades 8–9 | Grades 8–9 |
| 2 | Grades 8–9 | Grades 8–9 |
| 3 | Grades 8–9 | Grades 6–7 |
| 4 | Grades 8–9 | Grades 6–7 |
Table 6 shows the mobility scores in both the methods employed.
Table 6.
Mobility score at 6 months
| Procedure | Grades 0–1 | Grades 2–3 | Grades 4–5 | Grades 6–7 | Grades 8–9 |
|---|---|---|---|---|---|
| B.D.S.F | 0 | 0 | 0 | 0 | 12 |
| Conventional CC screw fixation | 0 | 0 | 0 | 13 | 5 |
| Total | 0 | 0 | 0 | 13 | 17 |
VAS score in follow-up visit as per garden staging is mentioned in Table 7
Table 7.
VAS score in follow-up visit as per garden staging
| Garden staging | BDSF | CCS |
|---|---|---|
| 1 | Grades 0–2 | Grades 0–2 |
| 2 | Grades 0–2 | Grades 3–5 |
| 3 | Grades 0–2 | Grades 3–5 |
| 4 | Grades 3–5 | Grades 6–8 |
Table 8 shows the VAS scores in both the methods employed.
Table 8.
VAS score at 6 months
| Procedure | Grades 0–2 | Grades 3–5 | Grades 6–8 | Grades 9–10 |
|---|---|---|---|---|
| BDSF | 4 | 8 | 0 | 0 |
| Conventional CC screw fixation | 3 | 11 | 4 | 0 |
| Total | 7 | 19 | 4 | 0 |
Complications: There were no significant complications in the study except for the discussed below.
Non-union and Osteonecrosis of Femoral Head
In our study, there is non-union and osteonecrosis of femoral head in 18% of patients managed by conventional CC screw fixation, while there is non-union in 8% of patients managed by B.D.S.F technique.
Discussion
Femoral neck fracture in elderly poses a great challenge in their treatment and rehabilitation. To avoid complications associated with long-term immobilization, internal fixation of these fractures has been accepted as the standard procedure. Successful treatment of femoral neck fracture depends on many factors such as age of the patient, general health status, medical co-morbidities, and their influence on the mobility and balance of the elderly patient, besides the commonly observed delay in surgical treatment due to financial and social reasons. Identification of possible causes of the fracture itself being unstable, situations beyond the control of surgeon, Osteopenia, age-, and gender-related variation may not allow the for ideal healing. The varus collapse, implant cut-out in head region, and intraarticular penetration remain the major causes of unacceptable outcome in failures. Various factors have been studied such as age and sex distribution, mode of trauma, and associated co-morbidities in this study along with method of fixation.
In our study, the mean age of the patients in the present study was 40.933 years as shown in Table 9. Females outnumbered males with 60% of female patients in the current study. Road Traffic Accident (RTA) set-up was the most common mode of trauma in the present study accounting for 53.33% of cases. High velocity trauma is the commoner cause of this fracture in the younger population. The high incidence of patients with RTA in the current study indicates the sample size to be comprising of predominantly younger population. The patients in elderly age group have higher number of associated medical co-morbidities mostly diabetes mellitus and hypertension. 40% of patients in the present study were associated with medical illness, most of which were diagnosed at the time of admission to the hospital. This highlights the fact that early mobilization is the key to prevent worsening of medical co-morbidities in patients suffering from fracture neck of femur. The average time between injury and surgery in the present study was 5.33 days as illustrated in Table 10. The delay in surgery in the present study in comparison with most studies is accounted by the concomitant association of various medical illnesses and other social and financial reasons. It is interesting that many patients were diagnosed to have medical illness only on hospitalization for this fracture. Table 10 shows comparison of present study with other authors.
Table 9.
Average age of patient sustaining femoral neck fracture
| Authors | Number of patients | Average age (years) |
|---|---|---|
| Filipov et al. | 88 | 76.9 |
| Garden et al. | 111 | 67.2 |
| Satish et al. | 64 | 60 |
| Tidermark et al. | 102 | 80 |
| Blomfeldt et al. | 60 | 84 |
| Guruswami et al. | 395 | 73.9 |
| Current study | 30 | 40.93 |
Table 10.
Trauma surgery interval
| Authors | Trauma surgery interval |
|---|---|
| Satish et al. | 2 days |
| Blomfeldt et al. | 2.75 days |
| Guruswami et al. | 1.54 days |
| Garden et al. | 3.68 days |
| Current study | 5.33 days |
Table 12.
Percentage of union achieved in various studies
| Authors | Total number of patients | Union (%) |
|---|---|---|
| Filipov et al. | 88 | 98.86 BDSF |
| Blomfeldt et al. | 60 | 86.67 CCS |
| Garden et al. | 111 | 81 CCS |
| Current study | 30 | 83.33 BDSF + CCS |
The average operating time was 65 min with a range of 50–90 min (Table 11). The variation in operating time was mainly influenced by whether the patient was operated by a trainee resident or a consultant and its other causes have not been compared with other works. Union was achieved in 83.33% patients in the present study which is comparable to rates reported in literature as shown in Table 12. Out of which union was achieved in 91.67% patients operated by BDSF technique, while union was achieved in 83.33% patients operated by conventional CC screw fixation technique. The average time to clinico-radiological union in current study was 13.72 weeks with a range of 9–19 weeks, which was comparable to that reported in literature in various series depicted in Table 13.
Table 11.
Duration of surgery in various studies
| Authors | Number of patients | Average duration of surgery (minutes) |
|---|---|---|
| Filipov et al. | 88 | 39 |
| Blomfeldt et al. | 60 | 19 |
| Tidermark et al. | 102 | 20 |
| Current study | 30 | 65 |
Table 13.
Average time of union in weeks
| Authors | Average time to union (weeks) |
|---|---|
| Satish et al. | 10 |
| Guruswami et al. | 14.28 |
| Current study | 13.72 |
The average time to clinico-radiological union in BDSF techniques is 12 weeks, with a range of 9–15 weeks. The average time to clinico-radiological union in conventional CC screw fixation techniques is 14.92 weeks, with a range of 11–19 weeks.
Harris hip score was developed in 1969 to assess the outcome following total hip arthroplasty [2]. It consists of eight questions and a physical examination. It has been used in a number of studies over the years for both fixation and arthroplasty, and has been shown to have high reliability and validity.
Table 14 shows that the average Harris hip score in the current study was 91.13, with 56.67% of total patients in excellent grade and 43.33% in good grade at one year. Mean HHS in patients treated by BDSF technique is 95.83, while Mean HHS in patients treated by conventional CC screw fixation technique is 88.27.
Table 14.
Harris hip score in various studies at one year
| Authors | Number of patients | Mean HHS |
|---|---|---|
| Filipov et al. | 88 | 84.26 |
| Lee et al. | 102 | 86.6 |
| Current study | 30 | 91.13 |
Most of the cases in the present study were unstable in which the outcome of deliberate valgus reduction in femoral neck fractures was analyzed to have diminished rates of screw cut-out and facilitate consolidation. Hence, we advocate anatomical reduction, if not valgus reduction in femoral neck fractures to achieve reliable functional and radiological outcomes.
Various studies has revealed fixation of fracture neck femur by conventional method has failure rate to be as high as 20–42% [3] . Reason for this failure is due to the entry point of the screws, which lies in cancellous region of proximal femur such that inter-fragmentary compression is achieved intra-operatively, so this amount of inter-fragmentary compression is not achieved in this osteoporotic bone which leads to high failure in conventional CC screw fixation 8.
Biplane double-supported screw fixation method (BDSF) is superior in this regard as it takes purchase of distal screw in cortical bone and proximal screws lie in different plane with that of distal screw.
The distal screw is the beam screw which transmits weight from head of femur to femur diaphysis directly reducing stress in cancellous proximal femur. Biplane arrangement allows enough space in neck and femur head for screw placement. Due to increased distance between entry points of proximal and distal screws, the forces are spread over large area of proximal femur which in turn reduces the incidence of fracture subtrochanteric femur which is common with conventional CC screw fixation. Placement of guidewire need to be learnt with time.
Conventional CC screw fixation and BDSF methods are similar in terms of learning curve, cost, operative time, and operation theater set-up.
Conclusion
Both BDSF and conventional CC screw fixation are good fixation methods for fracture neck of femur. But functional outcome and fracture union rates are better with BDSF Technique. Although, there are some minor problems noted in BDSF technique such as outer cortical fracture at the entry point of beam screw and opening up of anterior cortex of oblique fracture patterns. Thus, BDSF method provides reliable fixation in which early mobilization and partial weight bearing of the patient may be allowed. In our study, the sample size is small and long-term follow-up is lacking. So, other studies by different authors having large sample size and longer follow-up are required to establish BDSF method as a standard method of fixation for fracture neck of femur.
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Filipov OB. Biplane double-supported screw fixation of femoral neck fractures: Surgical technique and surgical notes. Journal of American Academy of Orthopaedic Surgeons. 2019;27(11):e507–e515. doi: 10.5435/JAAOS-D-17-00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wamper KE, Sierevelt IN, Poolman RW, Bhandari M, Haverkamp D. The Harris hip score: Do ceiling effects limit its usefulness in orthopedics? Acta Orthopaedica. 2010;81(6):703–707. doi: 10.3109/17453674.2010.537808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jilani LZ, Abbas MB, Shaan ZH, Ahmad S, Abbas M. Outcomes of BDSF technique for osteosynthesis of femoral neck fractures. Int J Burns Trauma. 2023;13(3):149–155. [PMC free article] [PubMed] [Google Scholar]


