Abstract
Introduction
Negative Pressure Wound Therapy (NPWT) is a well-established method to promote wound healing by delivering negative pressure (a vacuum) at the wound site. Enhancement of NPWT techniques may allow an innovative way of treating trauma and orthopaedic wounds which provide unique challenges. We explore the role of negative pressure wound therapy with instillation and dwell time (NPWTi-d-) in the management of trauma and orthopaedic wounds.
Materials and Methods
A comprehensive search strategy was conducted using databases of PubMed, Web of Science, Google Scholar, and Cochrane Library with the search words of 'NPWTid' or ‘NPWTi-d-’ or ‘NPWT with instillation’ or ‘Negative pressure wound treatment with instillation’ to generate this narrative review. The mechanism of action of NPWTi-d-, installation solutions and current applications in the trauma and orthopaedic wounds is evaluated.
Results
NPWTi-d- provides additional mechanism to promote wound healing in a spectrum of acute and chronic orthopaedic wounds. The technique allows local delivery of hydration and elution of antibiotics to support growth of healthy granulation tissue. Various mechanism of actions contribute in drawing the wound edges together, reduce oedema, help decontamination, deliver local antibiotic and promote healing.
Conclusion
NPWTi-d- permits an enhanced, supplementary technique to encourage wound healing in challenging traumatic and orthopaedic wounds. Future applications of NPWTi-d- will depend on cost-effectiveness analysis and development of its application guidelines based on longitudinal, randomized controlled research trials.
Keywords: Negative pressure wound therapy, Granulation tissue, Wound healing, NPWT, NPWTi-d-, Instillation
Introduction
Trauma and orthopaedic wounds pose unique challenges in terms of their complex nature and potential complications, often requiring innovative and advanced treatment modalities for optimal healing. Among the emerging techniques, negative pressure wound therapy with instillation and dwell time (NPWTi-d-) has gained significant attention as a promising approach to address the complex wound management needs in orthopaedic practice [1–3]. NPWTi-d- combines the proven benefits of negative pressure wound therapy (NPWT) with the targeted delivery of topical solutions, offering a multifaceted approach to wound healing [4, 5].
The treatment of orthopaedic wounds necessitates a holistic approach that addresses not only the wound bed but also factors such as bone and soft tissue health, infection control, and overall patient well-being. NPWTi-d- encompasses the use of a specialized wound dressing coupled with negative pressure to create an environment conducive to wound healing [6–8]. Additionally, it introduces the instillation of topical solutions into the wound bed, allowing for targeted wound cleansing, removal of debris, and delivery of therapeutics, such as antimicrobial agents and wound healing-promoting substances [9, 10].
This review article aims to provide a comprehensive overview of the application of NPWTi-d- in the treatment of orthopaedic wounds. The underlying principles of NPWTi-d-, its mechanisms of action, and the scientific evidence supporting its efficacy and safety in the orthopaedic setting will be discussed. Furthermore, we will examine the various clinical scenarios in which NPWTi-d- has demonstrated beneficial outcomes, including open fractures, surgical site infections, complex soft tissue injuries, and non-healing wounds related to orthopaedic procedures. By delving into the current literature and clinical studies, this review seeks to elucidate the specific advantages and limitations of NPWTi-d- compared to traditional orthopaedic wound management approaches. Additionally, we will discuss practical considerations for the successful implementation of NPWTi-d-, including appropriate patient selection, wound preparation, instillation solutions, and monitoring parameters.
Ultimately, this comprehensive review aims to provide orthopaedic surgeons, wound care specialists, and healthcare professionals involved in managing orthopaedic wounds with an up-to-date understanding of the role of NPWTi-d- in optimizing wound healing outcomes. Through a critical evaluation of the available evidence, we aim to shed light on the potential benefits, challenges, and future directions of NPWTi-d- in the orthopaedic field, ultimately guiding clinical decision-making in the field of orthopaedic surgery.
Materials and Methods
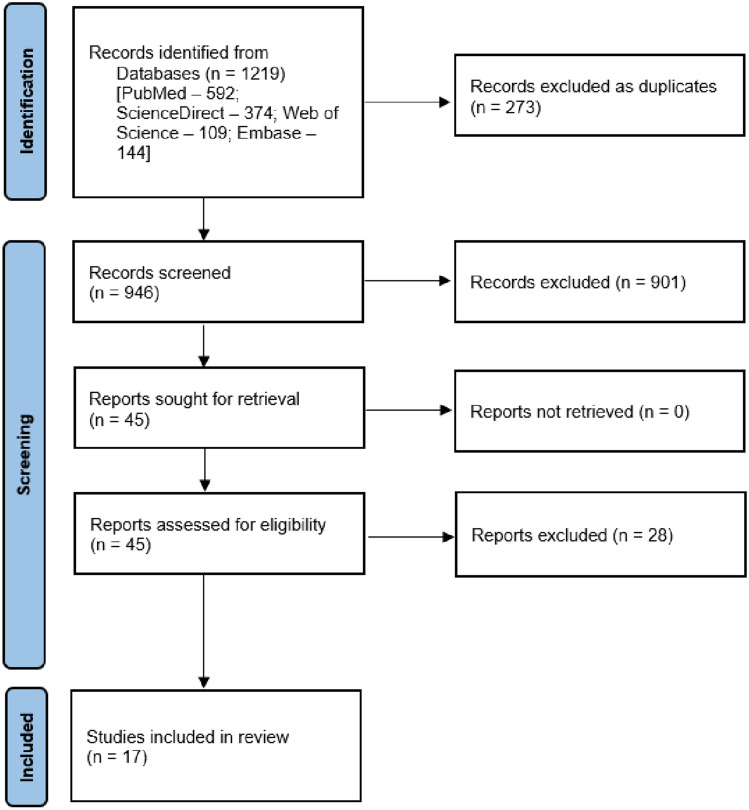
Search strategy and design: This narrative review was conducted after a comprehensive search of PubMed, ScienceDirect, Web of Science, and Embase on 01.06.2023. The following search terms were used: ‘NPWTid’ or ‘NPWTi-d-’ or ‘NPWT with instillation’ or ‘Negative pressure wound treatment with instillation’. Figure 1 depicts the articles included in this survey.
Fig. 1.
Flowchart of included literature in the study
RCTs, case–control studies, prospective and retrospective cohort studies, and case series with at least five patients were all included. There were no restrictions on the follow-up period. Exclusion criteria included pre-clinical investigations, ex vivo studies, and studies conducted in languages other than English. All titles and abstracts were evaluated by two independent reviewers. Following this first screening, the papers that matched the selection criteria were examined for full-text eligibility. In the event of a dispute between the two reviewers, a third reviewer was consulted to achieve a consensus.
Research Objectives are as follows.
RO 1: Elaborate mechanism of action of NPWTi-d-
RO 2: Current applications in the management of trauma and orthopaedic wounds
RO 3: To study significant benefits and challenges of NPWTi-d- in treatment of orthopaedic wounds
RO 4: To analyse future perspectives of NPWTi-d-
Results
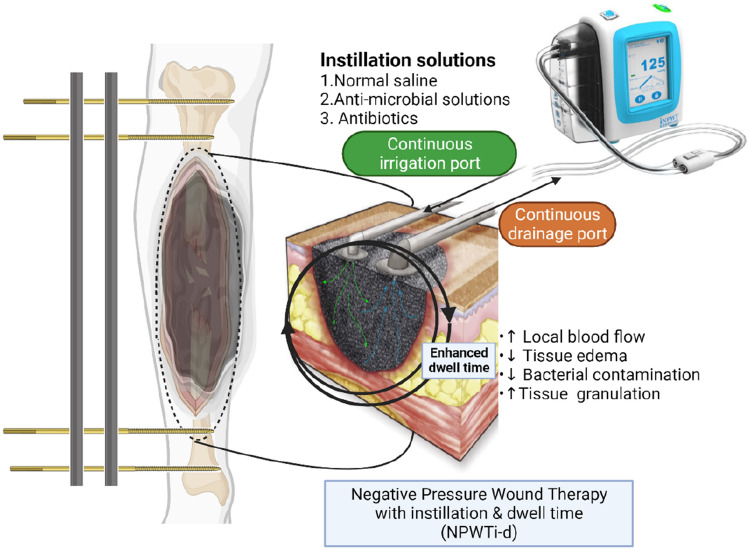
A comprehensive search strategy was conducted using databases of PubMed, Web of Science, Google Scholar, and Cochrane Library with the search words of 'NPWTid' or ‘NPWTi-d-’ or ‘NPWT with instillation’ or ‘Negative pressure wound treatment with instillation’ to generate this narrative review. Initially, a total of 251 studies met our selection criteria and after screening of abstracts and removing duplicates, 17 articles were eligible for final evaluation. The working model of NPWTi-d- is depicted in Fig. 2. The summary of 17 studies of NPWTi-d- is tabulated in Table 1.
Fig. 2.
Working model of negative pressure wound therapy with instillation and dwell time (NPWTi-d-)
Table 1.
Summary of clinical studies of NPWTi-d-
| Author (year) | Type of study | Diagnosis/type of injury | No. of patients | NPWTi-d- protocol | Solutions used | Final wound closure (duration) | Complications | Follow up |
|---|---|---|---|---|---|---|---|---|
| Leffler et al. [20] (2009) | Case series | Subacute/chronic osteomyelitis | 6 | Application of NPWTi-d- in chronic wounds and their outcomes | Polyhexanide | Six months post-surgery | No | After NPWTi-d-, bacterial swabs and tissue biopsies were sterile; after 3 to 10 months, there was no recurrence of osteomyelitis |
| Timmers et al. [21] (2009) | Prospective cohort study | Osteomyelitis of pelvis or lower limb | Case control cohort studies |
2 cohorts; I: NPWTi + debridement/antibiotics, C: standard of care (surgical debridement, gentamycin polymethyl-methacrylate beads implantation, long-term IV antibiotics) I stands for V.A.C. Instill Polyhexanide Solution; Dwell time: 10–15 min; NP: 300–600 mmHg; Mean days of treatment: 6 to 60 |
Polyhexanide Gentamicin PMMA beads |
Not available | The NPWTi-d- group underwent fewer operations and required a shorter stay in the hospital | |
| Lehner et al. [22] (2011) | Infected orthopedic implants (THA 62.5%, TKA 31.3%, 6.2% osteosynthetic material) | 32 | Polyhexanide | Not available | 86% (acutely infected) and 80% (chronically infected) of implants were retained | |||
| Brinkert et al. [23] (2013) | Various wound types that are infected or at high risk of infection (such as open fractures, infected hematomas, PUs, and non-healing postoperative dehiscence wounds) | Prospective case series to evaluate the outcomes of 131 patients with complex wounds treated with NPWTi-d- | NPWTi-d- case series; V.A.C. VeraFlo; Solution: Normal saline; Dwell time: 10 min; NP: 4–12 h; Pressure: 125 mmHg; Mean days of treatment: 12.2 | Saline | 12–19 days | No incidence of wound recurrence or dehiscence was observed at operated site |
Wound closure was achieved in 128 of 131 (98%) wounds • With respect to filling dead space more rapidly and completely, NPWTi-d- using saline showed improved granulation tissue production compared with NPWT |
|
| Fluieraru et al. [24] (2013) | Complex wounds (such as vast undermining tracts or deep wounds) or infected wounds that did not respond to NPWT |
Retrospective case series of 24 patients - 12 patients who had been unsuccessfully treated with NPWT - 12 patients with complex wounds |
Case series for NPWTi-d-; V.A.C. Instillation; Solution: Sterile saline; Dwell time: 10 min; NP: 4 h; Pressure: 125 mmHg; Days of treatment: 6–15 |
Isotonic saline | After one month | The lower extremities of the patient who did not recover was too devascularized to granulate effectively. The main outcomes of instillation therapy in these patients included encouraging the growth of granulation tissue and filling weakened holes | ||
| Gabriel et al. [25] (2014) |
Retrospective analysis comparing patients with NPWT (n = 34) with NPWTi-d- (n = 48) • A hypothetical economic model that compares patients with NPWT and NPWTi-d- utilising cost assumptions for debridement |
Saline or polyhexanide | The NPWT-instillation-treated wounds were closed in 29.6 ± 6.5 days |
Between NPWTi-d- and NPWT patients, there were significant differences (P 0.001) for the following: mean OR debridement (2.0 versus 4.4) - average length of hospital stay (8–1 vs. 27–4) - average LOT (4–1 versus 20–9) - Mean time to wound closure (4–1 days as opposed to 20–9) • The fictitious economic model suggested that there could be an average $8143 savings for OR debridement between NPWTi-d-($6786) and NPWT ($14 929) patients • The average cost of therapy varied between the two groups by $1418 ($799 for NPWTi-d- against $2,217 for NPWT) |
||||
| Goss et al. [26] (2014) | A substantial bacterial bioburden (> 105 CFU/g tissue) is present in DFUs, VSUs, and other wound aetiologies | Prospective pilot research in 13 patients |
Prospective contemporaneous cohort design; NPWT (C) vs. NPWTi-d- I: V.A.C. VeraFlo; C: Dakin's solution; Dwell time: 10 min; NP: 60 min; Pressure: 125 mmHg; Days of Treatment: 7 |
Dakin | Not available | NPWTi-d- wound treatment resulted in a decrease in the mean CFU/gram of tissue culture | ||
| Kim et al. [17] (2015) | Chronic wounds (neuropathic, ischaemic, traumatic) |
142 NPWT group: 74 patients • NPWTi-d- 6-min dwell group: 34 patients • NPWTi-d- 20-min dwell: 34 patients |
NPWT (C) vs. NPWTi-d- (I) (2 Subgroups I1 and I2); retrospective cohort-historical control design C: InfoV.A.C.; NP: -125 mm Hg, 7 days of treatment I1: V.A.C. VeraFlo; solution: polyhexanide + betaine; Dwell time: 6 min; NP: I1: 3.5 h; Pressure: − 125 mmHg; Days of treatment: 7 I2: V.A.C. VeraFlo; solution: polyhexanide + betaine; Dwell time: 20 min; NP: 2 h; Pressure: 125 mmHg; Days of treatment: 7 |
Prontosan | Not available | Patients treated with NPWTi-d- in the 6-min dwell group showed significantly lower rates of Higher percentages of wounds were closed before discharge (94% versus 62%) and had improved cultures for Gram-positive bacteria (90% versus 63%) (P 0001) | ||
| Wolvos [27] (2015) | Variety of infected or complex wounds | Pilot study of consecutive case series with seven patients |
NPWTi-d- case series V.A.C. VeraFlo; solution: Microcyn, Dakin’s; Dwell time: 5–10 min; NP: 2–4 h; Pressure: 100–125 mmHg; Days of treatment: 7–54 |
Microcyn®, Dakin’s Solution® (quarter strength) | Six months after surgery | No complications noted | The overall length of therapy ranged from 7 to 54 days. Wounds were closed by primary, secondary, delayed primary intention, or an STSG. Six of seven patients got NPWTi-d-, and one patient had NPWT alone | |
| Davis et al. [28] (2020) | Complex foot infections (Charcot arthropathy, collagen vascular disease, hypercoagulable state) | Randomized clinical study in 90 patients | Saline | 12 weeks | No | Between patients treated with various NPWT devices or NPWT with and without irrigation, we were unable to detect any appreciable differences in clinical outcomes or adverse events | ||
| Sung et al. [29] (2020) | Complex and infected wounds (necrotizing fasciitis, Fournier’s gangrene, and gas gangrene) | Prospective study in 51 patients | 0.9% Normal saline + 1% povidine iodine solution | Two individuals had partial graft failure, but after two weeks of secondary healing |
All wounds were closed Though graft failure was noted in 2 cases, they healed by secondary healing by 2 weeks |
|||
| Delapena et al. [30] (2020) | Necrotizing fasciitis | 10 | Wounds were intermittently managed with NPWTi-d- using HOCL | HOCL | Not available | No | Shorter hospital stays and improved wound care | |
| Schreiner et al. [31] (2020) | Sternoclavicular joint infection | 27 (21 men, 6 women) | Comparison of NPWT alone versus NPWTi-d- for the management of this condition | Polyhexanide | Not available | No | In patients with SCJI, the NPWTi-d-appears to be an effective therapy, resulting in a higher frequency of bacterial eradication and a shorter duration of wound care | |
| Elhessey et al. [32] (2021) | Complex infected orthopaedic wounds | Prospective study in 20 patients | The VeraLink Cassette (KCI, San Antonio, Texas) spike allowed to connect to the system. Vacuum-assisted closure (VAC) therapy was selected for the pre-programmed therapy unit, and it was started to offer a 20-min soak/dwell time followed by 2 h of therapy at a pressure of 125 mm Hg and medium pressure intensity | Prontosan | Wound closure at 6 weeks | Wound closure was achieved in 65% of cases | ||
| Zhang et al. [33] (2021) | Necrotizing fasciitis | 32 | Following aggressive surgical debridement, NPWTi-d- was initiated by instilling solution with a set dwell time of 5–10 min, followed by continuous NPWT of 125 mm Hg for 3–5 h | Prontosan | After 9–16 days | No | All wounds were successfully closed and no recurrence of infection or adverse event was observed during NPWTi-d-treatment | |
| Enodien et al. [34] (2021) | Diabetic foot syndrome | Following surgical debridement, ActiMaris sensitiveTM NPWTi-d- with super oxidised solution was infused. NaCl 1.2% and NaOCl 0.04% make up the alkaline (pH 8.5–10) hypertonic sea salt solution | Super oxidized solution | Six weeks | After 14 days of therapy, the wound and granulation tissue recovered quickly | |||
| Pellegrin et al. [35] (2023) | Chronic wounds in orthoplastic surgery | To compare outcome of NPWTi-d- vs standard of care in orthoplastic surgeries | Saline | Not available | No | The results demonstrated that infected wounds treated with NPWTi-d- had a successful outcome when compared to NPWT |
Mechanism of Action of NPWTi-d-
Negative pressure setting: The innermost dressing layer is accessible to the irrigation solution and the wound bed when the proper negative pressure setting is used during the NPWTi phase. The majority of investigations have demonstrated that 125psi of negative pressure has beneficial and encouraging effects. Therefore, according to international consensus and following the findings of the majority of experimental research, the proper negative pressure setting for NPWTi should be between 125 and 150 mmHg [11, 12].
Installation mode: Persistent and intermittent instillation modes are typically included in the instillation mode. The NPWTi-d- intermittent instillation mode, which allows the solution to freely infiltrate the whole wound, has cycles made up of two phases: the negative pressure phase and the instillation and dwell phase. As a result, the intermittent instillation mode of NPWTi-d- is the advised therapeutic mode, and a 2- to 3-h negative pressure phase is advised [6, 13, 14]. The negative pressure is halted or lessened when the solution is infused into the dressing and wound bed, allowing it to thoroughly penetrate the wound tissue and exudate. The solution’s capacity and dwell time, however, continue to be debatable. The amount of solution needed when the dressing foam is completely absorbed and saturated is referred to as the “suitable volume”. A volume that is too high will result in skin tissue infiltration at the margin of the incision, whereas a volume that is too low would compromise the irrigation effect. Longer dwell durations could have a harmful effect, so they are also crucial. It is currently uncertain how the installation solution will affect the dressing foam’s ability to last. The ideal dwell period is typically 10 min, and the best volume is thought to guarantee that the solution can completely penetrate the dressing foam up until the sealing film starts to bulge [15]. However, in clinical practice, these conditions are typically challenging to implement, and the sealing film is readily harmed due to the high likelihood of an excessive solution level or prolonged dwell time.
NPWTi duration time: The type of wound and the goal of treatment will determine how long NPWTi-d- will be administered. Acute non-infectious wounds require NPWTi-d- treatment for 3–14 days, and chronically infected wounds require treatment for 7–60 days, according to studies [7]. It is generally accepted that NPWTi-d- termination should be taken into consideration once clinical objectives have been met, which include satisfactory wound bed cleaning, stimulation of granulation tissue, preparation for skin grafting or skin flap surgery, and dressing replacement.
Installation Solutions
Normal saline: Commonly used, safe, and non-toxic, normal saline is well tolerated. It works well to improve the formation of granulation tissue and to remove necrotic tissue from all kinds of wounds. Leung et al. discovered that NPWTi with regular saline may effectively stimulate the production of granulation tissue in a pig acute trauma model [16]. Kim et al. discovered that the effects of NPWTi when coupled with ordinary saline were similar to those of NPWTi with an antimicrobial solution (0.1% PHMB) following surgical debridement [17]. Therefore, the first implanted fluid for NPWTi is advised to be normal saline, according to the global community.
Antimicrobial solutions: A range of chemical antiseptics, such as hypochlorous acid solution, sodium hypochlorite solution, silver ion solution, and polyhexamethylene biguanide (PHMB) solution, have been chosen as instillation solutions with NPWTi in the clinical setting. As compatible NPWTi instillation solutions, the international community often suggests antimicrobial solutions such as hypochlorous acid solution, sodium hypochlorite solution, acetic acid solution (0.25–1.0%), and polyhexamethylene biguanide (0.1%) + betaine (0.1%). PHMB (0.1%) and betaine (0.1%), which exhibit wide-ranging antibacterial activity, are the two main ingredients in the Prontosan solution [18]. Both bacterial growth and biofilm activity can be considerably inhibited by it. It is frequently used in chronic wound infections where bacterial biofilm development is strongly expected. Strong oxidizer solutions like Microcyn and Dermacyn are primarily made of sodium hypochlorite and hypochlorous acid. According to Landsman et al., irrigating diabetic foot sores with Microcyn solution effectively treats infections. Microcyn/Dermacyn instillation treatments for NPWTi are secure and efficient [19]. Sodium hypochlorite is the substance that makes Dakin’s solution effective. It has already been proven that Dakin’s solution has an antibacterial impact on Enterococcus, Pseudomonas aeruginosa, and MRSA. Additionally, publications have recognized the therapeutic benefits of additional antimicrobial solutions, such as iodine solution, oxygen-loaded solution, peroxy acid solution, and chlorhexidine solution, which are utilized for NPWTi.
Antibiotics: Although vancomycin, polymyxomycin B, and gentamicin have been documented, the use of antibiotics as a solution for instillation remains controversial.
Discussion
Negative pressure wound therapy, also known as vacuum-aided wound therapy, is a form of wound dressing that constantly or intermittently applies sub-atmospheric pressure to the surface of a wound to help in healing [20]. It was created in the 1990s and includes semipermeable foils, wound dressings, drainage tubes, and vacuum sources [7]. Despite the existence of numerous studies comparing the outcomes of NPWTi-d- with NPWT alone, there is a lack of evidence to support its benefits in the context of orthopaedic and plastic surgery, particularly in several complex wound types where advanced wound dressings or wet-to-moist dressing changes are used [20].
How NPWTi-d- Differs from Conventional NPWT
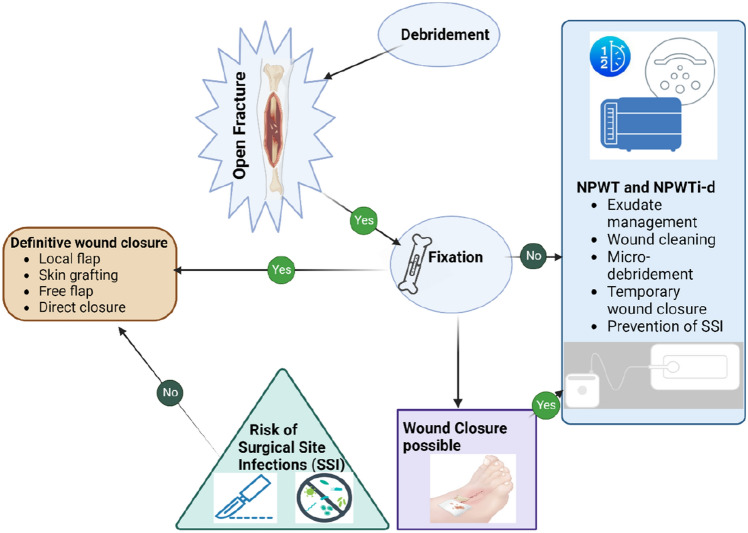
In 1998, Fleischmann proposed the extension of the NPWT technology by introducing the concept of instillation and dwell time (NPWTi-d-). The procedure was divided into three stages: irrigation, dwell, and drainage [7]. In addition to the effects of standard NPWT, which promote healing by increasing local blood flow, reducing tissue edema, reducing bacterial concentration in the area, and increasing tissue granulation, NPWTi-d- may provide additional benefits in terms of wound cleansing [20]. The treatment outcomes in animal studies have shown that NPWTi-d- generated more granulation tissue and lesser bacterial growth than conventional NPWT [8, 21–23]. Additionally, it can promote exudate and necrosis removal both before and following surgical debridement [7]. NPWTi-d- allows for the intermittent instillation of liquids into wounds while maintaining negative pressure in a sealed environment [15, 24]. The application of NPWTi-d- in orthopaedics is depicted in Fig. 3.
Fig. 3.
Application of NPWTi-d- in orthopaedics
Advantages of NPWTi-d-
De Pellegrin et al. stated that NPWTi-d- offers superior wound closure rates and fewer problems than NPTW or traditional dressings for the management of orthoplastic wounds (P < 0.05) [20]. Several comparison studies have shown that using NPWTi-d- and saline injection results in increased granulation tissue formation as compared to standard NPWT [25]. NPWTi-d- with polyhexanide instillation compared to NPWT, according to Kim et al. [3] there were fewer surgical visits, hospital stay was reduced, a shorter duration to the final surgical operation, and an increased proportion of wounds that are healed before discharge. NPWTi-d- has also been associated with fewer difficult and unpleasant dressing changes than NPWT. According to Gupta et al., the demonstrated clinical improvements make NPWTi-d- a potentially cost-effective supplementary technique of treating big, complex, and infected wounds in inpatient settings [22].
Disadvantages of NPWTi-d-
NPWTi-d- does not complement surgery or debridement. If the predetermined treatment plan and timeframe are not feasible, alternative treatment options should be considered. NPWTi-d- is advised not to use over split-thickness skin grafts, dermal replacements, wounds with organs and veins that are vulnerable and exposed, lesions covered in untreated abscesses, and critically ischemic wounds. NPWTi-d- should not be used as a bolster dressing, in contrast to normal NPWT. When hemostatic agents have been utilized in the wound bed, NPWTi-d- should not be started [26]. A case of tension pneuomocephalous has been report after the use of NPWTi-d- in post-surgical spinal infection [27].
Applications of NPWTi-d- in Orthopaedics
(a) Acute Wounds
In Orthopaedics, open fractures, necrotizing fasciitis, and soft tissue injuries are typical acute wounds. The basics of treating open fractures are to prevent and limit wound infection and to cover the wound as quickly as feasible. Active wound drainage is provided by NPWTi-d- and continuous wound irrigation guarantees that the wound is continuously cleaned, preventing secondary infection and cutting treatment time. Ali et al. described a case of an open tibia fracture that was successfully treated with NPWTi-d- and skin grafts [28]. The case's primary goals preserving the leg's structural integrity, achieving bone union, and preventing infection were all met.
Numerous issues, including inadequate blood flow and wound infection, are frequently present in severe soft tissue injuries. Because of infection or oedema, primary closure cannot be established, and tissue with low vitality may continue to necrose and discharge. In addition to covering and protecting the wound, NPWTi-d- may efficiently drain wound exudate, necrotic tissue, and toxins [29, 30]. This promotes the formation of granulation tissue, which in turn produces the ideal environment for secondary wound repair [31].
When Ali et al. used NPWT and NPWTi-d- to treat a soft tissue injury to the lower extremity, even when there is fibrous and non-viable tissue, granulation tissue immediately developed over the exposed bone and a skin graft was used to successfully seal the wound [28]. In contrast to NPWT alone, Omar used NPWTi-d- with normal saline solution to treat acute lower extremity soft tissue injuries [32]. The findings demonstrated that NPWTi-d- could greatly shorten hospital stays and speed up wound healing, but there was no discernible difference between the two therapies in terms of the therapeutic result.
(b) Chronic Wounds
Chronic refractory and complex orthopaedic wounds [chronic infected wounds, chronic osteomyelitis, and wounds with bone, tendon, or internal fixation exposure] are extremely prevalent and untreatable. In addition to successfully removing damaging inflammatory cytokines, enhancing the wound microenvironment, reducing wound infection, encouraging the development of granulation tissue, and setting the stage for secondary repair, NPWTi-d- is an excellent approach for treating chronic wounds [33–35].
Gabriel found that when treating a variety of complex infected wounds, NPWTi-d- dramatically reduced the wound microbial load, length of stay in the hospital, and wound healing when compared to traditional wound care [26]. Hu discovered that using NPWTi-d- with a silver ion solution effectively controlled wound infection and greatly decreased hospital stay, complication occurrence, and blood inflammation [36]. Goss et al. emphasized that the use of NPWTi-d- after surgical debridement in chronically infected lower extremity wounds can significantly reduce the wound microbial burden when compared to NPWT alone. These advantages are favorable for future wound restoration [34].
Delapena et al. found that in patients with SCJI, the NPWT in conjunction with instillation and dwell time appears to be an effective therapy, resulting in a higher incidence of bacterial eradication and shorter wound care [37]. Sung et al. [38] and Rupert et al. [39] discovered that following wound debridement, the use of NPWTi-d- dramatically reduced the risk of infection returning, the length of stay in the hospital, and the number of operations when compared to conventional treatments (conventional surgical debridement, placement of gentamicin with sustained release, and long-term intravenous antibiotic infusion) [38, 39]. Jukema et al. demonstrated a decrease in the length of the infection's therapy, the quantity of surgeries performed, the length of hospitalization, and the recurrence rate in a group of patients with post-traumatic osteomyelitis [40].
Diabetes-related foot ulcers, which are brought on by a confluence of vascular conditions, neuropathy, and impeded wound healing, are among the leading causes of morbidity and mortality in diabetes patients. The application of NPWTi-d- in treating diabetic foot infections is promising, because it may provide additional benefits over NPWT alone, such as a reduction in bacterial count in wound bed, promotion of the growth of granulation tissue, and offering wound irrigation in a secure setting [30, 41]. Enodien et al. found that NPWTi-d- with the instillation of a superoxidized solution assisted in wound healing, the removal of infectious material, and the prevention of infection transmission [42]. Additionally to antibiotics, with diabetic foot syndrome comorbidities, and heavily infected wounds, this approach may still be beneficial for certain individuals.
Comparing NPWTi-d- to conventional NPWT alone in the treatment of ischial and sacral pressure sores, it has been demonstrated that NPWTi-d- aids in irrigating the wound, removing fibrinous exudates, and encouraging the growth of granulation tissue, all of which are associated with a decrease in surgical debridements and a reduction in hospital stays [43]. After operative debridement, wound closure using various local flaps, and treatment with NPWTi-d-, patients with pressure ulcers in various locations showed improvements in terms of aiding preparing the wound bed for subsequent healing [7, 31, 44]. Instillation and dwell time as an adjunct to NPWT was used in colonised wounds showed significant decontamination, reduction in bacterial count and improved granulation tissue to provide successful reconstruction [45].
(c) Salvage Orthopedic Fixation Hardware
NPWTi-d- has been tried in patients with post-fracture fixation surgical site infection with good success. The patients were manged with intramedullary and subcutaneous antibiotics and NPWT without removal of implants [46].
Newer Advances in NPWTi-d-
Newer modifications to NPWTi-d- include a Reticulated open cell foam dressing with through holes (ROCF-CC) which has been shown to be effective in accelerating wound healing. ROCF-CC is made of a highly porous foam with through holes that allow for increased drainage of wound exudate and better oxygenation of the wound bed. A recent study found that ROCF-CC was more effective than traditional NPWTi dressings in promoting wound healing in patients with diabetic foot ulcers. The study found that ROCF-CC dressings led to a significantly faster reduction in wound area and a higher percentage of wounds that healed completely. Another recent study found that ROCF-CC dressings were effective in reducing pain and improving quality of life in patients with chronic wounds. The study found that ROCF-CC dressings led to a significant reduction in pain scores and an improvement in quality of life measures, such as sleep quality and ability to perform daily activities [47].
Smart NPWTi-d-: Smart NPWTi-d- dressings are made with materials that can respond to changes in the wound environment. For example, some smart NPWTi-d- dressings can change color when they are exposed to bacteria, which can help clinicians to identify infected wounds. Other smart NPWTi-d- dressings can release drugs or other therapeutic agents in response to changes in the wound pH or temperature [45].
NPWTi-d- with nanomaterials: Nanomaterials have the potential to improve the performance of NPWTi-d- dressings in a number of ways. For example, nanomaterials can be used to create NPWTi-d- dressings that are more porous, have a higher surface area, and are more resistant to bacterial colonization [48].
3D-printed NPWTi-d-: 3D printing can be used to create custom-made NPWTi-d- dressings that are specifically tailored to the needs of each individual patient. This can be particularly beneficial for patients with complex wounds or wounds that are difficult to dress with traditional methods [49].
Future of NPWTi-d-
NPWTi-d- is a promising new treatment for difficult wounds. It combines the benefits of drainage and irrigation to successfully control local infection, improve wound healing, and eliminate exudate and necrotic tissue. Numerous studies and applications of NPWTi-d- have produced encouraging results. It is anticipated that NPWTi-d- will be used to treat a wide range of difficult wounds in the future.
Limitations must be understood, though, as the effectiveness of NPWTi-d- is influenced by a variety of variables, including the patient’s overall health status, the wound characteristics and anatomical location and the treatment parameters. In addition, the majority of the current guidelines for the use of NPWTi-d- and its indications make reference to the conclusions of case review research and expert consensus. Therefore, additional randomized and controlled trial research are necessary to assure optimal treatment by choosing the right patient, treating the wound consistently, and creating an environment that addresses various wound types, as well as the customization, standardization, and improvement of therapy settings.
Another crucial topic of discussion is cost-effectiveness analysis, which enables comprehension of a medical or surgical procedure’s viability. NPTWi-d-’s cost-effectiveness in comparison to other methods of wound management in various fields has not yet been demonstrated in the literature. This is also consistent with the current review, which only uses data from one trial to determine if NPWTi-d- is cost-effective. The enhanced efficiency in achieving complete wound closure may justify the costs associated with its consumables, and it may also assist alleviate the costs associated with delayed healing, therefore, future research should pay particular attention to this important feature.
This review is limited by the lack of large-scale randomized controlled trials, which precludes definitive conclusions about the efficacy and safety of NPWTi-d-. Additionally, there is no consensus on several important aspects of NPWTi-d-, including its impact on patient pain and comfort, ideal patient profile selection, efficacy against Gram-positive and Gram-negative bacteria, optimal instillation solution and volume, and cost-effectiveness compared to standard treatments. Further clinical trials are needed to establish definitive guidelines for the use of NPWTi-d- in clinical practice. Despite these limitations, NPWTi-d- remains a promising candidate for the management of complex wounds.
Conclusions
NPWTi-d- emerges as a groundbreaking approach for addressing a wide spectrum of wounds encountered in trauma and orthopaedic clinical settings. Its multifaceted mechanism of action introduces an additional dimension to the management protocol for acute, chronic, and stubborn wounds. NPWTi-d- offers the valuable advantages of promoting wound hydration and facilitating localized antibiotic delivery. The future utilization of this technique in clinical practice will be further refined through the establishment of application guidelines, rigorous cost–benefit assessments, and the outcomes derived from longitudinal, randomized trials.
Funding
Nil.
Data Availability
No data available.
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Norman G, Shi C, Goh EL, Murphy EM, Reid A, Chiverton L, et al. Negative pressure wound therapy for surgical wounds healing by primary closure. The Cochrane Database of Systematic Reviews. 2022 doi: 10.1002/14651858.CD009261.pub7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elhessy AH, Chaudhry AR, Hammouda AI, Giacobbe SD, Gesheff MG, Conway JD. Experience with negative-pressure wound therapy with instillation in complex infected orthopaedic wounds. International Wound Journal. 2021;18(6):902–908. doi: 10.1111/iwj.13592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim PJ, Attinger CE, Crist BD, Gabriel A, Galiano RD, Gupta S, et al. Negative pressure wound therapy with instillation: Review of evidence and recommendations. Wounds: A Compendium of Clinical Research and Practice. 2015;27(12):S2–S19. [PubMed] [Google Scholar]
- 4.Gabriel A, Shores J, Heinrich C, Baqai W, Kalina S, Sogioka N, et al. Negative pressure wound therapy with instillation: A pilot study describing a new method for treating infected wounds. International Wound Journal. 2008;5(3):399–413. doi: 10.1111/j.1742-481X.2007.00423.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tingting S, Xinyue F, Tiantian Y, Xiao A, Rui L, Feng L, et al. Comparison of the effects of negative pressure wound therapy and negative pressure wound therapy with instillation on wound healing in a porcine model. Frontiers in Surgery. 2023;10:1080838. doi: 10.3389/fsurg.2023.1080838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fernández L. The utility of negative pressure wound therapy with instillation for wound bed preparation. Chronic Wound Care Management and Research. 2019;6:51–58. doi: 10.2147/CWCMR.S198418. [DOI] [Google Scholar]
- 7.Wu L, Wen B, Xu Z, Lin K. Research progress on negative pressure wound therapy with instillation in the treatment of orthopaedic wounds. International Wound Journal. 2022;19(6):1449–1455. doi: 10.1111/iwj.13741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giri P, Krishnaraj B, Chandra SS, Sistla S, Basu D, Shankar G, et al. Does negative pressure wound therapy with saline instillation improve wound healing compared to conventional negative pressure wound therapy?—A randomized controlled trial in patients with extremity ulcers. Annals of Medicine and Surgery. 2021;61:73–80. doi: 10.1016/j.amsu.2020.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faust E, Opoku-Agyeman JL, Behnam AB. Use of Negative-Pressure Wound Therapy With Instillation and Dwell Time: An Overview. Plastic and Reconstructive Surgery. 2021;147(1S–1):16S. doi: 10.1097/PRS.0000000000007607. [DOI] [PubMed] [Google Scholar]
- 10.Biermann N, Wallner S, Martini T, Spoerl S, Prantl L, Taeger CD. Negative pressure wound therapy with instillation: analysis of the rinsing fluid as a monitoring tool and approach to the inflammatory process: A pilot study. Journal of Clinical Medicine. 2023;12(2):711. doi: 10.3390/jcm12020711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Normandin S, Safran T, Winocour S, Chu CK, Vorstenbosch J, Murphy AM, et al. Negative pressure wound therapy: mechanism of action and clinical applications. Seminars in Plastic Surgery. 2021;35(3):164–170. doi: 10.1055/s-0041-1731792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meloni M, Izzo V, Vainieri E, Giurato L, Ruotolo V, Uccioli L. Management of negative pressure wound therapy in the treatment of diabetic foot ulcers. World Journal of Orthopedics. 2015;6(4):387–393. doi: 10.5312/wjo.v6.i4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim PJ, Attinger CE, Constantine T, Crist BD, Faust E, Hirche CR, et al. Negative pressure wound therapy with instillation: International consensus guidelines update. International Wound Journal. 2019;17(1):174–186. doi: 10.1111/iwj.13254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasan MY, Teo R, Nather A. Negative-pressure wound therapy for management of diabetic foot wounds: A review of the mechanism of action, clinical applications, and recent developments. Diabetic Foot & Ankle. 2015;6(1):27618. doi: 10.3402/dfa.v6.27618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aycart MA, Eble DJ, Ross KM, Orgill DP. Mechanisms of action of instillation and dwell negative pressure wound therapy with case reports of clinical applications. Cureus. 2018;10(9):e3377. doi: 10.7759/cureus.3377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leung BK, LaBarbera LA, Carroll CA, Allen D, McNulty AK. The effects of normal saline instillation in conjunction with negative pressure wound therapy on wound healing in a porcine model. Wounds: A Compendium of Clinical Research and Practice. 2010;22(7):179–187. [PubMed] [Google Scholar]
- 17.Kim PJ, Attinger CE, Oliver N, Garwood C, Evans KK, Steinberg JS, et al. Comparison of outcomes for normal saline and an antiseptic solution for negative-pressure wound therapy with instillation. Plastic and Reconstructive Surgery. 2015;136(5):657e–664e. doi: 10.1097/PRS.0000000000001709. [DOI] [PubMed] [Google Scholar]
- 18.Kanapathy M, Mantelakis A, Khan N, Younis I, Mosahebi A. Clinical application and efficacy of negative pressure wound therapy with instillation and dwell time (NPWTi-d): A systematic review and meta-analysis. International Wound Journal. 2020;17(6):1948–1959. doi: 10.1111/iwj.13487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Landsman A, Blume PA, Jordan DA, Vayser D, Gutierrez A. An open-label, three-arm pilot study of the safety and efficacy of topical Microcyn Rx wound care versus oral levofloxacin versus combined therapy for mild diabetic foot infections. Journal of the American Podiatric Medical Association. 2011;101(6):484–496. doi: 10.7547/1010484. [DOI] [PubMed] [Google Scholar]
- 20.De Pellegrin L, Feltri P, Filardo G, Candrian C, Harder Y, Galetti K, et al. Effects of negative pressure wound therapy with instillation and dwell time (NPWTi-d) versus NPWT or standard of care in orthoplastic surgery: A systematic review and meta-analysis. International Wound Journal. 2023;20(6):2402–2413. doi: 10.1111/iwj.14072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phillips PL, Yang Q, Schultz GS. The effect of negative pressure wound therapy with periodic instillation using antimicrobial solutions on Pseudomonas aeruginosa biofilm on porcine skin explants. International Wound Journal. 2013;10(s1):48–55. doi: 10.1111/iwj.12180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gupta S, Gabriel A, Lantis J, Téot L. Clinical recommendations and practical guide for negative pressure wound therapy with instillation. International Wound Journal. 2016;13(2):159–174. doi: 10.1111/iwj.12452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Novak A, Khan WS, Palmer J. The evidence-based principles of negative pressure wound therapy in trauma & orthopedics. The Open Orthopaedics Journal. 2014;8:168–177. doi: 10.2174/1874325001408010168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anghel EL, Kim PJ, Attinger CE. A solution for complex wounds: The evidence for negative pressure wound therapy with instillation. International Wound Journal. 2016;13(S3):19–24. doi: 10.1111/iwj.12664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brinkert D, Ali M, Naud M, Maire N, Trial C, Téot L. Negative pressure wound therapy with saline instillation: 131 patient case series. International Wound Journal. 2013;10(Suppl 1):56–60. doi: 10.1111/iwj.12176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gabriel A. Integrated negative pressure wound therapy system with volumetric automated fluid instillation in wounds at risk for compromised healing. International Wound Journal. 2012;9(Suppl 1):25–31. doi: 10.1111/j.1742-481X.2012.01014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Katsumi S, Shinohara A, Kajiwara T, Saito M. Tension pneumocephalus associated with negative pressure wound therapy with instillation and dwell time for methicillin-resistant staphylococcus aureus infection after spinal deformity surgery. European Spine Journal: Official Publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2022;31(12):3776–3781. doi: 10.1007/s00586-022-07367-9. [DOI] [PubMed] [Google Scholar]
- 28.Ali M, Reda FM, Abbassi H, Issaoui H, Gargouri M, Razanabola F. Management of a severe degloving injury with a type 2 open tibia fracture using negative pressure wound therapy with instillation and dwell time. Wounds: A Compendium of Clinical Research and Practice. 2020;32(12):E110–E113. [PubMed] [Google Scholar]
- 29.Reider K, McElroy E, Lemay S, Reider K, Faust E, Lemay S. The use of negative pressure with instillation and dwell for the treatment of necrotizing fasciitis. Cureus. 2018 doi: 10.7759/cureus.3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhao Y, Dai X, Sun Y, Liao W, Peng Y, Yang J. Efficacy and clinical value of negative-pressure wound therapy with instillation (NPWTi) of compound phellodendron liquid in the treatment of diabetic foot ulcer: A prospective cohort study. Computational and Mathematical Methods in Medicine. 2022;2022:e7540020. doi: 10.1155/2022/7540020. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 31.Matiasek J, Djedovic G, Kiehlmann M, Verstappen R, Rieger UM. Negative pressure wound therapy with instillation: effects on healing of category 4 pressure ulcers. Plastic and Aesthetic Research. 2018;5:36. doi: 10.20517/2347-9264.2018.50. [DOI] [Google Scholar]
- 32.Omar M, Gathen M, Liodakis E, Suero EM, Krettek C, Zeckey C, et al. A comparative study of negative pressure wound therapy with and without instillation of saline on wound healing. Journal of Wound Care. 2016;25(8):475–478. doi: 10.12968/jowc.2016.25.8.475. [DOI] [PubMed] [Google Scholar]
- 33.Hasegawa IG, Murray PC. Circumferential negative pressure wound therapy with instillation and dwell prior to delayed flap coverage for a type IIIB open tibia fracture. Cureus. 2019;11(4):e4511. doi: 10.7759/cureus.4511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goss SG, Schwartz JA, Facchin F, Avdagic E, Gendics C, Lantis JC. Negative pressure wound therapy with instillation (NPWTi) better reduces post-debridement bioburden in chronically infected lower extremity wounds than NPWT alone. The Journal of the American College of Clinical Wound Specialists. 2014;4(4):74–80. doi: 10.1016/j.jccw.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang C, Goss SG, Alcantara S, Schultz G, Lantis IJ, C. Effect of negative pressure wound therapy with instillation on bioburden in chronically infected wounds. Wounds: A Compendium of Clinical Research and Practice. 2017;29(8):240–246. [PubMed] [Google Scholar]
- 36.Si-ke HU. The laboratory indexes and clinical analysis of Vacuum Sealing Drainage (VSD) combined with silver ion urrigation in the treatment of infected wounds. Journal of Clinical Transfusion and Laboratory Medicine. 2019;21(2):211. doi: 10.3969/j.issn.1671-2587.2019.02.029. [DOI] [Google Scholar]
- 37.Delapena S, Fernández LG, Foster KN, Matthews MR. Negative pressure wound therapy with instillation and dwell time for the management of complex wounds: A case series. Wounds: A Compendium of Clinical Research and Practice. 2020;32(12):E96–E100. [PubMed] [Google Scholar]
- 38.Sung JY, Bae YC, Nam SB, Kim JH. Clinical outcomes of negative-pressure wound therapy with instillation without commercial devices in the treatment of complex wounds. Journal of Wound Management and Research. 2020;16(1):13–20. doi: 10.22467/jwmr.2019.00780. [DOI] [Google Scholar]
- 39.Rupert P, Ochoa RA, Punch L, Van Epps J, Gordon-Burroughs S, Martinez S. The use of NPWT-i technology in complex surgical wounds. Cureus. 2016;8(12):e920. doi: 10.7759/cureus.920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jukema GN, Timmers MS, Simmen H-P, Pape H-C. Posttraumatic osteomyelitis: Improvement in outcome by negative pressure wound therapy with instillation technique. Praxis. 2018;107(19):1015–1020. doi: 10.1024/1661-8157/a003055. [DOI] [PubMed] [Google Scholar]
- 41.Dalla PL. Diabetic foot wounds: The value of negative pressure wound therapy with instillation. International Wound Journal. 2013;10(s1):25–31. doi: 10.1111/iwj.12174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Enodien B, Hendie D, Pozza G, Lyzikov A, Taha-Mehlitz S, Taha A. Advantages of negative pressure wound therapy with instillation of super oxidized solution and dwell time in diabetic foot syndrome: a rare case report. Journal of Surgical Case Reports. 2021;2021(5):rjab167. doi: 10.1093/jscr/rjab167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arowojolu OA, Wirth GA. Sacral and ischial pressure ulcer management with negative-pressure wound therapy with instillation and dwell. Plastic and Reconstructive Surgery. 2021;147(1S-1):61S–67S. doi: 10.1097/PRS.0000000000007613. [DOI] [PubMed] [Google Scholar]
- 44.Broder KW, Nguyen B, Bodor RM, Broder KW, Nguyen B, Bodor RM. Negative pressure wound therapy with instillation in a chronic non-healing right hip trochanteric pressure ulcer. Cureus. 2016 doi: 10.7759/cureus.877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Diehm YF, Loew J, Will PA, Fischer S, Hundeshagen G, Ziegler B, et al. Negative pressure wound therapy with instillation and dwell time (NPWTi-d) with V. A. C. VeraFlo in traumatic, surgical, and chronic wounds-A helpful tool for decontamination and to prepare successful reconstruction. International Wound Journal. 2020;17(6):1740–1749. doi: 10.1111/iwj.13462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shimbo K, Saiki T, Kawamoto H, Koshima I. Implant salvage in patients with severe post-fracture fixation surgical site infection using negative pressure wound therapy with intramedullary and subcutaneous antibiotic perfusion. Wounds: A Compendium of Clinical Research and Practice. 2022;34(6):E47–E51. doi: 10.25270/wnds/21098. [DOI] [PubMed] [Google Scholar]
- 47.Fernández LG, Matthews MR, Ellman C, Jackson P, Villarreal DH, Norwood S. Use of reticulated open cell foam dressings with through holes during negative pressure wound therapy with instillation and dwell time: A large case study. Wounds: A Compendium of Clinical Research and Practice. 2020;32(10):279–282. [PubMed] [Google Scholar]
- 48.Kushwaha A, Goswami L, Kim BS. Nanomaterial-based therapy for wound healing. Nanomaterials (Basel, Switzerland) 2022;12(4):618. doi: 10.3390/nano12040618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Uchida DT, Bruschi ML. 3D Printing as a technological strategy for the personalized treatment of wound healing. An Official Journal of the American Association of Pharmaceutical Scientists. 2023;24(1):41. doi: 10.1208/s12249-023-02503-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data available.