Abstract
Tick-borne encephalitis (TBE) represents a potential health threat for tourists in high-risk areas, including the Dolomite Mountains in northeastern Italy. The present questionnaire-based survey was, therefore, designed in order to assess knowledge, attitudes, and preventive practices (KAP) in a convenience sample of Italian tourists visiting the Dolomite Mountains, who were recruited through online discussion groups. A total of 942 participants (39.2% males, with 60.2% aged under 50) filled in the anonymous survey from 28 March 2023 to 20 June 2023. Overall, 24.1% of participants were vaccinated against TBE; 13.8% claimed to have previously had tick bites, but no cases of TBE were reported. The general understanding of TBE was relatively low; while 79.9% of participants acknowledged TBE as a potentially severe disease, its occurrence was acknowledged as high/rather high or very high in the Dolomites area by only 51.6% of respondents. Factors associated with the TBE vaccine were assessed by the calculation of adjusted odds ratios (aOR) and 95% confidence intervals through a logistic regression analysis model. Living in areas considered at high risk for TBE (aOR 3.010, 95%CI 2.062–4.394), better knowledge on tick-borne disorders (aOR 1.515, 95%CI 1.071–2.142), high risk perception regarding tick-borne infections (aOR 2.566, 95%CI 1.806–3.646), a favorable attitude toward vaccinations (aOR 3.824, 95%CI 1.774–8.224), and a tick bite(s) in a previous season (aOR 5.479, 95%CI 3.582–8.382) were characterized as being positively associated with TBE vaccination uptake. Conversely, being <50 years old (aOR 0.646, 95%CI, 0.458–0.913) and with a higher risk perception regarding the TBE vaccine (aOR 0.541, 95%CI 0.379–0.772) were identified as the main barriers to vaccination. In summary, tourists to the high-risk area of the Dolomites largely underestimate the potential occurrence of TBE. Even though the uptake of the TBE vaccine in this research was in line with European data, public health communication on TBE is required in order to improve acceptance of this effective preventive option.
Keywords: tick-borne diseases, vaccines, health knowledge, attitudes, practices, encephalitis, tick-borne encephalitis virus, travel medicine
1. Introduction
Tick-borne encephalitis (TBE) is an acute clinical syndrome caused by the TBE virus (TBEV) [1,2,3,4], an RNA virus belonging to the family of Flaviviridae, genus Flavivirus [1,5,6], which targets the central nervous system (CNS) [6,7,8,9]. TBEV is currently classified into five subtypes, but nearly all the cases reported from the European Union/European Economic Area (EU/EEA) are associated with the TBEV-European (Eu) subtype, transmitted by the hard tick Ixodes ricinus [1,6]. TBEV-Eu usually causes infections that follow a biphasic course [3,10]. In the first phase, which occurs in 1/3 of cases after an incubation of around 7 days [1,11,12], viraemia is characterized by non-specific, influenza-like symptoms (e.g., fever, fatigue, headache, myalgia, and nausea), usually lasting from 2 to 10 days. In the second phase, which develops in 20 to 30% of cases after an interval lasting from 1 to 33 days, the pathogen enters the CNS and causes severe complications such as meningitis, meningoencephalitis, and myelitis, and even death [1,13,14]. The case-fatality ratio (CFR) for TBEV-Eu infections has been estimated at 0.9% [15], rarely exceeding 1.5% [16], but around 50% of the total number of patients develop a postencephalitic syndrome characterized by cognitive and neurological features, such as paralysis of the cranial nerves and hearing loss [15,17,18].
According to the European Centre for Disease Prevention and Control (ECDC), between 2015 and 2021, a total of 20,237 TBE diagnoses have been reported from EU/EEA member states [3,10]. Age-adjusted notification rates have increased from 0.39 to 0.88 cases per 100,000 people, and the underlying causes have been tentatively identified in relation to climate change (which increases the distribution of Ixodes and competent TBEV hosts) and behavioral factors [19,20]. Inappropriate levels of awareness of TBE among population groups at higher risk for tick bites would in turn impair their use of preventive options [21,22], ranging from behavioral strategies (e.g., avoiding off-trail activities, using appropriate personal protective equipment [PPE], etc.), to the uptake of TBE vaccines [13,17,23,24]. In fact, two TBE vaccines (effective in 96% to 99% of cases) are commercially available in Western Europe, i.e., FSME-IMMUN® (Pfizer SRL, Latina, Italy; which is the only vaccine licensed in Italy) and ENCEPUR® (Bavarian Nordic, Hellerup, Danemark) [16], and both immunizations can be used in adults and children ≥ 1 year old who live in high-risk TBE areas or who frequently visit forests and grasslands in high-risk areas [16,24].
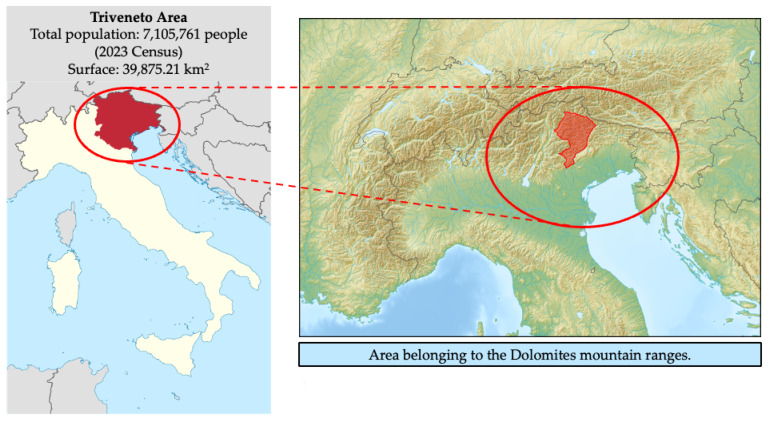
With an age-adjusted notification rate not exceeding 0.1 cases per 100,000 head of population [3], Italy is considered at low risk for TBE [16,25,26,27]. However, 94.1% of 203 Italian TBE cases reported from 2017 to 2023 were clustered within the subalpine autonomous provinces of Trento and Bolzano, and the northeastern regions of Veneto and Friuli-Venezia-Giulia (collectively known as the “Triveneto”) [22,25] (Figure A1 in Appendix A). The corresponding pooled notification rate for Triveneto has been estimated at 0.35 cases per 100,000 head of population (95% confidence interval [95%CI] 0.28–0.42) for the timeframe 2017–2020 [3,28,29,30]. Available estimates are, therefore, substantially lower than those from the nearby countries of Austria (range 2017–2021: 1.15–2.74 per 100,000) and Slovenia (range 2017–2021: 2.38–8.75 per 100,000), but some foci within the Triveneto have been characterized by notification rates exceeding 5 cases per 100,000 persons per year [21,25], which is the cut-off suggested by the World Health Organization (WHO) for high-risk areas where the TBE vaccine should be actively offered as a preventive option [16,18,27]. Some high-risk areas have been identified within the Dolomite Mountains [25], a popular holiday destination [21]. The Dolomites are characterized by large forests that provide an appropriate habitat for both Ixodes vector and suitable TBEV hosts (i.e., migratory birds and ungulates) [31], while the high number of mountain tourists and workers involved in outdoor activities (e.g., hunting, fishing, camping, collecting mushrooms and berries, forestry, farming, and even military training) increases the opportunities for human infections [21,22], in particular from April to November [21], when the ticks’ activity reaches its seasonal peak [13,18,23,24,32]. As very little is known about the awareness of TBE among tourists to the Dolomites area [31], the present study was designed in order to ascertain the following endpoints: (1) tourists’ awareness of the TBE and tick-borne infections; (2) their level of self-perceived risk for TBEV infection; (3) acceptance of the TBE vaccine.
Our results can, therefore, lead to the appropriate identification of key topics for the proper design of tailored prevention and control programs, not only from a travel medicine point of view but also for the general population.
2. Materials and Methods
2.1. Study Design and Sample Size
The present study was designed as a cross-sectional questionnaire-based survey (see the STROBE Checklist in Table S1 in the Supplementary), with a targeted convenience sample of around 1000 respondents. The minimum sample size (N) was calculated by assuming the annual incidence of tick bites to be 30.2% (a figure that we identified in a previous survey [22]), a Type I error of 5% (0.05), and a power of 95%:
| N = 1.962 × 0.302 × (1 − 0.32)/0.052 = 3.8416 × 0.302 × 0.698/0.0025 = 324 | (1) |
The questionnaire was delivered between 28 March 2023 and 20 June 2023 across 45 Facebook groups discussing tourism in the Dolomites. After the removal of shared subscriptions, a total of 20,444 unique members were potentially reached. Before posting the study invitation, the chief researcher (M.R.) contacted the responsible administrators and asked for their authorization to share an invitation link to the questionnaire. The link, in turn, led the potential participants to the informed consent form (Table S2) detailing the aims of the study and reassuring all participants about the anonymous design of the questionnaire, guaranteeing the confidentiality of all retrieved information and that all data would only be stored for the time needed for collective analyses. Only individuals who formally agreed to participate by answering a specifically designed dichotomous item could access the first page of the web survey (Google Forms; Google LLC; Menlo Park, CA, USA). No monetary or other compensation was offered to the participants.
2.2. Inclusion Criteria
The inclusion criteria were:
-
(1)
being aged 18 years or older;
-
(2)
having any previous knowledge of TBE;
-
(3)
having traveled to the Dolomite Mountains as a tourist in the 5 years before the inception of the questionnaire.
All the aforementioned criteria were assessed by three dichotomous (yes vs. no) questions, and only participants fulfilling the three criteria were able to access the subsequent sections of the questionnaire.
2.3. Instruments
The questionnaire was originally developed for a similar intervention among agricultural workers from the Autonomous Province of Trento and has been described elsewhere [21,22]. Regarding its content, retrieved personal data were deliberately restricted to general information that did not allow for the identification of the respondent. Moreover, an IP address, email address, or personal information unnecessary to the survey was neither requested nor retrieved. The questionnaire included the following areas of inquiry (Table S3).
2.3.1. Demographic Characteristics of the Participants
Data were gathered regarding age (by decennial groups); gender; any occupational background in healthcare settings and agricultural settings; the Italian Region where the respondents mainly worked and lived; their highest educational achievement; and having or not having any pet in their household.
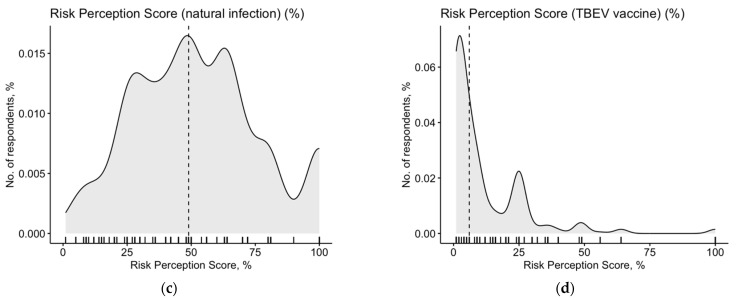
2.3.2. Knowledge Test
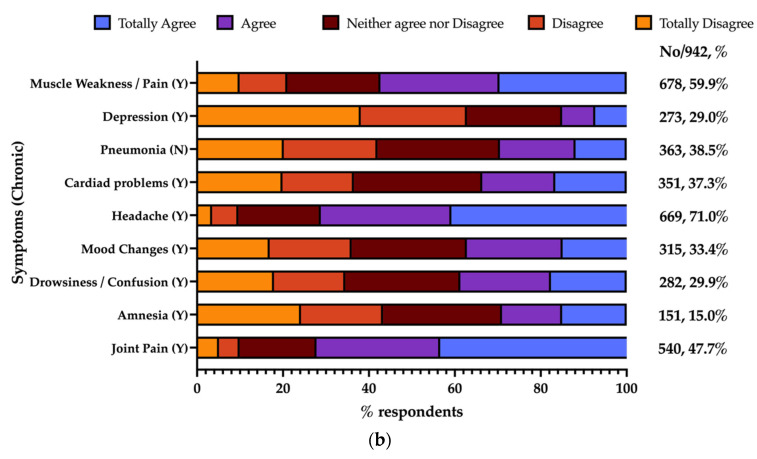
According to the original design of Zingg and Siegrist [33], participants received a previously validated knowledge test, containing a total of 12 true–false statements on TBE and tick-borne diseases, the design of which has been described elsewhere [21]. Each correctly answered question added +1 to a sum score (general knowledge score, GKS) while each wrong, missing, or “don’t know” answer added 0 to the sum score (potential range: 0 to 12). Participants were then asked to rate, through a 5-point Likert scale (from 1, “totally disagree”, to 5, “totally agree”), a series of acute (n = 10) and chronic (n = 9) signs and symptoms possibly related to previous tick bites. Answers were then dichotomized as somewhat agree (score 4 and 5) vs. somewhat disagree (score 1 to 3), and a sum score (symptom knowledge score, SKS; potential range, 0 to 19) was then calculated similarly to the GKS; when the participant agreed on a sign/symptom that was actually associated with TBE, +1 was added to the sum score, while all other answers added 0 to the sum score.
2.3.3. Risk Perception
According to the health belief model (HBM) [34,35], risk perception is a key effector of risk behavior [34]. It can be defined as the function of the perceived probability of an event and its expected consequences and has been assessed as the mathematical product of the perceived probability and severity of a certain outcome [35,36]. We, therefore, questioned the participants about the perceived probability of contracting a TBEV infection (Einf), the perceived probability of developing complications after delivery of the TBE vaccine (Evac), the perceived severity of natural infection from TBEV (Cinf), and the perceived severity of vaccine side effects (Cvac). Respondents rated the aforementioned items through a fully labeled 5-point scale (1: “almost zero”, 2: “low or rather low”, 3: “moderate”, 4: “high or rather high”, 5: “very high”), and two distinctive risk perception scores (RPS, potential range 1 to 25) for TBEV natural infection (RPSinf) and for TBEV vaccination (RPSvac) were calculated as follows:
| RPSinf = Einf × Cinf | (2) |
| RPSvac = Evac × Cvac | (3) |
2.3.4. Attitudes toward the TBE Vaccine
Attitudes have been defined as the learned tendency to evaluate a particular entity with some degree of favor or disfavor [37]. For the aims of this study, we specifically inquired as to the participants’ attitudes toward vaccines and immunizations, through a selected set of declarative sentences regarding the reasons to accept immunizations and, more specifically, TBE vaccination (i.e., “to avoid getting TBE”, “to avoid transmitting VPDs”, “to avoid complications of VPDs”, “to avoid VPDs in subjects who cannot be vaccinated”), or, rather, to refuse them (e.g., “to avoid shots/medications”, “uselessness”, “fear of side effects”, “religious/ethical reasons”, etc.). All items were presented as dichotomous options (yes vs. no). Even though TBEV exhibits no inter-human spreading, we deliberately included among the motivators to receive the TBE vaccine the statements “to avoid transmitting VPDs” and “to avoid VPDs in subjects who cannot be vaccinated”, in order to ascertain the degree of social desirability bias affecting the collected results.
2.3.5. Preventive Practices
Participants were initially questioned regarding their TBE immunization status. Participants having reported a tick bite in the previous holiday season were questioned about their follow-up (i.e., who removed the tick head; whether any antibiotic therapy was given; whether there was any laboratory follow-up; whether the participant was then diagnosed with TBEV infection, Lyme disease, or a skin infection associated with the tick bite). The preventive measures that they had put in place were then assessed using a 5-point Likert scale, ranging from never (score = 1) to always (score = 5), and the results were dichotomized as “often” to “always” vs. “never” to “sometimes”.
2.4. Ethical Considerations
In order to avoid any harm to or stigma on the participants, the anonymous design of the questionnaire was guaranteed by limiting the recall of personal information and avoiding any inquiry about clinical data regarding the potential participants. As the anonymous data were analyzed for statistical and research purposes, the present study did not configure itself as a clinical trial, but rather as an opinion-based questionnaire survey. To prevent stress, anxiety, and even panic potentially caused by an inappropriate understanding of an item included in the knowledge test, correct answers and detailed explanations were then provided after completion of the questionnaire. A preventive assessment by a competent Ethical Committee and Institutional Review Board was therefore not statutorily required (Italian Official Gazette no. 76, dated 31 March 2008; European Regulation 2016/679, point no. 26) (Supplementary Files S1 and S2) [38,39].
2.5. Data Analysis
Continuous variables were initially reported as mean ± standard deviation (SD), and their distribution was assessed through the D’Agostino-Pearson K2 test. Variables with a K2 test p-value of ≥ 0.100 were considered normally distributed and were compared using Student’s t-test for unpaired data or an ANOVA where appropriate, while their correlation was assessed by means of Pearson’s correlation coefficient. A K2 test p-value of <0.100 identified those variables not normally distributed, which were analyzed using a Mann–Whitney or Kruskal–Wallis test, while their correlation was analyzed by means of Spearman’s rank test.
Categorical variables were initially reported as percentage values. Cumulative scores (RPSinf, RPSvac, GKS, SKS) were initially normalized to a percentage value and then dichotomized by the median value as “high” vs. “low” estimates, these being managed as categorical variables. The distribution of the categorical variables was assessed through the chi-squared test with respect to the dichotomous outcome variable of having been or not been vaccinated against TBE. All variables that, in univariate analysis, were associated with an outcome variable with a p-value of < 0.05 were included in stepwise binary logistic regression analysis, along with the calculation of the corresponding adjusted odds ratio (aOR) and their 95% confidence intervals (95%CI).
The statistical analyses were performed using IBM SPSS Statistics 26.0 for Macintosh (IBM Corp. Armonk, NY, USA), R (version 4.3.1) [40], and Rstudio (version 2023.06.0 Build 421; Rstudio, PBC; Boston, MA, USA) software, by means of the packages epiR (version 2.0.62) and fmsb (version 0.7.5).
3. Results
3.1. Demographic Characteristics of the Participants
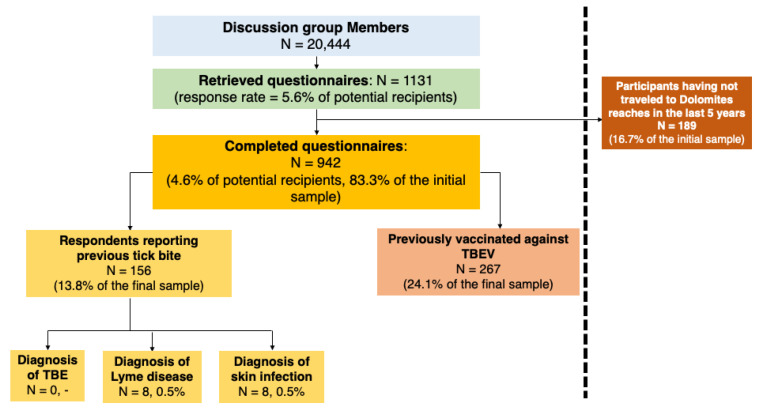
As shown in Figure 1, a total of 942 respondents fulfilled all the inclusion criteria (4.6% of potential recipients and 83.3% of the initial sample).
Figure 1.
Flow chart for the participants included in the final sample.
As shown in Table 1, 30.9% of participants had any occupational background in healthcare settings, while any background in agricultural settings was reported by 1.6% of participants. Around 69.1% of participants reported an educational achievement at university level, with 28.3% reporting up to 13 years of formal education. A pet within the household was reported by 43.9% of participants.
Table 1.
Characteristics of 942 tourists to the Dolomites area who participated in this survey (Italy, 2023).
| Variables | N/942, % |
|---|---|
| Age (years) | |
| <20 | 3, 0.3% |
| 20–29 | 57, 6.1% |
| 30–39 | 273, 29.0% |
| 40–49 | 234, 24.8% |
| 50–59 | 195, 20.7% |
| 60–69 | 141, 15.0% |
| ≥70 | 39, 4.1% |
| Male gender | 369, 39.2% |
| Region of Origin | |
| High-risk Areas for TBEV 1 | 561, 59.6% |
| Northern Italy 2 | 351, 37.3% |
| Central Italy 3 | 15, 1.6% |
| Southern Italy 4 | 12, 1.3% |
| Major Island 5 | 3, 0.3% |
| Any occupational background in healthcare settings | 291, 30.9% |
| Any occupational background in agricultural settings | 15, 1.6% |
| Educational achievement | |
| University (≥14 years of formal education) | 651, 69.1% |
| High school (9–13 years of formal education) | 267, 28.3% |
| Primary/Secondary school (≤8 years of formal education) | 24, 2.5% |
| Any pet in the household | 414, 43.9% |
| GKS > median value (58.33%) | 396, 42.0%% |
| Symptom score > median value (57.89%) | 441, 46.8% |
| RPS for tick-borne infections > median value (49.00%) | 465, 49.4% |
| RPS for TBE vaccine > median value (6.00%) | 405, 43.0% |
| Tick bite in the previous season | 156, 16.6% |
| Attitudes Toward Vaccines | |
| In general, somehow favorable | 840, 74.3% |
| Previously vaccinated against TBEV | 267, 28.3% |
| TBEV was recommended by any healthcare professional | 291, 30.9% |
| General Practitioner | 57, 6.1% |
| Medical Officer from Vaccination Services of the Local Health Unit | 102, 10.8% |
| Emergency Department | 9, 1.0% |
| Occupational physician | 9, 1.0% |
| Other non-medical HCWs | 114, 12.1% |
Note: TBEV = tick-borne encephalitis virus; HCWs = healthcare workers; GKS = general knowledge score; RPS = risk perception score; 1 = Autonomous Province of Trento, Province of Belluno, and Province of Gorizia; 2 = Piedmont, Liguria, Lombardy, Emilia-Romagna, Autonomous Province of Bolzano, Veneto (excluding the province of Belluno), and Friuli-Venezia-Giulia (excluding the province of Gorizia); 3 = Tuscany, Umbria, Marche, and Latium; 4 = Campania, Abruzzo, Basilicata, Molise, Apulia, and Calabria; 5 = Sicily and Sardinia.
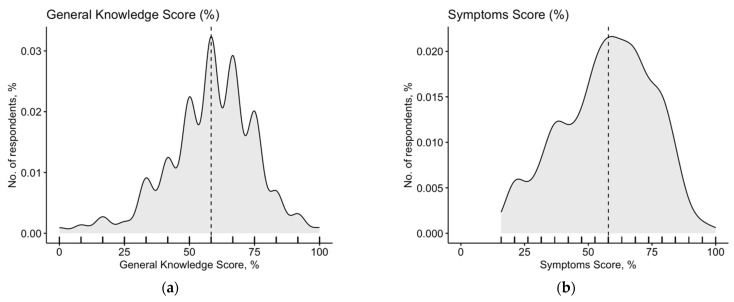
3.2. Knowledge Test
As shown in Table 2, a summary GKS of 58.17% ± 16.93 was calculated, with a median value of 58.33%. The corresponding SKS was estimated at 57.67% ± 17.70 (median value 57.89%). Both estimates were substantially skewed, as confirmed by the K2 test (K2 = 63.71, and 37.55, respectively; p < 0.001 for both summary scores) (Appendix A, Figure A2 and Figure A3). Cronbach’s alpha was estimated to be 0.824 for the knowledge test, which suggested good internal consistency (Appendix A, Table A1).
Table 2.
Summary of general knowledge score, symptom knowledge score, and risk perception score per tick-borne infection and for the tick-borne encephalitis virus (TBEV) vaccine.
| Cumulative Score | Average ± SD | Median (Range; Min–Max) |
K2 (p-Value) |
|---|---|---|---|
| General Knowledge Score | 58.17 ± 16.93 | 58.33 (1.00; 100) | K2 = 63.71, p < 0.001 |
| Symptom Knowledge Score | 57.67 ± 17.70 | 57.89 (15.79; 100) | K2 = 37.55, p < 0.001 |
| Risk Perception Score, Tick-borne Infections | 52.20 ± 24.28 | 49.00 (1.00; 100) | K2 = 30.11, p < 0.001 |
| Risk Perception Score, TBE Vaccine | 11.63 ± 15.42 | 6.00 (1.00; 100) | K2 = 569.1, p < 0.001 |
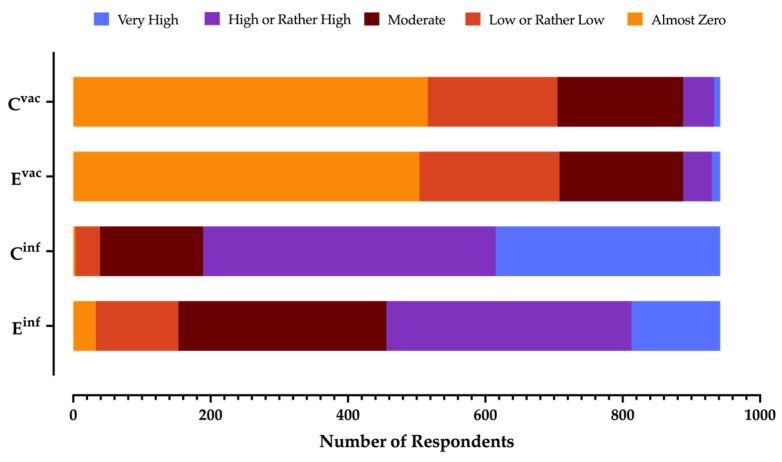
3.3. Risk Perception
The frequency of TBEV infection was perceived as high/very high by 51.6% of respondents, while the severity of the clinical syndrome was acknowledged as high/very high by 79.9% of respondents, with a corresponding RPSinf estimate of 52.20% ± 24.28. Conversely, only 5.7% of respondents acknowledged as being somewhat high both the frequency and severity of the side effects associated with the TBE vaccine (Figure 2 and Appendix A, Table A2), with a corresponding RPSvac of 11.63% ± 15.42 (Table 2 and Appendix A, Figure A2b,c). In both cases, normal distribution was eventually rejected (K2 test: p < 0.001).
Figure 2.
Summary of the perceived probability of contracting a TBEV infection (Einf); perceived probability of developing complications after the delivery of the TBE vaccine (Evac); perceived severity of natural infection from TBEV (Cinf); perceived severity of the vaccine side effects (Cvac), as reported by 942 participants (Italy, 2023).
3.4. Attitudes toward the TBE Vaccine
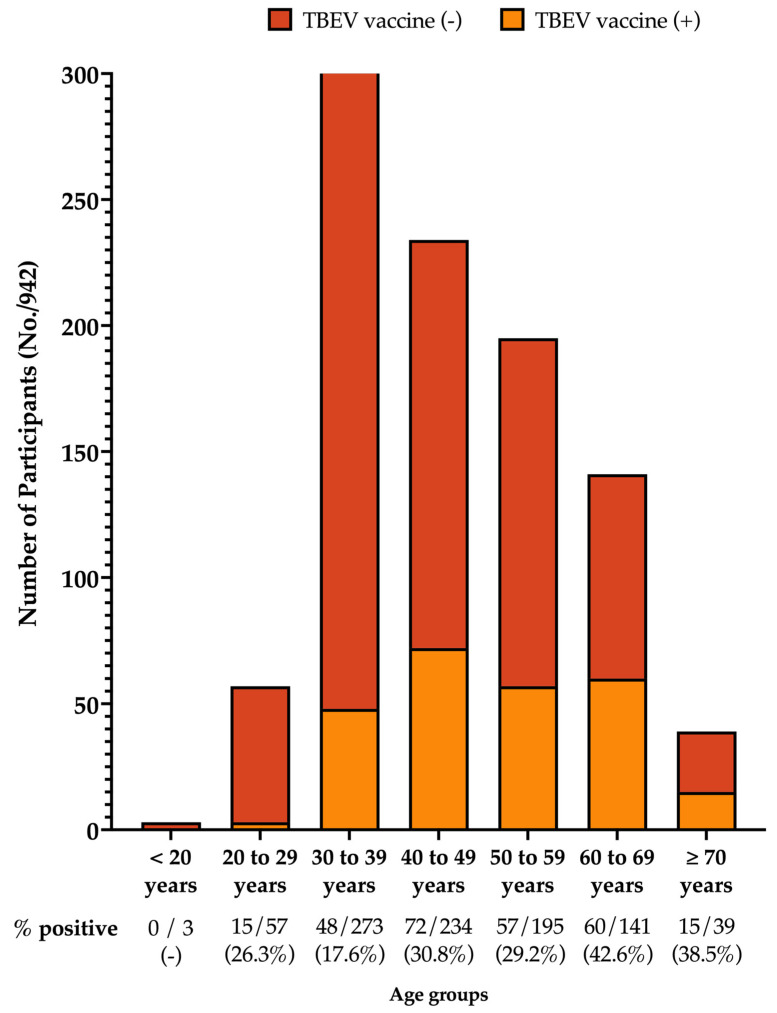
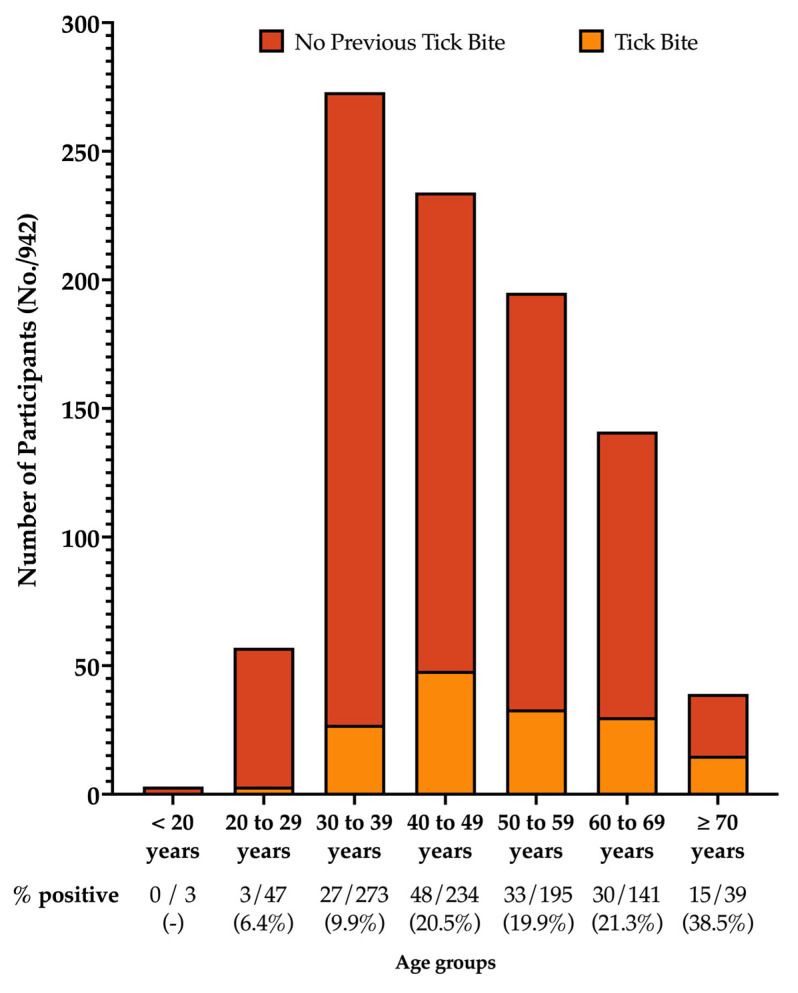
The large majority of respondents were somewhat in favor of vaccination practice (74.3%), and a total of 267 participants (28.3%) had reportedly been vaccinated against TBEV (216 out of 561 residents from a high-risk area; 38.5%). As shown in Figure 3, the peak level of vaccination coverage was reported in the age group of 60–69 years (42.6%), followed by ≥70-year-olds (38.5%), then by the age groups of 40–49 years (30.8%), 50–59 years (29.2%), 20–29 years (26.3%), and 30–39 years (17.6%). No previous TBE vaccinations were reported among those subjects under 20 years old.
Figure 3.
Vaccination rates for TBE according to age group, as reported by 942 participants (Italy, 2023).
A fairly large proportion of respondents (30.9%) had been recommended TBE vaccination by healthcare professionals, including personnel from the competent Local Health Unit (10.8%) and other medical professionals (i.e., their general practitioner, 6.1%; personnel from the emergency department, 1.0%; their occupational physician, 1.0%).
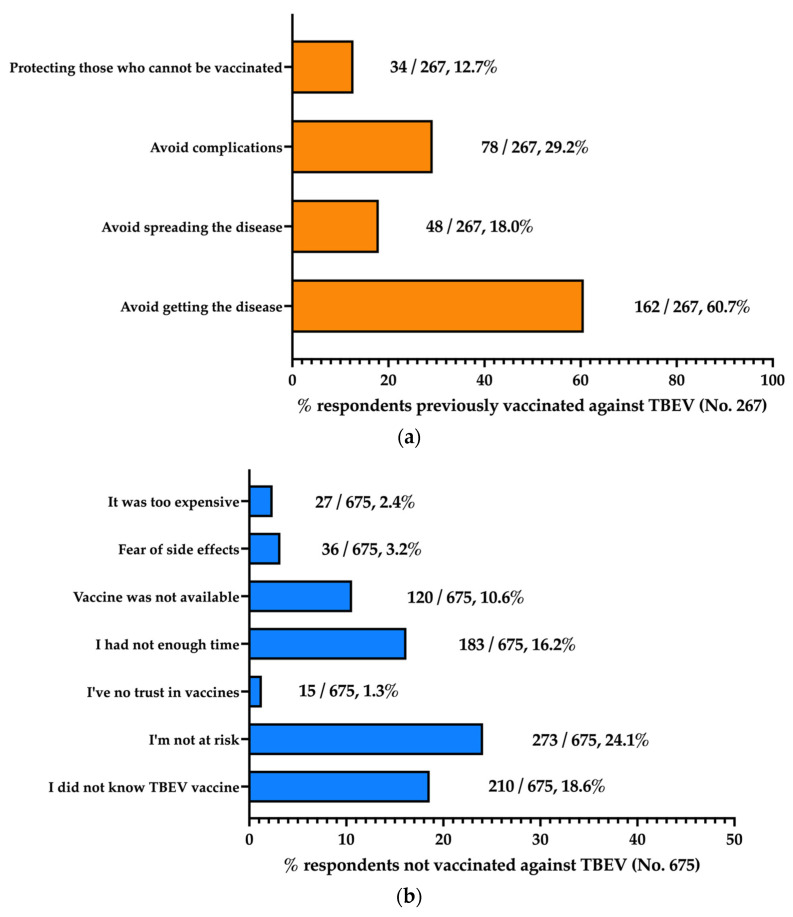
Personal reasons for being or not being vaccinated against TBEV are reported in Figure 4a and Figure 4b, respectively. The most frequently reported reason for being vaccinated was identified as “avoid getting the disease” (60.7%), followed by “avoid complications” (29.2%). Conversely, “avoid spreading the disease” and “protecting those who cannot be vaccinated” were reported by 18.0% and 12.7% of participants, respectively.
Figure 4.
Reasons for receiving (a) and not receiving (b) the TBEV vaccination protocol, as reported by 942 participants (Italy, 2023).
When dealing with perceived barriers, 18.6% of non-vaccinated individuals (N = 675) did not know that an effective vaccine against TBE exists. Nonetheless, the most frequently reported reason for avoiding or delaying TBE vaccination was identified as not perceiving the individual risk of getting TBEV infection (24.1%), followed by not having had enough time (16.2%), the unavailability of the TBE vaccine from vaccination services (10.6%), while the fear of side effects and the lack of trust in vaccines were reported by only 3.2% and 1.3% of participants, respectively. Interestingly, only 2.4% of the non-vaccinated respondents complained about the high cost of TBE vaccination.
3.5. Practices
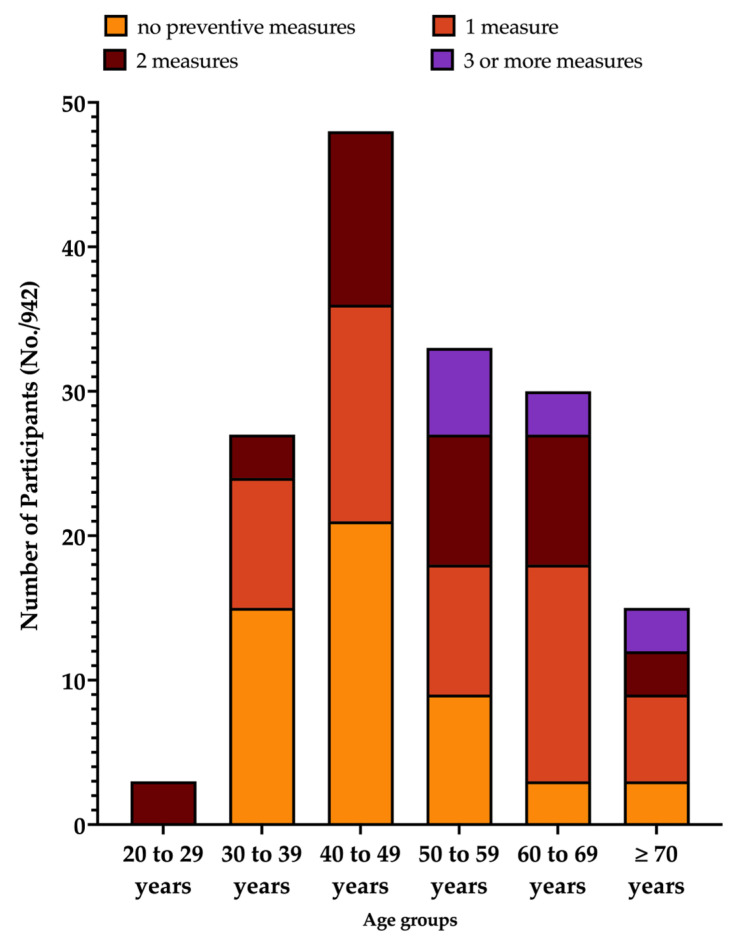
As shown in Table 3, 156 participants reported experiencing a tick bite during 2022 (16.6%), and the tick head was mostly removed by the participant himself/herself (71.2%) or by friends and relatives (21.1%). Only 7.7% of bitten participants were assisted by any HCW. The peak for tick bites occurred in individuals aged 70 years or more (38.5%), followed by the age groups of 60–69 years (21.3%), 40–49 years (20.5%), and 50–59 years (19.9%). Previous tick bites were reported by 9.9% of participants aged 30–39 years and by 6.4% of individuals aged 20–29 years, with no event occurring among individuals who were <20 years old (Appendix A, Figure A4). Antibiotic treatment was reported by 11.5% of participants, while a laboratory follow-up was performed for 19.2% of them. Interestingly, no case of TBE was identified, while 5.1% of participants reported an eventual diagnosis of Lyme disease, and a similar share of respondents was affected by any skin infection on the site of the tick bite.
Table 3.
Characteristics of the tick bites, as reported by 156 participants.
| Variable | N/156, % |
|---|---|
| Tick Removed by: | |
| Any HCW | 12, 7.7% |
| Friends/Relatives | 33, 21.1% |
| Him-/Herself | 111, 71.2% |
| Antibiotic treatment | 18, 11.5% |
| Laboratory follow-up | 30, 19.2% |
| Diagnosis of Lyme disease | 8, 5.1% |
| Diagnosis of TBEV infection | 0, - |
| Diagnosis of skin infection on tick bite | 8, 5.1% |
| Preventive Measures (Often/Always) | |
| Use of Repellent | 39, 25.0% |
| Wear light-colored clothing | 12, 7.7% |
| Wear long sleeves and pants | 21, 13.5% |
| Tuck pants into socks or boots | 66, 42.3% |
| Perform body check | 0, - |
| Wear a hat | 18, 11.5% |
| Avoid typical tick habitats | 18, 11.5% |
| Any | 105, 67.3% |
| 1 preventive measure | 54, 34.6% |
| 2 preventive measures | 39, 25.0% |
| 3 preventive measures or more | 12, 7.7% |
Notes: HCW = healthcare worker; TBE = tick-borne encephalitis; TBEV = TBE virus.
Overall, 67.3% of participants reported taking at least one preventive measure against tick bites, while 25.0% reported taking up to 2 preventive measures, and 7.7% of participants reported taking 3 or more preventive measures. The single most frequently reported intervention was tucking pants into socks or boots (42.3%), followed by the use of repellent (25.0%), wearing long sleeves and pants (13.5%), wearing a hat (11.5%), avoiding typical tick habitats (11.5%), and wearing light-colored clothing (7.7%). Interestingly, checking the body was never reported. Focusing on participants not reporting any preventive measure against tick bites, their proportion decreased from 55.56% in the 30–39 age group, to 43.75% in the 40–49 age group, 27.27% in the 50–59 age group, and 10.00% in the 60–69 age group, but the proportion was 20.00% in ≥70-year-old respondents (Appendix A, Figure A5).
3.6. Univariate Analysis
GKS and SKS were positively correlated (rho = 0.334, p < 0.001). Conversely, a negative correlation was found between RPSvac and RPSinf (rho = −0.078, p = 0.017). Moreover, both GKS and SKS were positively correlated with RPSinf (rho = 0.084, p = 0.009, and rho = 0.262, p < 0.001) and were negatively correlated with RPSvac (rho = −0.281, p < 0.001, and rho = −0.123, p < 0.001) (Appendix A, Table A3). In other words, a better performance in the general knowledge test was associated with a better understanding of the potential symptoms of TBE, and a better knowledge status was associated with a higher perception of the risk associated with TBEV and fewer concerns regarding the TBE vaccine.
Estimates for GKS (62.09% ± 13.19 vs. 56.38% ± 18.17; p < 0.001), SKS (59.63% ± 17.32 vs. 57.06% ± 17.85; p = 0.023), and RPSinf (62.88% ± 26.41 vs. 47.95% ± 22.13; p < 0.001) were significantly higher among those participants who had previously been vaccinated against TBEV than among those who had not. Conversely, RPSvac scores were higher among participants not reporting the previous uptake of the TBE vaccine than among vaccinated participants (6.79% ± 10.45 vs. 47.95% ± 22.13, p < 0.001).
The association between the descriptive variables and TBE vaccination status is detailed in Table 4. Briefly, previous TBE vaccination was more frequently reported among individuals from high-risk areas (80.9% vs. 50.7%, p < 0.001), scoring better GKS (50.6% vs. 36.9% among non-vaccinated individuals, p < 0.001) and SKS (55.1% vs. 42.7%, p = 0.002), reporting a higher risk perception for natural TBEV infection (68.5% vs. 47.1%, p < 0.001), exhibiting a better attitude toward vaccines (in general; 96.6% vs. 83.6%, p < 0.001), and reporting a tick bite in the previous holiday season (33.7% vs. 9.3%, p < 0.001). Conversely, TBE vaccination was less frequently reported among individuals aged under 50 (50.6% vs. 61.3%, p < 0.001) and in those having higher RPSvac scores (25.8% vs. 47.1%, p < 0.001).
Table 4.
Univariate analysis of the individual factors associated with previous vaccination against tick-borne encephalitis virus (TBEV). Comparisons were performed by means of the chi-squared test for categorical values and the Mann–Whitney U test for continuous variables.
| All Respondents | Previously Vaccinated Against TBEV | ||
|---|---|---|---|
| Yes (N/267, %) | No (N/675, %) |
p-Value | |
| General Knowledge Score (%, average ± SD) | 62.09 ± 13.19 | 56.38 ± 18.17 | <0.001 |
| Symptoms Score (%, average ± SD) | 59.63 ± 17.32 | 57.06 ± 17.85 | 0.023 |
| Risk Perception Score, Tick-Borne infection (%, average ± SD) | 62.88 ± 26.41 | 47.95 ± 22.13 | <0.001 |
| Risk Perception Score, TBE vaccine (%, average ± SD) | 6.79 ± 10.45 | 47.95 ± 22.13 | <0.001 |
| Age < 50 years | 135, 50.6% | 414, 61.3% | <0.001 |
| Male gender | 105, 39.3% | 255, 37.8% | 0.925 |
| Resident in high-risk areas | 216, 80.9% | 342, 50.7% | <0.001 |
| Any occupational background in healthcare settings | 93, 34.8% | 198, 29.3% | 0.177 |
| Any occupational background in agricultural settings | 6, 2.2% | 6, 0.9% | 0.106 |
| High educational achievement | 174, 65.2% | 459, 68.0% | 0.136 |
| Any pet in the household | 126, 47.2% | 285, 42.2% | 0.345 |
| Higher general knowledge score | 135, 50.6% | 249, 36.9% | <0.001 |
| Higher knowledge of symptoms score | 147, 55.1% | 288, 42.7% | 0.002 |
| High risk perception regarding tick-borne infections | 183, 68.5% | 273, 40.4% | <0.001 |
| High risk perception regarding TBE vaccine | 69, 25.8% | 318, 47.1% | <0.001 |
| Attitude toward vaccines (favorable) | 258, 96.6% | 564, 83.6% | <0.001 |
| Tick bite in the previous season | 90, 33.7% | 63, 9.3% | <0.001 |
Note: high-risk areas = Autonomous Province of Trento, the Province of Belluno, and the Province of Gorizia; SD = standard deviation.
3.7. Multivariable Analysis
The results of the multivariable analysis are reported in Table 5. The model included an age of <50 years, living in high-risk areas, high GKS, SKS, RPSvac, and RPSinf scores, reporting a favorable attitude toward vaccination, and reporting any tick bite during 2022.
Table 5.
Multivariable analysis of the factors associated with previous vaccination against tick-borne encephalitis virus (TBEV). Multi-adjusted odds ratios (aOR) and their corresponding 95% confidence intervals (95%CI) were calculated by means of two distinct binary logistic regression models, which included all factors that were associated in the univariate analysis with an outcome variable (p < 0.05).
| All Respondents | Previously Vaccinated Against TBEV | |
|---|---|---|
| aOR | 95% Confidence Interval | |
| Age < 50 years | 0.646 | 0.458; 0.913 |
| Living in high-risk areas | 3.010 | 2.062; 4.394 |
| Higher general knowledge score | 1.515 | 1.071; 2.142 |
| Higher knowledge of symptoms score | 1.009 | 0.714; 1.427 |
| High risk perception regarding tick-borne infections | 2.566 | 1.806; 3.646 |
| High risk perception regarding TBE vaccine | 0.541 | 0.379; 0.772 |
| Attitude toward vaccines (favorable) | 3.824 | 1.774; 8.244 |
| Tick bite in the previous season | 5.479 | 3.582; 8.382 |
Note: high-risk areas = Autonomous Province of Trento, the Province of Belluno, and the Province of Gorizia.
In fact, being resident in high-risk areas (aOR 3.010, 95%CI 2.062 to 4.394), higher GKS (aOR 1.515, 95%CI 1.71 to 2.142) or RPSinf (aOR 2.566, 95%CI 1.806 to 3.646) scores, reporting a better attitude toward vaccines (aOR 3.824, 95%CI 1.774 to 8.244), and reporting a tick bite during 2022 (aOR 5.479, 95%CI 3.582 to 8.382) were all collectively characterized as positive predictive variables. Conversely, being under 50 (aOR 0.646, 95%CI 0.458 to 0.913) and having higher RPSvac scores (aOR 0.541, 95%CI 0.379 to 0.772) were characterized as negative predictive variables.
4. Discussion
4.1. Key Results
In this cross-sectional study concerning tourists’ knowledge, attitudes, and practices (KAP) regarding TBE and TBE vaccination, a total of 942 questionnaires were ultimately collected. The self-reported TBE vaccination rate was 28.3% (38.5% in people living in high-risk areas). No cases of TBE were reported, but 5.1% of respondents with a previous tick bite did allegedly receive a diagnosis of Lyme disease. TBE was acknowledged as a serious disorder by 79.9% of participants, while the likelihood of its occurrence was considered high/very high by 51.6% of them. Overall knowledge status was substantially unsatisfactory, although the inclusion criteria may reasonably have led to the oversampling of individuals with a better understanding of TBE [16,30]. Individual factors positively associated with the uptake of the TBE vaccine were identified: being resident in high-risk areas; higher GKS and RPSinf scores; reporting a favorable attitude toward vaccines; and reporting a tick bite in the previous holiday season. Conversely, belonging to younger age groups and higher RPSvac scores were identified as negative explanatory variables. The occurrence of tick bites (16.6% of participants) and preventive interventions allegedly being put in place were heterogeneously distributed across the age groups, with a large share of participants reporting a low proportion of protective strategies, particularly among younger individuals (Table 3 and Appendix A, Figure A4). As the younger age groups also reported low rates of tick bites, some explanations can be tentatively proposed. First, younger people often practice a different kind of tourism [41] involving lower interaction with tick-populated environments, because of the seasonality or environmental features (e.g., altitude), or sports activities different from hiking (downhill racing, mountain biking, paragliding, etc.). Moreover, age is often associated with a different understanding of the risks associated with certain behaviors. Finally, we cannot rule out a certain recall bias, which, in turn, is associated with different tourism habits. Still, as shown in Appendix A, Table A4, younger age groups were characterized by a better knowledge status and no substantial differences in terms of RPSinf scores.
4.2. Interpretation
Although avoiding tick bites remains the most effective strategy for preventing the entirety of tick-borne diseases (e.g., Lyme disease, babesiosis, ehrlichiosis, Rocky Mountain spotted fever, anaplasmosis, or Crimean Congo hemorrhagic fever) [42,43,44], the efficacy of TBE vaccines has been well-documented [16,27,45,46]. Therefore, a rational public health approach for achieving the control of TBE in high-risk areas [16,18,27] cannot rule out interventions aimed at improving vaccination rates [24,47]. To date, Italian vaccination rates for TBE remain largely unknown [16,22,27,30]; previous KAP studies on TBE vaccines mostly focused on occupational settings [21,22], this being hardly representative of the general population because of the high background qualifications and literacy of the targeted occupational sub-group [21,48] and the well-defined geographical area (i.e., the Autonomous Province of Trento) [21,22,30] (Appendix A, Table A5).
To the best of our knowledge, here, we report on the first Italian study regarding TBE vaccine acceptance in people who may potentially be exposed to tick bites, not only within the domain of travel medicine but also among the general population living in high-risk areas [49,50,51], and our results appear to be substantially in line with previous international reports [52,53]. For instance, a recent survey from 20 European countries provided a pooled vaccination rate of 22% (range: 7% in Romania to 81% in Austria) [18,24], while a cross-sectional study from 11 European countries (year: 2018; Czech Republic, Estonia, Finland, Germany, Hungary, Latvia, Lithuania, Poland, Slovakia, Slovenia, and Sweden) identified an average vaccination rate of 25% [24,28]. Even in our previous study on farm workers from the Autonomous Province of Trento, a similar uptake of the TBE vaccine was reported (24.5%) [21].
Interestingly, the reported barriers and positive effectors regarding TBE vaccination uptake were also consistent with the available reports [24,53], which collectively stress the role of vaccine hesitancy (delay in acceptance or the refusal of vaccines despite the availability of vaccination services) [54] among the causes for low vaccination rates. While the general lack of trust in vaccines is usually considered a marginal barrier to the TBE vaccine [28], its uptake is more often affected by inappropriate TBE risk perception [23,24,28,45,46,55], particularly when dealing with its perceived incidence. Consistently with our estimates, in a previous international study, TBE was acknowledged as a severe condition by 78% of the participants, but its potential occurrence was perceived as significant by only 58% of them [28]. Similarly, a survey on travelers and travel clinics in Canada, Germany, Sweden, and the UK reported a low or even very low risk awareness of TBE, which was highly dependent on the actual prevalence of TBE in the parent country [53]. Conversely, in line with the HBM, living in an area with high TBE incidence rates is usually correlated with better vaccination propensity and vaccination rates for TBE [24,28,46,53,56], as well as having been bitten by a tick or having had any previous personal interaction with TBE cases [34,35]. However, the designation of a certain area as being at risk for TBE is sometimes unknown to the general population [24]; therefore, TBE vaccination uptake is more often modeled by the perceived endemicity of TBE than by its actual occurrence [45]. As a consequence, interventions improving general awareness and increasing media attention to TBE can considerably increase vaccine acceptance [24], particularly among individuals reporting a high frequency of visits to forests or other areas with TBE risk [53], or those who spend their leisure time in high-risk areas [28,45]. Therefore, the unsatisfactory knowledge status of participants, and its correlation with risk perception, collectively stress the potential significance of informative campaigns aimed at filling knowledge gaps in the general population [52,53]. In this regard, counseling by medical professionals has been characterized as a strong predictor of eventual vaccination [28] and should be taken into account when designing specific interventions [57,58].
A notable feature of our study was the very low proportion of respondents identifying the cost of the vaccine as a limitation, as the direct and indirect costs of TBE vaccines usually represent a potential barrier to achieving high vaccination rates [21,22,30,55]. This was somehow unexpected since in Italy, even in high-risk areas, the status of TBE vaccine pricing is quite variable. Depending on local regional recommendations, the vaccine can be delivered after either full payment or co-payment by interested citizens, or may even be totally free of charge, affecting people’s adherence to vaccination strategies. Even the recent Italian National Vaccination Plan 2023–2025 has identified some recommendations for the delivery of the TBE vaccine in occupationally exposed individuals [59,60] by including people living and traveling abroad in regions characterized by high TBE prevalence according to the WHO case definition, but the charge for this offer is still inconsistent across the various Italian regions, potentially impairing high vaccination rates in tourists visiting high-risk areas [21,25,26].
4.3. Limitations and Generalizability
Our study is affected by several limitations. First, the cross-sectional design cannot support conclusions on the causal relationships between the assessed risk factors and the targeted outcomes [61]; potential explanatory variables retain their significance only if they existed before the delivery of vaccine(s) [62]. As TBE vaccine uptake clearly existed before the delivery of the questionnaire, the actual role of potential explanatory variables such as knowledge status and risk perception, these being strongly influenced by personal experiences and media coverage at the time of the survey, should be quite cautiously acknowledged [63].
Second, our sample was collected by convenience sampling, and we cannot rule out some degree of self-selection bias, a substantial shortcoming shared by web-based cross-sectional studies [64] that ultimately leads to the over-sampling of individuals characterized by a particular attitude to sharing personal information through the internet and social media, a condition that is often associated with better literacy and younger age, and sharing increased interest on a specific topic [65]. Not coincidentally, our study oversampled individuals from younger age groups (60.2% of participants were younger than 50 years old at the time of the survey), the majority of participants were from geographic areas characterized by a high incidence of TBEV infections, and nearly 70% of the respondents reported having a university-level degree. Moreover, around 1/3 of the participants had an occupational background in a healthcare setting, reasonably sharing a stronger will to contribute to healthcare-related research, and probably a better understanding of this topic [22]. Studies on TBE vaccine acceptance have often reported a worse uptake of the vaccine among younger people [24,28,46]; being younger than 50 years was identified as a negative predictor of eventual acceptance of the TBE vaccine (aOR 0.646, 95%CI 0.458–0.913). This result is highly consistent with a recent study on Polish residents from high-risk areas, where the acceptance of the TBE vaccine was lesser among respondents aged 40 years or younger than among older individuals (OR 0.40, 95%CI 0.21 to 0.76) [23]. Nonetheless, since our study deliberately focused on people with previous knowledge of TBE, their better understanding of the subject has possibly inflated both the knowledge and risk perception estimates and, most notably, the reported vaccination rates. All the aforementioned potential shortcomings have been shared by other KAP surveys on healthcare topics [66,67]. Their potential role in modeling actual vaccine acceptance should, therefore, be accurately addressed [24,33,68], supporting a precautionary appraisal of our data, particularly when our estimates are compared to other reports, not only at an international [52,53] but also at a national level [68,69,70,71,72,73].
Third, the working definition of vaccination status has reasonably impaired the eventual reliability of our estimates. Compared to other immunization programs, the classical schedule of TBE vaccination is quite complicated, requiring a priming series of three doses, followed by a booster dose and several periodic shots [16,27]; the available studies on travelers suggest that up to 50% of reportedly vaccinated individuals may have failed to complete the full schedule [52,53]. As a consequence, we cannot rule out the possibility that a substantial share of the participants overstated their actual vaccination status. For example, Pilz et al. [24] have recently stressed that in sampled individuals from Poland, Hungary, and Slovakia, only 24% of persons in their study were actually protected against TBE. Nonetheless, a recent report from Pugh et al. [47] has suggested that travelers heading to high-risk areas could probably be protected against TBE for at least 5 months after two primary doses of FSME-IMMUN®, with the third dose still being required for achieving long-term protection. Hence, future iterations of the present study should more carefully retrieve information on the timeframe of the vaccination in order to provide more accurate estimates of actual protection against TBE.
Fourth, since the collected data were not externally validated, we cannot rule out a certain degree of declarative bias. It is plausible that some of the respondents did not truly adhere to the study requirements, having preferentially reported “socially desirable” status and attitudes instead of their actual ones. Not coincidentally, 18.0% of vaccinated responders acknowledged the aim of avoiding the spread of the disease as a key motivation for having been vaccinated against TBE, with 12.7% allegedly aiming to protect those who cannot be vaccinated. TBEV has shown no inter-human spreading [1,13], and even though this attitude may indirectly represent the solidaristic background often underlying vaccine propensity, a quite cautious appraisal of our estimates is forcibly warranted. In other words, not only did our study eventually oversample individuals with a fairly good understanding of tick-borne disorders but it is also reasonable that even the actual acceptance of vaccines and preventive interventions was similarly inflated [74].
Fifth, even though our sample largely fulfilled the minimum sample-size requirements, around 1000 respondents are relatively few when compared to the whole of the population from Italian regions as characterized by TBEV circulation, with millions of tourists each year traveling to the Dolomite Mountains; they may also be drawn from a potentially targeted population [41]. In fact, from a potential population of 20,444 individuals, our study had a 4.6% response rate, which impairs an extensive generalization of our results, particularly in a country such as Italy, which is characterized by extensive heterogeneities in health literacy. However, our sample was substantially in line, both in terms of its demographics and with the eventual results, with similar international studies, preserving its significance for comparison with the available estimates [52,53,75,76].
Sixth, due to its design, our survey does not provide any substantial insight into pediatric age groups (i.e., individuals < 18 years old). Although there is some evidence that the incidence of TBE is higher in older vs. younger children, and in adults vs. children [77], with younger age groups usually reporting a milder course of disease [77,78] and fewer neurological sequelae [77], recent reports have stressed that severe forms can also occur in children and adolescents [78], with an increasing number of cases being reported in pre-school children. As a consequence, a future follow-up of the present study should address the preventive practices implemented by parents in order to prevent TBE virus infection in their offspring, in order to better appreciate the pros and cons of pediatric vaccination strategies, at least for children living, traveling to, or with familiarity with high-risk areas [16,27,77,78].
Last but not least, previous studies have stressed the importance of media coverage of TBEV infections [45]. By raising the eventual risk perception about an otherwise often misunderstood infection, the eventual impact of new and social media on the acceptance of the TBE vaccine may even exceed that of other topics of public health interest [79]. As a proxy of the media coverage on TBE and other tick-borne infections, we specifically explored the relative search volumes provided by Google Trends™ [80,81]. As shown in Appendix A, Table A6, during the study period, no correlation was found for RPSinf, RPSvac, and their components. In other words, risk perception on TBE, TBEV infections, and tick-borne diseases among the study participants was seemingly not influenced by new media coverage.
5. Conclusions
Our study suggests that tourists to the Dolomite Mountains, a high-risk area for TBE and TBEV virus infection, collectively exhibit an extensive lack of knowledge of this pathogen, with inappropriate risk awareness. Moreover, actual uptake of the TBE vaccine, while still in line with European data, was largely unsatisfactory. As TBEV infection may be effectively countered through a combination of effective behavioral practices and TBE vaccination for people either living or performing outdoor activities in high-risk areas, 69 improving overall awareness of these preventive options could, therefore, be instrumental in reducing the eventual burden of TBEV infections (see Appendix A, Table A7).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/tropicalmed8110491/s1, Table S1: STROBE statement, giving a checklist of items that should be included in reports of cross-sectional studies; Table S2: Authors’ translation of the informed consent; Table S3: Authors’ translation of the questionnaire; File S1: Italian Official Gazette no. 76; File S2: European Regulation 2016/679.
Appendix A
Table A1.
The general knowledge score sheet. The internal consistency of the main test was assessed by the calculation of Cronbach’s alpha (0.824), which suggested a good level of consistency.
| Statement | Correct Answer | |
|---|---|---|
| Content | N./942, % | |
| Q01. Ticks feeding on cats and dogs may cause human disease. | TRUE | 402, 35.5% |
| Q02. Ticks prefer to live in damp, shady areas. | TRUE | 555, 49.1% |
| Q03. The majority of ticks that are found in Italy may spread severe human diseases. | FALSE | 330, 29.2% |
| Q04. Tick-borne human diseases are more frequently diagnosed between May and September. | TRUE | 746, 79.1% |
| Q05. The available vaccines protect against all tick-borne human diseases. | FALSE | 517, 45.7% |
| Q06. Ticks removed within 24 hours from their first bite do not require any treatment. | FALSE | 492, 43.5% |
| Q07. All tick-borne human diseases manifest themselves within 2 days of the first bite. | FALSE | 660, 58.4% |
| Q08. Tick-borne human diseases may always be treated with antibiotics. | FALSE | 498, 44.0% |
| Q09. Tick bites are frequently complicated by local infections. | TRUE | 684, 60.5% |
| Q10. Local treatment with alcohol on the bite site is appropriate for tick removal. | FALSE | 714, 63.1% |
| Q11. After tick removal, the bite site should be checked for the tick head. | TRUE | 873, 77.2% |
| Q12. The milk of animals affected by tick-borne disease may harbor pathogens. | TRUE | 105, 9.3% |
Table A2.
Summary of the perceived probability of contracting a TBEV infection (Einf); the perceived probability of developing complications after the delivery of TBE vaccine (Evac); the perceived severity of the natural infection from TBEV (Cinf); the perceived severity of vaccine side effects (Cvac), as reported by 942 participants (Italy, 2023).
| Almost Zero (N, %) |
Low or Rather Low (N, %) |
Moderate (N, %) |
High or Rather High (N, %) |
Very High (N, %) |
|
|---|---|---|---|---|---|
| Einf | 33, 3.5% | 120, 12.7% | 303, 32.2% | 357, 37.9% | 129, 13.7% |
| Cinf | 3, 0.3% | 36, 3.8% | 150, 15.9% | 426, 45.2% | 327, 34.7% |
| Evac | 504, 53.5% | 204, 21.7% | 180, 19.1% | 42, 4.5% | 12, 1.3% |
| Cvac | 516, 54.8% | 189, 20.1% | 183, 19.4% | 45, 4.8% | 9, 1.0% |
Table A3.
Correlation between the sum scores. Analyses were performed by the calculation of Spearman’s rho (ρ) and the corresponding p-values. (Note: TBEV = tick-borne encephalitis virus; GKS = general knowledge score; SKS = symptom knowledge score; RPSinf = risk perception score for natural TBEV infection; RPSvac = risk perception score for side effects of the TBE vaccine.)
| Cumulative Score | GKS | SKS | RPSinf | RPSvac |
|---|---|---|---|---|
| GKS | - | ρ = 0.334 p < 0.001 |
ρ = 0.085 p = 0.009 |
ρ = −0.281 p < 0.001 |
| SKS | ρ = 0.334 p < 0.001 |
- | ρ = 0.262 p < 0.001 |
ρ = −0.123 p < 0.001 |
| RPSinf | ρ = 0.085 p = 0.009 |
ρ = 0.262 p < 0.001 |
- | ρ = −0.078 p = 0.017 |
| RPSvac | ρ = −0.281 p < 0.001 |
ρ = −0.123 p < 0.001 |
ρ = −0.078 p = 0.017 |
- |
Table A4.
Comparison of the cumulative scores (general knowledge score, symptom knowledge score, risk perception score per tick-borne infection and for the tick-borne encephalitis virus (TBEV) vaccine) according to age group (an analysis of variance, or ANOVA, with Dunnet’s post hoc test). For all comparisons, the age group of 60 years old or more was considered to be the reference group.
| Cumulative Score | Age Group | ||
|---|---|---|---|
| <40 Years | 40 to 59 Years | 60 Years or Over | |
| General Knowledge Score (%) | 61.79 ± 17.59 (p = 0.001) |
56.12 ± 16.03 (p = 0.972) |
56.39 ± 16.74 (REFERENCE GROUP) |
| Symptom Knowledge Score (%) | 59.98 ± 16.51 (p < 0.001) |
58.29 ± 16.51 (p < 0.001) |
51.93 ± 19.50 (REFERENCE GROUP) |
| Risk Perception Score, Tick-borne Infections (%) |
51.62 ± 23.00 (p = 0.877) |
53.27 ± 24.03 (p = 0.367) |
50.73 ± 27.03 (REFERENCE GROUP) |
| Risk Perception Score, TBE Vaccine (%) |
13.74 ± 18.79 (p = 0.001) |
11.27 ± 13.62 (p = 0.088) |
8.62 ± 11.54 (REFERENCE GROUP) |
Table A5.
Incident cases and doses of tick-borne encephalitis virus vaccine delivered in the Autonomous Province between 2016 and 2021 (detailed reports are available from: https://www.vaccinarsintrentino.org/, accessed on 1 September 2023).
| Year | Total Population | Cases of TBEV (Crude Incidence per 100,000 People) |
Delivered Doses (Doses per 100 People) |
Total Vaccine Doses (% TBE) |
|---|---|---|---|---|
| 2016 | 539,513 | 20 (3.7) | 0 (-) | 164,095 (-) |
| 2017 | 540,280 | 21 (3.9) | 673 (0.1) | 216,053 (0.3%) |
| 2018 | 541,966 | 8 (1.5) | 16,525 (3.0) | 243,733 (6.8%) |
| 2019 | 543,721 | 13 (2.4) | 21,473 (3.9) | 244,555 (8.8%) |
| 2020 | 545,425 | 11 (2.0) | 13,351 (2.5) | 265,184 (5.0%) |
| 2021 | 542,166 | 5 (0.9) | 6,354 (1.2) | 199,215 (3.2%) |
Table A6.
Summary of the correlation between the relative search volumes (RSV) from Google TrendsTM on tick-borne encephalitis (Italian: “encefalite da zecche”) and the probability of contracting a TBEV infection (Einf); perceived probability of developing complications after the delivery of TBE vaccine (Evac); perceived severity of a natural infection from TBEV (Cinf); perceived severity of vaccine side effects (Cvac); risk perception score regarding TBEV infection (RPSinf), and risk perception score regarding the TBE vaccine (RPSvac), as reported by 942 participants (Italy, 2023) (Note: 95%CI = 95% confidence interval). Google TrendsTM is an open-access online tool, provided by Alphabet, reporting the overall queries on a certain keyword as the normalized ratio over the total of web queries in that specific timeframe.
| RSV on Tick-Borne Encephalitis | ||
|---|---|---|
| Spearman’s Rho (95%CI) | p-Value | |
| Einf | −0.020 (95%CI −0.131 to 0.092) | 0.722 |
| Cinf | −0.107 (95%CI −0.217 to 0.004) | 0.054 |
| Evac | 0.021 (95%CI −0.091 to 0.133) | 0.709 |
| Cvac | −0.066 (95%CI −0.176 to 0.047) | 0.239 |
| RPSinf | −0.066 (95%CI −0.176 to 0.047) | 0.239 |
| RPSvac | 0.027 (95%CI −0.086 to 0.138) | 0.633 |
Table A7.
Summary of the meaning of the present article.
| What did you want do address in this study? |
| Tick-borne encephalitis (TBE) is a human viral infectious disease transmitted by the bite of infected ticks and affecting the central nervous system. Climate changes and increased human interactions in at-risk areas (mostly woodlands in Central Europe and alpine ranges), including the Dolomite Mountains, have stressed the importance of vaccination campaigns as a reliable instrument for achieving TBE control in countries in the European Union/European Economic Areas. We wanted to investigate the TBE vaccination rates and individual preventive measures for tick bites among tourists to the Dolomite Mountains and ascertain which individual factors were associated with TBE vaccination uptake. |
| What have we learned from this study? |
| Vaccination rates in the tourist population were low (<30% for the sample as a whole), even in individuals from Italian regions considered at high risk for TBE (i.e., the Autonomous Provinces of Trento and Bolzano and the regions of Veneto and Friuli Venezia Giulia, <40%). Participants exhibited an unsatisfactory level of knowledge of TBE and tick-borne disorders, which was associated with a similarly inappropriate risk perception about its occurrence. The main effectors of vaccination status were identified as age, living in high-risk areas, having previously been bitten by a tick, knowledge status, and risk perception, which, in turn, was well-correlated with knowledge status. |
| What are the implications of your findings for public health? |
| Information campaigns aimed at improving disease awareness among tourists traveling to high-risk areas can improve their risk perception regarding TBE and more in general regarding tick-borne diseases. By improving vaccination status in individuals potentially at high risk of contracting TBE and other tick-borne diseases, properly designed interventions, including appropriate pre-travel counseling, could contribute to the better control of TBE in northeastern Italy. |
Figure A1.
Triveneto Region and the Dolomite mountain ranges (https://commons.wikimedia.org/wiki/File:Alps_location_map.png (access on 1 August 2023); https://it.wikipedia.org/wiki/Regione_ecclesiastica_Triveneto#/media/File:Ecclesiastical%20region%20Triveneto%20in%20Italy.svg (access on 1 August 2023)). The Dolomites are a well-confined mountain range in northeastern Italy in the eastern part of the Southern Alps, between the Austrian border in the north and the Venetian plain in the south (Appendix A, Figure A1) [41,82,83]. With an average height under 3000 m and their highest peak (the Marmolada Mountain) at an elevation of around 3343 m above sea level, the Dolomites are relatively low compared to nearby ranges. Their area (15,942 km2) is shared by the Italian provinces of Belluno, Vicenza, Verona, Trento, Bolzano, Udine, and Pordenone. The alpine climate of the Dolomites is characterized by harsh winter temperatures and summer heavy rainfall [82,83], but compared to the border regions of Austria and Switzerland, the Dolomite Mountains are characterized by warmer temperatures and less precipitation; therefore, they are highly accessible in both the cold and warm seasons. These features, as well as being one of the 218 natural UNESCO world heritage sites, collectively contribute to their wide tourism appeal, with far more than 20 million overnight stays per year [41]. To date, Ixodes ticks are usually found at altitudes < 1500 m above sea level from spring to autumn at temperatures above 10 °C, even though global warming is progressively raising this altitude level [31,84,85].
Figure A2.
Distribution of the general knowledge score (GKS; a), a summary score for symptoms associated with tick-borne diseases (symptoms score; b), a risk perception score (RPS) for tick-borne diseases (c), and the RPS for side effects of the TBE vaccine (d). For all sum scores, distribution did not pass a normality check according to the D’Agostino–Pearson test (GKS: K2 = 63.71, p < 0.001; symptom score: K2 = 37.55, p < 0.001; RPS for natural infection: K2 = 30.11, p < 0.001; RPS for the TBE vaccine: K2 = 569.1, p < 0.001).
Figure A3.
Frequency of acute (a) and chronic (b) symptoms associated with tick-borne infections, as reported by the 942 Italian subjects participating in the survey. In both cases, the number of respondents either agreeing or strongly agreeing with the presented sign/symptom is reported.
Figure A4.
Occurrence of tick bites, as reported by 942 participants (Italy, 2023), shown according to age group.
Figure A5.
Number of preventive measures reported by 156 participants with a previous history of tick bite(s). Overall, the share of respondents reporting no preventive measures was 55.56% in the 30–39 age group, 43.75% in the 40–49 age group, 27.27% in the 50–59 age group, 10.00% in the 60–69 age group, and 20.00% in ≥70-year-old respondents, while participants aged 20–29 years all reported 2 preventative measures.
Author Contributions
Conceptualization, M.R.; data curation, M.R. and M.B.; formal analysis, M.R. and F.M.; funding acquisition, F.M.; investigation, M.R.; methodology, M.B., F.M. and S.C.; resources, F.M.; software, M.R.; supervision, F.M. and M.B.; validation, S.C.; writing—review and editing, M.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Preventive ethical review and approval were waived for this study because of its anonymous, observational design and due to the lack of clinical data about patients that could configure the present research as a clinical trial. The study, therefore, did not configure itself as a clinical trial, and a preliminary evaluation by an ethical committee was not required, according to Italian law (Gazzetta Ufficiale no. 76, dated 31 March 2008).
Informed Consent Statement
Informed written consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Johnson N., Migné C.V., Gonzalez G. Tick-Borne Encephalitis. Curr. Opin. Infect. Dis. 2023;36:198–202. doi: 10.1097/QCO.0000000000000924. [DOI] [PubMed] [Google Scholar]
- 2.Nygren T.M., Pilic A., Böhmer M.M., Wagner-Wiening C., Went S.B., Wichmann O., Hellenbrand W. Tick-Borne Encephalitis: Acute Clinical Manifestations and Severity in 581 Cases from Germany, 2018–2020. J. Infect. 2023;86:369–375. doi: 10.1016/j.jinf.2023.02.018. [DOI] [PubMed] [Google Scholar]
- 3.ECDC . Tick-Borne Encephalitis Annual Epidemiological Report for 2020 Key Facts. ECDC; Solna, Sweden: 2020. [Google Scholar]
- 4.European Centre for Disease Prevention and Control . Tick-Borne Encephalitis Annual Epidemiological Report for 2018 Key Facts. European Centre for Disease Prevention and Control; Solna, Sweden: 2019. [Google Scholar]
- 5.Martello E., Gillingham E.L., Phalkey R., Vardavas C., Nikitara K., Bakonyi T., Gossner C.M., Leonardi-Bee J. Systematic Review on the Non-Vectorial Transmission of Tick-Borne Encephalitis Virus (TBEv) Ticks Tick-Borne Dis. 2022;13:102028. doi: 10.1016/j.ttbdis.2022.102028. [DOI] [PubMed] [Google Scholar]
- 6.Chiffi G., Grandgirard D., Leib S.L., Chrdle A., Růžek D. Tick-borne Encephalitis: A Comprehensive Review of the Epidemiology, Virology, and Clinical Picture. Rev. Med. Virol. 2023;33:e2470. doi: 10.1002/rmv.2470. [DOI] [PubMed] [Google Scholar]
- 7.Ricco M., Peruzzi S., Balzarini F. Epidemiology of West Nile Virus Infections in Humans, Italy, 2012–2020: A Summary of Available Evidences. Trop. Med. Infect. Dis. 2021;6:61. doi: 10.3390/tropicalmed6020061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riccò M., Peruzzi S., Balzarini F., Zaniboni A., Ranzieri S. Dengue Fever in Italy: The “Eternal Return” of an Emerging Arboviral Disease. Trop. Med. Infect. Dis. 2022;7:10. doi: 10.3390/tropicalmed7010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Leur S.W., Heunis T., Munnur D., Sanyal S. Pathogenesis and Virulence of Flavivirus Infections. Virulence. 2021;12:2814–2838. doi: 10.1080/21505594.2021.1996059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.ECDC . Epidemiological Situation of Tick-Borne Encephalitis in the European Union and European Free Trade Association Countries. ECDC; Solna, Sweden: 2012. [Google Scholar]
- 11.Xing Y., Schmitt H.J., Arguedas A., Yang J. Tick-Borne Encephalitis in China: A Review of Epidemiology and Vaccines. Vaccine. 2017;35:1227–1237. doi: 10.1016/j.vaccine.2017.01.015. [DOI] [PubMed] [Google Scholar]
- 12.Ruzek D., Avšič Županc T., Borde J., Chrdle A., Eyer L., Karganova G., Kholodilov I., Knap N., Kozlovskaya L., Matveev A., et al. Tick-Borne Encephalitis in Europe and Russia: Review of Pathogenesis, Clinical Features, Therapy, and Vaccines. Antivir. Res. 2019;164:23–51. doi: 10.1016/j.antiviral.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 13.Caputo M., Stumpe V., Rübsamen N., Mikolajczyk R.T., Karch A. Implementation of Preventive Measures against Tick-Borne Infections in a Non-Endemic Area for Tick-Borne Encephalitis—Results from a Population-Based Survey in Lower Saxony, Germany. Ticks Tick-Borne Dis. 2019;10:614–620. doi: 10.1016/j.ttbdis.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 14.Charrel R.N., Attoui H., Butenko A.M., Clegg J.C., Deubel V., Frolova T.V., Gould E.A., Gritsun T.S., Heinz F.X., Labuda M., et al. Tick-Borne Virus Diseases of Human Interest in Europe. Clin. Microbiol. Infect. 2004;10:1040–1055. doi: 10.1111/j.1469-0691.2004.01022.x. [DOI] [PubMed] [Google Scholar]
- 15.Kohlmaier B., Schweintzger N.A., Sagmeister M.G., Švendová V., Kohlfürst D.S., Sonnleitner A., Leitner M., Berghold A., Schmiedberger E., Fazekas F., et al. Clinical Characteristics of Patients with Tick-Borne Encephalitis (Tbe): A European Multicentre Study from 2010 to 2017. Microorganisms. 2021;9:1420. doi: 10.3390/microorganisms9071420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Panatto D., Domnich A., Amicizia D., Reggio P., Iantomasi R. Vaccination against Tick-Borne Encephalitis (TBE) in Italy: Still a Long Way to Go. Microorganisms. 2022;10:464. doi: 10.3390/microorganisms10020464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haglund M., Günther G. Tick-Borne Encephalitis—Pathogenesis, Clinical Course and Long-Term Follow-Up. Vaccine. 2003;21:S11–S18. doi: 10.1016/S0264-410X(02)00811-3. [DOI] [PubMed] [Google Scholar]
- 18.Coyer L., Sogan-Ekinci A., Greutélaers B., Kuhn J., Saller F.S., Hailer J., Böhm S., Brosch R., Wagner-Wiening C., Böhmer M.M. Knowledge, Attitudes and Behaviors Regarding Tick-Borne Encephalitis Vaccination and Prevention of Tick-Borne Diseases among Primary Care Physicians in Bavaria and Baden-Wuerttemberg, Germany, May–September 2022. Microorganisms. 2023;11:961. doi: 10.3390/microorganisms11040961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vonesch N., D’Ovidio M.C., Melis P., Remoli M.E., Ciufolini M.G., Tomao P. Climate Change, Vector-Borne Diseases and Working Population. Ann. Ist. Super. Sanità. 2016;52:397–405. doi: 10.4415/ANN_16_03_11. [DOI] [PubMed] [Google Scholar]
- 20.Alkishe A.A., Peterson A.T., Samy A.M. Climate Change Influences on the Potential Geographic Distribution of the Disease Vector Tick Ixodes Ricinus Climate Change Influences on the Potential Geographic Distribution of the Disease Vector Tick Ixodes Ricinus. PLoS ONE. 2017;12:e0189092. doi: 10.1371/journal.pone.0189092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Riccò M., Bragazzi N.L., Vezzosi L., Balzarini F., Colucci M.E., Veronesi L. Knowledge, Attitudes, and Practices on Tick-Borne Human Diseases and Tick-Borne Encephalitis Vaccine among Farmers from North-Eastern Italy (2017) J. Agromedicine. 2020;25:73–85. doi: 10.1080/1059924X.2019.1659204. [DOI] [PubMed] [Google Scholar]
- 22.Riccò M., Gualerzi G., Ranzieri S., Ferraro P., Bragazzi N.L. Knowledge, Attitudes, Practices (KAP) of Italian Occupational Physicians towards Tick Borne Encephalitis. Trop. Med. Infect. Dis. 2020;5:117. doi: 10.3390/tropicalmed5030117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bojkiewicz E., Toczylowski K., Grygorczuk S., Zelazowska-Rutkowska B., Dunaj J., Zebrowska A., Czupryna P., Moniuszko-Malinowska A., Sulik A. The Prevalence of Asymptomatic Infections with Tick-Borne Encephalitis Virus and Attitude towards Tick-Borne Encephalitis Vaccine in the Endemic Area of Northeastern Poland. Vaccines. 2022;10:1294. doi: 10.3390/vaccines10081294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pilz A., Erber W., Schmitt H.J. Vaccine Uptake in 20 Countries in Europe 2020: Focus on Tick-Borne Encephalitis (TBE) Ticks Tick-Borne Dis. 2023;14:102059. doi: 10.1016/j.ttbdis.2022.102059. [DOI] [PubMed] [Google Scholar]
- 25.Rezza G., Farchi F., Pezzotti P., Ruscio M., lo Presti A., Ciccozzi M., Mondardini V., Paternoster C., Bassetti M., Merelli M., et al. Tick-Borne Encephalitis in North-East Italy: A 14-Year Retrospective Study, January 2000 to December 2013. Eurosurveillance. 2015;20:30034. doi: 10.2807/1560-7917.ES.2015.20.40.30034. [DOI] [PubMed] [Google Scholar]
- 26.Cocchio S., Bertoncello C., Napoletano G., Claus M., Furlan P., Fonzo M., Gagliani A., Saia M., Russo F., Baldovin T., et al. Do We Know the True Burden of Tick-Borne Encephalitis? A Cross-Sectional Study. Neuroepidemiology. 2019;54:227–234. doi: 10.1159/000503236. [DOI] [PubMed] [Google Scholar]
- 27.Amicizia D., Domnich A., Panatto D., Lai P.L., Cristina M.L., Avio U., Gasparini R. Epidemiology of Tick-Borne Encephalitis (TBE) in Europe and Its Prevention by Available Vaccines. Hum. Vaccin. Immunother. 2013;9:1163–1171. doi: 10.4161/hv.23802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Erber W., Schmitt H.J. Self-Reported Tick-Borne Encephalitis (TBE) Vaccination Coverage in Europe: Results from a Cross-Sectional Study. Ticks Tick-Borne Dis. 2018;9:768–777. doi: 10.1016/j.ttbdis.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 29.Vonesch N., Binazzi A., Bonafede M., Melis P., Ruggieri A., Iavicoli S., Tomao P. Emerging Zoonotic Viral Infections of Occupational Health Importance. Pathog. Dis. 2019;77:ftz018. doi: 10.1093/femspd/ftz018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Riccò M. Epidemiology of Tick-Borne Encephalitis in North-Eastern Italy (2017–2020): International Insights from National Notification Reports. Acta Biomed. 2021;92:e2021229. doi: 10.23750/abm.v92i5.11474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alfano N., Tagliapietra V., Rosso F., Ziegler U., Arnoldi D., Rizzoli A. Tick-Borne Encephalitis Foci in Northeast Italy Revealed by Combined Virus Detection in Ticks, Serosurvey on Goats and Human Cases. Emerg. Microbes Infect. 2020;9:474–484. doi: 10.1080/22221751.2020.1730246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kunze U., Kunze M. The Austrian Vaccination Paradox: Tick-Borne Encephalitis Vaccination Versus Influenza Vaccination. Cent. Eur. J. Public Health. 2015;23:223. doi: 10.21101/cejph.a4169. [DOI] [PubMed] [Google Scholar]
- 33.Zingg A., Siegrist M. Measuring People’s Knowledge about Vaccination: Developing a One-Dimensional Scale. Vaccine. 2012;30:3771–3777. doi: 10.1016/j.vaccine.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 34.Gaube S., Lermer E., Fischer P. The Concept of Risk Perception in Health-Related Behavior Theory and Behavior Change. In: Raue M., Streicher B., Lermer E., editors. Perceived Safety. Risk Engineering. Springer; Cham, Switzerland: 2019. pp. 101–118. [Google Scholar]
- 35.Yates F.J., Stone E.R. Risk-Taking Behaviour. John Wiley & Sons.; Chichester, UK: 1992. The Risk Construct; pp. 1–25. [Google Scholar]
- 36.Betsch C., Wicker S. Personal Attitudes and Misconceptions, Not Official Recommendations Guide Occupational Physicians’ Vaccination Decisions. Vaccine. 2014;32:4478–4484. doi: 10.1016/j.vaccine.2014.06.046. [DOI] [PubMed] [Google Scholar]
- 37.Haddock G., Maio G.R. 6 Attitudes: Content, Structure and Functions. In: Hewstone M., Stroebe W., Jonas K., editors. An Introduction to Social Psychology. BPS Blackwell; Chichester, UK: 2012. pp. 112–133. [Google Scholar]
- 38.Arghittu A., Dettori M., Azara A., Gentili D., Serra A., Contu B., Castiglia P. Flu Vaccination Attitudes, Behaviours, and Knowledge among Health Workers. Int. J. Environ. Res. Public. Health. 2020;17:3185. doi: 10.3390/ijerph17093185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.European Union. European Council. European Parliament . Europea Union (EU) Regulation N. 2016/679 on the Protection of Natural Persons with Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95/46/EC (General Data Protection Regulation) European Union; Strasbourg, France: 2016. [Google Scholar]
- 40.R Development Core Team . R a Language and Environment for Statistical Computing: Reference Index. R Foundation for Statistical Computing; Vienna, Austria: 2010. [Google Scholar]
- 41.Province of Belluno. Autonomous Province of Bolzano. Autonomous Province of Trento. Province of Udine. Autonomous Region of Friuli Venezia Giulia . THE DOLOMITES THE WORLD NATURAL HERITAGE LIST UNESCO Nomination of the Dolomites for Inscription on the World Natural Heritage List UNESCO. Autonomous Province of Bolzano; Bolzano, Italy: 2009. [Google Scholar]
- 42.Belobo J.T.E., Kenmoe S., Kengne-Nde C., Emoh C.P.D., Bowo-Ngandji A., Tchatchouang S., Wobessi J.N.S., Mikangue C.A.M., Tazokong H.R., Bebey S.R.K., et al. Worldwide Epidemiology of Crimean-Congo Hemorrhagic Fever Virus in Humans, Ticks and Other Animal Species, a Systematic Review and Meta-Analysis. PLoS Negl. Trop. Dis. 2021;15:e0009299. doi: 10.1371/journal.pntd.0009299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maioli G., Pistone D., Bonilauri P., Pajoro M., Barbieri I., Patrizia M., Vicari N., Dottori M. Ethiological Agents of Rickettsiosis and Anaplasmosis in Ticks Collected in Emilia-Romagna Region (Italy) during 2008 and 2009. Exp. Appl. Acarol. 2012;57:199–208. doi: 10.1007/s10493-012-9535-z. [DOI] [PubMed] [Google Scholar]
- 44.Riccò M., Baldassarre A., Corrado S., Bottazzoli M., Marchesi F. Seroprevalence of Crimean Congo Hemorrhagic Fever Virus in Occupational Settings: Systematic Review and Meta-Analysis. Trop. Med. Infect. Dis. 2023;8:452. doi: 10.3390/tropicalmed8090452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zöldi V., Turunen T., Lyytikäinen O., Sane J. Knowledge, Attitudes, and Practices Regarding Ticks and Tick-Borne Diseases, Finland. Ticks Tick-Borne Dis. 2017;8:872–877. doi: 10.1016/j.ttbdis.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 46.Slunge D., Boman A. Learning to Live with Ticks? The Role of Exposure and Risk Perceptions in Protective Behaviour against Tick-Borne Diseases. PLoS ONE. 2018;13:e0198286. doi: 10.1371/journal.pone.0198286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pugh S.J., Moïsi J.C., Kundi M., Santonja I., Erber W., Angulo F.J., Jodar L. Effectiveness of Two Doses of Tick-Borne Encephalitis (TBE) Vaccine. J. Travel. Med. 2022;29:taab193. doi: 10.1093/jtm/taab193. [DOI] [PubMed] [Google Scholar]
- 48.Riccò M., Razio B., Poletti L., Panato C. Knowledge, Attitudes, and Sun-Safety Practices among Agricultural Workers in the Autonomous Province of Trento, North-Eastern Italy (2016) G. Ital. Dermatol. Venereol. 2020;155:31–40. doi: 10.23736/S0392-0488.17.05672-3. [DOI] [PubMed] [Google Scholar]
- 49.Angelo K.M., Kozarsky P.E., Ryan E.T., Chen L.H., Sotir M.J. What Proportion of International Travellers Acquire a Travel-Related Illness? A Review of the Literature. J. Travel. Med. 2017;24:tax046. doi: 10.1093/jtm/tax046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stefanati A., Pierobon A., Baccello V., DeStefani E., Gamberoni D., Furlan P., Sandri F., Stano A., Coin P., Baldo V., et al. Travellers’ Risk Behaviors and Health Problems: Post-Travel Follow up in Two Travel Medicine Centers in Italy. Med. Mal. Infect. 2020;51:279–284. doi: 10.1016/j.medmal.2020.10.009. [DOI] [PubMed] [Google Scholar]
- 51.Khan N.M., Jentes E.S., Brown C., Han P., Rao S.R., Kozarsky P., Hagmann S.H.F., LaRocque R.C., Ryan E.T. Pre-Travel Medical Preparation of Business and Occupational Travelers. J. Occup. Environ. Med. 2016;58:76–82. doi: 10.1097/JOM.0000000000000602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Poulos C., Boeri M., Coulter J., Huang L., Schley K., Pugh S.J. Travelers’ Preferences for Tick-Borne Encephalitis Vaccination. Expert. Rev. Vaccines. 2022;21:1495–1504. doi: 10.1080/14760584.2022.2108798. [DOI] [PubMed] [Google Scholar]
- 53.Marano C., Moodley M., Melander E., De Moerlooze L., Nothdurft H.D. Perceptions of Tick-Borne Encephalitis Risk: A Survey of Travellers and Travel Clinics from Canada, Germany, Sweden and the UK. J. Travel. Med. 2018;26:S10–S16. doi: 10.1093/jtm/tay063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.MacDonald N.E., Eskola J., Liang X., Chaudhuri M., Dube E., Gellin B., Goldstein S., Larson H., Manzo M.L., Reingold A., et al. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 55.Slunge D. The Willingness to Pay for Vaccination against Tick-Borne Encephalitis and Implications for Public Health Policy: Evidence from Sweden. PLoS ONE. 2015;10:e143875. doi: 10.1371/journal.pone.0143875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Paradowska-Stankiewicz I., Pancer K., Poznańska A., Hordowicz M., Skibicka M., Słowiński M., Motak G., Falkiewicz B. Tick-Borne Encephalitis Epidemiology and Surveillance in Poland, and Comparison with Selected European Countries before and during the COVID-19 Pandemic, 2008 to 2020. Eurosurveillance. 2023;28:2200452. doi: 10.2807/1560-7917.ES.2023.28.18.2200452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wendt S., Beier D., Paquet D., Trawinski H., Fuchs A., Lübbert C. Medical Advice for Travelers. Dtsch. Arztebl. Int. 2021;118:349–356. doi: 10.3238/arztebl.m2021.0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kogelman L., Barnett E.D., Chen L.H., Quinn E., Yanni E., Wilson M.E., Benoit C., Karchmer A.W., Ooi W.W., Jentes E.S., et al. Knowledge, Attitudes, and Practices of US Practitioners Who Provide Pre-Travel Advice. J. Travel. Med. 2014;21:104–114. doi: 10.1111/jtm.12097. [DOI] [PubMed] [Google Scholar]
- 59.Italian Health Ministry . Italian National Plan for the Prevention, Surveillance, and Response to Arboviroses (PNA) 2020–2025. Italian Health Ministry; Rome, Italy: 2019. [Google Scholar]
- 60.Italian Health Ministry . Piano Nazionale Di Prevenzione Vaccinale (PNPV) 2023–2025. Italian Health Ministry; Rome, Italy: 2023. [Google Scholar]
- 61.Tostrud L., Thelen J., Palatnik A. Models of Determinants of COVID-19 Vaccine Hesitancy in Non-Pregnant and Pregnant Population: Review of Current Literature. Hum. Vaccin. Immunother. 2022;18:2138047. doi: 10.1080/21645515.2022.2138047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lipschitz J.M., Fernandez A.C., Elsa Larson H., Blaney C.L., Meier K.S., Redding C.A., Prochaska J.O., Paiva A.L. Validation of Decisional Balance and Self-Efficacy Measures for HPV Vaccination in College Women. Am. J. Health Promot. 2013;27:299–307. doi: 10.4278/ajhp.110606-QUAN-240. [DOI] [PubMed] [Google Scholar]
- 63.Arnett D.K., Claas S.A. Clinical and Translational Science: Principles of Human Research: Second Edition. Elsevier Inc.; Amsterdam, The Netherlands: 2017. Introduction to Epidemiology; pp. 53–69. [Google Scholar]
- 64.Heiervang E., Goodman R. Advantages and Limitations of Web-Based Surveys: Evidence from a Child Mental Health Survey. Soc. Psychiat Epidemiol. 2011;46:69–76. doi: 10.1007/s00127-009-0171-9. [DOI] [PubMed] [Google Scholar]
- 65.Riccò M., Vezzosi L., Marchesi F. Vaccinating Front-Line Healthcare Workers: Results of a Pre-Pandemic Cross-Sectional Study from North-Eastern Italy on First Responders. Vaccines. 2022;10:1492. doi: 10.3390/vaccines10091492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Morrone T., Napolitano F., Albano L., Di G. Meningococcal Serogroup B Vaccine: Knowledge and Acceptability among Parents in Italy Meningococcal Serogroup B Vaccine: Knowledge and Acceptability among Parents in Italy. Hum. Vaccines Immunother. 2017;13:1921–1927. doi: 10.1080/21645515.2017.1313940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.MacDougall D.M., Langley J.M., Li L., Ye L., MacKinnon-Cameron D., Top K.A., McNeil S.A., Halperin B.A., Swain A., Bettinger J.A., et al. Knowledge, Attitudes, Beliefs, and Behaviors of University Students, Faculty, and Staff during a Meningococcal Serogroup B Outbreak Vaccination Program. Vaccine. 2017;35:2520–2530. doi: 10.1016/j.vaccine.2017.02.011. [DOI] [PubMed] [Google Scholar]
- 68.Riccò M., Peruzzi S. Tetanus Vaccination Status and Vaccine Hesitancy in Amateur Basketball Players (Italy, 2020) Vaccines. 2022;10:131. doi: 10.3390/vaccines10010131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gualano M.R., Bert F., Voglino G., Buttinelli E., D’Errico M.M., De Waure C., Di Giovanni P., Fantini M.P., Giuliani A.R., Marranzano M., et al. Attitudes towards Compulsory Vaccination in Italy: Results from the NAVIDAD Multicentre Study. Vaccine. 2018;36:3368–3374. doi: 10.1016/j.vaccine.2018.04.029. [DOI] [PubMed] [Google Scholar]
- 70.Riccò M., Cattani S., Veronesi L., Colucci M.E. Knowledge, Attitudes, Beliefs and Practices of Construction Workers towards Tetanus Vaccine in Northern Italy. Ind. Health. 2016;54:554–563. doi: 10.2486/indhealth.2015-0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bonaccorsi G., Lorini C., Santomauro F., Guarducci S., Pellegrino E., Puggelli F., Balli M., Bonanni P. Predictive Factors Associated with the Acceptance of Pandemic and Seasonal Influenza Vaccination in Health Care Workers and Students in Tuscany, Central Italy. Hum. Vaccin. Immunother. 2013;9:2603–2612. doi: 10.4161/hv.26036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Baig S.A., Hassan M., Ahmed S.M., Moazzam W., Inayat A. A Cross-Sectional Study to Investigate Pneumococcal Vaccination in the Elderly in a Low Income County: Patient Knowledge, Awareness, and Attitudes of Vaccination and Prevalence Rates by Socioeconomic Status. Hum. Vaccin. Immunother. 2014;10:1024–1027. doi: 10.4161/hv.27697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mckeirnan K., Colorafi K., Sun Z., Daratha K., Potyk D., Mccarthy J. Improving Pneumococcal Vaccination Rates among Rural Older Adults through Academic Detailing: Medicine, Nursing and Pharmacy Partnership. Vaccines. 2021;9:317. doi: 10.3390/vaccines9040317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Riccò M., Vezzosi L., Cella C., Pecoraro M., Novembre G., Moreo A., Ognibeni E.M., Schellenberg G., Maranelli G. Tetanus Vaccination Status in Construction Workers: Results from an Institutional Surveillance Campaign. Acta Biomed. 2019;90:269. doi: 10.23750/abm.v90i2.6759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Marano C., Moodley M., Melander E., De Moerlooze L., Nothdurft H.D. Multinational Survey Shows Low Awareness of Tick-Borne Encephalitis and Rabies among Travellers to Endemic Regions. J. Travel. Med. 2018;26:S1–S2. doi: 10.1093/jtm/tay069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Steffen R. Epidemiology of Tick-Borne Encephalitis (TBE) in International Travellers to Western/Central Europe and Conclusions on Vaccination Recommendations. J. Travel. Med. 2016;23:taw018. doi: 10.1093/jtm/taw018. [DOI] [PubMed] [Google Scholar]
- 77.Steffen R. Tick-Borne Encephalitis (TBE) in Children in Europe: Epidemiology, Clinical Outcome and Comparison of Vaccination Recommendations. Ticks Tick-Borne Dis. 2019;10:100–110. doi: 10.1016/j.ttbdis.2018.08.003. [DOI] [PubMed] [Google Scholar]
- 78.Parfut A., Laugel E., Baer S., Gonzalez G., Hansmann Y., Wendling M.J., Fafi-Kremer S., Velay A. Tick-Borne Encephalitis in Pediatrics: An Often Overlooked Diagnosis. Infect. Dis. Now. 2023;53:104645. doi: 10.1016/j.idnow.2023.01.005. [DOI] [PubMed] [Google Scholar]
- 79.Mahroum N., Watad A., Rosselli R., Brigo F., Chiesa V., Siri A., Ben-Ami Shor D., Martini M., Bragazzi N.L., Adawi M. An Infodemiological Investigation of the So-Called “Fluad Effect” during the 2014/2015 Influenza Vaccination Campaign in Italy: Ethical and Historical Implications. Hum. Vaccin. Immunother. 2018;14:712–718. doi: 10.1080/21645515.2017.1420448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kow R.Y., Mohamad Rafiai N., Ahmad Alwi A.A., Low C.L., Ahmad M.W., Zakaria Z., Zulkifly A.H. COVID-19 Infodemiology: Association Between Google Search and Vaccination in Malaysian Population. Cureus. 2022;14:e29515. doi: 10.7759/cureus.29515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Riccò M., Baldassarre A., Provenzano S., Corrado S., Cerviere M.P., Parisi S., Marchesi F., Bottazzoli M. Infodemiology of RSV in Italy (2017–2022): An Alternative Option for the Surveillance of Incident Cases in Pediatric Age? Children. 2022;9:1984. doi: 10.3390/children9121984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rota F., Casazza G., Genova G., Midolo G., Prosser F., Bertolli A., Wilhalm T., Nascimbene J., Wellstein C. Topography of the Dolomites Modulates Range Dynamics of Narrow Endemic Plants under Climate Change. Sci. Rep. 2022;12:1398. doi: 10.1038/s41598-022-05440-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bosellini A., Gianolla P., Stefani M. Geology of the Dolomites. Episodes. 2003;26:181–185. doi: 10.18814/epiiugs/2003/v26i3/005. [DOI] [Google Scholar]
- 84.Baráková I., Derdáková M., Selyemová D., Chvostáč M., Špitalská E., Rosso F., Collini M., Rosà R., Tagliapietra V., Girardi M., et al. Tick-Borne Pathogens and Their Reservoir Hosts in Northern Italy. Ticks Tick-Borne Dis. 2017;9:164–170. doi: 10.1016/j.ttbdis.2017.08.012. [DOI] [PubMed] [Google Scholar]
- 85.Nazzi F., Martinelli E., Del Fabbro S., Bernardinelli I., Milani N., Iob A., Pischiutti P., Campello C., D’Agaro P. Ticks and Lyme Borreliosis in an Alpine Area in Northeast Italy. Med. Vet. Entomol. 2010;24:220–226. doi: 10.1111/j.1365-2915.2010.00877.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on request.