Abstract
Study Design
Pedicle screw study.
Objective
The selection of pedicle screw parameters usually involves the surgeon’s analysis of preoperative CT imaging along with anatomical landmarks and tactile examination. However, there is minimal consensus on a standardized guideline for selection methods on pedicle screws. We aimed to determine the effects of thoracic screw diameter to pedicle width on pullout strength determined by cortical bone purchase.
Methods
Biomechanical study performed with human cadaveric thoracic vertebrae and experimentally validated three-dimensional finite element model instrumented with pedicle screws of various diameters. We used a variable (SD/PW) ratio to express the screw selection. We hypothesized a positive correlation between the pullout load determined by the bone purchase and the SD/PW. This relationship was first investigated in a validated finite element model considering bone purchase related to the strength of an upper thoracic vertebra. Then, the correlation to the entire spine is evaluated.
Results
The failure load ranged from 371.3 to 1601.0 N, respectively, for 3 and 6 mm screws. The determinant coefficient was increased to R2=.421 when a linear relationship between pullout load and the SD/PW ratio was used. The peak loads of 1216 and 1288N were found for an SD/PW ratio of .83.
Conclusion
We have found that the screw pullout load is more correlated to SD/PW than other pedicle measures for a maximized SD/PW ratio of .83. This particular value should be considered the upper limit of the indicated SD/PW ratio and a means to determine the optimal screw diameter to enhance pullout strength.
Keywords: pedicle screws, FEA, breaches, thoracic spine, biomechanics, pullout strength
Introduction
For instrumented fixation and correction of the spine, pedicle screw placement has become the predominant modality for cases such as fractures,1-3 scoliosis,4-6 degenerative spine, and kyphosis.7-11 Though complications are rarely associated with pedicle screws, they can occur through misplacement. The various types of complications related to pedicle screw misplacement include: dural lesions,12-14 neurological deficits,14-16 bent or broken screws,13,15 screw loosening, 16 screw-rod disconnections, 16 vertebral fractures,12,13,15,16 hematomas, 14 wound infections,12,14-16 and cerebrospinal fluid leakage.12,15,16 In the choosing of a pedicle screw, the surgeon must carefully consider the pedicle width and the screw diameter, length, trajectory, and entry point17-21 to minimize the morbidity and complications of screw placements.12-14,16 The selection of the screw parameters used involves the surgeon’s analysis of the patient’s anatomical landmarks and tactile examination 22 ; however, preoperative planning with CT and intraoperative imaging techniques such as intraoperative CT and fluoroscopy has been used more recently.23-26 In addition, it has been noted that larger screw diameters increased the pullout strength.27,28 Yet, there is minimal consensus on standardized guidelines for selecting screws and methods of assessment on the placement of the screws.29-31
In the past, the suggested diameter that can be inserted without causing a breaching during thoracic spinal surgeries was approximately under 80% of the pedicle width in adult or mature spines.10,12,28,32 Similarly, Liau et al 33 indicated that the optimal pedicle width compared to screw diameter should allow .5 mm cortical margin on both medial and lateral sides. It should also be noted that most surgeons use only a few screw diameter dimensions for the entire thoracic spine.34-36 Considering the variability in pedicle dimensions among spine levels and gender, 37 limitations on the applicability of these criteria are shown for segments and populations for which commercial screws are too small. 21 Additionally, in scoliotic patients, up to one-third of the mid-thoracic region is not appropriate for safe instrumentation due to pedicle width being smaller than the screw diameter. 32
This study aims to further assist surgeon preoperative planning providing information on the screw strength in addition to the morphometric visualization used in current planning approaches. The approach proposed in this study could shift screw selection from the paradigm that biggest as possible is better to a screw that is dimensioned to have enough strength to avoid failure for pullout. Most preoperative planning is performed on axial CT slices with the pedicle width reference the screw diameter.38,39 Therefore, we used the screw diameter and pedicle width (SD/PW) ratio to express the screw selection. Furthermore, we hypothesized that a positive correlation exists between the pullout load and the SD/PW if we consider the bone purchase as an indicator for the pullout strength.
This relationship has been first investigated in a validated finite element model of an upper thoracic vertebra. Then, the transposition of this correlation to the whole spine has been evaluated through pullout experiments on instrumented cadaveric vertebrae. We expect our findings to decrease preoperative planning time by providing a guideline for selecting screw diameter sizes relative to the pedicle dimensions, considering an important factor of bone purchase overlooked in the past as it is not usually available to surgeons. Estimation during planning of the pull-out load has the potential to reduce risk of loosening since it has been previously associated to pull-out strength.40,41
Materials and Methods
Informed consent was not required as the study was deemed exempt from the requirement as it was on a cadaveric specimen. The application of all data in this study was approved by the ethics committee of the UIC Office for the Protection of Research Subjects who determined that this study does not meet the definition of human subject research and is limited to cadaver specimens.
Computer Model of the Cadaveric Vertebra
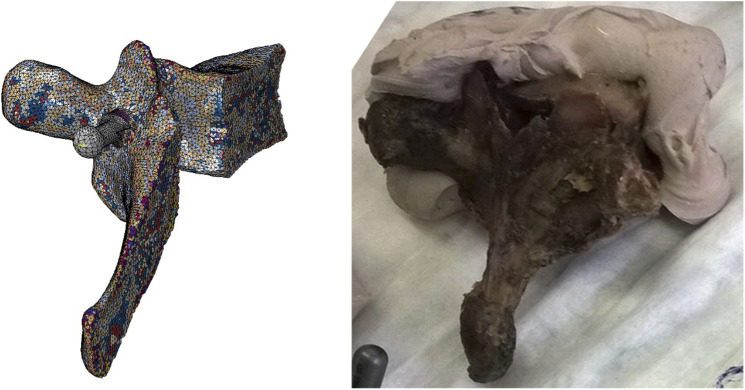
The screw was virtually implanted in a T3 vertebra selected from one of the cadaveric vertebras tested. This vertebra was chosen because previous studies have shown that T3 vertebra tolerated a wide range of screw dimensions for insertion. This selection varied from an SD/PW ratio of .55 42 to 1.16 used by Chan et al 34 When implanted with a screw in diameter of 5 mm and length of 35 mm through the anatomic approach, the cadaveric vertebra exhibited a failure load of 872.10 N (Figure 1). Following a CT scanning using a Bright Speed (GE Healthcare Technologies, Waukesha, WI, USA) scanner (slice thickness of .625 mm, pixel size of .312 mm), the vertebra was reconstructed in the Mimics Suite (Materialise, Leuven, Belgium) as shown in Figure 1A. The screw axis was evaluated through the cylinder best fitting the reconstructed hole and mirrored to the sagittal plane (see Figure1B) in the portion not damaged by the experiment. The material was assigned as elastic perfectly plastic with properties based on the Hounsfield values using the equations proposed by Giambini et al 43 A layer surrounding the screw was modeled to include a failure for shear at a value of .1. This value was found best to replicate the experimental value of the pullout load. The shear failure stress was considered because it has been previously associated with the static strength of threaded connections. 44 The contact between the screw and the bone was modeled as surface-to-surface contact with a coefficient of friction of .229,45,. 46
Figure 1.
Computer model created to simulate the pullout mechanism experimentally performed in the cadaveric vertebra on the right.
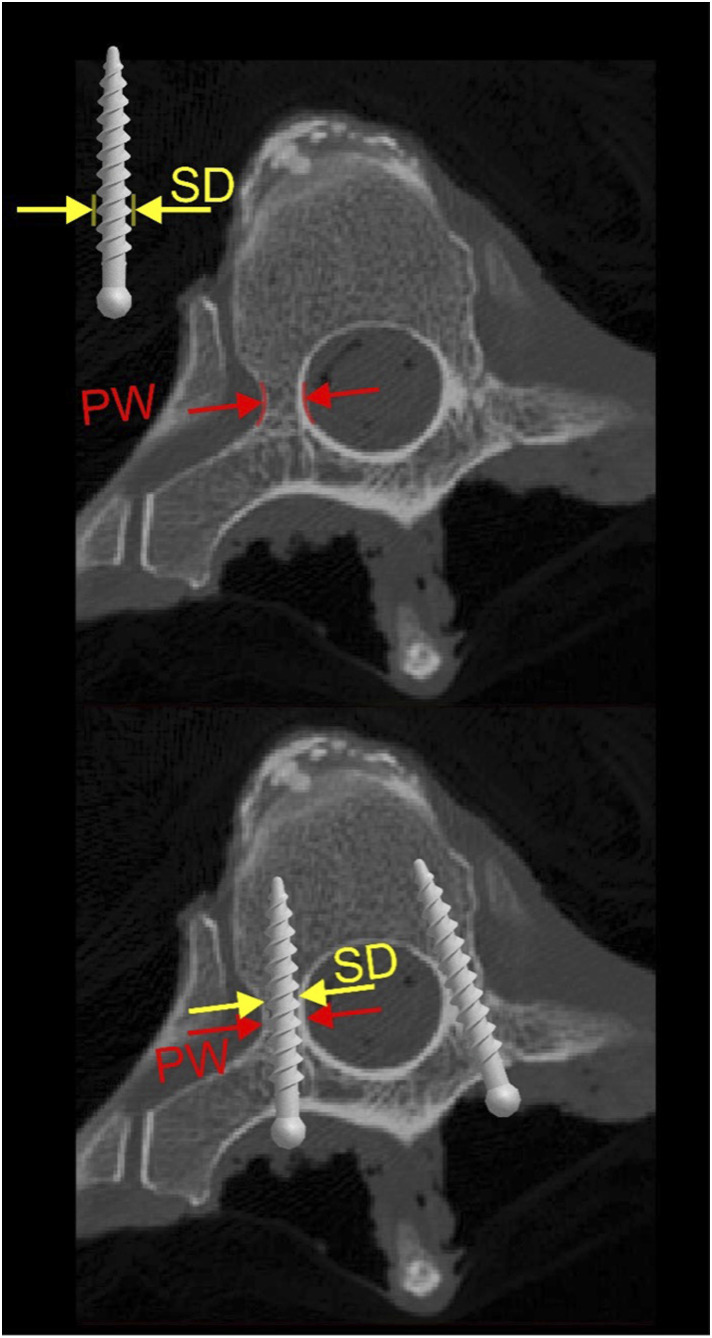
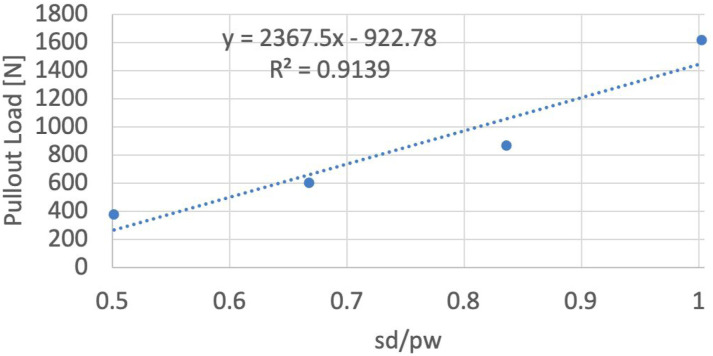
The four SD/PW ratios (see Figure 2) have been recreated by varying the screw diameter in values of 3, 4, 5, and 6 mm, scaling the screw about its longitudinal axis. With the exemption of the chips and the surrounding layer, the vertebra meshed with tetrahedral elements (C3D4), having sizes varying from 0.2 mm to 1 mm in correspondence with the external shell. To insure standard element size distribution across the implanted screw diameters, the vertebra was remeshed for each inserted screw. The screw pullout was performed applying a displacement of 1.32 mm, equivalent to half of the pitch, along the screw axis. 47 By imposing symmetrical conditions on the sagittal plane (zero transverse displacement and zero rotations) and constraining all the degree of freedom in the endplates, the articular surface of the superior facet and the edges of the inferior articular facet, the conditions simulated the restraining action of the capsular ligaments. The pullout force peaks measured in the four simulations were correlated to the values of SD/PW imposed using a linear regression model.
Figure 2.
Axial CT slice used to illustrate the pedicle width (PW) and screw diameter (SD) used for SD/PW ratio.
Cadaveric Specimens Testing
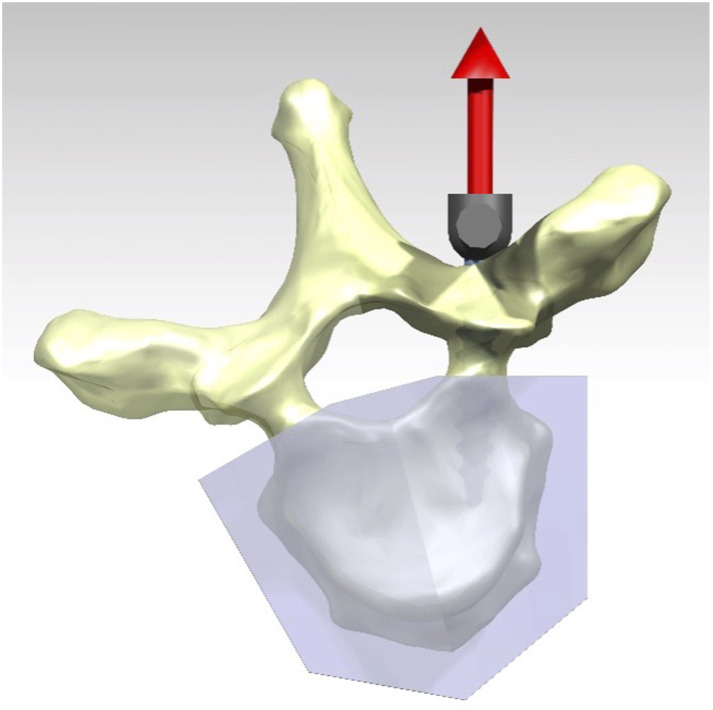
Cadaveric experiments were performed on two fresh frozen thoracic spines (T1-T10) with a similar bone mineral density (P=.122) with an average value of .906±.156 g/mm2. The harvested vertebrae were instrumented, avoiding pedicle breaches, with 30, 35, and 40 mm Depuy Expedium polyaxial screws in diameters ranging from 5 to 7 mm (DePuy Synthes, Warsaw, IN) and potted in polyester resin (Bondo Corp, Atlanta, GA). The absence of pedicle breaches was ensured by visual inspection before mechanical testing. Along the screw axis 48 a displacement at a rate of 5 mm/min was applied to the rod locked onto the screws with an Instron electromechanical system (Instron Model 5569, Instron Corp, Canton, MA) using a protocol 47 that accounts for the specifics of the ASTM F543 (see Figure 3). The data was recorded at a frequency of 100 Hz and 5N increments. Following a CT scan using BrightSpeed (GE Healthcare Technologies, Waukesha, WI, USA) scanner (slice thickness of .625 mm, pixel size of .312 mm), the vertebrae were segmented in the Mimics Suite (Materialise, Leuven, Belgium), and the pedicle dimensions were measured in their smaller section. In each section of the identified cortical shell, we measured the sagittal width, the outer width, the inner transverse widths, and the screw hole to determine the screw diameter. The cortical thickness was evaluated as half the difference between outer and inner transverse widths. Relationships between failure loads and characteristic dimensions of the pedicles were evaluated through linear regression.
Figure 3.
Experimental setup adopted for the testing of a cadaveric vertebra.
Results
Computer Model
The four screw diameters simulated resulted in SD/PW ratios varying from .50 to 1.00. All the screw dimensions had cortical bone purchase in the posterior cortex of the posterior elements. Screws in diameter of 5 and 6 mm had cortical purchase in the medial and lateral cortex of the pedicle.
The failure load ranged from 371.3 to 1601.0 N, respectively, for 3 and 6 mm screws. In the vertebra implanted with the 5 mm screw, the failure load was 866.2 N. This vertebra aimed to model the behavior of the cadaveric specimen (see Table 1).
Table 1:
Values calculated for pullout load in relation to the volume of bone purchase.
| screw diameter [mm] | 3 | 4 | 5 | 6 |
|---|---|---|---|---|
| pedicle width [mm] | 5.98 | |||
| SD/PW ratio | 0.50 | 0.67 | 0.84 | 1.00 |
| max force [N] | 371.3 | 596.6 | 866.2 | 1601.0 |
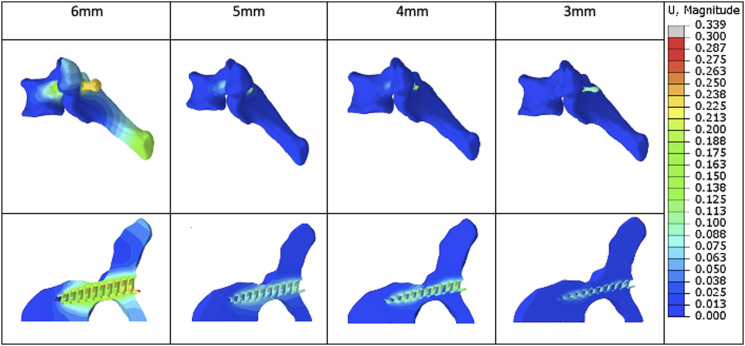
As shown in Figure 4, the screw with a diameter of 6 mm resulted in a stress pattern with values of 11.66 MPa that involved the vertebral body. It resulted in a deformation that extended throughout the entire vertebra (see Figure 33). A peak of 28.9 MPa was measured for the 6 mm screws, while, the 3 mm screw, the stress at the lateral cortex of the pedicle was negligible; however, we observed values of 15 MPa at the posterior cortex in contact with the thread. The 6 mm screw induced complete damage of the pedicle characterized by the avulsion of medial and lateral walls.
Figure 4.
Resulting vertebral deformation at peak loads measured for the four screw diameter considered.
The linear correlation between pullout load and the ratio of screw diameter over pedicle width had a coefficient of determination R2=.914 (see Figure 5).
Figure 5.
Pullout strength relation to SD/PW ratio.
Experimental Results
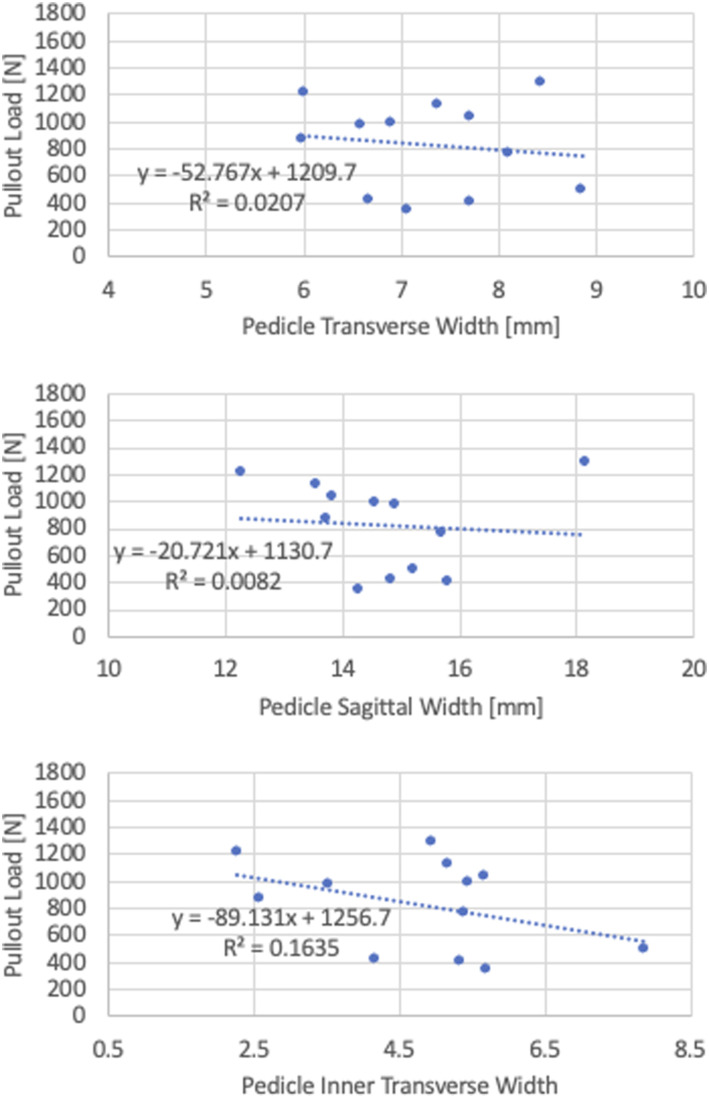
For both spines, we found that the failure load ranged from 346N to 1288N with an average of 825.4±336.1 N. The pedicle transverse width varied with 5.98 mm and 8.10, respectively, for T3 and T8 of the first spine, while the other specimen ranged from 6.91 mm in T4 to 8.86 mm in T9. The sagittal pedicle width in the first spine varied from 12.26 mm in T1 to 18.15 mm in T6. In the second spine, the variation in sagittal width was narrowed and ranged from 14.28 mm in T3 to 15.22 mm in T9. A linear correlation between the dimensions of the pedicle and the experimentally evaluated pullout load has not been found (see Figure 6). In contrast, a low determination coefficient has been found for the inner pedicle transverse width (R2=.163).
Figure 6.
Pullout force relation to pedicle dimensions.
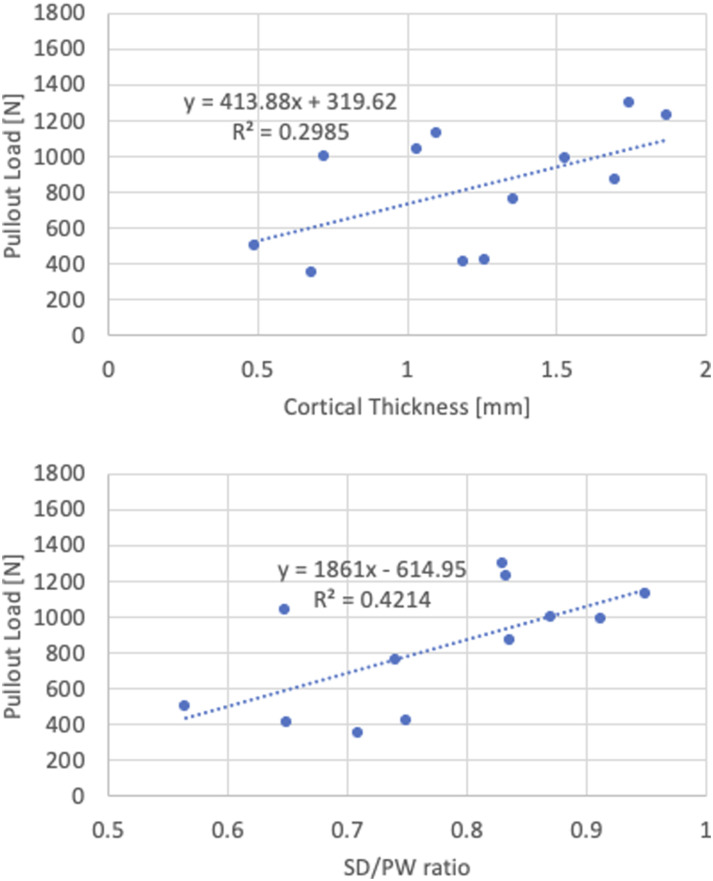
Even though the pedicle transverse and sagittal widths were not significantly different between the two spines (respectively P=.635 and .697), differences were found in terms of cortical thickness (P=.010). The first spine had a cortical thickness ranging from 1.09 mm in T7 to1.87 mm in T1, while the maximal thickness found in the second spine did not exceed 1.26 mm in T7. Considering the values from both spines, we found a weak linear relationship between the pullout load and cortical thickness with a coefficient of determination R2=.299. The coefficient of determination was increased to the value of R2=.421 when a linear relationship between pullout load and the ratio between screw diameter (SD) and pedicle width (PW) was considered. Outliers were identified in the peak loads of 1216 and 1288N found for an SD/PW ratio of .83 (Figure 7).
Figure 7.
Pullout force in relation to cortical bone thickness and SD-PW ratio.
Discussion
A commonly accepted criterion for pedicle screw selection has yet to be proposed. 49 There are research studies where primary screw selection have been suggested,10,12,28,32 but in light of our findings, additional testing supported by clinical evidence is needed. Spinal fixation requires an optimization of the pedicle screw paradigm in spine surgery. As spinal navigation and robotics become more standardized, precision and accuracy of placement of pedicle screws become evident, resulting in decreased mechanical breaches. Despite the fact that most of the pedicle breaches are asymptomatic, 50 the correlation between pullout strength and bone purchase has the potential to further improve clinical outcomes.
This study aimed to provide additional information to the surgeon in performing the screw selection to pedicle dimension to maximize biomechanical performances while avoiding pedicle breaches. We evaluated the pullout strength through computer modeling and the cadaveric testing of thoracic vertebrae. First, we simulated one T3 vertebral level and assessed the pullout strength using four different screw diameters. The failure load was highly correlated to the SD/PW ratio (R2=.914) for this particular level. Still, for SD/PW values greater than .80, there were avulsions of the medial and lateral pedicle regions. Clinically these avulsions could compromise neural structures or reduce the ultimate strength of fixation.
The limitations of the computer model proposed can be within the scope of the vertebral level we used. It only accounted for the T3 vertebral level. However, the extension of the results obtained for this particular vertebra to other spinal levels can be justified by its geometrical dimensions and by the resultant failure load. Measurements can be extrapolated to define different spine segments, but we believe this could be overcome by simply performing CT scans on all the vertebrae to be tested. The dimensions of the cadaveric vertebra tested had measures of 5.98, and 13.71 mm for width and height which are within the ranges of width (5.05±1.47 to 5.69±.80) and height 12.25±1.05 (range 8.69-15.85) reported in other morphometric studies for similar vertebral levels.18,27,33,51 A previous study has shown that T3 vertebrae have values of transverse width (5.6±1.4 mm) and sagittal widths (12.4±1.3) similar to the other upper thoracic vertebrae (T3-T7). 52 Regarding the failure load, the value of 596.57 N that we have found for the SD/PW ratio of .67 closely resembled the value of 596.0 N for an SD/PW approximating .55 found by Heller et al 42 for T3.
Further studies with various screw designs are also needed since different screw designs lead to different biomechanical strengths. 53 Furthermore, the ratio between the width and the length of the screw requires consideration due to the risk of perforating and injuring anterior vascular structures 54 and the impact of screw length on the pullout strength. 45
When we investigated pullout strength in the entire thoracic groups by performing experiments on the cadaveric vertebra, we found that the pullout was not correlated to the sagittal width, cortical bone thickness, or inner strength pedicle width. Still, it was moderately associated with the SD/PW ratio. Further examination of our experimental values obtained for all the spine segments, the lower correlation coefficient found for the relationship between pullout load and SD/PW ratio indicates a need for further studies. Therefore, our correlation is evaluated individually for each segment. However, the cadaveric experiments revealed that, among the thoracic levels, the highest pullout loads were observed for SD/PW of .83. Therefore, the moderate correlation should be considered due to the variability of vertebral morphology and bone quality among spine segments. Even though we only used vertebrae from two cadaveric specimens, we obtained pullout values in the range of 346N to 1288N with an average of 825.4±336.1 N that is comparable in terms of variability with values obtained in previous studies for the thoracic spine. Hongo et al 36 implanted 5.5 mm screws into thoracic levels T4-T9 with an SD/PW ranging from .78 to 1.15 with an average pullout strength of 672±412N. Another study evaluated the vertebral ranges of T4-T12 with varying screw diameters from 4.8-7.2. The pullout strength for the upper thoracic spine (T4-T8) was 531.7±213.8 N (224-1072N) with an SD/PW range of .52-1.67 and 807.9 ± 207N with an SD/PW range of .50-1.50 for the lower thoracic level (T9-T12). 48 Liljenqvist et al also note lateral screw penetration due to small pedicle width in certain vertebral levels.
Our findings allow a preoperative planning targeted to the maximization of the pullout load that has the potential to reduce loosening while minimizing screw diameter. Since CT measurements generally do preoperative planning for screw placements 55 and the surgeon’s decision, 22 defining a standard to guide the surgeon’s screw selection validates evidence-based medicine better than manual planning. This study is limited on quantifying the characteristics of the screw-bone interface through only the pullout strength while it must be recognized that other elements such as bone density and screw orientation play crucial role in determining the effective stability of the constructs. 47
In conclusion, for the T3 vertebra, we found a high correlation of SD/PW ratio with pullout strength. However, an SD/PW value above .84 failed from pedicle avulsion. In the cadaveric experiment, we found that the pullout load is more correlated to SD/PW than other pedicle measures and is maximized for a value of .83 without failure for pedicle avulsion. Therefore, this particular value should be considered the upper limit of the indicated SD/PW ratio at the time of surgery. Additional clinical testing is needed to identify the effective benefits of a planning tool that includes pull-out strength estimation and to validate that SD/PW approaching a value of .83 maximizes the pullout load without the potential failure for posterior arch avulsion.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The work has been partially supported by the Aurelio Caccamo Family Foundation.
ORCID iDs
Michelle C. Welborn, MD https://orcid.org/0000-0002-9422-6849
Ankit I. Mehta, MD https://orcid.org/0000-0001-6931-6095
Farid Amirouche, PhD https://orcid.org/0000-0002-3002-4199
References
- 1.Muralidhar BM, Hegde D, Hussain PSB. Management of unstable thoracolumbar spinal fractures by pedicle screws and rods fixation. J Clin Diagn Res JCDR. 2014;8(2):121-123. doi: 10.7860/JCDR/2014/5505.4025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Božík M, Magala M, Heger T, Matejička D, Baka J, Šimko P. [Pedicle screw fixation of thoracic spine fractures]. Acta Chir Orthop Traumatol Cech. 2014;81(2):140-151. [PubMed] [Google Scholar]
- 3.Sasso RC, Cotler HB, Reuben JD. Posterior fixation of thoracic and lumbar spine fractures using DC plates and pedicle screws. Spine. 1991;16(3 suppl l):S134-S139. doi: 10.1097/00007632-199103001-00019. [DOI] [PubMed] [Google Scholar]
- 4.Chen PQ. Management of scoliosis. J Formos Med Assoc Taiwan Yi Zhi. 2003;102(11):751-761. [PubMed] [Google Scholar]
- 5.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20(12):1399-1405. [PubMed] [Google Scholar]
- 6.Zheng CK, Kan WS, Li P, Zhao ZG, Li K. Treatment for severe idiopathic upper thoracic scoliosis in adolescence. J Spinal Disord Tech. 2013;26(2):107-111. doi: 10.1097/BSD.0b013e31824b7577. [DOI] [PubMed] [Google Scholar]
- 7.Abumi K, Shono Y, Taneichi H, Ito M, Kaneda K. Correction of cervical kyphosis using pedicle screw fixation systems. Spine. 1999;24(22):2389. doi: 10.1097/00007632-199911150-00017. [DOI] [PubMed] [Google Scholar]
- 8.Abumi K, Kaneda K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine. 1997;22(16):1853-1863. [DOI] [PubMed] [Google Scholar]
- 9.Chang KW. Oligosegmental correction of post-traumatic thoracolumbar angular kyphosis. Spine. 1993;18(13):1909-1915. doi: 10.1097/00007632-199310000-00032. [DOI] [PubMed] [Google Scholar]
- 10.Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine. 2001;26(18):2049-2057. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 11.Wu SS, Hwa SY, Lin LC, Pai WM, Chen PQ, Au MK. Management of rigid post-traumatic kyphosis. Spine. 1996;21(19):2260-2266. doi: 10.1097/00007632-199610010-00016. [DOI] [PubMed] [Google Scholar]
- 12.Di Silvestre M, Parisini P, Lolli F, Bakaloudis G. Complications of thoracic pedicle screws in scoliosis treatment. Spine. 2007;32(15):1655-1661. doi: 10.1097/BRS.0b013e318074d604. [DOI] [PubMed] [Google Scholar]
- 13.Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am. 1999;81(11):1519-1528. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 14.West JL, Ogilvie JW, Bradford DS. Complications of the variable screw plate pedicle screw fixation. Spine. 1991;16(5):576-579. doi: 10.1097/00007632-199105000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine. 1993;18(15):2231-2238. doi: 10.1097/00007632-199311000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Faraj AA, Webb JK. Early complications of spinal pedicle screw. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 1997;6(5):324-326. doi: 10.1007/BF01142678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alhabib H, Nataraj A, Khashab M, Mahood J, Kortbeek F, Fox R. Pedicle screw insertion in the thoracolumbar spine: comparison of 4 guidance techniques in the intact cadaveric spine: Laboratory investigation. J Neurosurg Spine. 2011;14(5):664-669. doi: 10.3171/2010.11.SPINE10177. [DOI] [PubMed] [Google Scholar]
- 18.Bunmaprasert T, Roobsoong A, Pongmanee S, Khunsree S, Laowatthanaphong S. Safety entry point, size and direction for placement of thoracic pedicle screw--a cadaveric study. J Med Assoc Thail Chotmaihet Thangphaet. 2014;97(12):1344-1351. [PubMed] [Google Scholar]
- 19.Chaynes P, Sol JC, Vaysse P, Bécue J, Lagarrigue J. Vertebral pedicle anatomy in relation to pedicle screw fixation: a cadaver study. Surg Radiol Anat SRA. 2001;23(2):85-90. doi: 10.1007/s00276-001-0085-z. [DOI] [PubMed] [Google Scholar]
- 20.Lehman RA, Polly DW, Kuklo TR, Cunningham B, Kirk KL, Belmont PJ. Straight-forward versus anatomic trajectory technique of thoracic pedicle screw fixation: a biomechanical analysis. Spine. 2003;28(18):2058-2065. doi: 10.1097/01.BRS.0000087743.57439.4F. [DOI] [PubMed] [Google Scholar]
- 21.Takeshita K, Maruyama T, Chikuda H, et al. Diameter, length, and direction of pedicle screws for scoliotic spine: analysis by multiplanar reconstruction of computed tomography. Spine. 2009;34(8):798-803. doi: 10.1097/BRS.0b013e3181895c36. [DOI] [PubMed] [Google Scholar]
- 22.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29(3):333-342. doi: 10.1097/01.brs.0000109983.12113.9b. [DOI] [PubMed] [Google Scholar]
- 23.Allam Y, Silbermann J, Riese F, Greiner-Perth R. Computer tomography assessment of pedicle screw placement in thoracic spine: comparison between free hand and a generic 3D-based navigation techniques. Eur Spine J. 2013;22(3):648-653. doi: 10.1007/s00586-012-2505-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boon Tow BP, Yue WM, Srivastava A, et al. Does Navigation Improve Accuracy of Placement of Pedicle Screws in Single-level Lumbar Degenerative Spondylolisthesis?: A Comparison Between Free-hand and Three-dimensional O-Arm Navigation Techniques. J Spinal Disord Tech. 2015;28(8):E472-E477. doi: 10.1097/BSD.0b013e3182a9435e. [DOI] [PubMed] [Google Scholar]
- 25.Braga BP, de Morais JV, Vilela MD. Free-hand placement of high thoracic pedicle screws with the aid of fluoroscopy: evaluation of positioning by CT scans in a four-year consecutive series. Arq Neuropsiquiatr. 2010;68(3):390-395. doi: 10.1590/s0004-282x2010000300012. [DOI] [PubMed] [Google Scholar]
- 26.Bydon M, Xu R, Amin AG, et al. Safety and efficacy of pedicle screw placement using intraoperative computed tomography: consecutive series of 1148 pedicle screws. J Neurosurg Spine. 2014;21(3):320-328. doi: 10.3171/2014.5.SPINE13567. [DOI] [PubMed] [Google Scholar]
- 27.Christodoulou AG, Apostolou T, Ploumis A, Terzidis I, Hantzokos I, Pournaras J. Pedicle dimensions of the thoracic and lumbar vertebrae in the Greek population. Clin Anat N Y N. 2005;18(6):404-408. doi: 10.1002/ca.20155. [DOI] [PubMed] [Google Scholar]
- 28.Misenhimer GR, Peek RD, Wiltse LL, Rothman SL, Widell EH. Anatomic analysis of pedicle cortical and cancellous diameter as related to screw size. Spine. 1989;14(4):367-372. doi: 10.1097/00007632-198904000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Bianco RJ, Arnoux PJ, Wagnac E, Mac-Thiong JM, Aubin CÉ. Minimizing Pedicle Screw Pullout Risks: A Detailed Biomechanical Analysis of Screw Design and Placement. Clin Spine Surg Spine Publ. 2017;30(3):E226-E232. doi: 10.1097/BSD.0000000000000151. [DOI] [PubMed] [Google Scholar]
- 30.Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine. 2007;32(3):E111-E120. doi: 10.1097/01.brs.0000254048.79024.8b. [DOI] [PubMed] [Google Scholar]
- 31.Matsukawa K, Yato Y, Imabayashi H, Hosogane N, Asazuma T, Nemoto K. Biomechanical evaluation of the fixation strength of lumbar pedicle screws using cortical bone trajectory: a finite element study. J Neurosurg Spine. 2015;23(4):471-478. doi: 10.3171/2015.1.SPINE141103. [DOI] [PubMed] [Google Scholar]
- 32.Gstoettner M, Lechner R, Glodny B, Thaler M, Bach CM. Inter- and intraobserver reliability assessment of computed tomographic 3D measurement of pedicles in scoliosis and size matching with pedicle screws. Eur Spine J. 2011;20(10):1771-1779. doi: 10.1007/s00586-011-1908-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liau KM, Yusof MI, Abdullah MS, Abdullah S, Yusof AH. Computed tomographic morphometry of thoracic pedicles: safety margin of transpedicular screw fixation in malaysian malay population. Spine. 2006;31(16):E545-E550. doi: 10.1097/01.brs.0000225978.97652.e0. [DOI] [PubMed] [Google Scholar]
- 34.Chan CYW, Kwan MK, Saw LB. Thoracic pedicle screw insertion in Asian cadaveric specimen: does radiological pedicle profile affect outcome? Surg Radiol Anat. 2011;33(1):19-25. doi: 10.1007/s00276-010-0726-1. [DOI] [PubMed] [Google Scholar]
- 35.Hart RA, Hansen BL, Shea M, Hsu F, Anderson GJ. Pedicle screw placement in the thoracic spine: a comparison of image-guided and manual techniques in cadavers. Spine. 2005;30(12):E326-E331. doi: 10.1097/01.brs.0000166621.98354.1d. [DOI] [PubMed] [Google Scholar]
- 36.Hongo M, Ilharreborde B, Gay RE, et al. Biomechanical evaluation of a new fixation device for the thoracic spine. Eur Spine J. 2009;18(8):1213-1219. doi: 10.1007/s00586-009-0999-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kretzer RM, Chaput C, Sciubba DM, et al. A computed tomography-based morphometric study of thoracic pedicle anatomy in a random United States trauma population. J Neurosurg Spine. 2011;14(2):235-243. doi: 10.3171/2010.9.SPINE1043. [DOI] [PubMed] [Google Scholar]
- 38.Fujimoto T, Sei A, Taniwaki T, Okada T, Yakushiji T, Mizuta H. Pedicle screw diameter selection for safe insertion in the thoracic spine. Eur J Orthop Surg Traumatol. 2012;22(5):351-356. doi: 10.1007/s00590-011-0846-2. [DOI] [Google Scholar]
- 39.Vaccaro AR, Rizzolo SJ, Allardyce TJ, et al. Placement of pedicle screws in the thoracic spine. Part I: Morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77(8):1193-1199. doi: 10.2106/00004623-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 40.Sandén B, Olerud C, Petrén-Mallmin M, Johansson C, Larsson S. The significance of radiolucent zones surrounding pedicle screws: DEFINITION OF SCREW LOOSENING IN SPINAL INSTRUMENTATION. J Bone Joint Surg Br. 2004;86-B(3):457-461. doi: 10.1302/0301-620X.86B3.14323. [DOI] [PubMed] [Google Scholar]
- 41.Parker SL, McGirt MJ, Farber SH, et al. Accuracy of free-hand pedicle screws in the thoracic and lumbar spine: analysis of 6816 consecutive screws. Neurosurgery. 2011;68(1):170-178. doi: 10.1227/NEU.0b013e3181fdfaf4. [DOI] [PubMed] [Google Scholar]
- 42.Heller JG, Shuster JK, Hutton WC. Pedicle and transverse process screws of the upper thoracic spine. Biomechanical comparison of loads to failure. Spine. 1999;24(7):654-658. doi: 10.1097/00007632-199904010-00008. [DOI] [PubMed] [Google Scholar]
- 43.Giambini H, Qin X, Dragomir-Daescu D, An KN, Nassr A. Specimen-specific vertebral fracture modeling: a feasibility study using the extended finite element method. Med Biol Eng Comput. 2016;54(4):583-593. doi: 10.1007/s11517-015-1348-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brickford J. An Introduction to the Design and Behavior of Bolted Joints. John H. Bickford. - Vanderbilt University. https://catalog.library.vanderbilt.edu/discovery/fulldisplay/alma991031710399703276/01VAN_INST:vanui Accessed April 18, 2022. [Google Scholar]
- 45.Chatzistergos PE, Magnissalis EA, Kourkoulis SK. A parametric study of cylindrical pedicle screw design implications on the pullout performance using an experimentally validated finite-element model. Med Eng Phys. 2010;32(2):145-154. doi: 10.1016/j.medengphy.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 46.Liu S, Qi W, Zhang Y, Wu ZX, Yan YB, Lei W. Effect of bone material properties on effective region in screw-bone model: an experimental and finite element study. Biomed Eng Online. 2014;13:83. doi: 10.1186/1475-925X-13-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Amirouche F, Solitro GF, Magnan BP. Stability and Spine Pedicle Screws Fixation Strength-A Comparative Study of Bone Density and Insertion Angle. Spine Deform. 2016;4(4):261-267. doi: 10.1016/j.jspd.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 48.Liljenqvist U, Hackenberg L, Link T, Halm H. Pullout strength of pedicle screws versus pedicle and laminar hooks in the thoracic spine. Acta Orthop Belg. 2001;67(2):157-163. [PubMed] [Google Scholar]
- 49.Solitro GF, Whitlock K, Amirouche F, Mehta AI, Mcdonnell A. Currently Adopted Criteria for Pedicle Screw Diameter Selection. Internet J Spine Surg. 2019;13(2):132-145. doi: 10.14444/6018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Smith ZA, Sugimoto K, Lawton CD, Fessler RG. Incidence of lumbar spine pedicle breach after percutaneous screw fixation: a radiographic evaluation of 601 screws in 151 patients. J Spinal Disord Tech. 2014;27(7):358-363. doi: 10.1097/BSD.0b013e31826226cb. [DOI] [PubMed] [Google Scholar]
- 51.Yu CC, Bajwa NS, Toy JO, Ahn UM, Ahn NU. Pedicle morphometry of upper thoracic vertebrae: an anatomic study of 503 cadaveric specimens. Spine. 2014;39(20):E1201-E1209. doi: 10.1097/BRS.0000000000000505. [DOI] [PubMed] [Google Scholar]
- 52.Zindrick MR, Wiltse LL, Doornik A, et al. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine. 1987;12(2):160-166. doi: 10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]
- 53.Christodoulou E, Chinthakunta S, Reddy D, et al. Axial pullout strength comparison of different screw designs: fenestrated screw, dual outer diameter screw and standard pedicle screw. Scoliosis. 2015;10:15. doi: 10.1186/s13013-015-0039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kakkos SK, Shepard AD. Delayed presentation of aortic injury by pedicle screws: report of two cases and review of the literature. J Vasc Surg. 2008;47(5):1074-1082. doi: 10.1016/j.jvs.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 55.Tian NF, Huang QS, Zhou P, et al. Pedicle screw insertion accuracy with different assisted methods: a systematic review and meta-analysis of comparative studies. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2011;20(6):846-859. doi: 10.1007/s00586-010-1577-5. [DOI] [PMC free article] [PubMed] [Google Scholar]