Abstract
Study Design
Retrospective cohort study.
Objectives
This study aimed to explore the effect of preoperative cervical spondylosis on the heterotopic ossification (HO) formation in different locations after cervical disc replacement (CDR).
Methods
The degree of preoperative cervical spondylosis was evaluated radiologically, including the intervertebral disc, uncovertebral joints, facet joints and ligaments. The effects of cervical spondylosis on the HO formation after CDR were analyzed according to the location of HO. Multivariate logistic regression was performed to identify the independent factors.
Results
149 patients with a total of 196 arthroplasty segments were involved in this study. HO, anterior HO (AHO), and posterior HO (PHO) developed in 59.69%, 22.96%, and 41.84% levels, respectively. The significant factors in univariate analysis for PHO after CDR included the disc height loss, anterior osteophytes, preoperative uncovertebral joint osteophytes and facet joint degeneration. The incidence of adjacent segment degeneration (ASD) was significantly higher in the PHO group compared to that without PHO at the last follow-up (P = .003). The disc height loss in high-grade HO was significantly more than that in low-grade group (P = .039). Multivariate analysis identified disc height loss was the only independent factor for PHO (P = .009). No significant degenerative factors related to the formation of AHO were found.
Conclusions
Preoperative cervical spondylosis predominantly affected the HO formation in the posterior disc space after CDR. The disc height loss was an independent risk factor for PHO formation. Rigorous criteria for the extent of preoperative disc height loss should be used when selecting appropriate candidates for CDR.
Keywords: cervical disc replacement, cervical spondylosis, heterotopic ossification, intervertebral disc height
Introduction
Cervical disc replacement (CDR) is a relatively new technique in cervical spine surgery as an alternative treatment to anterior cervical discectomy and fusion (ACDF) for cervical degenerative disc disease at 1 or more levels. The initial design concept of CDR is to preserve motion of the index level and diminish the adjacent segments’ stress transfer, which theoretically reduce degeneration at the adjacent levels compared to ACDF.1-3 Unfortunately, heterotopic ossification (HO) raised as an adverse outcome after CDR that may decrease the motion of index level and even develop to complete intervertebral fusion, which is against the design philosophy of disc replacement with motion-preserving. 4 An extensive body of literatures have emerged to investigate the incidence, predisposing factors and clinical implications since the phenomenon was noted. However, the underlying mechanism of HO has not been clearly elucidated until present.
Degenerative cervical spondylosis refers to age-related wear and tear that affect elements of the cervical spine over time, including the intervertebral discs, facet joints, and other connective-tissue structures. 5 Preoperative degenerative spondylosis is considered 1 of the contributors to HO formation after CDR. Wu et al. 6 reported that the rate of HO formation was significantly higher in patients with spondylosis compared to that with soft-disc herniations. In recent years, several qualitative or quantitative studies confirmed the degree of degeneration in the surgical level was positively correlated with postoperative HO,7-10 whilst some studies found preoperative degenerative changes exert no significant influence on the occurrence of HO.11,12 However, few studies investigated the effect of all the components of cervical spondylosis on HO. When evaluating the degenerative degree of cervical spondylosis, most investigations tended to involve the intervertebral discs and ligament elements, the effects of degeneration in uncovertebral joint and facet joint have been rarely studied. Chung et al. 13 identified preoperative uncovertebral hypertrophy as a significant risk factor for the occurrence of motion-affecting HO through a survivorship analysis. Cao et al. 14 found there was significant positive correlation between preoperative uncovertebral joints degeneration and HO. Due to the interdependent process among disc degeneration, uncovertebral joint degeneration and facet joint degeneration, the independent factors in preoperative spondylosis causing HO formation was still unclear. Furthermore, previous studies suggested that the mechanism of HO in anterior and posterior disc space may be different.15,16. The impacts of preoperative spondylosis on the occurrence of HO in different location has been poorly studied.
In the current study, preoperative spondylosis of intervertebral disc, uncovertebral joint, facet joint and ligament elements were comprehensively evaluated in patients who underwent CDR with a minimum follow-up of 24 months. This study aimed to investigate the influences of preoperative spondylosis at surgical segment on postoperative HO, and to explore whether the influence of degeneration on HO formation in anterior and posterior disc space is different.
Methods
Patient Population
This was a retrospective study and the study protocol was approved by the Ethics Committee of West China Hospital of Sichuan University (Project License Number 20190946). All patients provided written informed consent. Patients who underwent single-level and two-level cervical disc replacement using the Prestige-LP (Medtronic Sofamor Danek USA, Inc., Memphis, Tennessee, USA) from 2009 to 2018 and had a minimum of 2 years of follow-up data were included in this study. The inclusion criteria were as follows: 1) 18-65 years old; 2) single- or 2-level cervical disc disease causing symptomatic radiculopathy or myelopathy between C3 and C7; 3) failure of conservative treatment for at least 12 weeks. The exclusion criteria consisted of: 1) instability, irreducible kyphosis, or severe degeneration at the surgical segment; 2) ossification of the posterior longitudinal ligament; 3) ankylosing spondylitis, rheumatoid arthritis, or other autoimmune or metabolic bone disease; 4) osteoporosis (T-score ≤ -2.5); 5) prior cervical spine surgery.
Surgical Techniques
All operations were performed by the same senior spine surgeon. The patient was placed with the neck in a neutral position after general anesthesia, and a right-side Smith-Robinson approach was performed at the index level. After exposure, the anterior longitudinal ligament, intervertebral disc, posterior longitudinal ligament and osteophytes were removed to achieve a complete discectomy and decompression. A high-speed burr was used to carefully prepare the endplate and a trial implant was used to determine the size of prosthesis. Then, a rail cutter guide and bit were used to drill the fixation channels in the endplate and a correctly sized Prestige-LP disc was inserted into the prepared intervertebral space. After verification of the proper placement of implant through anterior-posterior and lateral fluoroscopy, copious irrigation with normal saline was used to wash away the bone dust during endplate preparation in every case. The same procedure was performed at other level in patients with double segmental lesions. A drainage tube was inserted after meticulous hemostasis before closing the incision. Nonsteroidal anti-inflammatory drugs were not routinely used in this cohort.
Radiological Evaluation
All the radiological data were collected preoperatively, 1 week and at last follow-up postoperatively. The degeneration degree of the index level was evaluated preoperatively in the neutral lateral radiographs using a quantitative scoring system proposed by Walraevens et al., 17 which consists of height loss (score 0-4), anterior osteophytes (score 0-3) and endplate sclerosis (score 0-2), with higher scores representing more severe degeneration. Height loss is defined as the middle disc height with respect to a normal middle disc height at an adjacent level. Anterior osteophytes are assessed through its length relative to the anteroposterior diameter of the middle of the corresponding vertebral body. The endplate sclerosis is distinguished among no apparent sclerosis, just detectable and definite sclerosis according to the degree of detectability.10,17 The uncovertebral joint was assessed preoperatively using the coronal reconstruction computed tomography (CT) to identify osteophytes at the uncovertebral joint area. Facet joint degeneration was evaluated using a computed tomographic grading system reported by Park et al. 11 (grade 1-4), with higher grade denoting more advanced degree of degeneration. HO was graded based on the McAfee classification criteria and classified into low-grade (grade 1-2) and high-grade HO (grade 3-4). 7 According to the location of HO on lateral neutral radiographs, index segments were divided into anterior heterotopic ossification (AHO) and non-AHO groups, posterior heterotopic ossification (PHO) and non-PHO groups, respectively 15 (Figure 1). Adjacent segment degeneration (ASD) was defined by the presence of at least 1 of the following conditions7,18: 1) new anterior or enlarging osteophyte formation, 2) narrowing of the disc space ≥ 10% compared to preoperative radiographs, 3) ossification of the anterior longitudinal ligament (OALL). The ligamentum nuchae ossification progression was defined as new or enlarging ossification of ligamentum nuchae at last follow-up compared with pre-operation. Shell angle was defined as the angle formed between the superior and inferior endplate of the prosthesis, and segmental range of motion (ROM) was measured on the flexion-extension radiographs. The above assessments were performed by 2 surgeons independently, and the discrepancies were settled by consulting a senior surgeon to achieve consensus.
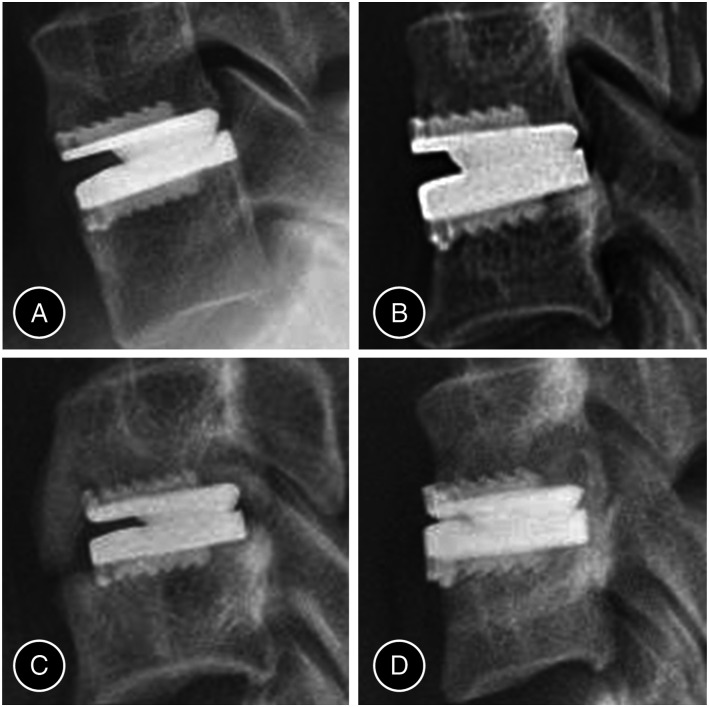
Figure 1.
Low-grade heterotopic ossification (HO): anterior HO (AHO) (A) and posterior HO (PHO) (B). High-grade HO: both AHO and PHO (C), and PHO (D). Abbreviation: HO, heterotopic ossification; AHO, anterior heterotopic ossification, PHO, posterior heterotopic ossification.
Clinical Outcomes
Clinical outcomes were assessed using the Japanese Orthopaedic Association (JOA) score, Neck Disability Index (NDI) functional score, and visual analog scale (VAS) score. The JOA score was used to evaluated the neurological status of patients with myelopathy, the NDI score was used to assess the function of the neck, and the VAS score was used to assess the neck and arm pain of the patients. The data were collected preoperatively and at the last follow-up postoperatively.
Statistical Analysis
Statistical analyses were performed using SPSS Version 25.0 software (IBM Corp., Armonk, New York, USA). The results were presented as mean ± standard deviation for continuous variables and number of cases and percentage for categorical variables. A paired t-test was used to compare pre- and post-operative parameters. The independent t-test or the Mann-Whitney U test was used to compare continuous variables depending on the normality of data. The Chi-square or Fisher’s exact test was used for categorical variables. A binary logistic regression analysis was used to identify risk factors for HO. Variables with P < .10 in the univariate analysis were included in the multivariate logistic regression analysis. Due to the lack of eligible variable in AHO group, variables with P < .15 in the univariate analysis were in included in the multivariate analysis. A 2-tailed P-values < .05 was considered statistically significant.
Results
Demographic Data
This retrospective study included 149 patients (64 male, 85 female) with a minimum 24 months follow-up data. The mean age of the patients was 43.32 ± 8.24 years. The median follow-up time was 41.0 months (25% quartile: 35.0, 75% quartile: 56.0 months; range 24-131 months). A total of 196 segments in 149 patients were evaluated, of whom 102 patients underwent single-level and 47 patients underwent 2-level CDR. The most common operated level was C5/6 (n = 116), followed by C4/5 (n = 42), C6/7 (n = 26) and C3/4 (n = 12). Overall, HO was diagnosed in 88 levels (constituent ratio: 44.90%) with low-grade HO and 29 levels (constituent ratio: 14.80%) with high-grade HO were identified. AHO occurred in 43 patients and in 45 levels (22.96%) and PHO was observed in 68 patients and in 82 levels (41.84%). The clinical outcomes including the JOA, NDI, VAS neck and VAS arm scores showed significant improvement at last follow-up compared to pre-operation (Table 1). No patients required a reoperation at the surgical level or adjacent levels during the course of this study.
Table 1.
Demographic Data.
| Variable | Value |
|---|---|
| Number of patients (segments) | 149 (196) |
| Age (years) | 43.32 ± 8.24 |
| Sex | |
| Male | 64 |
| Female | 85 |
| Follow-up (months) | 48.95 ± 23.14 |
| CDR level | |
| 1 | 102 |
| 2 | 47 |
| Level distribution | |
| C3/4 | 12 |
| C4/5 | 42 |
| C5/6 | 116 |
| C6/7 | 26 |
| JOA score | |
| Preoperative | 12.17 ± .95 |
| Last follow-up | 15.98 ± .66* |
| NDI score | |
| Preoperative | 22.43 ± 3.26 |
| Last follow-up | 5.66 ± .60* |
| VAS neck score | |
| Preoperative | 5.87 ± .50 |
| Last follow-up | 1.58 ± .51* |
| VAS arm score | |
| Preoperative | 5.68 ± .79 |
| Last follow-up | .97 ± .53* |
Abbreviation: CDR, cervical disc replacement; JOA, Japanese Orthopaedic Association; NDI, neck disability index; VAS, visual analog scale.
*Significant difference compared with the preoperative values.
Univariate Analysis of HO According to the Location and the Influence on clinical Outcomes
All the index level were divided into AHO and non-AHO group, PHO and non-PHO group, respectively, according to the location of HO occurrence. The factors of age, sex, follow-up time, level distribution and the assessment of preoperative spondylosis were involved in the univariate analysis. For the analysis of AHO, no significant factors were found. The degree of overall disc degeneration, disc height loss, anterior osteophytes were significantly higher in the PHO group than in the non-PHO group (P<.001 for overall disc degeneration score; P=.003 for mean disc height loss score; P=.006 for mean anterior osteophyte score) (Figure 2). Similarly, the presence of preoperative uncovertebral joint osteophytes and facet joint degeneration were also significantly frequent in the PHO group compared to non-PHO group (P = .045 for uncovertebral joint osteophyte; P = .035 for facet joint degeneration). There was no significant difference in the shell angle or ROM postoperatively neither comparing the AHO and non-AHO group nor the PHO and non-PHO group. At the last follow-up, the ROM at index level was significantly lower in the PHO group than the non-PHO group (6.92 ± 4.43 vs 8.81 ± 4.82, P = .003) while that in AHO group was lower compared to non-AHO group, but the difference was not significant (6.95 ± 5.18 vs 8.35 ± 4.58, P = .053). In addition, the incidence of ASD was significantly higher in the group with PHO compared to that without PHO (32.9% vs 14.9%, P = .003) at the last follow-up (Figure 3) (Table 2). There were no significant differences in JOA, NDI, VAS scores between patients with and without AHO, and patients with and without PHO at the last follow-up. Although larger ROM of C2-C7 was noted in patients without AHO than those with AHO and patients without PHO than those with PHO, the differences were not statistically significant at the last follow-up. The incidence of ASD was significantly higher in patients with PHO compared with those without PHO (41.2% vs 18.5%, P = .002) (Table 3).
Figure 2.
A 46-year-old woman who underwent cervical disc replacement using Prestige-LP at the C5/6 level. The preoperative lateral radiograph showed that a decreased intervertebral disc height, anterior osteophyte and ossification of anterior longitudinal ligament (OALL) at C5/6 level (A). The preoperative coronal reconstruction computed tomography (CT) images indicated the uncovertebral joint osteophyte (B). The preoperative magnetic resonance image (MRI) showed cervical spondylosis at the C5/6 level (C). One week postoperatively, lateral radiograph showed cervical disc replacement at C5/6 level (D). At 50 months follow-up, neutral X-ray (E), magnified view of C5/6 region (F) and dynamic X-rays indicated low-grade posterior heterotopic ossification at the C5/6 level and the range of motion of the prosthesis was 13.19° (G and H).
Figure 3.
A 52-year-old man who underwent cervical disc replacement using Prestige-LP at the C5/6 level. The preoperative lateral radiograph showed that a decreased intervertebral disc height, anterior osteophyte and ossification of anterior longitudinal ligament at C5/6 level (A). The preoperative coronal reconstruction computed tomograph images indicated the uncovertebral joint osteophyte (B). The preoperative MRI showed cervical spondylosis at the C5/6 level (C). One week postoperatively, lateral radiograph showed cervical disc replacement at C5/6 level (D). At 40 months follow-up, neutral X-ray (E), magnified view of C5/6 region (F) and dynamic X-rays (G and H) indicated high-grade posterior heterotopic ossification at the C5/6 level with limited prosthesis mobility and newly formed anterior osteophytes at caudal adjacent segment. The range of motion of the prosthesis was 3.07°.
Table 2.
Univariate Analysis of Heterotopic Ossification of Each Segment Depending on the Location at Last Follow-up.
| AHO | PHO | |||||
|---|---|---|---|---|---|---|
| (−) n=151 | (+) n=45 | P | (−) n=114 | (+) n=82 | P | |
| Age | 43.93 ± 8.34 | 42.16 ± 7.68 | .203 | 42.76 ± 8.20 | 44.59 ± 8.14 | .236 |
| Sex | .301 | .908 | ||||
| Male | 64 | 23 | 51 | 36 | ||
| Female | 87 | 22 | 63 | 46 | ||
| Follow-up (months) | 47.84 ± 21.62 | 54.82 ± 29.69 | .498 | 47.48 ± 20.53 | 52.17 ± 27.64 | .882 |
| Level distribution | .384 | .309 | ||||
| C3/4 | 9 | 3 | 8 | 4 | ||
| C4/5 | 35 | 7 | 20 | 22 | ||
| C5/6 | 90 | 26 | 68 | 48 | ||
| C6/7 | 17 | 9 | 18 | 8 | ||
| Overall degree of disc degeneration | 1.53 | 1.67 | .723 | 1.25 | 2.00 | <.001* |
| Mean height loss score | .54 | .49 | .718 | .39 | .71 | .003 * |
| Mean anterior osteophyte score | .79 | .96 | .256 | .68 | 1.04 | .006 * |
| Mean endplate sclerosis score | .20 | .22 | .687 | .17 | .26 | .196 |
| Pre-op posterior osteophyte | .339 | .278 | ||||
| Yes | 76 (50.3%) | 19 (42.2%) | 59 (51.8%) | 36 (43.9%) | ||
| No | 75 (49.7%) | 26 (57.8%) | 55 (48.2%) | 46 (56.1%) | ||
| Pre-op uncovertebral joint osteophyte | .575 | .045 * | ||||
| Yes | 81 (53.6%) | 22 (48.9%) | 53 (46.5%) | 50 (61.0%) | ||
| No | 70 (46.4%) | 23 (51.1%) | 61 (53.5%) | 32 (39.0%) | ||
| Facet joint degeneration | .720 | .035 * | ||||
| 1 | 117 (77.5%) | 36 (80.0%) | 95 (83.3%) | 58 (70.7%) | ||
| 2 | 34 (22.5%) | 9 (20.0%) | 19 (16.7%) | 24 (29.3%) | ||
| OALL | 26 (17.2%) | 10 (22.2%) | .447 | 21 (18.4%) | 15 (18.3%) | .982 |
| Pre-op ligamentum nuchae ossification | 28 (18.5%) | 4 (8.9%) | .124 | 14 (12.3%) | 18 (22.0%) | .071 |
| Progression of ligamentum nuchae | 13 (8.6%) | 4 (8.9%) | 1.000 | 8 (7.0%) | 9 (11.0%) | .331 |
| Post-op | ||||||
| Shell angle (°) | 4.94 ± 4.79 | 3.70 ± 5.17 | .137 | 4.86 ± 5.04 | 4.38 ± 4.69 | .739 |
| ROM at index level (°) | 6.77 ± 3.70 | 7.55 ± 3.59 | .144 | 6.90 ± 3.74 | 7.02 ± 3.61 | .757 |
| Last follow-up | ||||||
| Shell angle (°) | 1.64 ± 4.59 | 1.92 ± 5.67 | .739 | 2.13 ± 4.86 | 1.12 ± 4.80 | .151 |
| ROM at index level (°) | 8.32 ± 4.58 | 6.95 ± 5.16 | .053 | 8.81 ± 4.82 | 6.88 ± 4.42 | .003* |
| Changes of ROM | 1.55 ± 5.25 | −.60 ± 6.44* | .024 | 1.91 ± 5.80 | −.14 ± 5.11 | .011* |
| ASD | 32 (21.2%) | 12 (26.7%) | .440 | 17 (14.9%) | 27 (32.9%) | .003* |
Abbreviation: AHO, anterior heterotopic ossification; PHO, posterior heterotopic ossification; OALL, ossification of anterior longitudinal ligament; post-op, values at 1 week after surgery; ROM, range of motion; ASD, adjacent segment degeneration.
Bold values indicate these values would be included in multivariable logistic regression analysis.
*Significant difference between groups.
Table 3.
Clinical Outcomes of Patients with or Without Anterior Heterotopic Ossification and Patients with or Without Posterior Heterotopic Ossification at Last sollow-up.
| AHO | PHO | |||||
|---|---|---|---|---|---|---|
| (−) n=106 | (+) n=43 | P | (−) n=81 | (+) n=68 | P | |
| JOA score | 15.95 ± .64 | 16.08 ± .76 | .555 | 16.04 ± .69 | 15.92 ± .64 | .530 |
| NDI score | 5.69 ± .61 | 5.60 ± .58 | .537 | 5.65 ± .60 | 5.68 ± .61 | .672 |
| VAS neck score | 1.60 ± .51 | 1.53 ± .50 | .474 | 1.54 ± .50 | 1.63 ± .52 | .314 |
| VAS arm score | .97 ± .53 | .95 ± .53 | .847 | .93 ± .59 | 1.01 ± .44 | .289 |
| ROM of C2-C7 | 50.79 ± 12.99 | 46.59 ± 13.13 | .077 | 51.29 ± 12.55 | 47.53 ± 13.59 | .081 |
| ASD | 27 (25.5%) | 16 (37.2%) | .152 | 15 (18.5%) | 28 (41.2%) | .002* |
Abbreviation: AHO, anterior heterotopic ossification; PHO, posterior heterotopic ossification; JOA: Japanese Orthopaedic Association; NDI: neck disability index; VAS: visual analog scale; ROM, range of motion; ASD, adjacent segment degeneration.
*Significant difference between groups.
The univariate analysis was also performed between low-grade HO and high-grade HO. The disc height loss score of high-grade HO group was significantly higher than that of the low-grade HO group (P = .008) (Table 4). Regarding the clinical outcomes, no significant differences were noted for JOA, NDI, VAS scores, and ASD at the last follow-up between patients with and without high-grade HO. The ROM of C2-C7 was significantly lower in the high-grade HO groups than group without high-grade HO (41.41 ± 13.17° vs 51.38 ± 12.47°, P<.001) (Table 5).
Table 4.
Effects of Preoperative Spondylosis on the Degree of Heterotopic Ossification.
| Low-grade HO (n = 88) | High-grade HO (n = 29) | P | |
|---|---|---|---|
| Follow-up (months) | 48.47 ± 23.90 | 60.66 ± 33.71 | .129 |
| Level distribution | .086 | ||
| C3/4 and C4/5 | 30 | 5 | |
| C5/6 and C6/7 | 58 | 24 | |
| Overall degree of disc degeneration | 1.80 | 2.17 | .164 |
| Mean height loss score | .52 | .97 | .008* |
| Mean anterior osteophyte score | .99 | 1.07 | .751 |
| Mean endplate sclerosis score | .28 | .14 | .227 |
| Pre-op posterior osteophyte | .710 | ||
| Yes | 49 (55.7%) | 15 (51.7%) | |
| No | 39 (44.3%) | 14 (48.3%) | |
| Pre-op uncovertebral joint osteophyte | .619 | ||
| Yes | 38 (43.2%) | 11 (37.9%) | |
| No | 50 (56.8%) | 18 (62.1%) | |
| Facet joint degeneration | .523 | ||
| 1 | 66 (75.0%) | 20 (69.0%) | |
| 2 | 22 (25.0%) | 9 (31.0%) | |
| OALL | 19 (21.6%) | 4 (13.8%) | .359 |
| Ossification of ligamentum nuchae | 15 (17.0%) | 7 (24.1%) | .397 |
| Progression of ligamentum nuchae | 8 (9.1%) | 3 (10.3%) | .545 |
| ASD | 24 (27.3%) | 11 (37.9%) | .277 |
Abbreviation: AHO, anterior heterotopic ossification; PHO, posterior heterotopic ossification; OALL, ossification of anterior longitudinal ligament; ASD, adjacent segment disease.
*Significant difference between 2 groups.
Table 5.
Clinical Outcomes of Patients With or Without High-Grade Heterotopic Ossification at Last Follow-up.
| High-grade HO (−) (n = 122) | High-grade HO (+) (n = 27) | P | |
|---|---|---|---|
| JOA score | 16.00 ± .65 | 15.90 ± .74 | .665 |
| NDI score | 5.69 ± .58 | 5.56 ± .70 | .361 |
| VAS neck score | 1.57 ± .50 | 1.63 ± .56 | .705 |
| VAS arm score | .95 ± .54 | 1.04 ± .44 | .430 |
| ROM of C2-C7 | 51.38 ± 12.47 | 41.41 ± 13.17 | <.001* |
| ASD | 32 (26.2%) | 11 (40.7%) | .132 |
Abbreviation: HO: heterotopic ossification; JOA: Japanese Orthopaedic Association; NDI: neck disability index; VAS: visual analog scale; ROM, range of motion; ASD, adjacent segment degeneration.
*Significant difference between groups.
Multivariate Logistic Regression Analysis of HO According to the Location
Based on the results of univariate analysis, factors with P < .10 were involved in the multivariate logistic regression analysis of PHO group, including disc height loss, anterior osteophytes, preoperative osteophytes in the uncovertebral joint, facet joint degeneration and ligamentum nuchae ossification. Due to the lack of qualified factors in AHO group, we expanded the criteria to involve factors with P < .15 for multivariate analysis, including preoperative ligamentum nuchae ossification, postoperative shell angle and ROM at index level. No significant factors were identified in the analysis of AHO group (Table 6). For PHO group, height loss was identified as independent risk factors (P=.009, OR=1.820) (Table 7). The optimal cutoff score for disc height loss was .5, and the most suitable cutoff for the degree of disc height loss denoted as percentage 17 to predict PHO was 18.52%, with disc height loss ≥18.52% indicating a significant higher risk of PHO (P<.001, odds ratio [OR] 3.23, 95% CI 1.76-5.91). Besides, the incidence of PHO in segments with different disc height loss score were further investigated. As shown in Table 8, the incidence of PHO was significantly higher in segments with larger height loss score (P = .005).
Table 6.
Multivariate Logistic Regression Analysis of Risk Factors for Anterior Heterotopic Ossification.
| Risk factors | p | OR | 95% CI |
|---|---|---|---|
| Pre-op ligamentum nuchae ossification | .147 | .437 | .143-1.338 |
| Post-op shell angle | .225 | .956 | .890-1.028 |
| Post-op ROM at index level | .206 | 1.059 | .969-1.158 |
Abbreviation: Post-op, values at 1 week after surgery; ROM, range of motion.
Table 7.
Multivariate Logistic Regression Analysis of Risk Factors for Posterior Heterotopic Ossification.
| Risk factors | p | OR | 95% CI |
|---|---|---|---|
| Mean height loss score | .009* | 1.820 | 1.160-2.856 |
| Mean anterior osteophyte score | .052 | 1.454 | .997-2.120 |
| Pre-op uncovertebral joint osteophyte | .257 | 1.438 | .767-2.696 |
| Facet joint degeneration | .107 | 1.814 | .879-3.743 |
| Pre-op ligamentum nuchae ossification | .195 | 1.720 | .757-3.909 |
*Statistical significance.
Table 8.
The incidence of PHO in segments with different disc height loss score before surgery.
| 0 | 1 | 2 | P | |
|---|---|---|---|---|
| PHO | .005* | |||
| No | 75 (65.8%) | 33 (54.1%) | 6 (28.6%) | |
| Yes | 39 (34.2%) | 28 (45.9%) | 15 (71.4%) |
Abbreviation: PHO, posterior heterotopic ossification.
*Statistically significant.
Discussion
The theoretical advantages of CDR are based on the premise that motion preservation and load-sharing at the index level would mitigate the risk of ASD. 19 However, the occurrence of HO can be an intractable issue after CDR. Although previous studies have shown that HO did not worsen the patient-reported clinical outcomes, the progressive character of HO may lead to motion restriction at the treated level, which is contrary to the fundamental goal of CDR.2,7,20 Thus, identifying the real risk factors for HO and selecting appropriate candidates are of critical importance in the improvement of CDR. In the present study, we found that only HO in the posterior disc space is affected by preoperative degeneration. In the multiple elements of preoperative spondylosis, disc height loss may be the only independent risk factor for PHO formation.
A large number of studies has been conducted to explore the cause and risk factors for HO with different focus since it was first reported by Parkinson and Sekhon, 4 among which preoperative cervical spondylosis accounted for an important aspect. Cervical spondylosis is a generalized aging process encompassing a sequence of degenerative changes of cervical spine. The three-joint complex, including the 2 posterior joints and the intervertebral disc, and the bilateral uncovertebral joints are involved in the pathogenesis. 21 Although insignificant correlations were reported in a few studies, most studies emphasized the significant role of preoperative degeneration in the formation of HO following CDR. However, few studies investigated the effect of all the components of cervical spondylosis on HO. Chung et al 13 retrospectively reviewed 19 patients who underwent single-level CDR with Bryan. They found preoperative uncovertebral hypertrophy was a significant risk factor for high-grade HO through survivorship analysis. Wu et al. 6 evaluated forty patients who underwent single-level cervical arthroplasty using Bryan discs and divided them into a soft-disc herniation group and a spondylosis group. A significant higher rate of HO formation in spondylosis group was found compared with that with a soft-disc herniation. They defined the spondylosis in this study as disc disease with osteophytes, calcified disc, or marginal spurs. Jin et al. 15 reported HO in posterosuperior disc space was significantly related with the presence of preoperative ossification and ossification in the ligamentum nuchae. However, in a study of 170 patients, Yi et al. 11 evaluated the preoperative existing degenerative change including osteophytes, ossification of the ligaments and disc degeneration through detailed grades to investigate HO. Their results suggested only male gender and prosthesis type were the predisposing factors for HO and the preoperative degeneration of cervical spine exerted no significant influence on the occurrence of HO. In recent years, Tian et al. 9 revealed the only predisposing factor for high-grade HO after surgery was pre-existing paravertebral ossification before operation through a retrospective review of 71 patients treated with Bryan discs. Zhou et al. 7 found patients with more severe preoperative spondylosis had significant higher rates of postoperative HO using the Kellgren-Lawrence scale. Li et al. 8 also concluded the occurrence of HO after CDR is correlated to the severity of preoperative degeneration. In addition, a significant positive correlation between preoperative uncovertebral joints degeneration and postoperative HO was found in the study of Cao et al. 14 However, Guo et al. 12 analyzed 57 levels of cervical arthroplasty and no significant association was found between the HO formation and preexisting cervical degeneration. The discrepancy in results is probably due to the differences in the sample size, prosthesis type, population group, evaluating approach and components of preoperative cervical spondylosis.
In the analysis of 196 segments replaced by Prestige-LP discs, this study comprehensively assessed the preoperative spondylosis including the components of three-joint complex, uncovertebral joints and ligaments. The results of univariate analysis suggested preoperative height loss, anterior osteophytes, uncovertebral joint osteophytes and facet joint degeneration was significant degenerative factors for the occurrence of PHO after CDR. Further multivariate logistic regression analysis, however, identified the disc height loss before surgery was the only independent factor for PHO formation. This is probably due to the interdependently degenerative process among components in each cervical segment. The relationships between disc height loss and osteophyte formation in the vertebrae margins, uncovertebral joint osteophytes and facet joint degeneration have not been clearly defined. Walraevens et al. 17 indicated that height loss is the strongest predictor for disc degeneration. Previous study also demonstrated the importance of preoperative disc height loss and postoperative degree of distraction on the development of HO in CDR. 22 With aging, the degenerative cascade causes gradual desiccation of the intervertebral disc resulting in the loss of disc height, which transfer the biomechanical loads from the nucleus pulposus to the surrounding annulus fibers. 23 The decreased disc and facet joint stability lead to an altered biomechanical environment and abnormal motion. Traction stress related to instability may cause the development of anterior and posterior marginal endplate and uncinate spurs. 24 It was also stated that traction at the site of osseous attachment of annulus fibers to the vertebral surface may result in the reactive development of osteophytes.21,25 Sohn et al 26 found a significant correlation between the osteophytes formation and disc height loss in a cadaveric study. Besides, a numerical simulation study revealed that osteophyte formation is an adaptive bone remodeling process in response to the adjusted mechanical environment, which were mainly caused by the intervertebral disc degeneration. 27
Spondylosis of uncovertebral joint is characterized by osteophytes on the uncinate process 28 ; hence, the degeneration of uncovertebral joint was evaluated according to the presence of osteophyte in this study. This factor showed statistical significance in univariate analysis yet was insignificant in logistic regression analysis, which is probably because of its degenerative process resulted from the intervertebral disc degeneration. Traction stress due to instability may lead to the formation of uncinate osteophytes. 24 Besides, Cao et al. 14 also found a significant positive correlation between preoperative intervertebral space degeneration and uncovertebral joint degeneration. With progressive diminution of disc height related to degeneration of the cervical intervertebral joint, the bone protuberances about the uncovertebral articulations approach each other and are pressed firmly together, which might lead to the occurrence of osteophytes. 21 The impact of facet joint degeneration presented analogous pattern with uncovertebral degeneration in univariate and multivariate analysis. The three-joint complex in each cervical motion segment are highly functional interdependent, such that abnormalities of the disc tend to eventually affect the facet joints. 29 The diminution in disc height could cause pathologic loading of the facet joints, as less weight is supported by the disc when it becomes functionally incompetent.28,30 Nonetheless, the correlation between the degeneration of intervertebral disc and facet joints remains unclear. 5 In addition, our study suggested the disc height loss in high-grade HO was significantly higher in comparison with low-grade HO. Kim et al. 31 also found that the postoperative distraction height was significantly higher in the high-grade HO group, which usually accompany with more preoperative disc height loss. Therefore, the formation of high-grade HO is likely to restabilize the altered biomechanical environment at surgical segments.
Surgical procedures and postoperative biomechanical changes due to disc height loss may also contribute to the development of HO. Patients with more preoperative disc height loss may produce more bone dusts during endplate preparation and decompression procedures, which is considered an important predisposing factor for HO formation.32-34 Besides, segments with more disc height loss usually experience higher degree of distraction, resulting in greater changes in the postoperative biomechanical environments such as intervertebral height and segmental mobility.22,31 Ganbat et al 16 found that the addition of compressive force predominantly increased HO formation at the posterior parts of vertebrae, while HO was mainly formed in the anterior parts of vertebrae for anteriorly directly shear force through a three-dimensional finite element analysis. Likewise, prosthesis implantation at heigh loss segments could lead to greater pressure at the bone-implant interface compared to those with normal preoperative disc height, 35 which probably increase the risk for posterior HO. In the present study, no significant correlation was found between preoperative degeneration and the occurrence of AHO neither in the univariate analysis nor in the multivariate regression. Previous studies suggested that HO in the anterior disc space may be more related to the increased shear force rather than the degenerative factors.15,16,36 Thus, the mechanism and predisposing factors of AHO and its avoidance needed further investigation.
The prevention of ASD is 1 of the main goals of CDR. In the current study, we found that the rate of ASD was significantly higher in patients with PHO compared to those without PHO at the last follow-up. Interestingly, the correlation was not significant when further comparing the low-grade HO and high-grade HO affecting motion, which is consonant with previous report. 7 Zeng et al 37 found the progression rate of paravertebral ossification at the adjacent level was not significantly different from those of non-surgical and non-adjacent levels. These results may reveal that ASD tend to be the natural degeneration of cervical spine during follow-up rather than the complication caused by the changes of biomechanical environment. 38
However, there were several limitations to the study. First, the retrospective nature and a single institution study presented inherent weaknesses and limited generalizability of the results. Second, we use lateral X-ray rather than CT to detect HO and the ossification of uncovertebral joint area was not considered in our study. Previous studies have suggested a high incidence of HO in the uncovertebral region,9,37 which can be uneasy to detectable using plain films. However, radiography has a lower radiation dose and is more acceptable for patients when they do not have any clinical symptoms. Third, the follow-up time of our study was relatively short while the incidence and grade of HO may be more accurate and stable in a longer follow-up. Fourth, the study was limited to the Prestige-LP discs; thus, the results of HO formation may not be suitable in other type of prostheses with different design. Fifth, we did not identify significant factors for anterior HO neither in the univariate analysis nor in the logistic regression. Further studies concentrating on the biomechanical impacts are needed to be conducted.
Conclusion
In conclusion, this study revealed that preoperative cervical spondylosis predominantly affected the HO formation in the posterior disc space after CDR. The degree of preoperative disc height loss, anterior osteophytes, uncovertebral joint osteophytes and facet joints degeneration were more severe in patients with posterior HO after CDR. However, in the multiple elements of preoperative cervical spondylosis, only the disc height loss was an independent risk factor for posterior HO formation. Rigorous criteria for the degree of preoperative disc height loss should be used when selecting appropriate candidates for CDR.
Appendix.
List of abbreviations
- CDR
cervical disc replacement
- ACDF
anterior cervical discectomy and fusion
- HO
heterotopic ossification
- CT
computed tomography
- AHO
anterior heterotopic ossification
- PHO
posterior heterotopic ossification
- ASD
adjacent segment degeneration
- OALL
ossification of the anterior longitudinal ligament
- ROM
range of motion
- JOA
Japanese Orthopaedic Association
- NDI
neck disability index
- VAS
visual analog scale; SVA: sagittal vertical axis
Footnotes
Authors’ Contributions: Yi-Wei Shen and Yang Yi provided equal contribution to this study and should be considered co-first authors.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by research grants from the 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYJC18029), the National Natural Science Foundation of China (82002371), the Postdoctoral Science Foundation of China (2020M673240), and post-doctor research project, West China Hospital, Sichuan University (2019HXBH063).
ORCID iDs
Yi-Wei Shen https://orcid.org/0000-0003-1308-4584
References
- 1.Gornet MF, Burkus JK, Shaffrey ME, Schranck FW, Copay AG. Cervical disc arthroplasty: 10-year outcomes of the Prestige LP cervical disc at a single level. J Neurosurg Spine. 2019;31(3):317-325. doi: 10.3171/2019.2.Spine1956. [DOI] [PubMed] [Google Scholar]
- 2.Kim K, Hoffman G, Bae H, et al. Ten-year outcomes of 1- and 2-level cervical disc arthroplasty from the mobi-c investigational device exemption clinical trial. Neurosurgery . 2021;88(3):497-505. doi: 10.1093/neuros/nyaa459. [DOI] [PubMed] [Google Scholar]
- 3.Zhang X, Zhang X, Chen C, et al. Randomized, controlled, multicenter, clinical trial comparing BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion in China. Spine. 2012;37(6):433-438. doi: 10.1097/BRS.0b013e31822699fa. [DOI] [PubMed] [Google Scholar]
- 4.Parkinson JF, Sekhon LHS. Cervical arthroplasty complicated by delayed spontaneous fusion. Case report. J Neurosurg Spine . 2005;2(3):377-380. doi: 10.3171/spi.2005.2.3.0377. [DOI] [PubMed] [Google Scholar]
- 5.Theodore N. Degenerative cervical spondylosis. N Engl J Med . 2020;383(2):159-168. doi: 10.1056/NEJMra2003558. [DOI] [PubMed] [Google Scholar]
- 6.Wu JC, Huang WC, Tu TH, et al. Differences between soft-disc herniation and spondylosis in cervical arthroplasty: CT-documented heterotopic ossification with minimum 2 years of follow-up. J Neurosurg Spine . 2012;16(2):163-171. doi: 10.3171/2011.10.SPINE11497. [DOI] [PubMed] [Google Scholar]
- 7.Zhou F, Ju KL, Zhao Y, et al. Progressive bone formation after cervical disc replacement: Minimum of 5-year follow-up. Spine. 2018;43(3):E163-E170. doi: 10.1097/BRS.0000000000002264. [DOI] [PubMed] [Google Scholar]
- 8.Li G, Wang Q, Liu H, Yang Y. Postoperative heterotopic ossification after cervical disc replacement is likely a reflection of the degeneration process. World Neurosurg. 2019;125:e1063-e1068. doi: 10.1016/j.wneu.2019.01.244. [DOI] [PubMed] [Google Scholar]
- 9.Tian W, Fan M-X, Liu Y-j, et al. An analysis of paravertebral ossification in cervical artificial disc replacement: a novel classification based on computed tomography. Orthop Surg. 2016;8(4):440-446. doi: 10.1111/os.12286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou F, Li S, Zhao Y, et al. Quantitative analysis of the correlation between preoperative cervical degeneration and postoperative heterotopic ossification after cervical disc replacement: minimum 10-year follow-up data. J Neurosurg Spine . 2020;17:674-679. doi: 10.3171/2020.4.SPINE191303. [DOI] [PubMed] [Google Scholar]
- 11.Yi S, Shin DA, Kim KN, et al. The predisposing factors for the heterotopic ossification after cervical artificial disc replacement. Spine J . 2013;13(9):1048-1054. doi: 10.1016/j.spinee.2013.02.036. [DOI] [PubMed] [Google Scholar]
- 12.Guo Q, Fang Z, Guan H, Xiong W, Li F. The effect of footprint mismatch on heterotopic ossification after cervical disk replacement. Clin Spine Surg . 2020;33(6):E241-e250. doi: 10.1097/bsd.0000000000000943. [DOI] [PubMed] [Google Scholar]
- 13.Chung S-B, Muradov JM, Lee S-H, Eoh W, Kim E-S. Uncovertebral hypertrophy is a significant risk factor for the occurrence of heterotopic ossification after cervical disc replacement: survivorship analysis of Bryan disc for single-level cervical arthroplasty. Acta Neurochir . 2012;154(6):1017-1022. doi: 10.1007/s00701-012-1309-1. [DOI] [PubMed] [Google Scholar]
- 14.Cao S, Pan SF, Sun Y, et al. The correlation between the severity of uncovertebral joints degeneration and heterotopic ossification after single-level artificial cervical disc replacement. Zhonghua yi xue za zhi. 2020;100(45):3578-3583. doi: 10.3760/cma.j.cn112137-20200811-02347. [DOI] [PubMed] [Google Scholar]
- 15.Jin YJ, Park SB, Kim MJ, Kim KJ, Kim HJ. An analysis of heterotopic ossification in cervical disc arthroplasty: a novel morphologic classification of an ossified mass. Spine J . 2013;13(4):408-420. doi: 10.1016/j.spinee.2012.11.048. [DOI] [PubMed] [Google Scholar]
- 16.Ganbat D, Kim YH, Kim K, Jin YJ, Park WM. Effect of mechanical loading on heterotopic ossification in cervical total disc replacement: a three-dimensional finite element analysis. Biomech Model Mechanobiol. 2016;15(5):1191-1199. doi: 10.1007/s10237-015-0752-3. [DOI] [PubMed] [Google Scholar]
- 17.Walraevens J, Liu B, Vander Sloten J., Goffin J. Qualitative and quantitative assessment of degeneration of cervical intervertebral discs and facet joints. Eur Spine J . 2009;18(3):358-369. doi: 10.1007/s00586-008-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty: a prospective 2-year study. J Neurosurg Spine . 2005;3(6):417-423. doi: 10.3171/spi.2005.3.6.0417. [DOI] [PubMed] [Google Scholar]
- 19.Parish JM, Asher AM, Coric D. Complications and complication avoidance with cervical total disc replacement. Int J Spine Surg . 2020;14(s2):S50-S56. doi: 10.14444/7091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mehren C, Suchomel P, Grochulla F, et al. Heterotopic ossification in total cervical artificial disc replacement. Spine. 2006;31(24):2802-2806. doi: 10.1097/01.brs.0000245852.70594.d5. [DOI] [PubMed] [Google Scholar]
- 21.Resnick D. Degenerative diseases of the vertebral column. Radiology . 1985;156(1):3-14. doi: 10.1148/radiology.156.1.3923556. [DOI] [PubMed] [Google Scholar]
- 22.Wang XF, Liu H, Meng Y, et al. Effect of disc height and degree of distraction on heterotopic ossification after cervical disc replacement. World Neurosurgery. 2021;145:E100-E107. doi: 10.1016/j.wneu.2020.09.134. [DOI] [PubMed] [Google Scholar]
- 23.Ferrara LA. The biomechanics of cervical spondylosis. Adv Orthop. 2012;2012:493605. doi: 10.1155/2012/493605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Russell EJ. Cervical disk disease. Radiology. 1990;177(2):313-325. doi: 10.1148/radiology.177.2.2217760. [DOI] [PubMed] [Google Scholar]
- 25.Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988;168(1):177-186. doi: 10.1148/radiology.168.1.3289089. [DOI] [PubMed] [Google Scholar]
- 26.Sohn HM, You JW, Lee JY. The relationship between disc degeneration and morphologic changes in the intervertebral foramen of the cervical spine: a cadaveric MRI and CT study. J Korean Med Sci . 2004;19(1):101-106. doi: 10.3346/jkms.2004.19.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.He G, Xinghua Z. The numerical simulation of osteophyte formation on the edge of the vertebral body using quantitative bone remodeling theory. Joint Bone Spine . 2006;73(1):95-101. doi: 10.1016/j.jbspin.2005.03.019. [DOI] [PubMed] [Google Scholar]
- 28.Sarzi-Puttini P, Atzeni F, Fumagalli M, Capsoni F, Carrabba M. Osteoarthritis of the spine. Semin Arthritis Rheum . 2005;34(6 suppl 2):38-43. [PubMed] [Google Scholar]
- 29.Gellhorn AC, Katz JN, Suri P. Osteoarthritis of the spine: the facet joints. Nat Rev Rheumatol . 2013;9(4):216-224. doi: 10.1038/nrrheum.2012.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dunlop R, Adams M, Hutton W. Disc space narrowing and the lumbar facet joints. J Bone Joint Surg Br . 1984;66(5):706-710. doi: 10.1302/0301-620x.66b5.6501365. [DOI] [PubMed] [Google Scholar]
- 31.Kim KS, Heo DH. Do postoperative biomechanical changes induce heterotopic ossification after cervical arthroplasty?: A 5-year follow-up study. Clin Spine Surg . 2016;29(6):E309-E313. doi: 10.1097/bsd.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 32.Puzas JE, Miller MD, Rosier RN. Pathologic bone formation. Clin Orthop Relat Res . 1989(245):269-281. [PubMed] [Google Scholar]
- 33.Lee JH, Jung TG, Kim HS, Jang JS, Lee SH. Analysis of the incidence and clinical effect of the heterotopic ossification in a single-level cervical artificial disc replacement. Spine J . 2010;10(8):676-682. doi: 10.1016/j.spinee.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 34.Leung C, Casey AT, Goffin J, et al. Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial. Neurosurgery. 2005;57(4):759-763. doi: 10.1093/neurosurgery/57.4.759. [DOI] [PubMed] [Google Scholar]
- 35.Yuan W, Zhang H, Zhou X, Wu W, Zhu Y. The influence of artificial cervical disc prosthesis height on the cervical biomechanics: A finite element study. World Neurosurg. 2018;113:e490-e498. doi: 10.1016/j.wneu.2018.02.062. [DOI] [PubMed] [Google Scholar]
- 36.Wang XF, Meng Y, Liu H, et al. Association of cervical sagittal alignment with adjacent segment degeneration and heterotopic ossification following cervical disc replacement with Prestige-LP disc. J of Ortho Surg. 2020;28(3):2309499020968295. doi: 10.1177/2309499020968295. [DOI] [PubMed] [Google Scholar]
- 37.Zeng C, Tian W, Liu B, Fan M. The assessment of paravertebral ossification progression after cervical disc arthroplasty based onCTimages: A long-term follow-up. Orthop Surg . 2020;12(6):1760-1767. doi: 10.1111/os.12743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hui N, Phan K, Cheng HMK, Lin YH, Mobbs RJ. Complications of cervical total disc replacement and their associations with heterotopic ossification: a systematic review and meta-analysis. Eur Spine J . 2020;29(11):2688-2700. doi: 10.1007/s00586-020-06400-z. [DOI] [PubMed] [Google Scholar]