Abstract
Study Design
Retrospective analysis of prospectively database
Objective
Implant-related complications are an extremely important issue because they pose a burden to patients who underwent surgery. An understanding of these complications can help improve the postoperative management of patients undergoing spinal surgery. The current large-scale multicenter study aimed to identify postoperative implant-related complications that may require revision surgery.
Methods
In total, 3447 patients who underwent spinal fusion surgery were included in the analysis. Data about age at surgery, sex, preoperative diagnosis, surgical level, type of implant-related complications, causes of reoperation, and time from the initial to revision surgery were reviewed. Moreover, the characteristics of reoperation in 3 periods (within 30, 31–90, and over 90 days) were assessed.
Result
The overall incidence of implant-related complications was 4.6%. Adult spinal deformity was the most common diagnosis (9.9%), and thoracic-lumbar-sacral (42.9%) was the most common surgical level among patients with implant-related complications. Further, screw malposition was the most frequent implant-related complication (42.8%). In total, 89 (2.6%) patients underwent reoperation due to implant-related complications. The main causes of reoperation within 30, 31–90, and over 90 days were screw malposition (72.2%), screw loosening or pull out (81.8%), and rod or screw fracture (60.9%), respectively.
Conclusion
To the best of our knowledge, this was the first large-scale multicenter study that assessed the characteristics of patients who underwent reoperation due to spinal implant-related complications. The study results could improve the preoperative informed consent procedure about spinal fusion.
Keywords: implant-related complications, large-scale multicenter study, spinal fusion surgery, reoperation
Introduction
In recent years, the quality of spinal instruments including pedicle screws has significantly improved, and their use results in strong spinal fixation with excellent clinical outcomes.1,2 Accordingly, the number of spinal surgery such as long fusions with multiple osteotomy among elderly individuals has increased. 3 However, the reoperation rate caused by implant-related complications is also high because surgical procedures are challenging.4,5
Postoperative implant-related complications are a major issue after primary spinal fusion because they may affect postoperative recovery, length of hospital stay, quality of life, and healthcare costs. The cost of cases with complications after spinal surgery was $13,518.35 higher than that of cases without complication. In addition, the cost of major complications was $13,714.88 greater than that of minor complications based on a previous study. 6 Patients with postoperative complications had a longer length of hospital stay than those without. The average length of hospital stay of patients with postoperative complications was 5.1 ± 2.3 days, and that of patients without complications was 2.9 ± 6.9 days. 7 Nevertheless, complications are not preventable to some extent among patients undergoing surgery. Therefore, understanding the characteristics of implant complications in each disease and the timing of their occurrence can be useful in presurgical informed consent. Although there are several reports about spinal surgery complications, the number of studies about the types, frequency, and period of postoperative implant-related complications is limited. Moreover, only few reports have assessed implant-related complications that may require revision surgery. Postoperative complications can vary according to the length of the postoperative period, and there can also be an association between the period and cause of reoperation. Therefore, the current large-scale multicenter study aimed to identify postoperative implant-related complications among patients who underwent revision surgery after spinal fusion.
Methods
Data Collection and Sources
This was a retrospective study that used prospectively maintained surgical records. In total, 9101 patients underwent spinal surgery at four institutions from 2010 to 2019. We included 4974 patients who underwent spinal surgery with instrumentation. However, those who had spinal surgery without instrumentation and those with incomplete demographic data were excluded. Patients aged below 20 years were also eligible for the study. The final analysis included 3447 patients (Figure 1). We collected data about age at surgery, sex, preoperative diagnosis, surgical level, type of implant-related complications, causes of revision surgery, and time from the initial to revision surgery. The current research protocol was approved by the institutional review board of our institution (IRB no. 354-3) and all patients provided written informed consent.
Figure 1.
Flowchart of patient inclusion.
Implant-Related Complication
The preoperative diagnoses were degenerative spinal disease (DSD), adult spinal deformity (ASD), trauma, tumor, ossification of the posterior longitudinal ligament (OPLL) or ossification of the ligamentum flavum (OLF), and others (including infectious diseases such as discitis, ankylosing spondylitis, atlantoaxial rotatory fixation, os odontoideum, retro-odontoid pseudotumor, congenital and syndromic scoliosis, and cervical instability such as atlantoaxial subluxation, achondroplasia, and cervical flexion myelopathy). Surgical level was defined as the location of the fusion vertebrae and was classified as cervical, cervical-thoracic, cervical-thoracic-lumbar-sacral, thoracic, thoracic-lumbar, thoracic-lumbar-sacral, lumbar, and lumbar-sacral. The spinal implant-related complications included implant displacement such as screw malposition, loosening, or pull out; postoperative cage dislocation or subsidence; and implant breakage such as rod fracture and skin trouble. The definition of each implant-related complication was based on the discretion of the physician in charge at each institution.
Reoperation Associated With Implant-Related Complications
Information about reoperation was collected from the surgical records of each institution. Physicians who performed the surgery made the decision to reoperate. The number of days to reoperation was defined as the number of days from the date of the initial surgery to that of the revision surgery. The period from the initial to revision surgery was divided into three, which were as follows: within 30, 31–90, and over 90 days.
Statistical Analysis
Data were expressed as mean ± standard deviation for continuous variables. The Mann–Whitney U test was used to compare the mean values of continuous variables. The chi-square test was used, and residual analysis of the cross-tabulation tables was performed to analyze the mean values of categorial variables. Categorical data were expressed as numbers and percentages. A P value of < .05 was considered statistically significant. All statistical analyses were performed using the BellCurve add-ons for Excel (Social Survey Research Information Co., Ltd., Tokyo, Japan).
Results
In total, 3447 patients who underwent spinal fusion surgeries (mean age: 63.1 ± 15.4 years, 1655 men and 1792 women) were enrolled in this study. Table 1 shows the preoperative diagnosis and surgical level in all spinal fusion and implant-related complication cases. In all spinal fusion surgeries, DSD was the most common preoperative diagnosis (2114/3447 [61.3%]), and lumbar (1668/3447 [48.4%]) was the most frequent surgical fusion level.
Table 1.
Preoperative Diagnosis and Surgical Level About all Spinal Fusion and Implant-Related Complications Cases.
| Preoperative diagnosis | Total | Implant-related complication (%Total) |
| DSD | 2114 | 81(3.8) |
| ASD | 543 | 54(9.9) |
| Trauma | 384 | 12(3.1) |
| Tumor | 114 | 2(1.8) |
| OPLL or OLF | 161 | 4(2.5) |
| Others | 131 | 6(4.6) |
| Total | 3447 | 159(4.6) |
| Surgical level | ||
| Lumbar | 1668 | 55(3.3) |
| Cervical | 460 | 15(3.3) |
| Thoracic-lumbar | 454 | 22(4.8) |
| Lumbar-sacral | 452 | 24(5.3) |
| Thoracic | 226 | 3(1.3) |
| Cervical-thoracic | 100 | 4(4.0) |
| Thoracic-lumbar-sacral | 84 | 36(42.9) |
| Cervical-thoracic-lumbar-sacral | 3 | 0 |
| Total | 3447 | 159(4.6) |
DSD: degenerative spinal disease, ASD: adult spinal deformity, OPLL: Ossification of the posterior longitudinal ligament, OLF: Ossification of ligamentum flavum, Values are mean ± SD for each group.
Implant-Related Complications
The overall incidence of implant-related complications was 4.6% (159/3, 447). In total, 159 patients (49 men and 110 women) presented with implant-related complications, and the average age of patients with these complications was 66.3 ± 12.9 years. Further, patients with implant-related complications were older than those without (66.3 ± 12.9 vs 62.9 ± 15.5, P = .02). ASD was the most common preoperative diagnosis (9.9%), and thoracic-lumbar-sacral (42.9%) was the most frequent surgical level among patients with implant-related complications. The most usual implant-related complications were screw malposition (42.8%), followed by screw loosening or pull out (24.5%), implant breakage (22.0%), cage dislocation or subsidence (11.9%), and skin trouble (1.3%).
The most frequent implant-related complications among patients diagnosed with DSD were screw malposition (58.8%), screw loosening or pull out (64.1%), and cage dislocation or subsidence (57.9%). Further, the most common implant-related complications among patients diagnosed with ASD were implant breakage (62.9%) and skin issues (50.0%) (Table 2). Patients with DSD and ASD frequently had complications. Meanwhile, those with other diseases had fewer complications. With respect to the level of implant-related complications, screw malposition (38.2%) and cage dislocation/subsidence (57.9%) were most commonly observed at the lumbar level. Patients with thoracic-lumbar-sacral fusion typically presented with implant breakage (74.3%) and skin issues (100%) (Table 2). Patients who underwent lumbar or thoracolumbar spinal surgery commonly had a higher number of implant-related complications. In contrast, patients who underwent cervical spinal surgery had a lower number of implant-related complications.
Table 2.
Preoperative Diagnosis of each Implant-Related Complications.
| Diagnosis (%) | Surgical level (%) | |||||
|---|---|---|---|---|---|---|
| Variables | 1st | 2nd | 3rd | 1st | 2nd | 3rd |
| Screw malposition | DSD (58.8) | ASD (20.6) | Trauma (10.3) | Lumbar (38.2) | Thoracic-lumbar (19.1) | Lumbar-sacral (17.6) |
| Screw loosening or pulled out | DSD (64.1) | ASD (28.2) | Trauma (5.1) | Thoracic-lumbar (46.2) | Thoracic-lumbar or Lumbar-sacral (15.3) | Thoracic-lumbar-sacral (12.8) |
| Rod or screw fracture | ASD (62.9) | DSD (14.3) | Trauma (11.4) | Thoracic-lumbar-sacral (74.3) | Cervical or Lumbar-sacral (8.6) | Cervical-thoracic (5.7) |
| Cage dislocation or subsidence | DSD (57.9) | ASD (42.1) | — | Lumbar (57.9) | Thoracic-lumbar or Lumbar-sacral (15.8) | Thoracic-lumbar-sacral (10.5) |
| Skin trouble | ASD or Trauma (50.0) | — | — | Thoracic-lumbar-sacral (100) | — | — |
DSD: degenerative spinal disease, ASD: adult spinal deformity.
Reoperation Associated With Implant-Related Complications
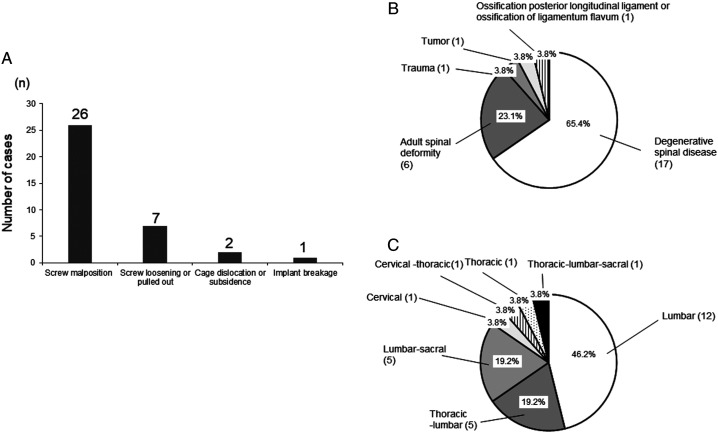
The overall incidence of reoperation caused by implant-related complications was 2.6% (89/3447). Figure 2 shows the reoperation rate for each implant-related complication. All patients with skin issues had reoperation. The reoperation rate of screw malposition (45.6%) and cage dislocation or subsidence (31.6%) was < 50%. Table 3 shows the period of reoperation with implant-related complications. The main cause of 30-, 31–90-, and over 90-day reoperation were screw malposition, screw loosening or pull out, and implant breakage, respectively.
Figure 2.
Reoperation rate of each implant-related complication. Each failure was overlapped.
Table 3.
The Period from the Initial to Revision Surgery With Implant-Related Complications.
| Implant failure variables (each failures were overlapped) | 30-day reoperation (N = 36) | 31–90 day reoperation (N = 11) | 90-day over reoperation (N = 42) |
|---|---|---|---|
| Screw malposition | 26* | 1 | 4* |
| Rod or screw fracture | 1* | 0 | 25* |
| Screw loosening or pulled out | 7 | 9* | 11 |
| Cage dislocation or subsidence | 2 | 1 | 3 |
| Skin trouble | 0 | 0 | 2 |
| * P <.001 |
Thirty-Day Reoperation
Screw malposition (72.2%) was the most common cause of 30-day reoperation among patients with implant-related complications. DSD (65.4%) and lumbar (46.2%) were the main primary disease and surgical level of reoperation caused by screw malposition, respectively. Lumbar DSD including lumbar canal stenosis was the frequent cause of screw malposition (Figure 3).
Figure 3.
Details about 30-day reoperation (A). Preoperative diagnosis (B). Surgical level (C) of reoperation caused by screw malposition.
Thirty-One to Ninety-Day Reoperation
Screw loosening or pull out (81.8%) was the main cause of 31–90-day reoperation, and ASD (66.7%) was the primary disease among patients who underwent reoperation due to screw loosening or pull out. Lumbar (44.4%) was the most common surgical level. Hence, screw loosening or pull out was more common in patients with ASD who underwent fixation at the lumbar level only, not up to the sacrum (Figure 4).
Figure 4.
Details of 31–90-day reoperation cases (A). Preoperative diagnosis (B). Surgical level of reoperation caused by screw loosening or pull out (C).
Over 90-Day Reoperation
Implant breakage (60.9%) was the most common cause of over 90-day reoperation. ASD (56.0%) and thoracic-lumbar-sacral (64.0%) were the primary disease and surgical level of reoperation caused by rod or screw fracture, respectively. Implant breakage was more frequently observed in patients with ASD that required correction and relatively extensive fusion (Figure 5).
Figure 5.
Details of over 90-day reoperation (A). Preoperative diagnosis (B). Surgical level of reoperation caused by implant breakage (C).
Discussion
This was the first large-scale multicenter study focusing on reoperation associated with spinal implant-related complications. Furthermore, the difference in reoperation rates from the initial spinal to revision surgery was evaluated. In our study, the overall incidence of implant-related complications was 4.6% (159/3447). Results showed that old age, ASD, and thoracic-lumbar-sacral level of surgery were associated with more implant-related complications.
In different spinal surgeries, the complication rates are relatively high among patients with ASD8,9 and, particularly, elderly individuals.10,11 Dinizo et al showed that the rate of unplanned reoperation within 30 days of ASD surgery is 2.8%, and hospital readmission and unplanned reoperation have major implications for all health care providers particularly if reoperations occur within 90 days. 12
However, previous studies focused on patients with ASD, and results showed that postoperative implant-related complications were more common in patients with ASD who underwent spinal fusion.
Screw malposition was the most common cause of implant-related complications. Previous reports revealed that deep surgical field, degeneration, proximity to neurovascular tissue, and vertebral with axial rotation could cause screw malposition.13-17 Notably, the current study showed that the most common preoperative diagnosis of screw malposition was DSD, and the most common surgical level was lumbar. Hence, screw malposition commonly occurs after surgeries for diseases including lumbar fusion, which are extremely common and performed in all facilities. In particular, when performing freehand screw insertion, the screw should be inserted cautiously even if it is a common surgery. The current study revealed that screw malposition was the most common cause of reoperation within 30 days. Shimizu et al showed the incidence and causes of 30-day reoperations after spinal surgery. 18 Moreover, the pedicle screw malposition (10.2%) was found to be a cause of 30-day reoperations. Similar to their report, our study showed that patients with motor paralysis or those with radicular pain caused by screw malposition required 30-day reoperation. In such cases, the screw must be replaced immediately.
In our series, screw loosening or pull out was the main cause of 31- to 90-day reoperation. This was a novel finding because no report has discussed the period of reoperation caused by screw loosening or pull out. ASD was the main preoperative diagnosis of reoperation caused by screw loosening or pull out, and the most common surgical level was the lumbar level. Lumbar level bone non-union was a cause of screw loosening or pull out among patients with ASD. 19 Bone union is a key factor for preventing pedicle screw loosening or pull out. Hence, adequate bone grafting and bone healing should be performed during surgery. Using a large-diameter screw, a long screw that penetrates the anterior cortex of the vertebral body and cement augmentation of the pedicle screw are considered to prevent screw backout attributed to bone non-union.20-22 This must be evaluated in the postoperative follow-up period because 31- to 90-day reoperation caused by screw loosening or pull out might be specific in patients who did not achieve early fixation based on this finding.
Out finding showed that implant breakage was the most common cause of over 90-day reoperation, and ASD was the primary disease of reoperation caused by implant breakage. Surgery for ASD is highly invasive, and the incidence of complications is significantly higher than that of surgery for degenerative diseases. The rates of reoperation for primary ASD vary from 8% to 58% 23 because of different factors including surgical procedure, patient characteristics, and instrumentation systems. Compared with other implant-related complications, implant breakage was more likely to result in revision surgery in all cases. Feng et al showed that implant breakage is the most common cause of reoperation in patients with ASD (23/62 [37.1%]). 24 The common implant breakage is rod fracture, and the main cause of rod fracture is pseudoarthrosis caused by fusion deficit increases the local load on implants.25,26 Residual local kyphosis was found to be a cause of rod fracture. In particular, residual postoperative kyphosis among patients who underwent osteotomy increases the local load on the rod, leading to rod fracture. 27 To prevent rod fracture, the most important method is to achieve bone fusion with sufficient bone graft. However, increasing the number of rods may also be considered.28,29
The current study had several limitations. First, it was retrospective in nature, and prospectively maintained surgical records were used. However, the study design could allow the use of more data for analysis due to fewer errors in data collection in this type of research than in a complete retrospective study.
Second, detailed data about comorbidity and surgical information such as surgeon experience and metal composition of implants are lacking because the study used information from the surgical databases of multiple hospitals. Therefore, further analysis must be conducted to identify factors that may affect implant-related complications. Third, the surgical procedure significantly varied in terms of the implant system used, such as screws and rods, among different surgeons.
Conclusions
We investigated implant-related complications after instrumentation surgery and factors associated with revision surgery using a multicenter database. The overall incidence of revision surgery was 2.6%, and the most common surgical causes of 30-, 31–90-, and over 90-day reoperation were screw malposition, screw loosening or pull out, and implant breakage, respectively. The current study could provide not only useful postoperative follow-up information for all spinal surgeons who use implants but also important insights for all health care professionals who are involved in postoperative management, as well as for patients and their families.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Hiroaki Nakashima https://orcid.org/0000-0002-0039-9678
Kei Ando https://orcid.org/0000-0002-1088-2903
Shiro Imagama https://orcid.org/0000-0002-6951-8575
Reference
- 1.Okamoto T, Neo M, Fujibayashi S, Ito H, Takemoto M, Nakamura T. Mechanical implant failure in posterior cervical spine fusion. Eur Spine J . 2012;21(2):328-334. doi: 10.1007/s00586-011-2043-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shea TM, Laun J, Gonzalez-Blohm SA, et al. Designs and techniques that improve the pullout strength of pedicle screws in osteoporotic vertebrae: current status. BioMed Res Int. 2014;2014:748393. doi: 10.1155/2014/748393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crawford CH, 3rd, Carreon LY, Bridwell KH, Glassman SD. Long fusions to the sacrum in elderly patients with spinal deformity. Eur Spine J . 2012;21(11):2165-2169. doi: 10.1007/s00586-012-2310-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am . 2003;85(11):2089-2092. doi: 10.2106/00004623-200311000-00004 [DOI] [PubMed] [Google Scholar]
- 5.Smith JS, Shaffrey CI, Glassman SD, et al. Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine. 2011;36(10):817-824. doi: 10.1097/BRS.0b013e3181e21783 [DOI] [PubMed] [Google Scholar]
- 6.Whitmore RG, Stephen J, Stein SC, et al. Patient comorbidities and complications after spinal surgery: a societal-based cost analysis. Spine. 2012;37(12):1065-1071. doi: 10.1097/BRS.0b013e31823da22d [DOI] [PubMed] [Google Scholar]
- 7.Gruskay J, Fu M, Bohl D, Webb M, Grauer J. Factors affecting length of stay following elective posterior lumbar spine surgery: a multivariate analysis. Spine J. 2013;15:1188-1195. doi: 10.1016/j.spinee.2013.10.022 [DOI] [PubMed] [Google Scholar]
- 8.Kim H-J, Zuckerman SL, Cerpa M, Yeom JS, Lehman RA, Jr, Lenke LG. Incidence and risk factors for early postoperative complications and mortality following adult spinal deformity surgery: data from the national surgical quality improvement program from 2011 to 2013. Clin Spine Surg. 2021;34:E566-E574. [DOI] [PubMed] [Google Scholar]
- 9.Manoharan SR, Baker DK, Pasara SM, Ponce B, Deinlein D, Theiss SM. Thirty-day readmissions following adult spinal deformity surgery: an analysis of the National surgical quality improvement program (NSQIP) database. Spine J . 2016;16(7):862-866. doi: 10.1016/j.spinee.2016.03.014 [DOI] [PubMed] [Google Scholar]
- 10.Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976). 2007;32(20):2238-2244. doi: 10.1097/BRS.0b013e31814cf24a [DOI] [PubMed] [Google Scholar]
- 11.Puvanesarajah V, Shen FH, Cancienne JM, et al. Risk factors for revision surgery following primary adult spinal deformity surgery in patients 65 years and older. J Neurosurg Spine . 2016;25(4):486-493. doi: 10.3171/2016.2.Spine151345 [DOI] [PubMed] [Google Scholar]
- 12.Dinizo M, Dolgalev I, Passias PG, Errico TJ, Raman T. Complications after adult spinal deformity surgeries: all are not created equal. Int J Spine Surg . 2021;15(1):137-143. doi: 10.14444/8018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Brien MF, Lenke LG, Mardjetko S, et al. Pedicle morphology in thoracic adolescent idiopathic scoliosis: is pedicle fixation an anatomically viable technique? Spine (Phila Pa 1976). 2000;25(18):2285-2293. doi: 10.1097/00007632-200009150-00005 [DOI] [PubMed] [Google Scholar]
- 14.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res . 1986;203:7-17. [PubMed] [Google Scholar]
- 15.Tian W, Lang Z. Placement of pedicle screws using three-dimensional fluoroscopy-based navigation in lumbar vertebrae with axial rotation. Eur Spine J . 2010;19(11):1928-1935. doi: 10.1007/s00586-010-1564-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vaccaro AR, Rizzolo SJ, Allardyce TJ, et al. Placement of pedicle screws in the thoracic spine. Part I: morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am . 1995;77(8):1193-1199. doi: 10.2106/00004623-199508000-00008 [DOI] [PubMed] [Google Scholar]
- 17.Vaccaro AR, Rizzolo SJ, Balderston RA, et al. Placement of pedicle screws in the thoracic spine. Part II: an anatomical and radiographic assessment. J Bone Joint Surg Am . 1995;77(8):1200-1206. doi: 10.2106/00004623-199508000-00009 [DOI] [PubMed] [Google Scholar]
- 18.Shimizu T, Fujibayashi S, Takemoto M, et al. A multi-center study of reoperations within 30 days of spine surgery. Eur Spine J . 2016;25(3):828-835. doi: 10.1007/s00586-015-4113-9 [DOI] [PubMed] [Google Scholar]
- 19.Wu X, Shi J, Wu J, et al. Pedicle screw loosening: the value of radiological imagings and the identification of risk factors assessed by extraction torque during screw removal surgery. J Orthop Surg Res. 2019;14(1):6-6. doi: 10.1186/s13018-018-1046-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polly DW, Jr, Orchowski JR, Ellenbogen RG. Revision pedicle screws: bigger, longer shims-what is best? Spine. 1998;23(12):1374-1379. [DOI] [PubMed] [Google Scholar]
- 21.Son HJ, Choi SH, Heo DR, et al. Outcomes of the use of cement-augmented cannulated pedicle screws in lumbar spinal fusion. Spine J . 2021;21(11):1857-1865. doi: 10.1016/j.spinee.2021.05.005 [DOI] [PubMed] [Google Scholar]
- 22.Tandon V, Kalidindi KKV, Pacha S, Bhat MR. A prospective study on the feasibility, safety, and efficacy of a modified technique to augment the strength of pedicle screw in osteoporotic spine fixation. Asian Spine J . 2020;14(3):357-363. doi: 10.31616/asj.2019.0211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mok JM, Cloyd JM, Bradford DS, et al. Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. Spine (Phila Pa 1976). 2009;34(8):832-839. doi: 10.1097/BRS.0b013e31819f2080 [DOI] [PubMed] [Google Scholar]
- 24.Zhu F, Bao H, Liu Z, et al. Unanticipated revision surgery in adult spinal deformity: an experience with 815 cases at one institution. Spine (Phila Pa 1976). 2014;39(26 Spec No.):B36-B44. doi: 10.1097/brs.0000000000000463 [DOI] [PubMed] [Google Scholar]
- 25.Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976). 2006;31(20):2329-2336. doi: 10.1097/01.brs.0000238968.82799.d9 [DOI] [PubMed] [Google Scholar]
- 26.Smith JS, Shaffrey CI, Ames CP, et al. Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery. 2012;71(4):862-867. doi: 10.1227/NEU.0b013e3182672aab [DOI] [PubMed] [Google Scholar]
- 27.Yang JS, Sponseller PD, Thompson GH, et al. Growing rod fractures: risk factors and opportunities for prevention. Spine (Phila Pa 1976). 2011;36(20):1639-1644. doi: 10.1097/BRS.0b013e31822a982f [DOI] [PubMed] [Google Scholar]
- 28.Guevara-Villazón F, Boissiere L, Hayashi K, et al. Multiple-rod constructs in adult spinal deformity surgery for pelvic-fixated long instrumentations: an integral matched cohort analysis. Eur Spine J . 2020;29(4):886-895. doi: 10.1007/s00586-020-06311-z [DOI] [PubMed] [Google Scholar]
- 29.Rocos B, Rioux-Trottier E, Machida M, et al. The use of three rods in correcting severe scoliosis. Spine Deform . 2021;9(4):969-976. doi: 10.1007/s43390-021-00300-y [DOI] [PubMed] [Google Scholar]