Abstract
Purpose.
The weathering hypothesis states that chronic exposure to social and economic disadvantage leads to accelerated decline in physical health outcomes and could partially explain racial disparities in a wide array of health conditions. This systematic review summarizes the literature empirically testing the weathering hypothesis and assesses the quality of the evidence regarding weathering as a determinant of racial disparities in health.
Methods.
Databases (Web of Science, Ovid MEDLINE, PubMed and Embase) were searched for studies published in English up to July 1, 2017. Studies that tested the weathering hypothesis for any physical health outcome and included at least one socially or economically disadvantaged group (e.g., Blacks) for whom the weathering hypothesis applies were assessed for eligibility. Threats to validity were assessed using the Quality in Prognostic Studies tool.
Results.
The 41 included studies were rated as having overall good methodological quality. Most studies found evidence in support of the weathering hypothesis, although the magnitude of support varied by the health outcome and population studied.
Conclusions.
Future evaluations of the weathering hypothesis should include an examination of additional health outcomes and interrogate mechanisms that could link weathering to poor health.
Keywords: weathering, race, health disparities, health inequalities
INTRODUCTION
Blacks have higher rates of morbidity and mortality than Whites for almost all health outcomes in the United States (U.S.) and this inequality increases with age. [1–8] While these racial disparities are notable, their underlying causes are unclear. [9, 10] The weathering hypothesis was proposed to explain racial health disparities. Weathering is the result of chronic exposure to social and economic disadvantage that leads to the acceleration of normal aging and earlier onset of unfavorable physical health conditions among disadvantaged (versus advantaged) persons of similar age (i.e. weathering pattern). [11–15]
The weathering hypothesis was motivated by observations of earlier onset of chronic diseases (e.g. hypertension) impacting birth outcomes in Blacks relative to Whites [16] and originated from Geronimus’ empirical studies on racial disparities in birth outcomes. [15] Contrary to the well-documented curvilinear relationship between maternal age and birth outcomes, where teenage and 30+ year old pregnant women are expected to have a higher risk for adverse birth outcomes than women in their mid-20s, studies by Geronimus revealed variations by race. She found that White teenage mothers had a higher risk for infant mortality and low birthweight than White mothers in their mid-to-late 20s, but Black teenage mothers had a lower risk for infant mortality and low birthweight than older Black mothers. [14, 15, 17]
Many studies use this hypothesis as an explanatory framework for racial disparities in health, but a systematic review of the studies that explicitly test this hypothesis has not been previously conducted. The goals of this systematic review are to: 1) provide an overview of the existing literature that empirically tests the weathering hypothesis across a variety of physical health outcomes; 2) assess the evidence for weathering as a determinant of racial disparities in health; and 3) evaluate the threats to validity of existing studies.
METHODS
Search Strategy
The systematic review methodology and reporting followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines for a review that does not contain a meta-analysis of studies. [18] First, a citation search was conducted in Web of Science to identify all articles published by Geronimus as well as articles that cited her original publications [14, 15] describing the weathering hypothesis. Second, keyword and medical subject headings searches in Ovid MEDLINE (MeSH), PubMed (MeSH) and Embase (Emtree) electronic databases were employed from the first mention of the hypothesis in 1986 to July 1, 2017; the keyword “weathering” was combined with the keyword “racial disparities” and MeSH terms (e.g. health status disparities, health care disparities, inequalities, ethnic group, race difference) to identify relevant articles for the systematic review. Third, the reference lists of the: 1) included studies, 2) conceptual/review articles identified in the search process, and 3) grey literature (non-peer reviewed) were examined to identify additional studies. All retrieved articles were imported and stored in an EndNote database.
Inclusion and Exclusion Criteria
Inclusion criteria for articles included in this review were as follows: 1) published in English-language peer-reviewed journals; 2) contained a statement in the abstract, introduction or methods that the weathering hypothesis was being tested in relation to physical health outcomes; and 3) compared at least one disadvantaged group with one advantaged group.
Study Selection
Applying the selection criteria to the retrieved articles, one reviewer examined the titles and abstracts for full text review and two reviewers independently assessed the eligibility of the full text articles, reaching a consensus on the final articles to include in the systematic review.
Data Extraction
One reviewer used a data collection form (Supplemental Table 2) to extract data from the included articles and a second reviewer verified the extracted data to ensure accuracy. The publication characteristics (author name, publication year), study characteristics (data source), participant characteristics (age, sex), weathering hypothesis characteristics (type of test employed to test the weathering hypothesis); and study characteristics related to potential risks of bias (participant selection and retention) were recorded for each article.
Risk of Bias Assessment
The methodological quality of the included articles was assessed using the Quality in Prognostic Studies (QUIPS) tool, [19] which we adapted for this review (Supplemental Table 2) by dichotomizing studies as low (combined original QUIPS criteria for low and moderate risk) or high (original QUIPS criteria for high risk) risk, and replacing the term prognostic factor with exposure.
Two reviewers independently assessed the likelihood of bias by examining the extracted study information on potential risk of bias (Supplemental Table 1) and then using the QUIPS (Supplemental Table 2) ‘basis for judgment’ criteria for six bias domains (study participation, study attrition, exposure measurement, outcome measurement, confounding, and statistical analysis and reporting) as a guide for evaluating the likelihood of bias. When reviewers disagreed on bias assessments, the studies in question (n=4) were formally discussed by both reviewers to arrive at a final decision.
RESULTS
The citation and database searches identified 817 records (Figure 1). After removal of duplicates, 617 articles were eligible for the title and abstract review, of which 341 articles underwent full-text review. Of these, 298 were excluded because they did not test the weathering hypothesis. Three studies were excluded because they lacked a comparison group. One additional article was added after reviewing the reference lists. In total, 41 articles were included in this review.
Figure 1.
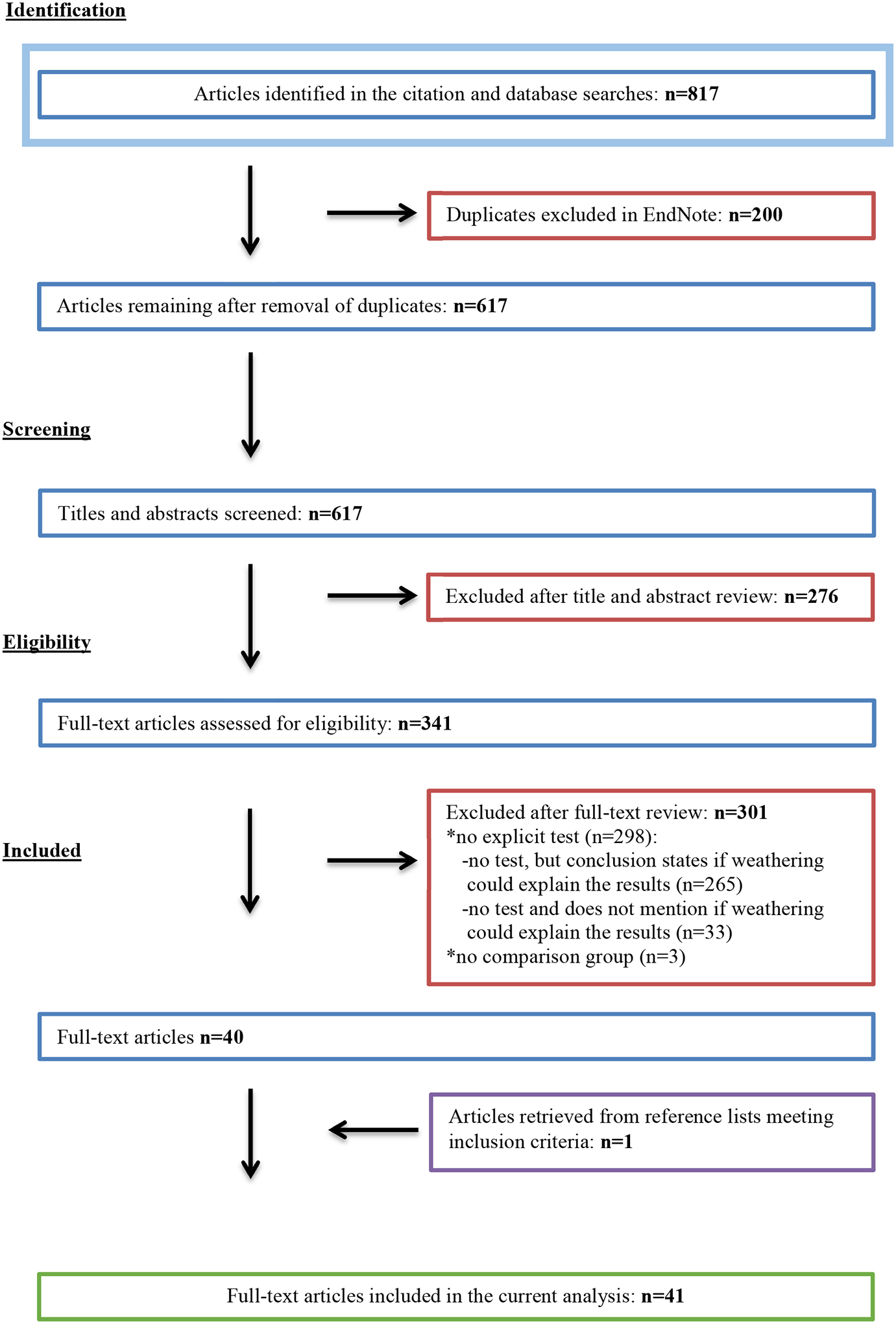
Flow Chart
Study and Participant Characteristics
The study and participant characteristics are presented in Table 1. The 41 studies in the review were published between 1996 and 2017. Most studies (78%) used a cross-sectional design and the remaining 22% of studies employed a cohort design. Only two studies were conducted outside of the U.S. (Taiwan and the United Kingdom). Study participant data were obtained from vital statistics and/or census data alone in 46% of studies or solely from survey data in 54% of studies. Sample sizes ranged from 100 to 26,578,118 participants, ages 10 to 86+ years. Females were the focus of 73% of studies, while 2% of studies included men only and 25% included both men and women.
Table 1.
Characteristics of Selected Studies Explicitly Testing the Weathering Hypothesis
| Participant Characteristics | Study Characteristics | Weathering Hypothesis | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Author & Publication Year | Age | Sex | Race/Ethnicity/Nativity | Geographic Location | Data Source | Sample Size | Study Design | Physical Health Outcome | Evidence of Weathering |
| Bird 2010 | 20–86y | Men & Women | -Blacks -Mexican Americans -Whites |
U.S. | NHANES III | 13,184 | Cross-sectional | -Allostatic load | Yes |
| Borrell 2010 | 25–65+y | Men & Women | -Blacks -Mexican Americans -Whites |
U.S. | NHANES III & NDI | 13,715 | Cohort | -All-cause mortality | Yes |
| Buescher 2006 | 15–35+y | Women | -Blacks -Whites |
North Carolina | BRFSS & North Carolina birth & infant death records | 495,551 | Cross-sectional | -Low birthweight, -Very low birthweight -Infant mortality -Neonatal mortality -Postneonatal mortality -Body mass index -High blood pressure -High cholesterol -Poor self-reported health |
Yes |
| Chinn 2016 | 18–85y | Women | -U.S.-born Black Hispanics -Foreign-born Black Hispanics -U.S.-born White Hispanics -Foreign-born White Hispanics -U.S.-born other-race Hispanics -Foreign-born other-race Hispanics |
U.S. | NHIS | 42,908 | Cross-sectional | -Functional Limitations | Yes |
| Chyu 2011 | 18–70+y | Women | -Blacks -U.S.-born Mexican Americans -Foreign-born Mexican Americans -Whites |
U.S. | NHANES IV | 5765 | Cross-sectional | -Allostatic load | Yes |
| Cohen 2016 | 12–40+y | Women | -Blacks -Mexican Americans -Whites |
U.S. | NCHS | 2,960,578 | Cross-sectional | -Infant mortality | Yes |
| Collins 2006 | <20–40+y | Women | -Extremely-Impoverished Blacks -Non-Impoverished Blacks |
Illinois | Illinois Vital Records, U.S. Census & Chicago Department of Public Health data | 46,725 | Cross-sectional | -Very low birthweight -Moderately low birthweight |
Yes |
| Collins 2009 | 14–35y | Women | -Blacks -Whites (stratified by early-life/adulthood residence income: low/low, low/high, high/low, high/high) |
Illinois | Illinois transgenerational dataset & U.S. Census | 267,303 | Cross-sectional | -Low birthweight | Yes |
| Collins 2012 | <20–35y | Women | -U.S.-born Mexican Americans -Foreign-born Mexican Americans |
Illinois | Illinois transgenerational dataset & U.S. Census | 267,303 | Cross-sectional | -Low birthweight -Preterm birth -Intrauterine growth retardation (IUGR) |
No |
| Collins 2015 | 14–35y | Women | -Former-low birthweight Blacks -Former-low birthweight Whites -Non-low birthweight Blacks -Non-low birthweight Whites |
Illinois | Illinois transgenerational dataset & U.S. Census | 70,580 | Cross-sectional | -Low birthweight -Small for gestational age |
Yes |
| Das 2013 | 57–85y | Men | -Blacks -Whites |
U.S. | NSHAP | 1455 | Cross-sectional | -Metabolic outcomes (blood sugar/diabetes, blood pressure, heart rate) | Yes |
| Dennis 2013 | 15–35y | Women | -Blacks -U.S.-born Hispanics -Foreign-born Hispanics -Whites |
U.S. | ECLS-B | 6150 | Cross-sectional | -Low birthweight | Yes |
| Geronimus 1996 | 15–34y | Women | -Blacks -Whites |
Michigan | Michigan Vital Records & U.S. Census | 54,888 | Cross-sectional | -Low birthweight -Very low birthweight |
Yes |
| Geronimus 2006 | 18–64y | Men & Women | -Blacks -Whites |
U.S. | NHANES IV | 6586 | Cross-sectional | -Allostatic load | Yes |
| Geronimus 2007 | 15–65y | Men & Women | -Blacks -Whites |
U.S. | NHANESIV | 5501 | Cross-sectional | -Hypertension | Yes |
| Geronimus 2010 | 49–55y | Women | -Blacks -Whites |
Boston, Chicago, Detroit, Oakland, Los Angeles, Newark, Pittsburgh | SWAN | 215 | Cohort | -Telomere length | Yes |
| Geronimus 2015 | 25–75+y | Men & Women | -Blacks -Mexican Americans -Whites |
Detroit | HEP Community Survey | 202 | Cross-sectional | -Telomere length | Yes |
| Goisis 2014 | 14–30+y | Women | -Blacks -Whites (stratified by area-level advantage/disadvantage, high/low education) |
United Kingdom | ONSLS | 45,856 | Cross-sectional | -Low birthweight | Yes |
| Hibbs 2016 | 14–35y | Women | -Black smokers & nonsmokers -White smokers & nonsmokers (stratified by quartiles of neighborhood income) |
Illinois | Illinois transgenerational dataset & U.S. Census | 267,303 | Cross-sectional | -Preterm birth | Yes |
| Holzman 2009 | 20–39y | Women | -Black smokers & nonsmokers -White smokers & nonsmokers (stratified by low/medium/high neighborhood deprivation) |
Philadelphia, Baltimore, 16 Michigan cities, 3 Maryland counties, 2 North Carolina counties | The Multilevel Modeling of Disparities Explaining Preterm Delivery Project & U.S. census | 182,938 | Cross-sectional | -Preterm birth | Yes |
| Howard 2016 | 25+y | Men & Women | -Blacks -Mexican Americans -Whites |
U.S. | NHANES III & NDI | 11,733 | Cross-sectional | -Mortality | Yes |
| Kaestner 2009 | 30–60y | Men & Women | -Blacks -U.S.-born Mexican Americans -Foreign-born Mexican Americans -Whites |
U.S. | NHANES III | 7010 | Cross-sectional | -Allostatic load | Yes |
| Khoshnood 2005 | 20–35+y | Women | -Blacks -Mexican Americans -Puerto Ricans -Whites |
U.S. | NCHS | 8,433,935 | Cross-sectional | -Low birthweight -Moderately low birthweight -Very low birthweight |
Yes |
| Kramer 2014 | 10–35+y | Women | -Blacks -Hispanics -Whites (stratified by low & high neighborhood deprivation) |
Georgia | Georgia birth records & U.S. Census | 1,000,437 | Cohort | -Preterm-low birthweight | Yes |
| Lin 2017 | 55–65y | Men & Women | -Blacks -Hispanics -Whites |
U.S. | HRS | 7715 | Cohort | -Functional limitations | Yes |
| Love 2010 | <20–35y | Women | -Blacks -Whites (stratified by early/adult neighborhood income: lower-lower, upper-lower, lower-upper, upperupper lifetime) |
Illinois | Illinois transgenerational dataset & U.S. Census | 70,615 | Cross-sectional | -Low birthweight -Small for gestational age -Preterm birth |
Yes |
| Osypuk 2008 | 15–45y | Women | -Blacks -Whites (stratified by segregation status: nonhypersegrated & hypersegregated metropolitan area) |
U.S. | NCHS & U.S. Census | 1,944,703 | Cross-sectional | -Preterm birth | Yes |
| Peek 2010 | 25–65+y | Men & Women | -Blacks -U.S.-born Mexican Americans -Foreign-born Mexican Americans -Whites |
Texas City | Texas City Stress & Health Study | 1410 | Cross-sectional | -Allostatic load | Yes |
| Powers 2013 | <20–40+y | Women | -Blacks -U.S.-born Mexican Americans -Foreign-born Mexican Americans -Whites |
U.S. | NCHS | 26,578,118 | Cross-sectional | -Infant mortality | Yes |
| Powers 2016 | 25–40+y | Women | -U.S.-born Mexican Americans -Foreign-born Mexicans Americans -Whites |
U.S. | NCHS | 14,542,120 | Cross-sectional | -Infant Mortality | Yes |
| Rauh 2001 | 20–39y | Women | -Blacks -Whites |
New York City | Bureau of vital statistics, New York City Department of Health & U.S. Census | 158,174 | Cross-sectional | -Moderately low birth weight -Very low birthweight |
Yes |
| Sheeder 2006 | 18–34y | Women | -Blacks -Hispanics -Whites |
Colorado | Colorado birth certificate data | 91,061 | Cross-sectional | -Small for gestational age | Yes |
| Simons 2016 | Mean=48.5y | Women | -Blacks | Georgia & Iowa | FACHS | 100 | Cohort | -Epigenetic measure of biological aging/methylation | Yes |
| Spence 2008 | 65–83y | Women | -Blacks -Whites |
U.S. | NLS-MW | 1608 | Cohort | -Functional limitations | No |
| Spence 2009 | 45–59y | Women | -Blacks -Whites |
U.S. | NLS-MW | 3769 | Cohort | -Longevity (post reproductive mortality) | Yes |
| Strutz 2014 | 11–32y | Women | -Blacks -Mexican Americans -Non-Mexican Latinas -Whites |
U.S. | Add Health | 5413 | Cohort | -Birthweight | Yes |
| Swamy 2012 | 15–44y | Women | -Blacks -Hispanics -Whites |
North Carolina | North Carolina birth record database | 510,288 | Cross-sectional | -Mean birthweight | Yes |
| Thorpe 2016 | 18–75+ | Men & Women | -Blacks -Whites |
U.S. | NHIS | 619,130 | Cross-sectional | -Hypertension -Stroke -Diabetes -Cardiovascular Disease |
Yes |
| Wallace 2013 | 20–35y | Women | -Blacks -Whites |
New Orleans | Tulane-Lakeside Hospital Department of Obstetrics & Gynecology | 123 | Cohort | -Birthweight, -Birthweight ratio -Gestational age -Birth length -Head circumference |
Yes |
| Wang 2012 | 15–35y | Women | -Aboriginals -Non-Aboriginals |
Taiwan | Taiwan birth registration database | 8432 | Cross-sectional | -Low birthweight or preterm birth | No |
| Wildsmith 2002 | 15–34y | Women | -U.S.-born Mexican Americans -Foreign-born Mexican Americans |
U.S. | NCHS | 387,909 | Cross-sectional | -Low birthweight -Anemia -Hypertension -Neonatal mortality |
Yes |
Add Health=National Longitudinal Study of Adolescent Health
BRFSS=Behavioral Risk Factor Surveillance System
ECLSB= Early Childhood Longitudinal Study-Birth Cohort
FACHS=Family and Community Health Study
HEP= The Healthy Environment Partnership
HRS=Health and Retirement Study
NCHS=National Center for Health Statistics
NDI=National Death Index
NHANES=National Health and Nutrition Examination Survey
NHIS=National Health Interview Survey
NLS-MW=National Longitudinal Survey of Mature Women
NSHAP= National Social Life, Health and Aging Project
ONSLS=Office for National Statistics longitudinal study
SWAN=Study of Women’s Health Across the Nation
The weathering hypothesis was tested most often for birth outcomes (58%). Potentially disadvantaged racial or ethnic groups to whom the weathering hypothesis was applied included U.S.-born Blacks, non-U.S.-born Blacks, Puerto Ricans, Black Hispanics, U.S.-born Mexican Americans, and Taiwan-born Aboriginals. In comparison, advantaged groups included Whites, White Hispanics, foreign-born Mexican Americans, and Non-Aboriginals. (Table 1) Black and White racial group comparisons appeared the most frequently across the studies (80%). Fifty one percent of the studies included disadvantaged groups other than Blacks and 22% of studies examined weathering by nativity status.
Overview of the Evidence by Type of Test of the Weathering Hypothesis
Age patterns.
Comparing the age patterns of health outcomes was employed as one of the first approaches to determine the presence of weathering. Among the 28 studies that used the age patterns test of weathering (Table 2a, Table 2b), evidence of weathering was more likely to be observed in studies on birth outcomes (37/44 tests) [low birthweight (11/14), [15, 20–27] mean birthweight (1/1), [28] moderately low birthweight (5/5), [23, 29, 30] very low birthweight (6/7), [15, 20, 23, 29] infant mortality (5/5), [20, 31–33] neonatal mortality (2/2), [20, 34] postneonatal mortality (1/1), [20] preterm birth (3/5), [35–37] small for gestational age (3/3), [21, 24, 38] and intrauterine growth retardation (0/1)] and for non-birth outcomes (11/15) [body mass index (1/1), [20] diabetes (1/1), [39] hypertension/blood pressure (4/4), [20, 34, 39, 40] stroke (1/1), [39] functional limitations (2/3), [41, 42] longevity (1/1), [43] self-reported health (1/1), [20] cardiovascular disease (0/1), cholesterol (0/1), and anemia (0/1)].
Table 2a.
Summary of the Evidence Among Studies Supporting the Weathering Hypothesis
| Author and Publication Year | Health Outcome | Population for Which Weathering was Hypothesized to Have the Greatest Impact | Comparison Population | Weathering Patterns by Socioeconomic Status (SES) * |
|---|---|---|---|---|
| Birth Outcomes | ||||
| Birthweight | ||||
| Buescher 2006 | Low birthweight | Blacks | Whites | • N/A |
| Collins 2009 | Low birthweight | N/A | N/A | • Weathering more pronounced in Blacks with lifelong residence in lower SES neighborhoods |
| Collins 2015 | Low birthweight | Former non-low birthweight Blacks | Whites, Former low birthweight Blacks | • Weathering more pronounced in non-low birthweight Blacks in lower SES neighborhoods |
| Dennis 2013 | Low birthweight | Blacks | Whites, Hispanics (U.S. born or Foreign-born) | • N/A |
| Geronimus 1996 | Low birthweight | Blacks | Whites | • Weathering more pronounced in lower SES Blacks |
| Goisis 2014 | Low birthweight | U.K. Blacks | U.K. Whites | • Weathering more pronounced in less-educated Blacks and Blacks in lower SES neighborhoods |
| Khoshnood 2005 | Low birthweight | Blacks | Whites | • N/A |
| Khoshnood 2005 | Low birthweight | Mexican Americans | Whites | • N/A |
| Khoshnood 2005 | Low birthweight | Puerto Ricans | Whites | • N/A |
| Kramer 2014 | Preterm-low birthweight | N/A | N/A | • Weathering more pronounced in Blacks with higher neighborhood deprivation |
| Love 2010 | Low birthweight | Blacks | Whites | • Weathering more pronounced in Blacks with lifelong residence in lower SES neighborhoods |
| Swamy 2012 | Mean birthweight | Blacks | Whites, Hispanics | • N/A |
| Collins 2006 | Moderately low birthweight | N/A | N/A | • Weathering more pronounced in Blacks living in lower SES neighborhoods |
| Khoshnood 2005 | Moderately low birthweight | Blacks | Whites | • N/A |
| Khoshnood 2005 | Moderately low birthweight | Mexican Americans | Whites | • N/A |
| Khoshnood 2005 | Moderately low birthweight | Puerto Ricans | Whites | • N/A |
| Rauh 2001 | Moderately low birthweight | Blacks | Whites | • Weathering more pronounced in lower SES Blacks |
| Buescher 2006 | Very low birthweight | Blacks | Whites | • N/A |
| Geronimus 1996 | Very low birthweight | Blacks | Whites | • Weathering more pronounced in lower SES Blacks |
| Khoshnood 2005 | Very low birthweight | Blacks | Whites | • N/A |
| Khoshnood 2005 | Very low birthweight | Mexican Americans | Whites | • N/A |
| Khoshnood 2005 | Very low birthweight | Puerto Ricans | Whites | • N/A |
| Rauh 2001 | Very low birthweight | Blacks | Whites | • No difference by SES |
| Mortality | ||||
| Buescher 2006 | Infant mortality | Blacks | Whites | • N/A |
| Cohen 2016 | Infant mortality | Blacks | Whites, Mexican Americans | • N/A |
| Powers 2013 | Infant mortality | Blacks | Whites | • N/A |
| Powers 2013 | Infant mortality | Mexican Americans | Whites | • N/A |
| Powers 2016 | Infant mortality | Mexican Americans | Whites | • N/A |
| Buescher 2006 | Neonatal mortality | Blacks | Whites | • N/A |
| Wildsmith 2002 | Neonatal mortality | U.S.-born Mexican Americans | Foreign-born Mexican Americans | • N/A |
| Buescher 2006 | Postneonatal mortality | Blacks | Whites | • N/A |
| Preterm birth | ||||
| Hibbs 2016 | Preterm birth | N/A | N/A | • Weathering more pronounced among cigarette smoking Blacks with early-life or lifelong residence in lower SES neighborhoods |
| Holzman 2009 | Preterm birth | Black smokers, Black nonsmokers, White smokers | White non-smokers | • Weathering more pronounced in Black and White smokers with higher neighborhood deprivation |
| Osypuk 2008 | Preterm birth | Blacks | Whites | • Weathering more pronounced for Blacks in hypersegregated neighborhoods |
| Small for gestational age | ||||
| Collins 2015 | Small for gestational age | Former non-low birthweight Blacks | Whites, former low birth-weight Blacks | • Weathering more pronounced in former non-low birthweight Blacks in lower SES neighborhoods |
| Love 2010 | Small for gestational age | Blacks | Whites | • Weathering more pronounced in Blacks with lifelong residence in lower SES neighborhoods |
| Sheeder 2006 | Small for gestational age | Blacks | Whites, Hispanics | • N/A |
| Non-Birth Outcomes | ||||
| Cardiovascular health | ||||
| Buescher 2006 | Body mass index | Blacks | Whites | • N/A |
| Thorpe 2016 | Diabetes | Blacks | Whites | • N/A |
| Buescher 2006 | High blood pressure | Blacks | Whites | • N/A |
| Geronimus 2007 | Hypertension | Blacks | Whites | • N/A |
| Thorpe 2016 | Hypertension | Blacks | Whites | • N/A |
| Wildsmith 2002 | Hypertension | U.S.-born Mexican Americans | Foreign-born Mexican Americans | • N/A |
| Thorpe 2016 | Stroke | Blacks | Whites | • N/A |
| Function | ||||
| Chinn 2016 | Functional limitations | U.S.-born Black Hispanics | White, Other-race Hispanics (U.S. and foreign-born), Foreign-born Black Hispanics | • N/A |
| Lin 2017 | Functional limitations | Blacks | Whites, Hispanics | • N/A |
| Other physical health outcomes | ||||
| Spence 2009 | Longevity | Blacks | Whites | • N/A |
| Buescher 2006 | Poor self-reported health | Blacks | Whites | • N/A |
Represents studies for which a group comparison for testing the weathering hypothesis was defined by SES alone, or in addition to a comparison defined by membership in a historically disadvantaged minority group versus an advantaged group.
U.S.=United States. U.K.=United Kingdom. N/A=not applicable.
Table 2b.
Summary of the Evidence Among Studies Not Supporting the Weathering Hypothesis
| Author and Publication Year | Health Outcome | Population for Which Weathering was Hypothesized to Have the Greatest Impact | Comparison Population | Weathering Patterns by Socioeconomic Status (SES) * |
|---|---|---|---|---|
| Birth Outcomes | ||||
| Birthweight | ||||
| Collins 2012 | Low birthweight | U.S.-born Mexican Americans | Foreign-born Mexican Americans | • No difference by neighborhood SES |
| Wildsmith 2002 | Low birthweight | U.S.-born Mexican Americans | Foreign-born Mexican Americans | • N/A |
| Wang 2013 | Low birthweight or preterm birth | Aboriginal | Non-Aboriginal | • N/A |
| Collins 2006 | Very low birthweight | N/A | N/A | • No difference by neighborhood SES |
| Other birth outcome | ||||
| Collins 2012 | Intrauterine growth retardation | U.S.-born Mexican Americans | Foreign-born Mexican Americans | • No difference by neighborhood SES |
| Preterm birth | ||||
| Collins 2012 | Preterm birth | U.S.-born Mexican Americans | Foreign-born Mexican Americans | • No difference by neighborhood SES |
| Love 2010 | Preterm birth | Blacks | Whites | • No difference by neighborhood SES |
| Non-Birth Outcomes | ||||
| Cardiovascular health | ||||
| Thorpe 2016 | Cardiovascular disease | Blacks | Whites | • N/A |
| Buescher 2006 | High cholesterol | Blacks | Whites | • N/A |
| Other physical health outcomes | ||||
| Spence 2008 | Functional limitations | Blacks | Whites | • N/A |
| Wildsmith 2002 | Anemia | U.S.-born Mexican Americans | Foreign-born Mexican Americans | • N/A |
Represents studies for which a group comparison for testing the weathering hypothesis was defined by SES alone, or in addition to a comparison defined by membership in a historically disadvantaged minority group versus an advantaged group.
U.S.=United States. N/A=not applicable.
While weathering age patterns were observed for most health outcomes, the results varied by the comparison group studied. Among the studies comparing the health of U.S. Blacks to Whites by age, all but four studies, (on preterm birth, [24] cholesterol level, [20] cardiovascular disease, [39] and functional limitations [44]) observed evidence of weathering. Given that this hypothesis is thought to have relevance for any disadvantaged population, evidence of weathering was also observed among disadvantaged groups, such as Blacks of Caribbean and African descent in the United Kingdom, [25] Puerto Ricans, [23] Mexican Americans [23, 31, 33, 34] and Black Hispanics. [42] However, evidence of weathering was not observed for any health outcome among the aggregated Hispanic ethnic group (for low birthweight, [22] mean birthweight, [28] small for gestational age, [38] functional limitations [41]) or among Taiwanese Aboriginals (for low birthweight [45]).
Socioeconomic Status.
In addition to studies that defined disadvantage by race or ethnicity, several studies [15, 21, 24–27, 29, 30, 35–37, 46] considered measures of socioeconomic disadvantage defined by individual or neighborhood poverty, education, and neighborhood segregation. Among these studies, 14/20 tests showed that weathering was more likely to be observed in the socioeconomically disadvantaged group than the socioeconomically advantaged group, and all studies supporting the weathering hypothesis were for birth outcomes [15, 21, 24–27, 29,30, 35–37] (Table 2a).
Biological/Physiological Mechanisms.
Several studies have investigated different biological/physiological mechanisms (i.e., allostatic load, telomere length, chronic stress, inflammation and epigenetics) hypothesized to link chronic exposure to social/economic disadvantage to racial or ethnic health disparities. Among thirteen studies, eight focused on allostatic load, two on telomere length and one study each on chronic stress, inflammation and epigenetics (Table 3).
Table 3.
Summary of the Evidence for Studies Exploring Biological/Physiological Mechanisms Underlying the Weathering Hypothesis
| Author and Publication Y ear | Health Outcome | Evidence of Weathering in the Overall Population |
|---|---|---|
| Birth outcomes | ||
| Birthweight | ||
| Strutz 2014 | Birthweight |
|
| Wallace 2013 | Birth length |
|
| Wallace 2013 | Birthweight |
|
| Wallace 2013 | Birthweight ratio |
|
| Wallace 2013 | Head circumference |
|
| Gestational age | ||
| Wallace 2013 | Gestational age |
|
| Non-birth outcome | ||
| Allostatic load | ||
| Bird 2010 | Allostatic load |
|
| Chyu 2011 | Allostatic load |
|
| Geronimus 2006 | Allostatic load |
|
| Kaestner 2009 | Allostatic load |
|
| Peek 2010 | Allostatic load |
|
| Cardiovascular Health | ||
| Das 2013 | Metabolic outcomes |
|
| Genetic Outcomes | ||
| Simons 2016 | Epigenetic measure/Methylation |
|
| Geronimus 2010 | Telomere length |
|
| Geronimus 2015 | Telomere length |
|
| Mortality | ||
| Borrell 2010 | All-cause mortality |
|
| Howard 2016 | Mortality |
|
U.S.=United States. -- =no evidence of weathering.
Five studies [47–51] included allostatic load as the primary health outcome and reported results that were supportive of weathering when considering either race or ethnicity [47–51] or socioeconomic status [47, 51] as measures of disadvantage (Table 3). Three additional studies [52–54] examining allostatic load as the primary exposure also showed evidence of weathering, where higher allostatic load was associated with increased mortality rates [52, 53] and lower gestational age [54] (Table3).
Studies on telomere length, chronic stress, inflammation and epigenetics also found support for weathering. Regarding telomere length as a marker of biological age, one study [55] reported that Black women had shorter telomere length than White women and the difference was partially explained by perceived stress and poverty. Another study [56] showed decreasing telomere length with age and observed an interaction between poverty and race or ethnicity. Chronic stress was associated with lower birthweight in Blacks, Mexican-origin Latinas and Non-Mexican-origin Latinas compared to Whites. [57] Inflammation arising from cumulative exposure to stress placed Black men at a greater risk for developing diabetes and cardiovascular disease than White men. [58] Having lower income versus higher income resulted in accelerated aging (as measured by methylation changes) among Black women [59] (Table 3).
Overall, most studies provided evidence in support of weathering that was more pronounced in racial or ethnic minority groups, lower SES groups and segregated neighborhoods, but results for studies including biological mechanisms were not necessarily restricted to racial or ethnic minority groups. (Table 3). Most studies were of good methodological quality (Table 4), but there were potential threats to validity most likely arising from selection bias.
Table 4.
Potential Risk of Bias Assessment for the Included Studies
| Author & Publication Year | Evidence of Weathering | Health Outcome | Geographic Location | Dataset | Sample Size | Study Design | Study Participation | Study Attrition | Exposure Measurement | Outcome Measurement | Study Confounding | Statistical Analysis & Reporting | Overall Potential for Bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Geronimus 2010 | Yes | Telomere length | Boston, Chicago, Detroit, Oakland, Los Angeles, Newark, Pittsburgh | SWAN | 215 | Cohort | High | High | Low | Low | Low | Low | High |
| Simons 2016 | Yes | Epigenetic measure of biological aging/methylation | Georgia & Iowa | FACHS | 100 | Cohort | High | High | Low | Low | Low | Low | High |
| Wallace 2013 | Yes | Gestational age | Louisiana | Tulane-Lakeside Hospital Department of Obstetrics &Gynecology | 123 | Cohort | High | High | Low | Low | Low | Low | High |
| Wallace 2013 | No | Birthweight | Louisiana | Tulane-Lakeside Hospital Department of Obstetrics & Gynecology | 123 | Cohort | High | High | Low | Low | Low | Low | High |
| Wallace 2013 | No | Birthweight ratio | Louisiana | Tulane-Lakeside Hospital Department of Obstetrics & Gynecology | 123 | Cohort | High | High | Low | Low | Low | Low | High |
| Wallace 2013 | No | Birth length | Louisiana | Tulane-Lakeside Hospital Department of Obstetrics & Gynecology | 123 | Cohort | High | High | Low | Low | Low | Low | High |
| Wallace 2013 | No | Head circumference | Louisiana | Tulane-Lakeside Hospital Department of Obstetrics & Gynecology | 123 | Cohort | High | High | Low | Low | Low | Low | High |
| Spence 2008 | No | Functional limitations | U.S. | NLS-MW | 1608 | Cohort | Low | High | Low | Low | Low | Low | High |
| Borrell 2010 | Yes | All-cause mortality | U.S. | NHANES III & NDI | 13,715 | Cohort | Low | High | Low | Low | Low | Low | High |
| Kramer 2014 | Yes | Preterm-low birthweight | Georgia | Georgia birth records & U.S. Census | 1,000,437 | Cohort | Low | High | Low | Low | Low | Low | High |
| Lin 2017 | Yes | Functional limitations | U.S. | HRS | 7715 | Cohort | Low | High | Low | Low | Low | Low | High |
| Spence 2009 | Yes | Longevity (post reproductive mortality) | U.S. | NLS-MW | 3769 | Cohort | Low | High | Low | Low | Low | Low | High |
| Strutz 2014 | Yes | Birthweight | U.S. | Add Health | 5413 | Cohort | Low | High | Low | Low | Low | Low | High |
| Geronimus 2015 | Yes | Telomere length | Detroit | HEP Community Survey | 202 | Cross-sectional | High | Low | Low | Low | Low | Low | High |
| Buescher 2006 | Yes | High blood pressure | North Carolina | BRFSS & North Carolina birth & infant death records | 495,551 | Cross-sectional | Low | Low | Low | High | High | Low | High |
| Buescher 2006 | Yes | Body mass index | North Carolina | Behavioral BRFSS & North Carolina birth & infant death records | 495,551 | Cross-sectional | Low | Low | Low | High | High | Low | High |
| Buescher 2006 | No | Cholesterol | North Carolina | BRFSS & North Carolina birth & infant death records | 495,551 | Cross-sectional | Low | Low | Low | High | High | Low | High |
| Wildsmith 2002 | Yes | Hypertension | U.S. | NCHS | 387, 909 | Cross-sectional | Low | Low | Low | High | High | Low | High |
| Wildsmith 2002 | No | Anemia | U.S. | NCHS | 387,909 | Cross-sectional | Low | Low | Low | High | High | Low | High |
| Thorpe 2016 | Yes | Diabetes | U.S. | NHIS | 619,130 | Cross-sectional | Low | Low | Low | High | Low | Low | High |
| Thorpe 2016 | Yes | Hypertension | U.S. | NHIS | 619,130 | Cross-sectional | Low | Low | Low | High | Low | Low | High |
| Thorpe 2016 | Yes | Stroke | U.S. | NHIS | 619,130 | Cross-sectional | Low | Low | Low | High | Low | Low | High |
| Thorpe 2016 | No | Cardiovascular disease | U.S. | NHIS | 619,130 | Cross-sectional | Low | Low | Low | High | Low | Low | High |
| Buescher 2006 | Yes | Infant mortality | North Carolina | BRFSS & North Carolina birth & infant death records | 495,551 | Cross-sectional | Low | Low | Low | Low | High | Low | High |
| Buescher 2006 | Yes | Low birth weight | North Carolina | BRFSS & North Carolina birth & infant death records | 495,551 | Cross-sectional | Low | Low | Low | Low | High | Low | High |
| Buescher 2006 | Yes | Neonatal mortality | North Carolina | BRFSS & North Carolina birth & infant death records | 495,551 | Cross-sectional | Low | Low | Low | Low | High | Low | High |
| Buescher 2006 | Yes | Postneonatal mortality | North Carolina | Behavioral Risk Factor Surveillance System (BRFSS) & North Carolina birth & infant death records | 495,551 | Cross-sectional | Low | Low | Low | Low | High | Low | High |
| Buescher 2006 | Yes | Self-reported health | North Carolina | BRFSS & North Carolina birth & infant death records | 495,551 | Cross-sectional | Low | Low | Low | Low | High | Low | High |
| Buescher 2006 | Yes | Very low birth weight | North Carolina | BRFSS & North Carolina birth & infant death records | 495,551 | Cross-sectional | Low | Low | Low | Low | High | Low | High |
| Wildsmith 2002 | Yes | Neonatal mortality | U.S. | NCHS | 387, 909 | Cross-sectional | Low | Low | Low | Low | High | Low | High |
| Wildsmith 2002 | No | Low birthweight | U.S. | NCHS | 387,909 | Cross-sectional | Low | Low | Low | Low | High | Low | High |
| Bird 2010 | Yes | Allostatic load | U.S. | NHANES III | 13,184 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Chinn 2016 | Yes | Functional limitations | U.S. | NHIS | 42,908 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Collins 2006 | No | Very low birth weight | Illinois | Illinois Vital Records, U.S. Census & Chicago Department of Public Health data | 46,725 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Chyu 2011 | Yes | Allostatic load | U.S. | NHANES IV | 5765 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Cohen 2016 | Yes | Infant mortality | U.S. | NCHS | 2,960,578 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Collins 2006 | Yes | Moderately low birth weight | Illinois | Illinois Vital Records, U.S. Census & Chicago Department of Public Health data | 46,725 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Collins 2009 | Yes | Low birth weight | Illinois | Illinois transgeneration al dataset & U.S. Census | 267,303 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Collins 2012 | No | Low birthweight | Illinois | Illinois transgeneration al dataset & U.S. Census | 267,303 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Collins 2012 | No | Preterm birth | Illinois | Illinois transgeneration al dataset & U.S. Census | 267,303 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Collins 2012 | No | Intrauterine growth retardation | Illinois | Illinois transgeneration al dataset & U.S. Census | 267,303 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Collins 2015 | Yes | Low birth weight | Illinois | Illinois transgeneration al dataset & U.S. Census | 70,580 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Collins 2015 | Yes | Small for gestational age | Illinois | Illinois transgeneration al dataset & U.S. Census | 70,580 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Das 2013 | Yes | Metabolic outcomes (blood sugar/diabetes blood pressure, heart rate) | U.S. | NSHAP | 1455 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Dennis 2013 | Yes | Low birth weight | U.S. | ECLS-B | 6150 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Geronimus 1996 | Yes | Low birth weight | Michigan | Michigan Vital Records & U.S. Census | 54,888 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Geronimus 1996 | Yes | Very low birth weight | Michigan | Michigan Vital Records & U.S. Census | 54,888 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Geronimus 2006 | Yes | Allostatic load | U.S. | NHANESIV | 6586 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Geronimus 2007 | Yes | Hypertension | U.S. | NHANES IV | 5501 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Goisis 2014 | Yes | Low birth weight | United Kingdom | ONSLS | 45,856 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Hibbs 2016 | Yes | Preterm birth | Illinois | Illinois transgeneration al dataset & U.S. Census | 267,303 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Holzman 2009 | Yes | Preterm birth | Philadelphia, Baltimore, 16 Michigan cities, 3 Maryland counties, 2 North Carolina counties | The Multilevel Modeling of DisparitiesExpl aining Preterm Delivery Project & U.S. census | 182,938 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Howard 2016 | Yes | Mortality | U.S. | NHANES III & NDI | 11,733 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Kaestner 2009 | Yes | Allostatic load | U.S. | NHANES III | 7010 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Khoshnood 2005 | Yes | Low birth weight | U.S. | NCHS | 8,433,935 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Khoshnood 2005 | Yes | Moderately low birth weight | U.S. | NCHS | 8,433,935 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Khoshnood 2005 | Yes | Very low birth weight | U.S. | NCHS | 8,433,935 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Love 2010 | Yes | Low birth weight | Illinois | Illinois transgeneration al dataset & U.S. Census | 70,615 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Love 2010 | Yes | Small for gestational age | Illinois | Illinois transgeneration al dataset & U.S. Census | 70,615 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Love 2010 | No | Preterm birth | Illinois | Illinois transgeneration al dataset & U.S. Census | 70,615 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Osypuk 2008 | Yes | Preterm birth | U.S. | NCHS & U.S. Census | 1,944,703 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Peek 2010 | Yes | Allostatic load | Texas City | Texas City Stress & Health Study | 1410 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Powers 2013 | Yes | Infant mortality | U.S. | NCHS | 26,578,118 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Powers 2016 | Yes | Infant mortality | U.S. | NCHS | 14,542,120 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Rauh 2001 | Yes | Moderately low birth weight | New York City | Bureau of vital statistics, New York City Department of Health & U.S. Census | 158,174 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Rauh 2001 | Yes | Very low birth weight | New York City | Bureau of vital statistics, New York City Department of Health & U.S. Census | 158,174 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Sheeder 2006 | Yes | Small for gestational age | Colorado | Colorado birth certificate data | 91,061 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Swamy 2012 | Yes | Mean birth weight | North Carolina | North Carolina birth record database | 510,288 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
| Wang 2012 | No | Low birthweight or preterm birth | Taiwan | Taiwan birth registration | 8432 | Cross-sectional | Low | Low | Low | Low | Low | Low | Low |
Add Health=National Longitudinal Study of Adolescent Health
BRFSS=Behavioral Risk Factor Surveillance System
ECLSB= Early Childhood Longitudinal Study-Birth Cohort
FACHS=Family and Community Health Study
HEP= The Healthy Environment Partnership
HRS=Health and Retirement Study
NCHS=National Center for Health Statistics
NDI=National Death Index
NHANES=National Health and Nutrition Examination Survey
NHIS=National Health Interview Survey
NLS-MW=National Longitudinal Survey of Mature Women
NSHAP= National Social Life, Health and Aging Project
ONSLS=Office for National Statistics longitudinal study
SWAN= Study of Women’s Health Across the Nation
DISCUSSION
The weathering hypothesis has been tested for several health outcomes among a diverse group of participants. Most studies focused on birth outcomes for Blacks versus Whites, consistent with the original framing of the weathering hypothesis. Generally, however, findings supported the weathering hypothesis for both birth and non-birth outcomes. The most common approach used to test the weathering hypothesis was to compare disadvantaged to advantaged groups across different ages to determine if age-related patterns of adverse health outcomes were accelerated among disadvantaged versus advantaged groups. Fewer studies focused on biological mechanisms explaining these patterns or how SES may exacerbate the relationship between age and poor health.
This review identified a diverse literature on the weathering hypothesis that was determined to be of good methodological quality, although there was some concern about the potential for selection bias and the temporal ambiguity. The cross-sectional nature of the data prevented the longitudinal examination of health outcomes over the life course and introduced potential selection bias. Specifically, prevalence-incidence bias or selective survival bias was a possibility because a disproportionately high percentage of cases with long duration (prevalent cases) and better average survival could have been included in cross-sectional studies, whereas, those with shorter duration (incident cases) who represented the complete range of severity of the health outcome would have a lower probability of being included. The studies that examined short-acting health conditions were less likely to be impacted by this bias. Among the cohort studies, there appeared to be adequate response rates and attempts to collect information on participants who were not included in the studies, but studies with significant differences in participation and attrition were judged as being more likely to have appreciable selection bias that impacted the results. In contrast, while temporality in cross-sectional studies is often difficult to establish, temporal inference in the context of weathering is less problematic, as weathering is presumed to begin at birth (or even in utero) and therefore precede the health outcome.
While measurement error was less likely, the few studies rated as high risk for measurement error either failed to use valid and reliable measurements (e.g. self-reported outcomes that would only be reported if notified by a physician). Confounding was also less likely since most studies included valid and reliable measurement and analysis of confounders that were clearly defined.
Some important limitations of our review should be noted. Relevant studies that may have inexplicitly tested the weathering hypothesis, but were omitted because weathering or Geronimus’ seminal articles were not specified, were likely relevant to a comprehensive review of the weathering hypothesis. The presence of publications bias was likely, but there was not sufficient information to assess publication bias.
The weathering hypothesis has contributed significantly to the literature on racial disparities in birth outcomes. The number of studies that tested the applicability of this hypothesis to other outcomes and racial or ethnic groups has grown since the publication of Geronimus’ earliest studies on weathering and birth outcomes. However, few studies examined weathering within the Hispanic population by race or within the Black population by nativity status, making this an important target for future research on weathering. While discrimination was not examined in any of the studies, it may be experienced differently by Blacks than other racial and ethnic minority groups and therefore could explain racial or ethnic differences in weathering patterns. The rigor of future research can be enhanced by (1) studying clinical disease outcomes using gold standard outcome assessments (rather than participant self-report), (2) including additional health outcomes (e.g., cancer, dementia, pulmonary disease), (3) conducting analyses on the health of ethnic groups by race and on racial groups by nativity status, (4) characterizing the precise nature of social and economic disadvantage of most relevance (e.g., racial discrimination, neighborhood effects, poverty), and (5) utilizing longitudinal studies beginning early in the life-course to better characterize how disadvantage and health co-evolve over the life course.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to show our gratitude to Sharon Schwartz, PhD who provided many helpful insights during this review. This work was supported by the National Institutes of Health/National Heart, Lung, and Blood Institute [grant number 5F31HL117613-02].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Mensah GA, et al. , State of disparities in cardiovascular health in the United States. Circulation, 2005. 111(10): p. 1233–41. [DOI] [PubMed] [Google Scholar]
- 2.Mokdad AH, et al. , The continuing increase of diabetes in the US. Diabetes Care, 2001. 24(2): p. 412–412. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, et al. , Prevalence and trends in obesity among US adults, 1999–2008. Jama, 2010. 303(3): p. 235–241. [DOI] [PubMed] [Google Scholar]
- 4.Geronimus AT, et al. , Excess mortality among blacks and whites in the United States. N Engl J Med, 1996. 335(21): p. 1552–8. [DOI] [PubMed] [Google Scholar]
- 5.Levine RS, et al. , Black-white inequalities in mortality and life expectancy, 1933–1999: implications for healthy people 2010. Public Health Rep, 2001. 116(5): p. 474–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong MD, et al. , Contribution of major diseases to disparities in mortality. New England Journal of Medicine, 2002. 347(20): p. 1585–1592. [DOI] [PubMed] [Google Scholar]
- 7.Carter-Pokras O and Baquet C, What is a “health disparity”? Public Health Rep, 2002. 117(5): p. 426–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams DR and Collins C, US socioeconomic and racial differences in health: patterns and explanations. Annual review of sociology, 1995. 21(1): p. 349–386. [Google Scholar]
- 9.Williams DR, Miles to go before we sleep racial inequities in health. Journal of health and social behavior, 2012. 53(3): p. 279–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krieger N, Embodying inequality: epidemiologic perspectives. 2005: Baywood Publishing Company Inc. [Google Scholar]
- 11.Colen CG, Addressing racial disparities in health using life course perspectives. Du Bois Review: Social Science Research on Race, 2011. 8(01): p. 79–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adler NE and Stewart J, Health disparities across the lifespan: meaning, methods, and mechanisms. Annals of the New York Academy of Sciences, 2010. 1186(1): p. 5–23. [DOI] [PubMed] [Google Scholar]
- 13.Geronimus AT, Understanding and eliminating racial inequalities in women’s health in the United States: the role of the weathering conceptual framework. Journal of the American Medical Women’s Association (1972), 2000. 56(4): p. 133–6, 149–50. [PubMed] [Google Scholar]
- 14.Geronimus AT, The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethnicity & disease, 1992. 2(3): p. 207–21. [PubMed] [Google Scholar]
- 15.Geronimus AT, Black/white differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Social science & medicine, 1996. 42(4): p. 589–597. [DOI] [PubMed] [Google Scholar]
- 16.Geronimus AT, Andersen HF, and Bound J, Differences In Hypertension Prevalence Among United-States Black-And-White Women Of Childbearing Age. Public Health Reports, 1991. 106(4): p. 393–399. [PMC free article] [PubMed] [Google Scholar]
- 17.Geronimus AT, On Teenage Childbearing And Neonatal-Mortality In The United-States. Population and Development Review, 1987. 13(2): p. 245–279. [Google Scholar]
- 18.Moher D, et al. , Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International journal of surgery, 2010. 8(5): p. 336–341. [DOI] [PubMed] [Google Scholar]
- 19.Hayden JA, et al. , Assessing bias in studies of prognostic factors. Annals of internal medicine, 2013. 158(4): p. 280–286. [DOI] [PubMed] [Google Scholar]
- 20.Buescher PA and Mittal M, Racial disparities in birth outcomes increase with maternal age: recent data from North Carolina. N C Med J, 2006. 67(1): p. 16–20. [PubMed] [Google Scholar]
- 21.Collins JW, Rankin KM, and Hibbs S, The maternal age related patterns of infant low birth weight rates among non-latino whites and african-americans: The effect of maternal birth weight and neighborhood income. Maternal and child health journal, 2015. 19(4): p. 739–744. [DOI] [PubMed] [Google Scholar]
- 22.Dennis JA and Mollborn S, Young maternal age and low birth weight risk: An exploration of racial/ethnic disparities in the birth outcomes of mothers in the United States. Social Science Journal, 2013. 50(4): p. 625–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khoshnood B, Wall S, and Lee KS, Risk of low birth weight associated with advanced maternal age among four ethnic groups in the United States. Maternal and Child Health Journal, 2005. 9(1): p. 3–9. [DOI] [PubMed] [Google Scholar]
- 24.Love C, et al. , Exploring weathering: effects of lifelong economic environment and maternal age on low birth weight, small for gestational age, and preterm birth in African-American and white women. American journal of epidemiology, 2010: p. kwq109. [DOI] [PubMed] [Google Scholar]
- 25.Goisis A and Sigle-Rushton W, Childbearing Postponement and Child Well-being: A Complex and Varied Relationship? Demography, 2014. 51(5): p. 1821–1841. [DOI] [PubMed] [Google Scholar]
- 26.Kramer MR, Dunlop AL, and Hogue CJ, Measuring women’s cumulative neighborhood deprivation exposure using longitudinally linked vital records: a method for life course MCH research. Maternal and child health journal, 2014. 18(2): p. 478–487. [DOI] [PubMed] [Google Scholar]
- 27.Collins JW, et al. , Women’s lifelong exposure to neighborhood poverty and low birth weight: a population-based study. Maternal and child health journal, 2009. 13(3): p. 326. [DOI] [PubMed] [Google Scholar]
- 28.Swamy GK, et al. , Maternal age, birth order, and race: differential effects on birthweight. Journal of Epidemiology and Community Health, 2012. 66(2): p. 136–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rauh VA, Andrews HF, and Garfinkel RS, The contribution of maternal age to racial disparities in birthweight: a multilevel perspective. American journal of public health, 2001. 91(11): p. 1815–1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Collins JW, et al. , Advancing maternal age and infant birth weight among urban African Americans: The effect of neighborhood poverty. Ethnicity & Disease, 2006. 16(1): p. 180–186. [PubMed] [Google Scholar]
- 31.Powers DA, Paradox Revisited: A Further Investigation of Racial/Ethnic Differences in Infant Mortality by Maternal Age. Demography, 2013. 50(2): p. 495–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen PN, Maternal age and infant mortality for white, black, and Mexican mothers in the United States. Sociological Science, 2016. 3: p. 32–38. [Google Scholar]
- 33.Powers DA, Erosion of Advantage: Decomposing Differences in Infant Mortality Rates Among Older Non-Hispanic White and Mexican-Origin Mothers. Population Research and Policy Review, 2016. 35(1): p. 23–48. [Google Scholar]
- 34.Wildsmith EM, Testing the weathering hypothesis among Mexican-origin women. Ethn Dis, 2002. 12(4): p. 470–9. [PubMed] [Google Scholar]
- 35.Holzman C, et al. , Maternal weathering and risk of preterm delivery. American journal of public health, 2009. 99(10): p. 1864–1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Osypuk TL and Acevedo-Garcia D, Are racial disparities in preterm birth larger in hypersegregated areas? American journal of epidemiology, 2008. 167(11): p. 1295–1304. [DOI] [PubMed] [Google Scholar]
- 37.Hibbs S, et al. , The relation of neighborhood income to the age-related patterns of preterm birth among white and African-American Women: the effect of cigarette smoking. Maternal and child health journal, 2016. 20(7): p. 1432–1440. [DOI] [PubMed] [Google Scholar]
- 38.Sheeder J, Lezottte D, and Stevens-Simon C, Maternal age and the size of white, black, Hispanic, and mixed infants. Journal of pediatric and adolescent gynecology, 2006. 19(6): p. 385–389. [DOI] [PubMed] [Google Scholar]
- 39.Thorpe RJ, et al. , Accelerated Health Declines among African Americans in the USA. Journal of Urban Health, 2016. 93(5): p. 808–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Geronimus AT, et al. , Black-white differences in age trajectories of hypertension prevalence among adult women and men, 1999–2002. Ethn Dis, 2007. 17(1): p. 40–8. [PubMed] [Google Scholar]
- 41.Lin J and Kelley-Moore J, Intraindividual Variability in Late-Life Functional Limitations Among White, Black, and Hispanic Older Adults: Implications for the Weathering Hypothesis. Research on Aging, 2017. 39(4): p. 549–572. [DOI] [PubMed] [Google Scholar]
- 42.Chinn JJ and Hummer RA, Racial Disparities in Functional Limitations Among Hispanic Women in the United States. Research on Aging, 2016. 38(3): p. 399–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spence NJ and Eberstein IW, Age at first birth, parity, and post-reproductive mortality among white and black women in the US, 1982–2002. Social Science & Medicine, 2009. 68(9): p. 1625–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spence NJ, The Long-Term Consequences of Childbearing Physical and Psychological Well-Being of Mothers in Later Life. Research on Aging, 2008. 30(6): p. 722–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang S-C and Lee M-C, EFFECTS OF AGE, ETHNICITY AND HEALTH BEHAVIOURS ON THE PREVALENCE OF ADVERSE BIRTH OUTCOMES IN TAIWAN. Journal of Biosocial Science, 2012. 44(5): p. 513–524. [DOI] [PubMed] [Google Scholar]
- 46.Collins JW, Rankin KM, and Hedstrom AB, Exploring Weathering: the Relation of Age to Low Birth Weight Among First Generation and Established United States-Born Mexican-American Women. Maternal and Child Health Journal, 2012. 16(5): p. 967–972. [DOI] [PubMed] [Google Scholar]
- 47.Bird CE, et al. , Neighbourhood socioeconomic status and biological ‘wear and tear’in a nationally representative sample of US adults. Journal of epidemiology and community health, 2010. 64(10): p. 860–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chyu L and Upchurch DM, Racial and ethnic patterns of allostatic load among adult women in the United States: findings from the National Health and Nutrition Examination Survey 1999–2004. Journal of women’s health, 2011. 20(4): p. 575–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kaestner R, et al. , Stress, allostatic load, and health of Mexican immigrants. Social science quarterly, 2009. 90(5): p. 1089–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Peek MK, et al. , Allostatic load among non-Hispanic Whites, non-Hispanic Blacks, and people of Mexican origin: effects of ethnicity, nativity, and acculturation. American Journal of Public Health, 2010. 100(5): p. 940–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Geronimus AT, et al. , “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health, 2006. 96(5): p. 826–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Borrell LN, Dallo FJ, and Nguyen N, Racial/ethnic disparities in all-cause mortality in US adults: the effect of allostatic load. Public health reports, 2010. 125(6): p. 810–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Howard JT and Sparks PJ, The Effects of Allostatic Load on Racial/Ethnic Mortality Differences in the United States. Population Research and Policy Review, 2016. 35(4): p. 421–443. [Google Scholar]
- 54.Wallace ME and Harville EW, Allostatic load and birth outcomes among white and black women in New Orleans. Maternal and child health journal, 2013. 17(6): p. 1025–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Geronimus AT, et al. , Do US black women experience stress-related accelerated biological aging? Human Nature, 2010. 21(1): p. 19–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Geronimus AT, et al. , Race-ethnicity, poverty, urban stressors, and telomere length in a Detroit community-based sample. Journal of health and social behavior, 2015. 56(2): p. 199–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Strutz KL, et al. , Preconception stress, birth weight, and birth weight disparities among US women. American journal of public health, 2014. 104(8): p. e125–e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Das A, How does race get “under the skin”?: Inflammation, weathering, and metabolic problems in late life. Social Science & Medicine, 2013. 77: p. 75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Simons RL, et al. , Economic hardship and biological weathering: the epigenetics of aging in a US sample of black women. Social Science & Medicine, 2016. 150: p. 192–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


