Abstract
Background and objective
N-terminal pro-B-type natriuretic peptide (NT-proBNP) and soluble interleukin 1 receptor-like 1 ST2 (sST2) are biomarkers used to grade heart failure with reduced ejection fraction (HFrEF) severity. Both are potential targets of HFrEF treatment, but the first is associated with the patient’s hemodynamic status, while the second is more indicative of the inflammatory status and of myocardial fibrosis. The aim of this study was to assess the kinetics of these biomarkers after treatment with sacubitril/valsartan in HFrEF.
Methods
We analyzed blood samples of patients with HFrEF at baseline (before sacubitril/valsartan treatment), after 1, 2, and 3 months (respectively, after a month taking the 24/26 – 49/51 – 97/103 mg twice daily, or b.i.d., doses), and 6 months after the maximum-tolerated dose was reached (end study).
Results
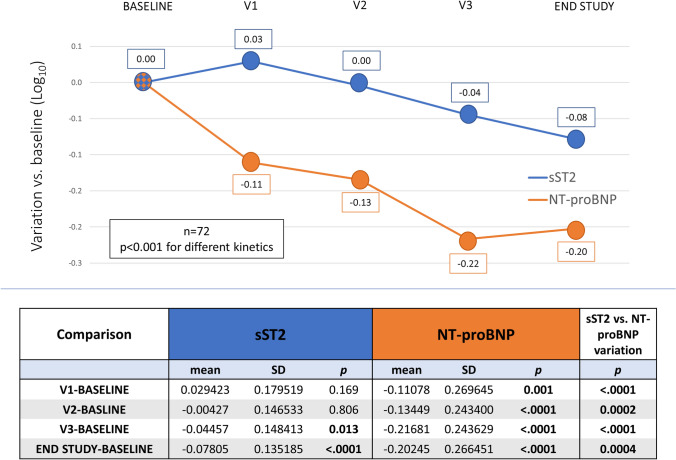
We obtained samples from 72 patients with HFrEF (age 64.0 ± 10.5 years, 83% males). NT-proBNP and sST2 values progressively and significantly reduced to 37% and 16%, respectively, with a greater reduction for NT-proBNP (p < 0.001). Specifically, NT-proBNP reduced from 1144 [593–2586] pg/mL to 743 [358–1524] pg/mL and sST2 from 27.3 [20.5–35.0] ng/mL to 23.1 [15.9–30.7] ng/mL, p for trend < 0.001 in both cases. The reduction of the two biomarkers over time occurred with statistically significant different kinetics: deferred for sST2 and faster for NT-proBNP. No significant changes in renal function and potassium levels were recorded.
Conclusion
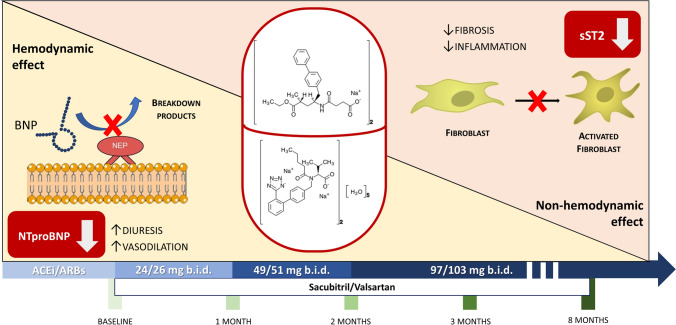
These findings suggest that, in patients with HF, sacubitril/valsartan effects on the cardiovascular system share a double pathway: a first, hemodynamic, faster pathway and a second, non-hemodynamic anti-fibrotic, delayed one. Both likely contribute to the sacubitril/valsartan benefits in HFrEF.
Key Points
| N-terminal pro-B-type natriuretic peptide (NT-proBNP) and soluble interleukin 1 receptor-like 1 ST2 (sST2) are biomarkers used to grade heart failure with reduced ejection fraction. |
| Our results show that the kinetics of these biomarkers after treatment with sacubitril/valsartan in HFrEF is different. |
| Sacubitril/valsartan effects on the cardiovascular system share a double pathway: a first, hemodynamic, faster pathway and a second, non-hemodynamic anti-fibrotic, delayed one. |
Introduction
N-terminal pro-B-type natriuretic peptide (NT-proBNP) and soluble interleukin 1 receptor-like 1 ST2 (sST2) are circulating biomarkers widely used in heart failure with reduced ejection fraction (HFrEF), providing complementary prognostic information [1, 2]. The first is strongly associated with the patient’s hemodynamic status being a marker of left ventricular (LV) diastolic wall stress and its decrease is considered a marker of reduced congestion. Instead, sST2 is a biomarker more related to immune modulation of cardiovascular disease than to the inflammatory component of HF and myocardial fibrosis [3, 4]. Sacubitril/valsartan, the first-in-class angiotensin receptor-neprilysin inhibitor (ARNI), has become a cornerstone in HFrEF therapy, and is demonstrated to reduce both NT-proBNP and sST2 values [3, 5]. However, little is known about the kinetics of changes in these molecules over time and at different drug doses.
The aim of this prospective, multicenter study is to analyze the kinetics of change of NT-proBNP and sST2 during a standardized protocol of up-titration of 8 months, in a cohort of patients with HFrEF who initiated treatment with sacubitril/valsartan, and escalated it to the maximum tolerated dose.
Materials and Methods
Between December 2018 and December 2019, we enrolled 113 consecutive outpatients with HFrEF referred to Centro Cardiologico Monzino (Milan) and Federico II University (Naples) HF units. Inclusion criteria were: suitability to start sacubitril/valsartan according to the 2016 ESC Guidelines [6], age 18–80 years, New York Heart Association Class (NYHA) II–III in stable clinical condition, and LV EF ≤ 35%. Patients affected by chronic obstructive pulmonary disease or needing oxygen supplement were excluded. Similarly, patients unable to tolerate 97/103 mg b.i.d. of sacubitril/valsartan were excluded from the analysis. A placebo arm was considered not conceivable by the Ethical Committees. At baseline, each patient underwent study procedures while taking background-guideline-directed HF therapy. After 36 hours of interruption of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, sacubitril/valsartan was introduced at a starting dose of 24/26 mg b.i.d. Thereafter, the dose was progressively uptitrated in a standard monthly fashion up to 97/103 mg b.i.d. or to the maximum-tolerated dose. Study procedures were performed at baseline, after 1, 2, and 3 months (respectively, after a month taking the 24/26 – 49/51 – 97/103 mg doses), and 6 months after the maximum-tolerated dose was reached (end study). Blood samples were drawn after assuring that any intense physical effort was avoided in the previous 3 h and after 5 min of rest in sitting position. Importantly, to avoid misinterpretation related to the function of the drug—sacubitril/valsartan exerts a direct action on BNP values per se [7]—we assayed the NT-proBNP values.
Statistical Analysis
Statistical analysis was performed using SAS software package (V. 9.4, SAS Institute Inc., Cary, NC). Continuous variables were expressed as mean ± standard deviation or median and [interquartile range] as appropriate, while categorical variables were expressed as absolute numbers and percentages. Comparisons between basal variables and end study variables were performed using paired t-tests for normally distributed variables, Wilcoxon signed rank test for non-normally distributed variables, and p for trend was calculated by Mann–Kendall test. The non-normally distributed variables were transformed into logarithms. Variations from baseline were calculated for each variable and differences tested using paired t-tests. The differences of delta between two biomarkers were tested by paired t-tests.
The imputation of the missing data was carried out via the PROC multiple imputation (MI) procedure with Markov Chain Monte Carlo (MCMC) method. From the 25 cases obtained, we randomly selected one for the main analysis of the work and assessed the consistency by calculating the % of times that the p-value was found to be significant (or non-significant). A sensitivity analysis was applied by repeating the analyses in patients who had data available for both variables of interest at all times. All tests were two-sided. A p-value ≤ 0.05 was considered as statistically significant.
Results
This study is a prespecified subanalysis of a prospective comprehensive trial dedicated to the evaluation of pathophysiological changes induced by sacubitril/valsartan in patients with HFrEF [8].
We evaluated a population of 113 enrolled patients with HFrEF from whom we collected NT-proBNP and sST2 five times, that is, at baseline and after 1, 2, and 3 months as well as at end study. A total of 72 patients (64%) were able to tolerate 97/103 mg b.i.d. of sacubitril/valsartan, and were therefore considered for the analysis. The main baseline characteristics of the analyzed population are reported in Table 1. NT-proBNP and sST2 values progressively reduced up to 37% and 16%, respectively, at the end of the study (p < 0.0001, values analyzed as logarithms). These significances are confirmed at 100% of the imputation scenarios (Table 2). Specifically, NT-proBNP reduced from 1144 [593–2586] pg/mL to 743 [358–1524] pg/mL and sST2 from 27.3 [20.5–35.0] ng/mL to 23.1 [15.9–30.7] ng/mL, p for trend < 0.001 in both cases. The kinetics of NT-proBNP compared with that of sST2 was significantly different, with a faster response for NT-proBNP (Fig. 1). Moreover, NT-proBNP reduced by 22.5% (p < 0.0001) from the first month of treatment, while sST2 was unchanged after both the first and second months of sacubitril/valsartan therapy (p = ns). These significances are confirmed at 100% and 80–88% of the imputation scenarios, respectively (Table 2). The kinetics remains statistically different throughout the study timeline, with a significant difference in the delta of change from baseline for the two biomarkers at each step. We did not observe significant changes in renal function and potassium levels across the entire study length, while systolic blood pressure significantly reduced from 118 ± 15 mmHg to 109 ± 14 mmHg (p < 0.001). During the study none of the patients changed their background HFrEF medical therapy.
Table 1.
General characteristics of the analyzed population (n = 72)
| n (%) | Mean ± SD | |
|---|---|---|
| Age (years) | 64.0 ± 10.5 | |
| Heart rate (bpm) | 67 ± 11 | |
| BMI (kg/m2) | 27.3 ± 4.3 | |
| LVVd (mL) | 198 ± 68 | |
| LVVs (mL) | 138 ± 55 | |
| LVEF (%) | 31.63 ± 4.59 | |
| Hemoglobin (g/dL) | 14.0 ± 1.6 | |
| eGFR (mL/min/1.73 m2) | 69.3 ± 19.5 | |
| K+(mmol/L) | 4.39 ± 0.40 | |
| Peak VO2 (mL/min/Kg) | 16.1 ± 4.5 | |
| Male | 60 (83%) | |
| NYHA II | 63 (88%) | |
| NYHA III | 9 (12%) | |
| Ischemic etiology | 37 (51%) | |
| CRT-D | 18 (25%) | |
| Hypertension | 45 (63%) | |
| Diabetes | 15 (21%) | |
| Moderate COPD | 8 (11%) | |
| Atrial fibrillation | 18 (25%) | |
| ACEI | 52 (72%) | |
| ARB | 18 (25%) | |
| BB | 71 (99%) | |
| MRA | 54 (75%) | |
| Loop diuretic | 58 (81%) | |
| Loop diuretic dose (mg) | 25 [25–50] |
BMI body mass index, LVVd left ventricle volume (diastole), LVVs left ventricle volume (systole), LVEF left ventricular ejection fraction, eGFR estimated glomerular filtration rate by Modification of Diet in Renal Disease formula, K+ potassium, Peak VO2 oxygen consumption at peak exercise, NYHA New York heart association class, CRT-D cardiac resynchronization therapy defibrillator, COPD chronic obstructive pulmonary disease, ACEI angiotensin-converting enzyme inhibitor, ARB angiotensin receptor blockers, BB beta blocker, MRA mineralocorticoid receptor antagonist
Table 2.
Confirmation of statistical significance of step-by-step biomarker changes in all imputation scenarios
| p-Value | % Confirmed | |
|---|---|---|
| ∆ ST2baseline – ST21moth | 0.1687 | 88% |
| ∆ ST2baseline – ST22moths | 0.8055 | 80% |
| ∆ ST2baseline – ST23moths | 0.013 | 96% |
| ∆ ST2baseline – ST2EndStudy | < 0.0001 | 100% |
| ∆ NT-proBNPbaseline – NT-proBNP1moth | 0.0008 | 100% |
| ∆ NT-proBNPbaseline – NT-proBNP2moths | < 0.0001 | 100% |
| ∆ NT-proBNPbaseline – NT-proBNP3moths | < 0.0001 | 100% |
| ∆ NT-proBNPbaseline – NT-proBNPEndStudy | < 0.0001 | 100% |
NT-proBNP N-terminal pro-B-type natriuretic peptide, ST2 soluble interleukin 1 receptor-like 1
Fig. 1.
NT-proBNP and sST2 variation versus baseline. The graph shows the percent variation of NT-proBNP and sST2 expressed as logarithms at each study step: baseline, after 1, 2, 3 months (respectively, after a month taking the 24/26 – 49/51 – 97/103 mg doses), and 6 months after the maximum-tolerated dose was reached (end study). NT-proBNP N-terminal pro-B-type natriuretic peptide, sST2 soluble interleukin 1 receptor-like 1
Discussion
Our results confirm the favorable effect of sacubitril/valsartan on circulating HFrEF biomarkers, a surrogate of clinical and prognostic benefits observed in multiple clinical trials conducted with ARNI during the last years [9–12]. Interestingly, while both NT-proBNP and sST2 progressively decreased as the drug dose increased, the overtime kinetics of these changes is significantly different. Indeed, NT-proBNP reduction is faster and can be observed since the first steps of treatment, a time interval in which sST2 is unchanged. On the other side, sST2 showed a more pronounced reduction at later steps. These data can be explained from a molecular point of view. Specifically, NT-proBNP changes suggest a rapid hemodynamic effect related to the vasodilation and diuretic properties of ARNI (Fig. 2, left side). Indeed, the drug is a combination of two different molecules. Sacubitril is a neprilysin inhibitor that can reduce the degradation of BNP, an endogenous diuretic produced by the body in response to HF and thus able to activate diuresis. The second component of the drug (i.e., valsartan), an angiotensin receptor blocker, carries well-known vasodilator properties [13]. In parallel, the combination of sacubitril and valsartan has already proven to be effective in the reduction of biomarkers involved in profibrotic signaling [5], which is altered in patients with HFrEF in response to increased metabolic load and shear stress. Our results on sST2 variations suggest that this mechanism follows a slower path, indicating that the anti-fibrotic—or better said “non-hemodynamic”— effect of sacubitril/valsartan treatment needs more time (or higher doses) to be elicited (Fig. 2, right). Finally, given the direct effect of sacubitril/valsartan on circulating BNP, in this trial we evaluated only NT-proBNP. However, considering the persistent BNP meaningful prognostic power also in patients taking the drug [7], further studies testing the parallel progressive changes in BNP would be interesting.
Fig. 2.
Hemodynamic and non-hemodynamic effects related to sacubitril/valsartan treatment depicted with their molecular mechanisms. BNP B-type natriuretic peptide, NEP neprilysin, NT-proBNP N-terminal pro-B-type natriuretic peptide, sST2 soluble interleukin 1 receptor-like 1
Conclusions
Taken together, these findings confirm the hypothesis that, in patients with HF, the effects of ARNIs on the cardiovascular system share a double pathway [14]: a first, hemodynamic, faster pathway and a second, non-hemodynamic, delayed pathway. Both likely contribute to the sacubitril/valsartan benefits in HFrEF.
Acknowledgments
After the acceptance of the article, an unrestricted support for open access publishing was provided by Novartis Farma S.p.A.
Declarations
Funding
The present study was supported by the Italian Ministry of Health (Ricerca Corrente).
Conflict of interest
None to declare.
Ethics approval
The protocol was approved by local ethic committee with number: CCM 898.
Institutional Review Board Statement
The present research protocol complies with World Medical Association Declaration of Helsinki and was approved by the Centro Cardiologico Monzino Ethical Committee (CCM 898). This observational cohort study was also registered to clinicaltrials.gov with ID: NCT04434170. Each subject provided written consent to the study.
Informed Consent Statement
Written informed consent for publication has been obtained from participating patients.
Consent to participate
Each participant signed a protoco-specific informed consent.
Consent for publication
N/A (no personal data or photographies included in the manuscript.
Data Availability Statement
Raw data will be available upon request on the website www.zenodo.org.
Code availability
Raw data and codes will be available upon request.
Author contributions
Conceptualization, P.A., M.M.; methodology, M.M., I.M., E.S.; formal analysis, A.B., N.C.; investigation, M.M., I.M., E.S., SP, CB. M.L.B.; data curation, I.M., E.S.; writing—original draft preparation, M.M., I.M., E.S. P.A.; writing—review and editing, SP, CB. M.L.B., P.A. P.P., A.B., N.C. All authors have read and agreed to the published version of the manuscript.
Footnotes
Massimo Mapelli and Irene Mattavelli shared first author privilege.
References
- 1.Shah RV, Januzzi JL., Jr ST2: a novel remodeling biomarker in acute and chronic heart failure. Curr Heart Fail Rep. 2010;7(1):9–14. doi: 10.1007/s11897-010-0005-9. [DOI] [PubMed] [Google Scholar]
- 2.McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–3726. doi: 10.1093/eurheartj/ehab368. [DOI] [PubMed] [Google Scholar]
- 3.McMurray JJ, Packer M, Desai AS, et al. Dual angiotensin receptor and neprilysin inhibition as an alternative to angiotensin-converting enzyme inhibition in patients with chronic systolic heart failure: rationale for and design of the Prospective comparison of ARNI with ACEI to Determine Impact on Global Mortality and morbidity in Heart Failure trial (PARADIGM-HF) Eur J Heart Fail. 2013;15(9):1062–1073. doi: 10.1093/eurjhf/hft052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weinberg EO, Shimpo M, De Keulenaer GW, et al. Expression and regulation of ST2, an interleukin-1 receptor family member, in cardiomyocytes and myocardial infarction. Circulation. 2002;106(23):2961–2966. doi: 10.1161/01.CIR.0000038705.69871.D9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zile MR, O'Meara E, Claggett B, et al. Effects of sacubitril/valsartan on biomarkers of extracellular matrix regulation in patients with HFrEF. J Am Coll Cardiol. 2019;73(7):795–806. doi: 10.1016/j.jacc.2018.11.042. [DOI] [PubMed] [Google Scholar]
- 6.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Rev Esp Cardiol (Engl Ed) 2016;69(12):1167. doi: 10.1016/j.rec.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 7.Myhre PL, Vaduganathan M, Claggett B, et al. B-type natriuretic peptide during treatment with sacubitril/valsartan: the PARADIGM-HF trial. J Am Coll Cardiol. 2019;73(11):1264–1272. doi: 10.1016/j.jacc.2019.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mapelli M, Mattavelli I, Paolillo S, et al. Effects of sacubitril/valsartan on exercise capacity: a prognostic improvement that starts during uptitration. Eur J Clin Pharmacol. 2023;79(9):1173–1184. doi: 10.1007/s00228-023-03527-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Velazquez EJ, Morrow DA, DeVore AD, et al. Angiotensin-neprilysin inhibition in acute decompensated heart failure. N Engl J Med. 2019;380(6):539–548. doi: 10.1056/NEJMoa1812851. [DOI] [PubMed] [Google Scholar]
- 10.Vardeny O, Claggett B, Kachadourian J, et al. Reduced loop diuretic use in patients taking sacubitril/valsartan compared with enalapril: the PARADIGM-HF trial. Eur J Heart Fail. 2019;21(3):337–341. doi: 10.1002/ejhf.1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mantegazza V, Volpato V, Mapelli M, et al. Cardiac reverse remodelling by 2D and 3D echocardiography in heart failure patients treated with sacubitril/valsartan. Diagnostics (Basel) 2021;11(10):1845. doi: 10.3390/diagnostics11101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371(11):993–1004. doi: 10.1056/NEJMoa1409077. [DOI] [PubMed] [Google Scholar]
- 13.Solomon SD, Zile M, Pieske B, et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet. 2012;380(9851):1387–1395. doi: 10.1016/S0140-6736(12)61227-6. [DOI] [PubMed] [Google Scholar]
- 14.Mapelli M, Mattavelli I, Salvioni E, et al. Impact of sacubitril/valsartan on surfactant binding proteins, central sleep apneas, lung function tests and heart failure biomarkers: hemodynamic or pleiotropism? Front Cardiovasc Med. 2022;9:971108. doi: 10.3389/fcvm.2022.971108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Raw data will be available upon request on the website www.zenodo.org.