Abstract
Background
The successful implementation of the Enhanced recovery after surgery (ERAS) concept in thoracic surgery has made it possible to complete the surgery in the day surgery unit. However, it is still unclear whether day surgery for lung cancer patients can achieve the same or even better results.
Methods
A systematic literature search was completed in common databases for studies published before May 2022 and the data analyzed using the Review Manager 5.3 software.
Results
We ultimately included 7 retrospective articles that met our criteria for the study. The results of age, smoking status, comorbidity and pulmonary function tests in day surgery group were better than in inpatient surgery group. Minimally invasive surgical method with segmentectomy was more used in day surgery group than in normal surgery group. The 30-day mortality was also lower in Day surgery group and it displayed that early discharged patients had fewer overall complications than the inpatient surgery group.
Conclusions
We demonstrate that younger patients, patients receiving segmental resections by VATS, and those with better pulmonary function tests or without comorbidity can be discharged early with low rates of complications and 30-day mortality, especial with ERAS program.
Keywords: Day surgery, Enhanced recovery after surgery, Lung cancer, Video assisted thoracic surgery, Complication
Introduction
Lung cancer is currently the most common disease and one of the leading causes of death in worldwide. In addition, with the popularization and application of low-dose CT (LDCT), more and more young patients are found with small pulmonary nodules in CT [1]. In today’s cost-conscious healthcare environment, it is critical to strike a balance between delivering high-quality healthcare How to provide high-quality medical protection, while also allowing patients to be discharged safely and shortening the length of stay (LOS), is a problem we have been exploring [2]. Enhanced recovery after surgery (ERAS) has been developed furtherly in thoracic surgery [3]. The incidence of perioperative complications and LOS of patients with lung cancer have been reduced obviously by ERAS program.
Day surgery refers to the discharge of a patient undergoing surgical treatment and discharged from the hospital on the first day after surgery through a preoperatively planned and accurately assessed surgical procedure [4, 5]. Although there are several reports on day surgery in patients with lung cancer, they are all retrospective single-center clinical studies [6–8]. Consequently, it is still unclear whether day surgery for lung cancer patients can achieve the same or even better results. We firstly performed this meta-analysis to explore and compare the outcomes of thoracic day surgery versus inpatient surgery.
Methods
Search strategy
A systematic literature search was completed in PubMed, Cochrane Library, EMBASE, CNKI, Medline, and Web of Science for studies published before May 2022. The key words used are as follows: (Enhanced recovery after surgery OR ERAS OR Fast track) AND (lung cancer OR lung carcinoma OR lung neoplasm OR lung malignancy) AND (day case OR day-case OR day surgery or day-surgery OR day-stay OR outpatient OR out-patient).
The inclusion criteria: (1) Studies comparing thoracic day surgery with inpatient surgery in patients with lung cancer; (2) Full-text articles including at least one of the following outcomes: operation time, average hospital cost, 30-day readmission, 30-day mortality, postoperative complications.
The exclusion criteria: (1) Review articles, case reports, letters to the editor, comments and meeting reports. (2) Non-human subject studies. (3) Studies without necessary data for statistical analysis. (4) The patients did not undergo day surgery. (5) Non-English Article.
Quality assessment
The guideline of Newcastle–Ottawa Scale (NOS) was used for evaluating this research. The assessment tool including the star system was used in this research. Specific evaluation system is that 8–9 stars are high quality; 6–7 stars are reasonable quality, and 6 stars less are bad.
Data collection
Two investigators separately collected relevant data from each included study. Any ambiguities or inconsistencies that arise during the data collection process are addressed through brainstorming. Excel in Tables 1, 2, 3, 4 and 5 is used to collect the basic information.
Table 1.
Characteristics of the included studies
| References | Country | Design | Study period | Group | Cases | Sex (M/F) | Age | Smoking | Comorbidity | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hypertension | Diabetes | Coronary heart disease | COPD | |||||||||
| Dong et al. [9] | China | R | 2019 | DG | 20 | 4/16 | 36.3 ± 11.7 | 2 | 1 | 0 | 0 | 1 |
| NG | 28 | 7/21 | 43.8 ± 13.2 | 2 | 2 | 1 | 0 | 0 | ||||
| Patel et al. [4] | USA | R | 2011–2019 | DG | 854 | 348/506 | 66.9 ± 2.5 | 223 | 484 | 147 | 0 | 129 |
| NG | 16,064 | 6668/9394 | 67.9 ± 3.5 | 5396 | 9521 | 2610 | 75 | 3364 | ||||
| Drawbert et al. [2] | USA | R | 2010–2015 | DG | 3819 | 1626/2193 | 68.5 ± 6.7 | – | – | – | – | – |
| NG | 3819 | 1613/2206 | 68.7 ± 4.8 | – | – | – | – | – | ||||
| Linden et al. [7] | USA | R | 2012–2017 | DG | 1821 | 773/1048 | 66 ± 3.5 | – | 1047 | 323 | 290 | 544 |
| NG | 44,504 | 19,180/25323 | 68 ± 5.9 | – | 27,226 | 8318 | 9034 | 15,816 | ||||
| Dong et al. [6] | China | R | 2020–2021 | DG | 136 | 25/111 | 43.30 ± 9.26 | 10 | 2 | 2 | – | 0 |
| NG | 217 | 40/177 | 42.76 ± 10.66 | 18 | 5 | 3 | – | 0 | ||||
| Towe et al. [8] | USA | R | 2007–2017 | DG | 448 | 204/244 | 62.3 ± 7.65 | – | 206 | 56 | 57 | – |
| NG | 613 | 273/340 | 64.87 ± 8.15 | – | 326 | 109 | 110 | – | ||||
| Geraci et al. [10] | USA | R | 2018–2020 | DG | 134 | 48/86 | 68.5 ± 6.7 | 72 | 60 | 18 | 14 | 7 |
| NG | 119 | 50/69 | 70.2 ± 7.8 | 50 | 75 | 33 | 18 | 9 | ||||
R retrospective study; DG day surgery group; NG normal surgery group; COPD chronic obstructive pulmonary disease; M male; F female; –, not available
Table 2.
Characteristics of the included studies
| References | Pulmonary function tests | Surgical methods | Operation approach | Tumor location | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FEV1% predicted | DLCO % predicted | Open | Minimally invasive | Lobectomy | Segmentectomy | RUL | RML | RLL | LUL | LLL | Other | |
| Dong et al. [9] | – | – | 0 | 20 | 10 | 10 | – | – | – | – | – | – |
| – | – | 0 | 28 | 17 | 11 | – | – | – | – | – | – | |
| Patel et al. [4] | – | – | 84 | 770 | – | – | – | – | – | – | – | – |
| – | – | 72 | 10,617 | – | – | – | – | – | – | – | – | |
| Drawbert et al. [2] | – | – | 1811 | 1400 | – | – | 1211 | 348 | 666 | 925 | 583 | 86 |
| – | – | 2068 | 1646 | – | – | 1206 | 315 | 677 | 906 | 617 | 98 | |
| Linden et al. [7] | 88.36 ± 10.45 | 78.65 ± 20.16 | 152 | 1669 | 1494 | 327 | – | – | – | – | – | – |
| 84.25 ± 12.17 | 74.14 ± 18.35 | 14,275 | 30,229 | 39,943 | 4561 | – | – | – | – | – | – | |
| Dong et al. [6] | – | – | – | – | 51 | 84 | 43 | 14 | 15 | 48 | 16 | |
| – | – | – | – | 92 | 124 | 75 | 20 | 31 | 63 | 28 | ||
| Towe et al. [8] | 85.31 ± 8.98 | 83.90 ± 15.21 | 2 | 446 | – | – | – | – | – | – | – | – |
| 75.62 ± 7.42 | 73.21 ± 13.96 | 33 | 580 | – | – | – | – | – | – | – | – | |
| Geraci et al. [10] | 89.12 ± 20.66 | 82.45 ± 13.12 | – | – | 53 | 79 | 36 | 12 | 23 | 46 | 15 | – |
| 85.43 ± 16.35 | 79.89 ± 11.28 | – | – | 71 | 37 | 43 | 8 | 25 | 23 | 16 | – | |
FEV1% predicted, percent of forced expiratory volume in 1 s predicted; DLCO% predicted, percent of diffusing capacity of the lung for carbon monoxide predicted
RUL right upper lobe; RML right middle lobe; RLL right lower lobe; LUL left upper lobe; LLL left lower lobe
Table 3.
Characteristics of the included studies
| References | Histology | TNM stage | NOS | |||||
|---|---|---|---|---|---|---|---|---|
| Adenocarcinoma | Squamous carinoma | Other | I | II | III | IV | ||
| Dong et al. [9] | 20 | 0 | 0 | 20 | 0 | 0 | 0 | 8 |
| 27 | 1 | 0 | 27 | 1 | 0 | 0 | ||
| Patel et al. [4] | – | – | – | – | – | – | – | 7 |
| – | – | – | – | – | – | – | ||
| Drawbert et al. [2] | 2489 | 764 | 566 | – | – | – | – | 8 |
| 2476 | 760 | 583 | – | – | – | – | ||
| Linden et al. [7] | – | – | – | – | – | – | – | 7 |
| – | – | – | – | – | – | – | ||
| Dong et al. [6] | 135 | 1 | – | 134 | 2 | – | – | 8 |
| 215 | 2 | – | 211 | 6 | – | – | ||
| Towe et al. [8] | – | – | – | – | – | – | – | 7 |
| – | – | – | – | – | – | – | ||
| Geraci et al. [10] | 85 | 9 | 29 | 76 | 7 | 6 | – | 8 |
| 70 | 12 | 20 | 69 | 8 | 11 | – | ||
NOS Newcastle–Ottawa scale
Table 4.
Results of the analysis of two groups
| References | Operation time (min) | Average hospital cost ($) | 30d Readmission | 30d Mortality | Postoperative compliactions | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Pneumothorax | Hydrothorax | Homorrhage | Arrhythmia | Lung infection | Chylothorax | Persist air leak | Hoarseness | |||||
| Dong et al. [9] | – | 6005.43 ± 534.25 | 0 | 0 | 1 | – | – | – | 0 | – | – | – | 1 |
| – | 7500.55 ± 1156.69 | 0 | 0 | 1 | – | – | – | 1 | – | – | – | 0 | |
| Patel et al. [4] | 142.5 ± 10.4 | – | 51 | 5 | 2 | 2 | – | – | – | – | – | – | – |
| 168.7 ± 17.7 | – | 1128 | 47 | 1 | 1 | – | – | – | – | – | – | – | |
| Drawbert et al. [2] | – | 197 | 90 | – | – | – | – | – | – | – | – | – | |
| – | 137 | 40 | – | – | – | – | – | – | – | – | – | ||
| Linden et al. [7] | 193.0 ± 40.7 | – | 114 | 5 | 92 | – | 5 | 5 | 32 | 11 | 1 | 36 | 2 |
| 240.0 ± 55.8 | – | 3485 | 169 | 10,537 | – | 490 | 1105 | 4292 | 805 | 124 | 3592 | 129 | |
| Dong et al. [6] | 68.81 ± 21.33 | 6,411.47 ± 657.76 | 1 | 0 | 16 | 2 | 1 | 3 | 0 | 1 | 1 | 6 | 2 |
| 98.15 ± 11.34 | 7,522.41 ± 1,471.84 | 3 | 0 | 25 | 4 | 2 | 4 | 0 | 0 | 2 | 10 | 3 | |
| Towe et al. [8] | 64.80 ± 41.22 | – | 0 | 0 | – | – | – | – | – | – | – | – | – |
| 87.25 ± 35.67 | – | 0 | 0 | – | – | – | – | – | – | – | – | – | |
| Geraci et al. [10] | 84.15 ± 15.35 | – | 1 | 0 | 13 | – | 3 | – | 3 | – | – | 7 | – |
| 101.34 ± 21.56 | – | 4 | 0 | 40 | – | 6 | – | 10 | – | – | 24 | – | |
Table 5.
Summary of all the researches
| References | Summary content |
|---|---|
| Dong et al. [9] | 20 patients were included in day surgery (DS) and 28 patients were applied inpatient surgery (IS). The average hospital day in DSgroup was significantly shorter than in IS group. The average hospital cost in DS group was significantly lower than in IS group.There was no significant difference in the incidence of postoperative complications between two groups |
| Patel et al. [4] | Only 854 (3.8%) of 22,585 patients that met inclusion criteria were discharged with day surgery. A minimally invasive approach wasthe strongest predictor of early discharge. Readmission rates were not significantly different for two groups. |
| Drawbert et al. [2] | 3879 (7.3%) patients were discharged on day 1, whereas 48951 (92.7%) were discharged after day 1. Factors associated with daysurgery included male sex, higher socioeconomic status, right middle lobectomy, minimally invasive surgery and high-volumecentres. |
| Linden et al. [7] | 1821 patients (3.9%) were discharged on day 1. In multivariable analysis, factors associated with day 1 discharge included age, bodymass index greater than 25, forced expiration value at 1 second, middle or upper lobectomy, minimally invasive technique, andprocedure time. Outpatient 30-day mortality was similar in two groups. Patients discharged on day 1 were not at increased risk ofreadmission. |
| Dong et al. [6] | 136 individuals in DS and 217 individuals in IS. With respect to the postoperative complications (PPCs), no difference between thetwo groups was found. In the DS, a shorter length of stay after surgery and reduced drainage time were found, while the drainagevolume per hour (mL/h) was not notably divergent between the relevant groups. No difference was observed in the cost ofequipment and materials between the two groups. However, the average hospital cost and drug cost of the DS were significantlylower than those of the IS. |
| Towe et al. [8] | DS after lung resection is multifactorial but is safe among selected patients. Age, lung function, procedure duration, and surgeon allinfluence DS. Complications after DS were rare. Education or enhanced recovery protocols may help overcome this barrier.Standardized pathways would likely help identify low-risk patients for expeditious discharge. |
| Geraci et al. [10] | 134 patients (53%) discharged by day 1. On multivariate analysis, never smokers and segmentectomy were associated with DS.Conversely, decreased baseline performance status and perioperative complications were associated with DS. There were 4readmissions (1.6%), of which one (0.4%) was after day 1 discharge. Patient satisfaction remained high throughout the study period. |
Statistical analysis
Review Manager 5.3 software were used for statistical analyses. The dichotomous variables were assessed by using odds ratios (OR) with a 95% confidence interval (CI) and the continuous variables using weighted mean difference (WMD) with a 95% CI. The I2 statistics were used to evaluate the heterogeneity. The potential publication bias was evaluated by visually inspecting the funnel plots. P < 0.05 was regarded as statistically significant.
Results
The selection of included studies
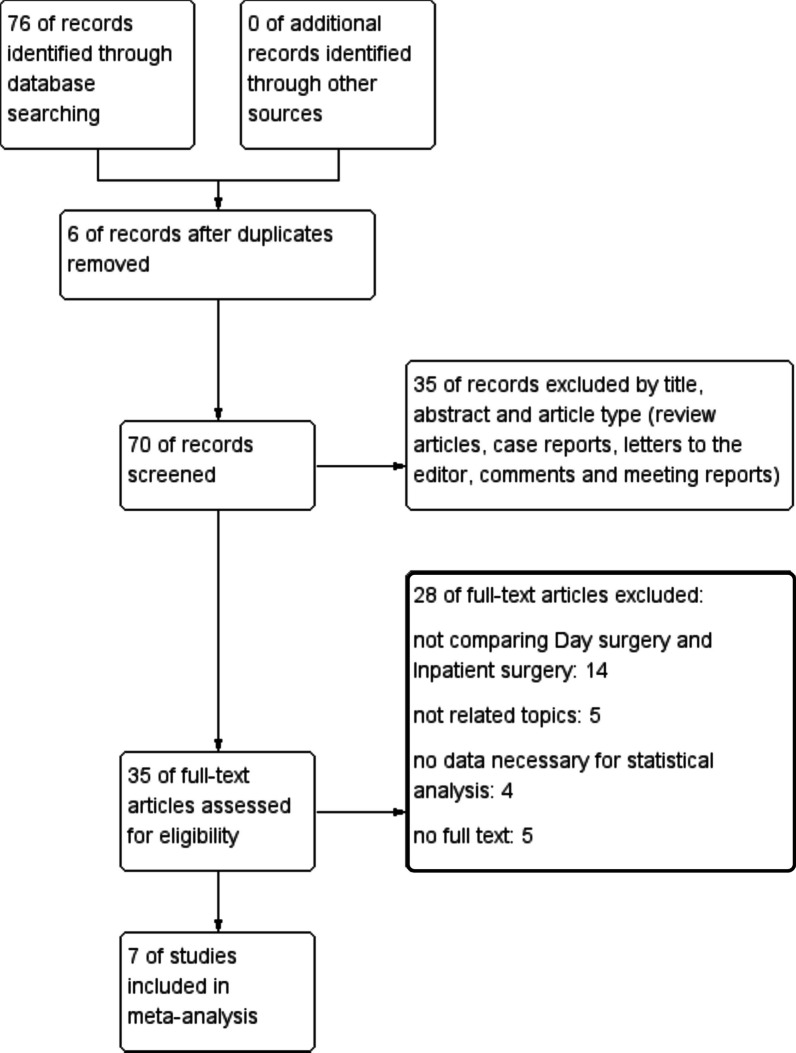
Databases were searched and total number of studies is 76 before May 2022. After removing 6 duplicate articles, we carefully read the remaining 70 articles. Then, 35 articles were excluded due to article type that did not meet our inclusion criteria. Subsequently, after a detailed reading of the remaining 35 papers, combined with our inclusion and exclusion criteria, 20 papers were finally excluded. In our meta-analysis, we finally included 7 retrospective articles that met our criteria for the study rigorously (Fig. 1).
Fig. 1.
Flow chart of literature search strategies
The characteristics of included studies
A prospective study was completed by Dong et al. [9]. The results were primarily analyzed for length of hospital stay, hospitalization costs and complications. Patel et al. [4] analyzed the outcomes of patients who were discharged on postoperative day 1 (POD1) with normal approach group. Drawbert et al. [2] summarized patients with stage I non-small cell lung cancer (NSCLC) from 2010 to 2015 and research objects including two groups. In Linden et al. [7] study, they found that carefully selected patients before the surgery may not increase risk of readmission or death. In Dong et al. [6] research, 353 patients were included with 136 persons in the day surgery group and 217 people in the inpatient surgery group. Towe et al. [8] reported that POD 1 discharge patients after lung resection is safe. Geraci et al. [10] evaluated safety for patients discharged by POD1 after different range resection of lobe.
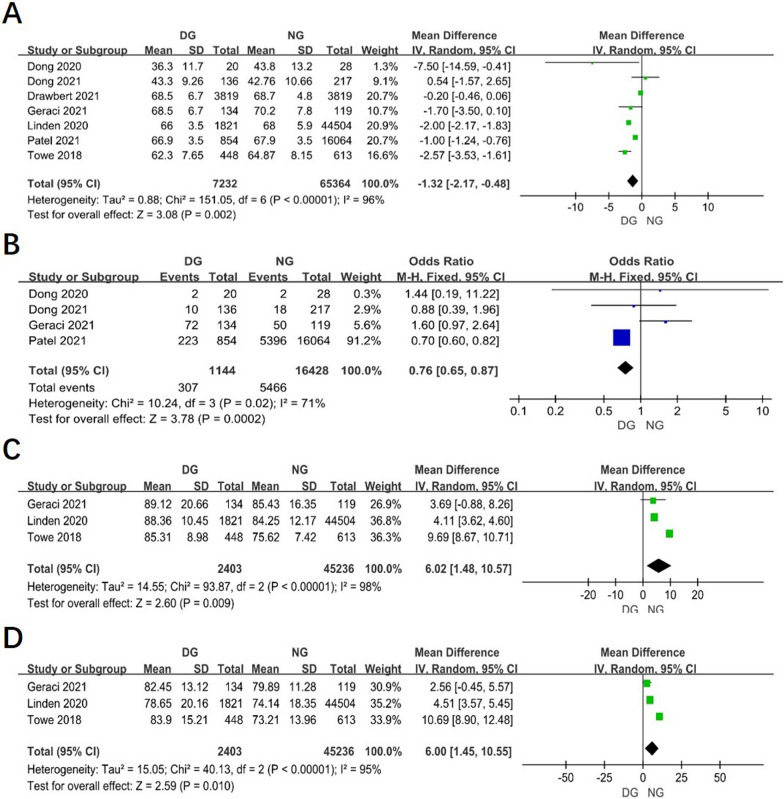
The age between two groups
Age of patients was reported in all studies. The combined data revealed that the age in Day surgery group (DG) was younger than in inpatient surgery group, or named Normal surgery group (NG) (WMD = − 1.32, 95% CI − 2.17 to − 0.48, P = 0.002, I2 = 96%). (Fig. 2A).
Fig. 2.
Forest plot of the meta-analysis. A Age. B smoking status of patient. C FEV1% predicted. D DLCO% predicted
The smoking status of patient between two groups
Briefly, four studies reported smoking status of patients between two groups. It revealed that the patients with smoking status in day surgery group were less than in normal group (OR 0.76, 95% CI 0.65–0.87, P = 0.0002, I2 = 71%). (Fig. 2B).
The pulmonary function tests between two groups
The results of 3 studies revealed that the pulmonary function tests in DG were better than in NG, especially in percent of forced expiratory volume in 1 s predicted (FEV1% predicted) (WMD = 6.02, 95% CI 1.48–10.57, P = 0.009, I2 = 98%) and percent of diffusing capacity of the lung for carbon monoxide predicted (DLCO% predicted) (WMD = 6.00, 95% CI 1.45–10.55, P = 0.009, I2 = 95%). (Fig. 2C, D).
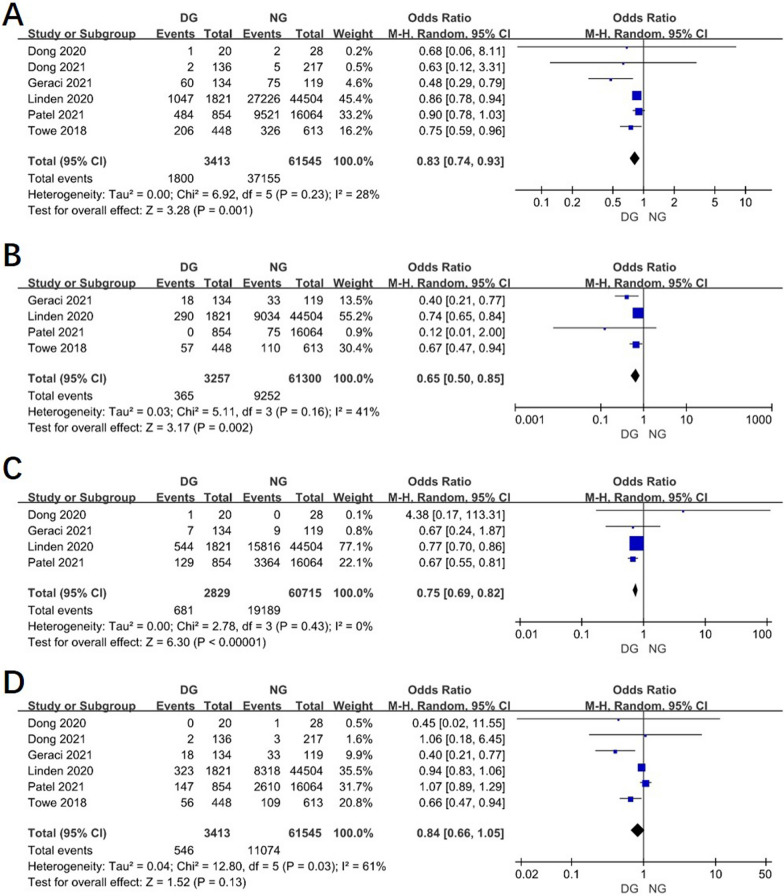
The comorbidity before the surgery between two groups
The data regarding the preoperative comorbidity were reported in most of studies. The result showed that patients in day surgery were less likely to have hypertension, coronary heart disease, and chronic obstructive pulmonary disease (COPD) than in normal group. (Fig. 3A, B, C) But there is no difference in patients with diabetes before the surgery in two groups (OR 0.84, 95% CI 0.66–1.05, P = 0.13, I2 = 61%). (Fig. 3D).
Fig. 3.
Forest plot of the meta-analysis. A Hypertension. B Coronary heart disease. C COPD. D Diabetes
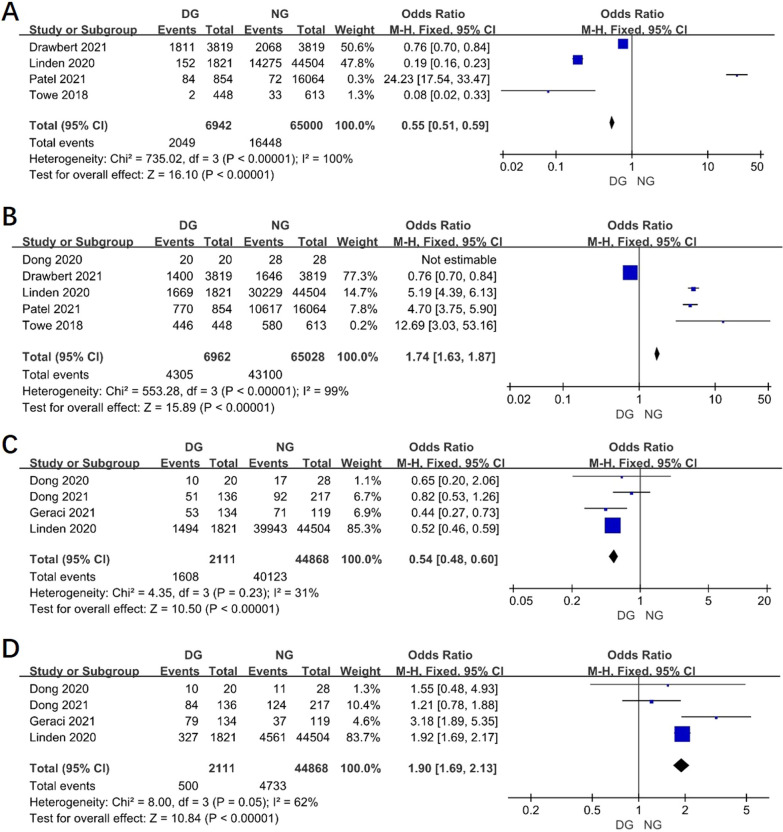
The surgical methods between two groups
4 researches reported the surgical method by open access in two groups and the result revealed that open access in DG was less than in NG (OR 0.55, 95% CI 0.51–0.59, P < 0.00001, I2 = 100%) (Fig. 4A). However, it showed minimally invasive surgical method was more popular in DG than in NG (OR 1.74, 95% CI 1.63–1.87, P < 0.00001, I2 = 99%) (Fig. 4B).
Fig. 4.
Funnel plot of the meta-analysis. A Surgical method by open access. B Surgical method by VATS. C Lobectomy. D Segmentectomy
The resection range of lobe between two groups
Lobectomy or segmentectomy was informed in 4 studies. The pooled data revealed that the lobectomy in DG was less than in NG (Fig. 4C), but segmentectomy in DG was more than in NG (OR 1.90, 95% CI 1.69–2.13, P < 0.00001, I2 = 62%) (Fig. 4D).
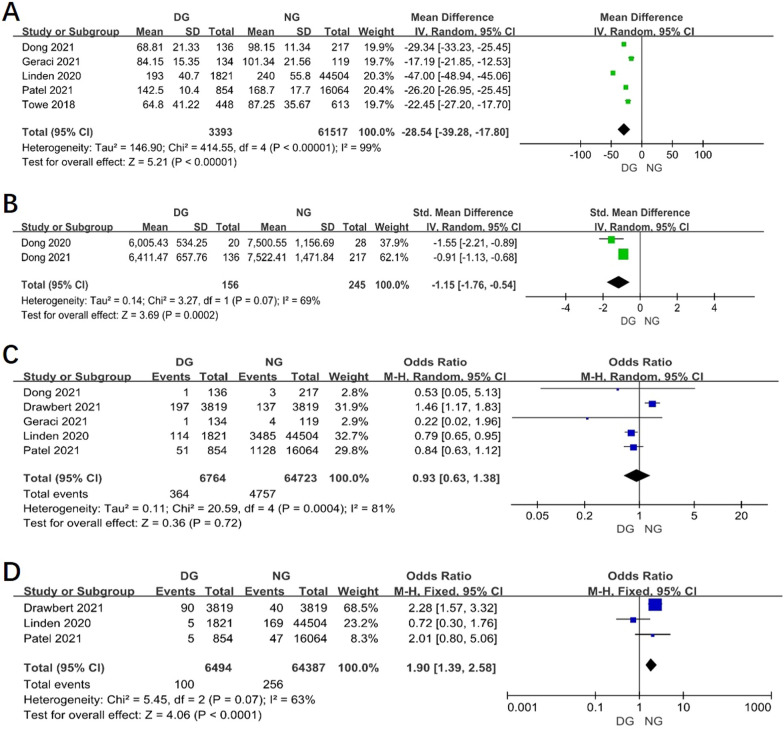
The operation time between two groups
Results of 5 studies showed that the operative time was shorter in day surgery group than in normal group (WMD = − 28.54, 95% CI − 39.28 to − 17.80, P < 0.00001, I2 = 99%). (Fig. 5A).
Fig. 5.
Funnel plot of the meta-analysis. A Operative time. B Average hospital cost. C 30-day readmission. D 30-day mortality
The average hospital cost between two groups
According the result of 2 studies, the average hospital cost in DG was lower than in normal group (WMD = − 1.15, 95% CI − 1.76 to − 0.54, P = 0.0002, I2 = 69%). (Fig. 5B).
The 30-day readmission between two groups
Results of 5 studies showed that there was no difference between two groups in 30-day readmission (OR 0.93, 95% CI 0.63–1.38, P = 0.72, I2 = 81%). (Fig. 5C).
The 30-day mortality between two groups
The 30-day mortality was lower in DG than in NG according to the result of 3 studies (OR 1.90, 95% CI 1.39–2.58, P < 0.0001, I2 = 63%). (Fig. 5D).
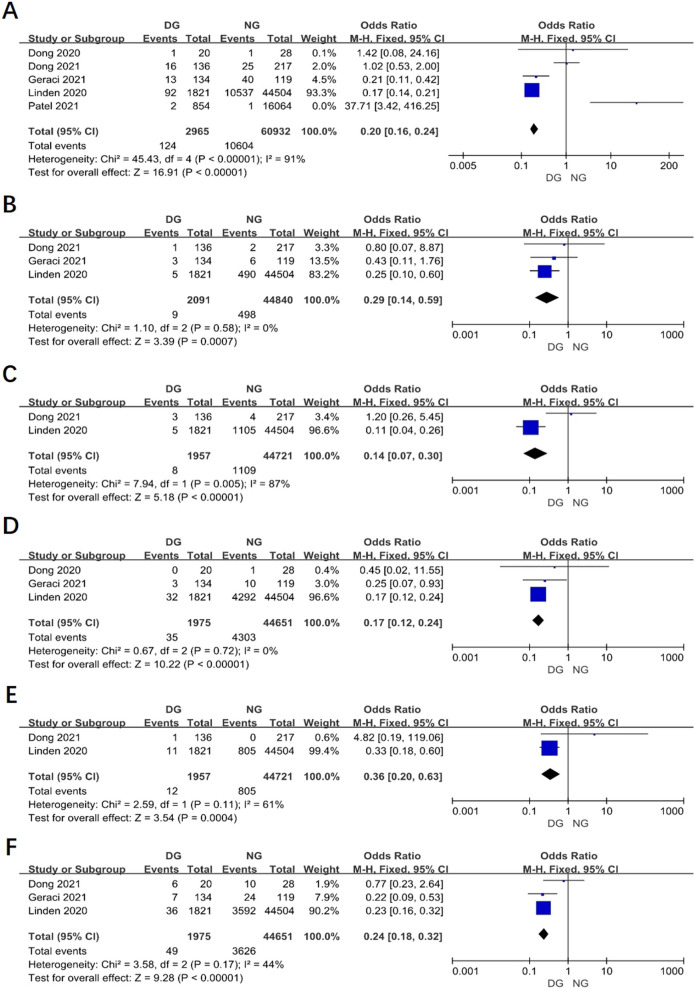
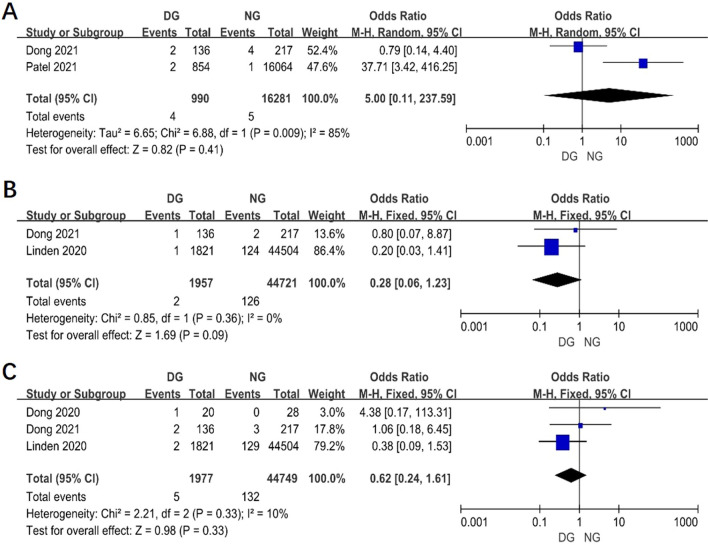
The postoperative complications between two groups
Postoperative complications of surgery patients was reported in 5 studies. The results showed that the postoperative complications in day surgery group was lower than in inpatient surgery group (OR 0.20, 95% CI 0.16–0.24, P < 0.00001, I2 = 91%) (Fig. 6A). From the Fig. 6B–F, in DG, it showed that postoperative complications including hydrothorax, hemorrhage, arrhythmia, lung infection and persist air leak were less than in NG. However, there is no statistical difference between two groups in pneumothorax, chylothorax and hoarseness (Fig. 7A, C).
Fig. 6.
Funnel plot of the meta-analysis. A Postoperative complications. B Hydrothorax. C Hemorrhage. D Arrhythmia. E Lung infection. F Persist air leak
Fig. 7.
Funnel plot of the meta-analysis. A Pneumothorax. B Chylothorax. C Hoarseness
Comment
Day surgery was first introduced by James Nicoll in 1909 [6]. The amount of day surgery in Europe and the United States has reached more than 80% of the total number of operations in their hospitals [11–13]. In the early days, the ERAS concept was more reflected in the optimization of the perioperative diagnosis and treatment process for patients undergoing general surgery [14]. Then, based on the application of laparoscopic minimally invasive technology, the positive role in the ERAS process is highlighted during the surgery [15]. Compared with traditional surgical methods, minimally invasive surgery itself has the advantages of less trauma, less pain, faster postoperative recovery and shorter hospital stay. It not only reduces the stress response and complications in patients after the surgery, but also significantly improves the satisfaction of patients [3]. Since 2006, the clinical application of the ERAS concept with minimally invasive methods in thoracic surgery has been gradually carried out, especially in the optimization of perioperative management paths for patients with diseases in thorax [15].
The successful implementation of the ERAS concept in thoracic surgery has made it possible to complete the surgery in the day surgery unit. At the same time, the thoracic day surgery is also a further concentrated embodiment of the implementation of the ERAS concept. 7 studies were included in our research and we conducted the first meta-analysis to explore and compare the clinical efficacy of thoracic day surgery and inpatient surgery in patient with lung cancer.
Firstly, the result of meta-analysis found that the age, smoking status of patient, pulmonary function tests and comorbidity before the day surgery were better than in inpatient surgery group. The main reason might be that patients in day surgery were younger and fewer smoking histories than the normal, further reflecting the objective fact that fewer patients had preoperative comorbidities with better lung function. Surgeons can use these findings to develop patient-specific treatment plans and select patients that are most likely to succeed with an accelerated discharge [4]. But when we reviewed the included references again, which specifically mentioned studies on these relative contents in Dong’s two articles, there is no statistical difference between day surgery group and inpatient group. This means that the basic conditions of patients in day surgery and inpatient group are basically the same, and it also shows that the patients of day surgery is comparable to inpatient group. Further analysis of the remaining references, due to the late implementation of day surgery in thoracic surgery for lung cancer, it can be found from their data (Patel et al. and Linden et al.) that the number of day lung cancer surgery patients accounted for a relatively small part of total patients, which may cause the imbalance of baseline data when comparing the two groups in their researches. As the understanding of day surgery for patients with lung cancer increases, we believe that more and more patients will be included in the day surgery process, rather than those who are simply highly selected.
Regarding the surgical methods and resection range of lobe in operation, our meta-analysis data showed minimally invasive surgical method was more popular in DG than in NG and segmentectomy in day surgery group was more than in normal surgery group. In recent years, minimally invasive thoracoscopic surgery (video-assisted thoracoscopic surgery, VATS) for the treatment of ground glass nodule has basically reached a consensus, which is also a foundation for the development of thoracic day surgery [5]. Traditional lobectomy has a greater loss of pulmonary function, while segmentectomy can better preserve more pulmonary function, which is more conducive to the recovery of postoperative pulmonary function and the improvement of patients' quality of life [12]. Especially, the segmentectomy mentioned in our data does not include the wedge resection. In addition, results showed that the operative time was shorter in day surgery group than in normal group. With the popularization of VATS, the proficiency of surgical operations has been continuously improved, which has significantly shortened the operation time.
It is important to achieve the most effective patient care and optimal patient outcomes by reducing the LOS and postoperative readmission rates for patients [11]. 30-day readmission after lung cancer surgery can place additional financial burdens on patients. Therefore, it is critical to assess patient discharge from a financial and clinical perspective and to reduce the risk of readmission and early death after lung cancer surgery. Shorter LOS is also associated with lower hospital costs [13]. In our study, there is no difference between two groups in 30-day readmission. However, the 30-day mortality was lower in DG than in NG according to the result of 3 studies. According the result of Dong’ studies in 2020 and 2021, the average hospital cost in DG was lower than in normal group. By optimizing the perioperative management process of patients with lung cancer surgery, the main purpose is to minimize medical intervention, increase medical services, and ensure patient safety. On the premise of integrating more humanistic factors into treatment, it is possible to accelerate patient recovery and improve patient satisfaction with medical care. In addition, postoperative pain control is also a factor affecting the length of hospital stay, and difficulty in perioperative pain control may also be a barrier to discharge on the first postoperative day. Methods to reduce pain during surgery, such as minimally invasive techniques and changes in intraoperative analgesia, such as thoracoscopic intercostal nerve blocks (TINBs) together with a postoperative combination of acetaminophen and NSAIDs, may facilitate early discharge [6].
The occurrence of postoperative complications is also an important indicator for evaluating short-term results after surgery. The complications after lung cancer resection are hydrothorax, hemorrhage, arrhythmia, lung infection, persist air leak, pneumothorax, chylothorax and hoarseness [1]. The results of our meta-analysis displayed that POD1 patients had fewer overall complications than the inpatient surgery group. In DG, it showed that postoperative complications including hydrothorax, hemorrhage, arrhythmia, lung infection and persist air leak were less than in NG. However, there is no statistical difference between two groups in pneumothorax, chylothorax and hoarseness. We analyzed the included references, which specifically mentioned studies on complications, including Dong’s two articles, Patel’s article, Linden’s article, and Geraci’s article. The percentage of day surgeries planned in these papers that were completed were 95%, 88.2%, 99.8%, 94.9% and 90.3% respectively. There were several reasons for this situation. Firstly, minimally invasive surgery for the lung cancer has obvious significance in reducing postoperative complications than open thoracic surgery. Secondly, these factors have driven the adoption of ERAS after thoracic surgery. The focus of the ERAS program is reducing the incidence of complications in patients and the postoperative hospital stay can be safely shortened.
There are several limitations in this meta-analysis. Firstly, the number of studies included and the simple scale were relatively small. All studies included for meta-analysis were retrospective observational studies and lacked high-quality randomized controlled trials. Secondly, the age, comorbidity before the operation, pulmonary function tests and 30-day mortality had significant heterogeneity. Potential factors that could explain that compared with inpatient patients, day surgery patients are selectively younger, and have better physical fitness, better preoperative indicators, with fewer postoperative complications.
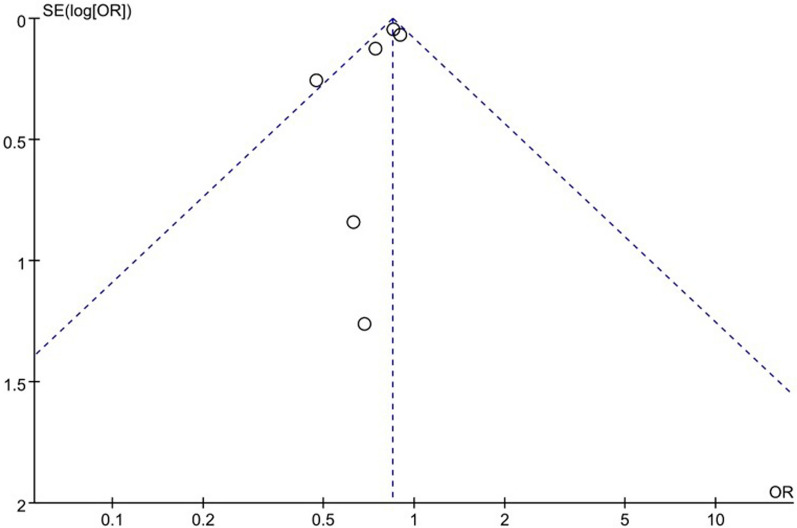
Publication of bias
A funnel plot of the overall complication was used to assess publication bias. The bilaterally symmetrical funnel plot of overall complication showed that no obvious evidence of publication bias was observed (Fig. 8).
Fig. 8.
Funnel plot of the meta-analysis
Conclusion
In summary, thoracic day surgery has more advantages over inpatient surgery in terms of length of postoperative hospital stay, operative time, average hospital cost, 30-day mortality and postoperative complications. We demonstrate that younger patients, patients receiving segmental resections by VATS, and those with better pulmonary function tests or without comorbidity can be discharged POD1 with low rates of complications and 30-day mortality, especial with ERAS program. More large-sample, high-quality studies are necessary to identify patient and institutional factors necessary for safe POD1 discharge in the future and day surgery for lung cancer incorporating the ERAS concept is a safe and effective modality.
Acknowledgements
We greatly appreciate the assistance of the staff of the Department of Thoracic Surgery, West-China Hospital, Sichuan University, and thank them for their efforts.
Author contributions
CS was involved in drafting the manuscript. CS was involved in acquisition of data. GC designed and revised the manuscript. All authors have read and approved the final manuscript.
Funding
National Natural Science Foundation of China (No. 72104161), Sichuan Province Science and Technology Support Program (No. 2020JDKP0023), Chengdu science and technology Support Program (No. 2022-YF05-01560-SN),
Declarations
Consent for publication
All the authors consent to publish the paper.
Competing interests
The authors have no conflicts of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Huang L, Kehlet H, Petersen RH. Reasons for staying in hospital after video-assisted thoracoscopic surgery lobectomy. BJS Open. 2022 doi: 10.1093/bjsopen/zrac050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drawbert HE, Hey MT, Tarrazzi F, Block M, Razi SS. Early discharge on postoperative day 1 following lobectomy for stage I non-small-cell lung cancer is safe in high-volume surgical centres: a national cancer database analysis. Eur J Cardio Thorac Surg Off J Eur Assoc Cardio Thorac Surg. 2022;61(5):1022–1029. doi: 10.1093/ejcts/ezab490. [DOI] [PubMed] [Google Scholar]
- 3.Chen T, Wei H, Yue W, Su Y, Fu X. Enhanced recovery after surgery management of perioperative period in surgical lung cancer patients: protocol for a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2022;12(2):e056068. doi: 10.1136/bmjopen-2021-056068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel DC, Leipzig M, Jeffrey Yang CF, et al. Early discharge after lobectomy for lung cancer does not equate to early readmission. Ann Thorac Surg. 2022;113(5):1634–1640. doi: 10.1016/j.athoracsur.2021.05.053. [DOI] [PubMed] [Google Scholar]
- 5.Jiang L, Lei T, Zhou K, Ma H, Che G. Pivotal role of video-assisted thoracoscopic surgery in improving survival outcome of stage I non-small cell lung cancer in day surgery patients. Thoracic Cancer. 2021;12(21):2865–2872. doi: 10.1111/1759-7714.14145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong Y, Shen C, Wang Y, et al. Safety and feasibility of video-assisted thoracoscopic day surgery and inpatient surgery in patients with non-small cell lung cancer: a single-center retrospective cohort study. Front Surg. 2021;8:779889. doi: 10.3389/fsurg.2021.779889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Linden PA, Perry Y, Worrell S, et al. Postoperative day 1 discharge after anatomic lung resection: a society of thoracic surgeons database analysis. J Thorac Cardiovasc Surg. 2020;159(2):667–78.e2. doi: 10.1016/j.jtcvs.2019.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Towe CW, Khil A, Ho VP, et al. Early discharge after lung resection is safe: 10-year experience. J Thorac Dis. 2018;10(10):5870–5878. doi: 10.21037/jtd.2018.09.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dong Y, Zhu D, Che G, et al. Clinical effect of day surgery in patients with lung caner by optimize operating process. Zhongguo fei ai za zhi = Chin J Lung Cancer. 2020;23(2):77–83. doi: 10.3779/j.issn.1009-3419.2020.02.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geraci TC, Chang SH, Chen S, Ferrari-Light D, Cerfolio RJ. Discharging patients by postoperative day one after robotic anatomic pulmonary resection. Ann Thorac Surg. 2021 doi: 10.1016/j.athoracsur.2021.06.088. [DOI] [PubMed] [Google Scholar]
- 11.Shi Y, Zhu P, Jia J, et al. Cost-effectiveness of same-day discharge surgery for primary total hip arthroplasty: a pragmatic randomized controlled study. Front Public Health. 2022;10:825727. doi: 10.3389/fpubh.2022.825727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paluch AJ, Matthews AH, Mullins S, Vanstone RJ, Woodacre T. Adopting the day surgery default in the provision of lumbar discectomy and decompressive surgery. J Perioper Pract. 2022 doi: 10.1177/17504589211054360. [DOI] [PubMed] [Google Scholar]
- 13.Olry de Labry Lima A, Lima A, Spacirova Z, Espin J. Description of day case costs and tariffs of cataract surgery from a sample of nine European countries. Cost Eff Resour Alloc. 2022;20(1):11. doi: 10.1186/s12962-022-00346-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yu Y, Li M, Kang R, et al. The effectiveness of telephone and internet-based supportive care for patients with esophageal cancer on enhanced recovery after surgery in China: a randomized controlled trial. Asia Pac J Oncol Nurs. 2022;9(4):217–228. doi: 10.1016/j.apjon.2022.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yeom J, Lim HS. Effects of the enhanced recovery after surgery (ERAS) program for colorectal cancer patients undergoing laparoscopic surgery. Clin Nutr Res. 2022;11(2):75–83. doi: 10.7762/cnr.2022.11.2.75. [DOI] [PMC free article] [PubMed] [Google Scholar]