Summary
Background
Community-acquired pneumonia (CAP) is a leading cause of mortality worldwide, but disease burden of CAP is not clear so far. We aim to explore the spatial and temporal trends of mortality and years of life lost (YLL) due to CAP during 2013–2021 in mainland China, especially the mortality changes before and during COVID-19 pandemic due to COVID-19 related non-pharmaceutical interventions (NPIs).
Methods
We used data from the National Mortality Surveillance System to estimate the age-standardized rates of death and YLL of CAP at national and provincial level in China during 2013–2021. Monthly and provincial NPIs data were obtained from Oxford COVID-19 Government Response Tracker. The Average annual percentage change (AAPC) and mortality reduction were estimated by log-linear regression and interrupted time series, respectively.
Findings
In China, most CAP that caused deaths had no clear etiology, and bacterial pneumonia and viral pneumonia were the leading 2 causes among CAP deaths with determined etiology before and during COVID-19 pandemic. The age-standardized CAP mortality rate decreased from 11.18 per 100,000 in 2013 to 8.76 per 100,000 in 2019, and to 5.74 per 100,000 in 2021 (AAPC −4.51% vs −7.89%). Trends were similar in age-standardized rate of YLL. Both rates declined more for viral pneumonia, compared with bacterial pneumonia. After adjusting for NPIs at provincial level after 2020, the NPIs for COVID-19 was associated with significant reductions in CAP mortality (−0.34 per 100,000, −0.41 to −0.27; p < 0.0001), and provinces that economically developed and conducted strict regular NPIs against COVID-19 contributed the most reduction.
Interpretation
We observed a decreasing trend of age-standardized CAP mortality from 2013 to 2019, and a dramatical reduction during COVID-19 pandemic, especially for viral pneumonia. Our study provided the evidence for the effectiveness of regular NPIs on the significant reductions in CAP mortality.
Funding
This work has been supported by Beijing Municipal Science and Technology Project Z191100006619101, Chinese Academy of Medical Sciences (CAMS) Innovation Fund for Medical Sciences (CIFMS 2021-I2M-1-048), CAMS Institute of Respiratory Medicine Grant for Young Scholars (2023-ZF-8) and the New Cornerstone Science Foundation.
Keywords: Community-acquired pneumonia, Age-standardized mortality, Years of life lost, COVID-19, Viral pneumonia
Research in context.
Evidence before this study
Community-acquired pneumonia (CAP) is a major health threat and results in high burden of disease both in morbidity and mortality globally. In China, the incidence of CAP was estimated as high as 7.13 per 1000 person-year and the number of CAP episodes was estimated over 9.5 million in 2016. As the aging of the large population and the pandemic of COIVD-19, the number of CAP episodes and following deaths would change rapidly, leading to the dynamic burden of CAP in China.
We identified literatures on PubMed from previous studies that focused on the disease burden of CAP with the search items (“disease burden” OR “mortality” OR “Years of life lost”) AND (“Community-acquired pneumonia”) AND (“trend” OR “dynamic∗” OR “temporal”) AND (“China”), with no language restrictions, from December 31, 2013 to May 1, 2023. We found that no studies have reported the temporal changes of mortality and Years of life lost (YLL) due to CAP in China yet.
Added value of this study
High-quality data source from the national mortality surveillance system was adopted in this study, reasonable to deduce the total death numbers, CAP mortality and YLLs at a national level. Particularly, we took the pandemic of COVID-19 into consideration, during which non-pharmaceutical interventions (NPIs) not only ceased the spread of COVID-19, but also weakened the transmission of many other pathogens.
Our findings indicate that the burden of CAP differed across seasons or geographic regions. Most CAP that caused deaths had no clear etiology, and CAP with clear etiology mainly included bacterial CAP and viral CAP. Before and during the COVID-19 pandemic in China, the age-standardized CAP mortality rate decreased significantly from 2013 to 2019 and to 2021, with more decline in viral pneumonia compared with bacterial pneumonia. By performing phased analysis, we found the NPIs for COVID-19 was associated with significant reductions in CAP mortality. These evidence from our study contributed to the estimation of global burden of disease on CAP, and consistent with the theory that implementing NPIs would benefit population by reducing burden of CAP.
Implications of all the available evidence
Our study, along with previous evidence, indicates that the huge mortality gap among age groups remains, re-emphasizing the calls for protection on the elderly, for example, by vaccinations. Our study illustrates that most deaths during the past decade were attributed to unspecified organism, indicating the difficulty also exists in determining etiology among CAP patients in China. Previous studies reported that strict domestic and international NPIs contributed to the control of COVID-19 and other respiratory infectious diseases, and finally led to the steeper reductions of CAP, especially for viral pneumonia. Our study verified the dramatical reduction on CAP mortality during 2020–2021, compared with the mortality before 2020.
Introduction
Community-acquired pneumonia (CAP) is an acute low respiratory tract infection involving lung parenchyma, which is one of the leading causes of mortality and morbidity globally, especially in patients with immunosuppression or immunocompromise.1 CAP has usually been considered accountable for the substantial medical and socioeconomic burden. Statistics in 2019 reported that CAP and influenza together contributed the most deaths among infectious diseases in United States.2 According to previous studies, CAP led to millions of ambulatory care and emergency department visits worldwide, and hospitalization rates and intensive care unit (ICU) admission rates due to CAP increased by year, especially among the elderly.3 The case-fatality rate of hospitalized CAP patients was 6.5%–8.7%,3,4 however, more than half of those hospitalized had complicated comorbidities or developed severe CAP; severe sepsis occurred in a fourth of the participants, among whom 27% died within 1 year.5
In China, although achieving the highest reduction in pneumonia incidence of children under 5 years old among developing countries from 2000 to 2015,6 the incidence of CAP was estimated as high as 7.13 per 1000 person-year and the number of CAP episodes was estimated over 9.5 million in 2016.7 As the aging of the large population and prolonged life expectancy in China, the number of CAP episodes and following deaths would predictably increase rapidly along with increasing number of the elderly, contributing to escalating high burden of CAP in China. Thus, understanding the mortality and years of life lost (YLL) of CAP is of strategic significance in promoting the management of CAP in health institutes and rational medical resource allocation by policymakers. However, no studies have reported the temporal changes of mortality and YLLs due to CAP in China yet.
To accurately explore the changes of CAP mortality and YLL in China, we must recognize the possible impact of the pandemic of coronavirus disease 2019 (COVID-19) and accompanying non-pharmaceutical interventions (NPIs). Research have claimed that NPIs during the pandemic not only ceased the spread of COVID-19, but also weakened the transmission of many other pathogens, like influenza viruses and human metapneumovirus.8 In both China and United States, considerable nationwide reductions in influenza activity due to NPIs were observed by surveillance.9 Therefore, a phased analysis of the CAP burden in China before and during the COVID-19 pandemic is warranted.
In this study, by using data from the national mortality surveillance system (NMSS) in mainland China, we aimed to provide national and provincial estimates of mortality and YLLs for CAP during 2013–2021, especially focusing on temporal, seasonal and age trends, and different change patterns before and during the COVID-19 pandemic. It will further provide clues for the government and health institute to improve the management of CAP in Chinese population.
Methods
Data source
Mortality and population data
The CAP mortality data were acquired from the National Mortality Surveillance System (NMSS) with national and provincial representativeness, managed by the Chinese Center for Disease Control and Prevention (China CDC).10,11 Detailed descriptions of NMSS have been published elsewhere.12 Briefly, this system collects deaths occurred in hospital and outside-of-hospital through an internet-based reporting platform, which covers over 300 million residents, approximately 24% of China's population, from 605 counties or districts in urban in 31 mainland provinces, municipalities, and autonomous regions. Data for under-reporting adjustment were derived from NMSS retrospective under-reporting field surveys implemented in 2015 and 2018 separately, which collect data for under-reporting rate (URR) during 2013–2017. The population data for each disease surveillance points (DSP) and province were extracted and updated annually from China National Bureau of Statistics.13 Data of Chinese sixth census in 2010 were served as standard population for age-standardization of rate.14
Definitions
The winter is defined as time period including November, December and January; spring includes February, March and April; summer includes May, June and July; autumn includes August, September and October.
COVID-19 NPIs data
The information on government's COVID-19 daily NPIs across China and its provinces (autonomous regions and municipalities) from January 1, 2020 to December 31, 2021 were downloaded from the Oxford COVID-19 Government Response Tracker (OxCGRT; https://github.com/OxCGRT/covid-policy-tracker-legacy. Accessed 27 April 2023.).15 The OxCGRT established a series of indicators on behalf of government's response during the COVID-19 pandemic, involving containment and closure (C1–C8), economic responses (E1–E4), health systems (H1–H7) and other miscellaneous responses (H1). The OxCGRT stringency index, ranging 0 to 100, systemically incorporated all above measures, and high values reflect more stringent restriction. Based on previous studies and epidemiological principles, our study selected nine NPI indicators with different ordinal scales, C1–C8 and H1, which played an important role in virus transmission. The indicators, C1–C8, mainly included school and working place closing, and restrictions on gather size and movement, and H1 refers to public information campaign. Each ordinal indicator was converted to a numeric score between 0 and 100 through the normalization method. Given the potential multicollinearity among these indicators, we used principal component analysis (PCA) to extract the first three components with the cumulative contribution rate having reached 70%. The first principal component (PC1) represented the restriction of personal contact, including closure of school, workplace, and public transport, and stay-at-home requirement. The second principal component (PC2) was closely related to enhancing self-protection, comprising of Restrictions on international travel and public information campaign. The third principal component (PC3) was dominated by crowd gatherings control, involving the cancellation of public events, and restrictions on gathering size and internal movement. We reconstructed the data along the principal component axes and because of standardization of data, the mean of each principal component is 0, and a larger value represents a higher level of stringency.
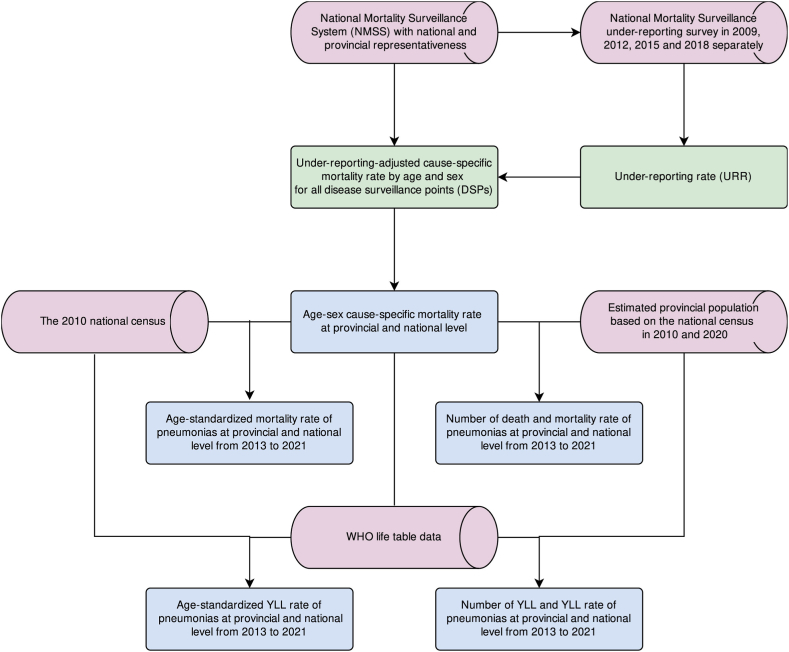
CAP mortality estimation
A flow chart of the estimation of mortality and YLL due to CAP was shown in Fig. 1. Firstly, we conducted the redistribution of garbage codes, defined as deaths with non-specific codes, or codes that could not be underly causes of death, which were reclassified by age, sex, location, and year to the most likely causes of death based on the methods developed by Naghavi and colleagues.16 Secondly, we used International Classification of Disease 10th Edition (ICD-10) to identify CAP deaths. Details of ICD codes were reported in Supplementary Table Sl. Thirdly, we calculated under-reporting rate (URR) annually among 31 provinces (autonomous regions and municipalities) during 2013–2017, and used splines regression to predict URR from 2018 to 2021. Besides, given that URR was almost stable from Jan. to Dec. of each year, so we used annual URR as a surrogate of monthly URR. Fourthly, we derived under-reporting-adjusted CAP mortality rate by age and sex for all provinces by dividing reported CAP mortality rate by (1-URR) during 2013–2021. Furthermore, we multiplied annually under-reporting-adjusted CAP mortality rate by age-sex-province group with the provincial population to obtain estimated number of CAP deaths, and calculated age-standardized rates by the direct method of standardization.
Fig. 1.
Flowchart of this study. Abbreviations: YLL, years of life lost.
Computation of YLL
The index YLL to measure premature deaths, was calculated as total deaths multiplied by the standard life expectancy at each age. We used a theoretical minimum risk reference life table, which was established based on selecting the lowest observed risk of death for each 5-year age group in all population over 5 million as standard life expectancy, to estimate the YLL for CAP during 2013–2021.17
Statistical analysis
Estimation of AAPC
We estimated the average annual percentage change (AAPC) to measure the trend change in rate and age-standardized rate during 2013–2019 and during 2013–2021 respectively by using a generalized linear regression model that obeys a gaussian distribution.18 We used Chi-square tests to compare the differences in the rates among regions, sexes, ages, and etiologies, and Benjamini-Hochberg correction to conduct multiple comparisons and post-hoc statistical analyses. We assessed the temporal trends of rates applying Mann–Kendall test. Two-tailed p < 0.05 were considered statistically significant.
COVID-19 NPIs and CAP mortality
We estimated monthly mortality rates due to CAP at the provincial and national level during 2013–2021. Monthly mortality rate in China were decomposed into seasonal and trend components using Seasonal-Trend decomposition procedure based on locally weighted regression (LOESS).19 The adjustments for the seasonal window parameter were made to ensure no season pattern in the residuals remained.
We used interrupted time series methods with seasonal autoregressive integrated moving average (SARIMA) to assess the effect of NPIs on regular CAP mortality for each province.20,21 The regular NPIs refer to China's specific regular COVID-19 epidemic prevention and control measures, including dynamic zero-COVID policy, health code, the long-term quarantine system, COVID-19 nucleic acid testing and vaccinations for the whole population, and the official accountability system, which were implemented all the time during the study period. We included a binary variable in this model to reflect the implementation of regular NPIs, taking a value of 0 from Jan 1, 2013 to Dec 30, 2019, and a value of 1 from Jan 1, 2020 to Dec 30, 2021. Models also were adjusted for the degree of the local government interventions, measured by OxCGRT stringency index, to reduce the impact of additional restrictions included lockdown during COVID-19 outbreak. Furthermore, we pooled province-specific associations between regular NPIs and CAP mortality applying fixed effect meta-analysis to obtain national average summary estimate. Besides, we modeled monthly mortality rates due to CAP before COVID-19 epidemic using ARIMA method, to estimate the expected CAP mortality in the absence of COVID-19 epidemic-related restrictions nationally and provincially during 2020–2021.
Moreover, we explored the relationship between various NPI measures and relative reduction of monthly CAP mortality across all provinces during 2021–2021 by using an individual-time fixed panel data model.22,23 The relative reduction of monthly CAP mortality was calculated as the difference of observed and expected mortality divided by expected mortality, while PC1-PC3 represented three kinds of NPI measures. Single NPI measure as the independent variable was also regressed on relative reduction of monthly CAP mortality. In the main analysis, we removed the data from January to March 2020 in Hubei province because observed CAP mortality rates were far greater than expected during COVID-19 outbreak. Given the impact of data filtration on the accuracy of results, we conducted the first sensitivity analysis that restricted the related reduction from January to March 2021 in Hubei province to be zero. Besides, in the second sensitivity analysis, we used linear mixed effect model, in which provinces were included as random effect factors, to regress the data from the main analysis to confirm the robustness of results. Furthermore, given that the implementation of various NPIs reduced the transmission of CAP, and thereby reduce the incidence rate. Generally, patients with CAP would die after a few days. We set the lag window (the time interval between onset and death) as 1 month. We then conducted the third sensitivity analysis to regress three PCs on relative reduction of monthly CAP mortality with a lag of one month using the data and methods from the main analysis. In this study, all analyses were performed in R version 4.0.4 (The R foundation for Statistical Computing).
Role of the funding source
The funders had no role in any aspects of the study.
Results
CAP mortality and YLL estimation
We estimated a total of 168,700 CAP deaths in 2013, 176,004 deaths in 2019, and 128,720 deaths in 2021. The CAP mortality rate per 100,000 people was 12.61 in 2013, 12.62 in 2019 (AAPC during 2013–2019: −0.47%, 95% CI −2.08% to −1.16%), and 9.02 in 2021 (AAPC during 2013–2021: −4.04%, 95% CI −6.64% to −1.36%). The age-standardized mortality rate per 100,000 people was significantly decreased from 11.18 in 2013 to 8.76 in 2019 (AAPC −4.51%, 95% CI −6.10% to −2.88%), and to 5.74 in 2021 (AAPC −7.89, 95% CI −10.37% to −5.34%). The age-standardized rate of YLL per 100,000 people was also significantly decreased in 2019 (183.92, AAPC −6.30%, 95% CI −8.02% to −4.55%) and 2021 (111.98, AAPC −9.78%, 95% CI −12.31% to −7.17%), compared with that in 2013. The estimated number of deaths, age-standardized mortality rate, and age-standardized rate of YLL due to CAP were higher in the male than that in the female during 2013–2021, and the female had higher AAPC in age-standardized mortality rate than that in the male (all p < 00001). (Table 1, Supplementary Figure S1).
Table 1.
The estimated number of deaths, mortality rate, and age-standardized mortality rate and YLL rate for CAP from 2013 to 2021 in China.
| Year | Estimated number of deaths |
Mortality rate (1/100,000)a |
Age-standardized mortality rate (1/100,000) |
Age-standardized YLL rate (1/100,000) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | Male | Female | Total | Male | Female | Total | |
| 2013 | 93,171 | 75,529 | 168,700 | 13.59 | 11.58 | 12.61 | 13.72 | 8.97 | 11.18 | 315.37 | 204.41 | 258.95 |
| 2014 | 100,198 | 82,375 | 182,573 | 14.56 | 12.58 | 13.59 | 14.17 | 9.32 | 11.58 | 326.52 | 207.91 | 266.49 |
| 2015 | 87,994 | 75,662 | 163,656 | 12.72 | 11.5 | 12.12 | 11.93 | 8.07 | 9.88 | 269.71 | 177.4 | 222.89 |
| 2016 | 88,626 | 75,472 | 164,098 | 12.73 | 11.4 | 12.08 | 11.49 | 7.66 | 9.46 | 262.59 | 163.19 | 212.54 |
| 2017 | 90,449 | 75,765 | 166,214 | 12.9 | 11.35 | 12.14 | 11.17 | 7.27 | 9.09 | 237.43 | 147.46 | 191.53 |
| 2018 | 95,579 | 79,552 | 175,131 | 13.52 | 11.81 | 12.69 | 11.26 | 7.28 | 9.14 | 238.48 | 149.89 | 193.08 |
| 2019 | 97,852 | 78,152 | 176,004 | 13.71 | 11.49 | 12.62 | 11.01 | 6.77 | 8.76 | 235.55 | 134.1 | 183.92 |
| AAPC during 2013–2019 (%) | −0.39 (−2.32, 1.59) | −0.58 (−1.92, 0.78) | −0.47 (−2.08, 1.16) | −4.14 (−5.99, −2.26) | −5.01 (−6.39, −3.62) | −4.51 (−6.10, −2.88) | −5.66 (−7.60, −3.68) | −7.24 (−8.78, −5.67) | −6.30 (−8.02, −4.55) | |||
| 2020 | 71,129 | 54,693 | 125,822 | 9.86 | 7.95 | 8.92 | 7.59 | 4.55 | 5.97 | 156.09 | 90.17 | 122.17 |
| 2021 | 73,749 | 54,970 | 128,720 | 10.1 | 7.88 | 9.02 | 7.43 | 4.29 | 5.74 | 145.31 | 80.92 | 111.98 |
| AAPC during 2013–2021 (%) | – | – | – | −3.51 (−5.94, −1.01) | −4.69 (−7.58, −1.72) | −4.04 (−6.64, −1.36) | −7.23 (−9.61, −4.80) | −8.76 (−11.41, −6.03) | −7.89 (−10.37, −5.34) | −9.03 (−11.56, −6.43) | −10.8 (−13.34, −8.18) | −9.78 (−12.31, −7.17) |
Abbreviations: CAP, community-acquired pneumonia; YLL, year of life lost; AAPC, average annual percent change.
Differences between groups were tests by Chi-square test and all p < 0.0001.
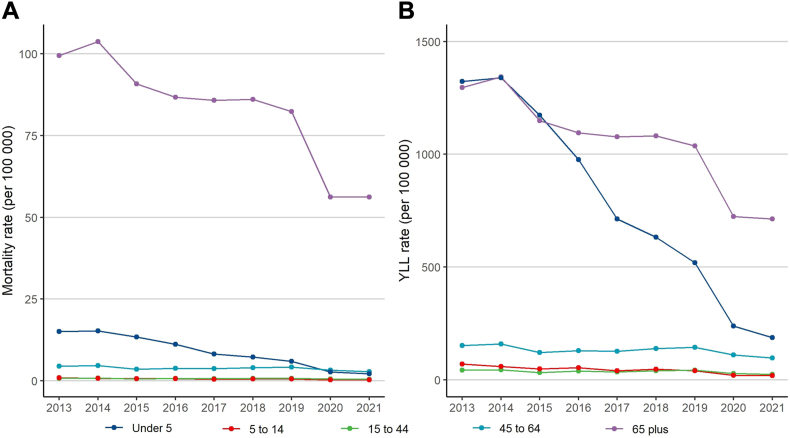
The mortality rates per 100,000 people in population aged over 65 remained the highest, and significantly decreased from 2013 to 2021 (99.48 vs 56.15). Similar trend was observed in the YLL rates for people aged over 65. For population aged under 5, the mortality rate declined gradually during this period, while the YLL rate plunged from 1323.33 per 100,000 people in 2013 to 519.01 per 100,000 people in 2019, and to 187.20 per 100,000 people in 2021 (Fig. 2).
Fig. 2.
Mortality rate and YLL rate for CAP by age groups from 2013 to 2021 in China. Abbreviations: YLL, years of life lost; CAP, community-acquired pneumonia.
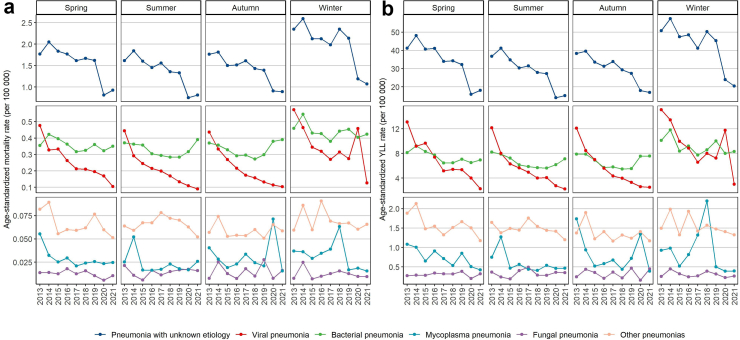
Seasonal and etiological distribution in CAP mortality
Overall, the CAP mortality was highest in winter, following by spring, during 2013–2021, and the major etiological type of pneumonia was pneumonia with unspecified organism, followed by bacteria pneumonia and viral pneumonia. Pneumonia with unspecified organism fluctuated in proportions among all cases from 67.1% in 2013 to 74.0% in 2019 and to 64.5% in 2021 and declined in age-standardized mortality rate during this period. The age-standardized mortality rate and YLL rates less changed for bacterial pneumonia during this period, but both rates considerably declined for viral pneumonia, especially from 2013 to 2014 and from 2020 to 2021. For other etiologies, the age-standardized mortality rates or YLL rates were relatively low, and comparable at most seasons or years (p values were not shown). (Fig. 3, Supplementary Figure S2).
Fig. 3.
Age-standardized mortality rate and YLL rate for CAP by season and etiology from 2013 to 2021 in China. Abbreviations: YLL, years of life lost; CAP, community-acquired pneumonia.
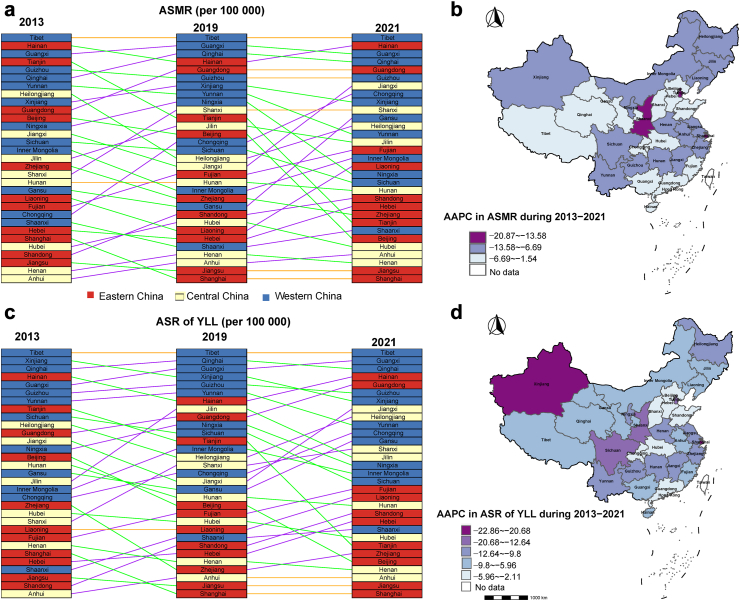
Regional geographic distribution of CAP mortality
As is shown in Fig. 4, the age-standardized mortality rates and YLL rates differed at the provincial level during 2013–2021 across China, and western China had the highest mortality and YLL, followed by eastern China and central China. All pairwise comparisons were statistically significant (p < 0.01) among different regions for the age-standardized mortality rates or YLL rates, except for the comparison between eastern China and central China on the age-standardized mortality rate in 2015 (p = 0.305). The age-standardized mortality rates and YLL rates were lowest in Shaanxi, Jiangsu, Henan, and Anhui provinces in 2021, and highest in Tibet, Guangxi, Qinghai, and Hainan provinces. AAPC was highest for Shaanxi province in age-standardized mortality rates, and highest for Tibet in age-standardized YLL rates (Fig. 4, Supplementary Table S2).
Fig. 4.
Changes and geographic distributions of ASMR and ASR of YLL for CAP from 2013 to 2021 by province in China. Note: Panel a and c show the rankings of provinces in 2013, 2019, and 2021 according to ASMR and ASR of YLL for CAP respectively, and the top rank means the highest and the bottom rank means the lowest ASMR or ASR of YLL in China; panel b and d display the AAPC from 2013 to 2021 in ASMR and ASR of YLL respectively. The cut-off values in panels (b and d) were determined based on the Jenks Natural Breaks method, which groups similar values that “minimize differences between values in the same class and maximum the difference between classes”. Abbreviations: CAP, community-acquired pneumonia; YLL, year of life lost; AAPC, average annual percent change; ASMR, age-standardized mortality rate; ASR, age-standardized mortality rate.
Impact of NPIs on CAP mortality
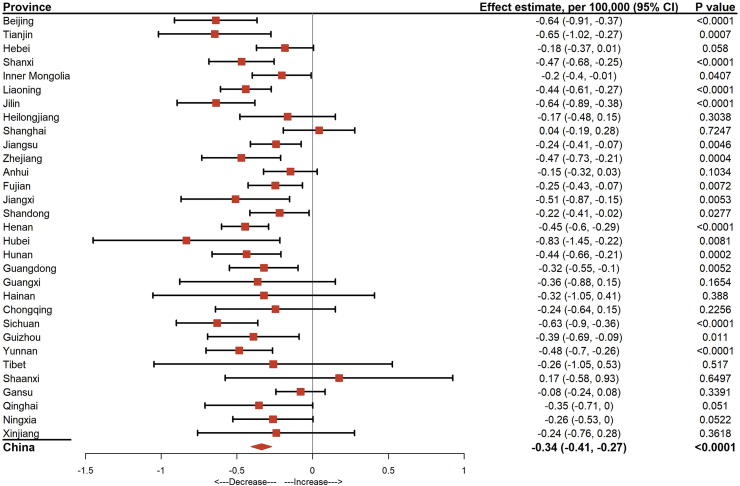
The implementation of regular NPIs during the COVID-19 epidemic was associated with a decrease of 0.34 per 100,000 population per month in CAP mortality (95% CI −0.40 to −0.27, p < 0.0001) (Fig. 5). We observed the significantly mortality reduction due to the implementation of regular NPIs in more than 50% (18/31) provinces, among which Hubei province had a maximum decrease (0.83 per 100,000 population), followed by Beijing, Tianjin, Liaoning, and Sichuan provinces, with a decrease of over 0.6 per 100,000 population in CAP mortality., and most of them were with a high level of stringency (Fig. 5, Supplementary Figure S3). We also observed that the mortality declined after NPIs implemented during COVID-19. The underlying decomposed trend rate was approximately one death per 100,000 people per month before 2020, approximately double the decomposed trend rate during the implementation of NPIs. Seasonality in the CAP mortality was evident, with rates peaking from December to January next year (Supplementary Figure S4).
Fig. 5.
The effect estimates of COVID-19 related NPIs on the reduction of CAP mortality at provincial and national levels in China. Note: Effect and 95% CI were estimated by interrupted time series model; the estimate represents the decrease in CAP mortality per 100,000 population per month. Abbreviations: CAP, community-acquired pneumonia; CI, confidence interval; NPIs, non-pharmaceutical interventions.
In the main analysis and the sensitivity analyses, we found the combination of certain NPIs, including PC1 (including closings of schools, closings of workplaces, closing of public transport and staying in place or at home) and PC3 (including cancelling public events, limits on gatherings and restrictions on internal travel), were significantly associated with the reduction of CAP mortality (Supplementary Figure S5). While taking each NPI into main analysis, closings of workplaces (p = 0.022), cancelling public events (p = 0.009), staying in place or at home (p = 0.046) and restrictions on internal travel (p = 0.039) showed significant effect on the decrease of CAP mortality (Supplementary Figure S6).
Discussion
In this study, we for the first time presented the decreasing trend of age-standardized CAP mortality and YLL from 2013 to 2019, and a dramatical reduction during COVID-19 pandemic in mainland China, especially on viral pneumonia. Notably, the reductions differed across provinces and gender, and the mortality in the elderly remained high. Our study indicated that most CAP that caused deaths had no clear etiology, and bacterial pneumonia and viral pneumonia were the leading 2 causes among CAP deaths with determined etiology before and during COVID-19 pandemic. Regular NPIs were proved effective through the significant reductions in CAP mortality.
The decreasing trend of CAP mortality before COVID-19 pandemic in our study may attribute to the integrated effect of the rapid development on social economy, education, living standard and quality of the residents, medical techniques, and philosophies of evidence-based medicine practice.24,25 National policy in China has proven its potent impetus in medical fields by series of five-year plans, and the Healthy China 2030 blueprint is furtherly devoted to health related strategies such as risk-factor elimination, population nutrition improvement and healthy lifestyles promotion.26 Meanwhile, guidelines of CAP were constantly written and updated to promote clinicians to diagnose, prescribe and treat rationally, with synthesized experiences home and aboard, by Chinese Thoracic Society of Chinese Medical Association. Of note, the crude mortality of CAP in study was comparable with that reported in the United States (13.4 per 100,000 for pneumonia, and 15.2 per 100,000 for influenza and pneumonia) in 2019,27,28 and lower than Peru.29 However, the huge gap among age groups re-emphasizes the calls for protection on the elderly, for example, to promote influenza, streptococcal, and COVID 19 vaccination.30
Also, seasonal differences on CAP mortality were notable, as more deaths occurred in winter and spring according to our study. Previous studies have shown that influenza and invasive pneumococcal infection rise and fall in an annual seasonal pattern, and the peaks of infection, admission and death mostly happened in winter, when the climate was relatively cooler and humidity was lower.31, 32, 33, 34 The possible hypotheses may lie in the seasonal variation in immune response host physiology,35 the increasing host biologic susceptibility of bacteria in respiratory tract secondary to virus infection, or even the cyclical variation's impact on the susceptibility.33 Nevertheless, the seasonal patterns of CAP were not unalterable; according to a recent study, during the pandemic of COVID-19, the non-COVID CAP admissions peaked every 6 months instead of only in winter due to complicated reasons.36 However, seasonal variations in CAP mortality are complicated in various factors, we cannot draw conclusions simply based on the phenomenon description but only provide clues to future investigations, and indicate that the medical resources should be allocated flexibly according to the rules of mortality change.
In our study, bacterial pneumonia kept slightly higher and maintained stable in mortality, compared with that of viral pneumonia. This is compensable, as 2016 clinical practice guidelines for the first time placed emphasis on the early diagnosis and anti-viral treatment of viral pneumonia in China,25 which, along with other efforts, such as the constant promotion of vaccination of influenza and other respiratory viruses, especially in high risk populations,37, 38, 39 contributed to the significantly decrease in the mortality of viral pneumonia we observed in this study. While for bacterial pneumonia, although experts in public health and clinical medicine have been recommending the vaccination of pneumococcal pneumonia, the mortality of bacterial pneumonia may not decline as expected. It still needs further studies to determine that implementing laboratory pathogen surveillance in each province would be helpful or not to reduce the mortality of CAP by locating the prevalent etiology.
We observed significant regional differences on CAP mortality reduction across provinces in this study. The underlying factors contributing to the discrepancy may be due to the economic development level, the proficiency in epidemic prevention policies implement, the compliance of local community residents, and strict level of NPIs. Most of these factors were gradually improved for different provinces, especially where the COVID-19 ever outbroke during 2020–2021. However, although varies among provinces, our study verified the dramatical reduction on CAP mortality in China during 2020–2021, compared with the mortality of CAP before 2020, especially for viral pneumonia, which may be more sensitive to NPIs. Strict domestic and international NPIs like closing of public transport, staying in place or at home and restrictions on internal travel contributed to the control of COVID-19 and other respiratory infectious diseases, and finally led to the steep reduction of CAP mortality.40,41 However, the uncertainties on the morbidity and mortality of CAP added as the pandemic has been declared over by WHO. NPIs has been getting relaxed, and the population with decreased exposure to respiratory pathogens would be more susceptible to get infected and evolve to severe CAP in the future, especially for the elderly. Recent study has shown that the COVID-19 pandemic was associated with increases in hospital mortality, ICU admission and invasive mechanical ventilation rates of non-COVID-19 CAP, because of decreased use of pneumococcal vaccine, aggravated comorbidities due to frequent COVID-19 and insufficient medical care, increased alcohol et al.36 The immunity gap may be filled with vaccinations of influenza virus and pneumococcal pneumonia, but more efforts focus on more interventions should be taken by the authorities and health care institutes, and be prepared for the potential rebound of CAP.
This study has some limitations. First, the CAP deaths were counted only if CAP was coded by ICD-10 and noted as the underlying cause of death. The quality of coding relied heavily on local doctors of the survey site, which differed across different provinces or regions in China. Thus, the mortality of CAP may be underestimated. Second, the detailed etiology of CAP deaths was hard to retrieve as the information were lack in the system. Third, although sepsis and septic shock are important fatal cause of CAP, while the information is missing in the database. Forth, although NPIs were proved potentially effective in decreasing the mortality of CAP, data on other possible confounding factors like vaccination of COVID-19, influenza and pneumococcal pneumonia, undetected COVID-19 infections and asymptomatic infections were unavailable, which inevitably restricted the causal inference in our study. Fifth, this study explored the populational, regional and temporal distributions of the underlying cause of CAP death and provided detailed information by various subgroup analyses, for example, sex and age, and discussed these factors in Discussion. However, more information on potential confounders like comorbidity or BMI were unavailable in NMSS. To investigate the impact of the cofounders on CAP mortality, cohort or case–control studies are warranted in the future.
Conclusion
We observed a decreasing trend of age-standardized CAP mortality and YLL from 2013 to 2019, and a dramatical reduction during COVID-19 pandemic, with more decline in viral pneumonia compared with bacterial pneumonia. Our study also provided the evidence for the effectiveness of regular NPIs on the significant reductions in CAP mortality.
Contributors
BC and MGZ had the idea for and designed the study and had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. BC, GHF, ZYC and FZ drafted the paper. BC, GHF, YCZ, FZ, and ZGY performed the analysis, and all authors critically revised the manuscript for important intellectual content and gave final approval for the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. None of the material has been published or is under consideration elsewhere, including the Internet.
Data sharing statement
Readers can access the data by contacting the corresponding authors to acquire permission.
Editorial note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
All authors declared no conflicts of interest.
Acknowledgements
We acknowledge all health-care workers involved in this study.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100968.
Contributor Information
Maigeng Zhou, Email: zhoumaigeng@ncncd.chinacdc.cn.
Bin Cao, Email: caobin_ben@163.com.
Appendix A. Supplementary data
References
- 1.Metlay J.P., Waterer G.W., Long A.C., et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American thoracic society and infectious diseases society of America. Am J Respir Crit Care Med. 2019;200(7):e45–e67. doi: 10.1164/rccm.201908-1581ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heron M. Deaths: leading causes for 2019. Natl Vital Stat Rep. 2021;70(9):1–114. [PubMed] [Google Scholar]
- 3.Ramirez J.A., Wiemken T.L., Peyrani P., et al. Adults hospitalized with pneumonia in the United States: incidence, epidemiology, and mortality. Clin Infect Dis. 2017;65(11):1806–1812. doi: 10.1093/cid/cix647. [DOI] [PubMed] [Google Scholar]
- 4.Falguera M., Pifarre R., Martin A., Sheikh A., Moreno A. Etiology and outcome of community-acquired pneumonia in patients with diabetes mellitus. Chest. 2005;128(5):3233–3239. doi: 10.1378/chest.128.5.3233. [DOI] [PubMed] [Google Scholar]
- 5.Yende S., D'Angelo G., Kellum J.A., et al. Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med. 2008;177(11):1242–1247. doi: 10.1164/rccm.200712-1777OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McAllister D.A., Liu L., Shi T., et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis. Lancet Glob Health. 2019;7(1):e47–e57. doi: 10.1016/S2214-109X(18)30408-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sun Y., Li H., Pei Z., et al. Incidence of community-acquired pneumonia in urban China: a national population-based study. Vaccine. 2020;38(52):8362–8370. doi: 10.1016/j.vaccine.2020.11.004. [DOI] [PubMed] [Google Scholar]
- 8.Olsen S.J., Winn A.K., Budd A.P., et al. Changes in influenza and other respiratory virus activity during the COVID-19 pandemic-United States, 2020-2021. Am J Transplant. 2021;21(10):3481–3486. doi: 10.1111/ajt.16049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feng L., Zhang T., Wang Q., et al. Impact of COVID-19 outbreaks and interventions on influenza in China and the United States. Nat Commun. 2021;12(1):3249. doi: 10.1038/s41467-021-23440-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang W., Liu Y., Liu J., et al. Mortality and years of life lost of cardiovascular diseases in China, 2005-2020: empirical evidence from national mortality surveillance system. Int J Cardiol. 2021;340:105–112. doi: 10.1016/j.ijcard.2021.08.034. [DOI] [PubMed] [Google Scholar]
- 11.Weng L., Zeng X.Y., Yin P., et al. Sepsis-related mortality in China: a descriptive analysis. Intensive Care Med. 2018;44(7):1071–1080. doi: 10.1007/s00134-018-5203-z. [DOI] [PubMed] [Google Scholar]
- 12.Liu S., Wu X., Lopez A.D., et al. An integrated national mortality surveillance system for death registration and mortality surveillance, China. Bull World Health Organ. 2016;94(1):46–57. doi: 10.2471/BLT.15.153148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Bureau of Statistics National data. https://data.stats.gov.cn/english/easyquery.htm?cn=E0103
- 14.Department of Population and Employment & Statistics National Bureau of Statistics of China . China Statistics Press; Beijing: 2012. China population and employment Statistics yearbook 2011. [Google Scholar]
- 15.Hale T., Angrist N., Goldszmidt R., et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker) Nat Hum Behav. 2021;5(4):529–538. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- 16.Naghavi M., Makela S., Foreman K., O'Brien J., Pourmalek F., Lozano R. Algorithms for enhancing public health utility of national causes-of-death data. Popul Health Metr. 2010;8:9. doi: 10.1186/1478-7954-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.GBD 2017 Causes of Death Collaborators Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gao S., Yang W.S., Bray F., et al. Declining rates of hepatocellular carcinoma in urban Shanghai: incidence trends in 1976-2005. Eur J Epidemiol. 2012;27(1):39–46. doi: 10.1007/s10654-011-9636-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cleveland R.B., Cleveland W.S., Terpenning I. STL: a seasonal-trend decomposition procedure based on loess. J Off Stat. 1990;6(1):3. [Google Scholar]
- 20.Beard E., Marsden J., Brown J., et al. Understanding and using time series analyses in addiction research. Addiction. 2019;114(10):1866–1884. doi: 10.1111/add.14643. [DOI] [PubMed] [Google Scholar]
- 21.Penfold R.B., Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr. 2013;13(6 Suppl):S38–S44. doi: 10.1016/j.acap.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 22.Zhou M., He G., Liu Y., et al. The associations between ambient air pollution and adult respiratory mortality in 32 major Chinese cities, 2006-2010. Environ Res. 2015;137:278–286. doi: 10.1016/j.envres.2014.12.016. [DOI] [PubMed] [Google Scholar]
- 23.Wooldridge J.M. MIT press; Cambridge, MA: 2010. Econometric analysis of cross section and panel data. [Google Scholar]
- 24.Collaborators GBDLRI Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. 2018;18(11):1191–1210. doi: 10.1016/S1473-3099(18)30310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cao B., Huang Y., She D.Y., et al. Diagnosis and treatment of community-acquired pneumonia in adults: 2016 clinical practice guidelines by the Chinese Thoracic Society, Chinese Medical Association. Clin Respir J. 2018;12(4):1320–1360. doi: 10.1111/crj.12674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tan X., Liu X., Shao H. Healthy China 2030: a vision for health care. Value Health Reg Issues. 2017;12:112–114. doi: 10.1016/j.vhri.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 27.CDC FastStats–pneumonia. https://www.cdc.gov/nchs/fastats/pneumonia.htm [EB/OL]
- 28.CDC FastStats - influenza. https://www.cdc.gov/nchs/fastats/flu.htm [EB/OL]
- 29.Sanchez C.A., Rivera-Lozada O., Lozada-Urbano M., Best-Bandenay P. Herd immunity in older adults from a middle-income country: a time-series trend analysis of community-acquired pneumonia mortality 2003-2017. Health Sci Rep. 2023;6(5):e1224. doi: 10.1002/hsr2.1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rothberg M.B. Community-acquired pneumonia. Ann Intern Med. 2022;175(4):Itc49–itc64. doi: 10.7326/AITC202204190. [DOI] [PubMed] [Google Scholar]
- 31.Ruchiraset A., Tantrakarnapa K. Time series modeling of pneumonia admissions and its association with air pollution and climate variables in Chiang Mai Province, Thailand. Environ Sci Pollut Res Int. 2018;25(33):33277–33285. doi: 10.1007/s11356-018-3284-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bull G.M. The weather and deaths from pneumonia. Lancet. 1980;1(8183):1405–1408. doi: 10.1016/s0140-6736(80)92666-5. [DOI] [PubMed] [Google Scholar]
- 33.Dowell S.F., Whitney C.G., Wright C., Rose C.E., Jr., Schuchat A. Seasonal patterns of invasive pneumococcal disease. Emerg Infect Dis. 2003;9(5):573–579. doi: 10.3201/eid0905.020556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Uyeki T.M., Hui D.S., Zambon M., Wentworth D.E., Monto A.S. Influenza. Lancet. 2022;400(10353):693–706. doi: 10.1016/S0140-6736(22)00982-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dowell S.F. Seasonal variation in host susceptibility and cycles of certain infectious diseases. Emerg Infect Dis. 2001;7(3):369–374. doi: 10.3201/eid0703.010301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee T., Walley K.R., Boyd J.H., Cawcutt K.A., Kalil A., Russell J.A. Impact of the COVID-19 pandemic on non-COVID-19 community-acquired pneumonia: a retrospective cohort study. BMJ Open Respir Res. 2023;10(1) doi: 10.1136/bmjresp-2023-001810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang D., Zhang Y., Wang Q., et al. The effectiveness of influenza vaccination in preventing hospitalizations in elderly in Beijing, 2016-18. Vaccine. 2019;37(13):1853–1858. doi: 10.1016/j.vaccine.2019.02.013. [DOI] [PubMed] [Google Scholar]
- 38.Zhou S., Greene C.M., Song Y., et al. Review of the status and challenges associated with increasing influenza vaccination coverage among pregnant women in China. Hum Vaccin Immunother. 2020;16(3):602–611. doi: 10.1080/21645515.2019.1664230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dong J., Zhou Y., Pu J., Liu L. Status and challenges for vaccination against avian H9N2 influenza virus in China. Life. 2022;12(9) doi: 10.3390/life12091326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pannu J. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-international travel-related measures. Emerg Infect Dis. 2020;26(9):2298–2299. doi: 10.3201/eid2609.201990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fong M.W., Gao H., Wong J.Y., et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-social distancing measures. Emerg Infect Dis. 2020;26(5):976–984. doi: 10.3201/eid2605.190995. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.