Abstract
Introduction
Adhesive Capsulitis is a common condition of the shoulder with significant morbidity and protracted disease. It is usually characterized by sudden onset with progressive symptoms of pain and loss of function. This systematic review compares platelet rich plasma (PRP) intra-articular injections with corticosteroids (CS) injections and physiotherapy.
Material and methods
A literature search was performed using online databases (Pubmed, Cochrane, EMBASE, Medline and CINAHL) including all the studies performed on humans through April 2023. Prospective comparative studies were included in this review of patients with adhesive capsulitis assessing the use of PRP injections versus corticosteroid injections or physiotherapy. The standardized mean difference (SMD) with 95 % confidence interval in VAS/DASH/SPADI and ROM scores was calculated using a random effects model, comparing PRP to corticosteroids injections and physiotherapy across studies.
Results
A total of 11 studies and 971 patients, with a mean age of 52.1, were included in this analysis with 7 being randomised trials and four cohort studies. The control group was corticosteroid injections in 8 studies and physiotherapy in the other three studies. Overall PRP lead to a statistically significant improved outcome at 3 and 6 months follow up for all outcome parameters. The outcome measures at three months includes VAS 0.73 (0.31, 1.16) SMD, DASH 0.66 (0.36, 0.96) SMD, SPADI 1.50 (0.43, 2.57) SMD, ER 1.47 (0.27, 2.66) SMD and Abduction 1.10 (0.21, 1.98) SMD. Six months assessment similarly favoured PRP with VAS 3.17 (1.26, 5.08) SMD and DASH 2.10 (1.66, 2.55) SMD scores. Furthermore, a subgroup analysis demonstrated that PRP was favourable to corticosteroids as control with significant improvement in pain (VAS) at 3 months 0.65 (0.29, 1.00) and 6 months 3.17 (1.26, 5.08) SMD.
Conclusion
This review demonstrated that intra-articular PRP injections for adhesive capsulitis produces favourable outcomes when compared to corticosteroid injections and physiotherapy. PRP produces improved pain and functional scores as well as range of motion, which is statistically significant from 3 to 6 months post intervention. PRP seems to be a safe and effective alternative non-invasive treatment modality for patients with adhesive capsulitis.
Keywords: PRP, Platelet-rich plasma, Physiotherapy, Corticosteroids, Frozen shoulder, Adhesive capsulitis, Systematic review
1. Introduction
Adhesive Capsulitis (AC) is a common condition of the shoulder with significant morbidity and protracted disease. It is usually characterized by sudden onset with progressive symptoms of pain and loss of function (range of motion) both actively and passively.1 AC has an incidence of about 2–5%, with numbers as high as 38 % in patients with Diabetes Mellites and Thyroid disease. The peak incidence of AC is in patients aged between 40 and 60 with a higher ratio affecting women.2 AC is also known as frozen shoulder coined by Codman in 1934,3 this is a pathological condition which entails excessive scarring and adhesions of the glenohumeral joint (GHJ).4 The exact mechanism behind AC still remains unclear, although it is postulated to be as a consequence of minor insult to the GHJ which initiates an inflammatory response. This eventually leads to excessive accumulation of fibroblasts that releases type I and III collagen, which in turn results in a disparity between fibrosis and normal collagenous remodelling with clinical stiffness of the joint.5
The aims of treatment are to relieve the pain, restore range of motion and eventually regain pre-injury shoulder function.6 Intra-articular CS injection and physiotherapy still remains the most commonly used non-operative treatment options for AC.6 There are multiple studies available demonstrating its success in improving pain and function in patients with AC, as well as limiting the development of capsular fibrosis.7 But the risks of corticosteroid injections are also well known and described which includes hyperglycaemia, chondrolysis, risk of tendon ruptures, skin depigmentation and atrophy of subcutaneous tissue.8 Physiotherapy alone has also been shown to be an effective treatment modality to reduce pain and improve function in patients with AC.9 But despite these treatment options AC remains a difficult condition to treat and can often lead to protracted disability and pain. This necessitates the ongoing need and desire to search for new and possibly improved treatment modalities. Platelet rich plasma (PRP) has gained favour over the last two decades in treating patients with musculoskeletal conditions.
The aim of this study is to compare the efficacy of PRP intra-articular shoulder injections with commonly used non-surgical treatment modalities, such as corticosteroid injections and physiotherapy.
2. Materials and methods
The authors reported this review as per the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. The data search performed used five different online databases (Pubmed, Cochrane, EMBASE, Medline and CINAHL) looking for all published studies performed on humans through April 2023. All the electronic databases were searched with a detailed search strategy with two key concepts assessing the use of PRP in patients with AC (Table 1).
Table 1.
The Full search syntax used to identify studies.
| Database | Search terms | Hits |
|---|---|---|
| PubMed | (PRP OR “Platelet rich plasma” [tw] OR “Platelet-rich Plasma” [tw] OR “Platelet-Rich Plasma” [Mesh]) AND (“Frozen shoulder”[tw] OR “Adhesive Capsul*" [tw] OR “Periarthritis Shoulder” [tw]) | 32 |
| Medline | (PRP OR “Platelet rich plasma” OR “Platelet-rich Plasma” OR “Platelet-Rich Plasma" [Mesh]) AND (“Frozen shoulder” OR “Adhesive Capsul*" OR “Periarthritis Shoulder”) | 26 |
| CINHAL | (PRP OR “Platelet rich plasma” OR “Platelet-rich Plasma” OR “Platelet-Rich Plasma" [Mesh]) AND (“Frozen shoulder” OR “Adhesive Capsul*" OR “Periarthritis Shoulder”) | 15 |
| EMBASE | ((PRP or “Platelet rich plasma” or “Platelet-rich Plasma”) and (“Frozen shoulder” or “Adhesive Capsul*" or “Periarthritis Shoulder”)).mp. | 38 |
| Cochrane | #1 MeSH descriptor: [Platelet-Rich Plasma] explode all trees #2 (PRP) OR (“platelet-rich plasma”) #3 (“Frozen Shoulder”) OR (“adhesive capsul*") OR (“Periarthritis Shoulder”) (#1 OR #2) AND #3 |
29 |
2.1. Inclusion and exclusion criteria
Prospective comparative studies comparing the use of PRP injections in patients with AC: to either corticosteroid (CS) injections or physiotherapy were included in this study. With the following studies being excluded: (1) Retrospective studies, (2) non-comparative studies, (3) non-English studies, (4) in-vivo and in-vitro studies (5) PRP used in combination with other drugs as intervention, (6) control other than CS or physiotherapy, (7) studies including patients suffering from other shoulder conditions and (8) pre-clinical trials.
2.2. Quality assessment and data extraction
Two evaluators independently reviewed the articles for the risk for bias using the modified Jadad scale to assess the randomised trials. The Methodological Index for Non-Randomized Studies (MINORS) tool was used to assess the non-randomised trials. If any differences were identified then this was resolved with discussion between the two researchers and if needed this was escalated to the senior investigator. A Jadad score of 4–8 was considered high quality (0–3 low quality) and a MINORs score of <15 low, 15–19 moderate and 20–24 high.
Two reviewers assessed the initial results with a standardised eligibility criteria to select the appropriate studies for inclusion in the article. If there were any disagreements between the reviewers then this was resolved through open discussion and would then be either included or removed at this point, with the senior investigator being involved to resolve disagreements. The extracted data included is: study design, date of publication, country, mean age of patients involved, number of groups and patients, intervention in each group and the outcomes measured as well as the time interval this was measured.
2.3. Measurement of treatment outcome
The outcomes measured in the studies included were pain, function and range of motion (ROM). Pain was measured with the visual analogue scale (VAS). Function was measured with the disability of arm, shoulder and hand questionnaire (DASH); the shoulder pain and disability index (SPADI) and the university of California-Los Angeles shoulder scale (UCLA). The ROM measured was flexion, extension, abduction, external rotation (ER) and internal rotation (IR). The mean difference as well as the standard error (SE) was extracted from all the included studies with regards to outcome measurements VAS, DASH, SPADI and ROM at different time intervals. Multiple different outcomes was used across the different studies and the reviewers combined the relevant studies that used the same outcome measure. The follow up time periods that was used for analysis was 4 weeks, 6 weeks, 3 months and 6 months. For simplification of analysis 3 weeks and 4 weeks follow were combined.
2.4. Data synthesis
The statistical analyses were carried out and Forest plots were generated using the Comprehensive Meta-Analysis statistical software. The effect size of treatment on the disease was expressed as standardized mean difference (SMD), with 95 % Confidence Intervals (Cis). We considered a SMD value between 0.2 and 0.5 as small, with values between 0.5 and 0.8 medium, and the values of >0.8 were classified as large. A p value of P < 0.05 (2-tailed) was considered statistically significant. The random effect model is recommended for studies with smaller sample sizes.10,11 Therefore, the pooled effect sizes for the entire analysis were calculated using both fixed and random-effects models. Within-study and between-study variances were accounted by using ‘weighting by inverse variance’ method.12 Statistical heterogeneity was assessed with Q statistic and the I2 index in the analysis. Z-scores were also produced by the analysis. P < 0.05 was considered as heterogeneity between included studies.13
3. Results
3.1. Search results
The search strategy produced 134 studies, of which only 61 studies remained after duplicates were removed. Furthermore, the authors screened the titles and abstracts, and a further 47 studies were excluded in light of the study question and inclusion/exclusion criteria. 14 studies underwent full text assessment, with the final number of studies included for the analysis being 11 articles. These three studies were excluded as 2 studies compared PRP with saline injections and one full text article was not retrievable. This finally left 11 studies for qualitative and quantitative analysis. The following flow chart demonstrates the details and numbers of the search performed (Fig. 1).
Fig. 1.
Flow of the selection process.
3.2. Study characteristics
The extracted data from the 11 articles can be appreciated in Table 2. The studies included a total of 971 patients with a mean age of 52.1 excluding Yadav et al.,14 where this information was omitted. VAS scoring system was used to assess pain in 10 of 11 studies. With DASH (4 of 11) and SPADI (4 of 11) being the most frequently used tools to assess functional outcome, whereas UCLA (2 0f 11) and Constant (1 of 11) scoring systems were used infrequently. The ROM was assessed in 5 of 10 included studies. Most of the studies continued their follow up until three months (6 of 11), with four studies following up till 6 months and only Thu et al.15 stopped their outcome measurements as early as 6 weeks following intervention. PRP was compared to physiotherapy as control group in three of the included studies.15, 16, 17 The other 8 studies measured the efficacy of PRP injection against corticosteroid injections. Most of the studies was performed in India (7 of 11), with the rest being performed in Pakistan, Turkey, China and Korea.
Table 2.
Summary of study characteristics.
| Author | Study Design | Date | Country | Mean Age | Groups | N | Intervention | Outcome measurement | Follow-up | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Barman et al. | Comparative analysis | 2019 | India | 50.0 ± 6.31 | Group 1 | 28 | PRP 2 ml stat | VAS, ROM, SPADI | 3w, 6w, 12w |
| 50.26 ± 5.94 | Group 2 | 27 | Methylprednisilone 80 mg stat | |||||||
| 2 | Barman et al. | Prospective cohort study | 2021 | India | 48.8 ± 5.9 | Group 1 | 35 | PRP 4 ml stat | VAS, SPADI, ROM | 3w, 6w, 12w |
| 49.6 ± 5.7 | Group 2 | 35 | Physio 10 sessions in 2 weeks | |||||||
| 3 | Gupta et al. | PROBE | 2022 | India | 46.7 ± 7.13 | Group 1 | 30 | PRP 2 ml stat | VAS, DASH | 4w,12w,24w |
| 47.8 ± 9.56 | Group 2 | 30 | Triamcinilone 80 mg stat | |||||||
| 4 | Hafiz et al. | RCT | 2021 | Pakistan | 52.41 ± 2.67 | Group1 | 102 | PRP 2 ml stat | VAS, UCLA, ROM | 12w |
| 53.0 ± 3.74 | Group 2 | 100 | Methylprednisilone 80 mg stat | |||||||
| 5 | Karabas et al. | RCT | 2021 | Turkey | 57.3 ± 7.3 | Group 1 | 20 | PRP 3 ml 2* 2 weekly | VAS, SPADI, ROM | 2w, 6w, 12w |
| 56.8 ± 5.9 | Group 2 | 20 | Physio alone | |||||||
| 6 | Kothari et al. | Randomised comparative study | 2017 | India | 51.9 ± 10.1 | Group 1 | 62 | PRP 2 ml stat | VAS, QuickDASH, ROM | 3w, 6w, 12w |
| 52.7 ± 8.6 | Group 2 | 60 | Depo-Medrone 80 mg | |||||||
| 51.2 ± 11.7 | Group 3 | 58 | Ultrasonic therapy | |||||||
| 7 | Kumar et al. | Comparative analysis | 2019 | India | 50.60 ± 5.47 | Group 1 | 30 | PRP 2 ml stat | VAS, QuickDASH | 1 m, 2 m, 6 m |
| 52.93 ± 4.47 | Group 2 | 30 | Methylprednisilone 80 mg stat | |||||||
| 8 | Lin et al. | RCT | 2018 | China | 59.8 ± 4.3 | Group 1 | 30 | PRP 2 ml (3*2 weekly) | VAS,UCLA | 1w, 1 m, 3 m, 6 m |
| 58.2 ± 4.6 | Group 2 | 30 | Hydrocortizone 25 mg (3* 2 weekly) | |||||||
| 9 | Thu et al. | Randomised Trial | 2021 | Korea | 52.84 ± 6.92 | Group 1 | 32 | PRP 4 ml stat | VAS, DASH, ROM | 1w, 3w, 6w |
| 57.17 ± 6.93 | Group 2 | 32 | Physio 3 * weekly | |||||||
| 10 | Upadhyaya et al. | Randomised comparative analysis | 2020 | India | 47.6 ± 3.2 | Group 1 | 60 | PRP 2 ml stat | SPADI | 1 m, 3 m, 6 m |
| 46.4 ± 4.3 | Group 2 | 60 | Methylprednisilone 80 mg stat | |||||||
| 11 | Yadav et al. | Prospective cohort study | 2021 | India | Not mentioned | Group 1 | 30 | PRP 2 ml stat | VAS, Constant | 1w,1 m,3 m |
| Not mentioned | Group 2 | 30 | Methylprednisilone 80 mg stat |
RCT, randomised controlled trial; PROBE, Prospective randomized open blinded end-point; PRP, platelet rich plasma; VAS, visual analogue scale; DASH, disability of arm, shoulder and hand questionnaire; SPADI, the shoulder pain and disability index; UCLA, the university of California-Los Angeles shoulder scale.
3.3. Risk of bias
All 7 randomised trials included in this analysis scored 4 or higher using the modified Jadad scoring system. This indicates that there is a low risk of bias in all these studies with the lowest scoring article not describing the withdrawals/dropouts, nor method used to assess adverse effects.18 None of the included studies was double blinded (Table 3). Assessing the non-randomised trials both Barman et al. (2019) and Barman et al. (2021) scored high with a low risk of bias. Whereas Kumar et al.19 received a moderate score and Yadav et al.14 scored low with a high risk of bias which can be appreciated in Table 4.
Table 3.
Randomised trials assessed with Modified Jadad score.
| Modified Jadad score: | Kothari et al. | Upadhyaya et al. | Hafiz et al. | Karabas et al. | Thu et al. | Lin et al. | Gupta et al. | |
|---|---|---|---|---|---|---|---|---|
| 1 | Was the study described as Randomised? (0,1) | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 2 | Was the method of randomization appropriate? (−1 if innapropriate) | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 3 | Was the study described as blinded? | 1 | 1 | 1 | 1 | 1 | 0 | 1 |
| 4 | Was the method of blinding appropriate (double blind)? (−1 if innapropriate) | −1 | −1 | −1 | −1 | −1 | 0 | −1 |
| 5 | Was there a description of withdrawals and dropouts? | 1 | 1 | 0 | 1 | 1 | 1 | 1 |
| 6 | Was there a clear description of the inclusion/exclusion criteria? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 7 | Was the method used to assess adverse effects described? | 0 | 1 | 0 | 0 | 0 | 1 | 1 |
| 8 | Was the method of statistical analysis described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Total score (4–8 high, 0–3 low) | 5 | 6 | 4 | 5 | 5 | 6 | 6 |
Table 4.
Non- Randomised trials assessed according to MINORS criteria.
| MINORS criteria | Barman et al., 2019. | Kumar et al. | Barman et al., 2021 | Yadav et al. | |
|---|---|---|---|---|---|
| 1 | A clearly stated aim (0,1 or 2) | 2 | 2 | 2 | 2 |
| 2 | Inclusion of consecutive patients | 2 | 1 | 2 | 2 |
| 3 | Prospective collection of data | 2 | 2 | 2 | 2 |
| 4 | Endpoints appropriate to the aim of the study | 2 | 2 | 2 | 2 |
| 5 | Unbiased (blinded) assessment of the study endpoint | 2 | 0 | 2 | 0 |
| 6 | Follow-up period appropriate to the aim of the study | 2 | 2 | 2 | 2 |
| 7 | Loss to follow up less than 5 %: | 1 | 0 | 1 | 0 |
| 8 | Prospective calculation of the study size | 2 | 0 | 2 | 0 |
| 9 | An adequate control group | 2 | 2 | 2 | 2 |
| 10 | Contemporary groups: | 2 | 2 | 2 | 2 |
| 11 | Baseline equivalence of groups | 1 | 2 | 2 | 0 |
| 12 | Adequate statistical analyses | 2 | 0 | 2 | 0 |
| Total (20–24 high, 15–19 mod, <15 low) | 22 | 15 | 23 | 14 |
MINORS, methodological index for non-randomized studies.
3.4. Outcome of the meta-analysis
Adhesive capsulitis treated with PRP injections led to a statistically significant improved pain, function and ROM when compared to the control group (physiotherapy and corticosteroids combined). The standardized mean difference of VAS at 3 months is 0.73 with a 95 % CI of 0.31–1.16. With significant improvement in pain lasting till 6 months: VAS 3.17 (1.26, 5.08) SMD (Fig. 2).
Fig. 2.
VAS meta-analysis PRP versus Steroid/Physiotherapy.
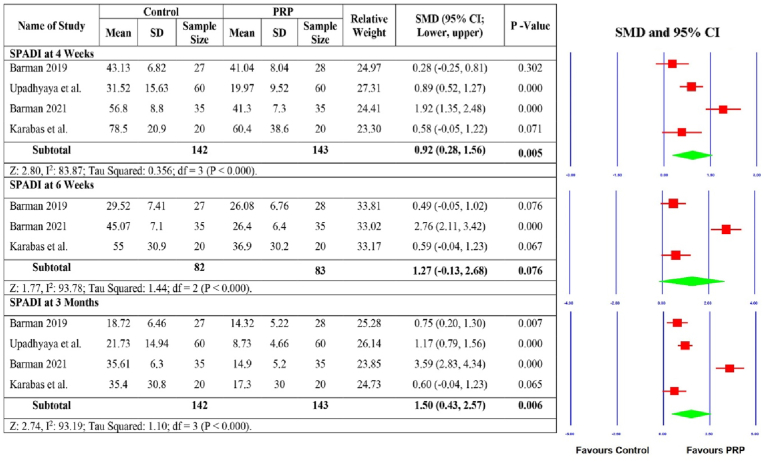
The functional improvement was statistically significant with the meta-analysis of the DASH and the SPADI scoring systems demonstrating improved outcomes. DASH included four studies with significant improved outcomes at 6 weeks 0.31 (0.02, 0.60), three months 0.66 (0.36, 0.96) SMD and 6 months 2.10 (1.66, 2.55) (Fig. 3). SPADI scoring system was also used in four studies with improved outcomes at all time points 4 weeks 0.92 (0.28, 1.56) SMD, 3 months 1.50 (0.43, 2.57) SMD with statistically non-significant improvement at 6 weeks 1.27 (−0.13, 2.68) SMD (Fig. 4). Improved ROM was also demonstrated in the PRP group at three months follow up most significant with regards to abduction 1.10 (0.21, 1.98) SMD and external rotation 1.47 (0.27, 2.66) SMD (Fig. 5, Fig. 6).
Fig. 3.
DASH PRP versus control.
Fig. 4.
SPADI PRP versus control.
Fig. 5.
Abduction PRP vs Control.
Fig. 6.
PRP vs Control External Rotation.
Furthermore, a subgroup analysis was performed on the VAS score only comparing corticosteroids as control with PRP. This analysis included 7 studies and demonstrated that PRP lead to statistically significant improved pain scores at 3 months 0.65 (0.29, 1.00) SMD and 6 months 3.17 (1.26, 5.08) SMD (Fig. 7).
Fig. 7.
VAS PRP versus Steroid alone meta-analysis.
4. Discussion
This study is the first systematic review and meta-analysis comparing PRP with corticosteroid and physiotherapy according to the authors knowledge. This meta-analysis demonstrated that PRP injections lead to improved outcomes in patients with adhesive capsulitis in comparison to the control group with regards to pain, function and ROM. These findings were echoed by Harna et al.20 who performed a systematic review with descriptive analysis of 11 studies looking at the use of PRP in AC. As well as, yu et al.21 who performed a meta-analysis that included four studies assessing the efficacy of PRP with other modalities of conservative management. Both of these studies demonstrated better results in the PRP group in reducing pain and improving ROM.
As mentioned in the introduction AC is a protracted and complicated condition to treat with multiple treatment options which has its own benefits and risks. The goal in treating AC is to restore function and reduce pain. It is generally necessary to follow a multimodal approach when treating AC. The treatment options include oral analgesics, physiotherapy, intra-articular injections, hydro-dissection, manipulation under anaesthesia and surgery (synovectomy and capsular release). All these treatment modalities are aimed at improving the symptoms of the patient and not treating the patho-anatomy of the disease.20 In all the included studies comparing PRP and corticosteroids injections, they would also provide all the patients with the same physical therapy exercises after the injections. Three studies compared PRP injections in isolation with physiotherapy alone.
Of the 8 studies included comparing PRP with corticosteroids intra-articular injections five were randomised trials and three prospective comparative cohort studies. The authors were able to perform a subgroup meta-analysis assessing only the use of PRP with corticosteroids which demonstrated statistically significant improvement in pain (VAS score) in the PRP group at 3 and 6 months; 0.65 (0.29, 1.00) SMD and 3.17 (1.26, 5.08) SMD respectively (Fig. 7).
PRP was compared with triamcinolone injections by Gupta et al.22 with 60 patients being randomised into two groups and followed up for six months. The PRP group demonstrated significant improvement of pain at three months and 6 months, as well as function with an improved DASH score at three and 6 months. Statistical significance was demonstrated at 6 months for both pain and function (p = 0001 and p = 0.0001 respectively).
Shahzad et al.18 performed a randomised controlled trial on 202 patients with group A receiving 2 ml of PRP and group B receiving 2 ml of methylprednisolone given via the anterior approach. The outcomes assessed included ROM, UCLA and the VAS score. The study demonstrated statistically significant improvement in all the assessed outcomes for the PRP group at the three months mark.
In a randomised comparative study performed by Kothari et al.23 195 patients were randomised into three groups receiving either 2 ml of PRP, 2 ml of methylprednisolone or ultrasonic therapy. With PRP treatment resulting in statistically significant improvements over both corticosteroids and ultrasound therapy at three months with regards to VAS, DASH and ROM scores. However, at 6 weeks the improvement noted for all three outcomes was non-significant when compared to corticosteroids injections.
These findings were echoed in a prospective randomised assessor-blind comparative analysis performed by Chansoria et al.24 comparing PRP and corticosteroids. A total of 120 patients where randomised with one group receiving PRP and the other receiving methylprednisolone. This study was one of the few with a six month follow up, with results demonstrating that PRP injections led to constant improvement in both pain and function up to six months. Whereas the corticosteroid injections were effective at the initial stage but scores worsened at 6 months for both VAS and SPADI scoring systems. The PRP group demonstrated statistically significant improvement in VAS and SPADI scores at 6 weeks, three months and 6 months when compared to corticosteroid injections.
In another randomised controlled trial, with a 6 month follow up, performed by Lin25 statistically significant improved outcomes for both VAS and UCLA scores were demonstrated. In this study 60 patients were randomised into two groups with one group receiving 4 ml of PRP injections and the other receiving 25 mg Hydrocortisone injections. The participants received three injections in total two weekly in both groups. This study concluded that PRP is beneficial to reduce pain in frozen shoulder and to improve function with good tolerance, showing a promising alternative treatment strategy with low risk of adverse effects.
In another study performed by Barman et al.,26 a prospective cohort study was performed on 60 patients with 30 patients receiving 80 mg methylprednisolone and the other half receiving 4 ml PRP intra-articular glenohumeral injections under ultrasound guidance. Outcomes which included VAS, ROM and SPADI were measured up to 3 months. The study didn't report any major complications. They concluded that at 3 months follow up, PRP injections are more effective than corticosteroid injections, with regards to improvements in pain and function.
In a comparative analysis performed by Kumar et al.19 60 patients were included with PRP and Methylprednisolone being injected, with outcomes measured (DASH and VAS) up to 6 months post intervention. The outcome was excellent among 10 %, good among 66.67 %, fair amongst 13.33 % and poor amongst 10 %. Both PRP and corticosteroids produced significant improvement in both the pain and function of patients suffering from AC. But there was no statistically significant difference between the two interventions, which led to the authors concluding that both PRP and corticosteroids are equally effective in treating AC.
Furthermore, a study performed by Yadav et al.14 produced similar results demonstrating that both steroids and PRP produced excellent improvement in symptoms when treating frozen shoulder. This study included 60 patients who were divided randomly and equally into two groups: with one group receiving a single injection of PRP and the other methylprednisolone. This injection resulted in statistically significant improvement in VAS and Constant score for both PRP and corticosteroids groups. The PRP subgroup producing excellent outcomes in 23.33 % of patients, good in 43.33 % and poor in 33.33 %, with the corticosteroid subgroup producing similar results.
Three of the studies analysed compared intra-articular PRP injections with physiotherapy. Karabas et al.17 included 40 patients with idiopathic adhesive capsulitis who where randomly assigned to the PRP group or control group. The PRP group received 2 injections biweekly, whereas the control group only received stretching and Codman exercises as a home-based program. Both groups produced significant improvement in VAS, SPADI and ROM scores for all the time points compared to baseline. The only statistically significant difference identified was ROM at three months follow up. The authors concluded that PRP in addition to an exercise program can improve a patient's mobility, but not pain and function.
An RCT published by Thu et al.15 included 64 patients, comparing physiotherapy with PRP injections, produced similar results with significant improvement in VAS, DASH and ROM for both groups at all time points. The results didn't demonstrate any significant difference in the measured outcomes for both groups. They advised that PRP is a useful option in treating AC, particularly in patients with poor compliance to physiotherapy and contra-indications to corticosteroid injections.
In another study Barman et al.16 performed a prospective cohort study comparing PRP injections with physiotherapy in 70 diabetic patients with AC. 35 patients received a stat dose of 4 ml PRP and the other 35 patients were given institution-based physiotherapy which included ten 30-min sessions of planned physiotherapy over a 2-week period. These patients were followed up for three months. The study demonstrated greater improvement in pain (p < 0.001), ROM and SPADI scores (p < 0.001) compared to the patients receiving physiotherapy at the three month follow up. The authors concluded that PRP is well tolerated and produces significantly improved shoulder pain and function in patient with diabetes suffering from AC.
What is evident from reviewing the studies available is that there is still no standardised protocol to investigate the efficacy and importance of PRP. The number of PRP injections varies between studies from a stat dose up to three doses fortnightly. The current data available is controversial with some studies suggesting that multiple injections lead to improved outcomes,27 with other finding no difference28 and some lead to no difference in pain but improved ROM.29 Furthermore, an important risk that has been demonstrated is that repeated injections could lead to more frequent local side effects.30 Overall, none of the studies included in this review demonstrated any significant adverse effects with PRP injections and this has been well established in published research.31, 32, 33 Another point of controversy is whether ultrasound guided injections might be more effective than using anatomical landmarks. A recent systematic review that included 12 randomised controlled trials with 891 patients found that ultrasound guided injections lead to superior pain relieve and functional improvement, when compared to anatomical landmark guided injections, in patients with subacromial impingement syndrome.34
This review is unique as this is the only systematic review and meta-analysis comparing the use of PRP with corticosteroids and physiotherapy in patients suffering from AC. The strengths of this article is that it only included prospective comparative studies and it used a systematic approach to analysing the studies with validated quality assessment tools. The use of standard and validated outcome measures such as (VAS, DASH, SPADI and ROM) across most of the included studies assisted in direct comparison.
The study however had some limitations with the heterogeneity of the included studies being prime among them: many different outcome measures, different length of follow up with different timeframes for repeat assessments, varying sample sizes with some studies including fairly small numbers, two different interventions acting as control and difference in study designs. This effected the number of studies included in quantitative analysis and made it difficult to perform any sensible subgroup analysis. There wasn't a standardised protocol used in the preparation and administration of PRP among the reviewed articles. Further large multicentre randomised controlled trials are required to provide clearer results with regards to the efficacy of PRP in patients with adhesive capsulitis.
5. Conclusion
This systematic review and meta-analysis demonstrated that intra-articular PRP injections for adhesive capsulitis produces favourable outcomes when compared to corticosteroid injections and physiotherapy. PRP produces improved pain and functional scores as well as range of motion, which is statistically significant from 3 to 6 months post intervention. PRP seems to be a safe and effective alternative non-invasive treatment modality for patients with adhesive capsulitis. Further well-constructed large multicentre randomised controlled trials with a standardised protocol and outcome measures are essential to clarify the efficacy of PRP in adhesive capsulitis.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
No ethical approval required.
Informed consent
Not required.
CRediT authorship contribution statement
Jacques Pretorius: Study design, writing manuscript, Writing – review & editing, Data synthesis. Rayyan Mirdad: Data extraction, Bias assessment, Formal analysis. Nouman Nemat: Investigation, Literature review, Data extraction. Bishoy Zaher Ghobrial: Investigation, Literature review, Bias assessment. Colin Murphy: Supervision.
Declaration of competing interest
No conflicts of interest to declare.
Acknowledgement
I would like to thank and acknowledge that this manuscript was produced with the guidance of my supervisor and the Surgical Masters Programme (ChM) in Trauma and Orthopaedics provided by the University of Edinburgh.
Contributor Information
Jacques Pretorius, Email: Jacquespretorius2015@gmail.com.
Rayyan Mirdad, Email: Rayyan.mirdad@gmail.com.
Nouman Nemat, Email: noumannemat@gmail.com.
Bishoy Zaher Ghobrial, Email: bishoyzaher@gmail.com.
Colin Murphy, Email: cmurphy@rcsi.ie.
References
- 1.Kelley M.J., Mcclure P.W., Leggin B.G. Frozen shoulder: evidence and a proposed model guiding rehabilitation. J Orthop Sports Phys Ther. 2009;39:135–148. doi: 10.2519/jospt.2009.2916. [DOI] [PubMed] [Google Scholar]
- 2.Zappia M., di Pietto F., Aliprandi A., et al. Multi-modal imaging of adhesive capsulitis of the shoulder. Insights Imaging. 2016;7:365–371. doi: 10.1007/s13244-016-0491-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uppal H.S. Frozen shoulder: a systematic review of therapeutic options. World J Orthoped. 2015;6:263. doi: 10.5312/wjo.v6.i2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bouaicha S., Wieser K., Kriechling P., Scholz-Odermatt S.M. A large-scale assessment of the healthcare burden of adhesive capsulitis of the shoulder joint. Swiss Med Wkly. 2020 doi: 10.4414/smw.2020.20188. [DOI] [PubMed] [Google Scholar]
- 5.Akbar M., McLean M., Garcia-Melchor E., et al. Fibroblast activation and inflammation in frozen shoulder. PLoS One. 2019;14 doi: 10.1371/journal.pone.0215301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koh K. Corticosteroid injection for adhesive capsulitis in primary care: a systematic review of randomised clinical trials. Singap Med J. 2016;57:646–657. doi: 10.11622/smedj.2016146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang K.-V., Wu W.-T., Han D.-S., Özçakar L. Static and dynamic shoulder imaging to predict initial effectiveness and recurrence after ultrasound-guided subacromial corticosteroid injections. Arch Phys Med Rehabil. 2017;98:1984–1994. doi: 10.1016/j.apmr.2017.01.022. [DOI] [PubMed] [Google Scholar]
- 8.Waterbrook A.L., Balcik B.J., Goshinska A.J. Blood glucose levels after local musculoskeletal steroid injections in patients with diabetes mellitus: a clinical review. Sport Health: A Multidisciplin. Appr. 2017;9:372–374. doi: 10.1177/1941738117702585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Page P., Labbe A. Adhesive capsulitis: use the evidence to integrate your interventions. N Am J Sports Phys Ther. 2010;5:266–273. [PMC free article] [PubMed] [Google Scholar]
- 10.Egger M., Smith G.D., Phillips A.N. Meta-analysis: principles and procedures. BMJ. 1997;315:1533–1537. doi: 10.1136/bmj.315.7121.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borenstein M., Hedges L.V., Higgins J.P.T., Rothstein H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 12.Hedges L.V., Vevea J.L. Fixed- and random-effects models in meta-analysis. Psychol Methods. 1998;3:486–504. doi: 10.1037/1082-989X.3.4.486. [DOI] [Google Scholar]
- 13.Higgins J.P.T. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yadav R., Pandit R.S., Kumar N. Comparative assessment of the significance of platelet rich plasma (PRP) and corticosteroid injection in management of adhesive capsulitis of shoulder. Int J Pharmaceut Chem Res. 2021;13:513–517. [Google Scholar]
- 15.Thu A.C., Kwak S.G., Shein W.N., et al. Comparison of ultrasound-guided platelet-rich plasma injection and conventional physical therapy for management of adhesive capsulitis: a randomized trial. J Int Med Res. 2020;48 doi: 10.1177/0300060520976032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barman A., Mukherjee S., Sinha M.K., et al. The benefit of platelet-rich plasma injection over institution-based physical therapy program in adhesive capsulitis patients with diabetes mellitus: prospective observational cohort study. Clin Shoulder Elb. 2021;24:215–223. doi: 10.5397/cise.2021.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karabaş Ç., Çalış H.T., Topaloğlu U.S., Karakükçü Ç. Effects of platelet-rich plasma injection on pain, range of motion, and disability in adhesive capsulitis: a prospective, randomized-controlled study. Turk J Phys Med Rehabil. 2021;67:462–472. doi: 10.5606/TFTRD.2021.6690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shahzad H.F., Taqi M., Gillani S.F.U.H.S., et al. Comparison of functional outcome between intra-articular injection of corticosteroid versus platelet-rich plasma in frozen shoulder: a randomized controlled trial. Cureus. 2021 doi: 10.7759/cureus.20560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumar S., Singh P. Comparative analysis on efficacy of injection methyl prednisolone vs autologous PRP in adhesive capsulitis/peri arthritis/frozen shoulder. 2019. Original Research Article 278:278–81. [DOI]
- 20.Harna B., Gupta V., Arya S., et al. Current role of intra-articular injections of platelet-rich plasma in adhesive capsulitis of shoulder: a systematic review. Bioengineering. 2023;10 doi: 10.3390/bioengineering10010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu S., Hu R., Feng H., Huang D. Efficacy of platelet-rich plasma injection in the treatment of frozen shoulder: a systematic review and meta-analysis. J Back Musculoskelet Rehabil. 2022:1–14. doi: 10.3233/bmr-220034. [DOI] [PubMed] [Google Scholar]
- 22.Gupta G.K., Shekhar S., Haque Z.U., et al. Comparison of the efficacy of platelet-rich plasma (PRP) and local corticosteroid injection in periarthritis shoulder: a prospective, randomized, open, blinded end-point (PROBE) study. Cureus. 2022 doi: 10.7759/cureus.29253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kothari S.Y., Srikumar V., Singh N. Comparative efficacy of platelet rich plasma injection, corticosteroid injection and ultrasonic therapy in the treatment of periarthritis shoulder. J Clin Diagn Res. 2017;11:RC15–RC18. doi: 10.7860/JCDR/2017/17060.9895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chansoria M., Upadhyay S., Jorule K., Varma H.S. Ongoing efficacy of platelet-rich plasma vs corticosteroid injection in patients with adhesive capsulitis: a prospective randomized assessor-blind comparative analysis. J. Recent Advan. Pain. 2020;6:10–16. doi: 10.5005/jp-journals-10046-0160. [DOI] [Google Scholar]
- 25.Lin J. Platelet-rich plasma injection in the treatment of frozen shoulder: a randomized controlled trial with 6-month follow-up. Int J Clin Pharmacol Therapeut. 2018;56:366–371. doi: 10.5414/CP203262. [DOI] [PubMed] [Google Scholar]
- 26.Barman A., Mukherjee S., Sahoo J., et al. Single intra-articular platelet-rich plasma versus corticosteroid injections in the treatment of adhesive capsulitis of the shoulder: a cohort study. Am J Phys Med Rehabil. 2019;98:549–557. doi: 10.1097/PHM.0000000000001144. [DOI] [PubMed] [Google Scholar]
- 27.McLarnon M., Heron N. Intra-articular platelet-rich plasma injections versus intra-articular corticosteroid injections for symptomatic management of knee osteoarthritis: systematic review and meta-analysis. BMC Muscoskel Disord. 2021;22 doi: 10.1186/s12891-021-04308-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Örsçelik A., Yildiz Y. Comparison of single and triple platelet rich plasma injections in the treatment of patellofemoral pain syndrome. Turkiye Klinikleri J Med Sci. 2015;35:78–87. doi: 10.5336/medsci.2014-42651. [DOI] [Google Scholar]
- 29.Vilchez-Cavazos F., Millán-Alanís J.M., Blázquez-Saldaña J., et al. Comparison of the clinical effectiveness of single versus multiple injections of platelet-rich plasma in the treatment of knee osteoarthritis: a systematic review and meta-analysis. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119887116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Campbell K.A., Saltzman B.M., Mascarenhas R., et al. Does intra-articular platelet-rich plasma injection provide clinically superior outcomes compared with other therapies in the treatment of knee osteoarthritis? A systematic review of overlapping meta-analyses. Arthrosc J Arthrosc Relat Surg. 2015;31:2213–2221. doi: 10.1016/j.arthro.2015.03.041. [DOI] [PubMed] [Google Scholar]
- 31.Rayegani S.M., Raeissadat S.A., Taheri M.S., et al. Does intra articular platelet rich plasma injection improve function, pain and quality of life in patients with osteoarthritis of the knee? A randomized clinical trial. Orthop Rev. 2014;6:5405. doi: 10.4081/or.2014.5405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jang S.-J., Kim J.-D., Cha S.-S. Platelet-rich plasma (PRP) injections as an effective treatment for early osteoarthritis. Eur J Orthop Surg Traumatol. 2013;23:573–580. doi: 10.1007/s00590-012-1037-5. [DOI] [PubMed] [Google Scholar]
- 33.Shen L., Yuan T., Chen S., et al. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2017;12:16. doi: 10.1186/s13018-017-0521-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Deng X., Zhu S., Li D., et al. Effectiveness of ultrasound-guided versus anatomic landmark–guided corticosteroid injection on pain, physical function, and safety in patients with subacromial impingement syndrome. Am J Phys Med Rehabil. 2022;101:1087–1098. doi: 10.1097/PHM.0000000000001940. [DOI] [PMC free article] [PubMed] [Google Scholar]