Abstract
PURPOSE
To compare the safety and efficacy of sclerotherapy and lymphatic embolization (LE) in the treatment of symptomatic iatrogenic lymphoceles following the placement of a percutaneous drainage catheter.
METHODS
This is a retrospective study of 46 patients who underwent sclerotherapy (17 patients) or LE (29 patients) for the management of symptomatic iatrogenic lymphoceles following percutaneous drain placement between January 2017 and December 2021. The demographic characteristics, time between surgery and lymphatic intervention, clinical presentation, number of procedures, drain output pre- and post-intervention, time from intervention to drain removal, and adverse events were collected and compared for both groups. The clinical success rate, defined as the successful removal of the drain after one procedure, was calculated. Adverse events were reported according to the Society of Interventional Radiology classification. A statistical analysis was conducted using SPSS, and the P value for statistical significance was set at 0.05. The Mann–Whitney U test was used to compare differences in the scale variables, and Fisher’s exact test was used to compare the categorical and ordinal variables between both groups.
RESULTS
A total of 46 patients with 49 lymphoceles met the inclusion criteria of the study. Of these patients, 17 patients (19 lymphoceles) underwent sclerotherapy, and 29 patients (30 lymphoceles) underwent LE as their initial procedures. The clinical success after one procedure was significantly higher (83% vs. 47%, P = 0.011), and the median time between the first intervention and drain removal was significantly shorter in the LE group (median duration of 6 vs. 13 days, P = 0.018) compared with the sclerotherapy group. No statistically significant difference in adverse events was noted between both groups (0.26 vs. 0.10, P = 0.11).
CONCLUSION
This study found that LE had a higher clinical success rate after the first procedure and a shorter time to drain removal compared with sclerotherapy. There was no difference in the rate of adverse events between both groups. Although LE is a safe and promising technique, a prospective study is needed to further compare the efficacy of both treatment modalities.
Keywords: Embolization, lymphangiography, lymphatic, lymphocele, sclerotherapy
Main points
• Symptomatic lymphoceles are a relatively common occurrence after lymph node dissection in oncological surgery.
• Percutaneous drainage is the treatment of choice, but it may require prolonged drain dwell times, which affect patients’ quality of life.
• Sclerotherapy is the primary treatment to decrease the drain dwell time, but it often requires multiple procedures.
• Intranodal lymphangiography and lymphatic embolization (LE) are newer treatment options.
• This retrospective study showed that LE was associated with a significantly shorter drainage drain dwell time than sclerotherapy and required fewer procedures.
Lymph node dissection is an integral part of oncological surgery. Lymphatic injury and lymphocele development is a known complication of lymph node dissection. The reported incidence of lymphocele varies in the literature, with incidences of symptomatic lymphoceles ranging between 2.5% and 34.5%.1,2 Symptoms are often due to infection within the lymphocele, or pressure on surrounding structures, with urinary frequency, constipation, hydronephrosis, pain and lower extremity edema all reported in the literature.3
Percutaneous catheter drainage is the mainstay of treatment for symptomatic lymphoceles. However, further intervention is often required to decrease the drain output, and subsequently, the drain dwell time.4,5 Sclerotherapy induces local inflammation and fibrosis of the wall of the lymphocele with subsequent obliteration of the lymphatic leak, and safety and efficacy has been reported.6 Although this treatment is sometimes successful after one session, the literature reports the average number of required sclerotherapy procedures to be between one and four procedures, with patients sometimes requiring up to 14 procedures.7 Lymphangiography followed by lymphatic embolization (LE) is another approach to identify and occlude the source of lymphatic leak. The intranodal technique has made lymphangiography much less cumbersome and technically demanding than in the past. Once the leak has been identified, LE using an n-butyl cyanoacrylate (n-BCA) and lipiodol mixture is conducted under fluoroscopic guidance, and safety and efficacy has also been reported.8
Studies comparing these two treatment modalities are limited.3,9 The aim of this single center retrospective study is to compare the efficacy and safety of sclerotherapy and LE in the treatment of pelvic and abdominal iatrogenic lymphoceles following oncologic surgery.
Methods
Patient population
This retrospective study was approved by the Memorial Sloan Kettering Cancer Center Institutional Review Board under protocol number 16-402, and the need for informed consent was waived. Medical records were reviewed to identify patients with abdominal or pelvic iatrogenic symptomatic lymphoceles following oncological surgery. Patients treated with percutaneous drainage followed by sclerotherapy or LE were included. Patients were excluded if no follow-up data was available to evaluate the clinical outcome or if the percutaneous drain was removed before clinical resolution was confirmed through decreased drain output.
A total of 55 patients with 59 lymphoceles were identified (Table 1). The decision to treat with sclerotherapy or LE was based on the operator’s discretion. One patient had lymphangiography followed by sclerotherapy in the same session when no leak was identified and was subsequently excluded from further analysis. Eight patients had the drain removed on the same day as the sclerotherapy procedure, and there were no available data to evaluate the success of the treatment later. Therefore, they were excluded, as this clinical approach was later abandoned. The remaining 46 patients were divided into 17 patients (19 lymphoceles) who underwent sclerotherapy and 29 patients (30 lymphoceles) who underwent intra-nodal lymphangiography (INL) and LE as their initial procedures (Figure 1). Twenty of the 29 patients who underwent LE in this study were also involved in a prior study that was focused on proving the safety and efficacy of LE.8 They have been included in this study as part of the LE cohort, as this study focuses on comparing the outcomes of LE and sclerotherapy.
Table 1. Baseline characteristics of the study population.
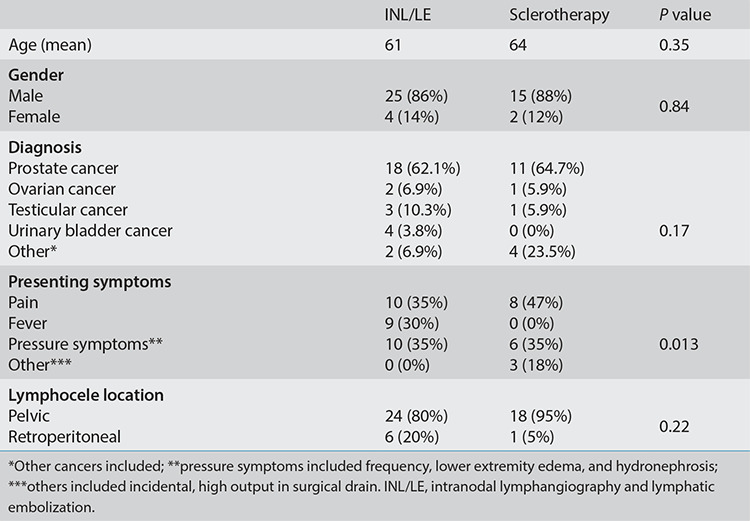
Figure 1.
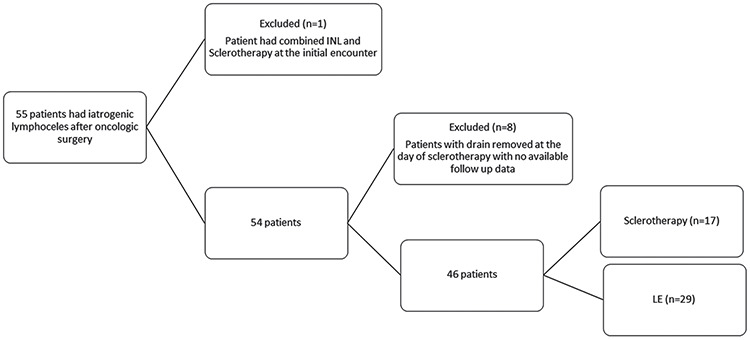
Flowchart for study inclusion. INL, intra-nodal lymphangiography; LE, lymphatic embolization.
The most common cancer diagnosis was prostate cancer (63%). No statistically significant difference was noted in the baseline characteristics except in the presenting symptoms, as no patients in the sclerotherapy group presented with fever.
Sclerotherapy technique
The procedure was performed under moderate sedation. Under aseptic conditions, all patients had a percutaneous drain placed under imaging guidance [computed tomography (CT) or ultrasound]. The fluid collection was drained fully, and the drained volume was recorded. A similar volume of iodinated contrast was then injected into the lymphocele cavity under fluoroscopic imaging or CT to ensure the absence of communication with adjacent structures (Figure 2). The contrast was then aspirated, and the sclerosant material was injected through the drain and left to dwell in the collection for 30–120 minutes according to the operator’s preference. Absolute ethanol and povidone iodine volumes were determined based on the amount of contrast that was required to fill the cavity without having pericatheter leakage or intravasation. In cases of sodium tetradecyl sulphate (STS) 3% (Sotradecol, AngioDynamics, Inc., Queensbury, NY, USA), it was mixed with air in a 1:3 ratio to form foam, which was then instilled through the drain. It was then aspirated, and the drain was left in place. The drain output was monitored over the following days. The drain was removed once the output dropped below 20 cc/24 hrs over 3 consecutive days. If the drain output remained consistently elevated for several days following the procedure, the sclerotherapy procedure was repeated based on the interventional radiologist’s assessment. The sclerosant materials that were used included absolute ethanol, STS 3%, doxycycline, and/or povidone iodine (Betadine, Purdue-Frederick, Norwalk, Conn). The choice of the sclerosant and dwell time was based on the operator’s preference.
Figure 2.
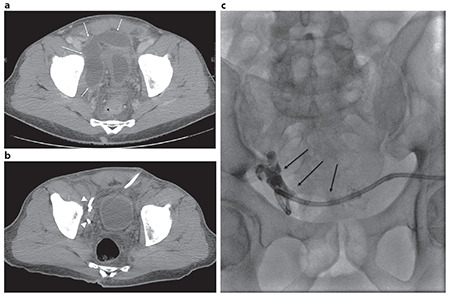
A 57-year-old male with a history of robotic prostatectomy and pelvic lymphadenectomy presenting with pelvic pain. (a) Computed tomography of the abdomen and pelvis showing right pelvic fluid collection (white arrows). (b) Collection completely drained with a 10.5 Fr drainage catheter (white arrow heads), but a consistently high output of 195 cc/day was noted for the following 2 weeks. (c) The residual cavity filled with 12 cc of contrast with no evidence of communication with the surrounding structures (black arrows). A total of 12 cc of 3% sodium tetradecyl sulphate (STS) mixture (2 mL STS, 8 mL iodinated water-soluble contrast, 2 mL air) was subsequently injected (not shown) and allowed to dwell for 2 hours. Output subsequently dropped to 5 cc/day, and the drain was removed after 7 days.
Lymphangiography and lymphatic embolization technique
The procedure was performed under moderate sedation by one of six interventional radiologists with 2–26 years of experience. Under ultrasound imaging guidance, a 25-gauge needle was placed into an inguinal lymph node at the side of the pelvic lymphocele with the tip located at the corticomedullary junction (Figure 3). Bilateral lymph node access was obtained in cases of bilateral pelvic lymphoceles or retroperitoneal lymphoceles. A total of 6 cc of lipiodol (Guerbet, Villepinte, France) was injected by hand under intermittent fluoroscopy. Once the contrast extravasation was noted into the lymphocele, the point of leak was identified. LE was then performed by advancing a 20- or 22-gauge needle into the leaking lymphatic vessel or the closest proximal lymph node under fluoroscopic guidance (Video 1). An injection of dextrose 5% through the 22-gauge needle with the clearing of the lipiodol in the lymphatic vessel confirmed access (Video 2). LE was then performed using a mixture of lipiodol and n-BCA (Trufill; Codman Neuro, Raynham, Massachusetts) (Video 3). The dilution of the n-BCA was determined based on the distance between the site of injection and the point of leak according to the operator’s preference, ranging between 1:2 and 1:10. If the drain output remained consistently elevated for several days following the procedure, the lymphangiogram procedure was repeated based on the interventional radiologist’s assessment.
Figure 3.
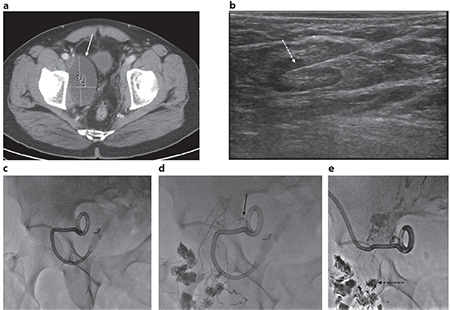
A 61-year-old male with a history of prostatectomy and pelvic lymphadenectomy presenting with pelvic pain and right lower extremity edema. (a) Computed tomography of the abdomen and pelvis showing right pelvic fluid collection (white arrow) compressing the external iliac vein. Consistently high output of the drain noted (200 cc/day). (b) Ultrasound-guided access in one of the right inguinal lymph nodes with the needle tip placed at the corticomedullary junction (dotted white arrow). (c, d) Fluoro spot images before and during intra-nodal lymphangiography showing the focal area of contrast extravasation within the expected location of the collection (black arrow). Leak confirmed by flushing and aspirating the drain (not shown). (e) Access obtained under fluoroscopy to the lymph node closest to the leak (dotted black arrow). Position confirmed by injecting 5% dextrose, and then embolization was performed with 0.33 cc of n-butyl cyanoacrylate/lipiodol mixture (1:4). The output dropped, and the drain was removed 7 days later.
Outcomes
Technical success of sclerotherapy was defined as the ability to inject sclerosant and complete the procedure. Technical success of INL was defined as the ability to inject lipiodol and visualize the lymphatic vessels under fluoroscopy. Technical success of LE was defined as the ability to inject n-BCA into the leaking lymphatic vessel or closest proximal lymph node when a leak was identified. Clinical success was defined as a reduction in the drain output to less than 20 cc/24 hrs for 3 consecutive days with subsequent drain removal. The need to repeat the procedure and the number of procedures needed to achieve clinical success were recorded. Changes in the drain output and the time to drain removal following the first procedure were calculated. Adverse events after the procedure were reported according to the Society of Interventional Radiology classification.
Statistical analysis
Baseline demographics of patients and clinical characteristics were compared using Fisher’s exact test and an independent sample t-test as appropriate. IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, N.Y., USA) was used for the statistical analysis. The differences in the treatment outcomes between the two procedures were tested using different statistical tests based on the outcome variable category. The Mann–Whitney U test was used to compare the differences in the scale variables, and Fisher’s exact test was used to compare the categorical and ordinal variables between both groups.
Results
All sclerotherapy and INL procedures were technically successful (Table 2). In the INL/LE group, lymphatic leak was identified and subsequently embolized in 31 out of 35 procedures. Clinical success occurred after the first sclerotherapy procedure in eight out of 17 patients (47%). Five patients needed one additional sclerotherapy procedure, and four patients needed two additional sclerotherapy procedures. Clinical success following the first INL/LE was achieved in 24/29 patients (83%), which was significantly higher than the sclerotherapy group (83% vs. 47%, P = 0.011). Four patients needed one additional procedure, and one patient needed two additional procedures (Figure 1).
Table 2. Clinical outcomes of the procedure.
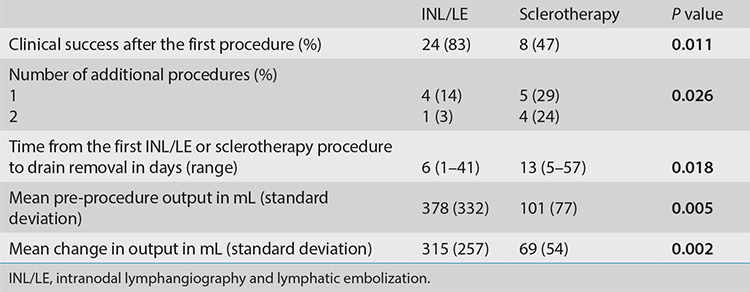
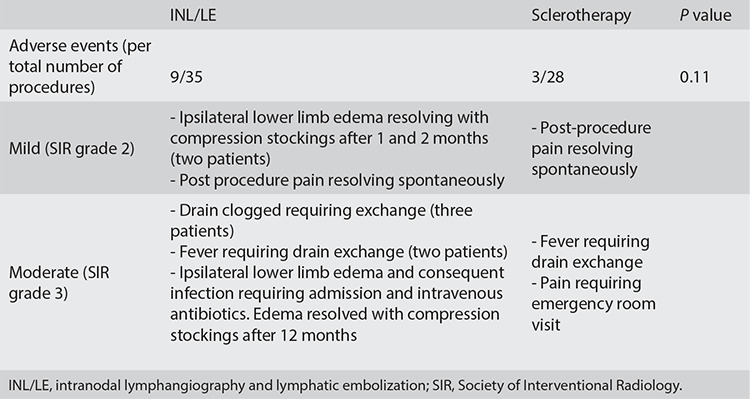
The INL/LE group had the drain for a significantly shorter duration (median of 6 vs. 13 days, P = 0.018). In the 27 patients who had recorded an output prior to sclerotherapy or INL/LE, the pre-procedure output (378 vs. 101 mL, P = 0.005) and change in the output after the first procedure (315 vs. 69 mL, P = 0.002) were higher in the INL/LE group. In the sclerotherapy group, the sclerosants were used as per the operator’s discretion and included absolute ethanol (18 times, median volume of 9 cc), sodium-tetradecyl sulfate 3% (four times, median volume 6.5 cc), povidone iodine (three times, median volume of 10 cc), doxycycline (one time, volume of 20 cc), and a combination of sclerosants was used four times (absolute ethanol three times, STS 3% one time, povidone iodine was used in the post-procedure drain flushes in the outpatient setting). No statistically significant difference was noted in the rate of adverse events between both groups (Table 3). Post-procedure pain and fever were noted in patients within both groups. The drain was clogged and had to be changed in three patients after INL/LE. Ipsilateral lower limb edema that resolved with conservative treatment was noted after INL/LE.
Table 3. Adverse events.
Discussion
The results show that INL/LE is associated with a higher clinical success rate after one procedure, fewer procedures for treatment, and a shorter drain dwell time. Those superior results were in spite of a higher initial daily drain output.
Percutaneous drainage and sclerotherapy have long been the standard treatment of symptomatic lymphoceles due to superior outcomes compared with drainage alone.3,5,10,11 To the authors’ knowledge, no specific sclerosant has been proven to be superior to others.5,7 Multiple studies have shown the efficacy of INL/LE in the treatment of lymphoceles; INL alone was associated with clinical success in around 70% of cases, which dropped to 35% in cases with high outputs (>500 mL/day).12,13,14 When combined with LE, clinical success climbs up to 100% with an average drain dwell time of 5–7 days.3,8,15,16,17,18 Concern for a lengthy procedure, similar to thoracic duct embolization procedures, is unfounded, as lipiodol has to travel a much shorter distance to the site of leakage in the pelvis or retroperitoneum, rather than all the way to the cisterna chyli.3,8
There is a paucity of data comparing the two treatment approaches, which is the primary objective of this study. In their systematic review of literature, Ten Hove et al.3 did not identify any studies comparing both modalities for the treatment of lymphoceles. However, they did note a higher proportion of success and shorter duration of treatment in studies using INL/LE. Kim et al.9 compared INL/LE with ethanol sclerotherapy in their cohort of 33 patients, which included patients with chylous ascites in the INL/LE group. They found a higher success rate with INL/LE of 83.3% compared with 43.8% with sclerotherapy, which they attributed to their institutional limitations on the number of procedures and duration of treatment. This is in line with the reported rate of clinical success after one sclerotherapy procedure of 47% that was reported in this study, which increased to 77% after a second sclerotherapy procedure. In the INL/LE group, clinical success after one procedure was 83%, which was significantly higher.
This head-to-head comparison emphasizes the difference in clinical success and, equally important, the difference in drain dwell time between the two treatment modalities. Percutaneous drainage catheters significantly affect patients’ quality of life, as they limit clothing and activities. In their study, Kim et al.9 noted a mean shorter drain dwell time with an INL/LE of 7.1 days vs. 12.3 days in the sclerotherapy group. However, the difference was not statistically significant. This study found a statistically significant lower median drain dwell time of 6 days in the INL/LE group compared with 13 days in the sclerotherapy group, which can be attributed to the larger sample size.
There were no major adverse events in either group. The incidence of mild or moderate adverse events with sclerotherapy was 10.7%, which is comparable to the incidence reported in the literature (0%–24%). There was no report of sclerosant extravasation, which is the most serious complication reported in the literature.5,7,10,11,19,20,21 The complication rate with LE was higher than the sclerotherapy group (26.4%) but not statistically significant, and it was slightly higher than in other studies (8%–20%).9,14 Most adverse events noted with LE were related to the drain occlusion having to be exchanged, which is why the authors advocate for exchanging the drainage catheter after LE in the same session. Ipsilateral lower limb edema was also noted in three patients in the LE group and is likely related to the occlusion of the lymphatic vessels draining that limb during embolization. In all cases, the edema resolved with compression stockings and no additional procedures, though it took up to 1 year in one patient.
The main limitations of this study are its retrospective nature and small sample size. The choice of treatment modality was based on the operator’s preference, which introduces a selection bias. INL/LE is a relatively novel procedure compared with sclerotherapy, which also contributes to the selection bias; however, the authors controlled that factor by limiting the start date to 2017. The heterogeneity of the sclerotherapy technique is also a limitation of this study, but it reflects the real-world experience, where sclerotherapy techniques vary greatly between operators, even those within the same institution. The experience of the different operators with INL/LE is not homogeneous, even within this study, which can limit the generalization of the results to other settings with a smaller number of cases.
In conclusion, INL/LE is a safe and effective treatment for symptomatic lymphoceles that develop after oncological surgeries. It is associated with a higher clinical success rate after the first procedure and shorter drain dwell time than sclerotherapy. A randomized, prospective study comparing the two treatment modalities is needed to confirm these results.
Video 1 link: https://www.youtube.com/watch?v=uWXhbp79P2A
Video 1. Fluoroscopy-guided lymph node access. The most proximal lymph node is targeted with the 20-gauge needle under fluoroscopic guidance.
Video 2 link: https://www.youtube.com/watch?v=Kc2slfYC0RQ
Video 2. Dextrose 5% intranodal flush. Dextrose 5% is injected after needle placement to confirm an adequate needle position. Notice the flow of the lipiodol in the lymphatic vessels toward the leak as it gets pushed by the D5% flush. Also note the lymph node getting less dense as the lipiodol is pushed out of it.
Video 3 link: https://www.youtube.com/watch?v=_PtgyYyeikE
Video 3. n-butyl cyanoacrylate (n-BCA) embolization. The N-BCA/lipiodol combination fills the access lymph node and the lymphatic vessels, causing a leak and the complete embolization of the leaking vessel. Injection stopped when extra-nodal extravasation was noted.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
Funding
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748.
References
- 1.Tsaur I, Thomas C. Risk factors, complications and management of lymphocele formation after radical prostatectomy: A mini-review. Int J Urol. 2019;26(7):711–716. doi: 10.1111/iju.13964. [DOI] [PubMed] [Google Scholar]
- 2.Song SY, Park M, Kang BH, et al. Distribution of lymphocele following lymphadenectomy in patients with gynecological malignancies. Obstet Gynecol Sci. 2020;63(6):700–708. doi: 10.5468/ogs.20110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ten Hove AS, Tjiong MY, Zijlstra IAJ. Treatment of symptomatic postoperative pelvic lymphoceles: a systematic review. Eur J Radiol. 2021;134:109459. doi: 10.1016/j.ejrad.2020.109459. [DOI] [PubMed] [Google Scholar]
- 4.Kim JK, Jeong YY, Kim YH, Kim YC, Kang HK, Choi HS. Postoperative pelvic lymphocele: treatment with simple percutaneous catheter drainage. Radiology. 1999;212(2):390–394. doi: 10.1148/radiology.212.2.r99au12390. [DOI] [PubMed] [Google Scholar]
- 5.Alago W Jr, Deodhar A, Michell H, et al. Management of postoperative lymphoceles after lymphadenectomy: percutaneous catheter drainage with and without povidoneiodine sclerotherapy. Cardiovasc Intervent Radiol. 2013;36(2):466–471. doi: 10.1007/s00270-012-0375-3. [DOI] [PubMed] [Google Scholar]
- 6.Khorshidi F, Majdalany BS, Peters G, et al. Minimally invasive treatment of abdominal lymphocele: a review of contemporary options and how to approach them. Lymphology. 2021;54(2):56–67. [PubMed] [Google Scholar]
- 7.Mahrer A, Ramchandani P, Trerotola SO, Shlansky-Goldberg RD, Itkin M. Sclerotherapy in the management of postoperative lymphocele. J Vasc Interv Radiol. 2010;21(7):1050–1053. doi: 10.1016/j.jvir.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 8.Moussa AM, Camacho JC, Maybody M et al. Percutaneous lymphatic embolization as primary management of pelvic and retroperitoneal Iatrogenic lymphoceles. J Vasc Interv Radiol. 2021;32(11):1529–1535. doi: 10.1016/j.jvir.2021.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim SW, Hur S, Kim SY, et al. The efficacy of lymph node embolization using n-butyl cyanoacrylate compared to ethanol sclerotherapy in the management of symptomatic lymphorrhea after pelvic surgery. J Vasc Interv Radiol. 2019;30(2):195–202. doi: 10.1016/j.jvir.2018.09.038. [DOI] [PubMed] [Google Scholar]
- 10.Kim Y, Jeon GS, Choi SY, Kim MD, Lee SJ. Evaluation of sclerotherapy for the treatment of infected postoperative lymphocele. Taiwan J Obstet Gynecol. 2017;56(4):477–481. doi: 10.1016/j.tjog.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Klode J, Klötgen K, Körber A, Schadendorf D, Dissemond J. Polidocanol foam sclerotherapy is a new and effective treatment for postoperative lymphorrhea and lymphocele. J Eur Acad Dermatol Venereol. 2010;24(8):904–909. doi: 10.1111/j.1468-3083.2009.03546.x. [DOI] [PubMed] [Google Scholar]
- 12.Alejandre-Lafont E, Krompiec C, Rau WS, Krombach GA. Effectiveness of therapeutic lymphography on lymphatic leakage. Acta Radiol. 2011;52(3):305–311. doi: 10.1258/ar.2010.090356. [DOI] [PubMed] [Google Scholar]
- 13.Gruber-Rouh T, Naguib NNN, Lehnert T, et al. Direct lymphangiography as treatment option of lymphatic leakage: indications, outcomes and role in patient’s management. Eur J Radiol. 2014;83(12):2167–2171. doi: 10.1016/j.ejrad.2014.09.013. [DOI] [PubMed] [Google Scholar]
- 14.Hur S, Jun H, Jeong YS. Novel interventional radiological management for lymphatic leakages after gynecologic surgery: lymphangiography and embolization. Gland Surg. 2021;10(3):1260–1267. doi: 10.21037/gs-2019-ursoc-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smolock AR, Nadolski G, Itkin M. Intranodal glue embolization for the management of postsurgical groin lymphocele and lymphorrhea. J Vasc Interv Radiol. 2018;29(10):1462–1465. doi: 10.1016/j.jvir.2018.04.020. [DOI] [PubMed] [Google Scholar]
- 16.Baek Y, Won JH, Chang SJ, et al. Lymphatic embolization for the treatment of pelvic lymphoceles: preliminary experience in five patients. J Vasc Interv Radiol. 2016;27(8):1170–1176. doi: 10.1016/j.jvir.2016.04.011. [DOI] [PubMed] [Google Scholar]
- 17.Chu HH, Shin JH, Kim JW, Noh SY, Yang WJ, Park S. Lymphangiography and lymphatic embolization for the management of pelvic lymphocele after radical prostatectomy in prostatic cancer. Cardiovasc Intervent Radiol. 2019;42(6):873–879. doi: 10.1007/s00270-019-02209-6. [DOI] [PubMed] [Google Scholar]
- 18.Hur S, Shin JH, Lee IJ, et al. Early experience in the management of postoperative lymphatic leakage using lipiodol lymphangiography and adjunctive glue embolization. J Vasc Interv Radiol. 2016;27(8):1177–1186. doi: 10.1016/j.jvir.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 19.Baboudjian M, Tadrist A, Gondran-Tellier B, et al. Povidone-iodine sclerotherapy of primary symptomatic lymphocele after kidney transplantation. Int Urol Nephrol. 2021;53(4):685–690. doi: 10.1007/s11255-020-02709-2. [DOI] [PubMed] [Google Scholar]
- 20.Kerlan RK Jr, LaBerge JM, Gordon RL, Ring EJ. Bleomycin sclerosis of pelvic lymphoceles. J Vasc Interv Radiol. 1997;8(5):885–887. doi: 10.1016/s1051-0443(97)70678-x. [DOI] [PubMed] [Google Scholar]
- 21.Zuckerman DA, Yeager TD. Percutaneous ethanol sclerotherapy of postoperative lymphoceles. AJR Am J Roentgenol. 1997;169(2):433–437. doi: 10.2214/ajr.169.2.9242748. [DOI] [PubMed] [Google Scholar]


