Abstract
This mini-review examines the management of atrial fibrillation (AF) in patients at high risk of bleeding, with a focus on stroke prevention and intracranial hemorrhage risk. Anticoagulant therapy is commonly advised for AF patients, but it can elevate the risk of intracranial hemorrhage in certain individuals prone to bleeding. Two primary perspectives for managing high-risk patients are discussed: adhering to strict anticoagulation therapy or opting for alternative treatments like left atrial appendage closure (LAAC) or aspirin. The benefits and drawbacks of each approach are evaluated, emphasizing the importance of a personalized management plan based on patient risk profiles, comorbidities, and preferences. Ongoing research, including artificial intelligence, advances in LAAC devices, and combination therapies, is explored to enhance stroke prevention and minimize bleeding risk in AF management. A multidisciplinary approach and continuous investigation are vital to achieving better patient outcomes and overall care in this context.
Keywords: Atrial fibrillation, intracranial hemorrhage, stroke
Introduction
Atrial fibrillation (AF) is a common cardiac arrhythmia that affects approximately 33 million people around the world and is linked to increased stroke and mortality risks (Chugh et al., 2014).[1] Oral anticoagulant (OAC) therapy is usually advised for AF patients to avert thromboembolic events like strokes (Kirchhof et al., 2016).[2] Nevertheless, this therapy may raise the risk of intracranial hemorrhage (ICH) in patients prone to bleeding (Cuker et al., 2020)[3], making patient management a topic of considerable discussion among neurosurgeons and cardiologists. There are two primary perspectives for managing patients with AF at high risk of bleeding: adhering to strict anticoagulation therapy or forgoing it in favor of alternative treatments like left atrial appendage closure (LAAC) (Holmes et al., 2014[4]) or aspirin (Saxena and Koudstaal, 2004)[5]. Both strategies have their pros and cons, which will be discussed in this literature review and summarized in Table 1. Gaining a comprehensive understanding of the benefits and drawbacks of each approach is crucial for developing a personalized management plan that considers the patient’s risk profile, comorbidities, and preferences, ultimately leading to the best possible outcomes.
Table 1.
Pros and cons of atrial fibrillation treatments
| VKAs |
| Long-term use has been studied extensively |
| Applicable for patients with mechanical heart valves |
| Inexpensive |
| Requires regular monitoring and dose adjustments |
| Can interact with other medications and foods |
| High risk of bleeding and hemorrhage |
| LAAC |
| Effective alternative for patients who cannot undergo anticoagulation therapy |
| Minimally invasive procedure |
| May reduce the need for long-term anticoagulation therapy |
| Requires a specialized procedure and an experienced operator |
| May require implant removal or replacement |
| Complications related to the device, such as fluid buildup around the heart (pericardial effusion) or clot formation on the device (device thrombosis), might arise |
| DOACs |
| Quick action onset and cessation |
| Standardized dosing without regular monitoring |
| Reduced likelihood of intracranial bleeding compared to warfarin |
| Limited data on long-term use |
| Can be more expensive than other anticoagulants |
| Lack of specific antidotes in cases of bleeding or overdose |
| Antiplatelets |
| Widely available and used for multiple indications |
| Lower risk of bleeding compared to anticoagulants |
| Lower cost compared to anticoagulants |
| Limited effectiveness for stroke prevention in AF patients |
| May not be effective in patients with multiple comorbidities |
| Less potent anticoagulant effect compared to other therapies |
VKAs: Vitamin K antagonists, LAAC: Left atrial appendage closure, DOACs: Direct oral anticoagulants, AF: Atrial fibrillation
Anticoagulation versus Placebo
The American Stroke Association (ASA) and American Heart Association (AHA) guidelines advocate for anticoagulation treatment in AF patients with a CHA2DS2-VASc score of 2 or above, a strategy aimed at reducing the likelihood of stroke and other thromboembolic incidents (January et al., 2019).[6] However, some experts argue that all AF patients should receive anticoagulation therapy, regardless of their bleeding risks, given the therapy’s well-established efficacy in reducing stroke and mortality risk. Advocates of this broader approach emphasize the critical role of careful patient selection and vigilant monitoring in minimizing the risk of ICH. Numerous studies have demonstrated the effectiveness of anticoagulation therapy, which employs Vitamin K antagonists (VKAs) or direct OACs (DOACs), in reducing the risk of stroke, systemic embolism, and mortality among AF patients. A large-scale meta-analysis encompassing more than 45,000 AF patients revealed that anticoagulation therapy led to a 64% decrease in the risk of stroke or systemic embolism and a 26% reduction in overall mortality when contrasted with placebo or no intervention (Hart et al., 2007).[7]
These findings underscore the value of anticoagulation therapy as an essential component of AF management. However, it is crucial to balance its benefits against the potential bleeding risk. Notably, anticoagulation therapy is associated with a 67% increased risk of major bleeding relative to placebo or no treatment (Hart et al., 2007).[7] Despite this increased risk, the net clinical benefit demonstrates that the advantages of anticoagulation therapy – namely, its capacity to reduce stroke, systemic embolism, and mortality risks – outweigh the associated bleeding risks. This underscores the importance of a comprehensive assessment and ongoing monitoring of AF patients receiving anticoagulation therapy, allowing health-care providers to optimize patient outcomes while minimizing potential complications.
Vitamin K Antagonist versus Direct Oral Anticoagulants
In patients with AF receiving anticoagulation therapy, the risk of ICH is a significant concern. A comprehensive meta-analysis that included over 100,000 AF patients showed that DOACs were linked to a lower ICH risk compared to VKAs, with a 50% reduction in ICH risk (Ruff et al., 2014).[8] The analysis covered 11 randomized controlled trials and seven observational studies, demonstrating a significant reduction in ICH risk for DOACs compared to VKAs (odds ratio [OR] 0.50, 95% confidence interval [CI] 0.43–0.58, P < 0.001). Furthermore, the meta-analysis found that ICH risk was lower for DOACs than for no anticoagulation therapy, suggesting that DOACs’ benefits in reducing stroke and systemic embolism risk outweigh the ICH risk (Ruff et al., 2014).[8] The study also indicated that DOACs had a reduced risk of major bleeding compared to VKAs (OR 0.89, 95% CI 0.81–0.98, P = 0.01); however, there was no significant difference in all-cause mortality risk between the two groups (OR 0.95, 95% CI 0.88–1.03, P = 0.21), implying that DOACs may be a safer alternative to VKAs regarding ICH risk for AF patients requiring anticoagulation therapy.
These meta-analyses provide strong evidence supporting the effectiveness of anticoagulation therapy in reducing stroke, systemic embolism, and mortality risks among AF patients (Ruff et al., 2014).[8] Although anticoagulation therapy is associated with an increased risk of major bleeding, its net clinical benefit outweighs the risks. In addition, DOACs may have a lower ICH risk compared to VKAs. Careful patient selection and proper monitoring can help mitigate ICH risk. The AHA and ASA guidelines recommend a thorough evaluation of high bleeding-risk patients, such as those with a history of ICH or recurrent gastrointestinal bleeding, before initiating anticoagulation therapy (January et al., 2019).[6] The guidelines also advise regular patient monitoring to ensure therapeutic range adherence and periodic bleeding risk reassessment. The benefits of using anticoagulation therapy for all AF patients include reduced stroke risk and mortality and the availability of reversal agents to minimize bleeding risk. Disadvantages of this approach include the increased ICH risk, the need for routine monitoring, and the potential for drug interactions.
Anticoagulant versus Left Atrial Appendage Closure
While anticoagulation therapy effectively reduces stroke and mortality risk in patients with AF, some experts argue that the risk of ICH might outweigh the benefits for certain patients, particularly those with a history of ICH or other bleeding risk factors (Pisters et al., 2010).[9] Research has shown that anticoagulation therapy use in patients with a history of ICH was linked to a higher risk of recurrent ICH, as indicated by an elevated CHA2DS2-VASc score[10] (adjusted hazard ratio [HR] 2.23, 95% CI 1.29–3.85; Nielsen et al., 2015). Patients with other bleeding risk factors, like a high HAS-BLED score, might also experience an increased ICH risk with anticoagulation therapy (Lip et al., 2011).[11] In these cases, alternative treatments like LAAC or aspirin might be considered. Numerous studies have investigated the use of LAAC in AF patients who are ineligible for anticoagulation therapy due to a high bleeding risk (Holmes et al.,[4] 2014; Reddy et al.,[12] 2013).
A study discovered a considerable decrease in stroke and major bleeding risk related to LAAC when compared to aspirin (Reddy et al., 2014).[13] Furthermore, the Left Atrial Appendage Occlusion for Stroke Prevention in AF (PREVAIL) trial determined that LAAC was as effective as warfarin in averting stroke or systemic embolism while also demonstrating a lower risk of significant bleeding and cardiovascular death (Holmes et al., 2014).[4] These results indicate that LAAC might be a suitable substitute for prolonged anticoagulation treatment in certain AF patients with a heightened risk of bleeding or who have contraindications for OACs. In addition, research has shown that aspirin use in AF patients with a low risk of stroke and bleeding was not less effective than anticoagulation therapy in terms of stroke or systemic embolism risk (ROCKET AF investigators, 2011).[14] These studies demonstrate that alternative treatments may be appropriate for certain AF patients and can offer effective stroke prevention without increasing bleeding risk. Deciding to avoid anticoagulation therapy in specific AF patients has advantages and disadvantages that must be weighed. One significant benefit of this approach is the reduced risk of ICH, a severe complication associated with anticoagulation therapy (Pisters et al., 2010).[9] In addition, forgoing anticoagulation therapy may create opportunities to use alternative treatments that effectively reduce stroke and systemic embolism risk.
Anticoagulant versus Antiplatelets
On the other hand, there are several drawbacks to forgoing anticoagulation therapy that need to be taken into account. Patients who do not receive anticoagulation therapy face a heightened risk of stroke and mortality in comparison to those who undergo appropriate anticoagulation treatment. For example, a systematic review and meta-analysis encompassing 22 studies with 266,128 AF patients revealed that those not receiving anticoagulation therapy had a significantly elevated stroke risk compared to those who did (HR = 1.65, 95% CI: 1.49–1.82) (Wang et al., 2015).[15] Furthermore, the evidence supporting alternative therapies such as aspirin or dual antiplatelet therapy is limited and may not be as efficacious as anticoagulation therapy. A meta-analysis of 13 randomized controlled trials involving 16,267 AF patients discovered that aspirin correlated with a higher stroke risk compared to anticoagulation therapy (risk ratio = 1.51, 95% CI: 1.21–1.89) (Hart et al., 2007).[7] Lastly, it is crucial to meticulously select patients to determine who has a low risk of stroke and bleeding and who may benefit from alternative therapies or no anticoagulation therapy. As a result, the decision to forgo anticoagulation treatment in specific patients should be determined individually, considering each patient’s distinct risk factors and preferences, while generally following the guidelines outlined in Figure 1’s flowchart.
Figure 1.
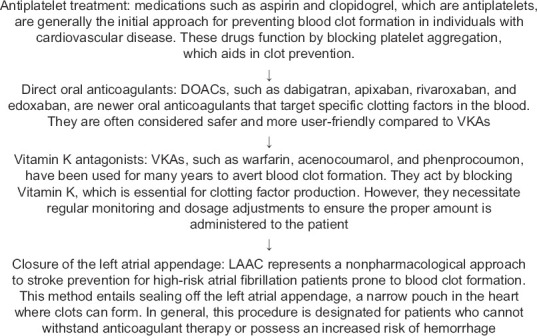
Flowchart of atrial fibrillation treatment. This figure depicts the various treatments employed to prevent blood clot formation in individuals with cardiovascular disease, encompassing antiplatelet therapy, direct oral anticoagulants, and Vitamin K antagonists. In addition, it demonstrates the nondrug-based approach of left atrial appendage closure for reducing stroke risk in patients with atrial fibrillation. DOAC: Direct oral anticoagulant, VKAs: Vitamin K antagonists, LAAC: Left atrial appendage closure
Risk of Embolism in Atrial Fibrillation Patients
The risk of embolism in patients with AF is a crucial aspect to consider in the clinical management of the disease, significantly influenced by the presence and nature of associated heart lesions. An enlarged left atrium, for instance, can lead to blood stasis and clot formation, potentially increasing the embolic risk. In addition, ventricular lesions and decreased contractility can disrupt normal blood flow, thereby promoting thrombus formation and consequently embolism (January, 2014).[16] Valve lesions, particularly in the case of valvular AF, can also contribute to a heightened embolic risk due to abnormal blood flow and clot formation at the site of the valve abnormality (Steffel, 2021).[17] In managing such patients, it is generally recommended to use anticoagulant therapy for stroke prevention, particularly in those with low cardiac risk and low bleeding risk (Lip, 2021).[11] However, decisions regarding the use of anticoagulation in AF should be individualized and based on a careful assessment of both thromboembolic and bleeding risks (Kirchhof, 2016).[2]
Artificial Intelligence in Anticoagulant Therapy
According to the AHA, an innovative solution for balancing stroke prevention and ICH risk in AF management is to use artificial intelligence (AI) to personalize anticoagulant therapy (January, 2019).[6] AI algorithms can be trained to analyze a patient’s medical history, including factors such as age, sex, comorbidities, and medication use, and use that information to predict the patient’s risk of stroke and ICH (Xu et al., 2020).[18] The algorithm can then use that information to recommend a personalized anticoagulant therapy plan that minimizes the risk of both stroke and ICH. This approach has the potential to improve patient outcomes by providing more accurate and personalized treatment recommendations, while also reducing the risk of adverse events associated with anticoagulant therapy (Constantinides et al., 2018).[19] It could also help health-care providers make more informed decisions about anticoagulant therapy and reduce the likelihood of treatment-related complications. While this solution is still in its early stages, there is growing interest in using AI to personalize medical treatment, and it has the potential to be a game changer in the management of AF (Mairesse et al., 2018).[20]
Hypothesis
The implementation of a personalized risk assessment tool using comprehensive patient-specific factors, including but not limited to genetic predispositions, specific heart lesions, lifestyle factors, and prior medical history, will enhance the prediction of both stroke and ICH risks in patients with AF, leading to improved outcomes through individualized anticoagulant management strategies.
This hypothesis could potentially contribute new insights to the field of stroke prevention and management of ICH risk in AF. The current risk models, such as the CHA2DS2-VASc score for stroke risk and HAS-BLED score for bleeding risk, though valuable, have limitations and do not account for a comprehensive range of patient-specific factors. For instance, they do not account for genetic predispositions, specific types of heart lesions, or lifestyle factors that could potentially influence a patient’s risk. The proposed risk assessment tool would take these factors into account, enabling more precise risk prediction and more personalized management strategies. Testing this hypothesis would involve developing and validating this new tool in clinical trials, involving large patient cohorts with diverse characteristics. If successful, this tool could help clinicians make more informed decisions about anticoagulant therapy, balancing the potential benefits of stroke prevention against the risks of ICH on an individual patient basis. Moreover, this could also pave the way for research into how these factors specifically influence stroke and bleeding risk, leading to a deeper understanding of the pathophysiology of these complications in AF.
Future Directions of Left Atrial Appendage Closure
Recent years have seen a growing interest in the development of new LAAC devices, with the aim of enhancing procedural success, reducing complications, and addressing the limitations of currently available devices, like the Watchman device (Price et al., 2021).[21] Devices such as the Amulet and WaveCrest feature different designs and delivery methods, offering potential advantages over existing standard care devices (Price et al., 2021).[21] These innovations are expected to enhance device efficacy, safety, and ease of use, leading to more widespread adoption of LAAC in clinical practice. Research is also examining the use of LAAC in combination with other therapies, like antiplatelet therapy (Holmes et al., 2014).[4] This approach could potentially enhance the effectiveness of stroke prevention while minimizing bleeding risks. In addition, the research could investigate whether LAAC combined with novel anticoagulants could offer synergistic benefits in stroke prevention.
As LAAC becomes more widely adopted in clinical practice, it will be important to evaluate the long-term outcomes and cost-effectiveness of the procedure compared to traditional anticoagulation therapy. This information will be crucial in informing clinical decision-making and health-care resource allocation. As LAAC continues to gain acceptance as a substitute for anticoagulation therapy in selected patients, there is a growing need for standardized training and procedural guidelines to ensure consistency and quality of care across different institutions (Gillinov, 2007).[22] This may include the development of certification programs, hands-on training sessions, and ongoing education to keep health-care providers abreast of the latest advancements in LAAC technology and techniques. Advancements in imaging and guidance techniques will likely play a significant role in improving the efficacy and safety of LAAC procedures (Pellegrino et al., 2016).[23] For example, the use of three-dimensional transesophageal echocardiography and intracardiac echocardiography can provide more accurate visualization of the left atrial appendage and better guidance during device deployment. Future research should continue to explore and refine imaging techniques to minimize procedural complications and improve patient outcomes.
Ensuring effective management of anticoagulation therapy for patients with AF is vital to minimize the risk of ICH (Zhang et al., 2019).[24] Although evidence advocates for anticoagulation therapy in all AF patients, meticulous patient selection and proper monitoring are essential for reducing ICH risk. Furthermore, alternative treatments, such as LAAC and aspirin, may effectively lower the stroke and systemic embolism risk for patients who cannot receive anticoagulation therapy due to high bleeding risk. However, employing a multidisciplinary approach is crucial to tailor patient management based on their risk profiles, comorbidities, and preferences, ultimately leading to optimal outcomes. To further improve the management of patients with ICH due to anticoagulation, future research should focus on the development of improved imaging techniques and new treatment strategies. Diffusion tensor imaging has shown promise in identifying the white matter changes associated with anticoagulant-related ICH, which can enable early intervention and prevent severe neurological deficits (Zhang et al., 2017).[24] Furthermore, the use of tranexamic acid has been shown to reduce bleeding and improve outcomes in traumatic brain injury (Rowell et al., 2020),[25] and its effectiveness in anticoagulant-related ICH warrants further investigation. Finally, randomized controlled trials can be conducted to evaluate the efficacy and safety of different treatment options, including early hematoma evacuation, minimally invasive surgery, and other medical interventions. With more research in these areas, neurologists, internists, and cardiologists can continue to improve the management and outcomes of patients with ICH due to anticoagulation, leading to better overall care and outcomes for these patients (Greenberg 2022).[26]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129:837–47. doi: 10.1161/CIRCULATIONAHA.113.005119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Europace. 2016;18:1609–78. doi: 10.1093/europace/euw295. [DOI] [PubMed] [Google Scholar]
- 3.Cuker A, Burnett A, Triller D, Crowther M, Ansell J, Van Cott EM, et al. Reversal of direct oral anticoagulants: Guidance from the Anticoagulation Forum. American Journal of Hematology. 2020;95:677–89. doi: 10.1002/ajh.25475. [DOI] [PubMed] [Google Scholar]
- 4.Holmes DR, Doshi SK, Kar S, Price MJ, Sanchez JM, Sievert H. Left atrial appendage closure as an alternative to warfarin for stroke prevention in atrial fibrillation: a patient-level meta-analysis. Journal of the American College of Cardiology. 2014;63(25 Pt A):2617–24. doi: 10.1016/j.jacc.2015.04.025. [DOI] [PubMed] [Google Scholar]
- 5.Van Walraven C, Hart RG, Singer DE, Laupacis A, Connolly S, Petersen P, et al. Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta-analysis. JAMA. 2002;288:2441–8. doi: 10.1001/jama.288.19.2441. [DOI] [PubMed] [Google Scholar]
- 6.January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology. 2019;74:104–32. doi: 10.1016/j.jacc.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Annals of Internal Medicine. 2007;146:857–67. doi: 10.7326/0003-4819-146-12-200706190-00007. [DOI] [PubMed] [Google Scholar]
- 8.Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. The Lancet. 2014;383:955–62. doi: 10.1016/S0140-6736(13)62343-0. [DOI] [PubMed] [Google Scholar]
- 9.Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138:1093–100. doi: 10.1378/chest.10-0134. [DOI] [PubMed] [Google Scholar]
- 10.Nielsen PB, Larsen TB, Skjø th F, Lip GY. Outcomes associated with resuming warfarin treatment after hemorrhagic stroke or traumatic intracranial hemorrhage in patients with atrial fibrillation. JAMA Internal Medicine. 2015;175:609–15. doi: 10.1001/jamainternmed.2016.9369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2011;137:263–72. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 12.Reddy VY, Doshi SK., Sievert H., Buchbinder M., Neuzil P., Huber K., Whisenant B. Percutaneous left atrial appendage closure for stroke prophylaxis in patients with atrial fibrillation: 2.3-Year Follow-up of the PROTECT AF (Watchman Left Atrial Appendage System for Embolic Protection in Patients with Atrial Fibrillation) Trial. Circulation. 2013;127(6):720–729. doi: 10.1161/CIRCULATIONAHA.112.114389. [DOI] [PubMed] [Google Scholar]
- 13.Reddy VY, Mö bius-Winkler S, Miller MA, Neuzil P, Schuler G, Wiebe J, et al. Left atrial appendage closure with the Watchman device in patients with a contraindication for oral anticoagulation: the ASAP study (ASA Plavix Feasibility Study With Watchman Left Atrial Appendage Closure Technology) Journal of the American College of Cardiology. 2013;61:2551–6. doi: 10.1016/j.jacc.2013.03.035. [DOI] [PubMed] [Google Scholar]
- 14.ROCKET AF Investigators. Rivaroxaban-once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation: rationale and design of the ROCKET AF study. American Heart Journal. 2011;159:340–7.e1. doi: 10.1016/j.ahj.2009.11.025. [DOI] [PubMed] [Google Scholar]
- 15.Wang KL, Lip GY, Lin SJ, Chiang CE. Non-Vitamin K Antagonist Oral Anticoagulants for Stroke Prevention in Asian Patients With Nonvalvular Atrial Fibrillation: Meta-Analysis. Stroke. 2015;46:2555–61. doi: 10.1161/STROKEAHA.115.009947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.January CT, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation. 2014;130:e199–267. doi: 10.1161/CIR.0000000000000041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bö hm M, et al. ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2022;24:4–131. doi: 10.1002/ejhf.2333. [DOI] [PubMed] [Google Scholar]
- 18.Xu Y, Zhao L, Zhang L, Han Y, Wang P, Yu S. Left Atrial Enlargement and the Risk of Stroke: A Meta-Analysis of Prospective Cohort Studies. Front Neurol. 2020;11:26. doi: 10.3389/fneur.2020.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Constantinides P, Fitzmaurice DA. Artificial intelligence in cardiology: applications, benefits, and challenges. British Journal of Cardiology. 2018;25:86–90. [Google Scholar]
- 20.Mairesse GH, Moran P, Van Gelder IC, Elsner C, Rosenqvist M, Mant J, et al. ESC Scientific Document Group. Screening for atrial fibrillation: a European Heart Rhythm Association (EHRA) consensus document endorsed by the Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), and Latin American Society of Stimulation Cardiac and Electrophysiology (SOLAECE) Europace. 2017;19:1589–623. doi: 10.1093/europace/eux177. [DOI] [PubMed] [Google Scholar]
- 21.Price MJ, Gibson DN, Yakubov SJ. A new generation of left atrial appendage closure devices: Technology, techniques, and outcomes. Journal of the American College of Cardiology: Clinical Electrophysiology. 2021;7:233–46. [Google Scholar]
- 22.Gillinov AM. Advances in surgical treatment of atrial fibrillation. Stroke. 2007;38(2 Suppl):618–23. doi: 10.1161/01.STR.0000247934.04848.79. [DOI] [PubMed] [Google Scholar]
- 23.Pellegrino PL, Fassini G, DI Biase M, Tondo C. Left Atrial Appendage Closure Guided by 3D Printed Cardiac Reconstruction: Emerging Directions and Future Trends. J Cardiovasc Electrophysiol. 2016;27:768–71. doi: 10.1111/jce.12960. [DOI] [PubMed] [Google Scholar]
- 24.Zhang J, Zhang Y, Wang L, Sang L, Yang J, Yan R, et al. Disrupted structural and functional connectivity networks in ischemic stroke patients. Neuroscience. 2017;364:212–25. doi: 10.1016/j.neuroscience.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 25.Rowell SE, Meier EN, McKnight B, Kannas D, May S, Sheehan K, et al. Effect of out-of-hospital tranexamic acid vs placebo on 6-month functional neurologic outcomes in patients with moderate or severe traumatic brain injury: The prehospital anti-fibrinolytics for traumatic coagulopathy and hemorrhage (MATTERs) II randomized clinical trial. JAMA. 2020;324:1547–57. doi: 10.1001/jama.2020.8958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Greenberg SM, Ziai WC, Cordonnier C, Dowlatshahi D, Francis B, Goldstein JN, et al. American Heart Association/American Stroke Association. 2022 Guideline for the Management of Patients With Spontaneous Intracerebral Hemorrhage: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2022;53:e282–361. doi: 10.1161/STR.0000000000000407. [DOI] [PubMed] [Google Scholar]


