Abstract
Raising the minimum age of sale for tobacco products to 21 years (Tobacco 21) could help prevent and delay tobacco product initiation among youth. This study examined changes in U.S. adults’ attitudes toward Tobacco 21 policies during 2014–2017. Data came from the 2014–2017 annual Summer Styles surveys, an Internet-based, cross-sectional survey of U.S. adults aged ≥18 years, drawn from GfK’s KnowledgePanel®. Sample sizes ranged from 4107 in 2017 to 4269 in 2014. Each year, respondents were asked if they “strongly favor,” “somewhat favor,” “somewhat oppose,” or “strongly oppose” Tobacco 21 policies. Weighted prevalence estimates of favorability (strongly or somewhat favor) were assessed each year; differences in favorability between years were assessed by chi square tests. Adjusted odds ratios (aOR) of favorability with 95% confidence intervals (CI) were calculated using logistic regression for the year 2017. Tobacco 21 policy favorability was reported by 75.0% in 2014; 72.3% in 2015; 78.4% in 2016; and 75.2% in 2017; the difference in favorability between 2014 and 2017 was not statistically significant. In 2017, lower odds of favorability toward Tobacco 21 policies were observed for current (aOR = 0.49, CI = 0.37–0.64) and former (aOR = 0.54, CI = 0.44–0.66) cigarette smokers, and current other tobacco product users (aOR = 0.54, CI = 0.49–0.64) than respective nonusers. Among U.S. adults, Tobacco 21 favorability has remained high since 2014, coinciding with a period of rapid state and local-level policy adoption. These results could be helpful for states and localities as they work to understand the feasibility of Tobacco 21 policies in their jurisdiction.
Keywords: Tobacco, Public policy, Adolescent
1. Introduction
Over 90% of adult smokers start smoking cigarettes before the age of 18 years (U.S. Department of Health and Human Services, 2012). Youth initiating tobacco use behaviors at younger ages have a greater risk of nicotine addiction, progression to daily use, and difficulties quitting (U.S. Department of Health and Human Services, 2012). Chronic exposure to nicotine during adolescence, a critical period of brain development, is associated with long-term negative effects in reward-seeking behaviors, attention and cognition, mood, and other aspects of brain development (U.S. Department of Health and Human Services, 2016). Preventing or delaying the age at which young people experiment or use tobacco products could reduce the likelihood that they will become smokers in adulthood (Institute of Medicine, 2015).
Raising the minimum legal age of sale for tobacco products to 21 years (Tobacco 21 policies) is one strategy that could prevent or delay tobacco product experimentation or initiation by adolescents (U.S. Department of Health and Human Services, 2016; Institute of Medicine, 2015). Tobacco 21 policies began at the local-level; prior to the first state-wide policy, approximately 100 U.S. localities had enacted policies (University of Missouri – Columbia, Missouri Tobacco Control Research Center, 2018). As of November 2019, over 500 localities across 25 states had enacted Tobacco 21 legislation (Campaign for Tobacco-Free Kids, 2019). Hawaii was the first state to implement a Tobacco 21 policy (effective January 2016); since then, at least 15 additional states have implemented policies (Campaign for Tobacco-Free Kids, 2019; Centers for Disease Control and Prevention, n.d.), and several others have passed Tobacco 21 legislation citing forthcoming effective dates (Campaign for Tobacco-Free Kids, 2019; Centers for Disease Control and Prevention, n.d.). Additionally, a federal law was enacted on December 20, 2019 that raised the minimum age of sales of tobacco products from 18 to 21 years nationwide (116th U.S. Congress, 2019).
Understanding potential differences in public attitudes toward tobacco control interventions may inform health policy planning, practice, success, and sustainability. Thus, this study assessed socio-demographic differences in Tobacco 21 policy favorability and examined changes in U.S. adults’ attitudes toward Tobacco 21 policies during 2014–2017, a period of rapid local- and state-level policy adoption.
2. Methods
Data are from the 2014–2017 annual Summer Styles surveys, an internet-based cross-sectional survey of noninstitutionalized U.S. adults aged ≥18 years. Styles respondents are drawn from GfK’s KnowledgePanel®, which uses a probability-based sampling design to recruit panelists regardless of landline telephone or Internet access (GfK, n.d.). Summer Styles is the second in a series of annual surveys; each year, all respondents included in Summer Styles had participated in the previous Styles series (Spring Styles). Data were weighted to match the demographic distributions of U.S. adults presented in the Current Population Survey (GfK, n.d.). Sample sizes and response rates for Summer Styles were: 4269 (69%) in 2014; 4127 (67%) in 2015; 4203 (68%) in 2016; and 4107 (74%) in 2017. Styles data were licensed by Porter Novelli. Human subjects review was not required for this secondary analysis of de-identified data.
In 2014 and 2015, participants were asked, “Do you favor or oppose raising the legal minimum age to purchase all tobacco products from 18 to 21?” In 2016 and 2017, participants were asked, “Do you favor or oppose raising the minimum legal sale age for tobacco products to 21 years?” Each year, responses included “strongly favor,” “somewhat favor,” “somewhat oppose,” and “strongly oppose.” A response of “strongly favor” or “somewhat favor” was considered to reflect favorability toward Tobacco 21.
2.1. Statistical analysis
Analyses were conducted during 2019 using SUDAAN v11 (RTI International, NC). For 2017, the prevalence (with 95% confidence) of favorability was reported overall and by demographic characteristics: sex (male, female), age (18–24, 25–44, 45–64, 65+ years), race/ethnicity (white non-Hispanic, black non-Hispanic, Hispanic, other non-Hispanic), education (< high school, high school graduate, some college, college degree or higher), having a child aged <18 years (no, yes), current cigarette smoking status (never, former, current user), current other tobacco product use (no, yes; defined as past-30 day use of e-cigarettes, cigars, hookah, pipe tobacco, smokeless tobacco, or some other product), U.S. region (Northeast, Midwest, South, West), and annual household income (< $15,000, $15,000–$24,999, $25,000–$39,999, $40,000–$59,999, ≥$60,000). Multivariable logistic regression was used to assess the association between each covariate and Tobacco 21 favorability; adjusted odds ratios (aOR) with 95% confidence intervals (CI) were calculated.
The overall difference in the prevalence of Tobacco 21 favorability by year was assessed using the chi-square test. Differences in favorability were calculated between baseline (2014) and subsequent years (2015, 2016, and 2017), and during interim years (2015–2016; 2016–2017). For all analyses, a p-value < 0.05 was considered statically significant.
3. Results
Tobacco 21 favorability was reported as 75.0% 2014, 72.3% in 2015, 78.4% in 2016, and 75.2% in 2017. Year to year differences in favorability were observed from 2014–2015 (75.0% to 72.3%), 2015–2016 (72.3% to 78.4%), and 2016–2017 (78.4% to 75.2%). However, no difference in favorability was observed specifically between 2014 and 2017 (Fig. 1).
Fig. 1.
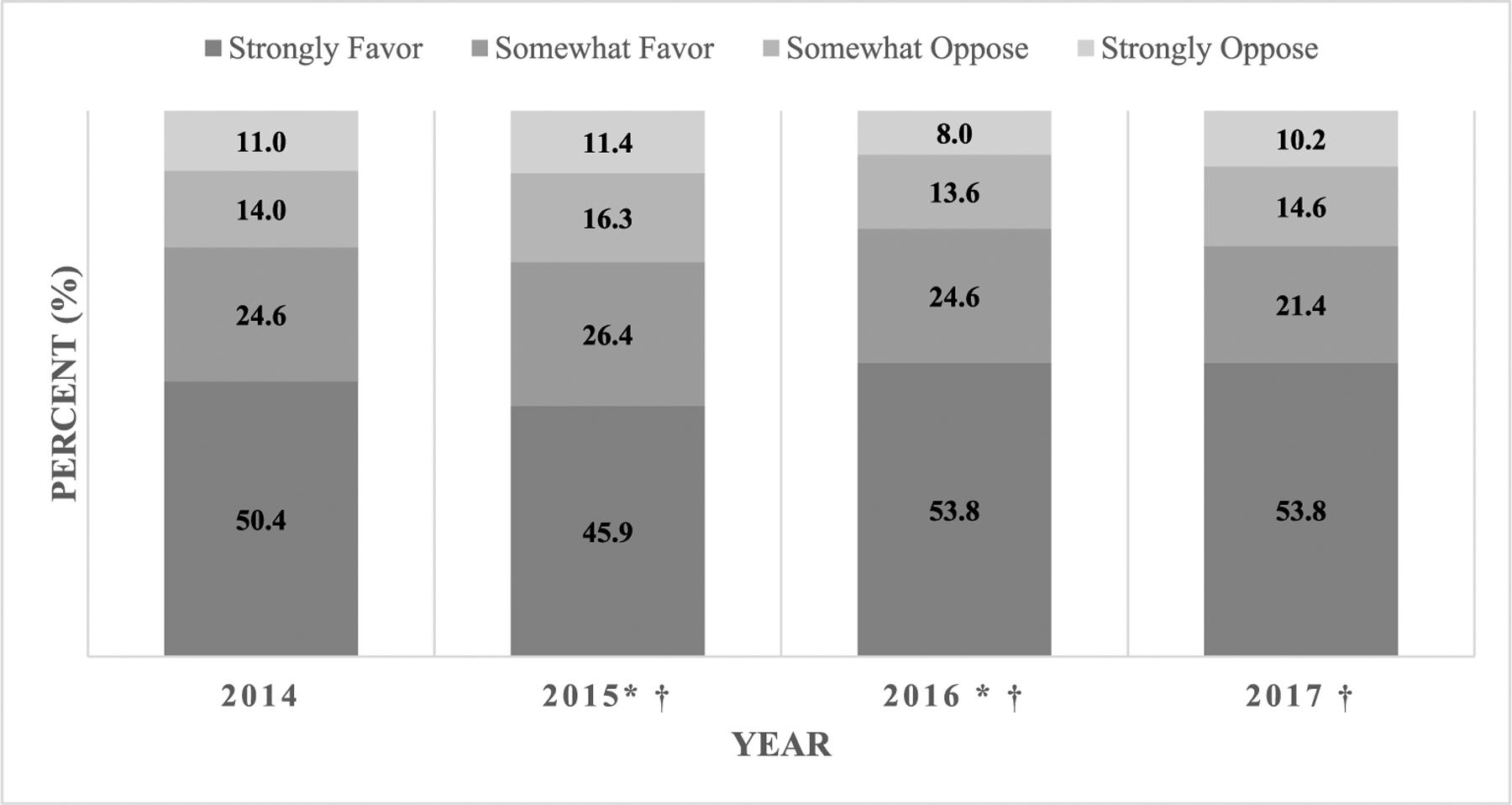
Favorability a toward raising the minimum legal age of sale of tobacco products to 21 years among adults in the United States, 2014–2017.b
a“Favorability” is defined as a response of “strongly favor” or “somewhat favor”; opposition is defined as a response of “somewhat oppose” or “strongly oppose”
bA statistically significant difference in overall Tobacco 21 favorability was observed across years (p < 0.001). Comparisons of favorability from baseline (2014) with subsequent years (2015, 2016, 2017) and interim years (2014–2015; 2015–2016; 2016–2017) was assessed by chi-square test (p < 0.05 considered statistically significant)
*Indicates a significant difference in favorability from baseline (2014). A significant difference was observed in in 2015 (p = 0.017) and 2016 (p = 0.003); a statistically significant comparison was not observed in 2017 (p = 0.876)
†Indicates a significant difference in favorability from previous reporting year. A significant difference was observed during 2014–2015 (p = 0.017), 2015–2016 (p < 0.001), and 2016–2017 (p = 0.004).
In 2017, Tobacco 21 favorability was significantly higher among females than males (79.4% vs. 70.6%); never cigarette smokers (80.0%) than former (72.4%) and current (64.7%) smokers; and current nonusers of other tobacco products (76.8%) than current users of other products (56.6%). Higher Tobacco 21 favorability was observed with increasing age and increasing annual household income (Table 1).
Table 1.
Correlates of favorability toward Tobacco 21 policies among adults, United States, 2017.
| na | Favors Tobacco 21 policy | |||
|---|---|---|---|---|
| % (95% CI)b | p-Value | aOR (95% CI)c | ||
| Overall | 4061 | 75.2 (73.7–76.7) | ||
| Sex | ||||
| Male | 1979 | 70.6 (68.3–72.9) | < 0.001 | 1.00 (ref) |
| Female | 2082 | 79.4 (77.4–81.3) | 1.32 (1.10–1.58) | |
| Age (years) | ||||
| 18–24 | 257 | 69.2 (63.0–74.7) | < 0.001 | 1.00 (ref) |
| 25–44 | 1331 | 70.8 (68.0–73.4) | 1.19 (0.85–1.66) | |
| 45–64 | 1711 | 77.1 (74.8–79.3) | 1.89 (1.37–2.61) | |
| ≥65 | 762 | 83.2 (80.0–86.0) | 3.19 (2.20–4.64) | |
| Race/ethnicity | ||||
| White, Non-Hispanic | 2973 | 74.5 (72.7–76.2) | 0.057 | 1.00 (ref) |
| Black, Non-Hispanic | 360 | 72.3 (66.8–77.2) | 0.94 (0.70–1.28) | |
| Hispanic | 491 | 80.0 (75.8–83.6) | 1.64 (1.22–2.19) | |
| Other, Non-Hispanic | 237 | 75.4 (68.5–81.3) | 1.16 (0.79–1.72) | |
| Education | ||||
| < High school | 255 | 71.1 (64.6–76.7) | 0.169 | 1.00 (ref) |
| High school | 1276 | 75.8 (73.1–78.3) | 1.04 (0.71–1.52) | |
| Some college | 1214 | 74.1 (71.2–76.8) | 0.93 (0.64–1.44) | |
| College degree or higher | 1316 | 77.3 (74.8–79.6) | 0.96 (0.64–1.44) | |
| Respondent has child < 18 years | ||||
| No | 2717 | 74.6 (72.7–76.4) | 0.180 | 1.00 (ref) |
| Yes | 1336 | 76.8 (74.0–79.3) | 1.37 (1.11–1.69) | |
| Current cigarette smoking statusd | ||||
| Never smoker | 2319 | 80.0 (78.1–81.8) | < 0.001 | 1.00 (ref) |
| Former smoker | 1084 | 72.4 (69.2–75.3) | 0.54 (0.44–0.66) | |
| Current smoker | 526 | 64.7 (59.9–69.2) | 0.49 (0.37–0.64) | |
| Current use - other tobacco productse | ||||
| Current nonuse | 3738 | 76.8 (75.2–78.3) | < 0.001 | 1.00 (ref) |
| Current use | 281 | 56.6 (50.0–62.9) | 0.54 (0.39–0.73) | |
| U.S. regionf | ||||
| Northeast | 781 | 75.4 (71.9–78.6) | 0.789 | 1.00 (ref) |
| Midwest | 888 | 74.3 (70.8–77.4) | 0.98 (0.75–1.29) | |
| South | 1476 | 74.8 (72.2–77.3) | 0.93 (0.73–1.18) | |
| West | 916 | 76.5 (73.2–79.4) | 1.01 (0.77–1.33) | |
| Annual household income | ||||
| < $15,000 | 203 | 62.5 (54.8–69.5) | < 0.001 | 1.00 (ref) |
| $15,000–$24,999 | 201 | 68.6 (61.3–75.1) | 1.26 (0.76–2.07) | |
| $25,000–$39,999 | 611 | 78.5 (74.6–81.9) | 1.55 (1.01–2.38) | |
| $40,000–$59,999 | 667 | 77.5 (73.9–80.7) | 1.43 (0.94–2.17) | |
| ≥$60,000 | 2379 | 76.5 (74.6–78.4) | 1.31 (0.88–1.94) | |
Abbreviations: aOR = adjusted odds ratio; CI = confidence interval; n = number, sample.
Sample size based on unweighted data; may not add up to total (n = 4061) due to missing data. n = 46 respondents were missing data on the outcome and thus are excluded from the analysis.
Computed using weighted data; differences in prevalence estimates assessed by the chi-squared test.
Computed using weighted data; differences in favorability are compared to the specified reference group adjusted for all other variables in the table (logistic regression).
Respondents were asked, (1) “Have you smoked at least 100 cigarettes in your entire life? One hundred cigarettes is equal to 5 packs of cigarettes.” (Yes, No), and (2) “Do you now smoke cigarettes every day, some days, or not at all?” Never smokers answered “no” to question (1). Former smokers answered “yes” to question (1) and “not at all” to question (2). Current smokers answered “yes” to question (1) and “every day” or “some days” to question (2).
Defined as use (past 30-days) of: e-cigarettes, cigars, hookah, pipe tobacco, smokeless tobacco, or “some other product.”
Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont. Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin. South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming.
The adjusted odds of favoring Tobacco 21 policies were lower for current (aOR = 0.49, CI: 0.37–0.64) and former (aOR = 0.54, CI: 0.44–0.66) cigarette smokers than never smokers and current users of other tobacco products (aOR = 0.54, CI: 0.49–0.64) than current nonusers of other tobacco products (Table 1). Respondents with children aged < 18 years had increased odds of Tobacco 21 policy favorability than respondents without children < 18 years (aOR = 1.37, CI: 1.11–1.69). The odds of favorability were higher among those aged 45–64 years (aOR = 1.89, CI: 1.37–2.61) and aged ≥65 years (aOR = 3.19, CI: 2.20–4.64) than those aged 18–24 years.
4. Discussion
In 2017, three-quarters of U.S. adults favored raising the minimum age of sale for tobacco products to 21 years. Favorable attitudes toward tobacco control policies, such as Tobacco 21, may result in more efficient policy adoption, implementation, and success (Schmidt et al., 2018). States and communities identifying opportunities to prevent youths’ tobacco product experimentation and initiation and use could use these results to support Tobacco 21 policies in their own regions, given the sustained and high favorability among U.S. adults (King et al., 2015) and youth (Glover-Kudon et al., 2019), who have a potential future stake in such policies.
Differences in favorability were observed across sociodemographic groups. Similar to previous literature, favorability was higher among females and Hispanic respondents (King et al., 2015; Lee et al., 2016). Additionally, Tobacco 21 favorability was higher among respondents with children < 18 years of age, likely in an effort to prevent their own children from using tobacco products. However, favorability was lower among those who may be directly impacted by the policy’s restrictions, including young adults and tobacco product users. Despite favorability being highest among never cigarette smokers and non-current tobacco product users, about two-thirds of current cigarette smokers and one-half of current users of other tobacco products still favored Tobacco 21 policies. This is consistent with previous literature (King et al., 2015; Winickoff et al., 2016) and the notion that many current smokers often regret they ever began smoking (Nayak et al., 2017).
Overall, public favorability toward Tobacco 21 policies remained high and stable during 2014–2017 (King et al., 2015), even though this represented a period of rapid policy adoption at the local and state levels (Campaign for Tobacco-Free Kids, 2019; Centers for Disease Control and Prevention, n.d.). In 2014, about three-quarters of adults, including nearly 70% of current cigarette smokers (King et al., 2015), reported Tobacco 21 favorability. Thus, there may have been little room for further increases in policy favorability over time. Additionally, other factors not assessed in the current study, such as personal or political beliefs and attitudes, the extent of other state-level tobacco control policies, or exposure to tobacco control media campaigns (Schmidt et al., 2018; Lee et al., 2016) could influence the support, success, and sustainability of various tobacco control policies, including Tobacco 21, over time.
Evidence suggests that Tobacco 21 policies could prevent or delay tobacco product initiation and use by adolescents and young adults (Institute of Medicine, 2015). The Institute of Medicine (IOM) concluded that raising the minimum age of sale for tobacco products to 21 years would have the greatest impact on youth aged 15 to 17 (Institute of Medicine, 2015), as most underage users obtain tobacco products through social sources (Pokorny et al., 2006) and such policies may substantially increase barriers to youth access (Institute of Medicine, 2015). Tobacco 21 policies can reduce the likelihood that individuals with legal access to tobacco products would interact with and provide tobacco products to school-aged youth, as may be the case with some high school students in jurisdictions where the legal minimum age of sale is 18 years (Institute of Medicine, 2015). In Needham, MA, the first U.S. community to pass Tobacco 21 legislation (effective 2005), a significant decline in youths’ current smoking and access to cigarettes in the retail environment was observed immediately following policy adoption relative to surrounding communities (Kessel Schneider et al., 2016). Additionally, California’s Tobacco 21 policy resulted in widespread retailer conformity, high retailer awareness and support, and a significant reduction in illegal tobacco sales to youth (Zhang et al., 2018). Local-level Tobacco 21 policy effects also may be observed for those aged 18–20 years; sub-state Tobacco 21 policies had resulted in a statistically significant reduction in smoking among 18 to 20 year-olds residing in areas where policies were implemented compared to those living in areas without policies (Friedman and Wu, 2019). However, adequate policy enforcement and monitoring of retailer compliance is essential to achieving the full benefits of Tobacco 21 policies (Macinko and Silver, 2018).
State governments typically have the authority to raise the minimum tobacco purchase age above the national level (Public Health Law Center, Tobacco Control Legal Consortium, 2016). However, local-level policies may be impacted by preemption, which occurs when higher levels of government (e.g., the state) prevent the authority of lower levels (e.g., local government) to pass laws on a certain issue (Public Health Law Center, Tobacco Control Legal Consortium, 2016). Between 2005 and November 2019, > 500 localities, including major U.S. cities such as Boston, Chicago, New York City, San Francisco, and Washington D.C., implemented Tobacco 21 policies (Campaign for Tobacco-Free Kids, 2019); most local-level policies were enacted after 2014 (University of Missouri – Columbia, Missouri Tobacco Control Research Center, 2018). During 2016–2019, statewide policies were enacted in 16 states, while at least two other states had adopted legislation with future enactment dates into 2020, indicating that progress toward Tobacco 21 policies was occurring at both the local and state levels (Campaign for Tobacco-Free Kids, 2019). Furthermore, a federal law was enacted on December 20, 2019 that raises the minimum age of sales of tobacco products from 18 to 21 years nationwide. This law requires the FDA to publish a final rule updating the current age of sale regulations within 180 days and does not preempt state or local entities from passing or enforcing their own age restriction laws, including over 21 years, within their jurisdictions (116th U.S. Congress, 2019). However, states and communities may continue to pass or update their own policies to align with the federal law to ease enforcement efforts and provide clarity and consistency with the federal policy.
Four states had previously raised the minimum age of sale for tobacco products to 19 years (Alaska, Alabama, New Hampshire, and Utah) (Centers for Disease Control and Prevention, n.d.), although Utah further passed a Tobacco 21 policy effective in 2020 (Campaign for Tobacco-Free Kids, 2019). According to the IOM, a minimum age of sale of 19 years would result in a lower impact on youth initiation rates compared to a policy setting the age of sale to 21 years, as it would not reduce the likelihood of social source availability in high schools (Institute of Medicine, 2015). Public support is similar, or possibly lower, for raising the age of sale to 19 years compared to age 21 years among U.S. adults (Lee et al., 2016). Furthermore, Tobacco 21 policies may simplify enforcement efforts by dovetailing with those for alcohol, given the consistent minimum age of sale for these substances (Institute of Medicine, 2015).
This paper is subject to some limitations. First, participants are drawn from an Internet-based panel, which may have limited generalizability compared to traditional population-based surveys. Second, the question assessing Tobacco 21 policy favorability changed slightly between 2015 and 2016, which may limit comparability over time. Finally, information about where respondents live was not available beyond their state of residence. Although the majority of Tobacco 21 policies in 2017 were implemented at the local level, favorability could not be compared among respondents living in locations with and without Tobacco 21 policies.
5. Conclusion
Sustained and high favorability toward Tobacco 21 policies was observed among U.S. adults during 2014–2017. As part of a comprehensive tobacco control program, states and localities could support the enforcement and implementation of Tobacco 21 policies to prevent or delay tobacco use among young people, thereby reducing the long-term health burden attributed to tobacco use in the United States.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Authors AG, RGK, AJ, and MT conceptualized and designed the study and critically reviewed and revised the manuscript. Author AG completed the statistical analyses and drafted the initial manuscript.
Portions of this article (2017 data) were previously presented at the 2018 Society for Research on Nicotine and Tobacco (SRNT) meeting.
Financial disclosures and conflicts of interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. No conflicts of interest were reported by the authors of this paper.
References
- Campaign for Tobacco-Free Kids, 2019. States and localities that have raised the minimum legal sale age for tobacco products to 21. https://www.tobaccofreekids.org/assets/content/what_we_do/state_local_issues/sales_21/states_localities_MLSA_21.pdf, Accessed date: 24 June 2019.
- Centers for Disease Control and Prevention State Tobacco Activities Tracking and Evaluation (STATE) system. custom report. https://nccd.cdc.gov/STATESystem/rdPage.aspx?rdReport=OSH_State.CustomReports, Accessed date: 24 June 2019.
- Friedman AS, Wu RJ, 2019. Do local Tobacco-21 laws reduce smoking among 19 to 20 year-olds? Nicotine Tob. Res. 10.1093/ntr/ntz123. E-pub ahead of print (July 26, 2019). [DOI] [PubMed]
- 116th U.S. Congress, 2019. Further Consolidated Appropriations Act, 2020, H.R. 1865.
- GfK KnowledgePanel ®: a methodological overview. https://www.gfk.com/fileadmin/user_upload/dyna_content/US/documents/KnowledgePanel_-_A_Methodological_Overview.pdf, Accessed date: 24 June 2019.
- Glover-Kudon R, Plunkett E, Lavinghouze R, Trivers KF, Wang X, Hu S, Homa DM, 2019. Association of peer influence and access to tobacco products with U.S. Youths’ Support of Tobacco 21 Laws, 2015. J. Adolesc. Health 65 (2), 202–209. 10.1016/j.jadohealth.2018.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine, 2015. Public health implications of raising the minimum age of legal access to tobacco products. The National Academies Press, Washington, DC. [PubMed] [Google Scholar]
- Kessel Schneider S, Buka SL, Dash K, Winickoff JP, O-Donnell L, 2016. Community reductions in youth smoking after raising the minimum tobacco sales age to 21. Tob. Control 25 (3), 355–359. 10.1136/tobaccocontrol-2014-052207. [DOI] [PubMed] [Google Scholar]
- King BA, Jama AO, Marynak KL, Promoff GR, 2015. Attitudes toward raising the minimum age of sale for tobacco among U.S. adults. Am. J. Prev. Med 49 (4), 583–588. 10.1016/j.amepre.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JGL, Boynton MH, Richardson A, Jarman K, Ranney LM, Goldstein AO, 2016. Raising the legal age of tobacco sales: policy support and trust in government, 2014–2015, U.S. Am. J. Prev. Med 51 (6), 910–915. 10.1016/j.amepre.2016.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macinko J, Silver D, 2018. Impact of New York City’s 2014 increased minimum legal purchase age on youth tobacco use. Am. J. Public Health 108 (5), 669–675. 10.2105/AJPH.2018.304340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nayak P, Pechacek TF, Slovic P, Eriksen MP, 2017. Regretting ever starting to smoke: results from a 2014 national survey. Int. J. Environ. Res. Public Health 14 (4), 390. 10.3390/ijerph14040390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokorny SB, Jason LA, Schoeny ME, 2006. Youth supplying tobacco to other minors: evaluating individual and town-level correlates. J. Youth Adolesc 35 (5), 704–714. 10.1007/s10964-006-9030-0. [DOI] [Google Scholar]
- Public Health Law Center, Tobacco Control Legal Consortium. Tips and Tools: Raising the Minimum Legal Sale Age for Tobacco and Related Products. http://www.publichealthlawcenter.org/sites/default/files/resources/phlc-Tobacco-21-Tips-Tools-2016.pdf October 2016. Accessed June 24, 2019. [Google Scholar]
- Schmidt AM, Kowitt SD, Myers AE, Goldstein AO, 2018. Attitudes toward potential new tobacco control regulations among U.S. adults. Int. J. Environ. Res. Public Health 15 (1), E72. 10.3390/ijerph15010072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, 2012. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, Atlanta, GA. [Google Scholar]
- U.S. Department of Health and Human Services, 2016. E-Cigarette Use Among Youth and Young Adults. A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center of Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, Atlanta, GA. [Google Scholar]
- University of Missouri – Columbia, Missouri Tobacco Control Research Center. T21 Communities – September 30, 2018: US Communities With Tobacco21 Ordinances [Electronic Mailing List Message]. [Google Scholar]
- Winickoff JP, McMillen R, Tanski S, Wilson K, Gottlieb M, Crane R, 2016. Public support for raising the age of sale for tobacco to 21 in the United States. Tob. Control 25 (3), 284–288. 10.1136/tobaccocontrol-2014-052126. [DOI] [PubMed] [Google Scholar]
- Zhang X, Vuong D, Andersen-Rodgers E, Roeseler A, 2018. Evaluation of California’s ‘Tobacco 21’ law. Tob. Control 27 (6), 656–662. 10.1136/tobaccocontrol-2017-054088. [DOI] [PMC free article] [PubMed] [Google Scholar]


