Abstract
Background:
Chinese women rarely undergo regular cervical screening. Women’s decisions about cervical screening may be influenced by their perception of the risk of cervical cancer. Therefore, understanding how women perceive the risk of cervical cancer, how personal risk factors are interpreted, and the influence of cultural issues on cervical screening behavior is important.
Objective:
The aim of this study is to understand cervical cancer risk perception and the role of personal risk factors as they influence screening behavior among Chinese women.
Method:
An exploratory qualitative research design was used. We conducted semistructured, in-depth interviews of 27 women in Changsha, a medium-size city in Hunan province, China.
Results:
Participants identified that cervical cancer had serious consequences, but they distanced themselves psychologically from the disease because they felt that “cervical cancer is a shameful and deadly disease.” Although women identified some of the risk factors for the disease, they had little specific knowledge of human papillomavirus infection, its association with cervical cancer, and the importance of cervical screening.
Conclusion:
This study contributes new knowledge to the understanding of cervical screening behavior within a specific social and cultural context. Better efforts should be made to educate Chinese women on the risk of cervical cancer and emphasize that effective cancer treatments are available and that there is a good chance of survival.
Implications for Practice:
Nurses working with Chinese women should ensure that the information they provide is culturally sensitive, particularly by acknowledging the normative beliefs of this population group.
Keywords: Cervical cancer, Cervical screening, Chinese women, Personal risk factors, Qualitative methods, Risk perception
Invasive cervical cancer remains one of the leading causes of cancer-related death in Chinese women.1 In China, the estimated number of cervical cancer cases was 78,400 in 2010 and is projected to reach 93500 in 2030.2 There is strong empirical evidence that high-risk, sexually transmitted types of human papillomavirus (HPV) are the main causal agent in cervical cancer development.3 Because HPV vaccine is not currently available in mainland China, cervical cancer screening (Papanicolaou test) remains the key strategy for prevention and early diagnosis of cervical cancer in that country. The incidence of cervical cancer and associated mortality has decreased dramatically owing to increased screening in the developed countries in the last 50 years.4,5 Guidelines from the Cancer Foundation of China recommends that women 21 years or older who have had sexual intercourse be screened.6 The frequency of screening is determined by the findings on each screening. The Cancer Foundation of China recommended that women undergo cervical smear test every 3 years if 1 previous cervical smear was normal and undergo smear every 5 to 8 years if 2 consecutive smears were normal. The Chinese government has developed several initiatives to provide gynecological examinations and cervical screening for married women. However, although data are limited, existing data suggest that Chinese women tend not to have regular cervical screening.7,8 A regional study in China demonstrated that only 10% of women residing in an urban district had received cervical cancer screening.9 Several studies have found that Chinese women tend to rate their risk for cervical cancer to be below average,10–12 which may be an influencing factor in women’s cervical screening decisions. Exploration of women’s perception of risk of cervical cancer is essential to understanding their subsequent screening behavior. Such an exploration would further inform programs for the promotion of cervical screening among Chinese women.
Theoretical Framework
Risk perception is defined as “an individual’s cognitive appraisal of the likelihood or probability of a harm or noxious event.”13(p102) Theories of health behavior claim that elevated levels of perceived risk and perceived severity alter people’s motivation to pursue preventive measures.13,14 The Protection Motivation Theory (PMT) (Figure) provides one of the most dominant accounts of the influence of an individual’s risk perception on his/her willingness to take protective measures.13 Early PMT models consisted of 3 components: the individual’s perceived magnitude of noxiousness of a depicted threat (severity), the probability of the threatened event’s actual occurrence (risk), and the efficacy of a protective response (response efficacy). Therefore, in the domain of cervical cancer prevention, protection behavior (eg, cervical screening) arises from the perception that cervical cancer is likely to occur (risk) and has serious consequences (severity), along with the belief that cervical cancer screening can effectively prevent the occurrence of cervical cancer (efficacy). Although the PMT model has received considerable empirical support, some studies also suggest that a fuller understanding of culture-related risk perception and screening behavior is needed.
Figure.
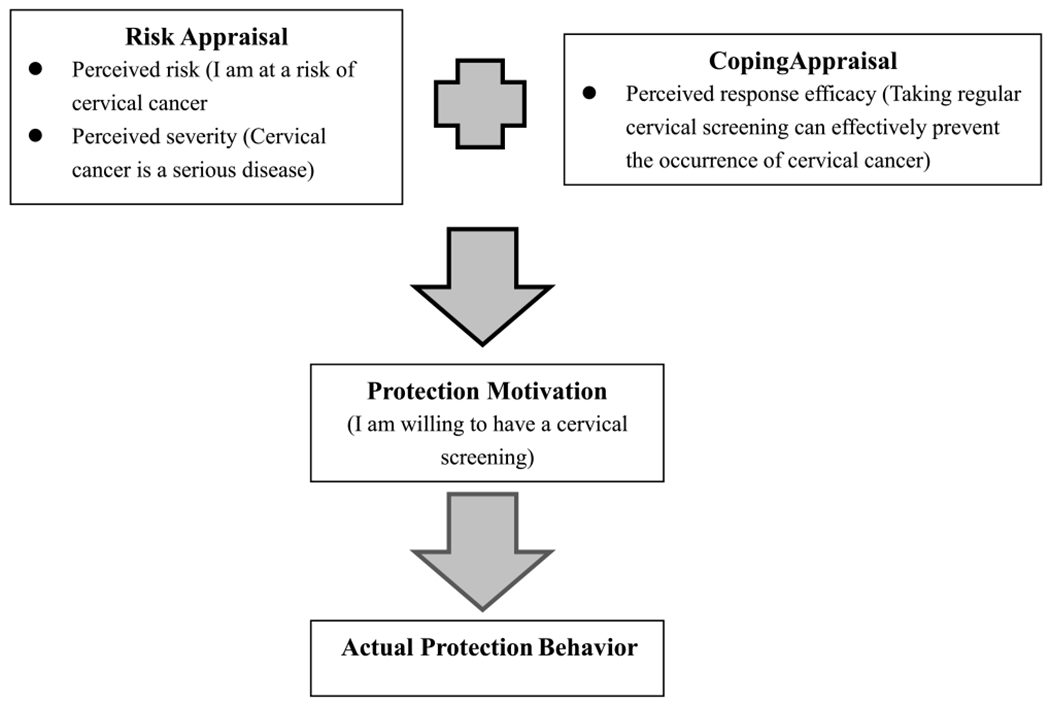
Protection motivation theory.
Background
Although multiple studies have explored risk perception of cervical cancer and screening utilization, few focused on Chinese women in China.10,15 Many studies have discussed risk perception of cervical cancer and screening utilization using a survey approach.16,17 However, these quantitative measurements have not adequately apprehended individuals’ complex feelings and perceptions about their cancer risk.18 A few qualitative studies have explored risk perception of cervical cancer and screening behavior. Ackerson et al19 reported that African American women who perceived a low risk of cervical cancer tend not to obtain a screening. Social influence from family and physicians was also suggested to influence screening attendance. McMullin et al20 conducted semistructured interviews with 20 Mexican immigrant women in the United States. They determined that cultural beliefs about cervical cancer—including associating cervical cancer risk with “unwise” sexual behavior and relying on symptoms to initiate screening behavior—played important roles in the decision of Latina immigrants to receive screening. Goldman and Risica21 conducted a study with Dominicans and Puerto Ricans in the United States and found that women attributed cervical cancer risk to carelessness or fatalism about healthcare and sexual behavior.
It has been suggested by previous studies that a fuller understanding of risk perception and screening uptake would be achieved by greater attention to social motivational processes and culture-related beliefs.16,21 In their survey of 167 Chinese women, Gu and colleagues10,15 suggested that cultural context not only had a significant effect on the way women perceive the risk of cervical cancer but also that it may contribute to a decision not to participate in cancer screening or a delay in participation.22 First, Chinese women’s perception of the risk of cervical cancer incorporates their cultural understanding of health.10,12 Chinese cultural beliefs about the body, health, and illness are conceptualized in a different way than in Western culture. The previous study suggests that traditional Chinese cultural views may include several constructs such as fatalism, a hot-cold balanced diet, conformity with nature, modesty, and self-care to avoid a medical visit.23 Chen24 described perceptions of disease prevention and health promotion among Chinese Americans. In Chen’s model, health is viewed holistically, with the ultimate goal of harmonizing the body with the environment. Second, a positive view of the efficacy of Chinese herbal medicine and a preference for using Chinese herbs over Western medicine has been identified in elderly Chinese cancer patients.25,26 These values may keep Chinese individuals from seeking help, such as regular screening, through Western medicine.25,27 Last, sexual relations in Chinese culture are regarded as necessary for achieving harmony with the universe, through the unity of interaction of yin (representing female) and yang (representing male).28,29 Chinese women tend to associate cervical cancer risk with immodesty or sexually inappropriate behavior, and this belief has been identified as a barrier to women taking part in cervical screening.30 Therefore, understanding the values and beliefs regarding sexual behavior among Chinese women is essential to fully understanding cultural influence on Chinese women’s attitudes toward cervical cancer risk and subsequent screening behavior. Further studies are needed to obtain a better insight into how women perceive cervical cancer risk and how personal risk factors are interpreted and whether these factors influence subsequent utilization of screening services within the Chinese cultural context.
The Study
Aim
The aim of this study is to understand the perception of cervical cancer risk and the role of personal risk factors as they influence screening behavior among women in Changsha, Hunan province, China.
Design
An exploratory qualitative research method was used in this study, which was a part of a large-scale mixed-methods study on Chinese women’s cervical screening behavior published in other papers.10,31
Participants
Chinese women aged 25 to 50 years were recruited for this project. Inclusion criteria were being sexually active (married or with a sexual partner) and willingness to share with the researcher their perceptions and feelings about the risk of cervical cancer. We purposively selected participants with a different levels (low, neutral [neither high nor low], and high) of risk perception of cervical cancer in the previous quantitative study. During the in-depth interview, study participants were asked to discuss their perceived risk and their risk factors for cervical cancer, their previous cervical screening experience, and their decision to take a screening test. A total of 27 women were interviewed, of which 11 were nonscreened (40.7%) and 16 were screened (59.3%). Of the 27 participants, 1 woman (3.7%) perceived a high risk of cervical cancer, 11 (40.7%) perceived a neutral risk, and 15 (55.6%) perceived a low risk.
Data Collection
The study was conducted in Changsha, China, the capital city of Hunan province. The study was approved by the institutional review boards of all the involved institutions. Female employees at 2 drugstores and 2 supermarkets were recruited. A study information sheet was given, and written consent was obtained before the in-depth interview. All the interviews were audio-taped. Both the time and place of interview were selected by the study participants. Semistructured, in-depth interviews were used to collect information from the participants about their perception of cervical cancer risk and personal risk factors. The interview schedule was developed by the researcher with information gained from a related project on Chinese women’s cervical screening behavior and from related literature.32 The interview schedule was tested on 4 women and revised accordingly. The revised schedule was then critically examined by a panel of experts consisting of 2 gynecologists and 2 senior researchers in qualitative study who identified any poorly worded or offensive questions or questions revealing the researcher’s own biases or personal values.33 Topics were arranged in an order appropriate for the purpose and included the use of prompts to ensure data consistency. The interviews were conducted in Mandarin by the first author. To ensure active inquiry and successful data collection, the interview included probing questions, which guided the participants to focus on the topic and helped them to explain their earlier answers in detail. Interviews took approximately 60 minutes (range, 35–85 minutes).
Data Analysis
The audio recordings of the in-depth interviews were transcribed verbatim in Chinese. Then, content analysis was used to analyze the data, with the researcher and an assistant coding and categorizing the first 4 transcripts independently. Subsequently, 2 researchers met and discussed the coding and categories to reconcile any discrepancies. Modifications were then made to provide the final consensus for the themes and categories that best described each response.34 Finally, the remaining 23 transcripts were coded and categorized. The data analysis also involved a comparison of the similarities and differences in themes and category between the screened and nonscreened women. The key quotes were then translated into English.
Results
The sociodemographic characteristics and sexual history of 27 participants are shown in the Table. The mean age of the participants was 32.3 years, and the ages ranged from 25 to 46 years. Most of the women were in paid employment (96.3% in full-time employment), were married (88.9%), had at least 1 child (77.8%), and had no family history of cancer (88.2%). Of the participants, 82% had a monthly household income of more than 2000 RMB (~ US$293). A substantial proportion (81.5%) of the participants reported that they first had sexual intercourse at the approximate age of 20 years, and 74.1% reported having had only 1 sexual partner.
Table.
Sociodemographic Characteristics, Sexual History, and Perceived Risk of Cervical Cancer of the Participants (n = 27)
| All (n = 27) | Not Screened (n = 11) | Screened (n = 16) | |
|---|---|---|---|
| Background characteristics | |||
| Age, y | |||
| 25–35 | 19 (70.4) | 9 (81.8) | 10 (62.5) |
| 36–50 | 8 (29.6) | 2 (18.2) | 6 (37.5) |
| Education level | |||
| Junior secondary or below | 2 (7.4) | 1 (9.1) | 1 (9.1) |
| Secondary graduate | 16 (59.3) | 7 (63.6) | 9 (56.3) |
| College or above | 9 (33.3) | 3 (27.3) | 6 (37.5) |
| Currently in paid employment | |||
| No | 1 (3.7) | 0 (0.0) | 1 (6.3) |
| Yes | 26 (96.3) | 11 (100.0) | 15 (93.8) |
| Monthly household income, RMB | |||
| <2000 | 4 (14.8) | 2 (18.2) | 2 (12.5) |
| 2000–2999 | 11 (40.7) | 5 (45.5) | 6 (37.5) |
| 3000–4999 | 4 (14.8) | 0 (0.0) | 4 (25.0) |
| ≥5000 | 3 (11.1) | 1 (9.1) | 2 (12.5) |
| Unsure | 5 (18.5) | 3 (27.3) | 2 (12.5) |
| Marital status | |||
| Single/divorced/widowed | 3 (11.1) | 3 (27.3) | 0 (0.0) |
| Married | 24 (88.9) | 8 (72.7) | 16 (100.0) |
| Children | |||
| None | 6 (22.2) | 6 (54.5) | 0 (0.0) |
| ≥1 | 21 (77.8) | 5 (45.5) | 16 (100.0) |
| Hysterectomy | |||
| No | 27 (100.0) | 11 (100.0) | 16 (100.0) |
| Cancer in relatives | |||
| No | 23 (85.2) | 9 (81.8) | 14 (87.5) |
| Yes | 4 (14.8) | 2 (18.2) | 2 (12.5) |
| Age at first intercourse | |||
| ≤20 y | 5 (18.5) | 3 (27.3) | 2 (12.5) |
| 21–30 y | 22 (81.5) | 8 (72.7) | 14 (87.5) |
| Number of sexual partners in the last year | |||
| 1 | 20 (74.1) | 8 (72.7) | 12 (75.0) |
| 2–3 | 3 (11.1) | 2 (18.2) | 1 (6.3) |
| Not willing to disclose | 4 (14.8) | 1 (9.1) | 3 (18.8) |
| Perceived risk of cervical cancer | |||
| High | 1 (3.7) | 0 (0) | 1 (6.3) |
| Neutral | 11 (40.7) | 5 (45.5) | 6 (37.5) |
| Low | 15 (55.6) | 6 (54.5) | 9 (56.2) |
Data are presented as n (%).
In our study, the constructs specified in the PMT model provided a conceptual framework to further understand how Chinese women perceived the risk of cervical cancer and how these perceptions influenced screening behavior. As shown in the Figure, the present study focused on the 2 main constructs of the PMT model, including perceived severity and perceived risk of cervical cancer, and the influence of these 2 constructs on cervical screening behavior. Categories under these 2 main constructs emerged from the interview data. The influence of response efficacy in the PMT model is not discussed in this article.
Perceived Seriousness of a Diagnosis of Cervical Cancer
The women’s perceptions of the seriousness of a diagnosis of cervical cancer were influenced by their personal experiences of their family members or friends who had had cervical cancer and died from the disease. Although most of the participants perceived cervical cancer as a deadly disease with no cure, a few expressed an optimistic view pertaining to cervical cancer, given that advanced treatments are now available. Here, we present their perception of the severity of cervical cancer in 4 categories: physical and psychological aspects, jeopardizing relationships, social pressure, and becoming a burden.
PHYSICAL AND PSYCHOLOGICAL ASPECTS
Some participants described the treatment trajectory for cervical cancer as a painful process and considered the diagnosis of cervical cancer as physically and psychologically devastating. They were reluctant to undergo treatment for cervical cancer and preferred death with dignity. Most also believed that high levels of anxiety, depression, and other emotional symptoms resulted from a diagnosis of cervical cancer. Cervical cancer was identified as a disease that entails tremendous stress, as well as emotional and physical suffering by both the patient and her family members. Women expressed an absence of confidence in treatment options for cervical cancer. A 32-year-old screened woman described it this way:
If a late stage of cervical cancer were detected in me, I would decline to have the operation, radiotherapy, and chemotherapy, since the final result is the same. I don’t care about having limited time to live. To me, what Mei Yangfang [a deceased movie star in Hong Kong who declined treatment] did is acceptable.
JEOPARDIZING SEXUAL AND MARITAL RELATIONSHIPS
Many participants described changes in sexual activity as the most important consequence of cervical cancer. For them, the invasive nature of the disease made it analogous to the body being devoured, which is an especially terrifying fate in Chinese culture. Participants believed that cervical cancer treatments would always lead to the removal of the uterus and ovaries. They believed that removal of the uterus would disable their sexual and fertility functions and would ultimately undermine their marital relations. As one 38-year-old screened woman said:
[Hysterectomy] influences family life, daily life, and the marital relationship. This most secret and precious organ [the uterus] makes you unique and gives you your feminine characteristics. If you have cancer and it’s necessary to remove the uterus, maybe you will lose both [uterus and ovaries]. Then you will have none of the distinctive traits of a woman anymore.
SOCIAL PRESSURE ASSOCIATED WITH CERVICAL CANCER
Some of the participants (n = 5) believed that cervical cancer was a particularly shameful disease compared with other types of cancer because it implied that the victim had been guilty of immoral sexual behavior. (In this context, the word immoral is synonymous with promiscuous.) One nonscreened participant expressed her concerns that even having a Papanicolaou test would be associated with promiscuity:
A cervical cancer patient is viewed as not good. She is viewed as dirty or disreputable. Leaving aside uterine cancer, even something like vaginitis or women’s infections, especially in the countryside, can provoke gossip. A woman may feel that she is under scrutiny because of having uterine cancer and cervical cancer.
BECOMING A FINANCIAL BURDEN ON THE FAMILY
The high cost of cervical cancer treatment was another dominant concern among these women. On average, it costs 40 million RMB per year to treat cervical cancer and breast cancer in Beijing, and this is a serious burden for the average Chinese.35 A non-screened 29-year-old woman typified the participants’ concerns:
[Cervical cancer] would definitely affect a family both financially and psychologically. If the woman is getting worse or in the late stage of the disease, the financial burden would be even more serious.
Perceived Risk of Cervical Cancer
We presented participants’ perceptions of risks associated with cervical cancer in 3 categories: understanding risk factors, perceived personal risk, and emotional response to risk.
UNDERSTANDING RISK FACTORS
A variety of general risk factors for cervical cancer were mentioned by the participants, including environment, dietary factors, stress, lifestyle behavior, and hereditary factors. Women were concerned about their basic health and took a variety of general preventive measures, such as eating a balanced diet, maintaining a healthy lifestyle, and avoiding environmental harm. All participants perceived sexual relations as constituting an important risk factor for cervical cancer. Specific risky behavior frequently cited by women included having unfaithful sexual partners, having too much sex (even with 1 partner), having sexual intercourse during menstruation, starting sexual activity too young, having an abortion, and taking contraceptive pills. Many of the women perceived that once they began to have sex, they would be likely to have an infection of some kind. Although the concept of infection was paramount in their perception of cervical cancer risk, they had little knowledge of the HPV as a precursor to cervical cancer. Carelessness was cited by many participants as a contributing factor for cervical cancer, largely in relation to not getting medical check-ups, not getting treatment for “women’s diseases,” or not going to the doctor when experiencing discomfort. Some participants further explained the concept that sexual risk factors and carelessness contributed to the possibility of infection and that an untreated infection would increase the risk of cervical cancer. One screened woman explained the concept this way:
It is mainly an issue of hygiene, and this is associated with sexual activity. If hygiene is not good, you are likely to get an infection. If the infection gets worse, it will develop into cancer. Cervicitis and cervical erosions can advance to a certain level, maybe moderate or serious; at the very beginning, it might be a precancerous lesion.
PERCEIVED PERSONAL RISK OF CERVICAL CANCER
In general, the participants gave a relatively low rating to their personal risk of cervical cancer. Some participants perceived low risk because they did not have any symptoms or did not have a family history of cervical cancer. Conversely, women with a family history of cervical cancer or any other cancer felt at increased risk. However, these women also believed that the increased risk could be offset, as they had no physical signs or symptoms themselves. This 29-year-old drugstore employee (non-screened) with a family history of cancer justified her perceived risk by saying:
Risk is related to family history. The doctor also said that. That means I am at a disadvantage. But I am 29 years old, nearly 30, and at present, I have no symptoms.
Only 1 participant perceived a higher risk compared with other women her age as she had received an abnormal smear result and had been recommended to have cytological surveillance as well as referral for colposcopy, which was confirmed to be an infection rather than cervical intraepithelial neoplasia.
Although the participants perceived sexual activity as an important risk factor for cervical cancer, those participants with a faithful sexual partner did not perceive themselves to be at risk for cervical cancer because neither they nor their spouses were involved in promiscuous sexual behavior. After the discussion of sexual risk factors, other participants stated that they were previously unaware of the role of the male partner in the development of cervical cancer.
EMOTIONAL RESPONSES TO CERVICAL CANCER RISK
Women described the emotional responses they associated with cervical cancer. These included fear of suffering from and dying of cancer, anxiety over test results, and pain from the test itself. Some of them said that fear of cervical cancer and death was the main driving force for them to have a Papanicolaou test test. Some participants indicated that anxiety and fear over screening results were powerful barriers for the screening participation. Many participants felt that a 3-year interval between smear tests was too long, and so the tests should be done every year or even every 6 months. A 30-year-old screened woman described how she feared a diagnosis of cervical cancer after she had received a positive smear result:
At that time, for sure it was terrible. If the report from the cancer hospital confirmed that it was cancer, what would I say? Then I suddenly got depressed. And I couldn’t be sure what I could do or how to face the reality. If it was true, what about my future life? What about the treatment?
Cervical Screening Behavior
Most of the screened women in our study obtained cervical screening service as part of a general well-woman examination organized by the community or the workplace.31 Data from the in-depth interviews revealed that perceived personal risk of cervical cancer, in itself, was not a sufficient motivator for screening behavior. Importantly, a personal connection to cervical cancer risk—rather than a perceived personal risk—served as a principal driver of women’s motivation to undertake screening.
Participants described uptake of cervical screening as a response to a cancer experience of friends or family members. They also relied on information on cervical cancer/cervical screening from mass media. They were motivated to get a screening because they did not want their families to go through the physical or emotional pain experienced by their friend or relative. These women reported that they felt strongly that the chief purpose of taking a screening test, for them, was to get the reassurance that a negative result would provide. As a 37-year-old screened woman said:
The TV program reported that even some young women had cancer, either cervical cancer or another type of cancer. After hearing that, I felt panicked, so I decided to get a check-up. Anyway, as a woman, I’ve witnessed this disease with friends of mine. Some of them had to get an operation to remove their uterus because of cervical cancer… But first of all, I knew I needed to get a check-up immediately to see if I had this disease.
Discussion
Although the participants believed that cervical cancer had serious consequences, they did not perceive themselves to be at risk for the disease. Indeed, our study reveals a discrepancy between the perceptions of severity and risk. This is because the perception of risk is constructed within a social and cultural context in which cervical cancer is considered a shameful and deadly disease. It follows from this that a woman’s perception of a high risk of cervical cancer holds an implication about her modesty and moral behavior. Not surprisingly, women were reluctant to explicitly claim that they considered themselves to have a high risk of cervical cancer. In this study, we found that cultural views about cervical cancer can arouse anxiety, and this anxiety could lead to behavioral responses such as avoidance of screening and even shunning of information about the disease and preventive measures.36
Our study could not establish a causal relationship between risk perception of cervical cancer and screening behavior because of the retrospective nature of the study. Indeed, screened women and nonscreened women in our study did not demonstrate a difference in risk appraisal variables (eg, perceived risk and perceived severity). This finding differs from the hypothesis of the PMT model.13 Empirical study also supports risk appraisal as a major factor in determining a woman’s likelihood to take part in cervical screening.14,37 It should be noted that, in our study, women’s generally low estimation of their own risk of developing cervical cancer could undermine the relationship between risk appraisal factors and screening behavior. Indeed, a number of controversial issues and criticisms of the PMT model have been raised by different authors. Some empirical studies suggest that it is questionable whether a high-risk appraisal is a sufficient condition for behavior modification.38,39 The meta-analytic review of Milne and colleagues40 showed that risk appraisal was a poor predictor of health-related behavior. Furthermore, high risk perception does not just predict desirable, preventive behavior but in fact can also predict undesirable behavior such as an avoidance response, resulting from a denial of the threat or a decision to avoid any information concerning the disease.41,42 Fear associated with disease risk could have a detrimental effect on prevention by inducing maladaptive coping, specifically defensive avoidance.42 A fear of finding something wrong has also been cited as a key obstacle to cervical screening among different populations including Hispanic, black, and Chinese women.30,43–45
However, women’s screening behavior cannot be considered outside the context of the risk of cervical cancer. The literature highlights that perceived risk and perceived severity combine to affect an individual’s choices.46 The effects of these variables should not be considered independently; if either the risk or the severity is perceived to be 0, a person will not be motivated to seek preventive care. Although women in this study did not explicitly claim that they were at risk of cervical cancer, more screened women (n = 6) described cervical screening behavior as a response to an experience of cancer through friends or family members and related information obtained from mass media than non-screened women (n = 2). This personal connection with cervical cancer risk served as a principal driver of women’s motivation to take a screening test. More important, this study found a variety of association between risk appraisal factors and cancer screening behavior that may reflect an ongoing process of change in the attitude of Chinese women to health prevention in the domain of cancer risk.
This study further revealed women’s beliefs about personal risk factors and cervical cancer. The results agree strongly with another study of Latina American women20 showing that women perceived a variety of sexual risk factors contributing to gynecological infection and that they believed that untreated infection could lead to cervical cancer. Interestingly, this concept, shared by both Latina and Chinese women, is consistent with the biomedical model of risk factors for cervical cancer.20 However, women in the present study demonstrated little specific knowledge of HPV infection and its association with cervical cancer. This finding concurred with previous studies in which women believed that infections caused cervical cancer but where none of them knew about HPV infection and its linkage to cervical cancer.19,20
Importantly, women’s beliefs concerning their personal risk factors may affect their motivation to engage in cervical cancer prevention activities, whether positively or negatively. For example, in this study, women believed that once they began a sexual relationship they could be at increased risk for an infection, which would then increase the risk of cervical cancer. Women who had become sexually active were therefore motivated to have a screening. Women’s awareness of the association between sexual risk factors and cervical cancer could motivate women to engage in primary prevention as well. They may use a natural approach to lowering the risk of the disease through adopting conservative attitudes toward sex.25,47 Finally, screened women emphasized more on not getting a health examination as a risk factor of cervical cancer than did nonscreened women. The importance of secondary prevention such as cervical screening was not recognized among nonscreened women. Inadequate knowledge of risk factors of cervical cancer, as shown in this study, may give women a false sense of security about their risk of cervical cancer and lead to a lower uptake of cervical screening.31
In this study, although women perceived that sexual relations constituted an important risk factor for cervical cancer, 88% of screened women and 64% of nonscreened women perceived that their sexual partner would not affect their risk of cervical cancer. This finding is parallel with the findings of previous studies,12 which indicated that women did not acknowledge the “male factor” in the development of cervical cancer. The low awareness of the male role in cervical cancer prevention may result from traditional patriarchal Chinese beliefs, in which women play a submissive and passive role in sexuality.48,49 Inequalities in power between the genders on issues of control and authority, and coercion within heterosexual relationships, often result in men having control over women’s sexual and reproductive decisions, such as when and how women will have sexual relations.49 Indeed, in this study, Chinese women’s attitudes to cervical screening included a concern for meeting male expectations of correct female behavior.41 Interrupting the transmission of HPV requires both men and women to be knowledgeable about the infection and the complexity of prevention strategies.50 The findings from this study identified significant barriers for women when negotiating with their male partners about taking preventive actions against cervical cancer, including participation in cervical screening.
Limitations
This study has several limitations. First, the small sample size and narrow demographic limit the generalizability of the findings. Most of the participants were in paid employment and living in urban area; therefore, more work is needed to explore perception of risk of cervical cancer among unemployed women in the urban communities, as well as among hard-to-reach groups in rural areas. Second, the researcher serves as clinician in the clinic where the study was conducted, which might have caused role conflict. Participants’ relationship to the researcher might have influenced their openness and truthfulness, and they may also have felt obliged to emphasize how “good” they had been by having regular smear tests.
Conclusion and Implications
This study contributes new knowledge to the understanding of cervical screening behavior within a specific social and cultural context and reveals the need for a fundamental and comprehensive change in the theoretical structure of cervical cancer care. It also increases understanding of the relationship between cervical cancer risk and preventive care from the perspective of Chinese women. The study reveals that Chinese women have only limited knowledge about the risk of cervical cancer, demonstrating an underestimation of personal risk.
Although the study does not support a causal relationship between perceived personal risk of cervical cancer and screening uptakes, Chinese women’s understanding of cervical cancer risk and the interaction between this understanding and subsequent preventive behavior can inform future programs for the promotion of cervical screening among this population. Given that some women intentionally distance themselves from cervical cancer risk, efforts to improve women’s risk perception of cervical cancer may not have an effect on their participation in screening. To mitigate the possible detrimental effect of affective conditions associated with cervical cancer risk—conditions such as worry, anxiety, and psychological distress—educational efforts should focus on creating messages to emphasize that effective cancer treatments are available and that there is a good chance of survival.
In this study, personal risk factors associated with cervical cancer were viewed by Chinese women through the prism of their own culture. Nurses working with Chinese women should ensure that the information they provide is culturally sensitive, particularly by acknowledging the normative beliefs and cultural values of that population group. Health policymakers from mainland China should also pay special attention to these issues, even though it is fortunate that at least some of women were motivated enough by the organized health program as a whole. Programs that explicitly recognize and incorporate the equal validity of the cultural and social components may promote cervical screening.
ACKNOWLEDGMENTS
The authors thank Prof Sheila Twinn for her contribution to this research. Special thanks are given to Professor Nancy Reynolds and Professor Angelo Alonzo for their constructive advice in completion of this manuscript.
This research was funded by a Chia Family Health Fellowship Award (primary investigator: Can Gu), contract grant number 2012CF01, and a China Medical Board Nursing Faculty Research Grant (primary investigator: Can Gu), contract grant number 13-168-201411.
Footnotes
The authors have no conflicts of interest to disclose.
Contributor Information
Can Gu, Department of Medicine, Xiangya Hospital, Central South University, Changsha, P.R. China; Xiang-Ya School of Nursing, Central South University, Changsha, P.R. China.
Wei-Ti Chen, School of Nursing, Yale University, West Haven, Connecticut.
Qiue Zhang, The Affiliated Cancer Hospital of Xiangya School of Medicine, Central South University, Changsha, P.R. China.
Ka Ming Chow, The Nethersole School of Nursing, The Chinese University of Hong Kong, Hong Kong.
Jianzhen Wu, Third Xiangya Hospital, Central South University, Changsha, P.R. China.
Lijian Tao, Department of Medicine, Xiangya Hospital, Central South University, Changsha, P.R. China.
Carmen W.H. Chan, The Nethersole School of Nursing, The Chinese University of Hong Kong, Hong Kong.
References
- 1.GLOBOCAN 2008. Fast stats: women, 2010. http://globocan.iarc.fr/factsheets/populations/factsheet.asp?uno=900#women. Accessed December 10, 2010.
- 2.Ferlay J, Bray F, Pisani P, et al. Globocan 2000: Cancer Incidence, Mortality and Prevalence Worldwide, Version 1.0 Lyon, France: IARC Press; 2001. IARC Cancerbase No. 5. [Google Scholar]
- 3.Bosch FX, Lorincz A, Muñoz N, et al. The causal relation between human papillomavirus and cervical cancer. J Clin Pathol. 2002;55(4):244–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Australian Institute of Health and Welfare. Cervical screening in Australia 2003-2004. http://www.aihw.gov.au/publications/index.cfm/title/10359. Accessed January 23, 2007.
- 5.NHS Cancer Screening Programme. NHS cervical screening, 2009. https://www.cancerscreening.nhs.uk/cervical/index.html. Accessed July 12, 2010.
- 6.Cancer Foundation of China. Guideline for early detection and treatment of cervical cancer in China, 2007. http://www.chinacancernet.org.cn/download/??????????.pdf. Accessed February 2, 2015.
- 7.Hislop TG, Teh C, Lai A, et al. Pap screening and knowledge of risk factors for cervical cancer in Chinese women in British Columbia, Canada. Ethn Health. 2004;9:267–281. [DOI] [PubMed] [Google Scholar]
- 8.Wang X, Fang C, Liu A, Ma GX. Evidence-based intervention to reduce access barriers to cervical cancer screening among underserved Chinese American women. J Womens Health. 2010;19(3):463–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tu D, Wang Q, Zhang R, et al. Analysis on opportunity screening of cervical cancer in Longgang Street, Longgang District, Shenzhen. China Cancer. 2011;20(12):903–905. [Google Scholar]
- 10.Gu C, Chan CWH, Twinn SF, et al. The influence of knowledge and perception of the risk of cervical cancer on screening behaviour in mainland Chinese women. Psycho-Oncology. 2012;21(12):1299–1308. [DOI] [PubMed] [Google Scholar]
- 11.Hou S Barriers to Pap screening among Chinese women in precontemplation stage—a qualitative approach. Paper presented at: English Qualitative Health Research Conference; April 4–6, 2002; Banff, Alberta, Canada. [Google Scholar]
- 12.Twinn S, Holroyd E, Adab P. The influence of intrinsic and extrinsic factors on uptake rates for cervical screening: a comparison of Hong Kong Chinese women and practitioners. Hong Kong Med J. 2006;12(suppl 2):S19–S21. [Google Scholar]
- 13.Rogers RW. A Protection Motivation Theory of fear appeals and attitude change. J Psychol. 1975;91(1):93–114. [DOI] [PubMed] [Google Scholar]
- 14.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q 1988;15(2):175–183. [DOI] [PubMed] [Google Scholar]
- 15.Gu C, Chan CWH, Twinn S, et al. Chinese women’s motivation to receive future screening: the role of social-demographic factors, knowledge and risk perception of cervical cancer. Eur J Oncol Nurs. 2013;17(2):154–161. [DOI] [PubMed] [Google Scholar]
- 16.Abotchie PN, Shokar NK. Cervical cancer screening among college students in Ghana: knowledge and health beliefs. Int J Gynecol Cancer. 2009;19(3):412–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan CWH, Yang SB, Gu C, et al. Perception of cervical cancer risk and screening behaviour: a literature review. Int J Nurs Knowl. 2015;26(1):2–18. [DOI] [PubMed] [Google Scholar]
- 18.Slovic P, Finucane M, Peters E, et al. The affect of heuristic. In: Gilivich T, Griffin D, eds. Heuristics and Biases: The Psychology of Intuition Judgment. New York: Cambridge University Press; 2002:397–420. [Google Scholar]
- 19.Ackerson K, Pohl J, Low LK. Personal influencing factors associated with Pap smear testing and cervical cancer. Policy Polit Nurs Pract. 2008;9:50–60. [DOI] [PubMed] [Google Scholar]
- 20.McMullin JM, Alba ID, Chavez LR, et al. Influence of beliefs about cervical cancer etiology on Pap smear use among Latina immigrants. Ethn Health. 2005;10(1):3–18. [DOI] [PubMed] [Google Scholar]
- 21.Goldman RE, Risica PM. Perceptions of breast and cervical cancer risk and screening among Dominicans and Puerto Ricans in Rhode Island. Ethnicity and Disease. 2004;14(1):32–42. [PubMed] [Google Scholar]
- 22.Kwok C, Sullivan G, Cant R. The role of culture in breast health practices among Chinese-Australian women. Patient Educ Couns. 2006;64(1–3):268–276. [DOI] [PubMed] [Google Scholar]
- 23.Liang W, Wang JH, Chen MY, et al. Developing and validating a measure of Chinese cultural views of health and cancer. Health Educ Behav. 2008;35(3):361–375. [DOI] [PubMed] [Google Scholar]
- 24.Chen YL. Conformity with nature: a theory of Chinese American elders’ health promotion and illness prevention processes. Adv Nurs Sci. 1996;19(2):17–26. [DOI] [PubMed] [Google Scholar]
- 25.Liang W, Yuan EH, Mandelblatt JS, et al. How Chinese women view health and cancer screening? Results from focus groups and implications for intervention. Ethn Health. 2004;9:283–304. [DOI] [PubMed] [Google Scholar]
- 26.Simpson PB. Family beliefs about diet and traditional Chinese medicine for Hong Kong women with breast cancer. Oncol Nurs Forum. 2003;30:834–840. [DOI] [PubMed] [Google Scholar]
- 27.Hoeman SP, Ku YL, Ohl DR. Health beliefs and early detection among Chinese women. West J Nurs Res. 1996;18(5):518–533. [DOI] [PubMed] [Google Scholar]
- 28.Chan HYL, Chui YY, Chan CWH, et al. Exploring the influence of traditional Chinese medicine on self-care among Chinese cancer patients. Eur J Oncol Nurs. 2014; 18:445–451. [DOI] [PubMed] [Google Scholar]
- 29.Zhang K, Li D, Li H, et al. Changing sexual attitudes and behaviour in China: implications for the spread of HIV and other sexual transmitted disease. AIDS Care. 1999;11(3):581–589. [DOI] [PubMed] [Google Scholar]
- 30.Hou S, Lessick M. Cervical cancer screening among Chinese women: exploring the benefits and barriers of providing care. AWHONN Lifelines. 2002;6(4):349–354. [DOI] [PubMed] [Google Scholar]
- 31.Gu C, Chan CWH, Twinn SF. How sexual history and knowledge of cervical cancer and screening influence Chinese women’s screening behavior in Mainland China. Cancer Nurs. 2010;33(6):445–453. [DOI] [PubMed] [Google Scholar]
- 32.Hay J, Shuk E, Cruz G, et al. Thinking through cancer risk: characterizing smokers’ process of risk determination. Qual Health Res. 2005;15(8):1074–1085. [DOI] [PubMed] [Google Scholar]
- 33.Berg BL. Qualitative Research Methods for the Social Sciences. 6th ed. Boston, MA: Pearson Education; 2007. [Google Scholar]
- 34.Marshall C, Rossman GB. Designing Qualitative Research. 4th ed. Thousands Oaks, CA: Sage Publications; 2006. [Google Scholar]
- 35.Han L, Qi Q, Wang Z, et al. Current status and screening results of cervical or breast cancer. Chine J Health Manage. 2011;5(5):292–294. [Google Scholar]
- 36.Agurto I, Bishop A, Sanchez G, et al. Perceived barriers and benefits to cervical cancer screening in Latin America. Prev Med. 2004;39:91–98. [DOI] [PubMed] [Google Scholar]
- 37.Walsh JC. The impact of knowledge, perceived barriers and perceptions of risk on attendance for a routine cervical smear. Eur J Contracept Reprod Health Care. 2006;11(4):291–296. [DOI] [PubMed] [Google Scholar]
- 38.Blanchard CM, Reid RD, Morrin LI, et al. Does Protection Motivation Theory explain exercise intentions and behavior during home-based cardiac rehabilitation? J Cardiopulm Rehabil Prev. 2009;29(3):188–192. [DOI] [PubMed] [Google Scholar]
- 39.Hoque M, Ibekwe CM, Ntuli-Ngcobo B. Screening and perceived severity of cervical cancer among women attending Mahalapye district hospital, Botswana. Asian Pac J Cancer Prev. 2009;10:1095–1100. [PubMed] [Google Scholar]
- 40.Milne S, Sheeran P, Orbell S. Prediction and intervention on health-related behavior: a meta-analytic review of Protection Motivation Theory. J Appl Soc Psychol 2000;30:106–143. [Google Scholar]
- 41.Ruiter RA, Verplanken B, Kok G, et al. The role of coping appraisal in reactions to fear appeals: do we need threat information? J Health Psychol. 2003;8(4):465–474. [DOI] [PubMed] [Google Scholar]
- 42.Leung DYP, Wong EML, Chan CWH. Adapting Champion’s Breast Cancer Fear Scale to colorectal cancer: psychometric testing in a sample of older Chinese adults. Eur J Oncol Nurs. 2014;18:281–285. [DOI] [PubMed] [Google Scholar]
- 43.Austin L, Ahmad F, McNally MJ, et al. Breast and cervical cancer screening in Hispanic women: a literature review using the Health Belief Model. Womens Health Issues. 2002;12:122–128. [DOI] [PubMed] [Google Scholar]
- 44.Friedman LC, Webb JA, Weinberg AD, et al. Breast cancer screening: racial/ethnic differences in behaviors and beliefs. J Cancer Educ. 1995;10:213–216. [DOI] [PubMed] [Google Scholar]
- 45.Kwok C, Fethney J, White K. Mammographic screening practices among Chinese-Australian women. J Nurs Scholarsh. 2011;44(1):11–18. [DOI] [PubMed] [Google Scholar]
- 46.Weinstein ND. Perceived probability, perceived severity, and health-protective behavior. Health Psychol. 2000;19(1):65–74. [DOI] [PubMed] [Google Scholar]
- 47.Wang JH, Liang W, Chen MY, et al. Influence of culture and cancer worry on colorectal cancer screening in older Chinese American women. Ethn Dis. 2006;16:404–411. [PMC free article] [PubMed] [Google Scholar]
- 48.Chapman J, Estcourt CS, Hua Z Saving ‘face’ and ‘othering’: getting to the root of barriers to condom use among Chinese female sex workers. Sex Health. 2008;5(3):291–298. [DOI] [PubMed] [Google Scholar]
- 49.Tang C, Wong C, Lee AM. Gender-related psychosocial and cultural factors associated with condom use among Chinese married women. AIDS Educ Prev. 2001;13:329–342. [DOI] [PubMed] [Google Scholar]
- 50.Frazer IH, Cox JT, Mayeaux EJJ, et al. Advances in prevention of cervical cancer and other human papillomavirus-related diseases. Pediatr Infect Dis J. 2006;25(suppl):S65–S81. [DOI] [PubMed] [Google Scholar]


