Abstract
Background:
Women with disabilities are less likely to receive reproductive health counseling than women without disabilities. Yet, little is known about reproductive health counseling and concerns among women with congenital heart defects (CHD) and disabilities.
Methods:
We used population-based survey data from 778 women aged 19 to 38 years with CHD to examine contraceptive and pregnancy counseling and pregnancy concerns and experiences by disability status, based on six validated questions on vision, hearing, mobility, cognition, self-care, and living independently. Multivariable Poisson regression was used to examine adjusted prevalence ratios between disability status and each outcome, adjusted for CHD severity, age, race/ethnicity, place of birth (Arkansas, Arizona, Georgia), and insurance type.
Results:
Women with disabilities (n = 323) were 1.4 and 2.3 times more likely than women without disabilities (n = 455) to receive clinician counseling on safe contraceptive methods and avoiding pregnancy because of their CHD. Women with CHD and disabilities, compared to those without disabilities, were more likely to be concerned about their ability to have children (aPR = 1.2) and to have delayed or avoided pregnancy (aPR = 2.2); they were less likely to have ever been pregnant (aPR = 0.7). Associations differed slightly across specific disability types. All associations remained after excluding 71 women with chromosomal anomalies.
Conclusion:
Among women with CHD, reproductive counseling, concerns, and experiences differ by disability status.
Keywords: congenital heart defect, disability, contraceptive counseling, pregnancy
Introduction
Approximately half a million adolescent and adult women are living with congenital heart defects (CHD) in the United States.1 Women with CHD are at increased risk of pregnancy complications and adverse outcomes, although most will have healthy pregnancies,2 and pregnancy is contraindicated only among a small subset.3 Women with certain types of CHD also have unique contraceptive needs4; combined hormonal contraceptives (containing estrogen and progestin) may have unacceptable health risks for some women with CHD, such as those with pulmonary arterial hypertension or Fontan circulation.5
The 2018 American Heart Association/American College of Cardiology Guidelines for the Management of Adults with CHD recommends that clinicians counsel all women with CHD about their reproductive health, including contraception and pregnancy, soon after sexual maturity.6 Two small studies reported that 33% to 65% of women with CHD reported having a discussion with their provider about the risks of pregnancy7,8 and counseling on contraceptive use is also lacking.9
Over a third of women with CHD may have a disability.10 In general, women with disabilities are less likely to receive reproductive and contraceptive counseling from providers,11 but as likely to desire pregnancy.12 However, it is unknown what percentage of women with CHD and disability receive contraceptive and reproductive counseling and whether their rates of pregnancy are lower than women with CHD without disabilities. Therefore, the objectives of this analysis are to examine whether having a disability in general, and specific types of disabilities, are associated with receipt of reproductive health counseling and concerns among women with CHD.
Methods
Data for this analysis were from the Congenital Heart Survey To Recognize Outcomes, Needs, and well-beinG (CH STRONG).13 Individuals born between 1980 and 1997 with CHD according to the six-digit Centers for Disease Control and Prevention (CDC)-modified version of the British Paediatric Association (BPA) codes within the range 745–747 (with some exceptions for codes with low specificity for CHD) were identified through population-based birth defects surveillance systems with active case-finding methods in Arkansas (AR), Arizona (AZ), and metropolitan-Atlanta, Georgia (GA). Before recruitment, sites linked these individuals to their respective state death records through 2015 using probabilistic matching by date of birth, sex, and name; 9,312 individuals were not linked to a death record. Sites then found current contact information and mailed surveys to 6,943 eligible individuals.
From 2016 to 2019, 1,656 eligible individuals (54.0% female), or their proxies (e.g., parent), completed the CH STRONG survey, online or by paper (response rate among all eligible: 17.8%; response rate among those mailed a survey: 23.9%). Survey data were linked to birth defects surveillance system information. CH STRONG was approved by the Institutional Review Boards (IRB) of the CDC and the University of Arkansas for Medical Sciences. The University of Arizona relied on the CDC’s IRB.
The CH STRONG survey included questions on demographic characteristics, disability, reproductive health, and health care utilization. Survey respondents were asked a six-item set of Department of Health and Human Services Standard Disability Status Questions, the federal data standard for survey questions on disability.14 Specifically, participants were asked if they had serious difficulties with hearing, vision (even when wearing glasses), cognition (e.g., concentrating, remembering, or making decisions because of a physical, mental, or emotional condition), mobility (e.g., walking or climbing stairs), self-care (e.g., dressing or bathing), and living independently (e.g., doing errands alone because of a physical, mental, or emotional condition). We examined disabilities individually and dichotomized as none and one or more disability.
We examined six outcomes related to reproductive health counseling and experiences. The first three fell under contraceptive and pregnancy counseling. Survey questions asked “Has a doctor, nurse, or other healthcare worker ever…” (1) “talked with you about the safest type of birth control or contraception to use because of your heart problem?”; (2) “talked with you about special concerns about becoming pregnant because of your heart problem?”; and (3) “advised you to avoid pregnancy because of your heart problem?” The next three outcomes were related to pregnancy concerns and experiences.
Participants were asked, “How concerned are you about your ability to have children?,” with response options of not at all, not very, somewhat, and very concerned; “Have you ever delayed or avoided getting pregnant because of concerns about your heart problem?”; and “Have you ever been pregnant?” Respondents’ health and demographic characteristics derived from the birth defect surveillance system included CHD severity, age (based on date of birth and date of survey completion), place of birth, and presence of chromosomal anomalies; information from the survey included race/ethnicity, education, recent cardiology care, receipt of any health care in last 12 months, marital status, and proxy report.
We limited the analysis to individuals born female. We excluded from the analysis individuals missing information on variables of interest and compared characteristics of included to excluded females using chi square tests. Among the CH STRONG analytic sample of females, we examined prevalence of each of the six reproductive health outcomes (safe contraceptive counseling, clinician counseling on pregnancy, clinician advice to avoid pregnancy, concern about ability to have children, delayed or avoided pregnancy, and ever pregnant) by disability status (any/none) standardized to the birth year, maternal race/ethnicity, site, and CHD severity of the 4,515 eligible female population to reduce nonresponse bias.
We also examined differences in prevalence of reproductive health outcomes by each of the six disability types. Differences were assessed using chi-square tests. Using multivariable Poisson regression, we examined the associations between disability status (any/none) and each outcome adjusted for CHD severity, age, state of birth, race/ethnicity, and insurance type. In separate sensitivity analyses, we ran the same multivariable models after excluding individuals with proxy report, those with chromosomal anomalies, those without a cardiology visit in the past 5 years, and those without a health care visit in the past 12 months. We also stratified results by marital status.
Results
Of the 894 female CH STRONG respondents, 76 (8.5%) were missing data on reproductive health outcomes; of those with reproductive health information, 14 (1.7%) were missing data on disability; of women with information on reproductive health and disability, 26 (3.2%) were missing data on other variables of interest (Supplementary Table S1). Therefore, the final analytic sample included 778 (87.0%) females aged 19 to 38 years. Table 1 shows descriptive characteristics of the sample. Women with disabilities were more likely to have severe CHD, be nonwhite, have chromosomal anomalies, be born in AZ, have less education, have public insurance, and receive more recent cardiology care (p<0.05 for all). Overall, 41.5% of women with CHD reported one or more disabilities, with 10.9% reporting two or more disabilities. Overall, disability related to cognition was most common (31.0%), followed by living independently (22.3%), mobility (12.9%), self-care (6.8%), vision (5.5%), and hearing (4.8%).
Table 1.
Demographic and Health Characteristics of Women with Congenital Heart Defects, by Disability Status, CH STRONG, 2016–2019
| Characteristic levels | ≥1 disability |
No disability
|
Chi-Square
|
||
|---|---|---|---|---|---|
| N | Percent | N | Percent | p-value | |
|
| |||||
| Total | 323 | 455 | |||
| Age at survey completion | |||||
| 19–24 | 137 | 42.4 | 181 | 39.8 | 0.52 |
| 25–30 | 136 | 42.1 | 190 | 41.8 | |
| 31–38 | 50 | 15.5 | 84 | 18.5 | |
| CHD severity | |||||
| Nonsevere | 214 | 66.3 | 343 | 75.4 | 0.005 |
| Severe | 109 | 33.7 | 112 | 24.6 | |
| Race/ethnicity | |||||
| Hispanic | 39 | 12.1 | 36 | 7.9 | 0.04 |
| Multi/other | 23 | 7.1 | 30 | 6.6 | |
| NH black | 62 | 19.2 | 67 | 14.7 | |
| NH white | 199 | 61.6 | 322 | 70.8 | |
| Presence of chromosomal anomalies | |||||
| No | 262 | 81.1 | 445 | 97.8 | <0.001 |
| Yes | 61 | 18.9 | 10 | 2.2 | |
| Place of birth | |||||
| Arizona | 106 | 32.8 | 92 | 20.2 | <0.001 |
| Arkansas | 129 | 39.9 | 188 | 41.3 | |
| Georgia | 88 | 27.2 | 175 | 38.5 | |
| Education | |||||
| <High school | 38 | 11.8 | 12 | 2.6 | <0.001 |
| High school or equivalent | 136 | 42.1 | 68 | 14.9 | |
| >High school | 149 | 46.1 | 375 | 82.4 | |
| Insurance type | |||||
| Any private | 122 | 37.8 | 293 | 64.4 | <0.001 |
| Other, none, or unsure | 71 | 22 | 114 | 25.1 | |
| Public | 130 | 40.2 | 48 | 10.5 | |
| Receipt of health care in last 12 months | |||||
| No | 39 | 12.1 | 67 | 14.7 | 0.29 |
| Yes | 284 | 87.9 | 388 | 85.3 | |
| Most recent cardiology care | |||||
| ≤2 years | 177 | 54.8 | 180 | 39.6 | <0.001 |
| 3–5 years | 32 | 9.9 | 48 | 10.5 | |
| >5 years or never | 114 | 35.3 | 227 | 49.9 | |
| Proxy report | |||||
| Yes | 97 | 30 | 21 | 4.6 | <0.001 |
| No | 226 | 70 | 434 | 95.4 | |
CH STRONG, congenital heart survey to recognize outcomes, needs, and well-beinG; CHD, congenital heart defects.
Among women with CHD, those with disabilities, compared to those without disabilities, were 1.4 times more likely to have ever had a conversation with their provider about safe contraceptive methods (23.7% and 19.2%) and 2.3 times more likely to have received advice to avoid pregnancy because of their heart problem (18.3% and 8.2%; Fig. 1). Women with disabilities, compared to those without, were also 1.2 times more likely to report concern about their ability to have children (36.4% and 31.7%), 2.2 times more likely to have delayed or avoided pregnancy because of their heart (19.6% and 8.4%), and 0.7 times as likely to have ever been pregnant (30.0% and 39.1%; Fig. 2).
FIG. 1.
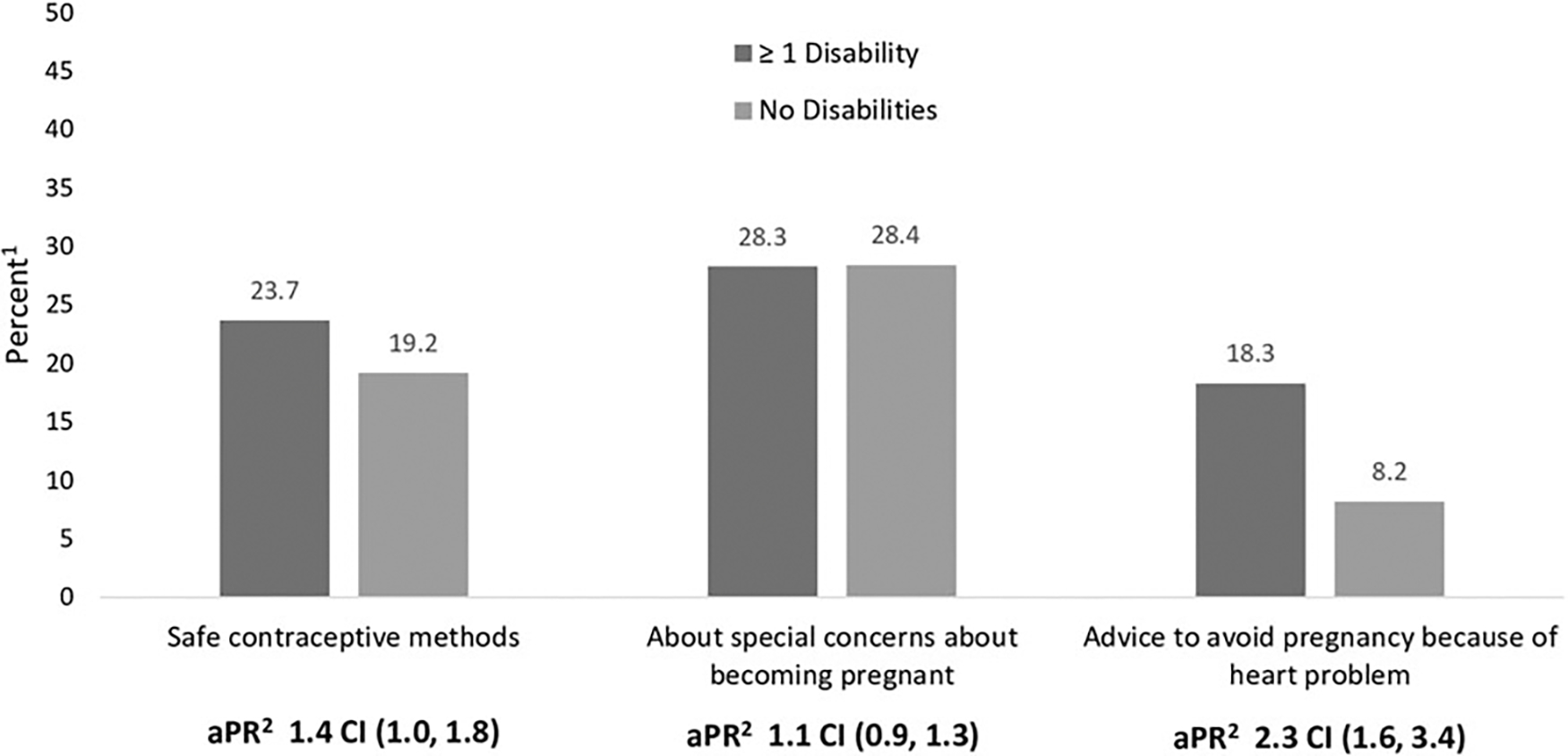
Receipt of clinician counseling on reproductive health issues among women with congenital heart defects, by disability status, CH STRONG, 2016–2019. 1Standardized to the birth year, maternal race/ethnicity, site, and CHD severity of the CH STRONG- eligible female population. 2Adjusted for state of birth, age, CHD severity, race/ethnicity, type of health insurance. aPR, adjusted prevalence ratio; CI, confidence interval; CH STRONG, Congenital Heart Survey To Recognize Outcomes, Needs, and well-beinG; CHD, congenital heart defects.
FIG. 2.
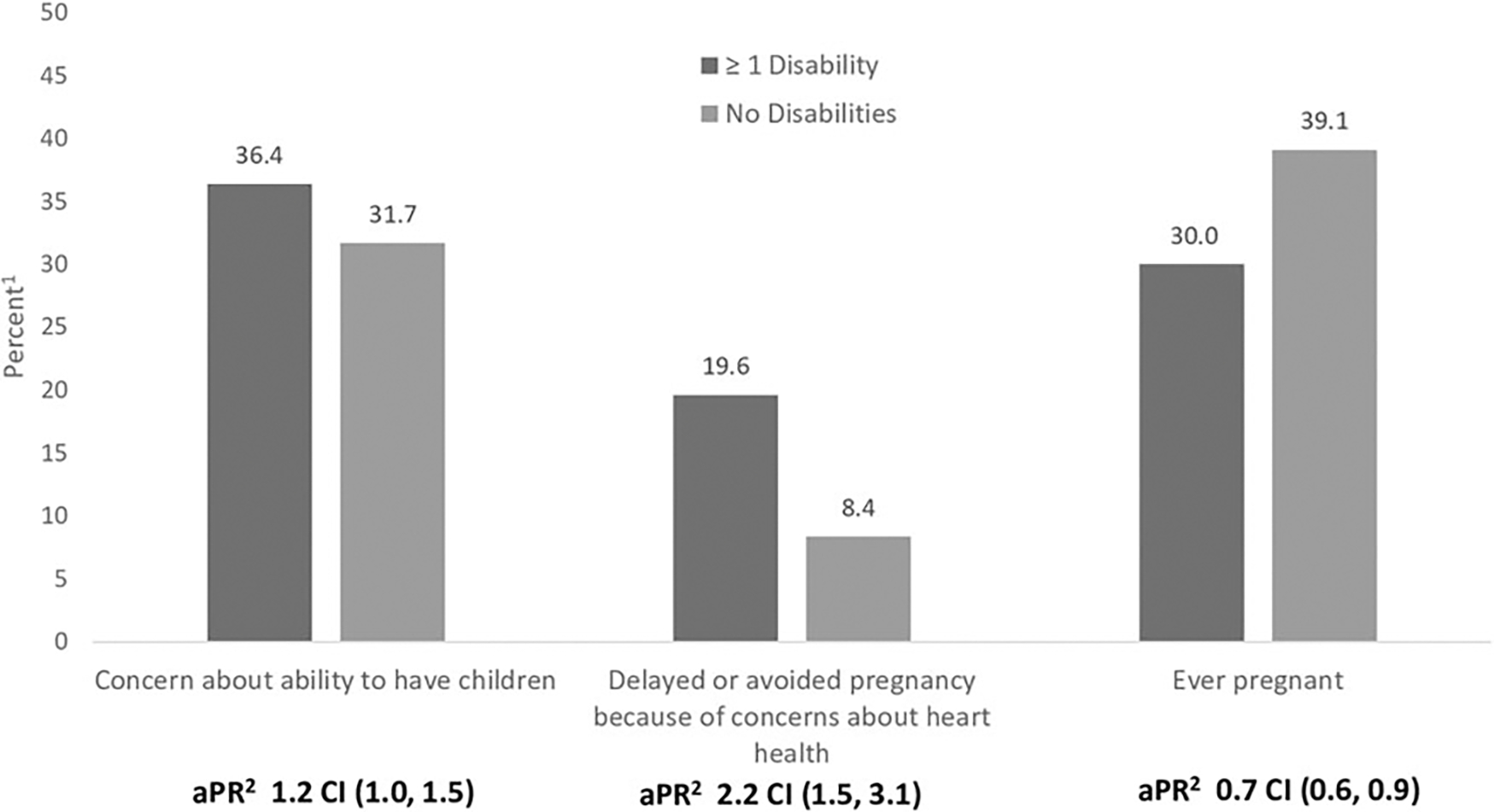
Report of reproductive health concerns and outcomes among women with congenital heart defects, by disability status, CH STRONG, 2016–2019. 1Standardized to the birth year, maternal race/ethnicity, site, and CHD severity of the CH STRONG- eligible female population. 2Adjusted for CHD severity, age, state of birth, race/ethnicity, type of health insurance.
Associations remained and sometimes increased in magnitude when analyses were limited to women who self-reported their survey responses, among women with no chromosomal anomalies, and among women who received health care in the past year and cardiology care in the past 5 years (Supplementary Tables S2A–S5B). Additionally, there were no differences in associations when stratified by marital status (Supplementary Tables S6A and S6B). However, in all sensitivity analyses, confidence intervals were wider due to lower sample size and reduced power.
Reproductive health outcomes also differed by disability type. Compared to women with CHD without the specific disability, the prevalence of clinician counseling on safe contraceptive methods was significantly elevated among women with vision disabilities and lower among women with self-care disabilities (Table 2). Prevalence of clinician counseling on special concerns about becoming pregnant was lower among women with disabilities related to self-care and living independently. Women with all disability types, except vision and self-care, had an elevated prevalence of receiving advice to avoid pregnancy, ranging from 18.2% to 27.3%.
Table 2.
Receipt of Clinician Counseling on Reproductive Health Among Women with Congenital Heart Defects, by Disability Type, CH STRONG, 2016–2019
| Disability type a | levels |
Type of clinician counseling received
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
Safe contraceptive methods
|
Special concerns about becoming pregnant
|
To avoid pregnancy because cf heart problem
|
|||||||||
| N | Standardized % (95% CI) | Chi-square p-value | N | Standardized % (95% CI) | Chi-square p-value | N | Standardized % (95% CI) | Chi-square p-value | |||
|
| |||||||||||
| Hearing | Yes | 10 | 24.7 (17.3–33.9) | 0.46 | 15 | 31.8 (23.9–40.9) | 0.47 | 13 | 21.9 (14.3–32.0) | 0.03 | |
| No | 168 | 21.3 (18.7–24.2) | 224 | 28.5 (25.8–31.4) | 91 | 11.6 (9.7–13.8) | |||||
| Mobility | Yes | 32 | 24.7 (18.3–32.5) | 0.31 | 36 | 34.9 (26.7–44.1) | 0.20 | 30 | 27.3 (20.1–36.0) | 0.0001 | |
| No | 146 | 20.8 (18.0–23.8) | 203 | 28.8 (26.1–31.8) | 74 | 11.0 (8.9–13.5) | |||||
| Vision | Yes | 14 | 27.6 (23.1–32.6) | 0.01 | 16 | 28.5 (20.4–38.1) | 0.91 | 9 | 9.6 (6.3–14.1) | 0.22 | |
| No | 164 | 20.4 (17.8–23.3) | 223 | 27.9 (25.2–30.8) | 95 | 12.3 (10.3–14.6) | |||||
| Self-care | Yes | 11 | 13.6 (8.2–21.8) | 0.04 | 8 | 14.6 (10.4–19.9) | <0.0001 | 10 | 13.3 (9.0–19.2) | 0.71 | |
| No | 167 | 21.4 (18.7–24.3) | 231 | 30.0 (27.3–32.8) | 94 | 12.3 (10.3–14.6) | |||||
| Cognition | Yes | 67 | 23.7 (18.9–29.2) | 0.14 | 78 | 28.1 (23.3–33.6) | 0.91 | 51 | 18.2 (14.1–23.2) | 0.0002 | |
| No | 111 | 19.1 (16.2–22.5) | 161 | 27.8 (24.7–31.1) | 53 | 8.9 (7.0–11.2) | |||||
| Living independently | Yes | 42 | 20.8 (16.2–26.3) | 0.79 | 41 | 20.2 (15.8–25.3) | 0.0001 | 35 | 18.5 (14.1–23.9) | 0.007 | |
| No | 136 | 21.6 (18.7–24.9) | 198 | 31.8 (28.7–35.0) | 69 | 11.2 (9.3–13.5) | |||||
“Yes”: woman has disability type (i.e., woman has the specific disability type only, or the specific disability type as well as other disability type(s); “No”: woman does not have disability type (i.e., woman may have no disabilities or a different disability type).
CI, confidence interval.
Prevalence of reporting concern about ability to have children was elevated among women with disabilities related to hearing, mobility, and cognition (Table 3). Compared to their counterparts, women with all disability types, except self-care and living independently, had elevated prevalence of having delayed or avoided pregnancy (range: 18.4%–28.4%); and women with disabilities related to hearing, vision, self-care, and living independently had a lower prevalence of having ever been pregnant (range: 16.4%–21.5%).
Table 3.
Report of Reproductive Health Concerns and Outcomes Among Women with Congenital Heart Defects, by Disability Type, CH STRONG, 2016–2019
| Disability type b | levels |
Reproductive health concerns and outcomes reported
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Concern about ability to have children
a
|
Delayed or avoided pregnancy because of concerns about heart health
|
Ever pregnant
|
||||||||
| N | Standardized % (95% CI) | Chi-square p-value | N | Standardized % (95% CI) | Chi-square p-value | N | Standardized % (95% CI) | Chi-square p-value | ||
|
| ||||||||||
| Hearing | Yes | 18 | 50.2 (39.4–61.0) | 0.004 | 11 | 28.4 (20.5–37.8) | 0.0008 | 4 | 16.4 (9.9–26.0) | <0.0001 |
| No | 252 | 33.4 (30.0–37.0) | 105 | 12.9 (10.7–15.5) | 262 | 36.9 (33.6—40.3) | ||||
| Mobility | Yes | 40 | 44.5 (36.1–53.1) | 0.02 | 29 | 25.6 (19.0–33.6) | 0.0008 | 32 | 31.3 (24.6–38.9) | 0.19 |
| No | 230 | 33.3 (29.7–37.0) | 87 | 12.4 (10.0–15.2) | 234 | 36.6 (33.2—40.1) | ||||
| Vision | Yes | 15 | 30.6 (21.8—41.0) | 0.52 | 10 | 22.4 (16.1–30.2) | 0.0159 | 12 | 21.5 (15.4–29.1) | 0.0002 |
| No | 255 | 33.9 (30.5–37.6) | 106 | 13.2 (11.0–15.8) | 254 | 36.2 (32.9–39.7) | ||||
| Self-care | Yes | 16 | 36.3 (28.4–45.0) | 0.70 | 12 | 17.2 (12.1–23.8) | 0.2024 | 9 | 17.8 (12.1–25.5) | <0.0001 |
| No | 254 | 34.5 (31.0–38.1) | 104 | 13.1 (10.9–15.7) | 257 | 37.3 (34.0–40.7) | ||||
| Cognition | Yes | 98 | 39.3 (32.9–46.0) | 0.03 | 51 | 18.4 (14.0–23.9) | 0.0027 | 74 | 30.9 (25.2–37.2) | 0.12 |
| No | 172 | 30.9 (27.0–35.1) | 65 | 10.1 (8–12.7) | 192 | 36.6 (32.8—40.6) | ||||
| Living independently | Yes | 60 | 34.2 (28.4–40.5) | 0.98 | 32 | 15.9 (11.8–21.1) | 0.1965 | 32 | 18.1 (13.6–23.6) | <0.0001 |
| No | 210 | 34.1 (30.3–38.2) | 84 | 12.4 (10.1–15.2) | 234 | 39.4 (35.9—43.1) | ||||
Percent of women reporting somewhat/very concerned (opposed to not at all/not very).
“Yes”: woman has the disability type; “No”: woman does not have the disability type.
Discussion
In this analysis of population-based data on almost 800 women with CHD, those with disabilities were more likely than those without disabilities to receive contraceptive counseling on safe methods, receive clinician advice to avoid pregnancy, have delayed or avoided pregnancy because of their heart, and have concern about their ability to have children; they were less likely to have ever been pregnant. In addition, women with many disability types had a higher prevalence of clinician advice to avoid pregnancy and delaying or avoiding pregnancy because of their heart, and a lower prevalence of having ever been pregnant, although some associations did not reach statistical significance. Findings were similar when women with known chromosomal anomalies were included and excluded from the sample.
Making comparisons between our findings and existing studies on contraceptive counseling among women with CHD is difficult because none has reported stratified findings by disability status. Most research on contraceptive counseling among women with CHD has been conducted at Adult CHD (ACHD) clinics, limiting generalizability of findings.7,8,15 Among participating women, between half and 83% reported any contraceptive counseling, while 25% to 46% reported contraceptive counseling specific to their heart or contraceptive counseling provided by a cardiologist or ACHD provider.7,15
These studies also reported that 12%7 and 45%8 of women had used a contraceptive method contraindicated for their heart condition. Predictors of reporting contraceptive counseling by an ACHD provider included patient non-Hispanic ethnicity and younger age.15 In two of the same studies, 65% and 67% of women with CHD reported receiving counseling on the risk of pregnancy on their heart condition, while 55% reported counseling on the risk of pregnancy on fetal health.7,8
In a systematic review of 54 studies examining contraceptive knowledge and use among women with intellectual, physical, or sensory disabilities in general, not limited to or stratified by CHD, authors found that women with disabilities used a narrower set of contraceptive methods and those with intellectual and sensory disabilities were less knowledgeable about contraception than women without disabilities.11 In CH STRONG, women with CHD and disabilities were more likely than those without disabilities to report counseling on safe contraceptive methods; however, contraceptive counseling may have been the result of clinicians more commonly advising them to avoid pregnancy.
The same systematic review also reported barriers to reproductive health-related knowledge and services experienced by women with disabilities.11 Youth with disabilities may have less access to pregnancy and contraceptive information than their peers without disabilities. Lack of plainlanguage information, information in accessible formats, negative attitudes, and discomfort in discussing sexuality by clinicians, as well as inaccessible clinics were some of the barriers to contraceptive and reproductive health services among women with disabilities.9 Over one in six women with CHD and disabilities in CH STRONG was advised to avoid pregnancy because of her heart problem. However, pregnancy is contraindicated in only a small percentage of women with CHD (e.g., those with pulmonary arterial hypertension, Eisenmenger syndrome).6
It is unknown whether the women with CHD and disabilities in CH STRONG had conditions that put them at the highest risk of adverse pregnancy outcomes; however, this finding suggests possible provider bias and need for training on guidelines on reproductive health counseling for women with CHD and disabilities. It is likely that women with CHD and disabilities experience similar barriers to reproductive health counseling and services as women with disabilities without CHD.
These CH STRONG findings have many strengths. The results are multisite population-based estimates of reproductive health counseling and concerns among almost 800 women with CHD, of whom over 4 in 10 reported disabilities. Sample size allowed for estimates overall and by disability type, as well as assessment of multiple risk factors. Standardization of prevalence estimates was used to produce population-based prevalence estimates, accounting for the CH STRONG response rate. However, this analysis also has limitations. Of CH STRONG women, 12% were excluded from the analysis due to missing data; women excluded from the analysis differed from those included by educational attainment, insurance status, proxy report, and presence of disability, specifically disabilities related to mobility, self-care, and living independently (Table 1 and Supplementary Table S1).
However, there were no statistically significant differences in reproductive health outcomes between included and excluded individuals, which may limit the impact of missing data on the estimates provided. The self- and proxy-reported survey data, including data on disabilities, were not validated among CH STRONG participants; however, the disability questions used have been validated in other populations and are the federal data standard after undergoing cognitive and field testing.14 In addition, results did not change when analyses were limited to self-reported data. We also did not have information on type of contraceptive methods used or specific content of counseling sessions or advice.
Overall, this analysis, among women of reproductive age with CHD, found differential receipt of reproductive health counseling and reproductive health outcomes by disability status. We found that among women with CHD, those with disabilities were more likely to receive contraceptive counseling on safe methods, although in both women with and without disabilities, less than one-third received contraceptive counseling. In addition, women with CHD and disabilities were more likely than those without disabilities to receive clinician advice to avoid pregnancy and have delayed or avoided pregnancy due to their CHD. Women with CHD and disabilities were less likely to have ever been pregnant. Clinical recommendations for reproductive health care for women with CHD exist, but they do not specifically mention disabilities.3,6,16,17
Efforts are critical to ensure women with disabilities, including those with CHD, receive comprehensive reproductive health care. Such measures may include information on disability in clinical guidelines, disability-related training and continuing medical education for health care providers, addressing negative attitudes and assumptions of clinicians and nonclinicians about sexuality, childbearing desires, and parenting ability of women with disabilities, making gynecology practices and materials accessible to people with disabilities, and providing evidence-based interventions to support people with disabilities.11
Supplementary Material
Acknowledgment
The authors thank Amanda Dorsey for replicating all analyses.
Funding Information
CH STRONG was funded by the Centers for Disease Control and Prevention.
Footnotes
Author Disclosure Statement
No competing financial interests exist.
Data Sharing Statement
CH STRONG data are available to external scientists when sponsored by a principal investigator. Contact Sherry Farr at sfarr@cdc.gov more information.
References
- 1.Gilboa SM, Devine OJ, Kucik JE, et al. Congenital Heart Defects in the United States: Estimating the Magnitude of the Affected Population in 2010. Circulation 2016;134:101–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Downing KF, Tepper NK, Simeone RM, et al. Adverse pregnancy conditions among privately insured women with and without congenital heart defects. Circ Cardiovasc Qual Outcomes 2020;13:e006311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canobbio MM, Warnes CA, Aboulhosn J, et al. Management of Pregnancy in Patients With Complex Congenital Heart Disease: A Scientific Statement for Healthcare Professionals From the American Heart Association. Circulation 2017;135:e50–e87. [DOI] [PubMed] [Google Scholar]
- 4.Abarbanell G, Tepper NK, Farr SL. Safety of contraceptive use among women with congenital heart disease: A systematic review. Congenit Heart Dis 2019;14:331–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindley KJ, Bairey Merz CN, Asgar AW, et al. Management of women with congenital or inherited cardiovascular disease from pre-conception through pregnancy and postpartum: JACC focus seminar 2/5. J Am Coll Cardiol 2021;77:1778–1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stout KK, Daniels CJ, Aboulhosn JA, et al. 2018 AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73:e81–e192. [DOI] [PubMed] [Google Scholar]
- 7.Hinze A, Kutty S, Sayles H, et al. Reproductive and contraceptive counseling received by adult women with congenital heart disease: A risk-based analysis. Congenit Heart Dis 2013;8:20–31. [DOI] [PubMed] [Google Scholar]
- 8.Kovacs AH, Harrison JL, Colman JM, et al. Pregnancy and contraception in congenital heart disease: What women are not told. J Am Coll Cardiol 2008;52:577–578. [DOI] [PubMed] [Google Scholar]
- 9.Vigl M, Kaemmerer M, Seifert-Klauss V, et al. Contraception in women with congenital heart disease. Am J Cardiol 2010;106:1317–1321. [DOI] [PubMed] [Google Scholar]
- 10.Downing KF, Oster ME, Klewer SE, et al. Disability Among Young Adults With Congenital Heart Defects: Congenital Heart Survey to Recognize Outcomes, Needs, and Well-Being 2016–2019. J Am Heart Assoc 2021;10:e022440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horner-Johnson W, Moe EL, Stoner RC, et al. Contraceptive knowledge and use among women with intellectual, physical, or sensory disabilities: A systematic review. Disabil Health J 2019;12:139–154. [DOI] [PubMed] [Google Scholar]
- 12.Bloom TL, Mosher W, Alhusen J, et al. Fertility Desiresand Intentions Among U.S. Women by Disability Status: Findings from the 2011–2013 National Survey of Family Growth. Matern Child Health J 2017;21:1606–1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farr SL, Klewer SE, Nembhard WN, et al. Rationale anddesign of CH STRONG: Congenital Heart Survey To Recognize Outcomes, Needs, and well-beinG. Am Heart J 2020;221:106–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Department of Health and Human Services. Implementation of Guidance on Data Collection Standards for Race, Ethnicity, Sex, Primary Language, and Disability Status: Office of the Assistant Secretary for Planning and Evaluation: US; 2011:1–10. [Google Scholar]
- 15.Miner PD, Canobbio MM, Pearson DD, et al. Contraceptive practices of women with complex congenital heart disease. Am J Cardiol 2017;119:911–915. [DOI] [PubMed] [Google Scholar]
- 16.American College of Obstetricians and Gynecologists’ Presidential Task Force on Pregnancy and Heart Disease and Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 212: Pregnancy and Heart Disease. Obstet Gynecol; 2019;133:e320–e356. [DOI] [PubMed] [Google Scholar]
- 17.American College of Obstetricians and Gynecologists’ Committee on Adolescent Health Care. Gynecologic Considerations for Adolescents and Young Women With Cardiac Conditions: ACOG Committee Opinion, Number 813. Obstet Gynecol; 2020;136:e90–e99. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
CH STRONG data are available to external scientists when sponsored by a principal investigator. Contact Sherry Farr at sfarr@cdc.gov more information.


